INFERTILITY Mr Mathews Anyanwu UTG Definition Unprotected coital









- Slides: 40
INFERTILITY Mr Mathews Anyanwu UTG

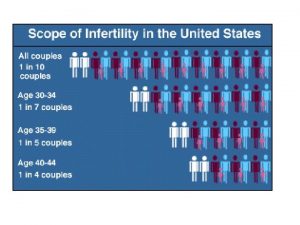
Definition Unprotected coital exposure for 12 months without conception.
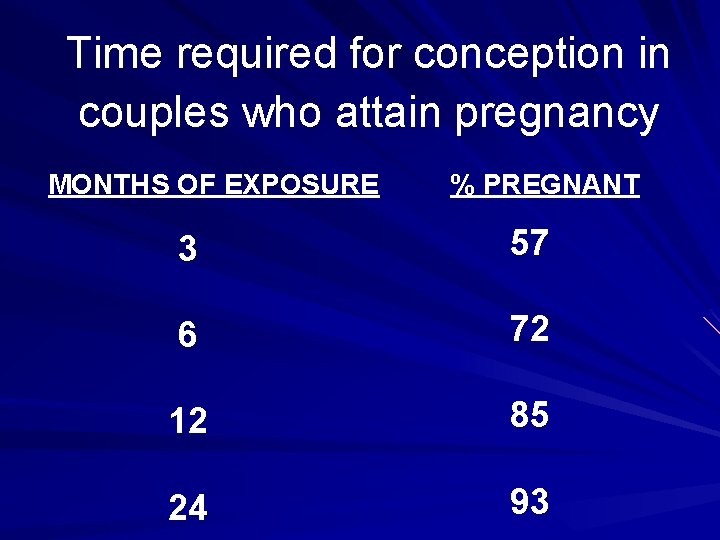
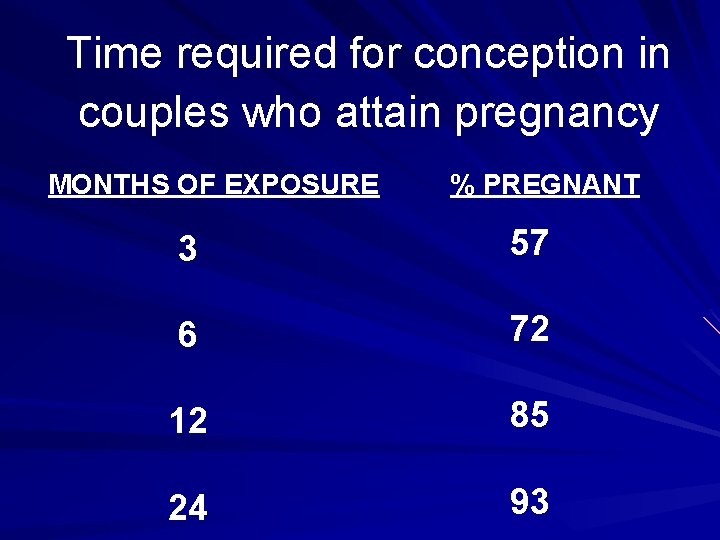
Time required for conception in couples who attain pregnancy MONTHS OF EXPOSURE % PREGNANT 3 57 6 72 12 85 24 93
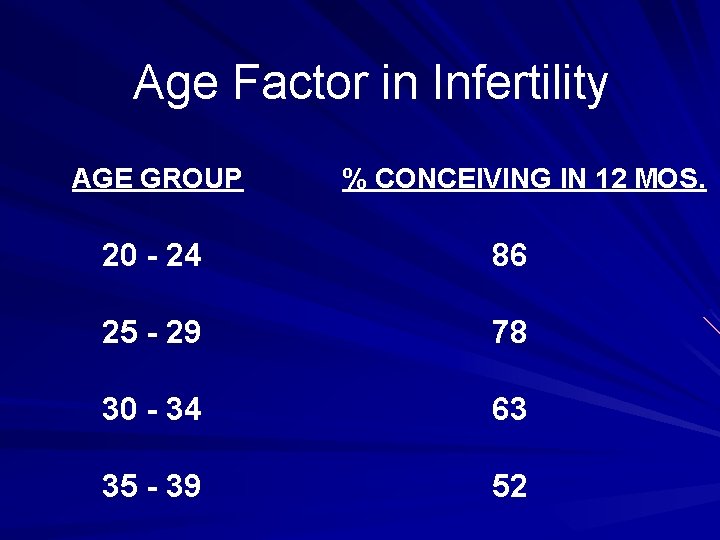
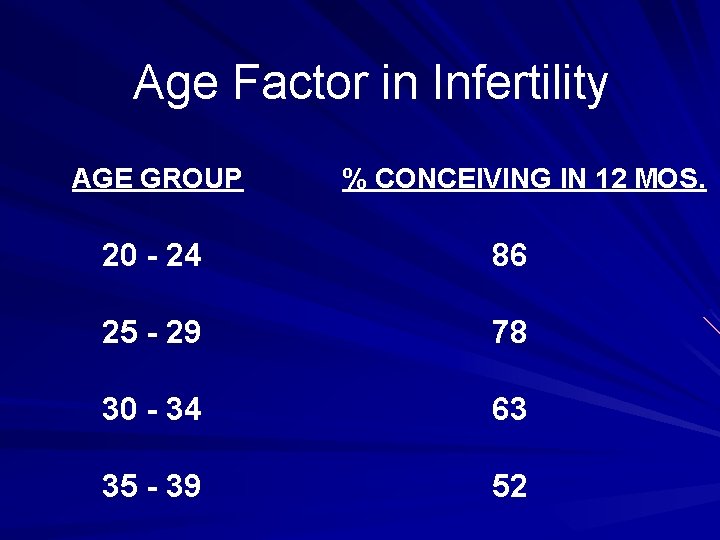
Age Factor in Infertility AGE GROUP % CONCEIVING IN 12 MOS. 20 - 24 86 25 - 29 78 30 - 34 63 35 - 39 52

Goals of Infertility Management Investigate and correct causes of infertility Provide accurate information and dispel myths Provide emotional support Counsel couples on when to stop
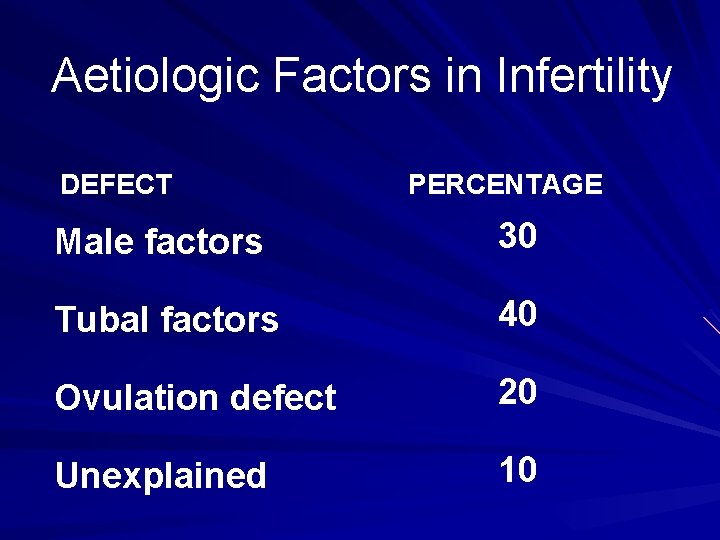
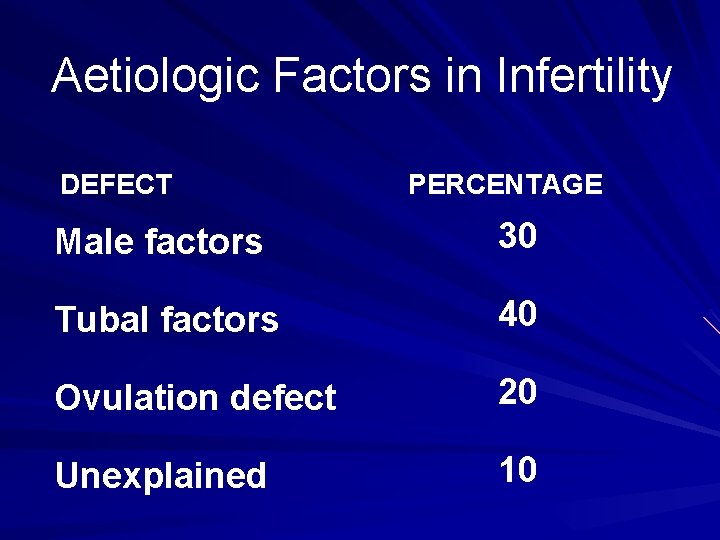
Aetiologic Factors in Infertility DEFECT PERCENTAGE Male factors 30 Tubal factors 40 Ovulation defect 20 Unexplained 10

Aetiologic Factors in Infertility the Gambia DEFECT PERCENTAGE Male factors 8. 9 Tubal factors 17. 8 Ovulation defect 13. 4 Unexplained 10
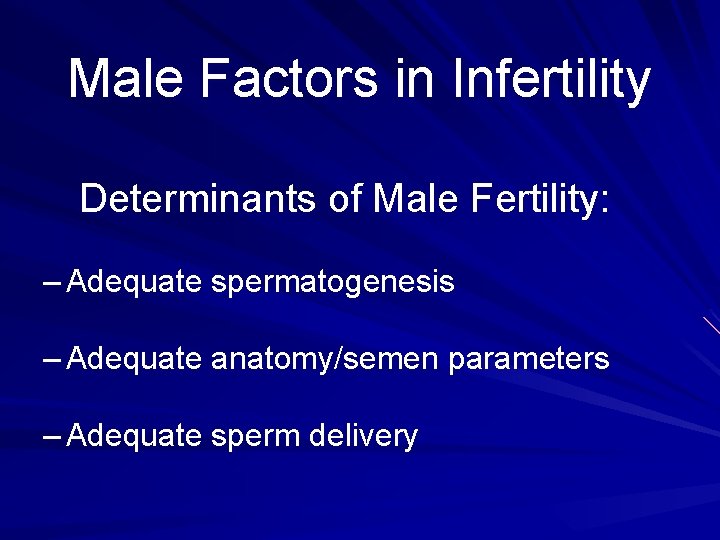
Male Factors in Infertility Determinants of Male Fertility: – Adequate spermatogenesis – Adequate anatomy/semen parameters – Adequate sperm delivery
Male Factors in Infertility: Defects in Spermatogenesis Endocrine dysfunction Genetic abnormalities Cryptorchidism Varicocele Exposure to elevated temperature Exposure to cytotoxic treatment or environmental toxins Infections
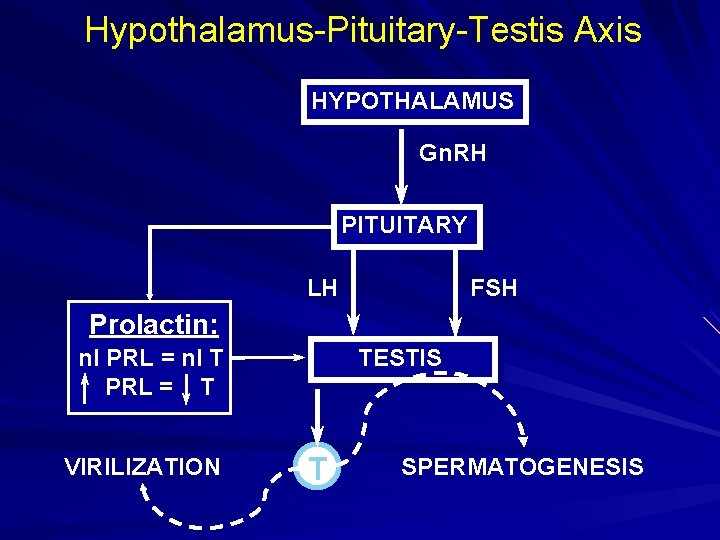
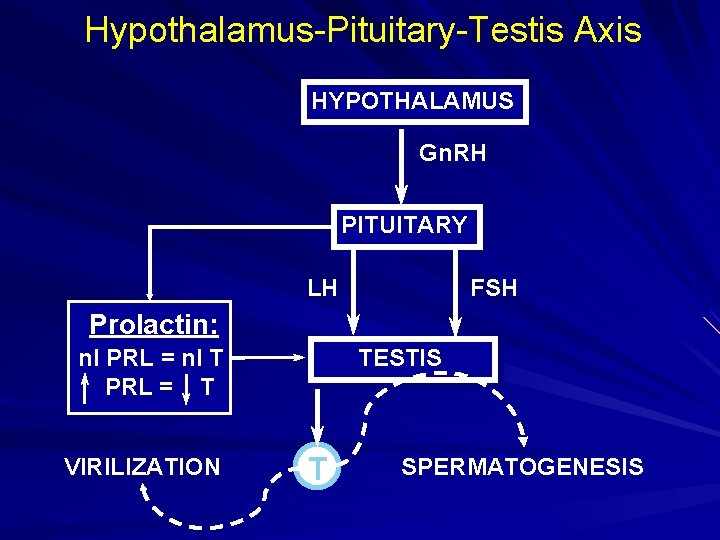
Hypothalamus-Pituitary-Testis Axis HYPOTHALAMUS Gn. RH PITUITARY LH FSH Prolactin: TESTIS nl PRL = nl T PRL = T VIRILIZATION T SPERMATOGENESIS
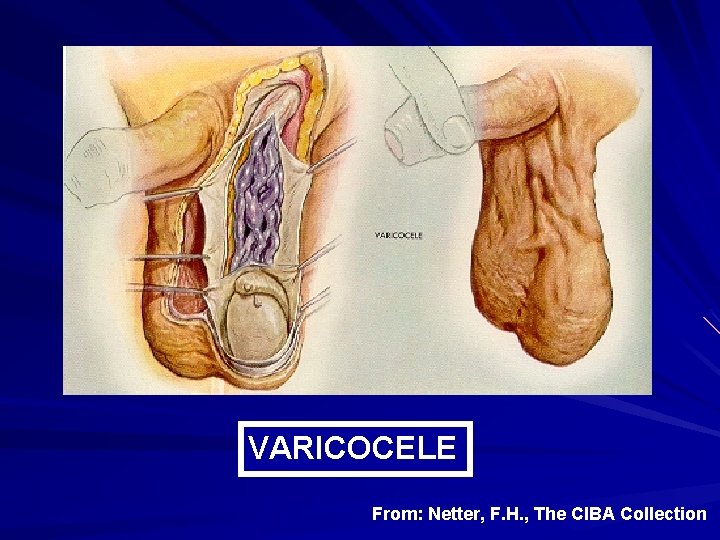
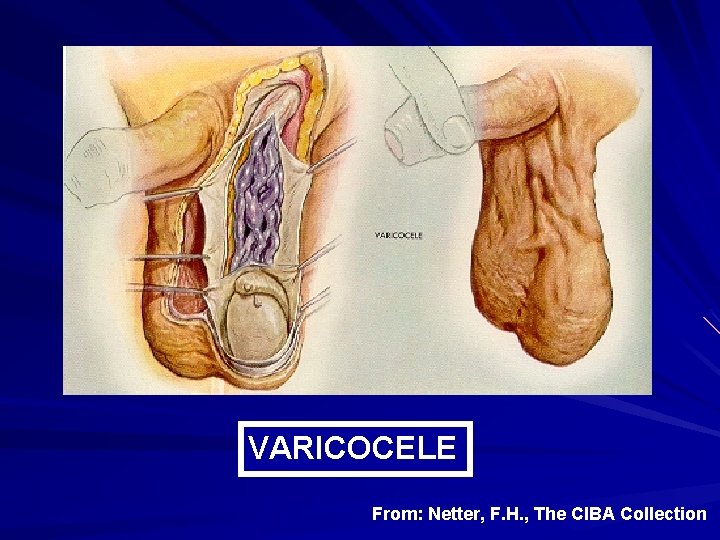
VARICOCELE From: Netter, F. H. , The CIBA Collection
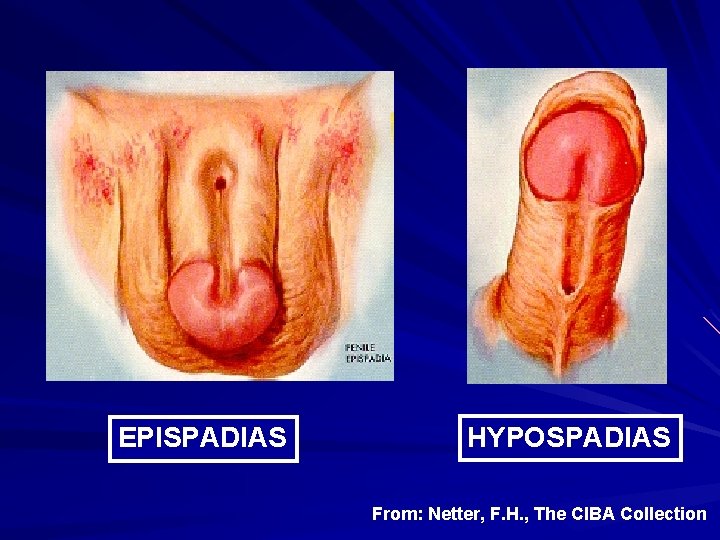
Male Factors in Infertility: Anatomical Abnormalities Congenital (e. g. , absence of vas deferens, hypo/epispadias) Acquired (infections, iatrogenic, traumatic)
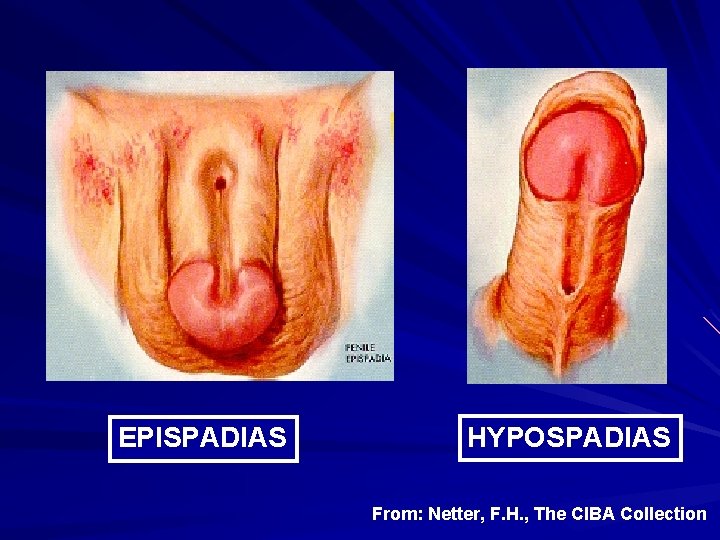
EPISPADIAS HYPOSPADIAS From: Netter, F. H. , The CIBA Collection
Male Factors in Infertility: Physiological Abnormalities Retrograde ejaculation – Postsurgical – Beta blockers – Diabetic neuropathy Anti-sperm antibody production Infections of accessory glands

Male Factors in Infertility: Inadequate Sperm Delivery Coital Factors: – Erectile dysfunction – Ejaculatory incompetence – Hypospadias – Premature ejaculation – Use of spermicidal lubricants
Male Infertility: Clinical Evaluation Basic Procedures: – Physical examination – Semen analysis – Endocrine profile: T, LH, FSH, PRL
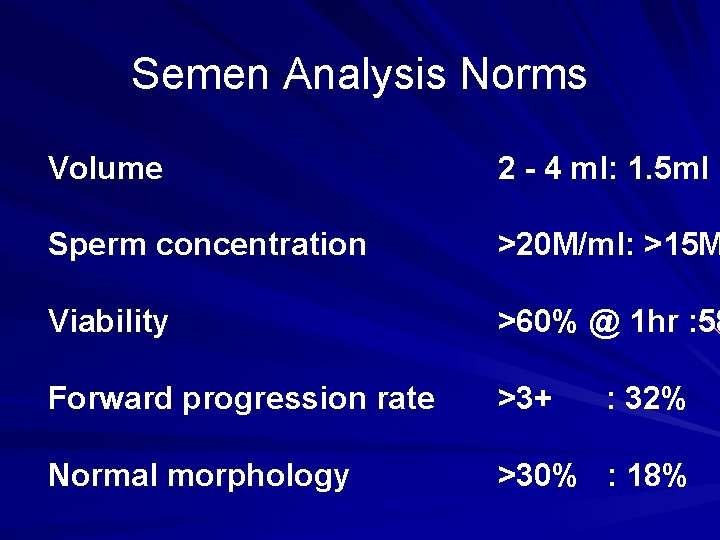
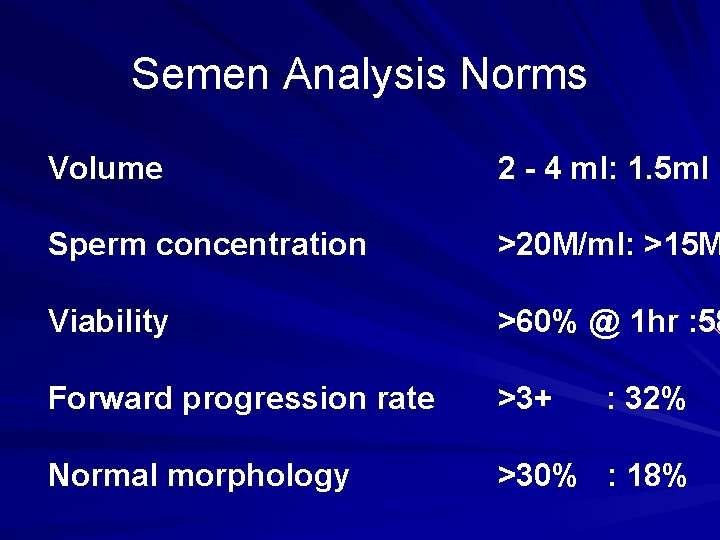
Semen Analysis Norms Volume 2 - 4 ml: 1. 5 ml Sperm concentration >20 M/ml: >15 M Viability >60% @ 1 hr : 58 Forward progression rate >3+ Normal morphology >30% : 18% : 32%

Male Infertility: Clinical Evaluation Adjunctive Procedures: – Postcoital test (obsolete) – Hamster ova penetration assay – Testicular biopsy – Antisperm antibody test

HUMSTER CELL HUMAN CHROMOSOMES NUCLEOLUS HAMSTER CHROMOSOMES
Female Factors in Infertility Endocrine factors; Ovulatory Cervical factors Tubal, peritoneal, and uterine factors
Female Factors in Infertility: Endocrine Factors Disorders of Ovulation: – Anovulation/Amenorrhea Causes: – Psychological dysfunction – Emotional stress – Genetic abnormalities – Nutritional deficiencies – CNS disease

Female Factors in Infertility: Endocrine Factors (cont. ) Disorders of Ovulation (cont. ): – Luteal phase dysfunction Causes: – Decreased Corpus Luteum progesterone production – Excessive body weight – Underweight conditions – Excessive exercise
Female Factors in Infertility: Endocrine Factors (cont. ) Clinical Evaluation: – Basal Body Temp (BBT) records: evidence of ovulation? – Endometrial biopsy: evidence of luteal defect, no longer required; obsolete – Endocrine profile: progesterone ( luteal phase) Day 21 progesterone test
Female Factors in Infertility: Cervical Factors Cervical mucus dysfunction Clinical Evaluation: – Postcoital test (not performed in primary evaluation): evidence of: quality of semen and cervical mucus adequacy of coital technique and anatomy evidence of sperm antibodies
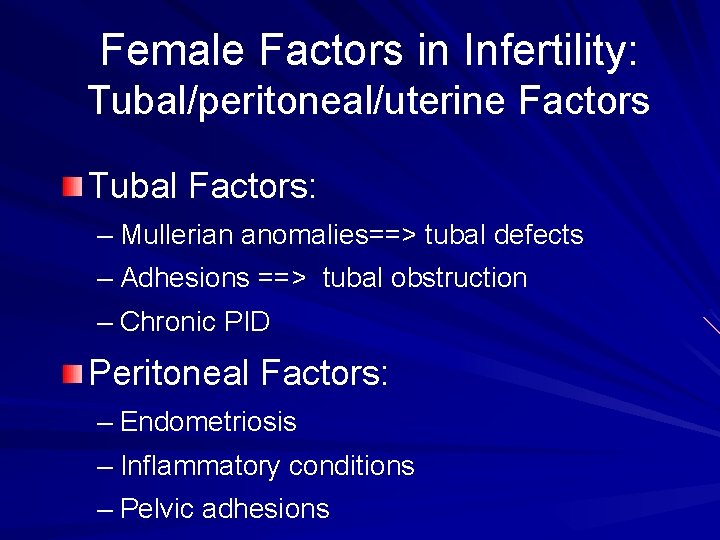
Female Factors in Infertility: Tubal/peritoneal/uterine Factors Tubal Factors: – Mullerian anomalies==> tubal defects – Adhesions ==> tubal obstruction – Chronic PID Peritoneal Factors: – Endometriosis – Inflammatory conditions – Pelvic adhesions
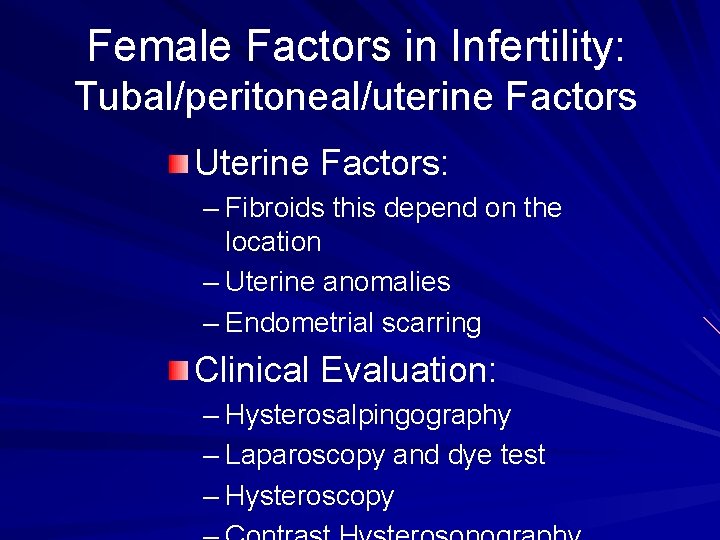
Female Factors in Infertility: Tubal/peritoneal/uterine Factors Uterine Factors: – Fibroids this depend on the location – Uterine anomalies – Endometrial scarring Clinical Evaluation: – Hysterosalpingography – Laparoscopy and dye test – Hysteroscopy
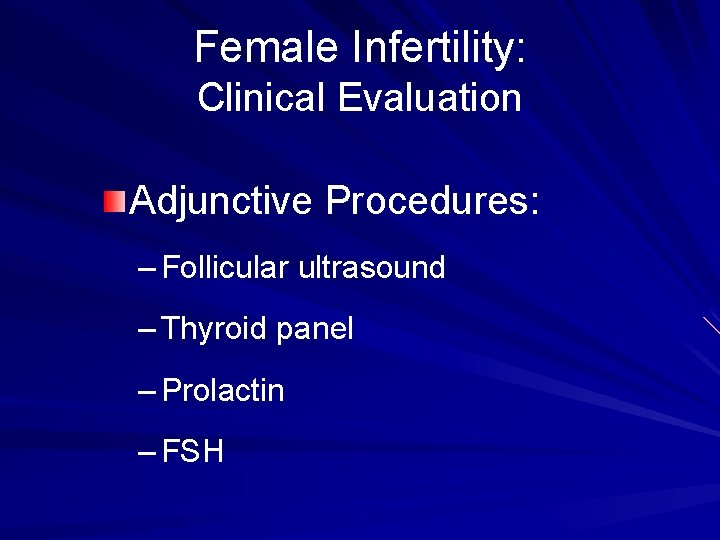
Female Infertility: Clinical Evaluation Adjunctive Procedures: – Follicular ultrasound – Thyroid panel – Prolactin – FSH
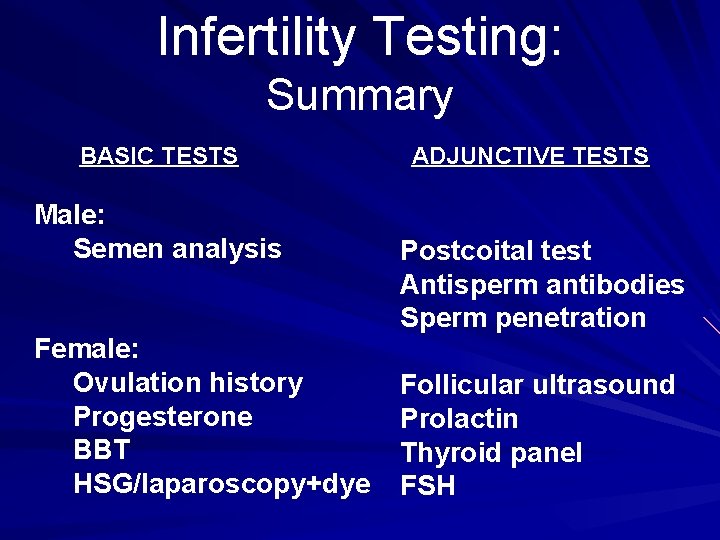
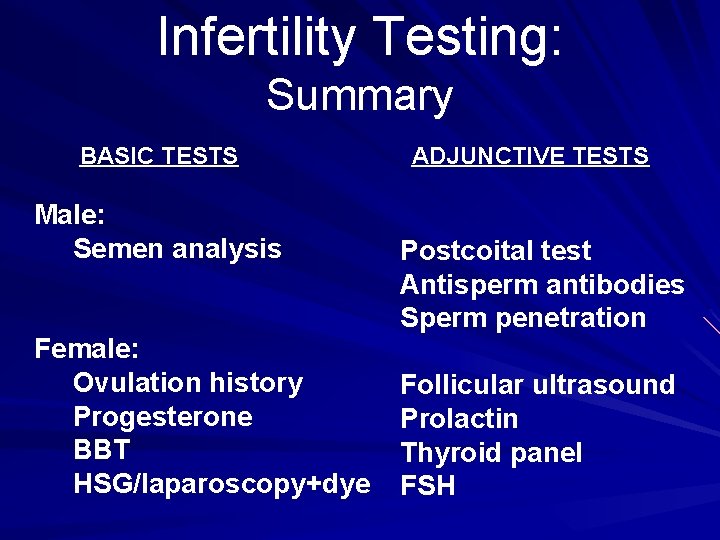
Infertility Testing: Summary BASIC TESTS Male: Semen analysis Female: Ovulation history Progesterone BBT HSG/laparoscopy+dye ADJUNCTIVE TESTS Postcoital test Antisperm antibodies Sperm penetration Follicular ultrasound Prolactin Thyroid panel FSH
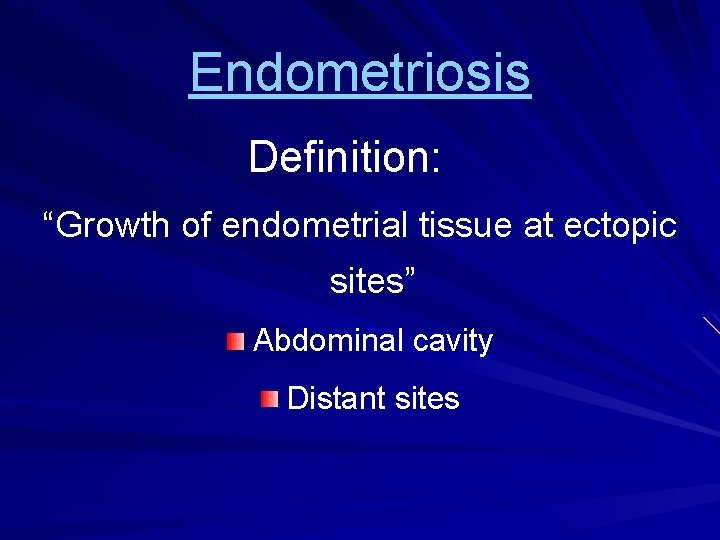
Endometriosis Definition: “Growth of endometrial tissue at ectopic sites” Abdominal cavity Distant sites
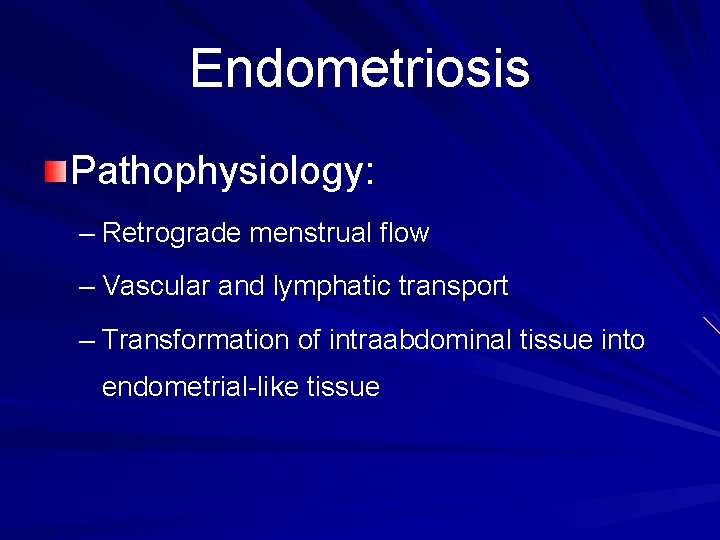
Endometriosis Pathophysiology: – Retrograde menstrual flow – Vascular and lymphatic transport – Transformation of intraabdominal tissue into endometrial-like tissue
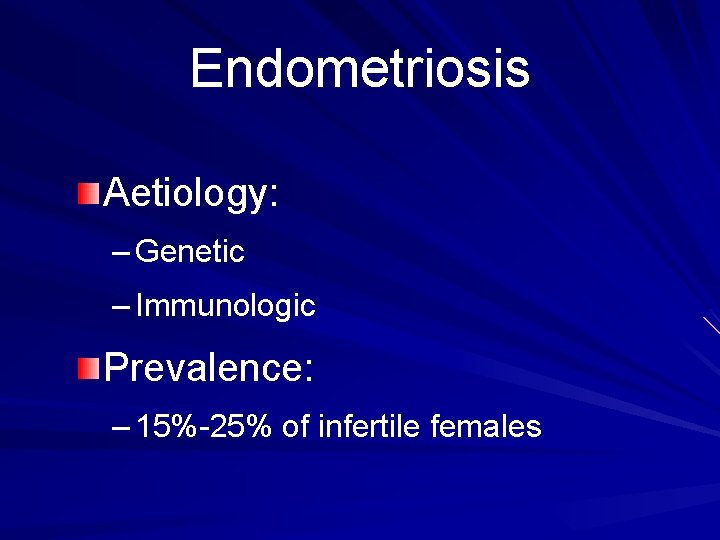
Endometriosis Aetiology: – Genetic – Immunologic Prevalence: – 15%-25% of infertile females
Endometriosis Myths: – Only affects women over 30 – Only affects White women – It does not occur before menarche – It is confined to nulliparous women
Endometriosis Clinical Manifestations: – Dysmenorrhea – Diffuse pain (bladder, rectum areas) – Low back pain – Premenstrual spotting – Dyspareunia (pain with intercourse)
Endometriosis and Infertility With ovarian involvement --> adhesions Without ovarian involvement: – Large implants result in: – Increased prostaglandins: Decreased tubal motility, or Impaired follicular maturation, or Impaired corpus luteum function
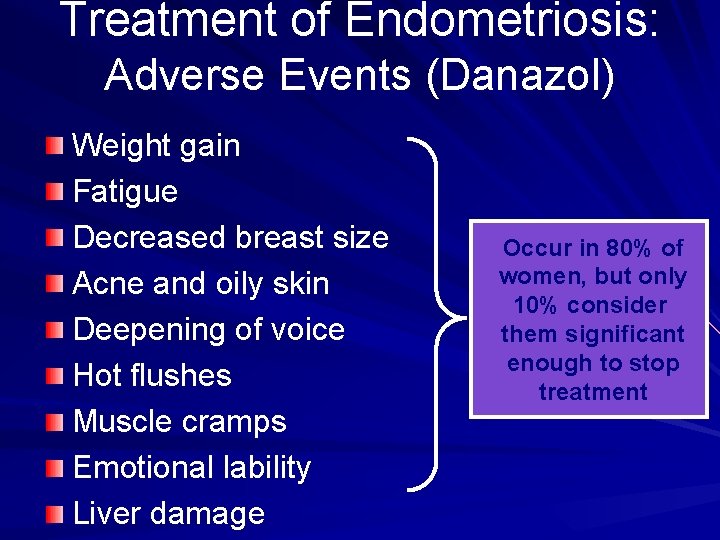
Treatment of Endometriosis: Hormonal Approach Principle: estrogen stimulates growth Approach: anti-estrogenic agents Until late 70 s: oral contraceptives Modern approach: Danazol Results (Danazol): – Hypoestrenism --> stops growth of implants – Amenorrhea --> stops new bleeding
Treatment of Endometriosis: Adverse Events (Danazol) Weight gain Fatigue Decreased breast size Acne and oily skin Deepening of voice Hot flushes Muscle cramps Emotional lability Liver damage Occur in 80% of women, but only 10% consider them significant enough to stop treatment

Treatment of Endometriosis: Surgical Approach Recommendation: > 1 cm Goal: restore anatomy and destroy growths Dangers: adhesions!! Success: related to extent of disease Approaches: – Conservative – Radical
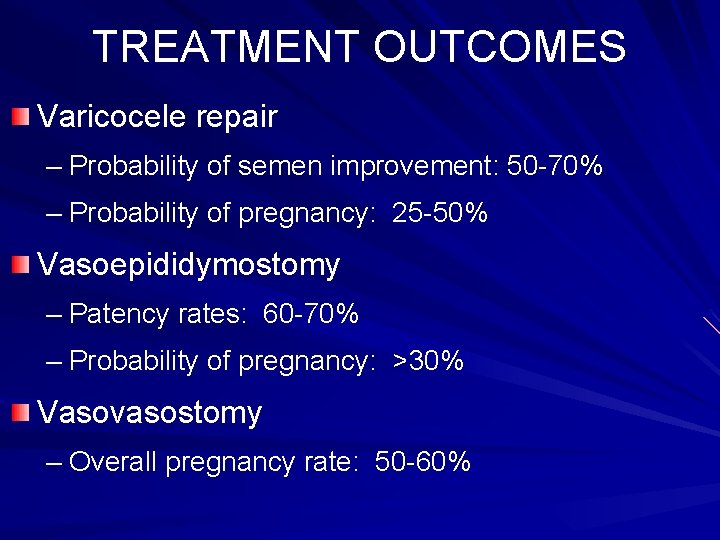
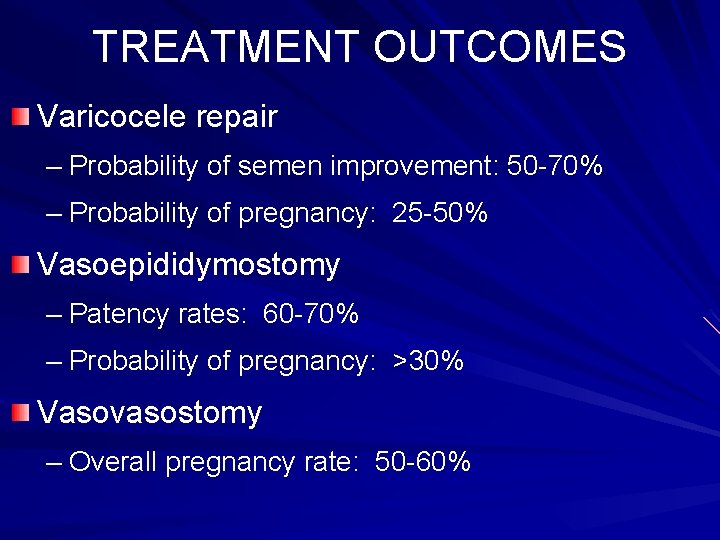
TREATMENT OUTCOMES Varicocele repair – Probability of semen improvement: 50 -70% – Probability of pregnancy: 25 -50% Vasoepididymostomy – Patency rates: 60 -70% – Probability of pregnancy: >30% Vasovasostomy – Overall pregnancy rate: 50 -60%

TREATMENT OUTCOMES Ejaculatory disorders – Sympathomimetic drugs: 20 -30% Retrograde ejaculation – Sperm rescue from urine: variable success rate Antisperm antibody – Immunosuppressive drugs: variable success
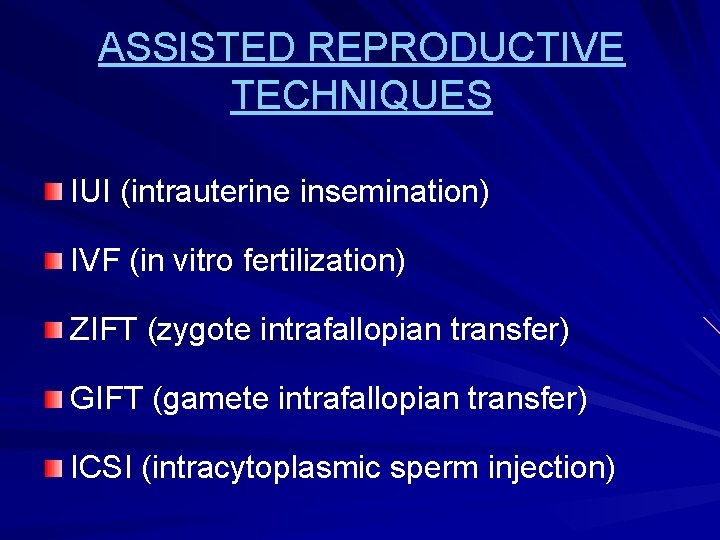
ASSISTED REPRODUCTIVE TECHNIQUES IUI (intrauterine insemination) IVF (in vitro fertilization) ZIFT (zygote intrafallopian transfer) GIFT (gamete intrafallopian transfer) ICSI (intracytoplasmic sperm injection)
 Coital incontinence
Coital incontinence Unprotected left main
Unprotected left main Risk of blood transfusion
Risk of blood transfusion Infertility definition
Infertility definition Hijama points for male infertility
Hijama points for male infertility Hijama points for female infertility
Hijama points for female infertility Female infertility
Female infertility Infertility center of st. louis
Infertility center of st. louis Cystic fibrosis male infertility
Cystic fibrosis male infertility Exposition in the outsiders
Exposition in the outsiders Talle tonge mathews phosa
Talle tonge mathews phosa Mathews v eldridge
Mathews v eldridge Two bit mathews thoughts about inner self
Two bit mathews thoughts about inner self Mathews practice
Mathews practice The mathews practice
The mathews practice Roy mathews bainbridge
Roy mathews bainbridge Talle tonge mathews phosa
Talle tonge mathews phosa Two bit mathews description
Two bit mathews description Mathews practice
Mathews practice Tj mathews
Tj mathews Tiffany mathews
Tiffany mathews Erin ledbetter
Erin ledbetter Elizabeth mathews
Elizabeth mathews Expository essay def
Expository essay def Operational definition psychology examples
Operational definition psychology examples Soziale wirklichkeit definition
Soziale wirklichkeit definition Energieumsatz
Energieumsatz Zakat meaning
Zakat meaning Career portfolio table of contents
Career portfolio table of contents Bildungsroman meaning
Bildungsroman meaning Tanzimat reforms definition
Tanzimat reforms definition Coconut shy definition
Coconut shy definition What is the definition of internal conflict
What is the definition of internal conflict New lights vs old lights apush
New lights vs old lights apush Marbury vs madison apush definition
Marbury vs madison apush definition Mini saga stories
Mini saga stories Narrative writing definition
Narrative writing definition How to write a good leq for ap world history
How to write a good leq for ap world history Expository paragraph meaning
Expository paragraph meaning Definition of concrete detail
Definition of concrete detail Writing an objective summary
Writing an objective summary