Inflammation Inflammation Definition Inflammation is biochemical structural and
Inflammation
Inflammation Definition Inflammation is biochemical, structural and cellular non-specific protective process occurring locally in vascularized tissues aimed to destroy impairing factors, or to remove they and to restart reparation of tissue, to separate the impairing agents and to limit their effect to the whole body and to induce specific immune response.
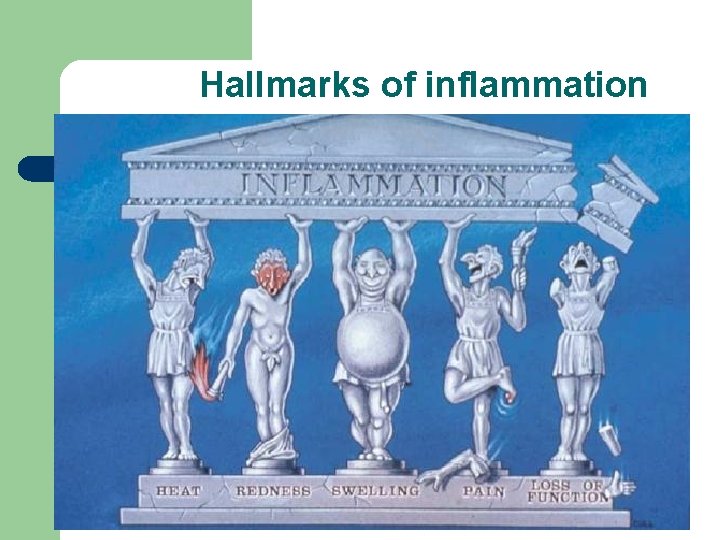
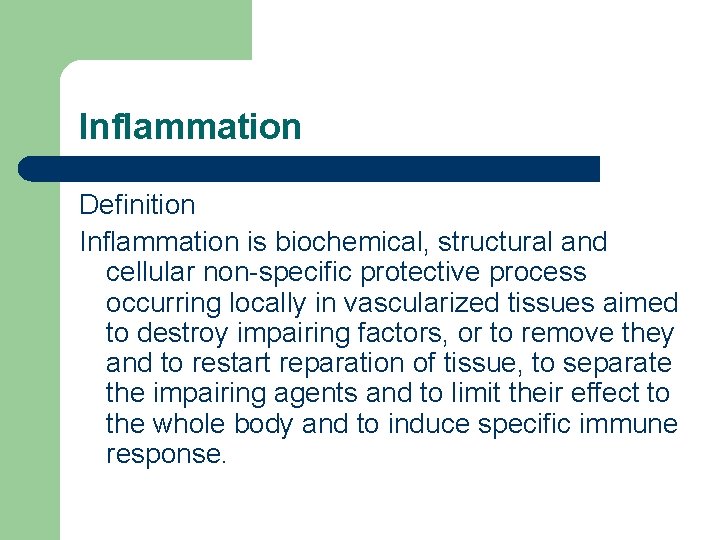
Hallmarks of inflammation
Hallmarks of inflammation l l l Rubor (redness) Calor (heat) Dolor (pain) Tumor (swelling) Functio laesa (loss of function)
Classification Type (course) l acute 6 – 14 days l subacute 3 – 6 weeks l chronic several months Pathology l alterative l exudative l proliferative l garanulomatous
Classification Etiology Exogenous l biological (viruses, bacteria, parasites) l physical (trauma, radiation, heat) l chemical (acids, poisons, toxins) Endogenous l dead cells l immunological defects l metabolic diseases
Stages of inflammation 1. Alteration primary l direct effect of pathogenic factor secondary l enzymes and other chemicals released from impaired cells l reactive oxygen species
Stages of inflammation 2. Microvascular reactions l l vasodilatation - hyperemia higher permeability – oedema 3. Acute cellular respose l granulocytes (Neu, Ba, Eo)
Stages of inflammation 4. Chronic cellular respose l monocytes, macrophages, lymphocytes 5. Reparation
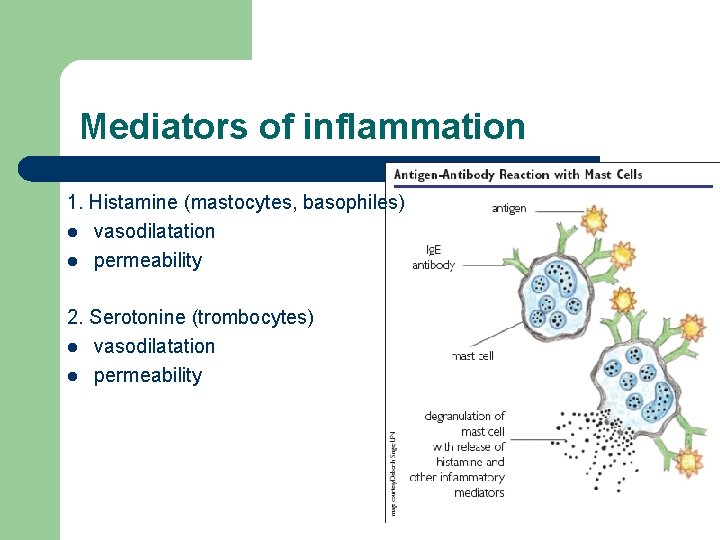
Mediators of inflammation 1. Histamine (mastocytes, basophiles) l vasodilatation l permeability 2. Serotonine (trombocytes) l vasodilatation l permeability
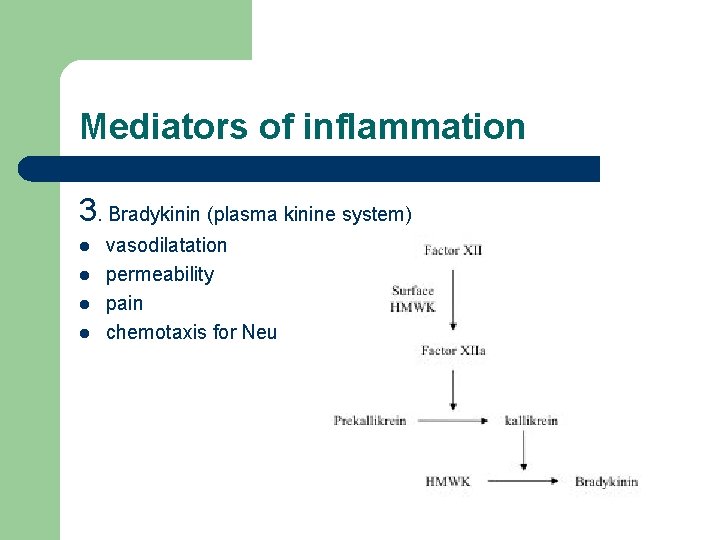
Mediators of inflammation 3. Bradykinin (plasma kinine system) l l vasodilatation permeability pain chemotaxis for Neu
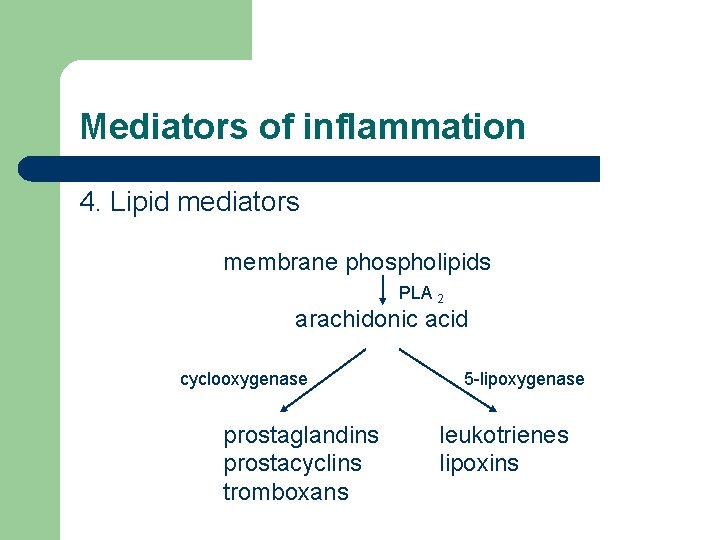
Mediators of inflammation 4. Lipid mediators membrane phospholipids PLA 2 arachidonic acid cyclooxygenase prostaglandins prostacyclins tromboxans 5 -lipoxygenase leukotrienes lipoxins
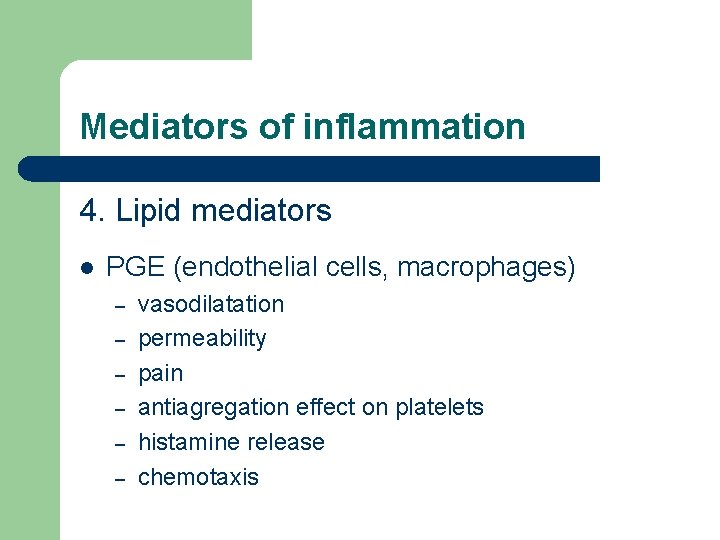
Mediators of inflammation 4. Lipid mediators l PGE (endothelial cells, macrophages) – – – vasodilatation permeability pain antiagregation effect on platelets histamine release chemotaxis
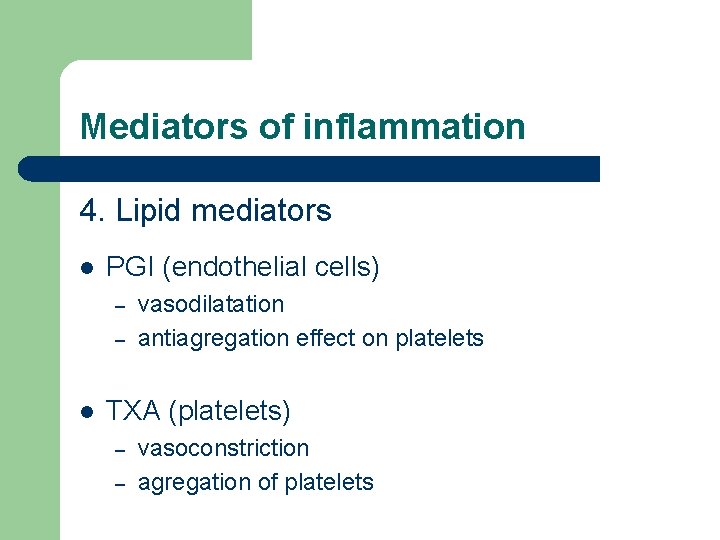
Mediators of inflammation 4. Lipid mediators l PGI (endothelial cells) – – l vasodilatation antiagregation effect on platelets TXA (platelets) – – vasoconstriction agregation of platelets
Mediators of inflammation 5. NO (EDRF) – vasodilatation
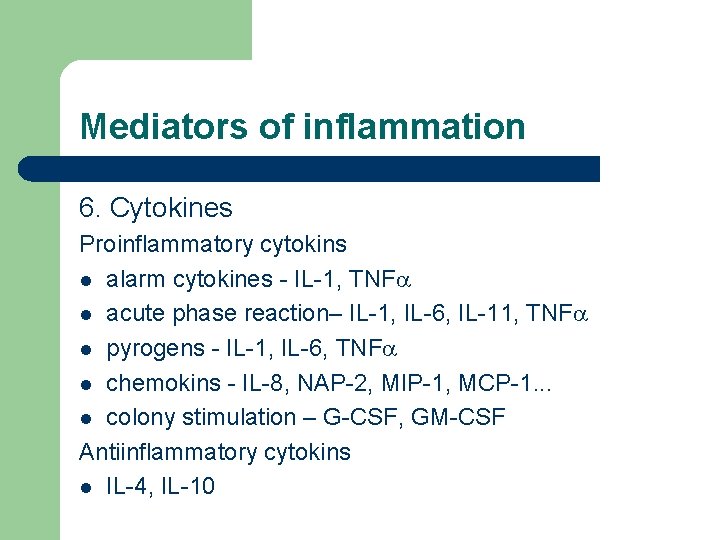
Mediators of inflammation 6. Cytokines Proinflammatory cytokins l alarm cytokines - IL-1, TNFa l acute phase reaction– IL-1, IL-6, IL-11, TNFa l pyrogens - IL-1, IL-6, TNFa l chemokins - IL-8, NAP-2, MIP-1, MCP-1. . . l colony stimulation – G-CSF, GM-CSF Antiinflammatory cytokins l IL-4, IL-10
Mediators of inflammation 7. Plasma protein systems l Complement – – – lysis of bacteria C 5 b 678(9)n opsonisation C 3 b, C 4 b mastocytes degranulation C 3 a, C 4 a, C 5 a permability C 3 a, C 4 a, C 5 a chemotactic factors C 5 b
Mediators of inflammation 7. Plasma protein systems l l l Clotting system – stops bleeding – prevents from spreading infection – keeps foreign bodies in the site of maximum fagocytosis Fibrinolytic system Kinin system – bradykinin
Cellular components of inflammation 1. Neutrophiles – – 2. Monocytes, macrophages – – – 3. chronic inflammation phagocytosis production of PGE, PGI Eosinophiles – – 4. acute inflammation phagocytosis allergy parasites Mastocytes, basofiles – production of histamin
Cellular components of inflammation 5. Lymphocytes – – – chronic inflammation production of mediators production of antibodies 6. Endothelial cells – – production of PGI, NO, lipid mediators production of adhesive molecules
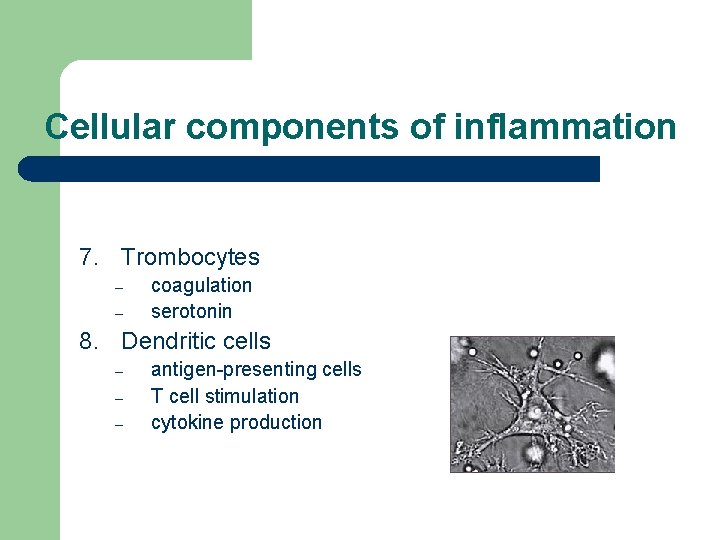
Cellular components of inflammation 7. Trombocytes – – coagulation serotonin 8. Dendritic cells – – – antigen-presenting cells T cell stimulation cytokine production
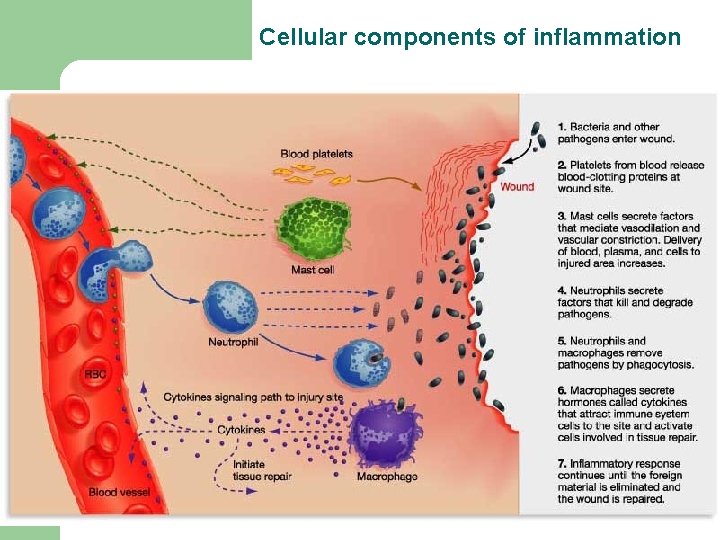
Cellular components of inflammation
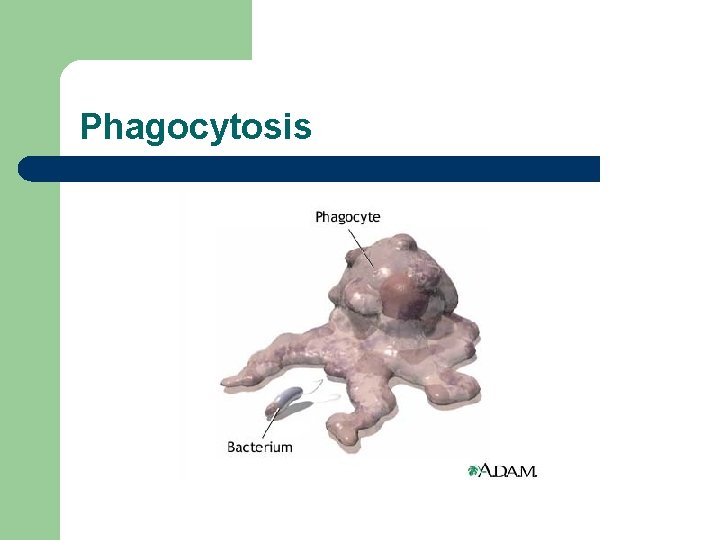
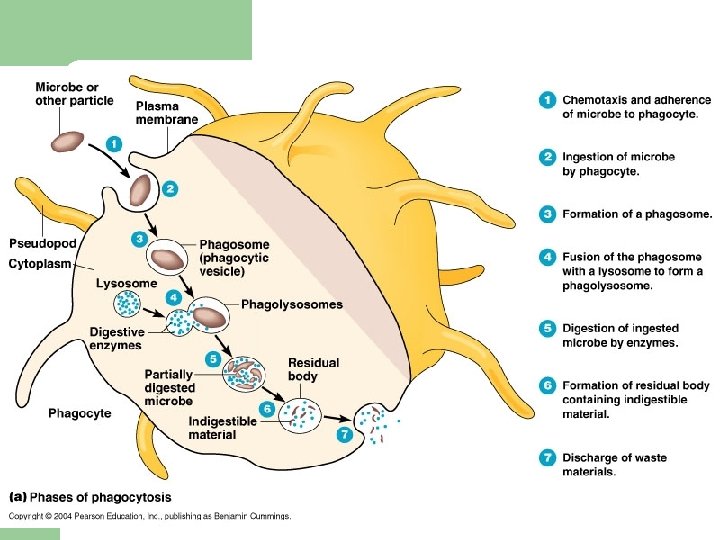
Phagocytosis
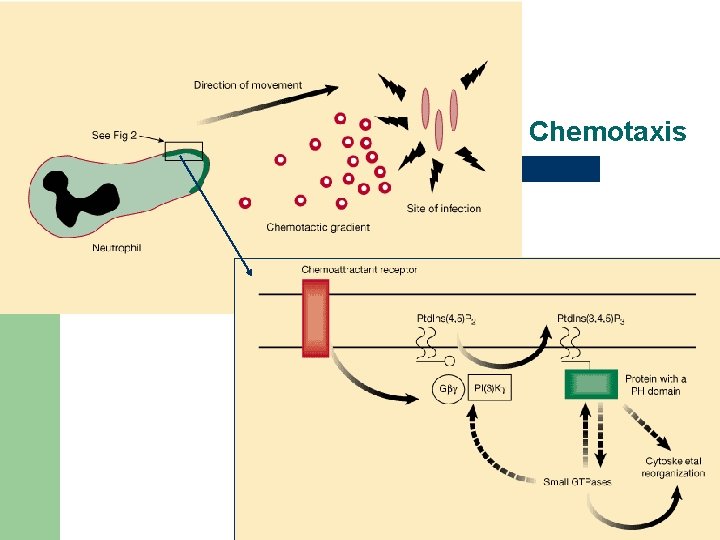
Chemotaxis
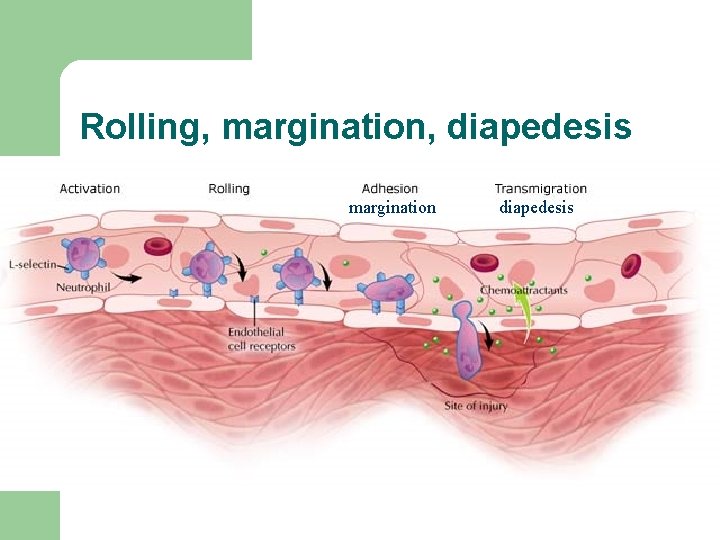
Rolling, margination, diapedesis margination diapedesis
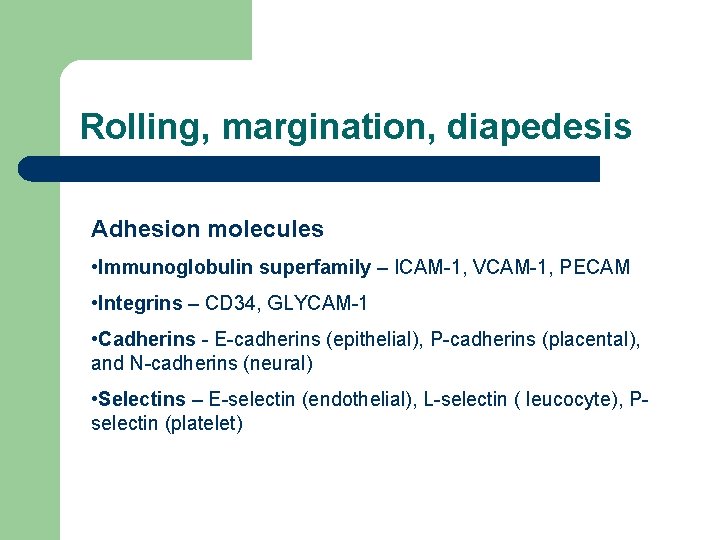
Rolling, margination, diapedesis Adhesion molecules • Immunoglobulin superfamily – ICAM-1, VCAM-1, PECAM • Integrins – CD 34, GLYCAM-1 • Cadherins - E-cadherins (epithelial), P-cadherins (placental), and N-cadherins (neural) • Selectins – E-selectin (endothelial), L-selectin ( leucocyte), Pselectin (platelet)
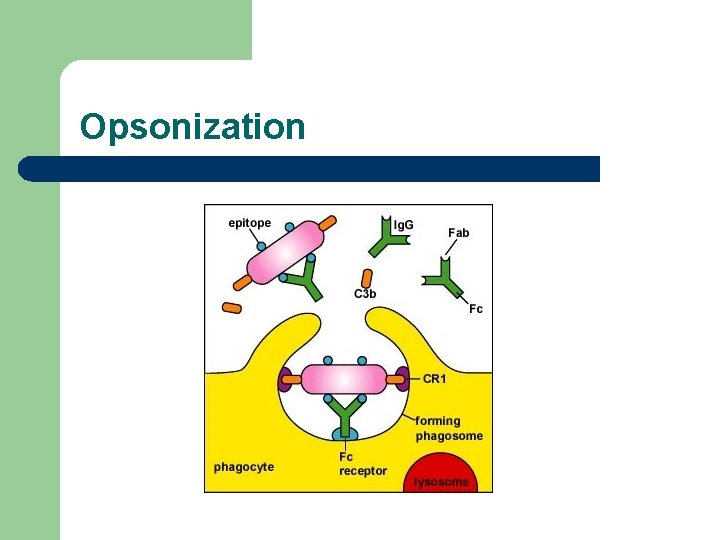
Opsonization
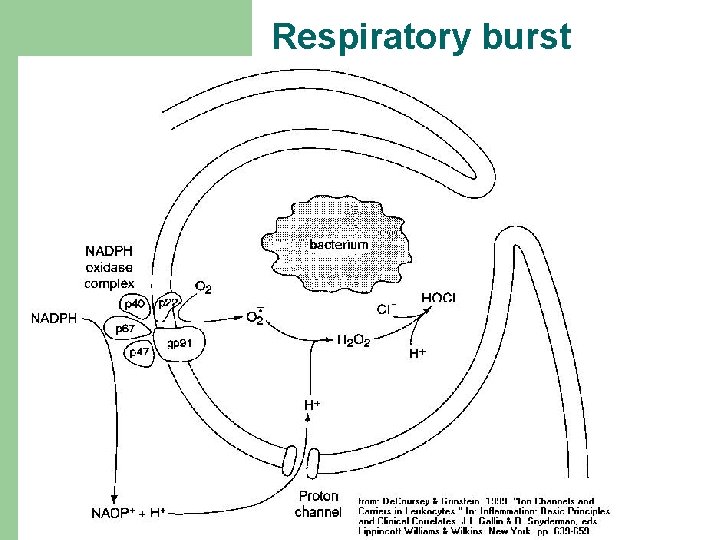
Respiratory burst
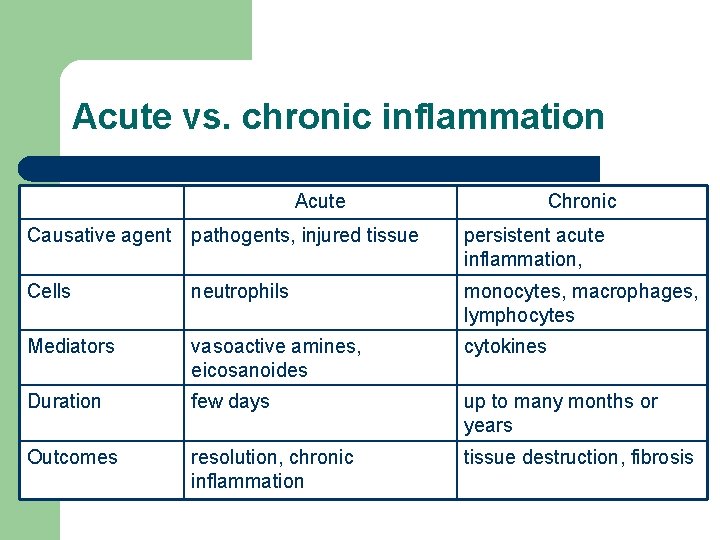
Acute vs. chronic inflammation Acute Chronic Causative agent pathogents, injured tissue persistent acute inflammation, Cells neutrophils monocytes, macrophages, lymphocytes Mediators vasoactive amines, eicosanoides cytokines Duration few days up to many months or years Outcomes resolution, chronic inflammation tissue destruction, fibrosis
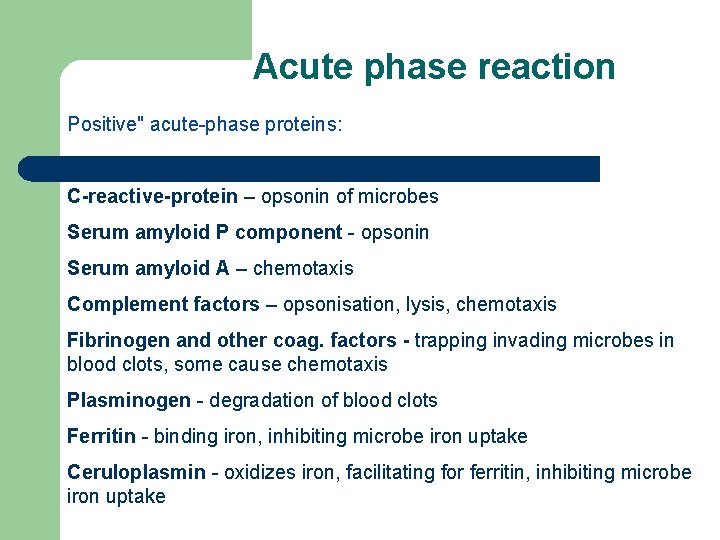
Acute phase reaction Positive" acute-phase proteins: C-reactive-protein – opsonin of microbes Serum amyloid P component - opsonin Serum amyloid A – chemotaxis Complement factors – opsonisation, lysis, chemotaxis Fibrinogen and other coag. factors - trapping invading microbes in blood clots, some cause chemotaxis Plasminogen - degradation of blood clots Ferritin - binding iron, inhibiting microbe iron uptake Ceruloplasmin - oxidizes iron, facilitating for ferritin, inhibiting microbe iron uptake
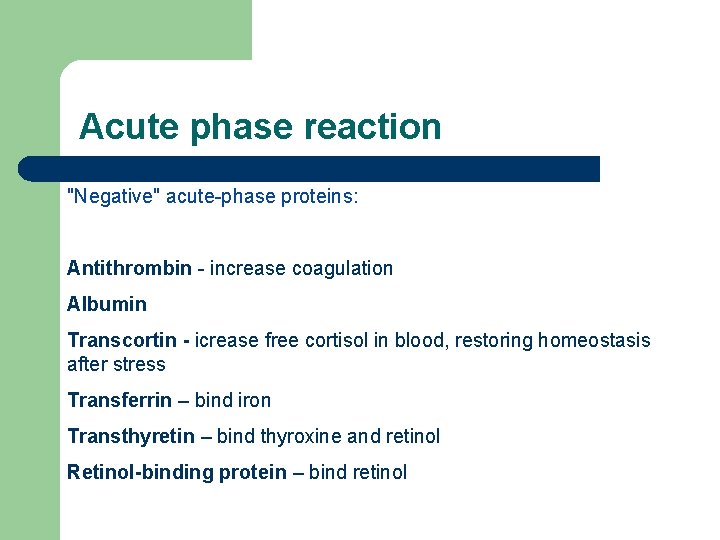
Acute phase reaction "Negative" acute-phase proteins: Antithrombin - increase coagulation Albumin Transcortin - icrease free cortisol in blood, restoring homeostasis after stress Transferrin – bind iron Transthyretin – bind thyroxine and retinol Retinol-binding protein – bind retinol
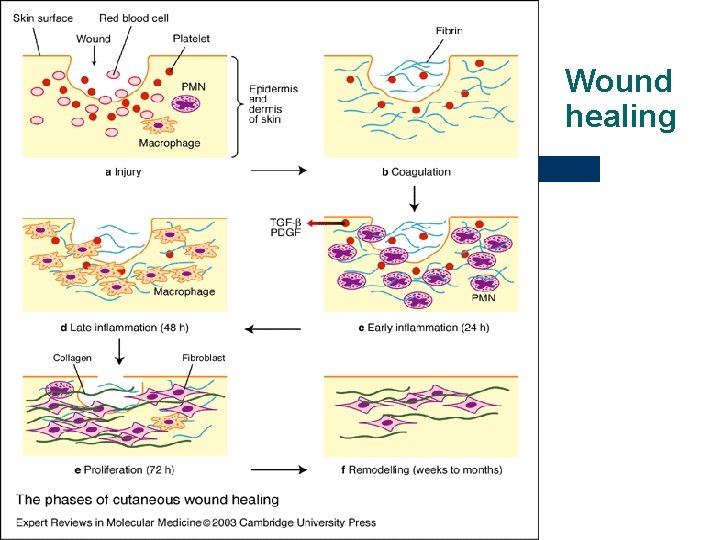
Wound healing 1. phase – Hemostasis l l vasoconstriction platelets adhesion coagulation growth factors – PDGF → activation of fibroblasts → collagen fibril construction 2. phase – Inflammation l l l vasodilatation from 6 -8 up to 24 -48 hours - polymorphonucler leucocytes – phagocytosis – „cleaning“ of the wound, clearing it from debris later – monocytes, macrophages - phagocytosis
Wound healing 3. phase – Granulation l l l angiogenesis – neovascularization - growth factors (EGF) – migration of endothelial cells - new vessels collagen deposition - migration of fibroblasts into wound – lay down collagen III glycosaminoglycans and proteogycans contribute to matrix deposition formation of granulation tissue contraction of wound – myofibroblasts (fibroblasts/smooth muscle cells) – reduction of wound size (40 - 80 %) epithelialization – epithelial cells – barrier between wound environment
Wound healing 4. phase – Remodeling l l l collagen production and degradation equilibrium collagen III is replaced by collagen I scar
Wound healing
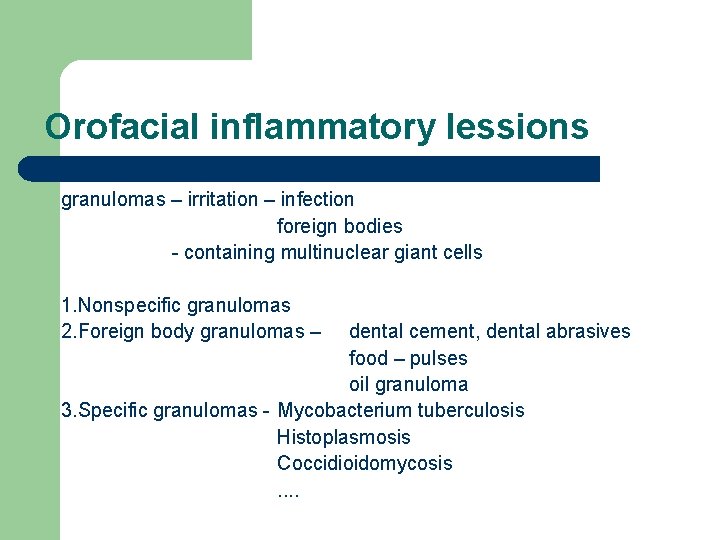
Orofacial inflammatory lessions granulomas – irritation – infection foreign bodies - containing multinuclear giant cells 1. Nonspecific granulomas 2. Foreign body granulomas – dental cement, dental abrasives food – pulses oil granuloma 3. Specific granulomas - Mycobacterium tuberculosis Histoplasmosis Coccidioidomycosis. .
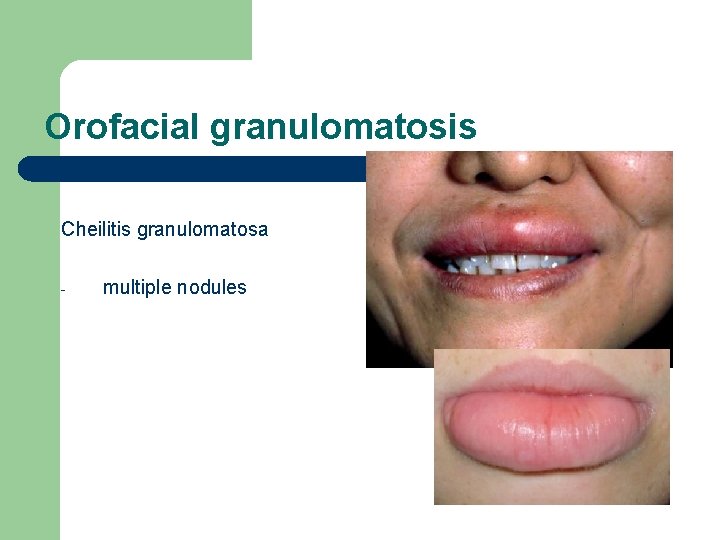
Orofacial granulomatosis Cheilitis granulomatosa - multiple nodules
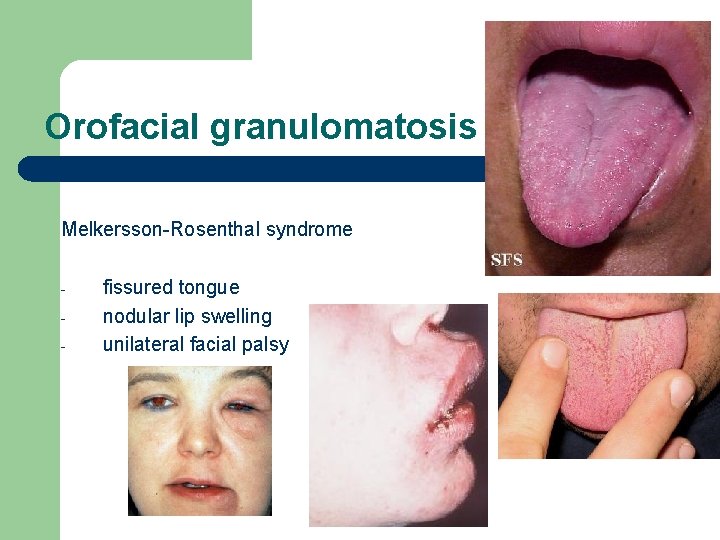
Orofacial granulomatosis Melkersson-Rosenthal syndrome - fissured tongue nodular lip swelling unilateral facial palsy
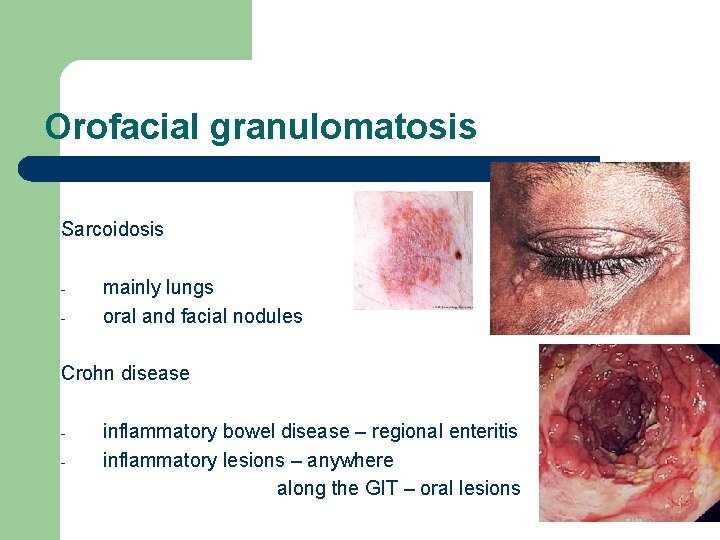
Orofacial granulomatosis Sarcoidosis - mainly lungs oral and facial nodules Crohn disease - inflammatory bowel disease – regional enteritis inflammatory lesions – anywhere along the GIT – oral lesions
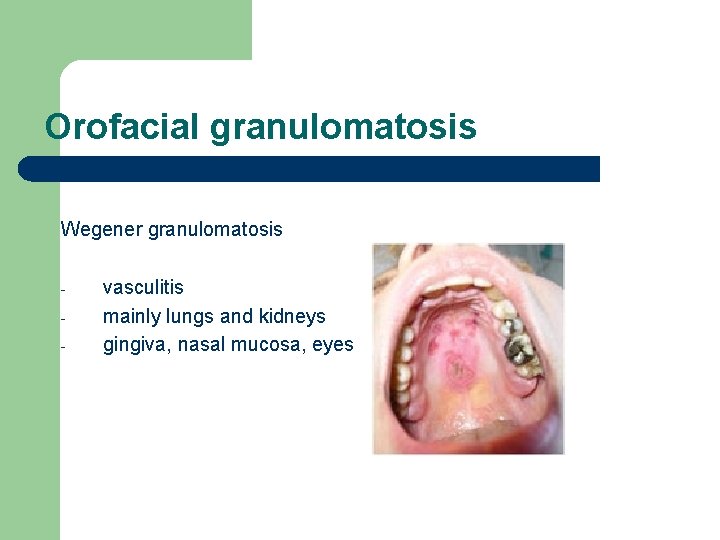
Orofacial granulomatosis Wegener granulomatosis - vasculitis mainly lungs and kidneys gingiva, nasal mucosa, eyes
- Slides: 41