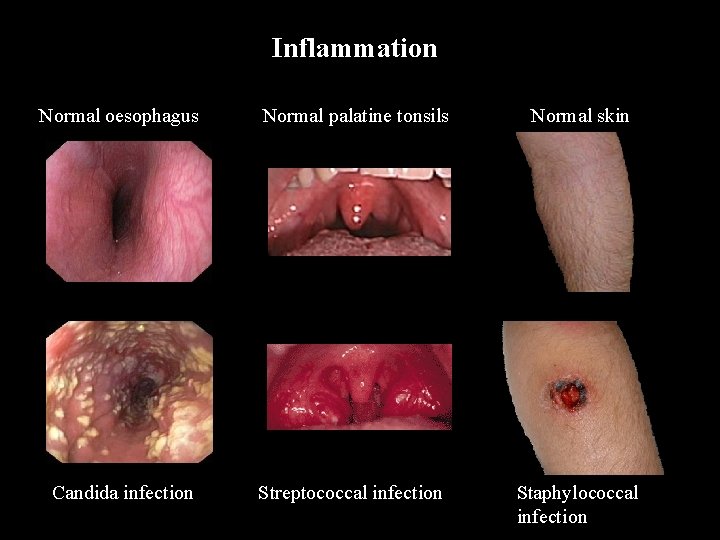
Inflammation Normal oesophagus Normal palatine tonsils Normal skin
- Slides: 32
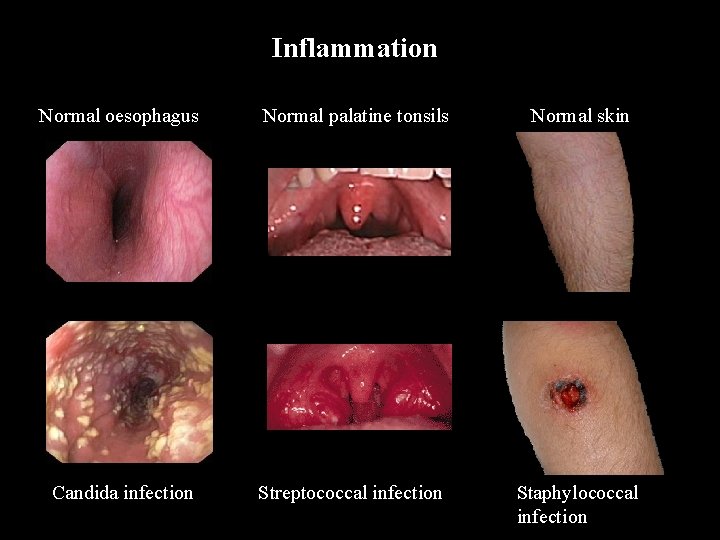
Inflammation Normal oesophagus Normal palatine tonsils Normal skin Candida infection Streptococcal infection Staphylococcal infection
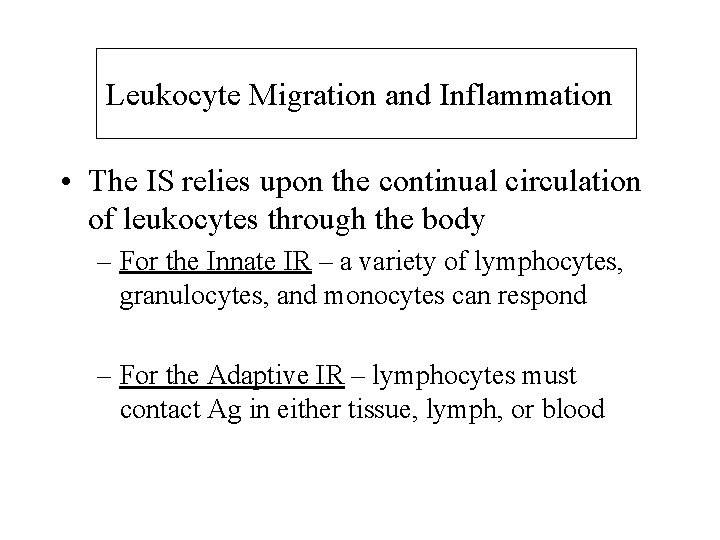
Leukocyte Migration and Inflammation • The IS relies upon the continual circulation of leukocytes through the body – For the Innate IR – a variety of lymphocytes, granulocytes, and monocytes can respond – For the Adaptive IR – lymphocytes must contact Ag in either tissue, lymph, or blood
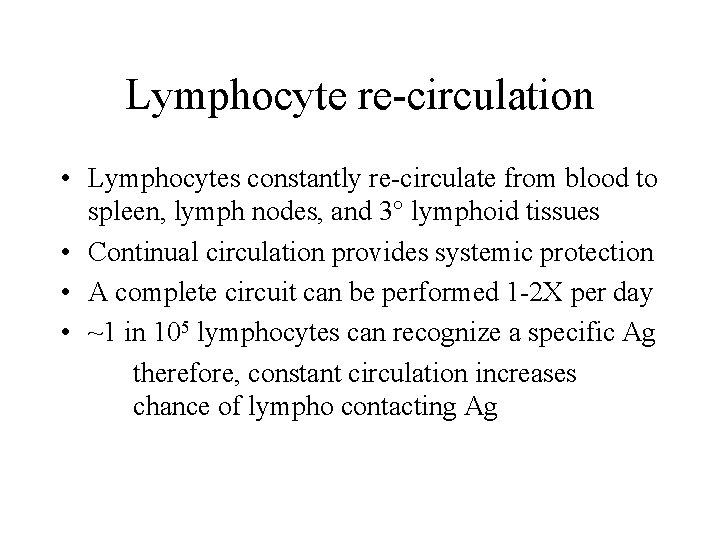
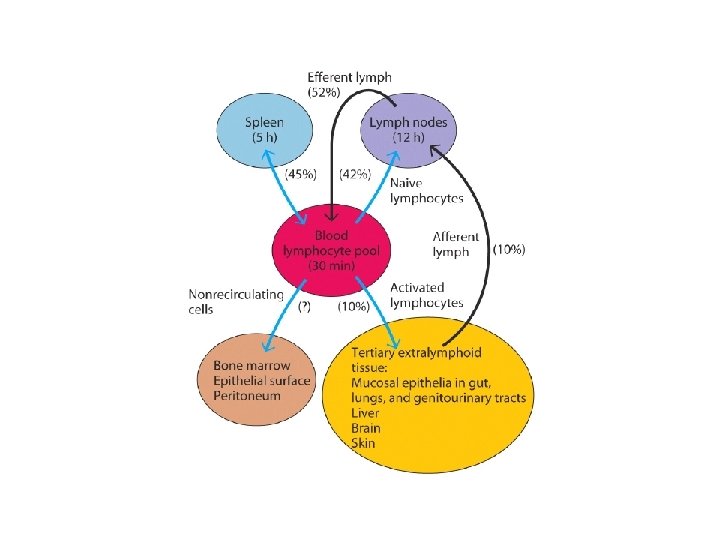
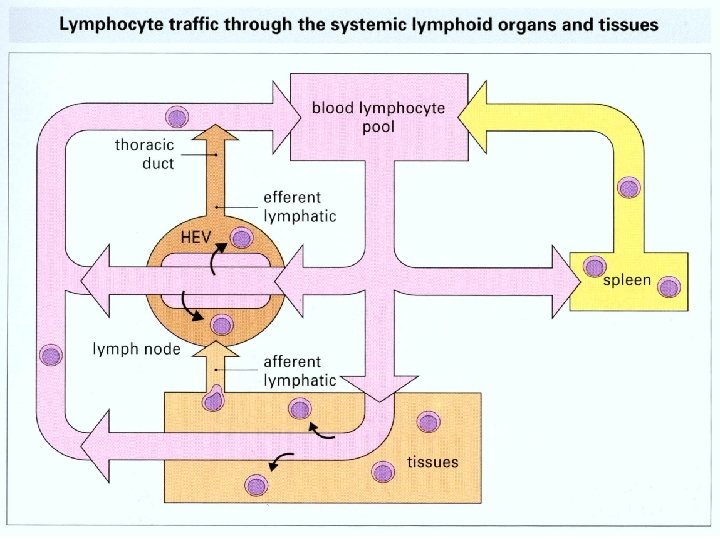
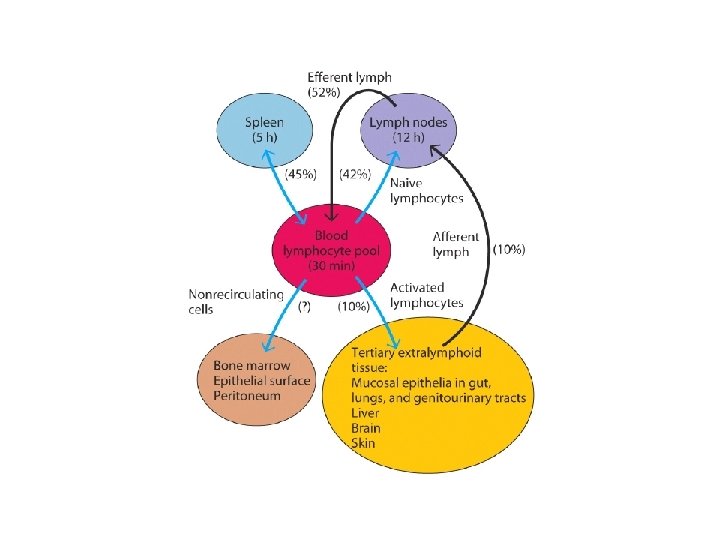
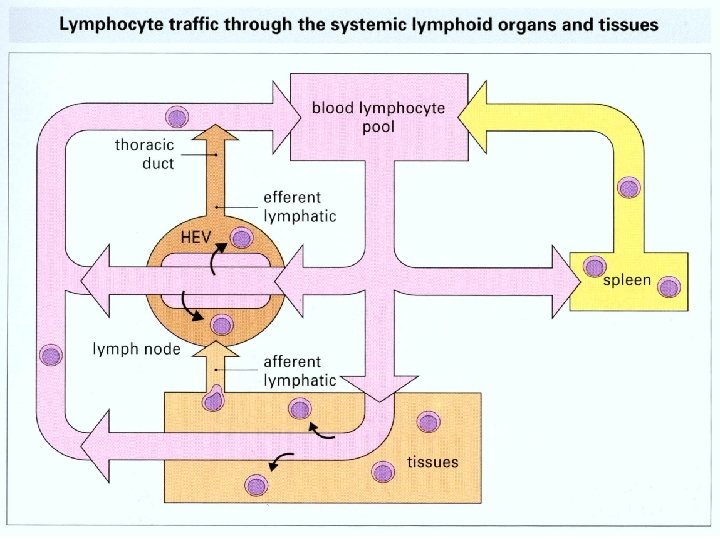
Lymphocyte re-circulation • Lymphocytes constantly re-circulate from blood to spleen, lymph nodes, and 3° lymphoid tissues • Continual circulation provides systemic protection • A complete circuit can be performed 1 -2 X per day • ~1 in 105 lymphocytes can recognize a specific Ag therefore, constant circulation increases chance of lympho contacting Ag
How do leukocytes transit the bloodstream? They must bind to an endothelial cell first! • Endothelial cells exhibit ‘cell adhesion molecules’ – CAM’s • Lympho’s, granulo’s, and mono’s form receptors which bind to CAM’s
From Here to There? • Lymphoid stem cell migrate to central lymphoid organs • Mature lymphocyte migrate to peripheral lymphoid organs • Recirculation of lymphocytes • Lymphocyte migrate to the sites of inflammation
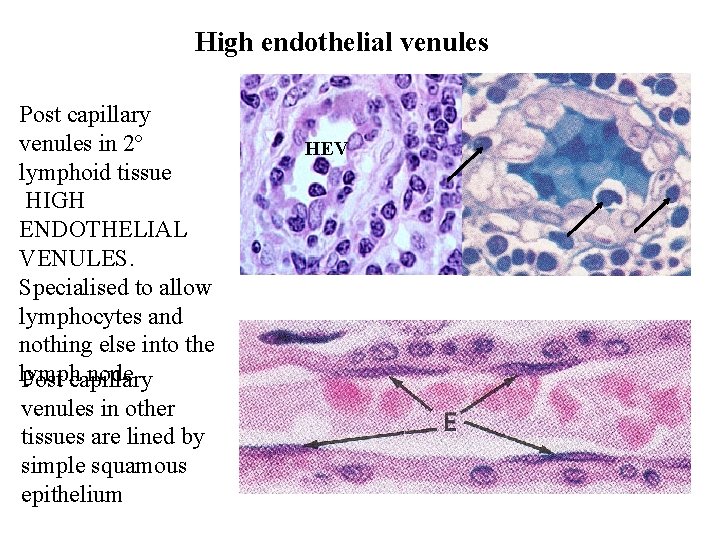
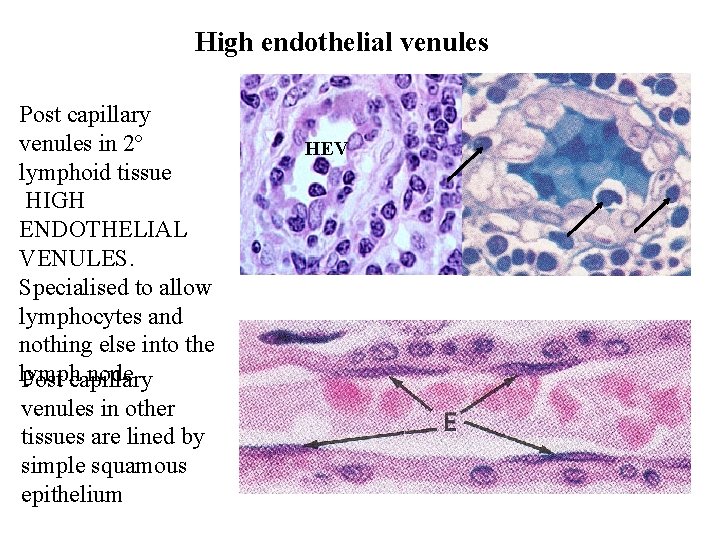
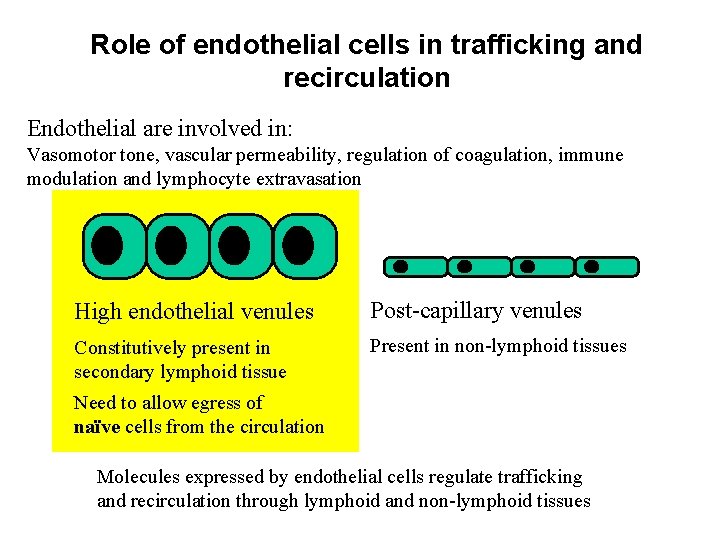
High endothelial venules Post capillary venules in 2º lymphoid tissue HIGH ENDOTHELIAL VENULES. Specialised to allow lymphocytes and nothing else into the lymph node Post capillary venules in other tissues are lined by simple squamous epithelium HEV
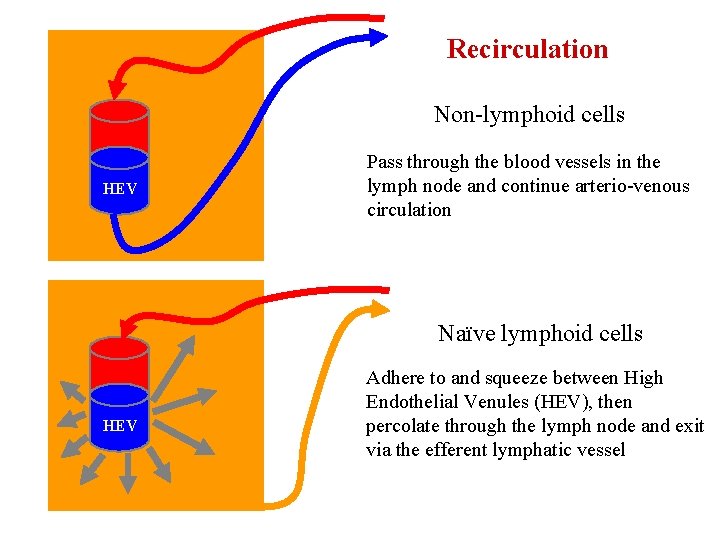
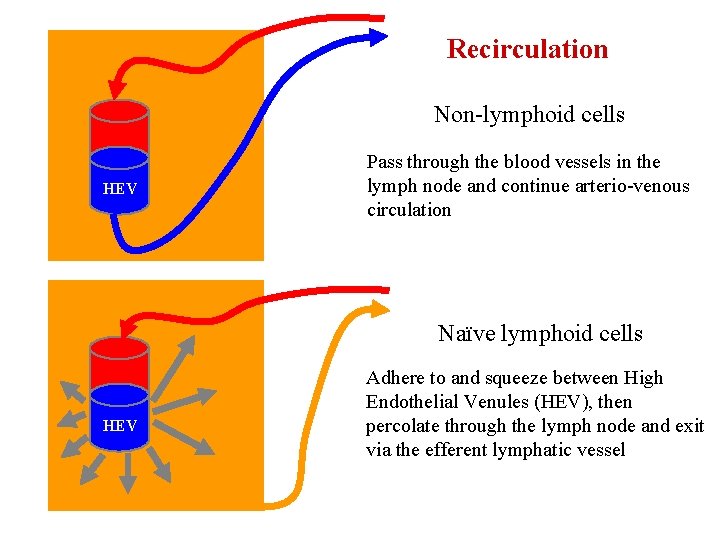
Recirculation Non-lymphoid cells HEV Pass through the blood vessels in the lymph node and continue arterio-venous circulation Naïve lymphoid cells HEV Adhere to and squeeze between High Endothelial Venules (HEV), then percolate through the lymph node and exit via the efferent lymphatic vessel
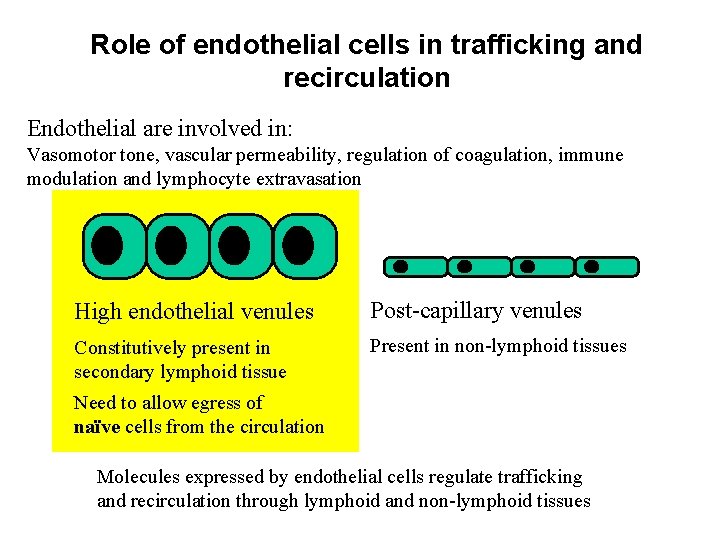
Role of endothelial cells in trafficking and recirculation Endothelial are involved in: Vasomotor tone, vascular permeability, regulation of coagulation, immune modulation and lymphocyte extravasation High endothelial venules Post-capillary venules Constitutively present in secondary lymphoid tissue Present in non-lymphoid tissues Need to allow egress of naïve cells from the circulation Molecules expressed by endothelial cells regulate trafficking and recirculation through lymphoid and non-lymphoid tissues
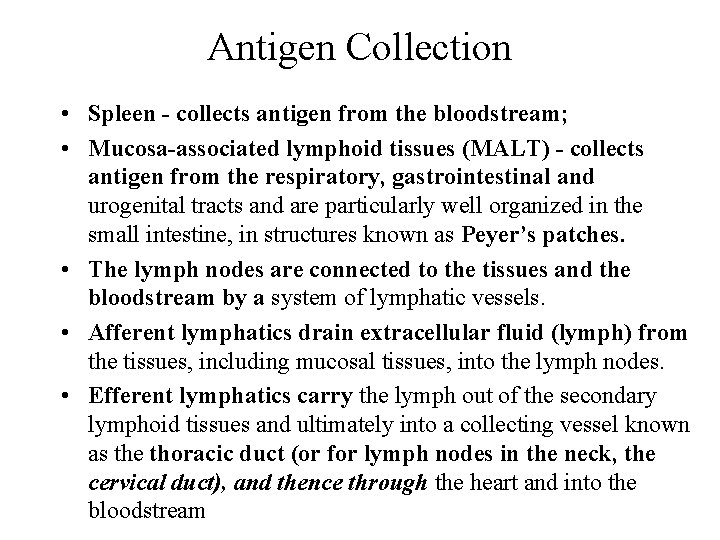
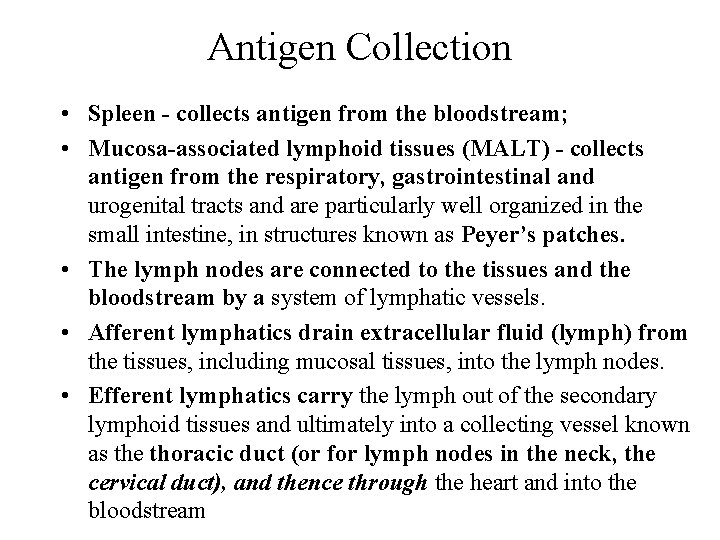
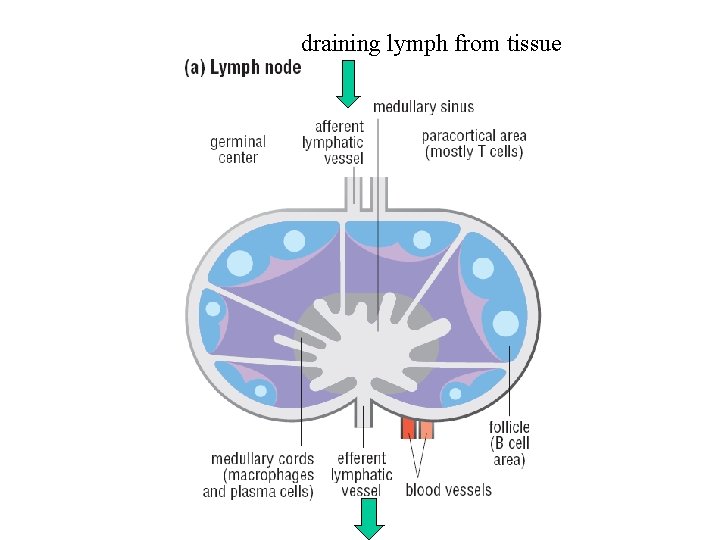
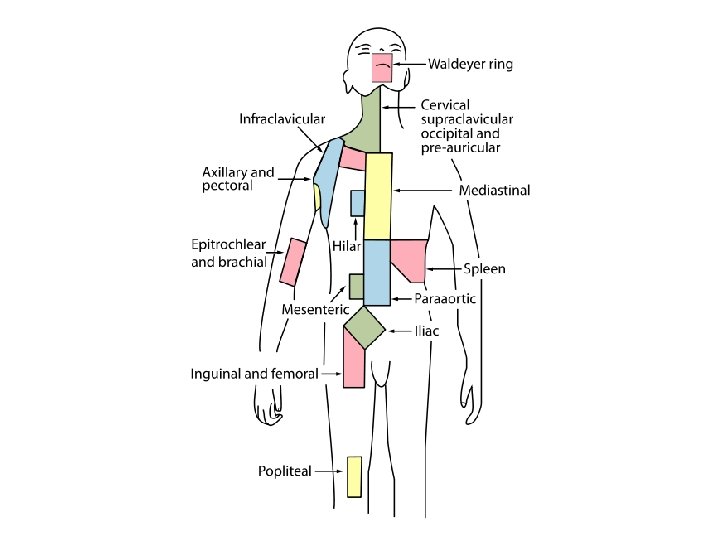
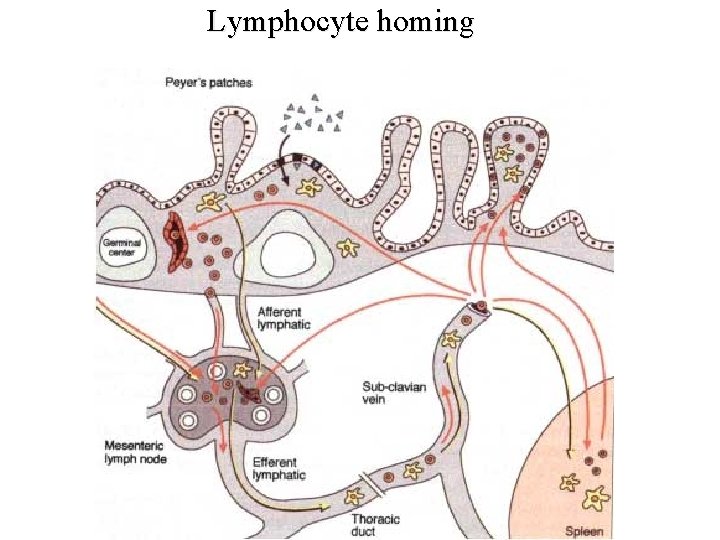
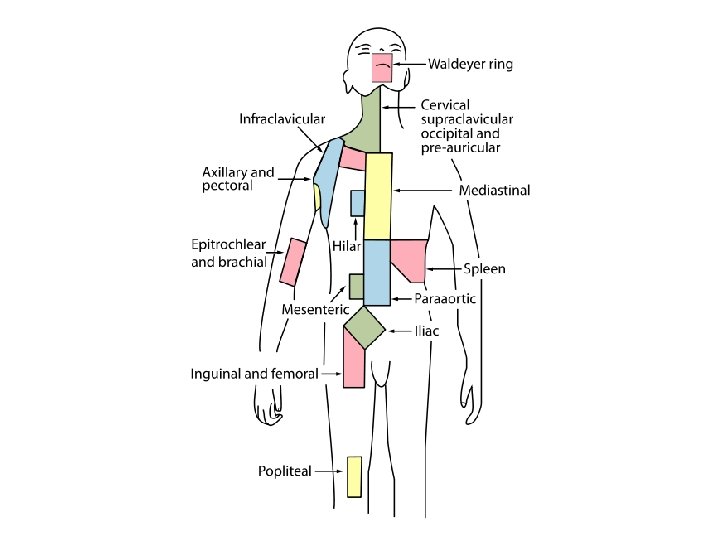
Antigen Collection • Spleen - collects antigen from the bloodstream; • Mucosa-associated lymphoid tissues (MALT) - collects antigen from the respiratory, gastrointestinal and urogenital tracts and are particularly well organized in the small intestine, in structures known as Peyer’s patches. • The lymph nodes are connected to the tissues and the bloodstream by a system of lymphatic vessels. • Afferent lymphatics drain extracellular fluid (lymph) from the tissues, including mucosal tissues, into the lymph nodes. • Efferent lymphatics carry the lymph out of the secondary lymphoid tissues and ultimately into a collecting vessel known as the thoracic duct (or for lymph nodes in the neck, the cervical duct), and thence through the heart and into the bloodstream
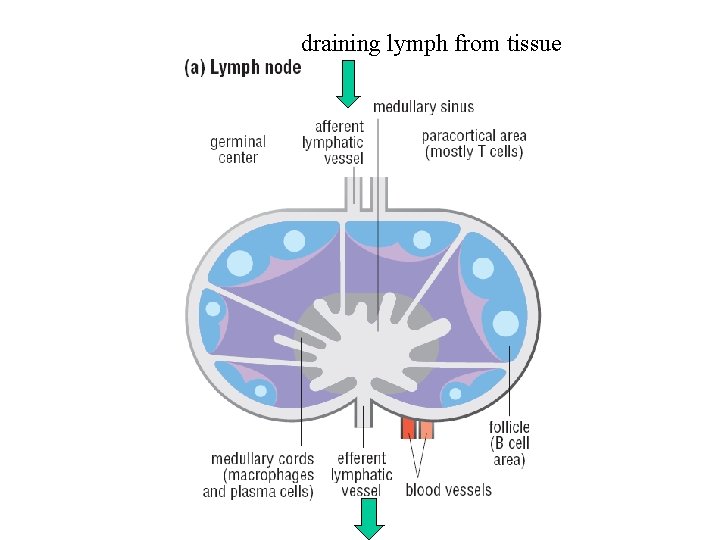
draining lymph from tissue
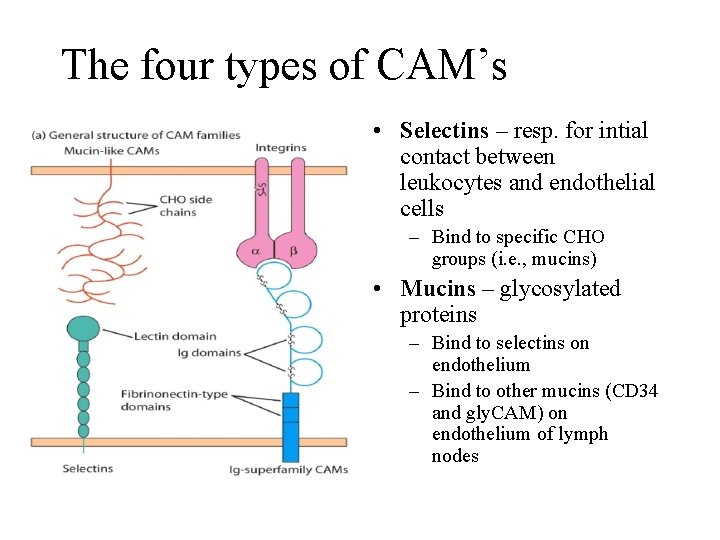
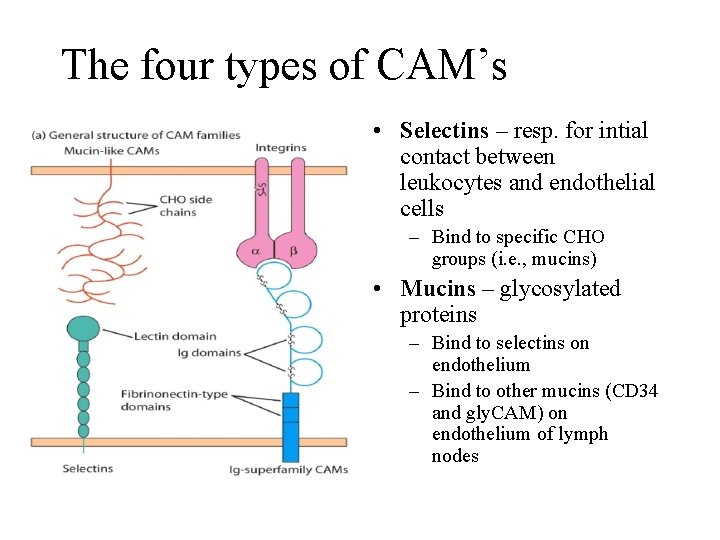
The four types of CAM’s • Selectins – resp. for intial contact between leukocytes and endothelial cells – Bind to specific CHO groups (i. e. , mucins) • Mucins – glycosylated proteins – Bind to selectins on endothelium – Bind to other mucins (CD 34 and gly. CAM) on endothelium of lymph nodes
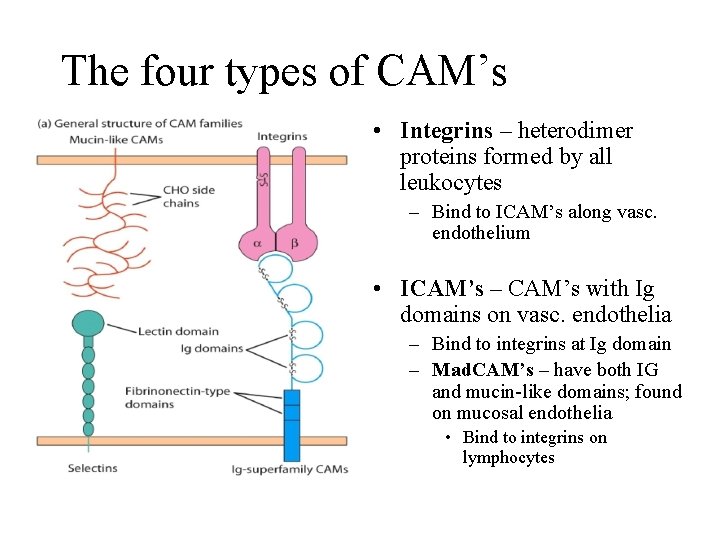
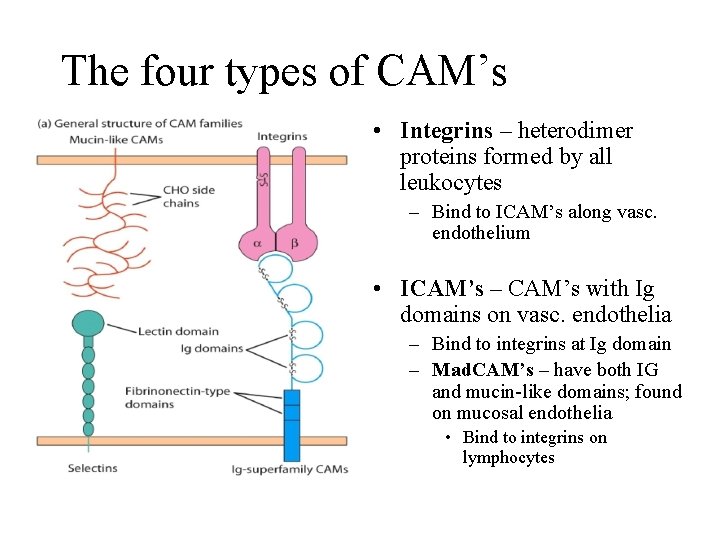
The four types of CAM’s • Integrins – heterodimer proteins formed by all leukocytes – Bind to ICAM’s along vasc. endothelium • ICAM’s – CAM’s with Ig domains on vasc. endothelia – Bind to integrins at Ig domain – Mad. CAM’s – have both IG and mucin-like domains; found on mucosal endothelia • Bind to integrins on lymphocytes
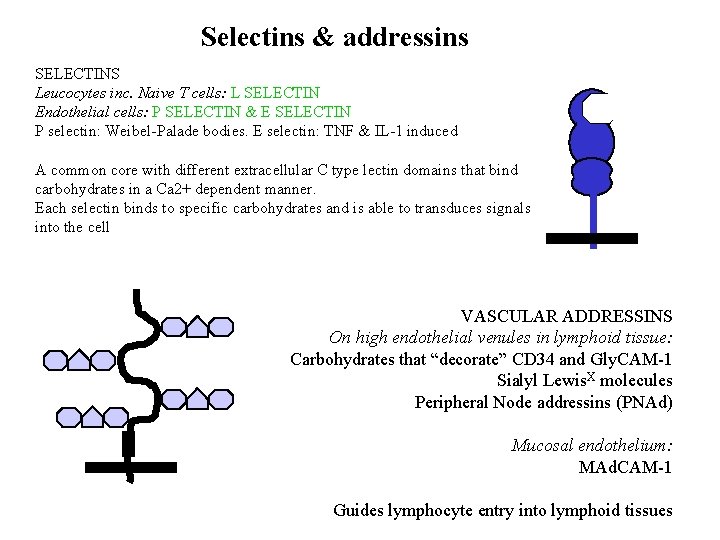
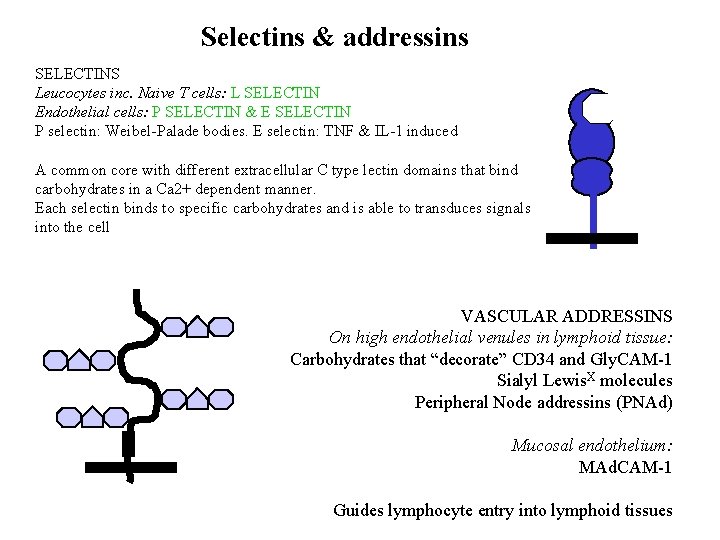
Selectins & addressins SELECTINS Leucocytes inc. Naive T cells: L SELECTIN Endothelial cells: P SELECTIN & E SELECTIN P selectin: Weibel-Palade bodies. E selectin: TNF & IL-1 induced A common core with different extracellular C type lectin domains that bind carbohydrates in a Ca 2+ dependent manner. Each selectin binds to specific carbohydrates and is able to transduces signals into the cell VASCULAR ADDRESSINS On high endothelial venules in lymphoid tissue: Carbohydrates that “decorate” CD 34 and Gly. CAM-1 Sialyl Lewis. X molecules Peripheral Node addressins (PNAd) Mucosal endothelium: MAd. CAM-1 Guides lymphocyte entry into lymphoid tissues
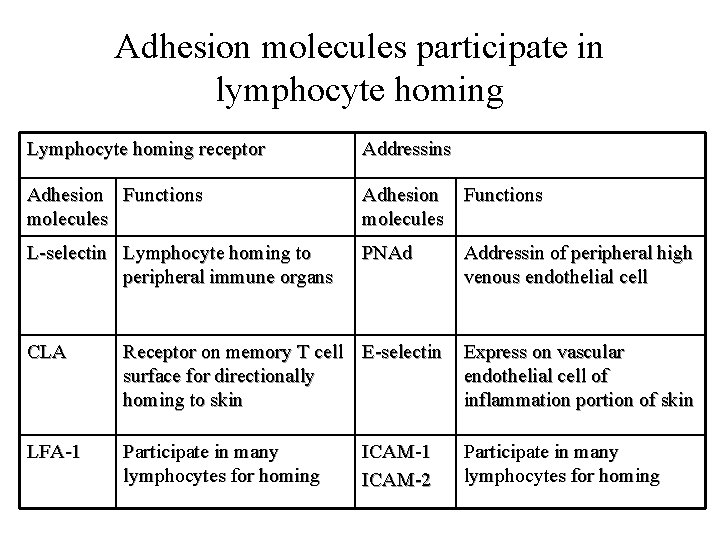
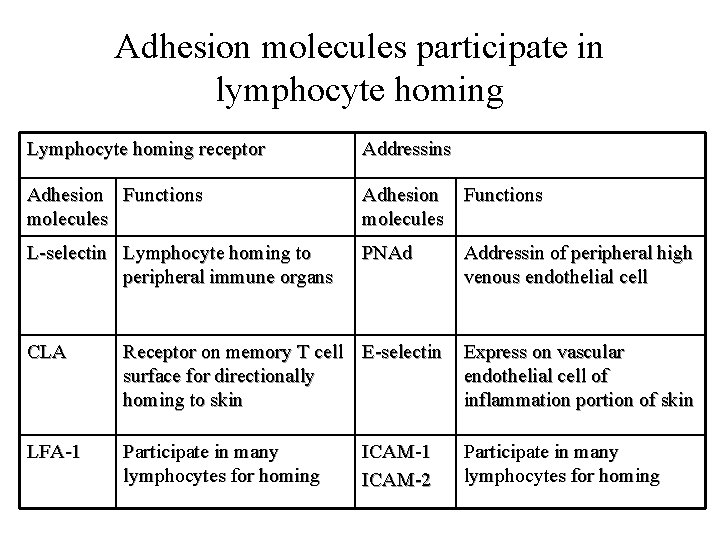
Adhesion molecules participate in lymphocyte homing Lymphocyte homing receptor Addressins Adhesion Functions molecules L-selectin Lymphocyte homing to peripheral immune organs PNAd Addressin of peripheral high venous endothelial cell CLA Receptor on memory T cell E-selectin surface for directionally homing to skin Express on vascular endothelial cell of inflammation portion of skin LFA-1 Participate in many lymphocytes for homing ICAM-1 ICAM-2
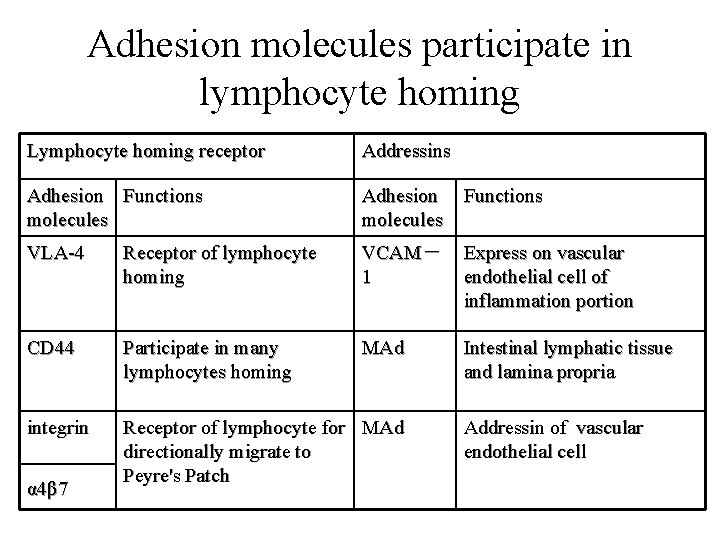
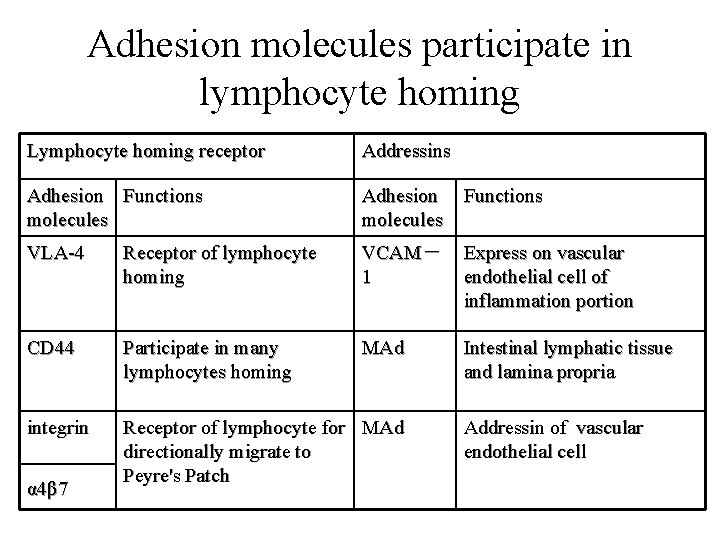
Adhesion molecules participate in lymphocyte homing Lymphocyte homing receptor Addressins Adhesion Functions molecules Adhesion molecules Functions VLA-4 Receptor of lymphocyte homing VCAM- 1 Express on vascular endothelial cell of inflammation portion CD 44 Participate in many lymphocytes homing MAd Intestinal lymphatic tissue and lamina propria integrin Receptor of lymphocyte for MAd directionally migrate to Peyre's Patch α 4β 7 Addressin of vascular endothelial cell
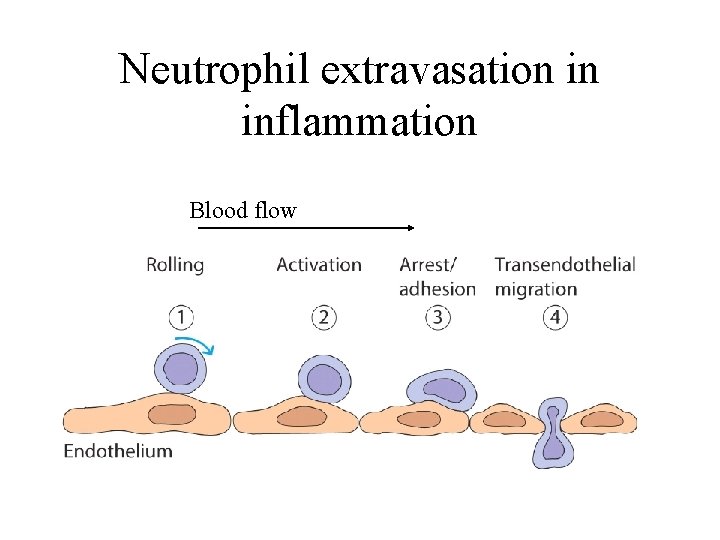
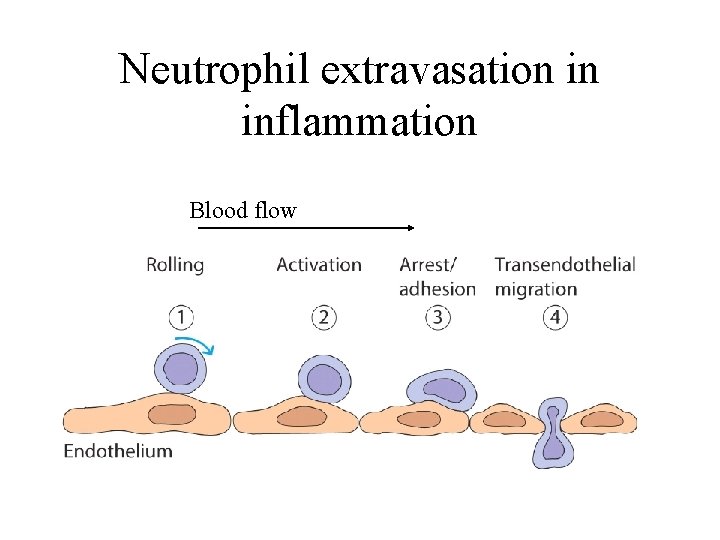
Neutrophil extravasation in inflammation Blood flow
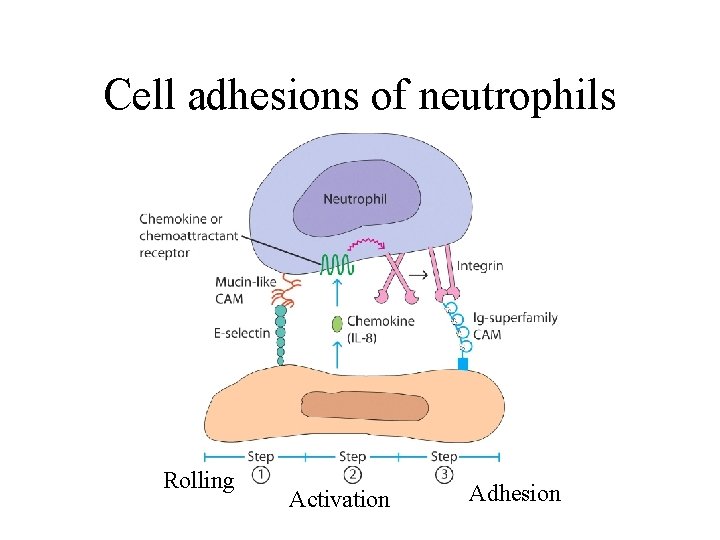
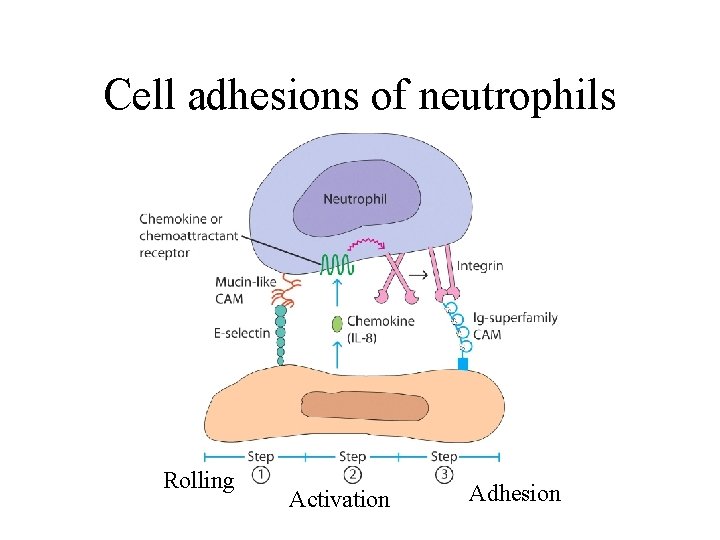
Cell adhesions of neutrophils Rolling Activation Adhesion
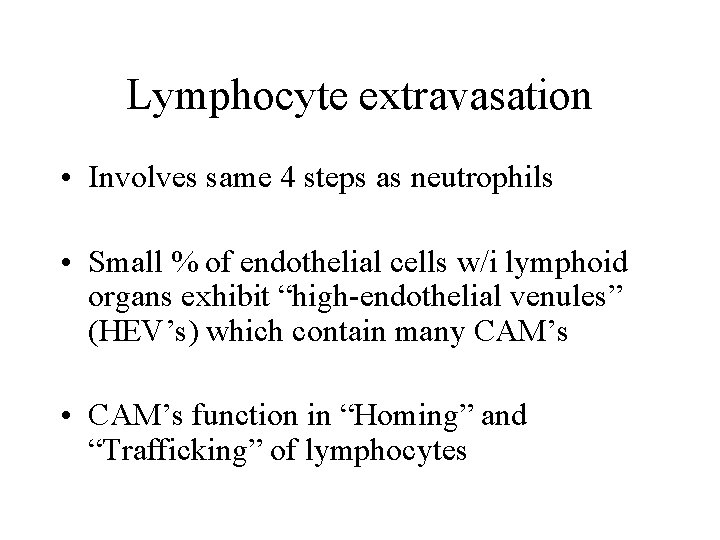
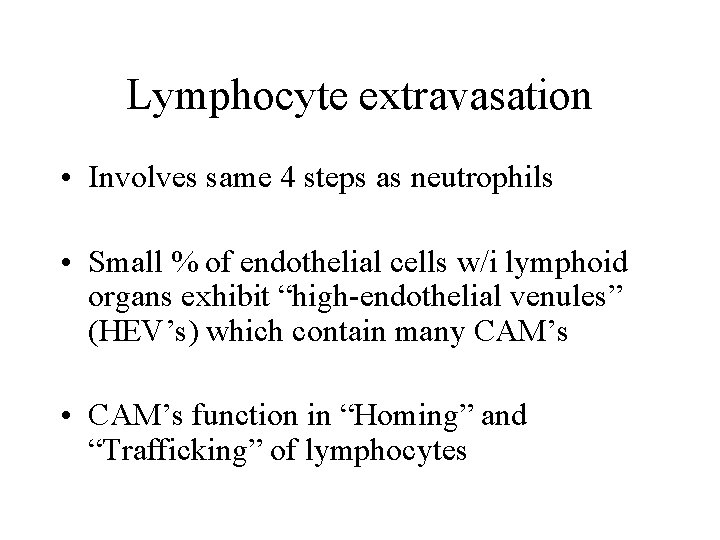
Lymphocyte extravasation • Involves same 4 steps as neutrophils • Small % of endothelial cells w/i lymphoid organs exhibit “high-endothelial venules” (HEV’s) which contain many CAM’s • CAM’s function in “Homing” and “Trafficking” of lymphocytes
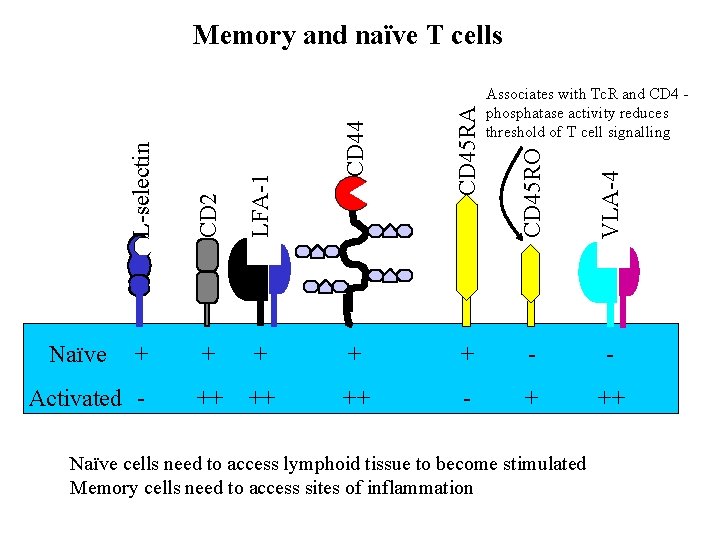
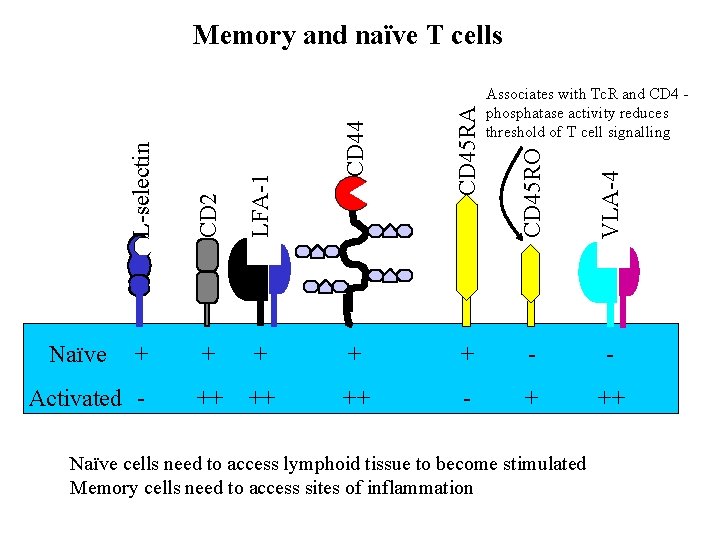
Memory and naïve T cells L-selectin LFA-1 CD 44 CD 2 CD 45 RA CD 45 RO VLA-4 Naïve Associates with Tc. R and CD 4 phosphatase activity reduces threshold of T cell signalling + + + - - ++ ++ ++ - + ++ Activated - Naïve cells need to access lymphoid tissue to become stimulated Memory cells need to access sites of inflammation
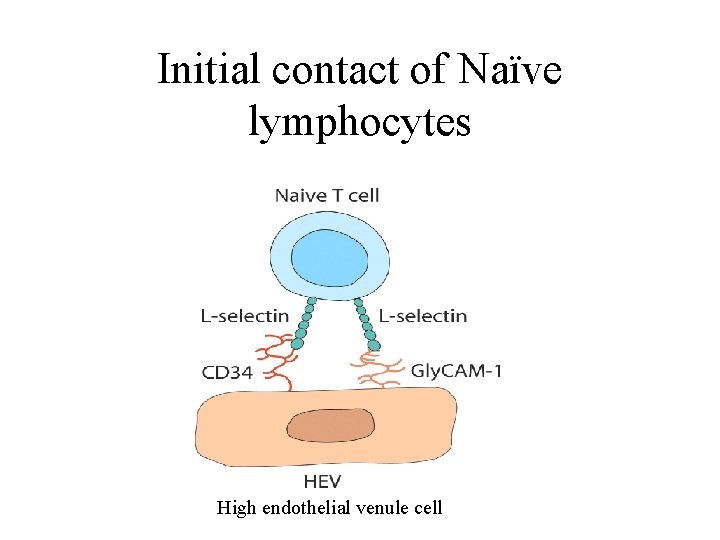
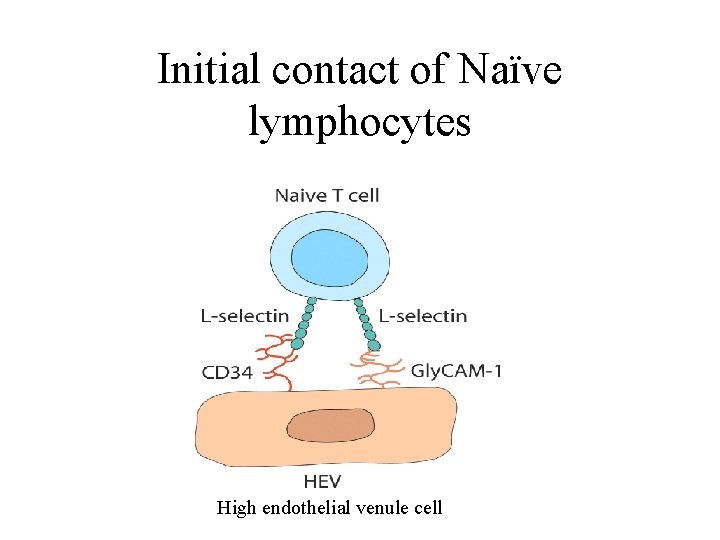
Initial contact of Naïve lymphocytes High endothelial venule cell
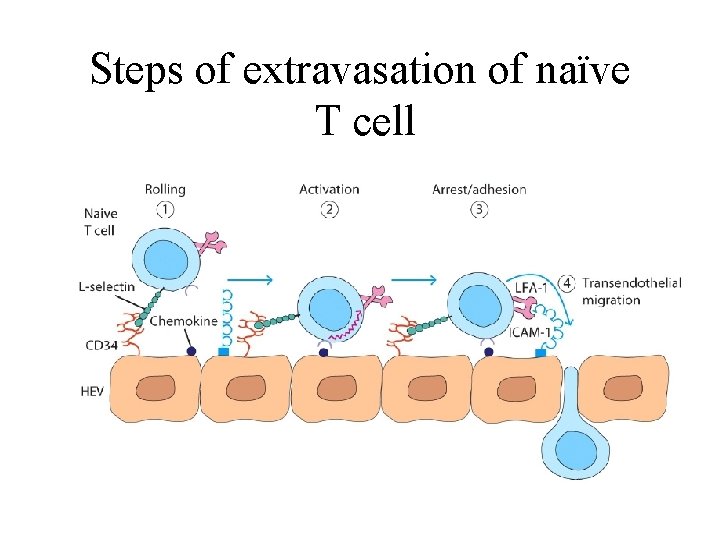
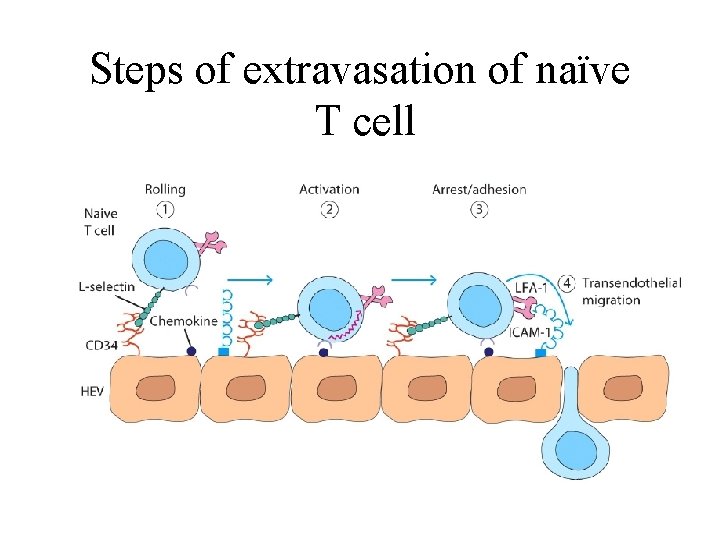
Steps of extravasation of naïve T cell
Trafficking, homing and adhesion Trafficking: Non-random movement of cells from tissues, blood or lymph. Includes migration to and from sites of lymphocyte maturation as well as homing. Adhesion: Binding of cells to other cells or extracellular matrix Homing: Tendency of lymphocytes activated in a particular region of the body to preferentially return to the same region Includes localisation of cells in distinct regions of lymphoid tissue.
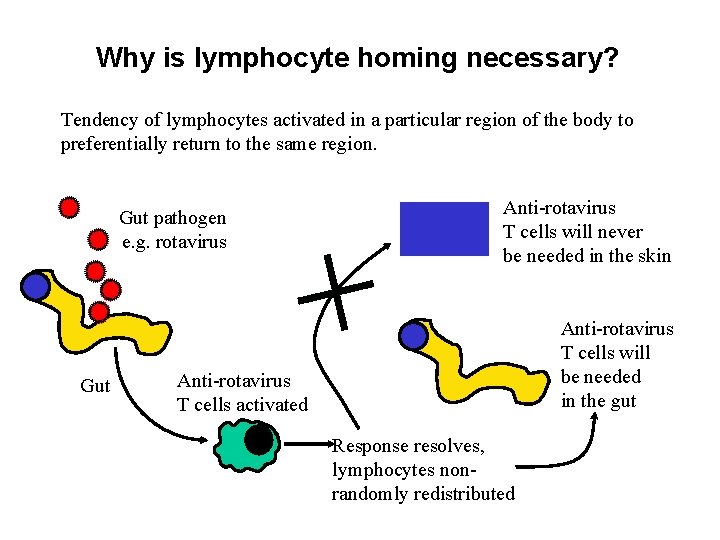
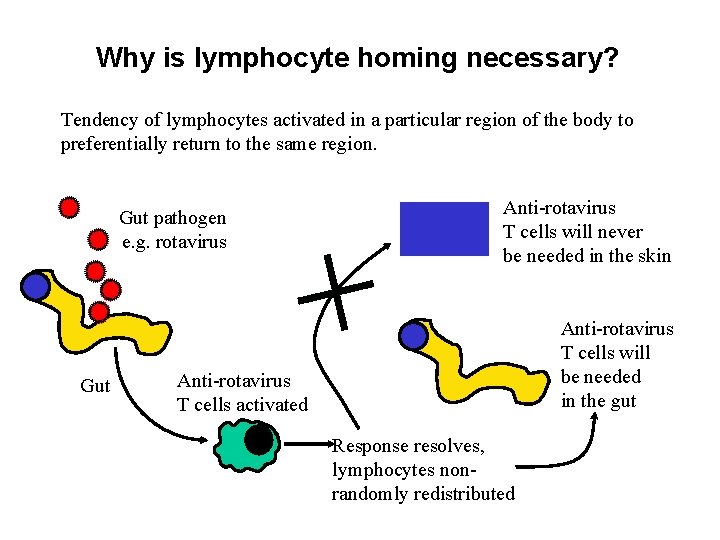
Why is lymphocyte homing necessary? Tendency of lymphocytes activated in a particular region of the body to preferentially return to the same region. Gut pathogen e. g. rotavirus Gut Anti-rotavirus T cells will never be needed in the skin Anti-rotavirus T cells will be needed in the gut Anti-rotavirus T cells activated Response resolves, lymphocytes nonrandomly redistributed
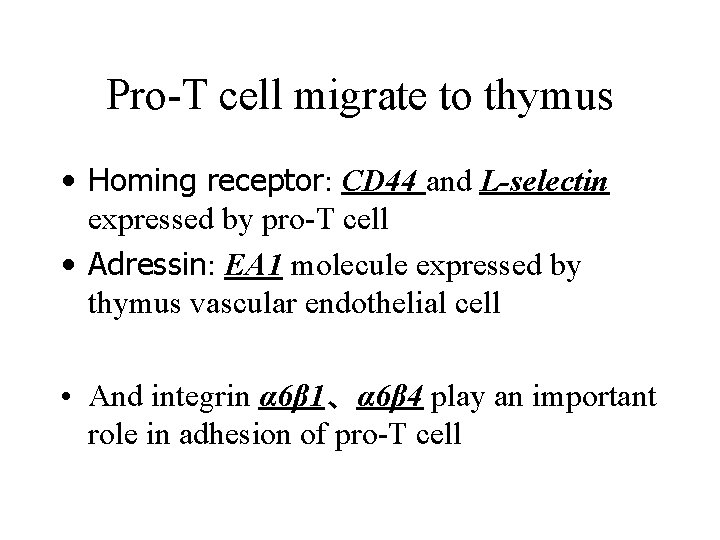
Pro-T cell migrate to thymus • Homing receptor: CD 44 and L-selectin expressed by pro-T cell • Adressin: EA 1 molecule expressed by thymus vascular endothelial cell • And integrin α 6β 1、α 6β 4 play an important role in adhesion of pro-T cell
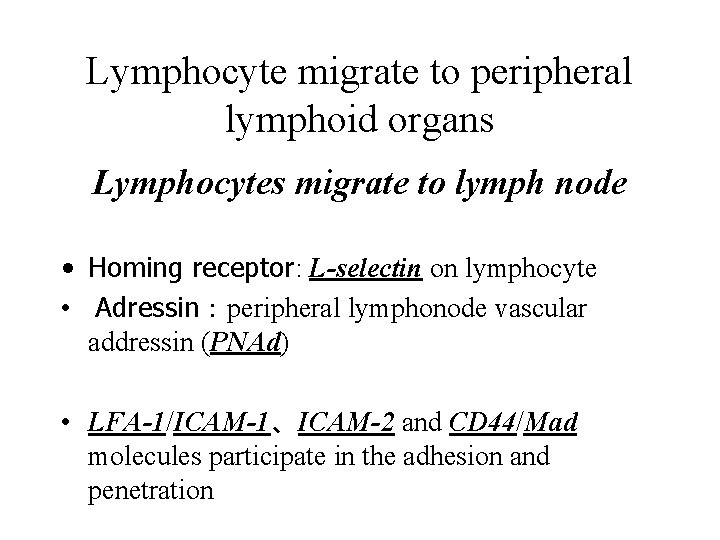
Lymphocyte migrate to peripheral lymphoid organs Lymphocytes migrate to lymph node • Homing receptor: L-selectin on lymphocyte • Adressin:peripheral lymphonode vascular addressin (PNAd) • LFA-1/ICAM-1、ICAM-2 and CD 44/Mad molecules participate in the adhesion and penetration
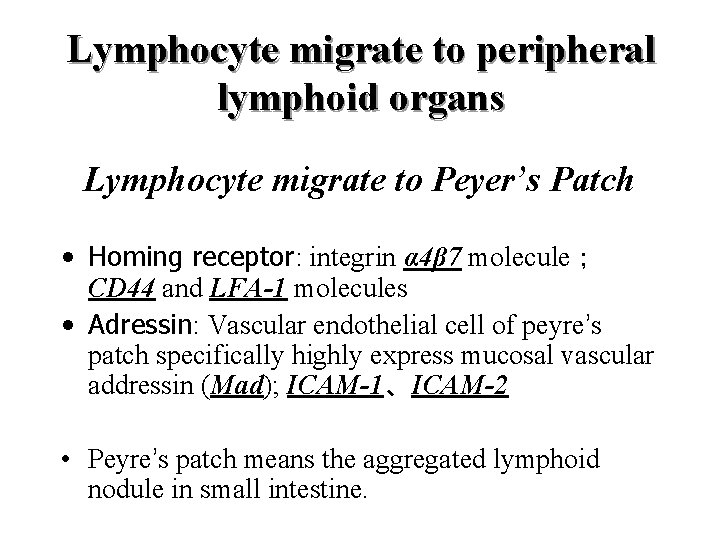
Lymphocyte migrate to peripheral lymphoid organs Lymphocyte migrate to Peyer’s Patch • Homing receptor: integrin α 4β 7 molecule; CD 44 and LFA-1 molecules • Adressin: Vascular endothelial cell of peyre’s patch specifically highly express mucosal vascular addressin (Mad); ICAM-1、ICAM-2 • Peyre’s patch means the aggregated lymphoid nodule in small intestine.
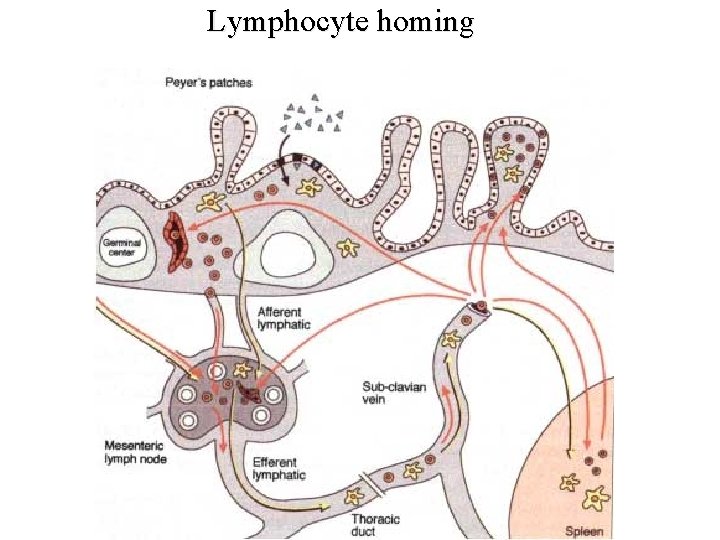
Lymphocyte homing
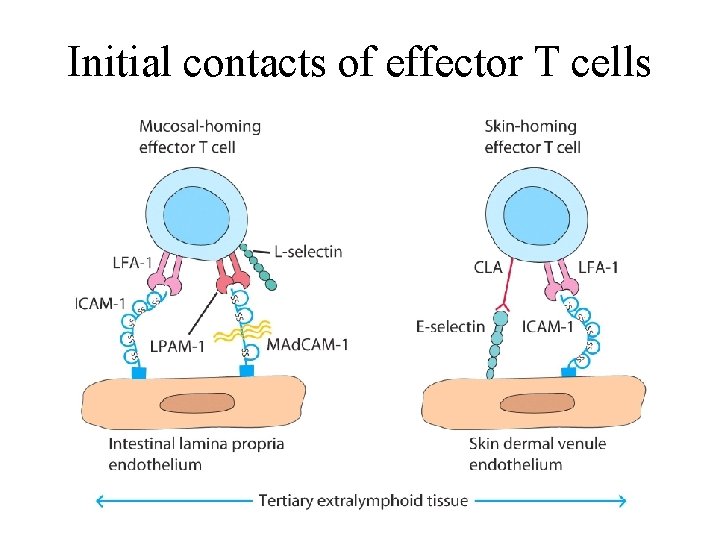
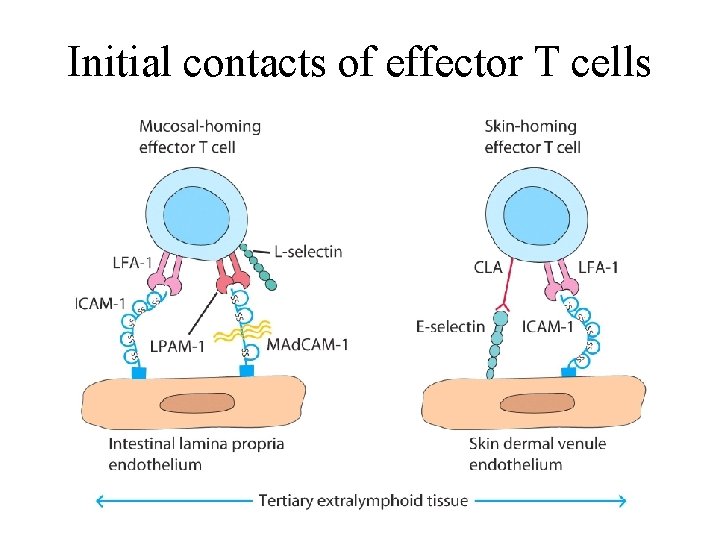
Initial contacts of effector T cells
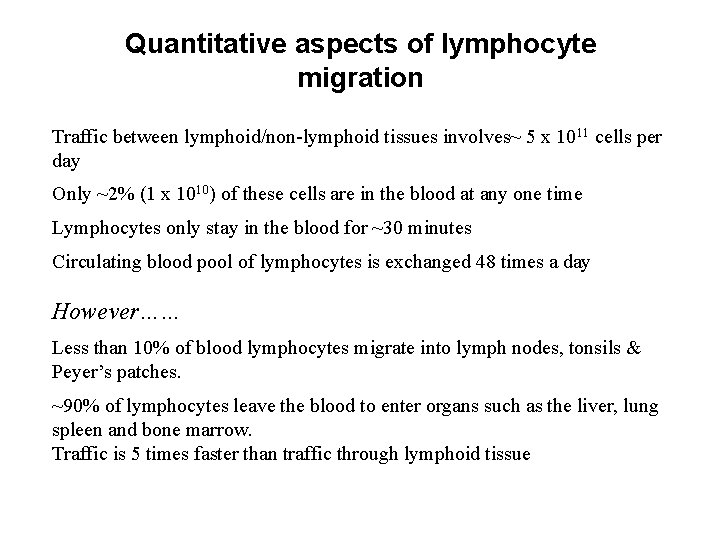
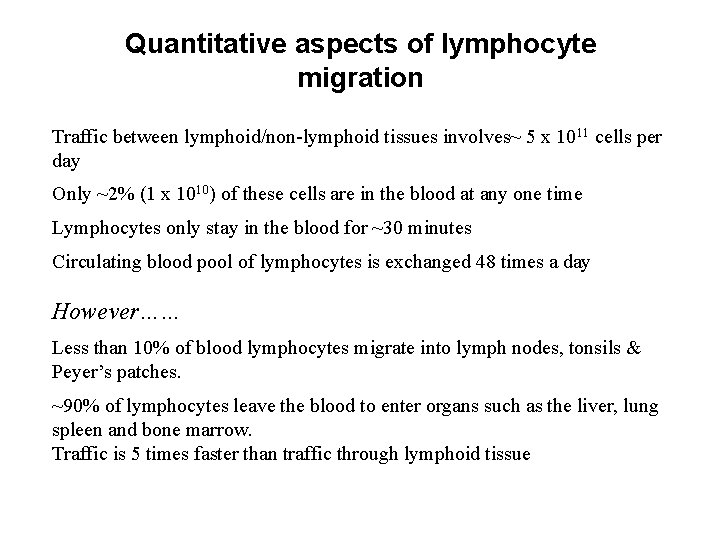
Quantitative aspects of lymphocyte migration Traffic between lymphoid/non-lymphoid tissues involves~ 5 x 1011 cells per day Only ~2% (1 x 1010) of these cells are in the blood at any one time Lymphocytes only stay in the blood for ~30 minutes Circulating blood pool of lymphocytes is exchanged 48 times a day However…… Less than 10% of blood lymphocytes migrate into lymph nodes, tonsils & Peyer’s patches. ~90% of lymphocytes leave the blood to enter organs such as the liver, lung spleen and bone marrow. Traffic is 5 times faster than traffic through lymphoid tissue