Inflammatory Bowel Diseases Crohns Disease and Ulcerative Colitis
Inflammatory Bowel Diseases Crohn’s Disease and Ulcerative Colitis Bruce Yacyshyn, MD Professor of Medicine University of Cincinnati office: 558 -5244

Specific IBD syndromes • • • Proctitis Proctosigmoiditis Left-sided ileitis Ileocolitis These behave as separate diseases but are grouped as either Ulcerative Colitis or Crohn’s

Endoscopic Features of Ulcerative Colitis (reproduced with permission, Schiller et al, 1986)
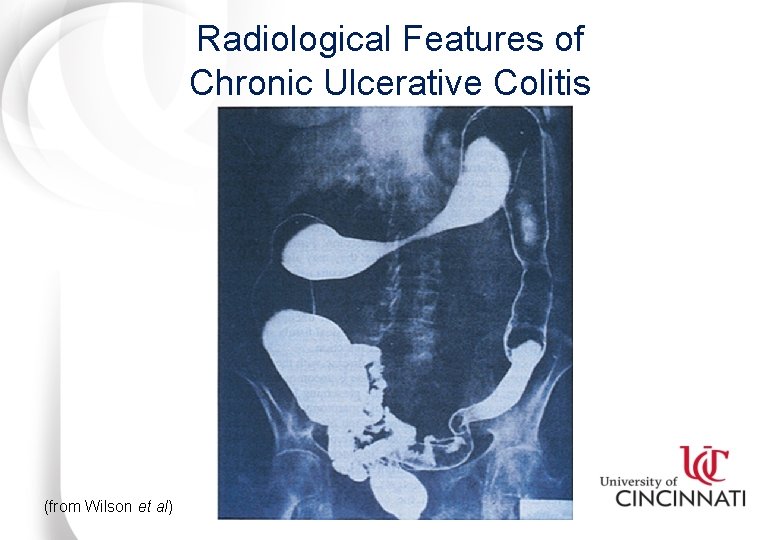
Radiological Features of Chronic Ulcerative Colitis (from Wilson et al)
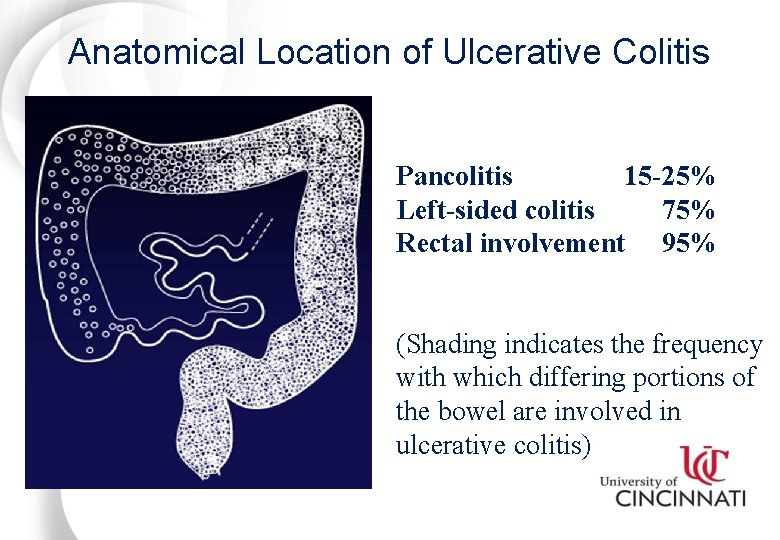
Anatomical Location of Ulcerative Colitis Pancolitis 15 -25% Left-sided colitis 75% Rectal involvement 95% (Shading indicates the frequency with which differing portions of the bowel are involved in ulcerative colitis)
Intestinal Complications of Ulcerative Colitis • • • Fibrosis Shortening of the colon Bleeding Stricture Bowel perforation Toxic megacolon
Systemic Complications of Ulcerative Colitis v Arthritis - RF negative peripheral polyarthritis(types 1 and 2) v Ankylosing spondylitis (HLA-B 27+) v Iritis/episcleritis, uveitis (HLA-27+) v Erythema nodosum v Pyoderma gangrenosum v (PSC) primary sclerosing cholangitis-watch for alkaline phosphatase 2 X ULN-HLA-B*+ v Aphthous stomatitis v Thromboembolic disorders
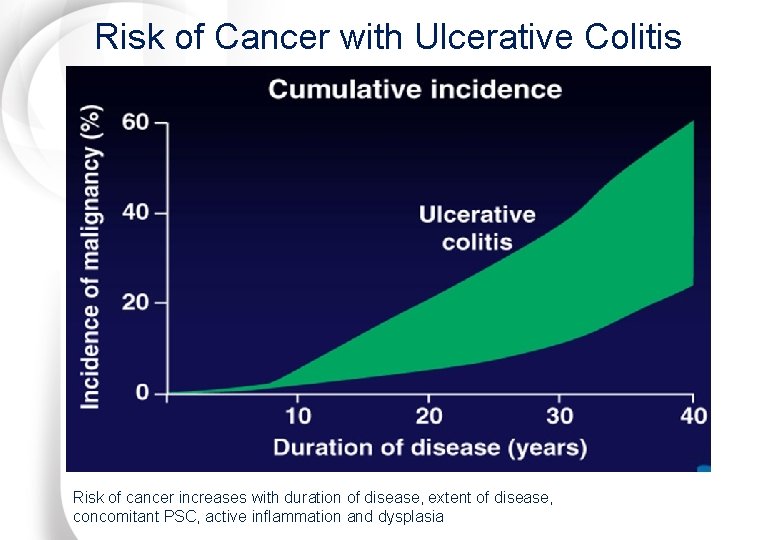
Risk of Cancer with Ulcerative Colitis Risk of cancer increases with duration of disease, extent of disease, concomitant PSC, active inflammation and dysplasia
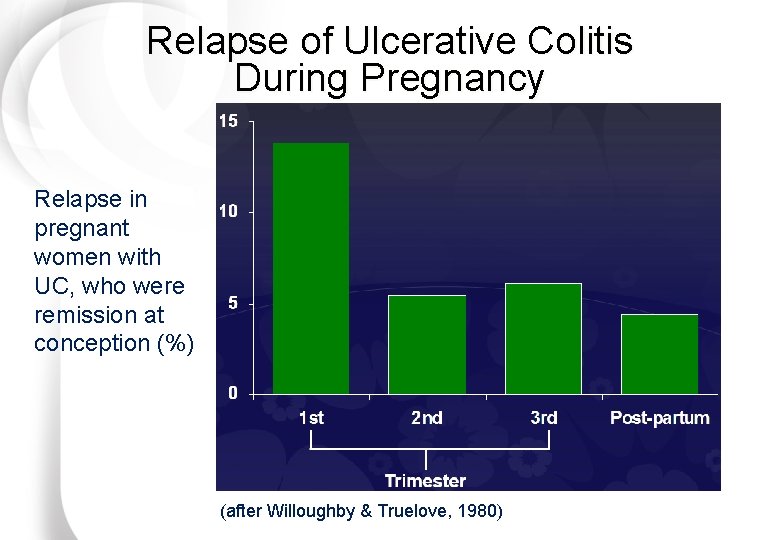
Relapse of Ulcerative Colitis During Pregnancy Relapse in pregnant women with UC, who were remission at conception (%) (after Willoughby & Truelove, 1980)
Clinical Presentation of Ulcerative Colitis Ø Bloody diarrhea Ø Fever Ø Cramping abdominal pain Ø Weight loss Ø Frequency and urgency of defecation Ø Tenesmus (feeling of incomplete evacuation) Ø General malaise
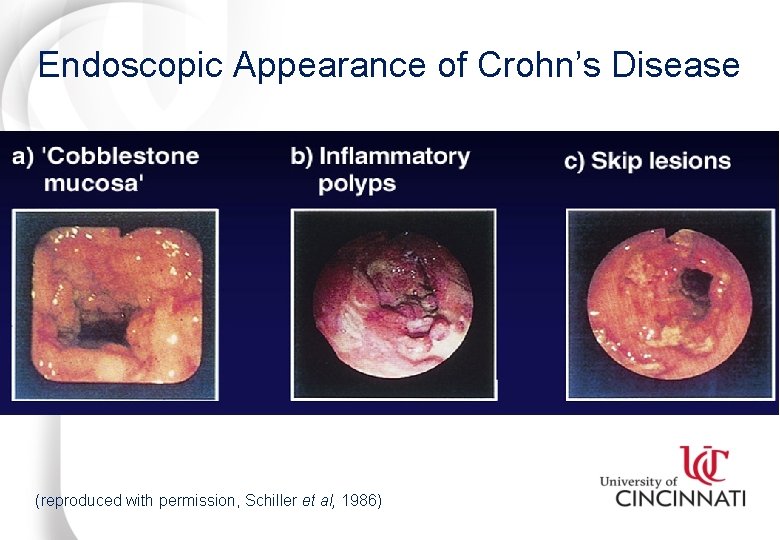
Endoscopic Appearance of Crohn’s Disease (reproduced with permission, Schiller et al, 1986)

Radiological Features of Crohn’s Disease (reproduced with permission from Mc. Graw-Hill) (courtesy of Dr. Sten Norby Rasmussen, Denmark)
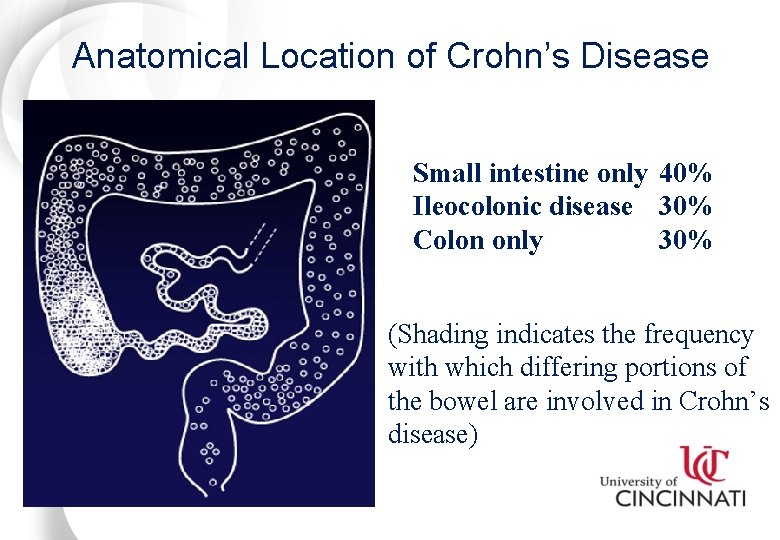
Anatomical Location of Crohn’s Disease Small intestine only 40% Ileocolonic disease 30% Colon only 30% (Shading indicates the frequency with which differing portions of the bowel are involved in Crohn’s disease)
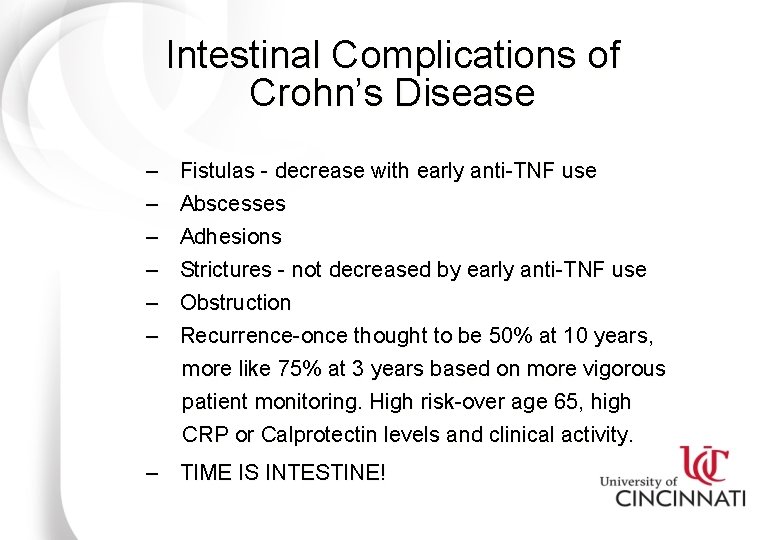
Intestinal Complications of Crohn’s Disease – – – Fistulas - decrease with early anti-TNF use Abscesses Adhesions Strictures - not decreased by early anti-TNF use Obstruction Recurrence-once thought to be 50% at 10 years, more like 75% at 3 years based on more vigorous patient monitoring. High risk-over age 65, high CRP or Calprotectin levels and clinical activity. – TIME IS INTESTINE!
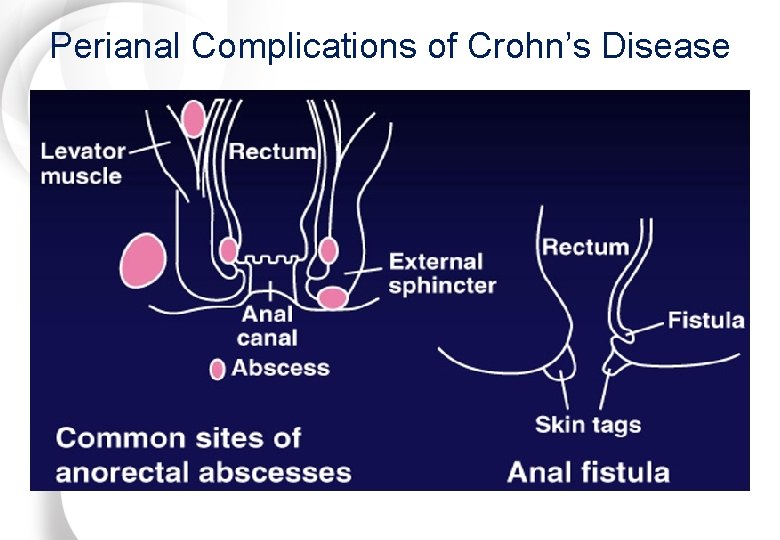
Perianal Complications of Crohn’s Disease
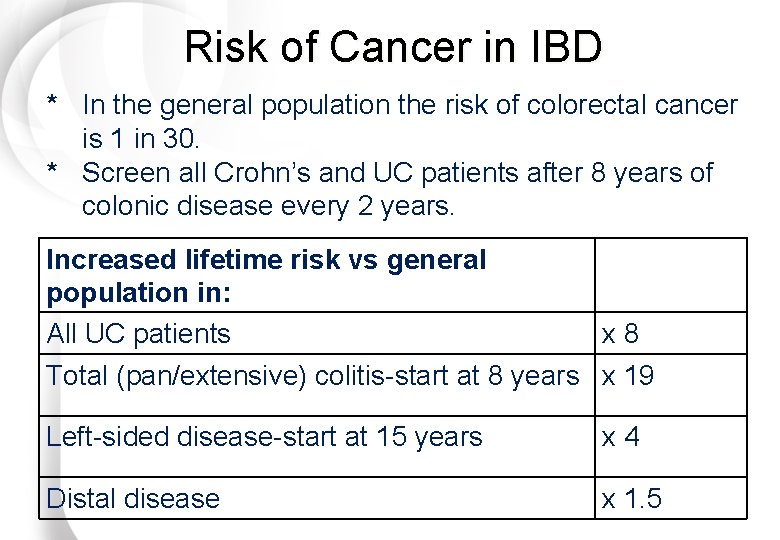
Risk of Cancer in IBD * In the general population the risk of colorectal cancer is 1 in 30. * Screen all Crohn’s and UC patients after 8 years of colonic disease every 2 years. Increased lifetime risk vs general population in: All UC patients x 8 Total (pan/extensive) colitis-start at 8 years x 19 Left-sided disease-start at 15 years x 4 Distal disease x 1. 5
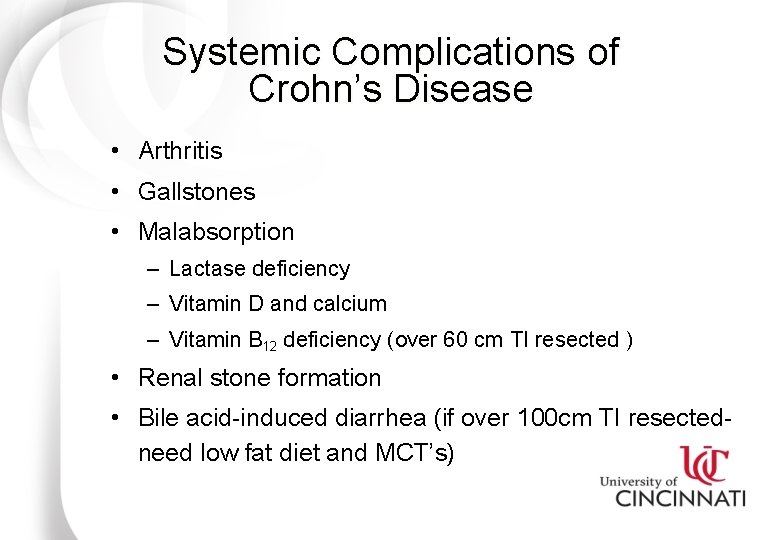
Systemic Complications of Crohn’s Disease • Arthritis • Gallstones • Malabsorption – Lactase deficiency – Vitamin D and calcium – Vitamin B 12 deficiency (over 60 cm TI resected ) • Renal stone formation • Bile acid-induced diarrhea (if over 100 cm TI resectedneed low fat diet and MCT’s)
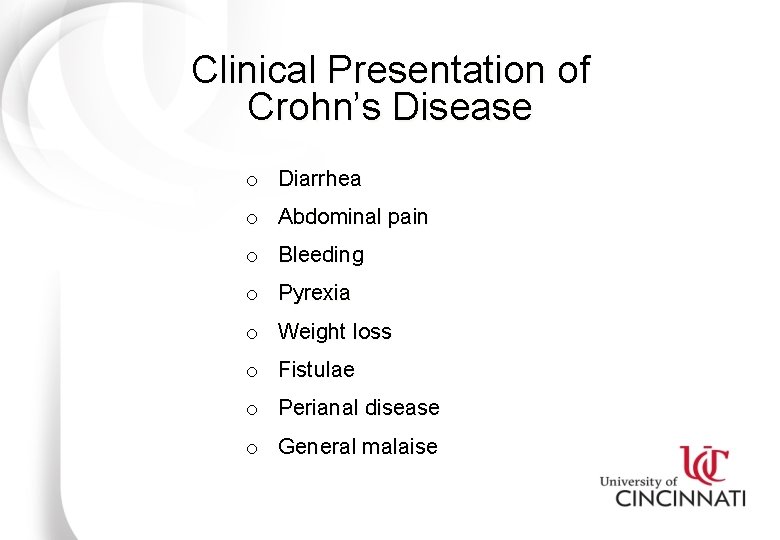
Clinical Presentation of Crohn’s Disease o Diarrhea o Abdominal pain o Bleeding o Pyrexia o Weight loss o Fistulae o Perianal disease o General malaise
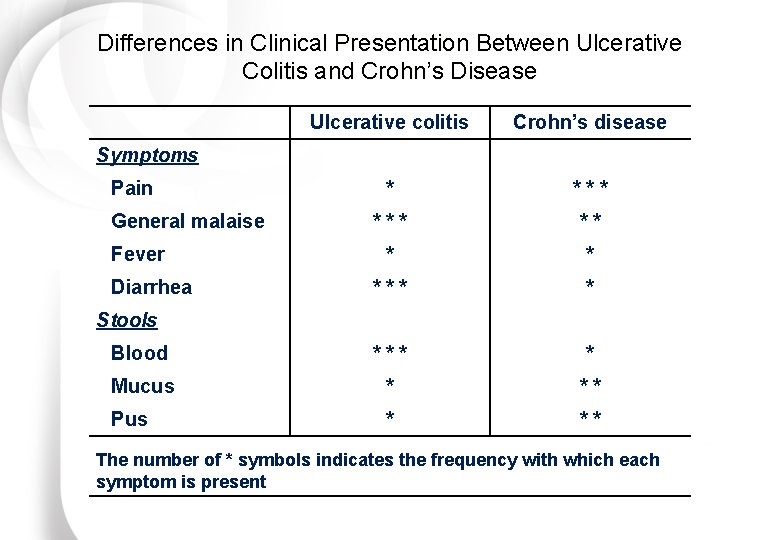
Differences in Clinical Presentation Between Ulcerative Colitis and Crohn’s Disease Ulcerative colitis Crohn’s disease * *** ** * * *** * Blood *** * Mucus * ** Pus * ** Symptoms Pain General malaise Fever Diarrhea Stools The number of * symbols indicates the frequency with which each symptom is present
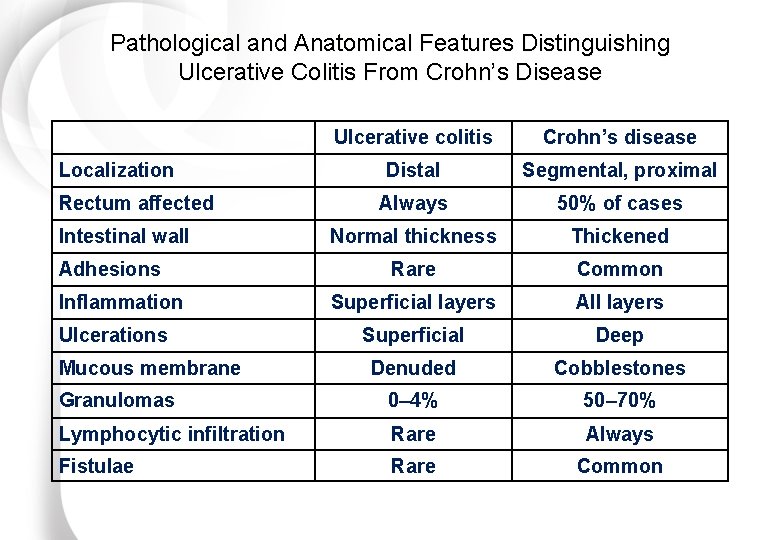
Pathological and Anatomical Features Distinguishing Ulcerative Colitis From Crohn’s Disease Ulcerative colitis Crohn’s disease Distal Segmental, proximal Always 50% of cases Normal thickness Thickened Rare Common Superficial layers All layers Superficial Deep Denuded Cobblestones Granulomas 0– 4% 50– 70% Lymphocytic infiltration Rare Always Fistulae Rare Common Localization Rectum affected Intestinal wall Adhesions Inflammation Ulcerations Mucous membrane
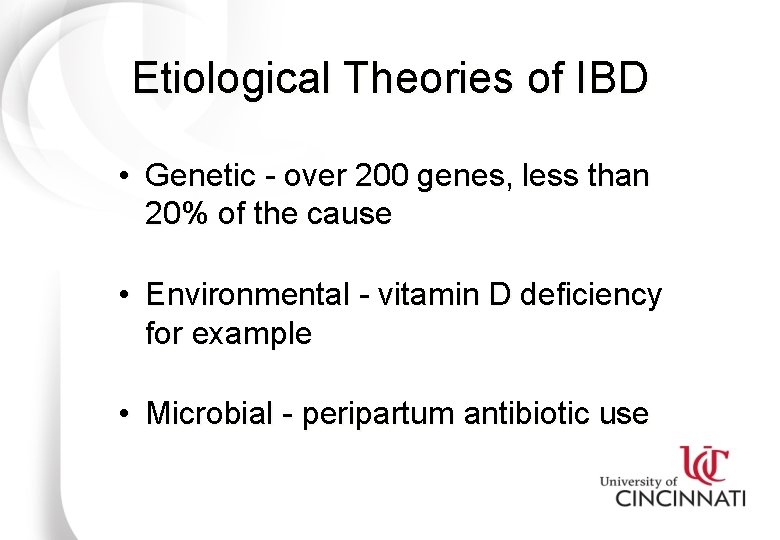
Etiological Theories of IBD • Genetic - over 200 genes, less than 20% of the cause • Environmental - vitamin D deficiency for example • Microbial - peripartum antibiotic use
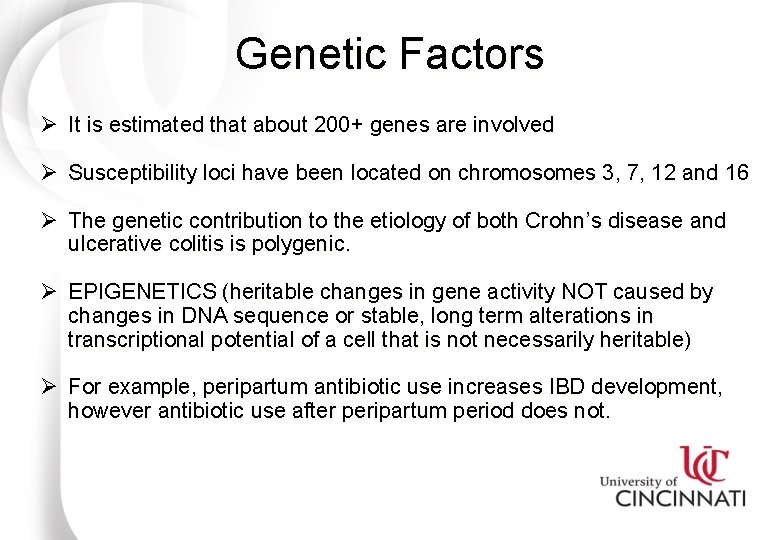
Genetic Factors Ø It is estimated that about 200+ genes are involved Ø Susceptibility loci have been located on chromosomes 3, 7, 12 and 16 Ø The genetic contribution to the etiology of both Crohn’s disease and ulcerative colitis is polygenic. Ø EPIGENETICS (heritable changes in gene activity NOT caused by changes in DNA sequence or stable, long term alterations in transcriptional potential of a cell that is not necessarily heritable) Ø For example, peripartum antibiotic use increases IBD development, however antibiotic use after peripartum period does not.
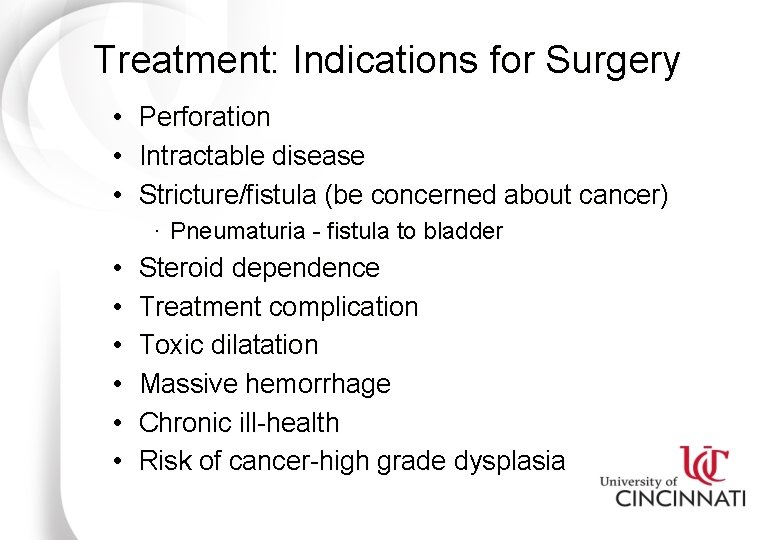
Treatment: Indications for Surgery • • • Perforation Intractable disease Stricture/fistula (be concerned about cancer) · Pneumaturia - fistula to bladder • • • Steroid dependence Treatment complication Toxic dilatation Massive hemorrhage Chronic ill-health Risk of cancer-high grade dysplasia
Pharmacological Treatment of IBD Ø 5 -ASA-containing compounds • Mesalazine and others, 75% response and 30% remission Ø Corticosteroids - mineralocorticoids, first pass metabolized steroids - (budesonide). Ø Short term use only. NOT definitive therapy. Ø Immunosuppressants 6 -MP, azathioprine - (caution in young males), Methotrexate - for combination use not for maintenance. Ø Anti-TNF agents (infliximab, adulimumab, certilizumab, biosimilars of these agents) Ø Anti-adhesion molecule targets (Integrins - mucosal addressins) Ø IL 17/23 -Ustekinumab Ø Non approved - new drugs in clinical investigation: JAK - (approval expected March 18, 2018 for UC) & pulse FMT-bacterial therapy.
Other Medical Complications of IBD q Osteoporosis – very common in Crohn’s disease, may be exacerbated by medications, supplement all patients with Vitamin D and calcium, test vitamin d levels q Medications such as steroids, chronic disease and vitamin D deficiency can exacerbate
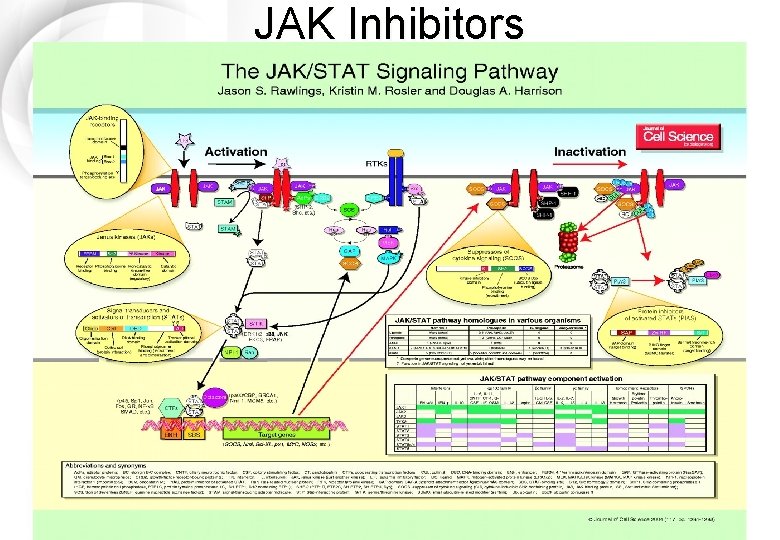
JAK Inhibitors
JAK Inhibitor for UC - Tofacitinib • Targets IL 4, IL 12, IL-23, interferon gamma • 4 JAK members that interact with specific combinations of signal transducers and cytokine receptors • Tofacitinib interacts with all 4 • FDA decision pending for UC tentatively March, 2018 • FDA approval for moderate to severe RA in 2012 • Dose is 10 mg bid • Watch for changes in lipids and cholesterol
Vignette 1: A patient with Crohn’s undergoes resection of 50 cm of TI for structuring disease. He subsequently develops voluminous diarrhea. Answer: This is bile salt diarrhea. Bile salts are normally reabsorbed in the terminal ileum. Pick the best answer from the following options: Even minimal resection of the TI can affect bile salt resorption. As bile salts stay intraluminally, they pass into the colon in higher than normal concentrations. A) Small intestinal bacterial overgrowth (SIBO) diarrhea Once in the colon, bile salts irritate the colonic mucosa and lead to a secretory diarrhea. When up to 100 cm of TI is removed, bile salt dumping occurs and B) C. difficile colitis diarrhea may ensue. When more than 100 cm is removed, there is virtually no ability to resorb bile salts, so the salts become totally depleted–there is none left to C) Fat malabsorption even dump into the colon. In this case there is a fat malabsorption and steatorrhea. So, both salt instances (<100 vs >100 cm resected) there is diarrhea, but the D) in. Bile diarrhea mechanism is different. When <100 cm is resected, the diarrhea is from a secretory diarrhea due to bile salt dumping. When >100 cm is resected, the E) 5 -ASA (mesalamine) diarrhea is from fat malabsorption. The former condition is treated with cholestyramine, and the latter with medium chain triglycerides.
Vignette 2: A patient with Crohn’s undergoes resection of 120 cm of TI for structuring disease. He subsequently develops voluminous diarrhea. Pick the best answer from the following options: Answer: This is fat malabsorption. Treatment is with a medium A) Small intestinal bacterial overgrowth (SIBO)chaindiarrhea triglyceride. B) C. difficile colitis C) Fat malabsorption D) Bile salt diarrhea E) 5 -ASA (mesalamine) diarrhea
Vignette 3: A patient with Crohn’s colitis develops worsening of diarrhea after beginning therapy with a mesalamine (5 ASA) dimer. Answer: Pick the best answer from the following options: This is likely 5 -ASA-induced diarrhea. Although 5 -ASA A) Small intestinal bacterial compounds are often used to treatovergrowth colitis-related(SIBO) diarrhea, diarrhea they can, themselves, induce diarrhea. In particular, the 5 -ASA dimer B) C. difficile colitis products are most prone to cause diarrhea (up to 1 in 5 patients C) Fatthis malabsorption suffers adverse event from 5 -ASA dimers). They have fallen out of favor for just this reason. D) Bile salt diarrhea E) 5 -ASA (mesalamine) diarrhea
Vignette 4: Patient with Crohn’s colitis develops severe diarrhea, fevers, and leukocytosis after starting metronidazole for perianal fistulizing disease. Answer: Pick the best answer from the following options: This is likely C. difficile colitis. As a general principle, IBD flares A) Small intestinal (SIBO) diarrhea should always prompt abacterial search forovergrowth underlying infection. In this case, patient developed B) C. the difficile colitis new-onset diarrhea after receiving metronidazole–a classic C. difficile culprit. C. difficile has become C) Fat malabsorption more and more prevalent, so it should always be high on the differential for anyone with diarrhea after antibiotics, IBD or no D) Bile salt diarrhea IBD. E) 5 -ASA (mesalamine) diarrhea
Vignette 5: Patient with fibrostenotic Crohn’s disease limited to the small intestine develops progressive bloating, abdominal discomfort, and diarrhea in the setting of an elevated folate level and a depressed vitamin B 12 level. Answer: Pick the best answer from the following options: This is small intestinal bacterial overgrowth (SIBO). Because SIBO A) Small intestinal bacterial overgrowth (SIBO) diarrhea has gained lots of attention in recent years, it is worth spending an extra to colitis review the definition, associations, diagnostic B) C. moment difficile testing strategies, and treatment of SIBO is marked by an C) Fat malabsorption abnormal displacement of colonic type flora into the small intestine, including gram-negative D) Bile salt diarrhea organisms, enterococcus, and anaerobes. SIBO is classically E) 5 -ASA (mesalamine) diarrhea
Vignette 5 Answer continued: classically associated with a range of conditions affecting small intestinal motility, structure, or immunity, including abdominal surgeries, diabetes, achlorhydria, scleroderma, ileocecal incompetence, and, as seen here, inflammatory bowel disease (especially when there is structuring). SIBO characteristically leads to the curious combination of low B 12 and high folate. This occurs because the bacteria consume cobalamin (B 12) and produce folate as a byproduct. Because SIBO can lead to a range of bothersome symptoms and sequelae (diarrhea, constipation, bloating, gas, abdominal pain, cobalamin deficiency, malabsorption, etc. ), efforts have been made to develop accurate diagnostic tests to allow timely identification and treatment.
Vignette 5 Answer continued: Breath Hydrogen testing for SIBO: Lactulose hydrogen breath testing (LHBT), in particular, has been advocated as the optimal method, since lactulose is not absorbed and thus remains eligible for fermentation in the distal small bowel. In contrast, glucose can be absorbed proximally, so distal SIBO may not be detected as readily with this agent. Importantly, HBT does not require knowledge of the full taxonomy of bowel flora.
Vignette 5 Answer continued: Treatment of SIBO is typically with a single 7 to 10 day course of an appropriate antibiotic, such as tetracycline, neomycin, norfloxaxin, or rifaximin, among others. Of course, where possible, the underlying condition should be treated as well. In this case, there is stasis related to small intestinal strictures, so surgery might ultimately be warranted.
Rule Out Infectious Causes of Colitis C. difficile- most important rule out E. coli 0157: H 57 Shigella Salmonella Yersinia Campylobacter-chronic relapsing course E. histolitica (amebiasis) Think about CMV especially in immunosuppressed
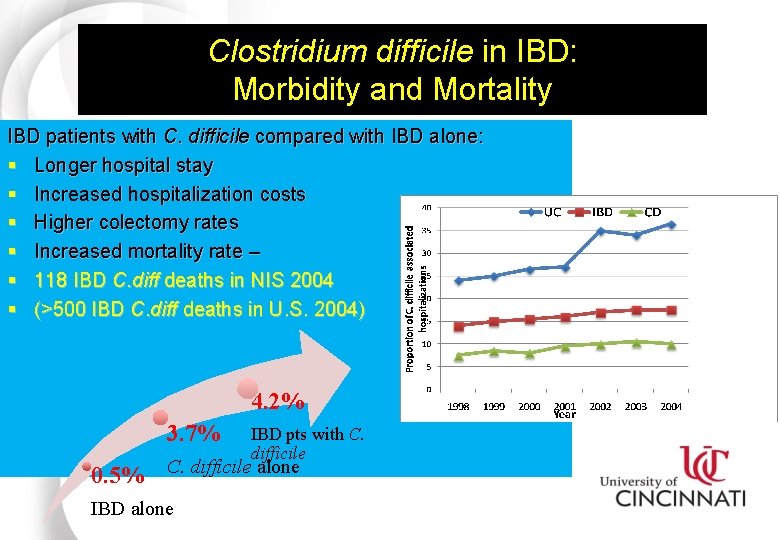
Clostridium difficile in IBD: Morbidity and Mortality IBD patients with C. difficile compared with IBD alone: § Longer hospital stay § Increased hospitalization costs § Higher colectomy rates § Increased mortality rate – § 118 IBD C. diff deaths in NIS 2004 § (>500 IBD C. diff deaths in U. S. 2004) 4. 2% 3. 7% IBD pts with C. difficile 0. 5% C. difficile alone IBD alone Ananthakrishnan, et al. Gut, 2008. 57(2): p. 205 -10.
- Slides: 37