Inflammatory Bowel Diseases Ulcerative Colitis Crohns disease Are
Inflammatory Bowel Diseases

Ulcerative Colitis & Crohns disease Í Are chronic inflammatory bowel diseases with protracted relapsing & remitting coarse. Í The incidence of ( IBD ) vary between population. Í The incidence of UC is 10/ 100000, while CD is 5 -7/100000. Í CD & UC had 2 peaks 1 st in young & 2 nd in 7 th decade.

Factors associated with the development of (IBD) Genetic: o o o More common in Jews. 10% have + ve FH of IBD. High concordance between identical twins. Associated with autoimmune thyroiditis & SLE. Four regions of linkage on chromosomes 16, 12, 6 & 14 (IBD 1 -4 ). o HLA-DR 103 associated with sever UC. o UC & CD with HLA-B 27 commonly develop ankylosing spondylitis.
Environmental: o UC is more common in non-smokers & exsmokers. o CD most patients are smokers. o Associated with low residue , high refined sugar diet. o Appendicectomy protects against UC.

Pathogenesis Of IBD TRIGGER e. NTEROCYTES MACROPHAGES tnf SYS. SYM. IL. 1 ADHESION MOLECULE NEUTROPHIL AGREGGATION Fibroblast activation Fibrosis INFLAMMATION Stim. cd 4 IL 8 Mast & plasma cell activation ACTIVATION OF NEUTROPHILS
Common patterns of IBD distribution: Ulcerative colitis: - 40 -50% proctitis or proctosigmoiditis. - 30 -40% left sided colitis or extensive colitis. - 20% pan colitis.

, Crohns disease: - 40% Ileal or ileocolonic. - 30 -40% small intestinal. - 20% Crohns colitis. - <10% perianal disease (alone).
Histopathology of IBDS v. Ulcerative Colitis: -- The inflammatory process is limited to the mucosa. Acute & chronic inflammatory cells infiltrate the lamina propria & crypts ( Cryptitis ). Crypt abscesses are typical. -- Distorted Goblet cell which loss its mucus. -- Dysplasia : increased mitotic rate + nuclear atypia which herald the development of Ca colon.

v. Crohn , s disease: --The whole wall of the intestine is oedematous & thickened , There are deep ulcers which appear as linear fissures with normal mucosa between them ( cobblestone). -- Fistulae & ulcers. -- The lesion is patchy ( skip lesion ). -- Chronic inflammatory cell infiltrate the whole layers -- Microgranuloma (aggregate of histeocytes which surrounded by lymphocytes & contain giant cells). -- Aphthus ulcer.
Clinical features of IBDS Ulcerative Colitis: -- The 1 st attack is most severe. -- Characterized by relapse & remission. -- Rarely chronic unremitting coarse.
Precipitating factors for acute relapse: Ø Gastroenteritis. Ø Antibiotic. Ø NSAIDS. Ø Emotional stress. Ø Intercurrent infection.
ÍProctitis: Rectal bleeding & mucous discharge some times with tenesmus , no constitutional symptoms. ÍProctosigmoiditis: bloody diarrhea with mucous , Small no. of patients with v. active limited disease develop fever, lethargy & abdominal discomfort. ÍExtensive colitis: bloody diarrhea with passage of mucous, in sever cases anorexia , nausea , weight loss & abdominal pain , patient is toxic with fever & tachycardia & signs of peritoneal inflammation.
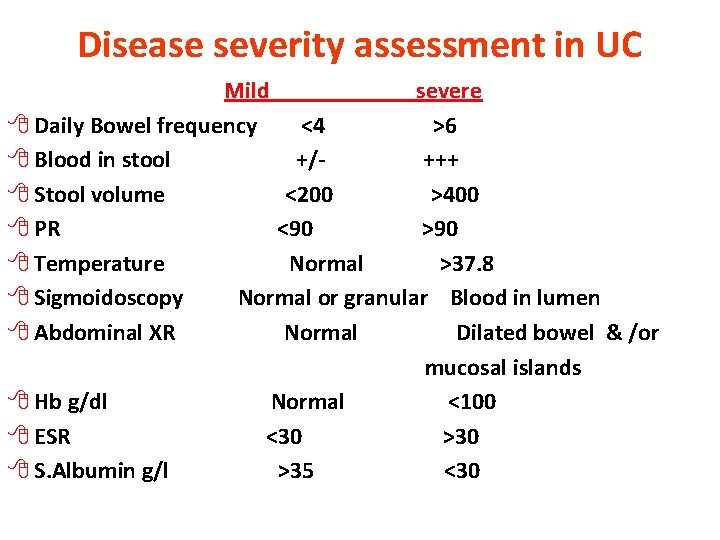
Disease severity assessment in UC Mild severe 8 Daily Bowel frequency <4 >6 8 Blood in stool +/+++ 8 Stool volume <200 >400 8 PR <90 >90 8 Temperature Normal >37. 8 8 Sigmoidoscopy Normal or granular Blood in lumen 8 Abdominal XR Normal Dilated bowel & /or mucosal islands 8 Hb g/dl Normal <100 8 ESR <30 >30 8 S. Albumin g/l >35 <30
Crohn , s disease: Ileal involvement: Abdominal pain which is associated with watery diarrhea (with out blood & mucous) + weight loss + features of protein & vitamines deficiencies. Crohn , s colitis: Like ulcerative colitis. *** Rectal sparing + Perianal disease*** Small bowel & colonic disease. Isolated Perianal disease. Severe oral ulceration.
Differences between UC & CD Ø 1 -UC involve only the colon while CD involve any part of GIT. Ø 2 -UC is continuous while CD is patchy. Ø 3 -Rectum is always involved in UC while rectal sparing in CD. Ø 4 -Histology: UC is superficial while CD affect all intestinal layers. Ø 5 -Pathology: UC there is Cryptitis & Crypt abscess While CD there is granuloma. Ø 6 -Presence of fistulae in CD > UC. Ø 7 -Presence of Perianal lesions in CD > UC. Ø 8 -Clinical presentation: bloody diarrhea in UC while in CD abdominal pain , wt. loss. Ø 9 -UC is more in non/ex-smoker while CD more in smokers. Ø 10 -Surgery is curative in UC & not in CD.
Complications of IBD v. Intestinal : § Severe colitis. § Perforation. § Hemorrhage. § Toxic megacolon. § Fistula. § Cancer of the colon.
v. Extra intestinal: § Seronegative arthritis & Sacroilitis/Ankylosing spondylitis. § Ocular: *Conjunctivitis , *Iritis , *Episcleritis. § * Mouth ulcers. § Hepatic. *Fatty liver, Sclerosing cholangitis & cholangiocarcinoma, *Liver abscess & *portal pyemia § Renal. Amyloidosis & Oxalate calculi § Vascular. *DVT, *Mesenteric or *portal vein thrombosis § *Erythema nodosum, *Pyoderma gangrenosum. .
Differential diagnosis of IBD FD. D of UC & Crohn , s colitis: v. Infective: § Bacterial: Salmonella, Shegella , Campylobacter pylori § Viral: Herpes simplex proctitis, Cytomegalovirus. § Protozoal: Amoebaiasis.
v. Non-Infective: § Vascular: Ischemic colitis, Radiation proctitis. § Idiopathic: Collagenous colitis. § Drugs: NSAIDs. § Neoplastic: Colonic carcinoma. § Other: Diverticulitis.
FD. D of small bowel CD: v. Other causes of right iliac fossa mass. Ø Caecal carcinoma Ø Appendicular mass Ø Infection ( TB , Yesinia , Actinomycosis ) v. Mesenteric adenitis. v. Pelvic inflammatory disease. v. Lymphoma.
Investigations of IBDs. z. Blood tests: HB, WBC , ESR, CRP, S. albumin. z. Bacteriology: Stool microscopy, culture, clostridium difficil toxin. Bl. Culture & serology.
Endoscopy: Indications for endoscopy: o Disease extent. o Stricture ( biopsy ). o Filling defect. o Differentiation between UC & CD. o For follow up: Random biopsies for dysplasia or cancer for UC > 8 ys. z. Radiolog: --Barium studies. MRI, Plain X-Ray of abdomen, US

Drugs used in treatment of IBDs Aminosalysilates: (( Mesalasine, Olsalazine , Balsalazide)) Modulate cytokine release from mucosa Delivered to the colon by: 1 -PH-dependent ( Asacol ) 2 -Time-dependent ( Pentasa ) 3 -Bacterial breakdown by colonic bacteria from carrier molecule ( Sulfasalazine, Olsalazine, Balsalized ).
Corticosteroid Prednisolon , Hydrocortisone , Budesonide. Anti-inflammatory ( topical, oral or I. V) Thiopurines: Azothiopurine , 6 -mercaptopurine Immunomodulation by inducing T-cell apoptosis. Is effective in 6 -8 ws after starting therapy.
Methotrexate • Anti-inflammatory • SE: Intolerance in 10 -18%, nausea , stomatitis, hepatotoxicity & pneumonitis. Infliximab: Chimeric anti-TNF monoclonal AB. Given as I. V infusion 4 -8 weekly. Induce apoptosis of inflammatory cells Uses: Moderately-severely active CD especially fistulating. Sever active UC. Ø Anaphylactic reaction after multiple infusions. Ø Contraindicated in presence of infection. • •
Ciclosporine v. Suppression of T cell expansion. v. As rescue therapy to prevent surgery in UC responding poorly to corticosteroid. v. No value in CD. SE: -Nephrotoxicity. -Neurotoxicity. -Hirsutism.
Antibiotics Antibacterial. Useful in perianal CD. SE: Peripheral neuropathy in long term metronidazole. Antidiarrhoeal agents: ( Codeine phosphate , Loperamide , lomotil) Avoided in moderately or severe active UC may precipitate colonic dilatation.
Treatment of IBDs Treatment of Ulcerative Colitis: q. Treatment of acute attacks( Induction of remission ). q. Prevent relapses (Maintenance ). Sulfasalasine, Aminosalysilate. q. Detect carcinoma at early stage. q. Select patients for surgery.

• Active Proctitis: In mild to moderate disease: Mesalazine enema or suppositories combined with oral mesalazine. Topical corticosteroids are less effective& are used for patients who are intolerant of topical mesalazine. Patients who fail to respond are treated with prednisolone 40 mg daily.
Active left-sided or extensive ulcerative colitis: o In mildly active cases: High dose Aminosalysilate Topical aminosalicylat & Corticosteroid o Oral prednisolon 40 mg for more active disease & if no response to topical therapy. Sever UC: Admission& managed by physician, surgeon. 1 -Clinically: for presence of abd. Pain, Temp. , PR , stool bl. & frequency. 2 -Lab. : Hb% , WBC count , Alb. , Electrolytes , ESR & CRP. 3 -Radiologically: For colonic dilatation on plain abd.
Medical management of fulminant UC 1 -I. V fluid. 2 -Transfusion if Hb< 10 gm/L. 3 -I. V methylprednisolone ( 60 mg daily ) or Hydrocortisone. 4 -Antiboitic for proven infection. 5 -Nutritional support. 6 -Subcutanous heparin for prophylaxis of venous thromboembolism. 7 -Avoidance of Opiates & Antidiarrhoeal agents. 8 -I. V Ciclosporine ( 2 mg/kg) or Infliximab ( 5 mg/kg ) in stable patient not responding to steroid 3 -5 days
Indication for Urgent Colectomy Colonic dilatation >6 cm on plain abdominal X-Ray. Lab. & Clinical deterioration. No response after 7 -10 days.
Indications for Colectomy Impaired quality of life. -Loss of occupation or education. -Disruption of family life. Failure of medical therapy. -Dependence on corticosteroids. -Complications of drug therapy.
Indications for Colectomy Fulminant colitis. Disease complications unresponsive to medical therapy. -Arthritis. -Pyoderma Gangerinosum. Colon cancer or severe dysplasia.
Maintenance of remission in UC: -Life-long treatment for all patients with extensive disease & distal disease with more than once per year relapse. -Oral Aminosalysilate ( Mesalasine or Balsalazide ) or Salazopyrine ( for patients with arthropathy ). v If no response Thiopurine.
Medical treatment of CD Active Colitis or Iliocolitis: Like UC ( AS + Steroid ). Isolated Ileal: Corticosteroid( Budesonide) if no response surgery. Anti-TNF AB (Infliximab) : v. I. V infusion 4 -8 weekly on 3 occasions induce remission in patients with CD at any site of GIT v. For refractory cases to steroid. v. Heals enterocutanous fistulae & maintains longer remissions.
v. Effective in the management of Pyoderma gangerosum & arthritis. v. It is contraindicated in presence of infection like TB. v. Relapse occur after 12 weeks so combine with Disease modifying drugs like methotrexate or thiopurine. v. It cause remarkable mucosal healing---- scaring & stricturing so used with caution in stenosing disease.
Extensive & diffuse iliocolonic: Drug therapy +Nutritional (Prolonged Parantral Nutrition )+Surgical Intervention +Endoscopic Balloon dilatation. Fistulating & Perianal disease: Ø -Metronidazol or Ciprofloxacin. Ø -Localize fistula by Ba. radiography , CT , MRI. Ø -Surgical treatment. Ø -Corticosteroid & nutritional therapy ( TPN ). Ø -Thiopurine for chronic disease. Ø -Infliximab infusion 4 -8 weekly.
Maintenance of remission in CD: 1 -Smoking cessation. 2 -Aminosalysilate have minimal efficacy. 3 -Patients with relapse more than once per year: Thiopurine. 4 -If patient intolerant to thiopurine or 6 mercaptopurine then use once weekly methotrexate + Folic acid. 5 -More severe & aggressive disease: Combined immunomodulating agents + Infliximab.
- Slides: 39