InferiorRight Ventricular Infarction CLINICAL PRESENTATION AND TREATMENT Prepared

- Slides: 24
Inferior/Right Ventricular Infarction CLINICAL PRESENTATION AND TREATMENT Prepared by Shane Barclay MD
Rt. Ventricular MI Isolated Right Ventricular Myocardial Infarction (RVMI) is rare. More commonly occurs with inferior wall MI, occurring in 30 -50 % of such cases. Approximately 50% patients with RVMI have profound hemodynamic and electrical complications. However long term outcomes are usually very good.
Clinical Presentation RVMI: suspect in Inferior MI when patient presents also with: 1. Hypotension 2. Bradycardia 3. JVD 4. Clear chest sounds (no edema)
Right versus Left Ventricle Oxygen demand is significantly lower in the Rt Ventricle because of smaller mass and lower afterload Coronary perfusion in the Rt occurs in both systole and diastole There is more extensive collateral circulation from left to right coronary arteries. SA and AV node are supplied by arteries that also supply the Right Ventricle.
Hemodynamic consequences of RVMI Right ventricular failure may cause limited filling pressures in the Rt Ventricle from decreased cardiac output, bi-ventricular failure or both. Increasing Right Ventricular filling pressures (via fluid infusion) may cause shifting of the septum into the left ventricle which then impairs left ventricular filling and function.
Hemodynamic consequences of RVMI Rt. Ventricular output may further be compromised by: 1. Hypoxemia from pulmonary edema 2. Alpha-adrenergic agonists 3. Mechanical ventilation with PEEP
Electrical Consequences – Inferior/RVMI Bradycardia: can arise from SA and AV node dysfunction Tachycardia and Ventricular Fibrillation occur in up to 30% of patients
Treatment Usual STEMI protocol, ie ASA, IVs, monitor TNK Cautious use of Nitrates, beta blockers, diuretics, opioids and bladder catheterization as these may impact preload, heart rate and contractility.
Treatment If evidence of significant RV dysfunction or cardiogenic shock 1. IV fluid boluses, but try to limit to maximum 1 liter N/S If still hypotensive/cardiogenic shock after one liter N/S 2. Pressors – Norepinephrine, Dobutamine
Treatment – Pressors Norepinephrine Start 0. 1 mcg/kg/min IV Dobutamine Start 2 mcg/kg/min -titrate
Treatment – Analgesics Fentanyl – Usually has minimal or no effect on BP and cardiac output. May have some negative chronotropic effect (decrease HR) which if necessary can be treated with atropine. Dose: 20 -25 mcg IV aliquots
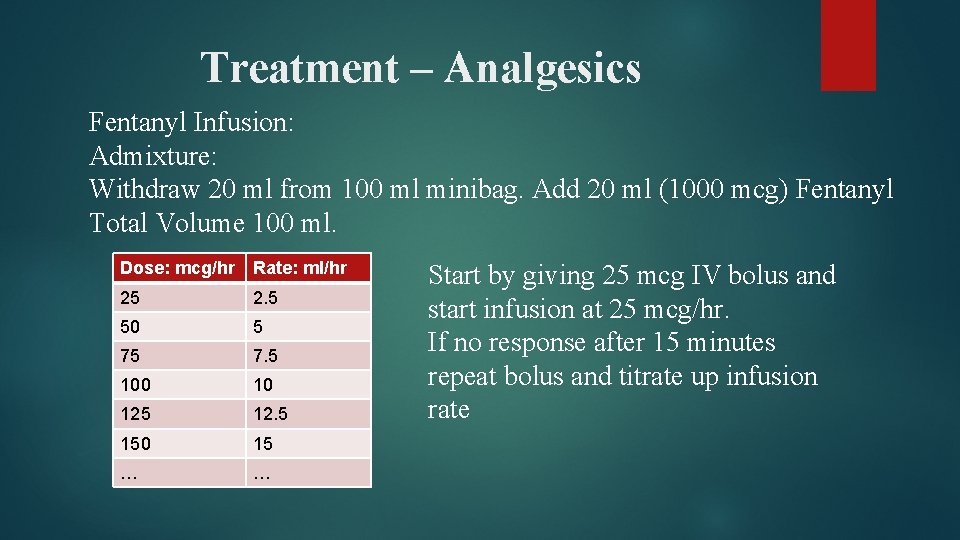
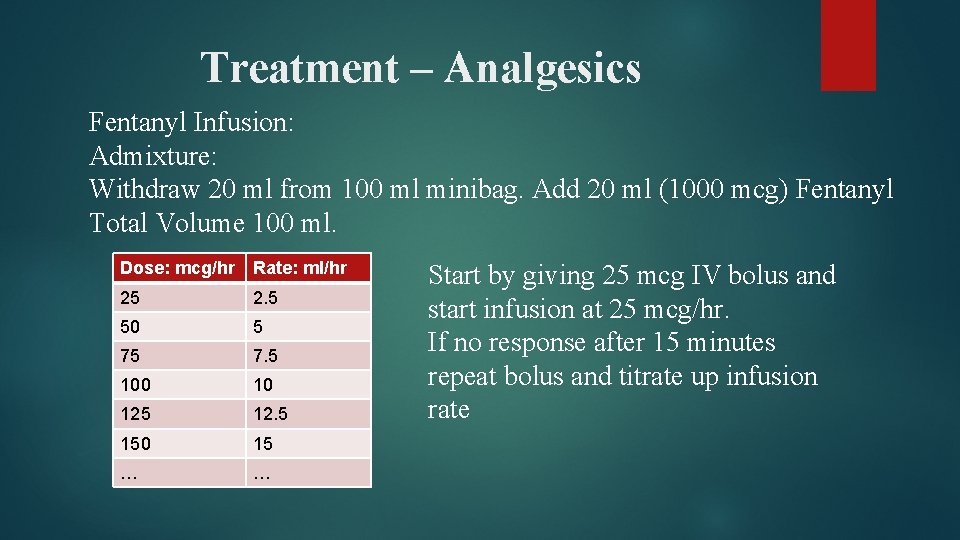
Treatment – Analgesics Fentanyl Infusion: Admixture: Withdraw 20 ml from 100 ml minibag. Add 20 ml (1000 mcg) Fentanyl Total Volume 100 ml. Dose: mcg/hr Rate: ml/hr 25 2. 5 50 5 75 7. 5 100 10 125 12. 5 150 15 … … Start by giving 25 mcg IV bolus and start infusion at 25 mcg/hr. If no response after 15 minutes repeat bolus and titrate up infusion rate
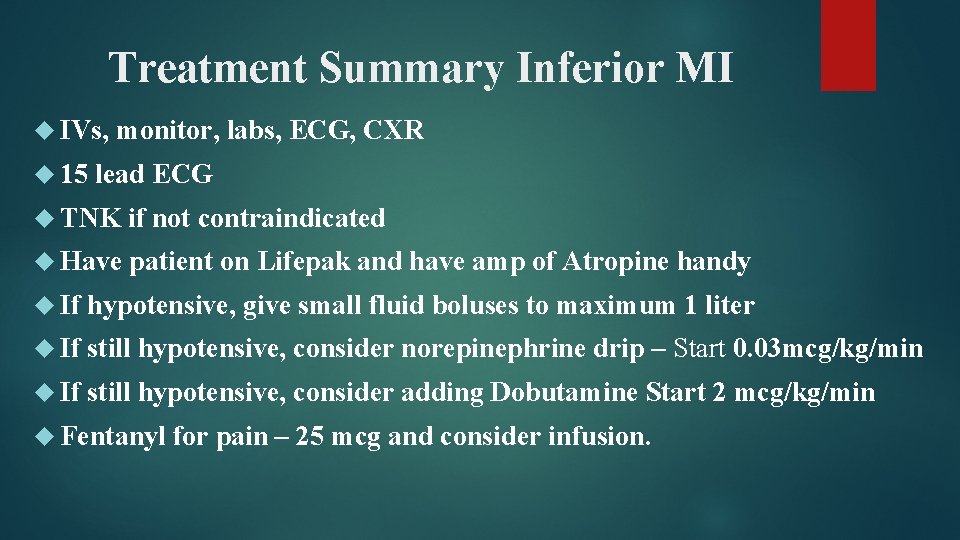
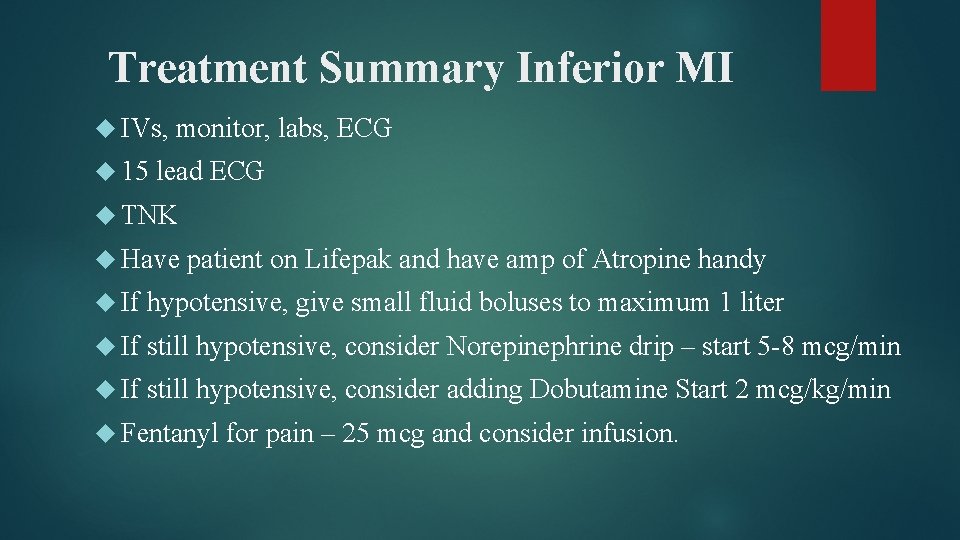
Treatment Summary Inferior MI IVs, 15 monitor, labs, ECG, CXR lead ECG TNK if not contraindicated Have patient on Lifepak and have amp of Atropine handy If hypotensive, give small fluid boluses to maximum 1 liter If still hypotensive, consider norepinephrine drip – Start 0. 03 mcg/kg/min If still hypotensive, consider adding Dobutamine Start 2 mcg/kg/min Fentanyl for pain – 25 mcg and consider infusion.
Clinical Scenario
Clinical Scenario 54 year old male, previously completely healthy, presents with a history of waking with epigastric pain and burping. This increased in severity and is now “ 10/10” pain.

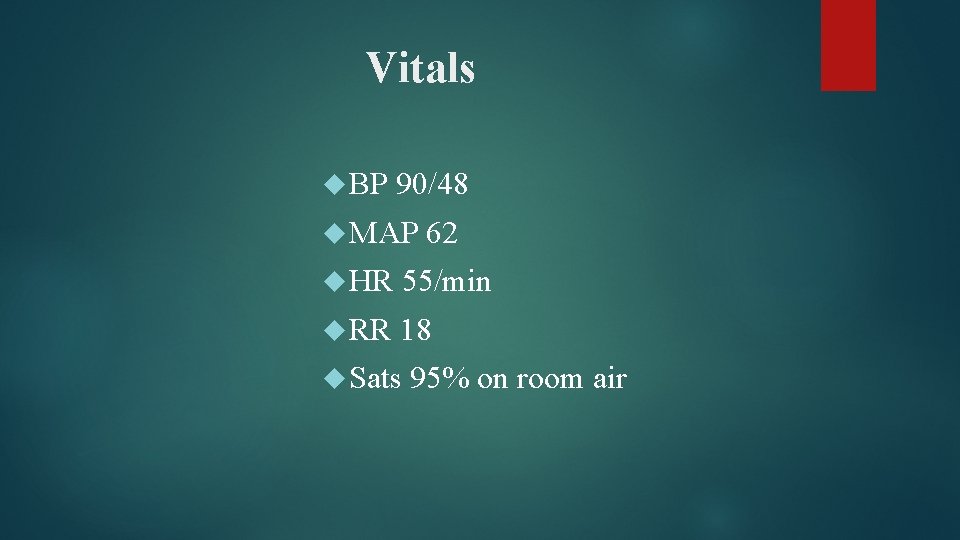
Vitals BP 90/48 MAP 62 HR 55/min RR 18 Sats 95% on room air
Exam Appears in acute distress, moaning and clutching his chest (i. e. real ‘man pain’. Can answer questions and seems oriented Heart sounds are normal Chest is clear JVD just under the ear lobe.
What are you going to do?
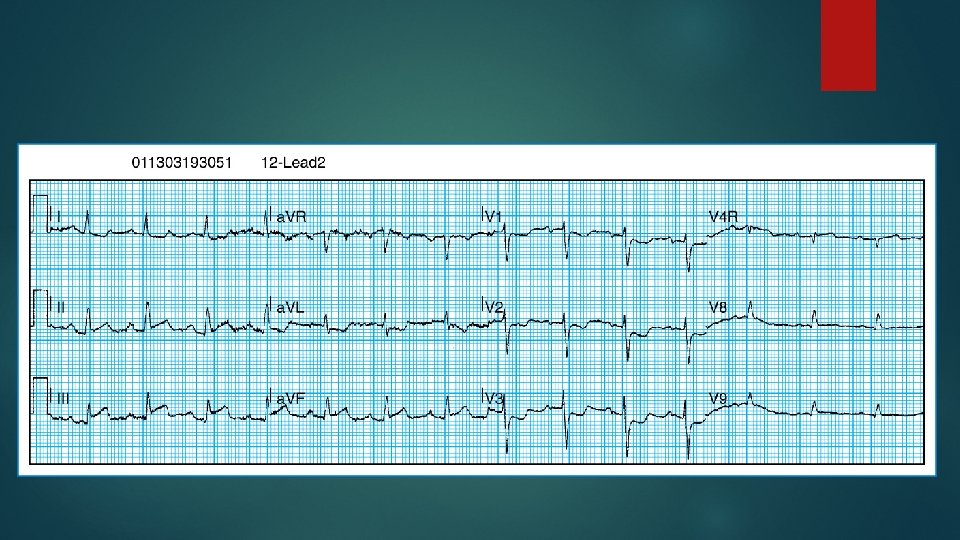
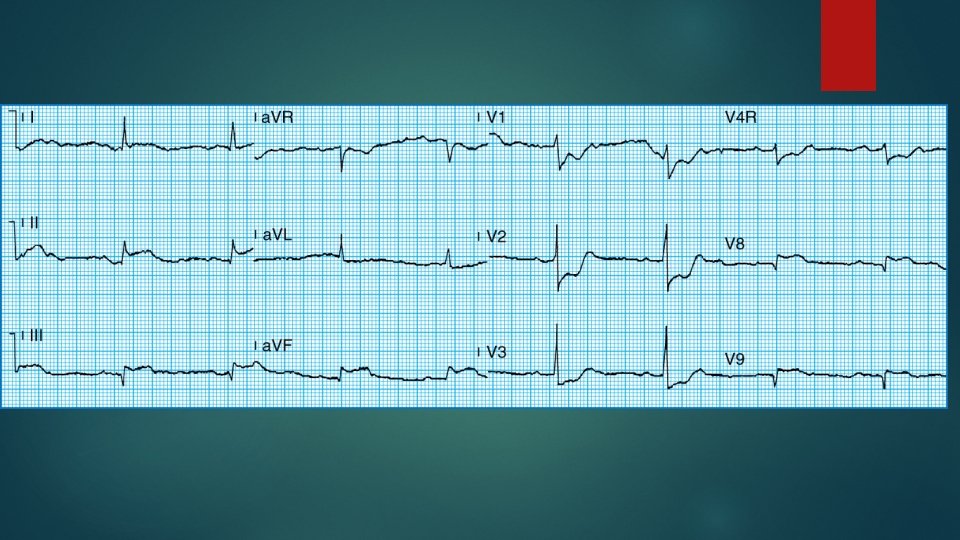
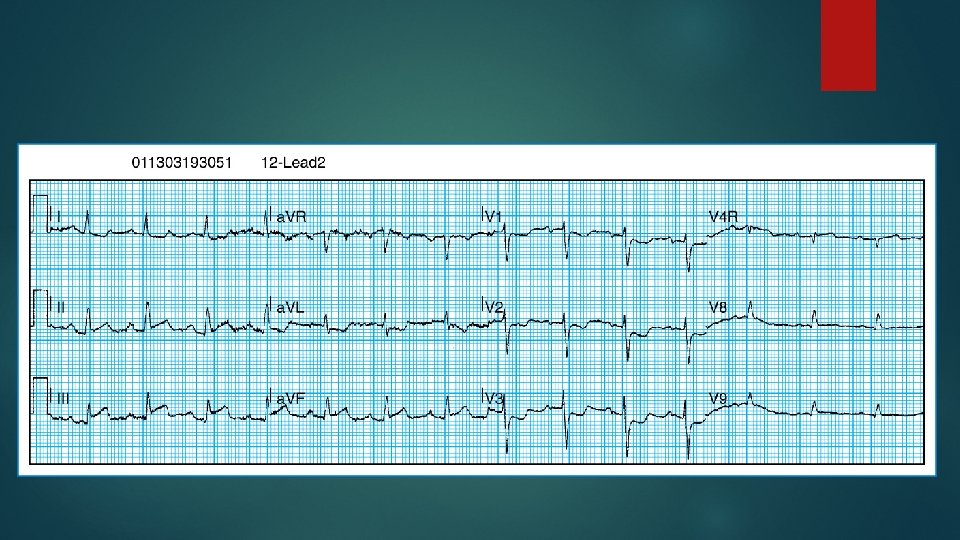
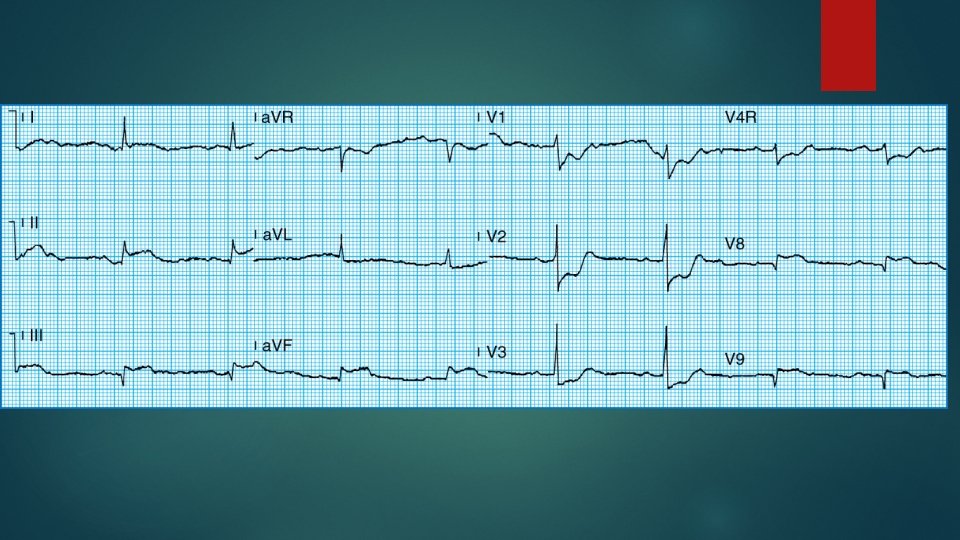
ECG X-ray tech is coming, will be about 5 minutes.
Labs Lab tech is taking labs, will be about 5 -10 minutes.
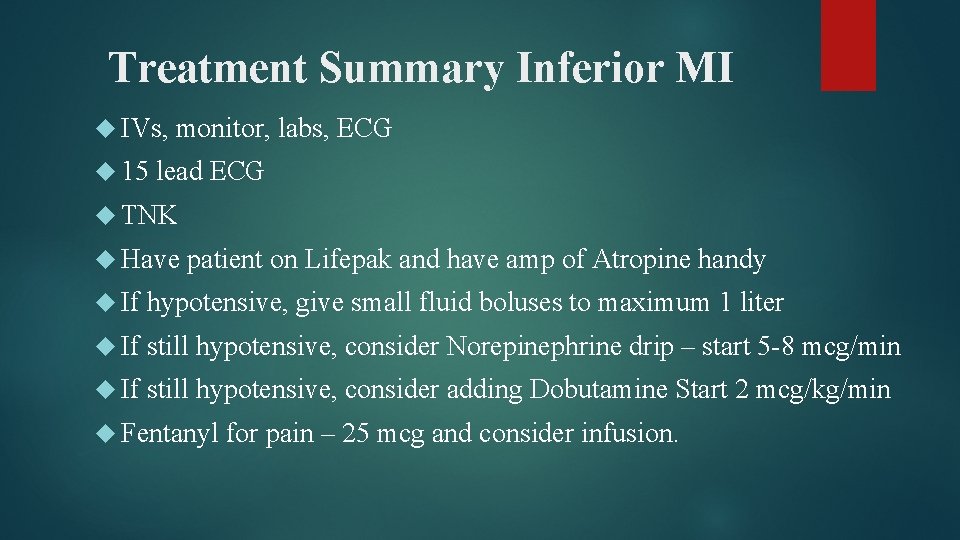
Treatment Summary Inferior MI IVs, 15 monitor, labs, ECG lead ECG TNK Have patient on Lifepak and have amp of Atropine handy If hypotensive, give small fluid boluses to maximum 1 liter If still hypotensive, consider Norepinephrine drip – start 5 -8 mcg/min If still hypotensive, consider adding Dobutamine Start 2 mcg/kg/min Fentanyl for pain – 25 mcg and consider infusion.