Inflammation and atherosclerosis Immune cells dominate early lesions
- Slides: 34
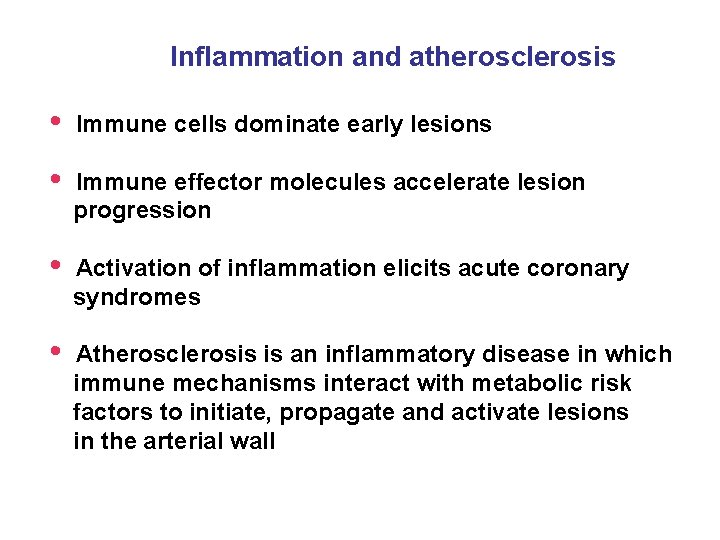
Inflammation and atherosclerosis • Immune cells dominate early lesions • Immune effector molecules accelerate lesion progression • Activation of inflammation elicits acute coronary syndromes • Atherosclerosis is an inflammatory disease in which immune mechanisms interact with metabolic risk factors to initiate, propagate and activate lesions in the arterial wall
The numbers • CAD causes 38% of all deaths in North America • Most common cause of death in men under 65 y. o. and second most common cause of women • Dispite advances in control of hypercholesterolemia (statins), CVD expected to be the main cause of death globally over the next 15 years due to rapidly increasing prevalence of obesity and diabetes
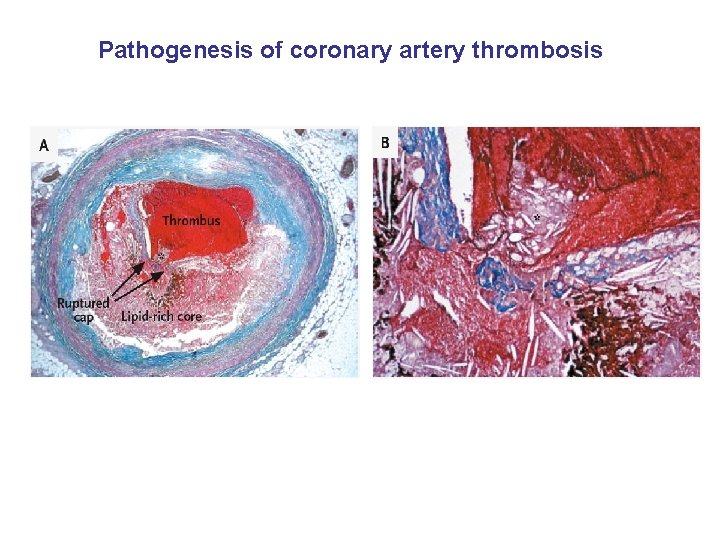
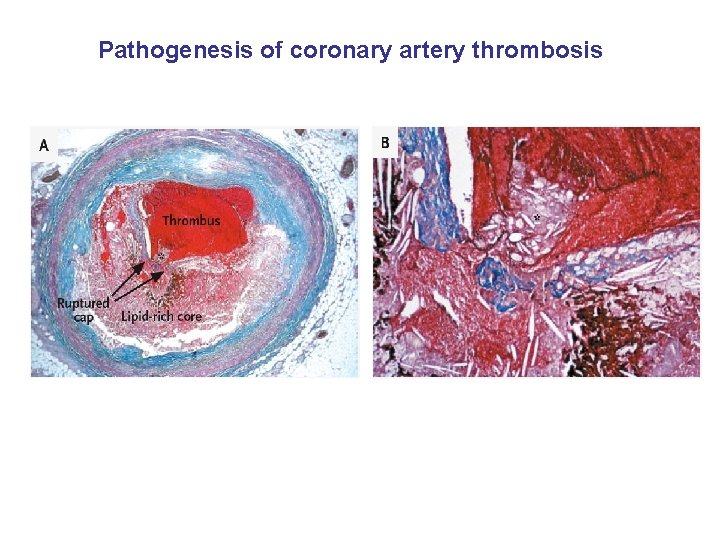
Pathogenesis of coronary artery thrombosis
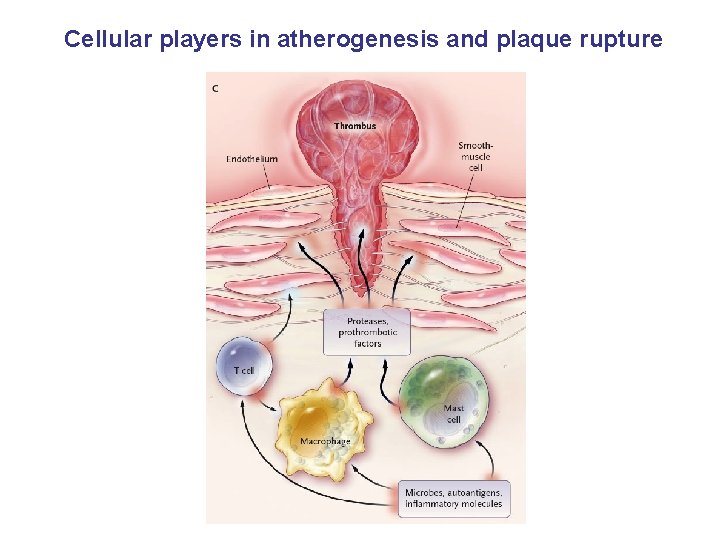
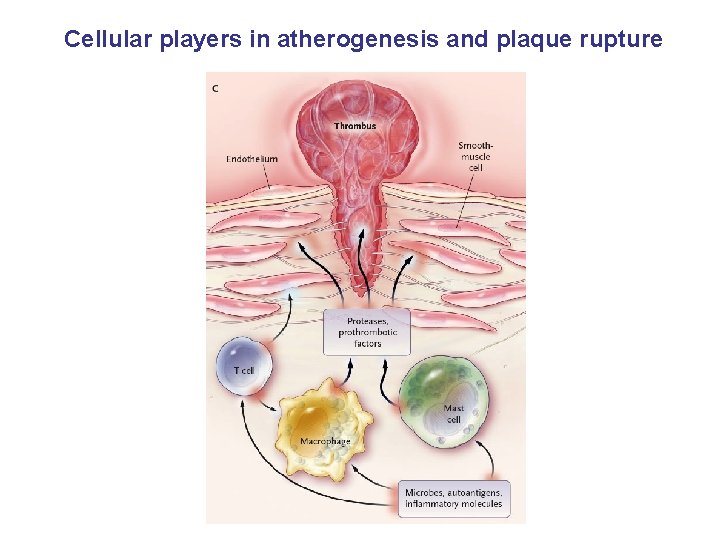
Cellular players in atherogenesis and plaque rupture
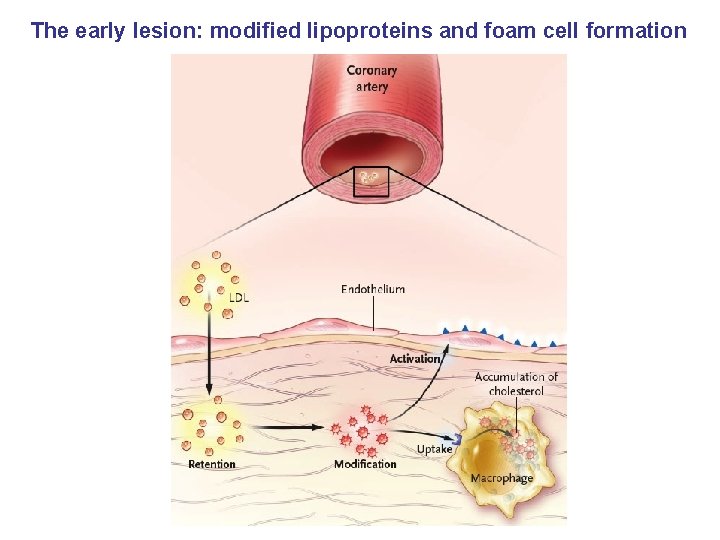
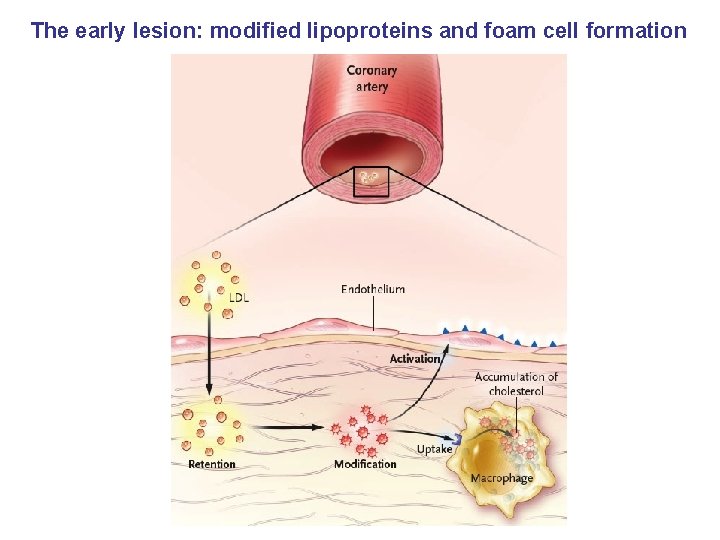
The early lesion: modified lipoproteins and foam cell formation
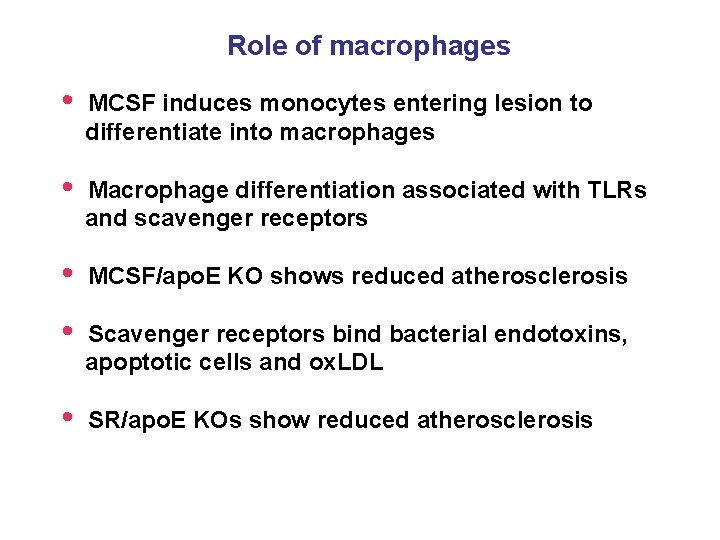
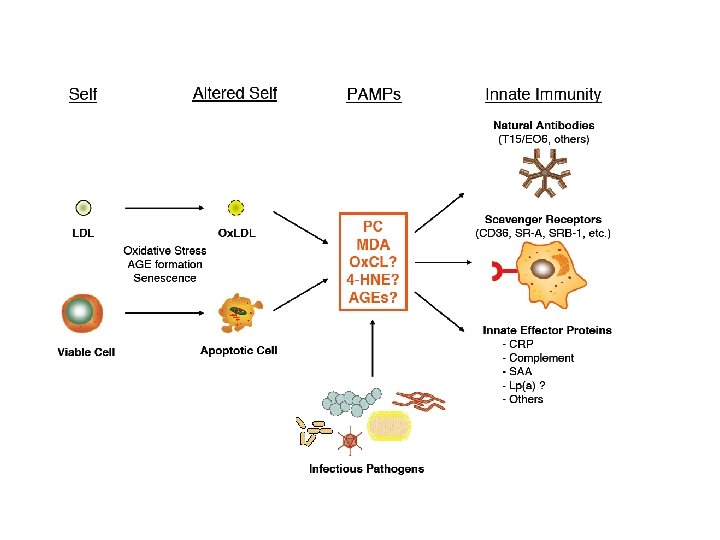
Role of macrophages • MCSF induces monocytes entering lesion to differentiate into macrophages • Macrophage differentiation associated with TLRs and scavenger receptors • MCSF/apo. E KO shows reduced atherosclerosis • Scavenger receptors bind bacterial endotoxins, apoptotic cells and ox. LDL • SR/apo. E KOs show reduced atherosclerosis
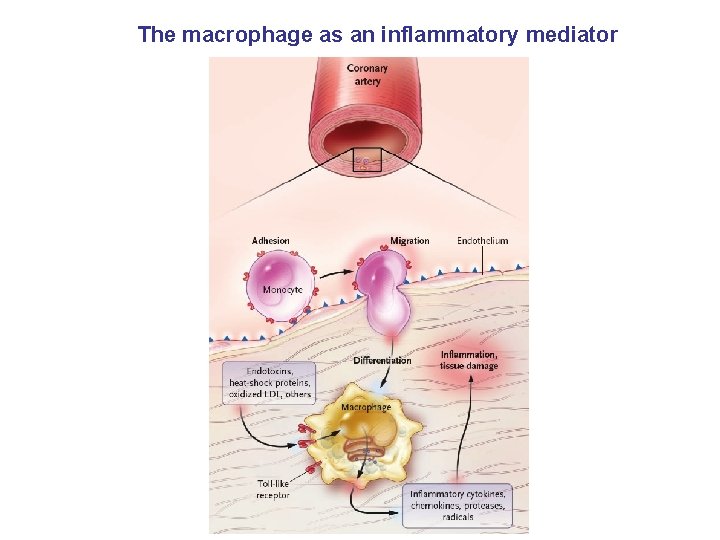
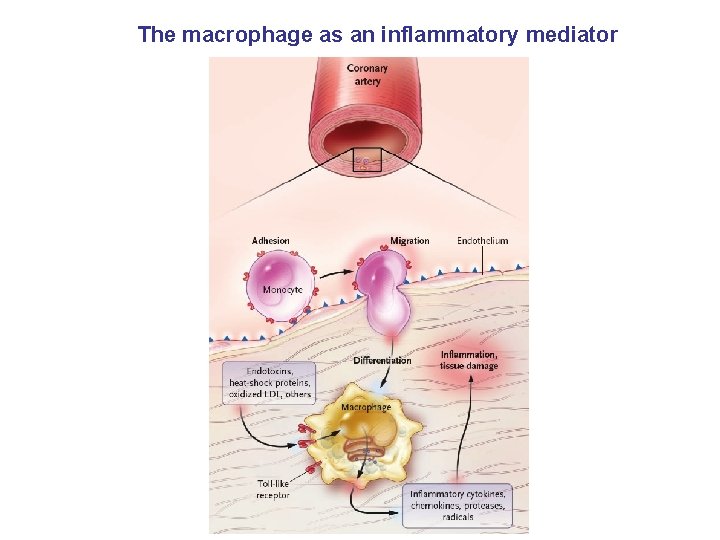
The macrophage as an inflammatory mediator
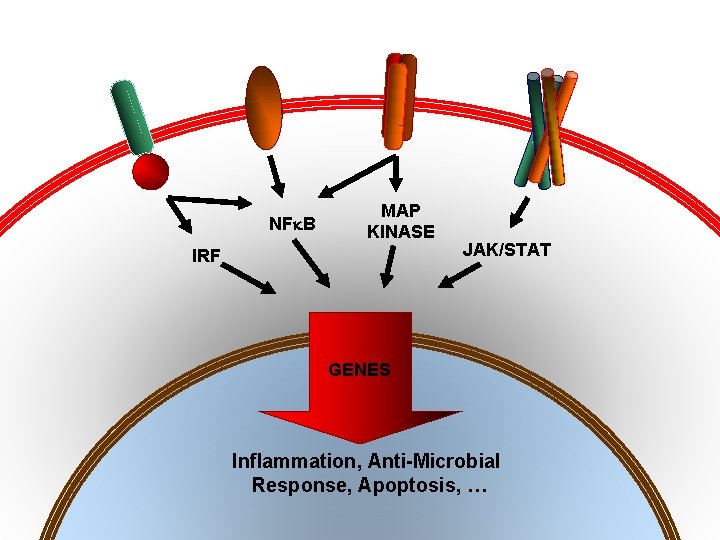
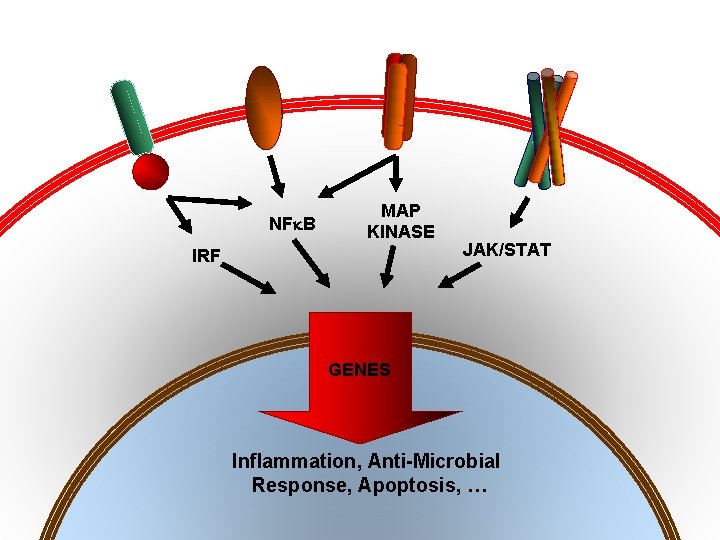
TNF-R IL-1 R IFN-g. R Toll-like NF B MAP KINASE IRF JAK/STAT GENES Inflammation, Anti-Microbial Response, Apoptosis, …
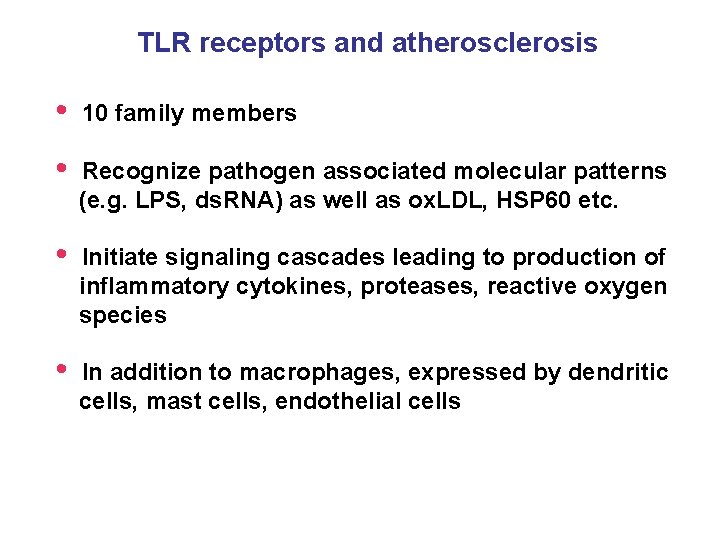
TLR receptors and atherosclerosis • 10 family members • Recognize pathogen associated molecular patterns (e. g. LPS, ds. RNA) as well as ox. LDL, HSP 60 etc. • Initiate signaling cascades leading to production of inflammatory cytokines, proteases, reactive oxygen species • In addition to macrophages, expressed by dendritic cells, mast cells, endothelial cells
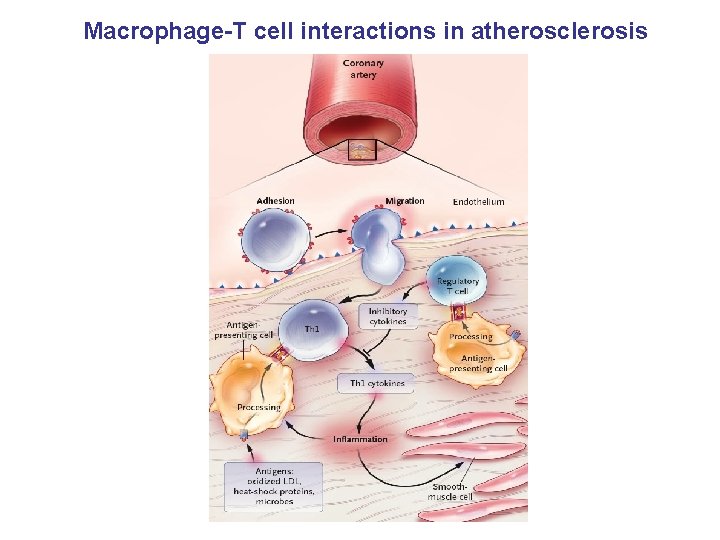
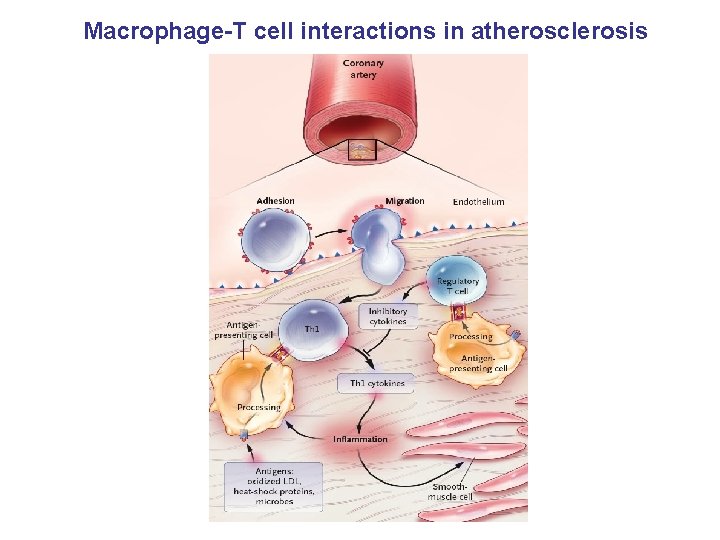
Macrophage-T cell interactions in atherosclerosis
T cells and atherosclerosis • Immune cells patrol tissues in search of antigen • T cell infiltrate is common feature of atherosclerotic lesions • Predominantly CD 4+ cells, recognize antigen/MHC II • CD 4+ T cells reactive to ox. LDL, HSP 60, bacterial products detected in human lesions • NK cells present in early lesions, recognize lipid antigens • NK activation increases athero in apo. E KO mice
T cell responses • Th 1 response activates macrophages and functions in the defense against intracellular pathogens • • Th 2 response elicits allergic inflammation • Activated Th 1 effector cells in lesions produce macrophage activating cytokine IFNg • IFNg improves efficiency of ag presentation and augments synthesis of TNFa and IL-1 • IFNg, TNFa and IL-1 in turn stimulate production of many other inflammatory mediators • apo. E mice lacking IFNg or downstream mediators such as IL-18 or T-bet show reduced athero Atherosclerotic lesions contains cytokines that promote Th 1 responses
Anti-inflammatory factors and atherosclerosis • Anti-inflammatory factors such as TGF and IL-10 are protective • IL-10 KO increases athero in mice and exacerbates thrombosis • Abrogation of TGF signaling in T cells leads to large unstable atherosclerotic lesions
Immune cells and plaque rupture • Preferentially occurs where fibrous cap is thin • Active immune cells are abundant at site of rupture • Immune cells produce inflammatory molecules and proteolytic enzymes that weaken cap, activate cells in the core and transform stable plaque into vulnerable, leading to plaque rupture • MMPs likely to play important roles
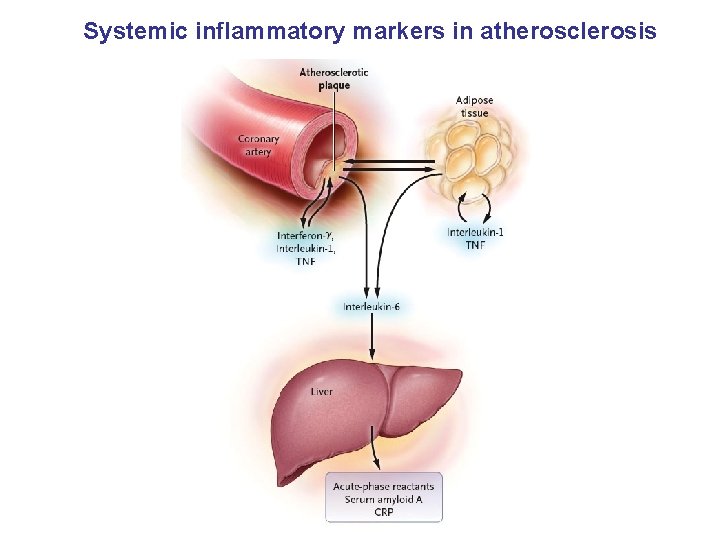
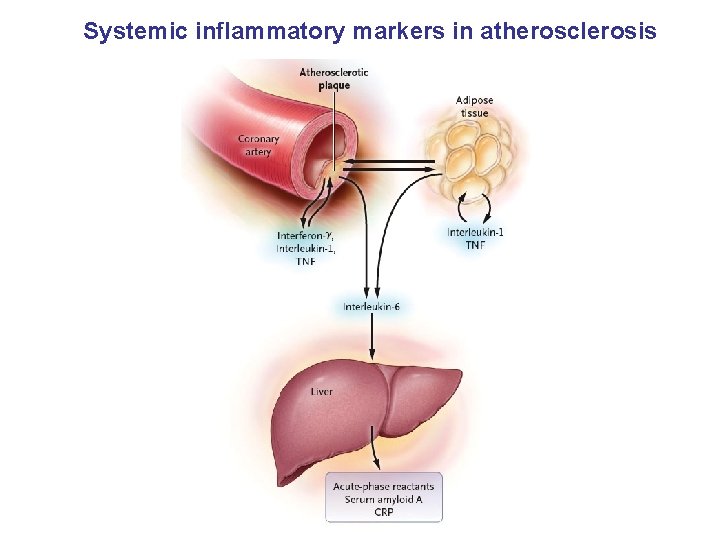
Systemic inflammatory markers in atherosclerosis
Systemic indicators of inflammation • Inflammatory process in lesions may lead to increased plasma levels of cytokines and acute phase proteins • CRP and IL-6 are elevated in patients with unstable angina and MI • Levels correlate with prognosis
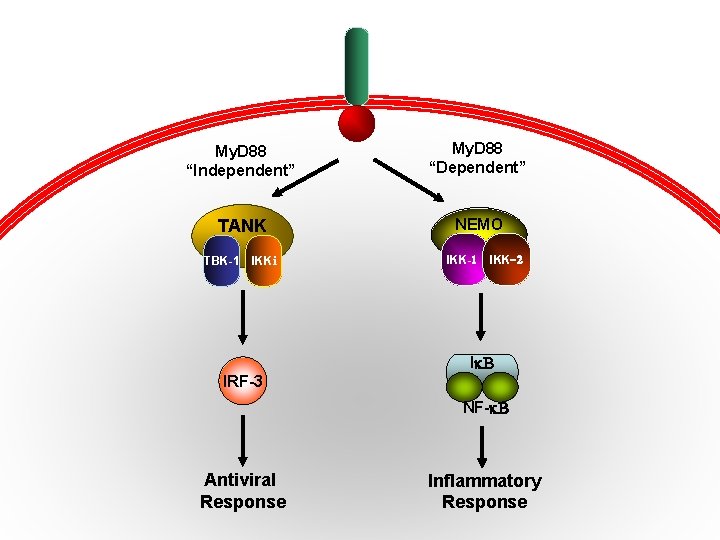
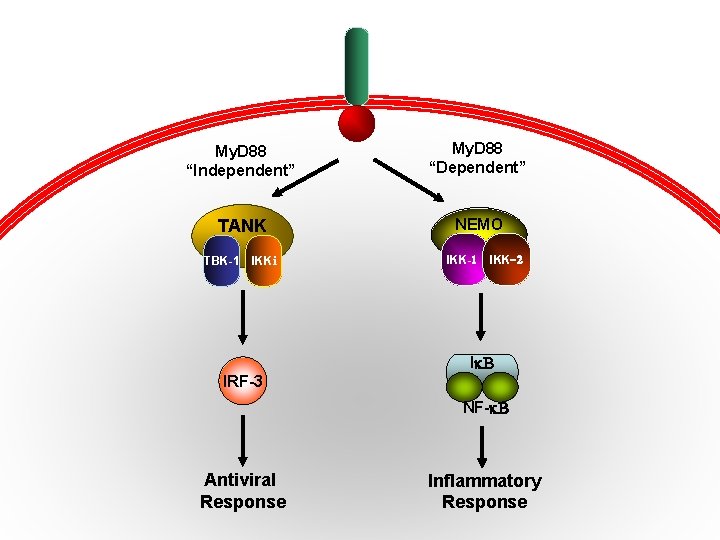
TLR-3/4 My. D 88 “Independent” My. D 88 “Dependent” TANK NEMO TBK-1 IKKi IKK-1 IKK-2 I B IRF-3 NF- B Antiviral Response Inflammatory Response
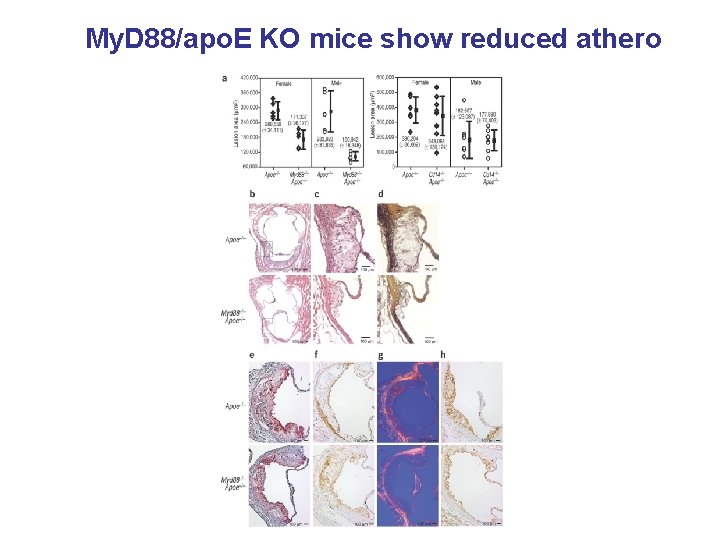
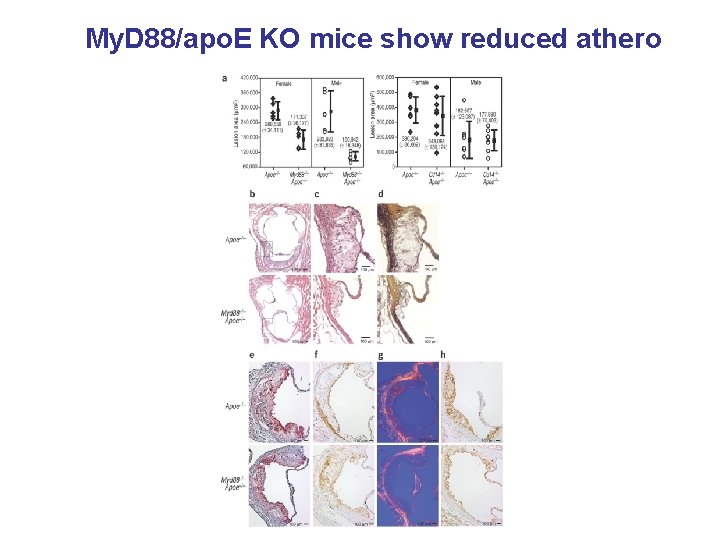
My. D 88/apo. E KO mice show reduced athero
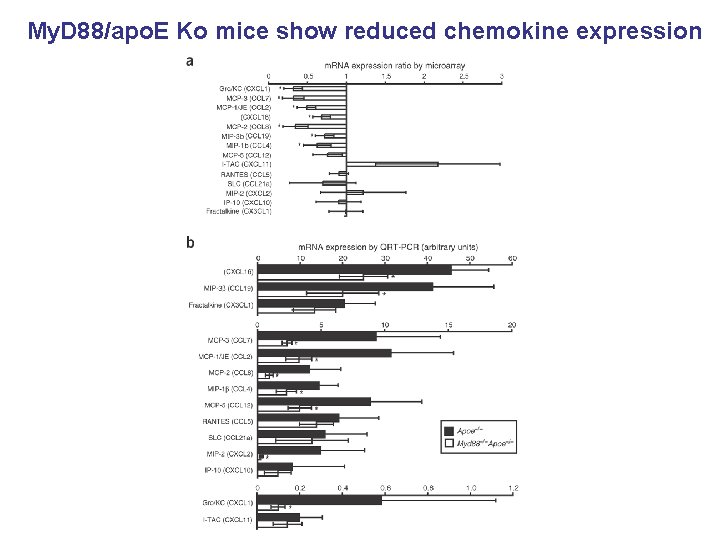
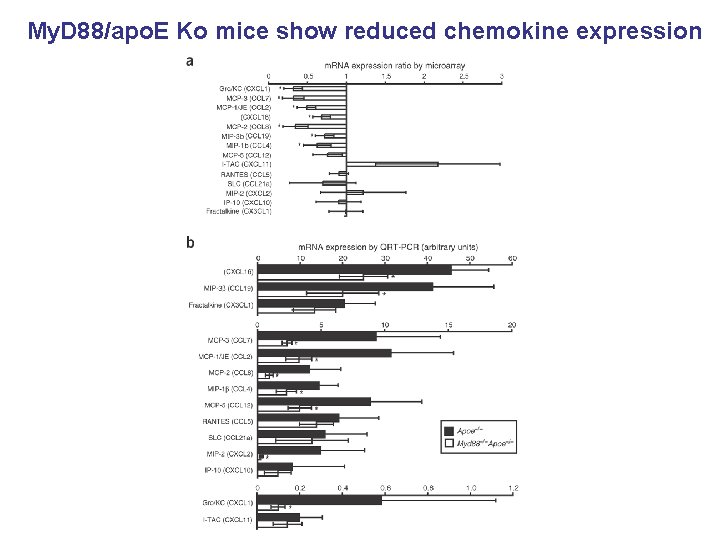
My. D 88/apo. E Ko mice show reduced chemokine expression
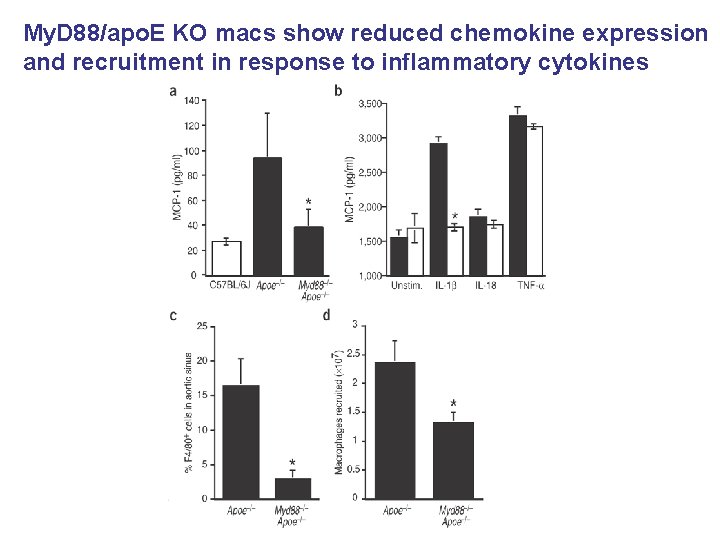
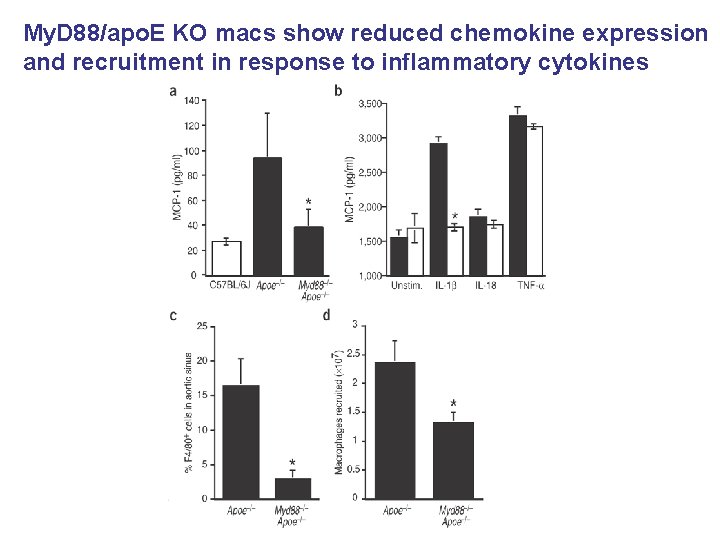
My. D 88/apo. E KO macs show reduced chemokine expression and recruitment in response to inflammatory cytokines
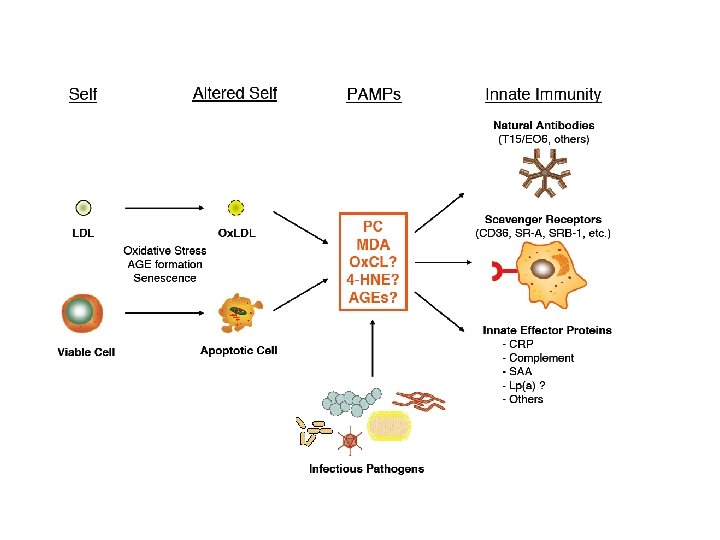
Links between infection and atherosclerosis • Unlikely to be caused by single organism • Diverse pathogens have been detected within lesions • Bacteria and viruses accelerate athero in murine models
Potential mechanisms • Stimulation of inflammatory cytokines • Alteration of adhesion molecule expression ? Lipid metabolism ?
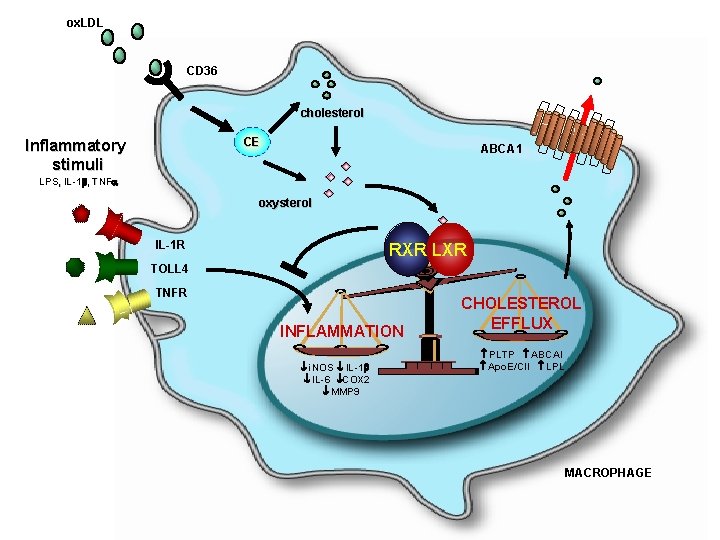
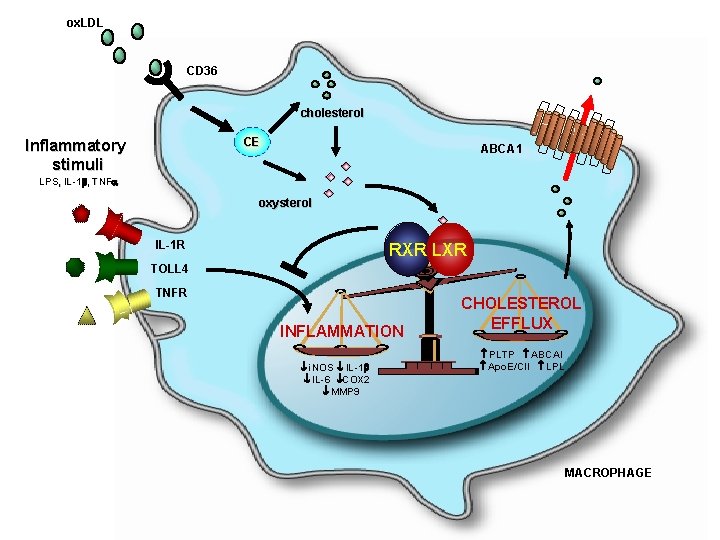
ox. LDL CD 36 cholesterol CE Inflammatory stimuli ABCA 1 LPS, IL-1 , TNFa oxysterol IL-1 R RXR LXR TOLL 4 TNFR INFLAMMATION i. NOS IL-1 IL-6 COX 2 MMP 9 CHOLESTEROL EFFLUX PLTP ABCAI Apo. E/CII LPL MACROPHAGE
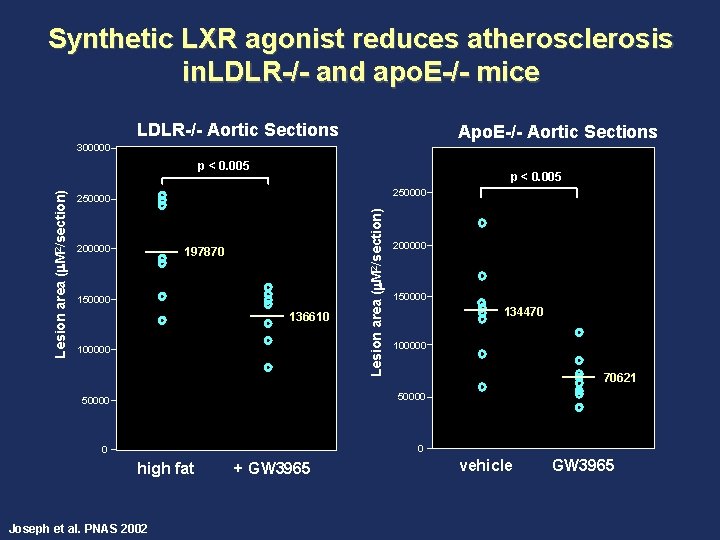
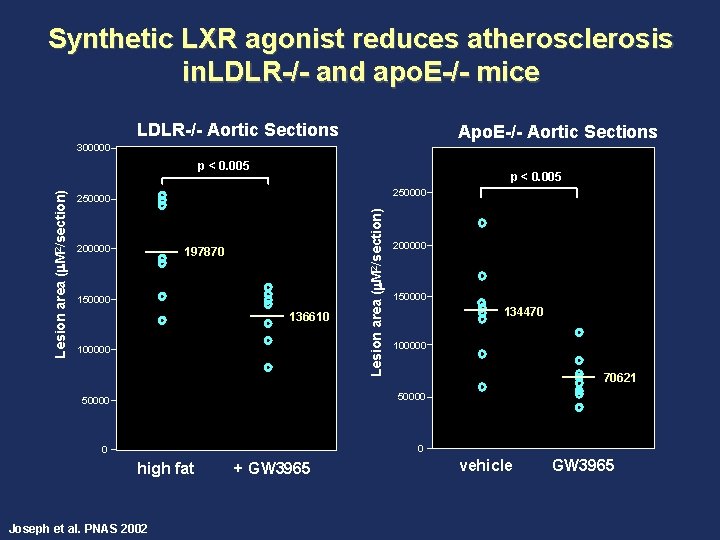
Synthetic LXR agonist reduces atherosclerosis in. LDLR-/- and apo. E-/- mice LDLR-/- Aortic Sections Apo. E-/- Aortic Sections 300000 p < 0. 005 250000 200000 197870 150000 136610 100000 Lesion area (m. M 2/section) p < 0. 005 200000 150000 134470 100000 70621 50000 0 0 high fat Joseph et al. PNAS 2002 + GW 3965 vehicle GW 3965
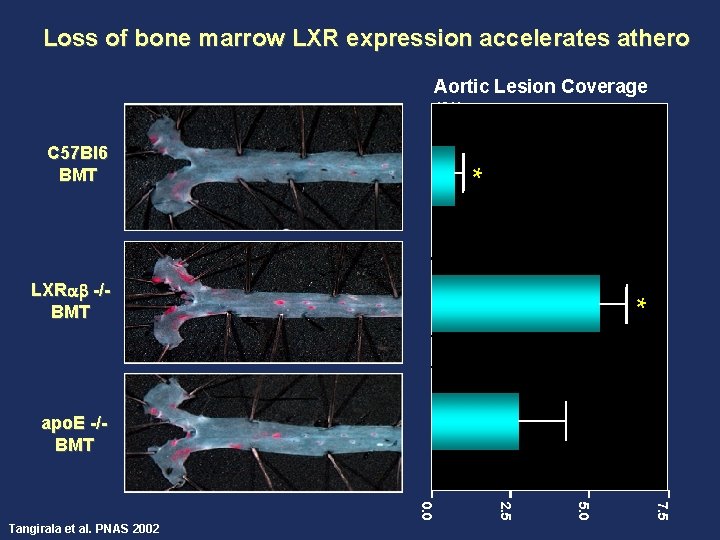
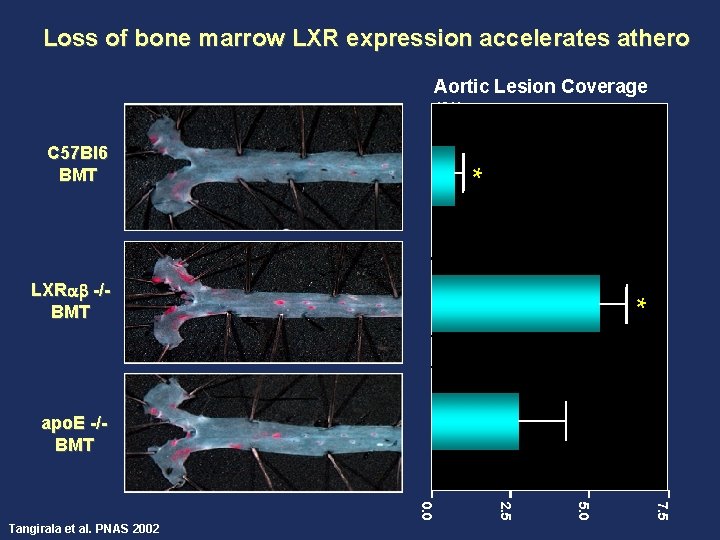
Loss of bone marrow LXR expression accelerates athero Aortic Lesion Coverage (%) * C 57 Bl 6 BMT * LXRa -/BMT apo. E -/BMT 7. 5 5. 0 2. 5 0. 0 Tangirala et al. PNAS 2002
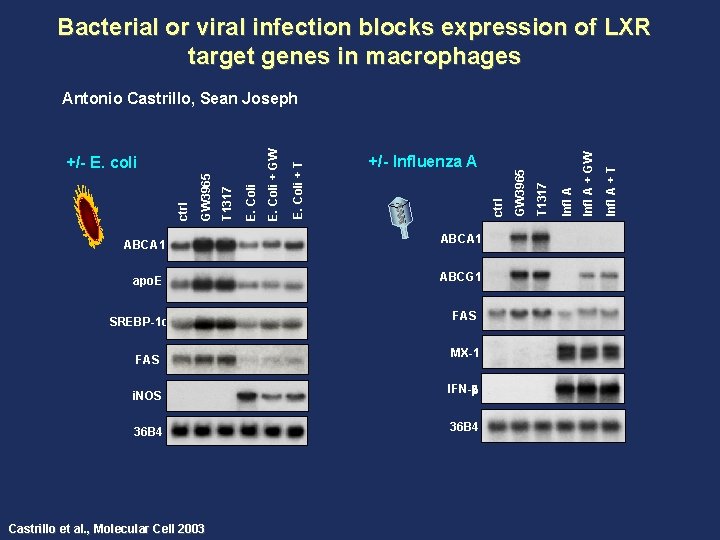
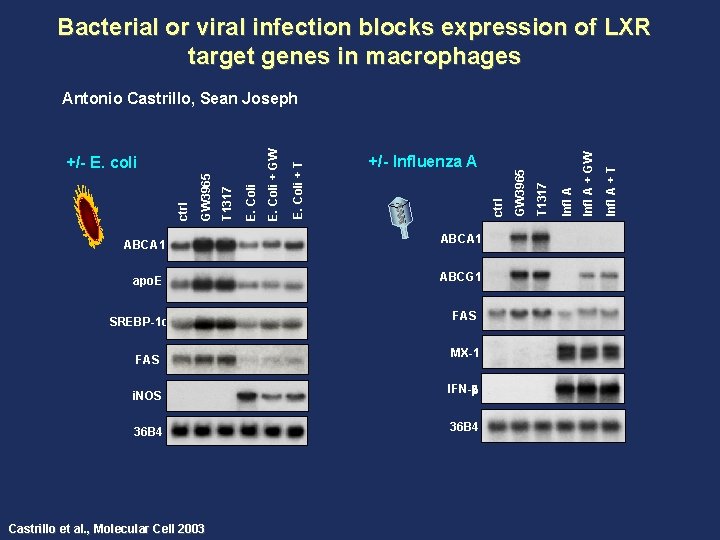
Bacterial or viral infection blocks expression of LXR target genes in macrophages ABCA 1 apo. E ABCG 1 SREBP-1 c FAS i. NOS 36 B 4 Castrillo et al. , Molecular Cell 2003 FAS MX-1 IFN- 36 B 4 Infl A + T Infl A + GW Infl A T 1317 GW 3965 +/- Influenza A ctrl E. Coli + T E. Coli T 1317 GW 3965 ctrl +/- E. coli E. Coli + GW Antonio Castrillo, Sean Joseph
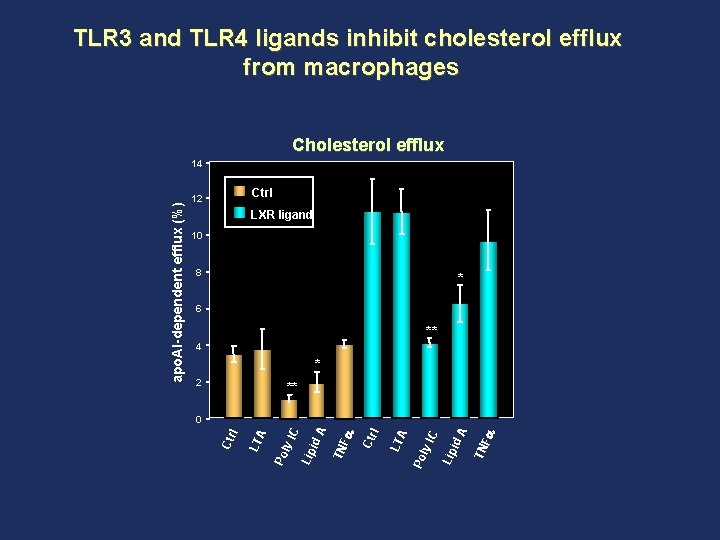
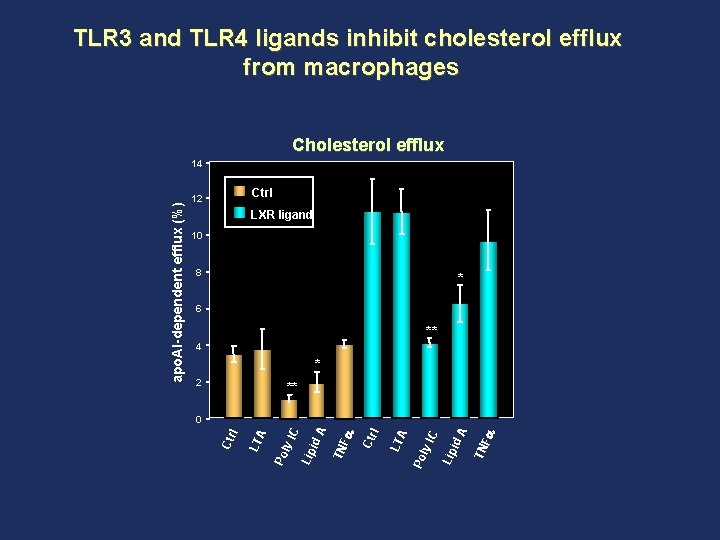
TLR 3 and TLR 4 ligands inhibit cholesterol efflux from macrophages Cholesterol efflux Ctrl 12 LXR ligand 10 8 * 6 ** 4 * 2 ** TN Fa Lip id A C ly I Po A LT l Ctr TN Fa C Lip id A ly I Po A LT l 0 Ctr apo. AI-dependent efflux (%) 14
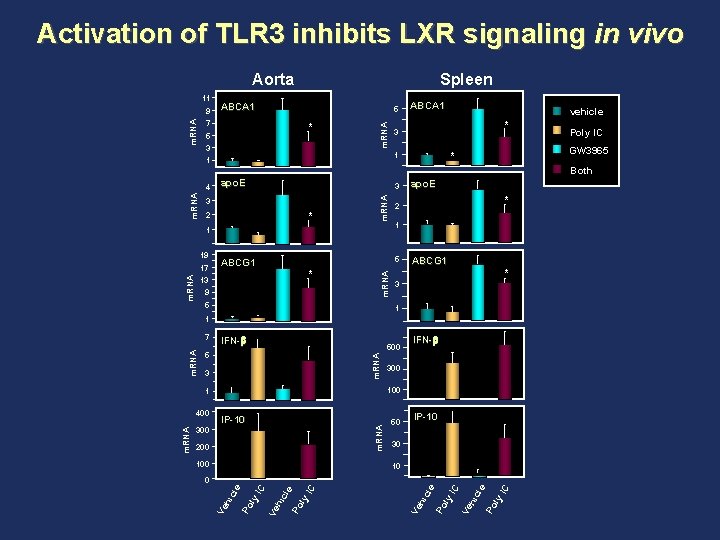
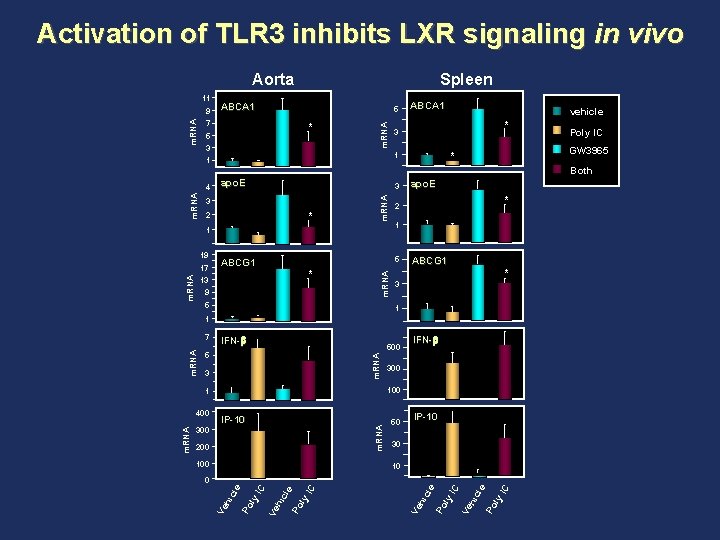
Activation of TLR 3 inhibits LXR signaling in vivo Aorta m. RNA 9 ABCA 1 5 7 * 5 3 1 m. RNA 11 Spleen ABCA 1 vehicle * 3 GW 3965 * 1 Poly IC Both 3 3 * 2 m. RNA 4 apo. E 1 m. RNA 17 * 13 9 5 * 2 1 5 ABCG 1 m. RNA 19 apo. E ABCG 1 * 3 1 1 IFN- 500 5 m. RNA 3 m. RNA IP-10 200 100 50 IP-10 30 10 icl e Po ly IC IC Ve h le Po ly hic IC IC le Po ly hic Ve Po ly hic le 0 Ve m. RNA 300 100 1 400 IFN- Ve m. RNA 7
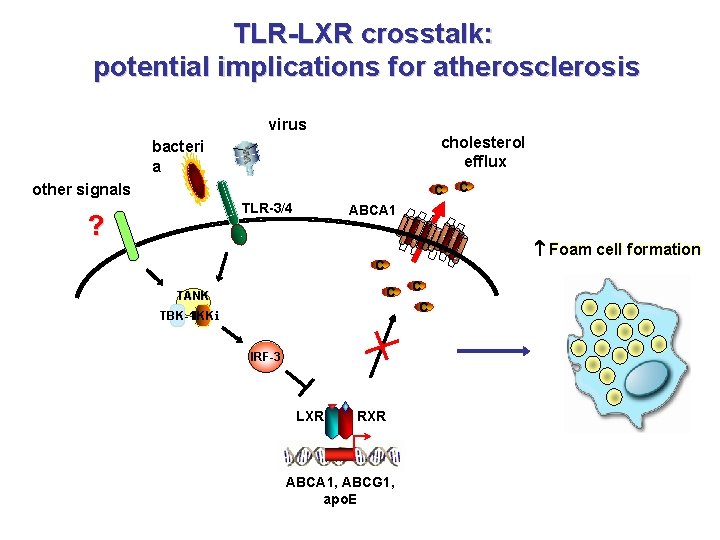
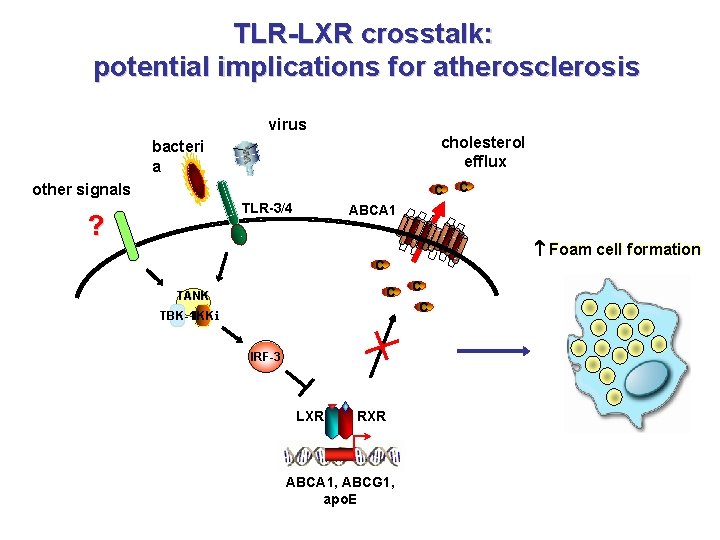
TLR-LXR crosstalk: potential implications for atherosclerosis virus cholesterol efflux bacteri a other signals C TLR-3/4 ? C ABCA 1 Foam cell formation C C TANK TBK-1 IKKi IRF-3 LXR RXR ABCA 1, ABCG 1, apo. E C C
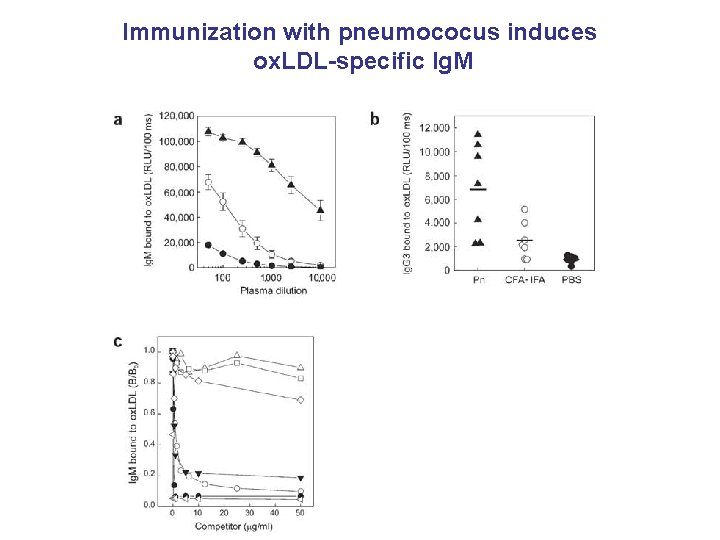
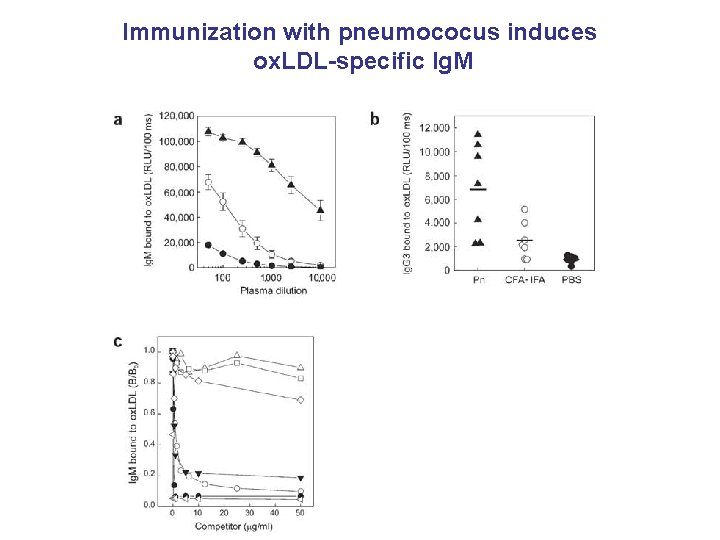
Immunization with pneumococus induces ox. LDL-specific Ig. M
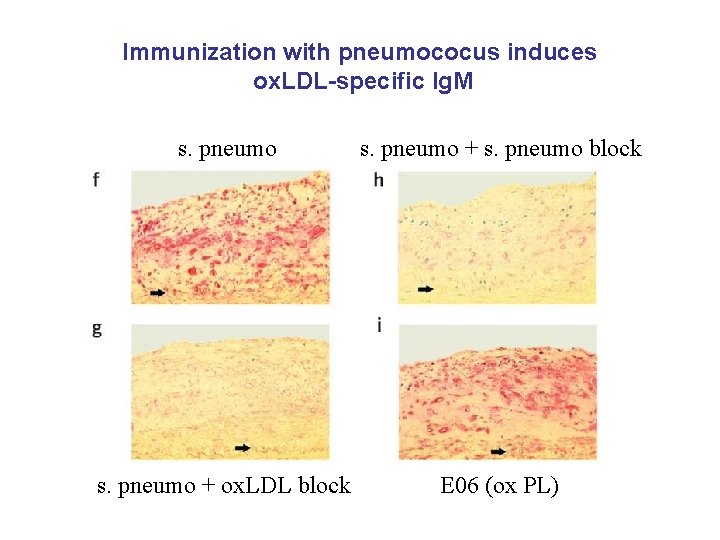
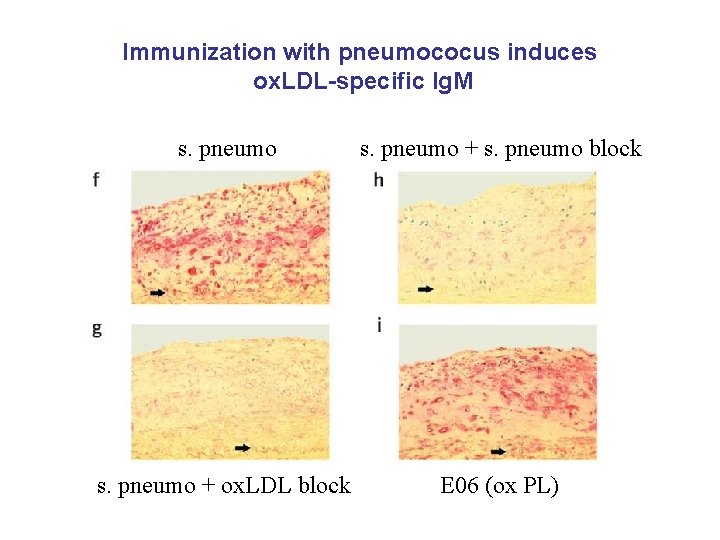
Immunization with pneumococus induces ox. LDL-specific Ig. M s. pneumo + s. pneumo block s. pneumo + ox. LDL block E 06 (ox PL)
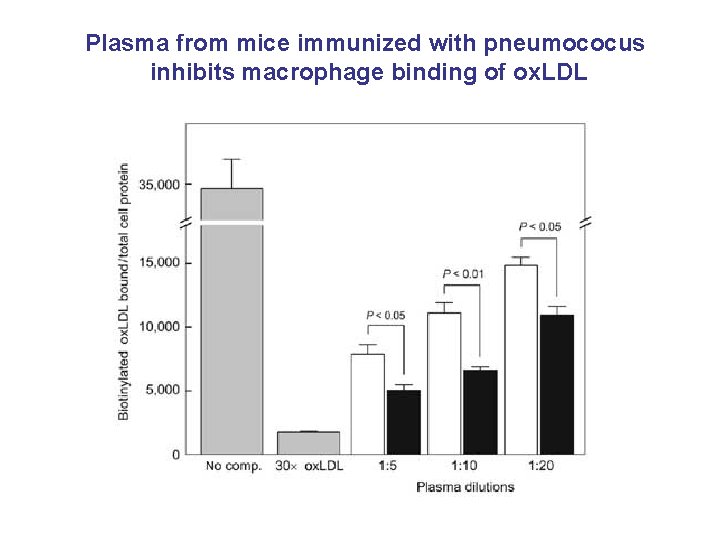
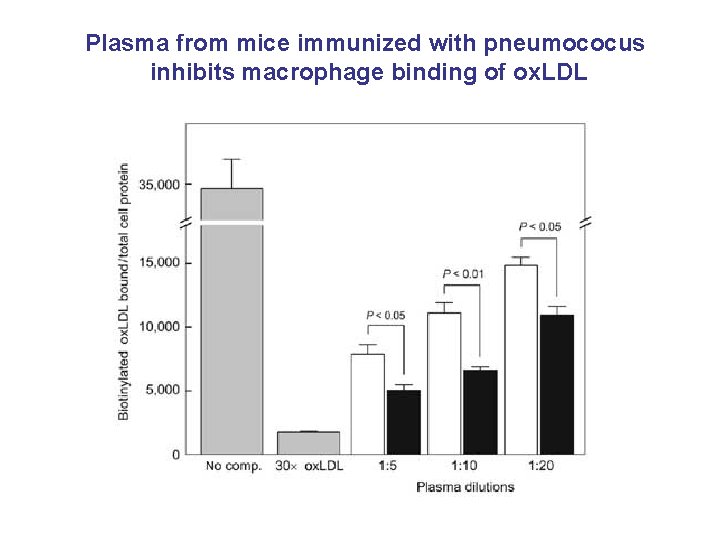
Plasma from mice immunized with pneumococus inhibits macrophage binding of ox. LDL
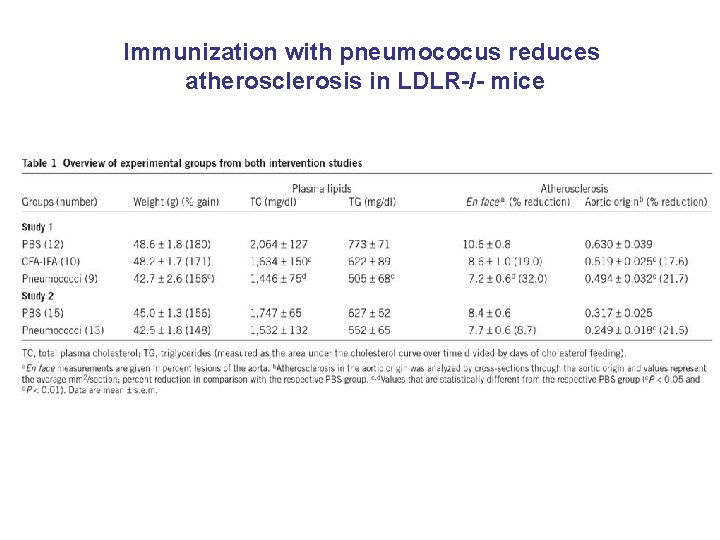
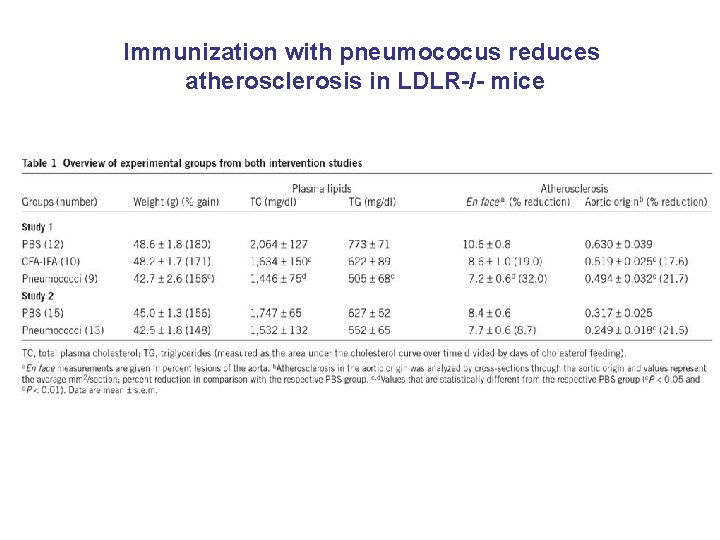
Immunization with pneumococus reduces atherosclerosis in LDLR-/- mice