INFECTIVE ENDOCARDITIS 1 INFECTIVE ENDOCARDITIS Colonisation invasion of





- Slides: 64
INFECTIVE ENDOCARDITIS 1
INFECTIVE ENDOCARDITIS Colonisation / invasion of HEART VALVES & ENDOCARDIUM by a microbe Bulky friable vegetations Destruction of cardiac tissues 2
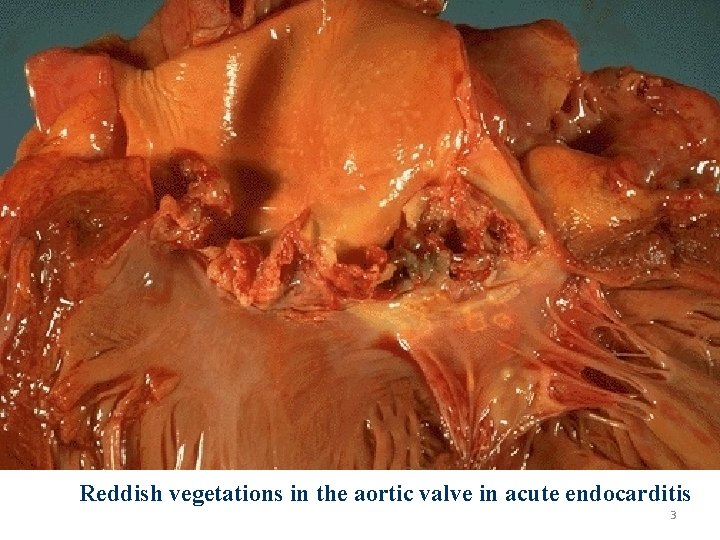
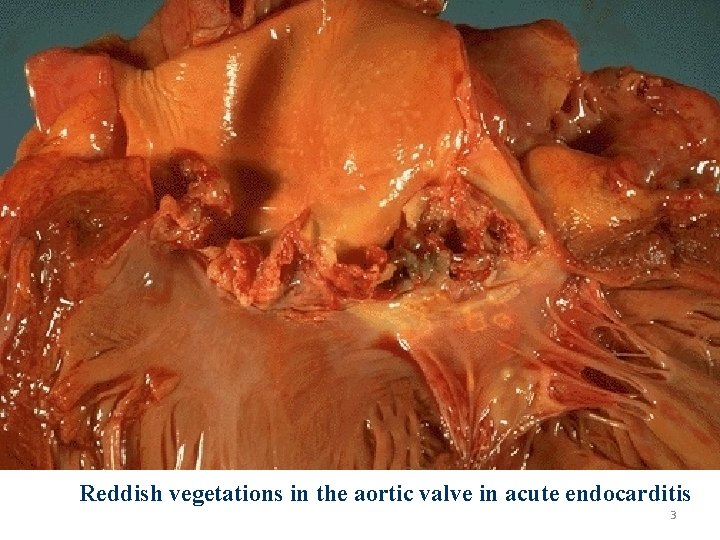
Reddish vegetations in the aortic valve in acute endocarditis 3
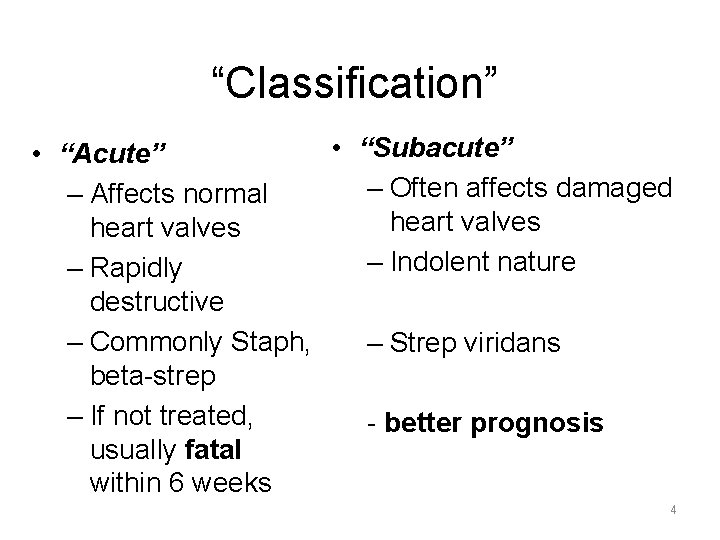
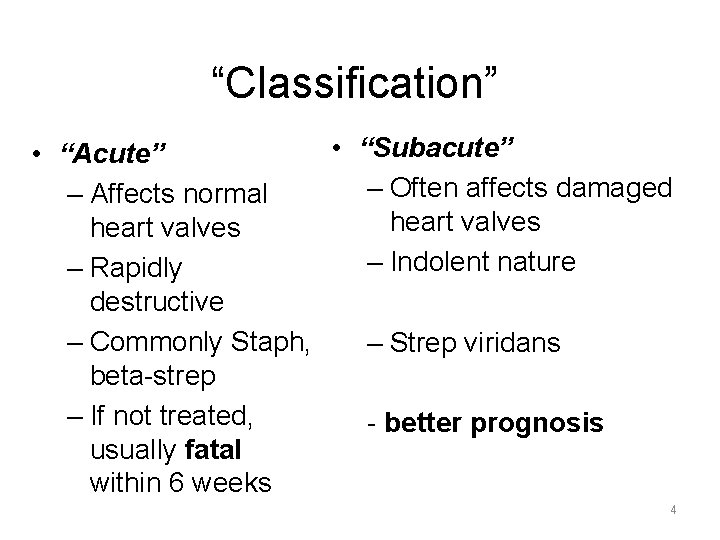
“Classification” • “Subacute” • “Acute” – Often affects damaged – Affects normal heart valves – Indolent nature – Rapidly destructive – Commonly Staph, – Strep viridans beta-strep – If not treated, - better prognosis usually fatal within 6 weeks 4
Etiology & Pathogenesis Organisms Events leading to seeding of blood Abnormal Host Heart factors 5
Organisms • S. Viridans – Most common causative organism • Gram negative bacilli – Neonates & immunocompromised – Prosthetic valves • HACEK organisms – Hemophilus, Actinobacillus, Cardiobacterium, Eikenella, Kingella – Frequently affect damaged valves and can cause emboli 6
Events Seeding of Blood Obvious infection elsewhere Dental / surgical proceedure Injection of contaminated material by Drug abusers Occult sources in gut / oral cavity bacteriemia 7
Abnormal Heart RHD (Rheumatic Heart Disease) Myxomatous degeneration of Mitral valve Degenerative calcific valvular stenosis Bicuspid aortic valves Prosthetic valves 8
Host Factors Neutropenia Immunodeficiency Malignancy Diabetis Mellitus Alcohol & drug abuse 9
Pathogenesis • Thrombi • Hemodynamic • Microbe adherence 10
Pathogenesis 1. Turbulent blood flow disrupts the endocardium making it “sticky” 2. Bacteremia delivers the organisms to the endocardial surface 3. Adherence of the organisms to the endocardial surface 4. Eventual invasion of the valvular leaflets 11
Prosthetic Heart Valve • a serious complication • positive blood culture in patients with underlying prosthetic valves can be a harbinger of endocarditis 12 12
IV Drug Use • • Recurrent Polymicrobial Staph aureus tricuspid valve 13 13
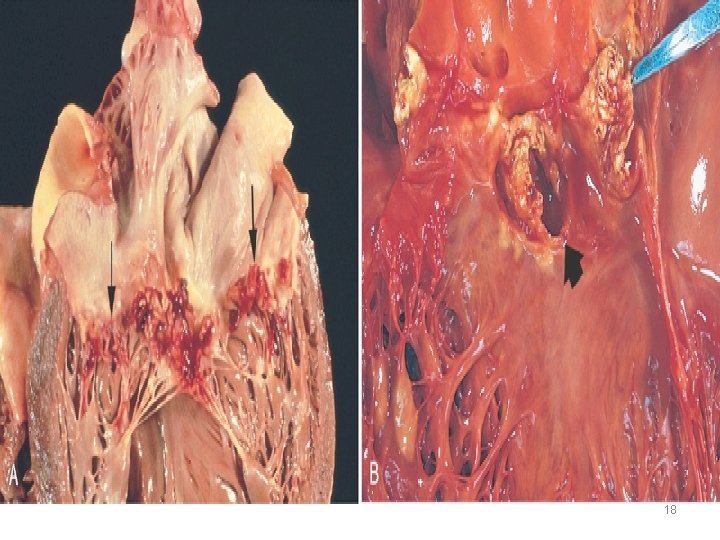
Pathology • Local destruction of intracardiac infection: valve, chordae tendineae, fistula, paravalvular abscess, conduction • Distant embolization with infarct or infection: 45— 65% (autopsy), 70% pulmonary embolism 14
Pathology • Hematogenous seeding with bacteremia: metastatic infection, • Immune-complex or antibody reaction: Ig. M, Ig. A, Ig. G, Rheumatoid factor, Osler’s node, Roth’s spot 15
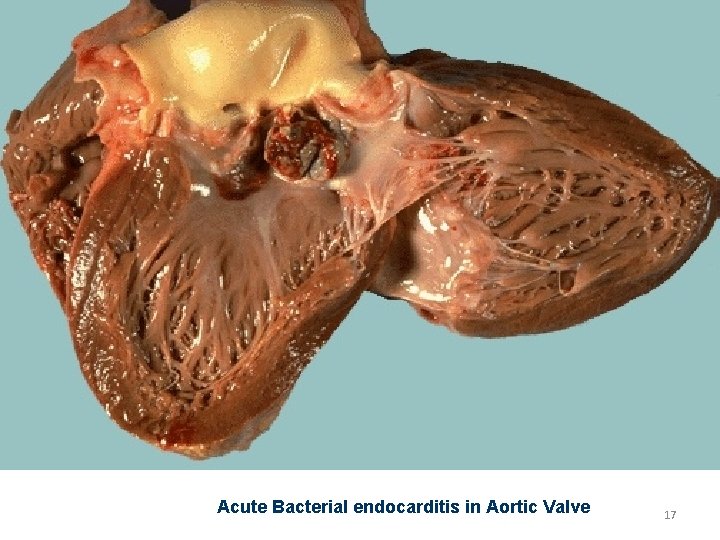
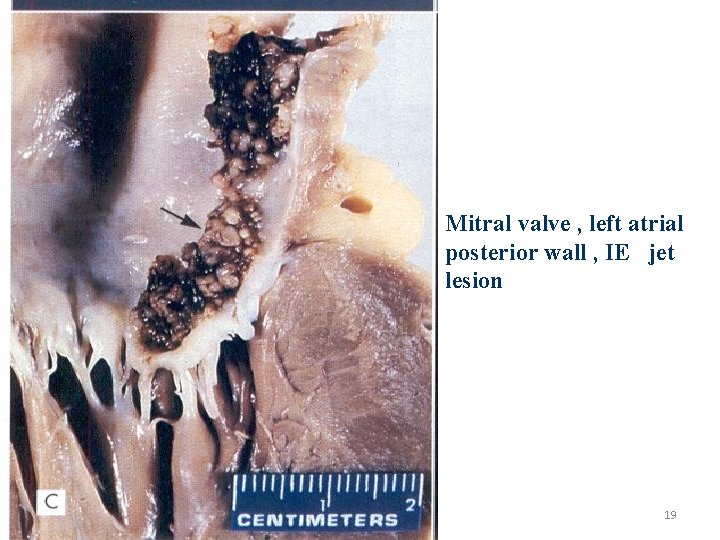
Morphology Friable bulky vegetations on Heart valves containing fibrin , inflammatory cells, bacteria Aortic & Mitral valves most affected Right side valves – drug abusers Ring abscess Septic infarcts in brain , kidneys , myocardium , other tissues 16
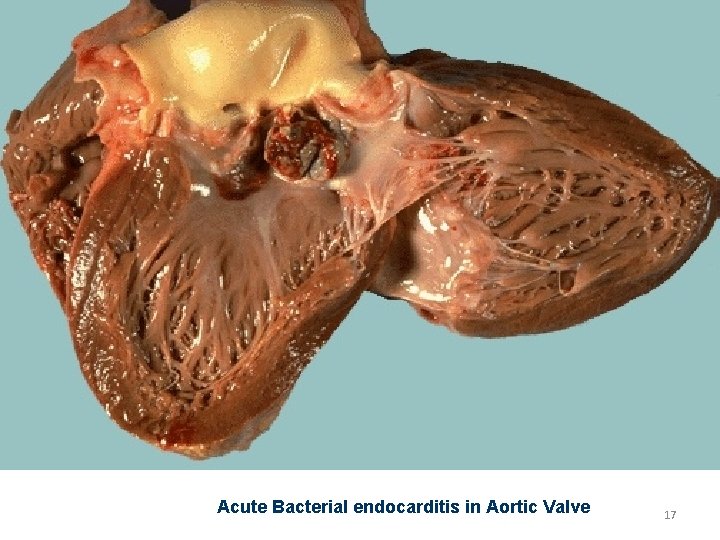
Acute Bacterial endocarditis in Aortic Valve 17
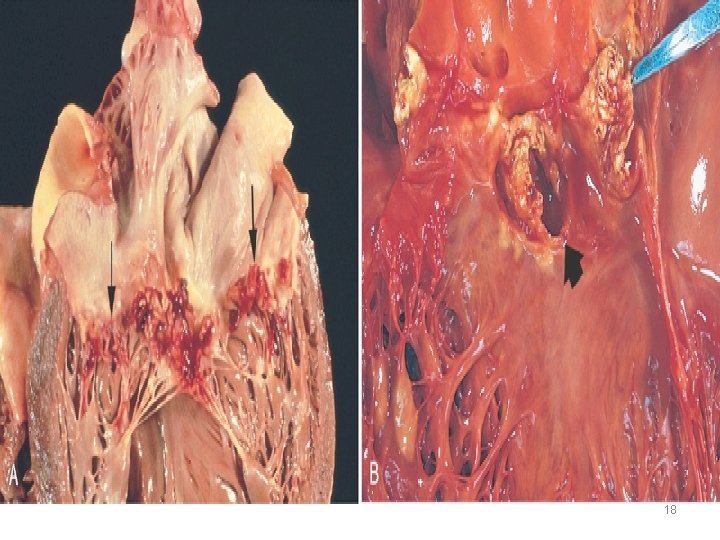
18
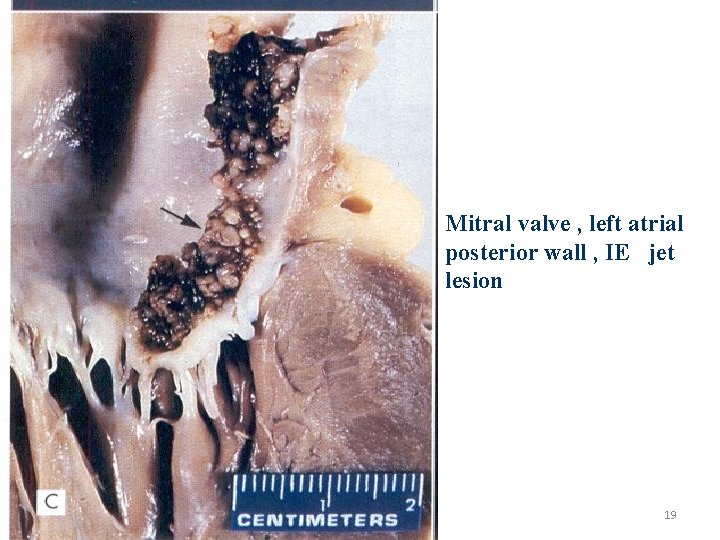
Mitral valve , left atrial posterior wall , IE jet lesion 19
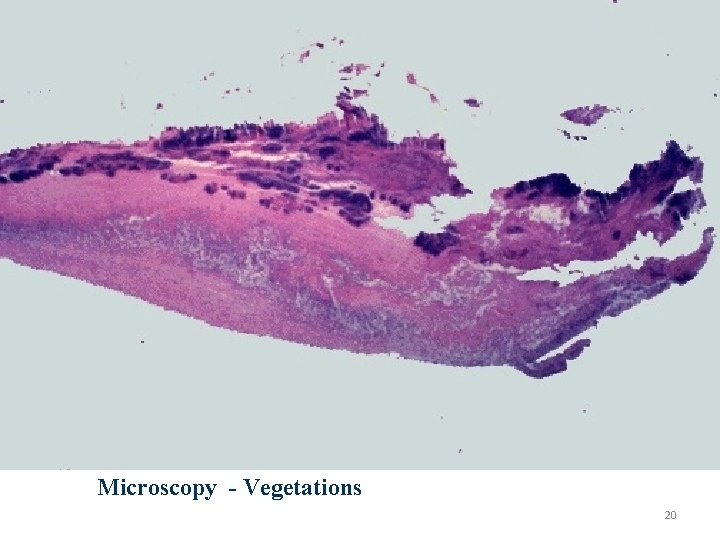
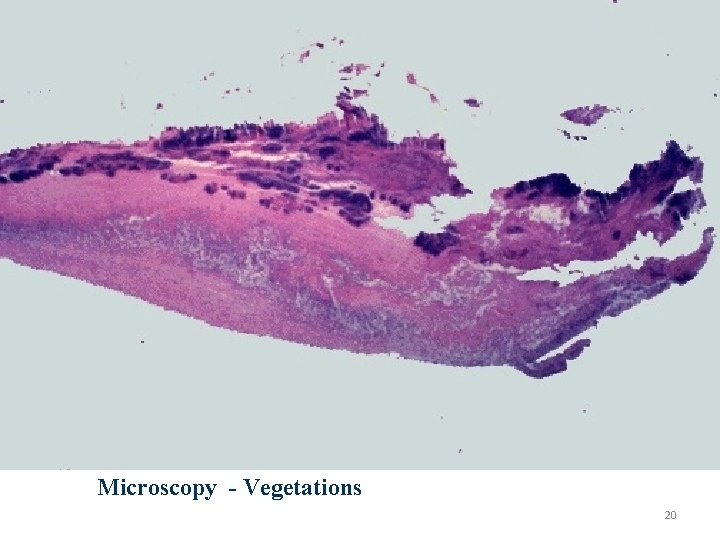
Microscopy - Vegetations 20
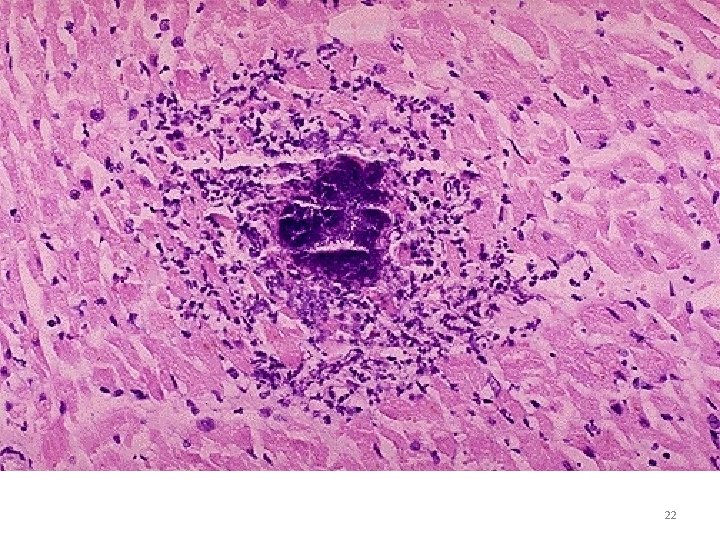
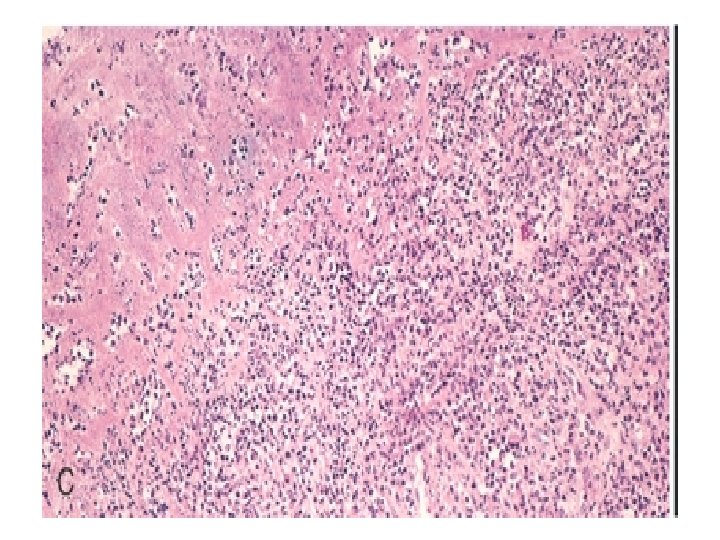
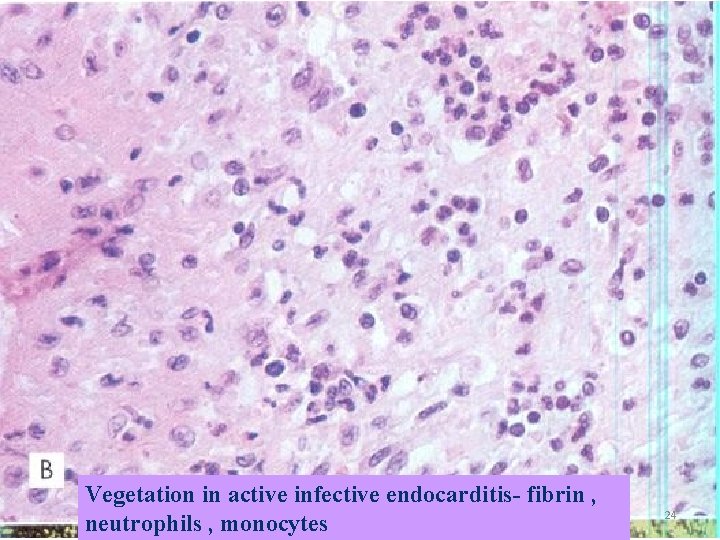
• Layer of fibrin & platelets • Bacterial colonies • Inflammatory reaction on the cusp 21
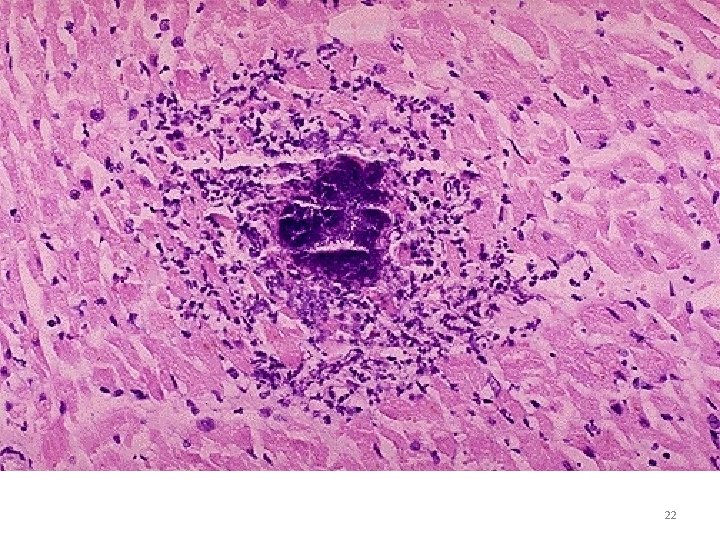
22
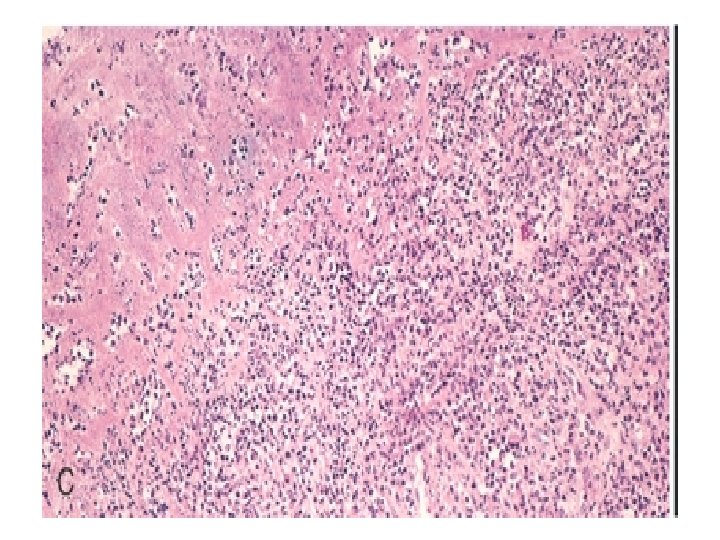
23
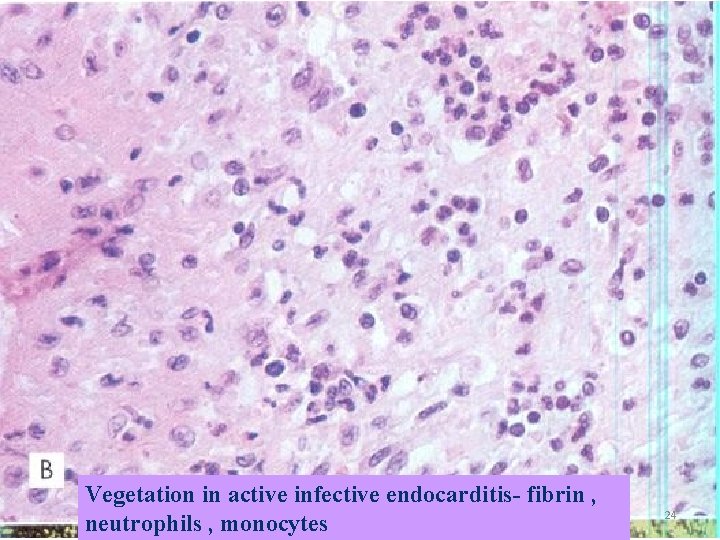
Vegetation in active infective endocarditis- fibrin , neutrophils , monocytes 24
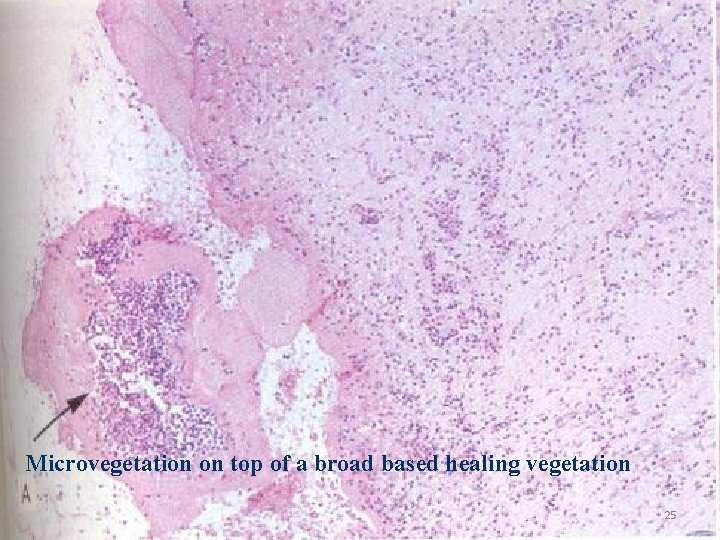
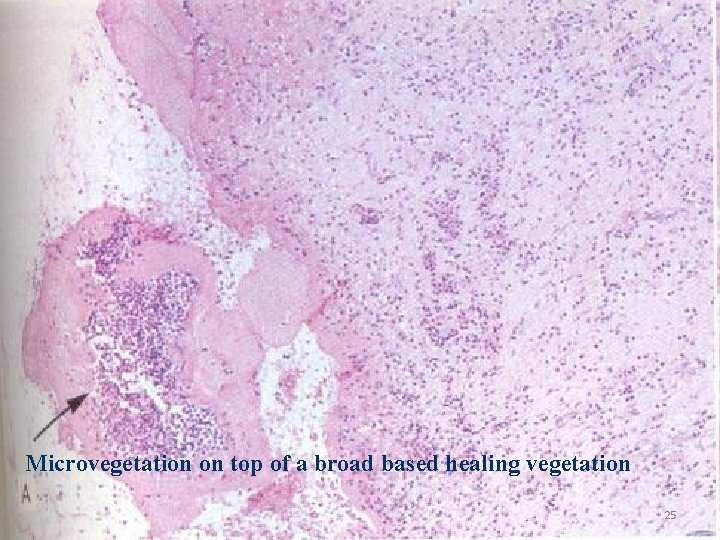
Microvegetation on top of a broad based healing vegetation 25

26
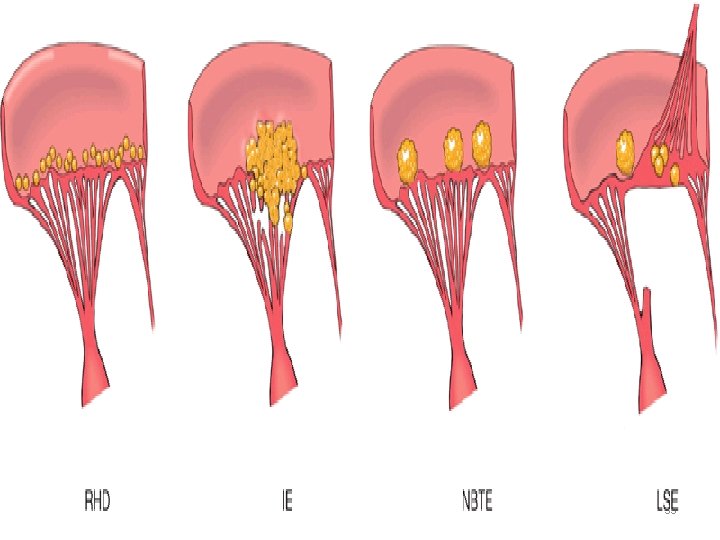
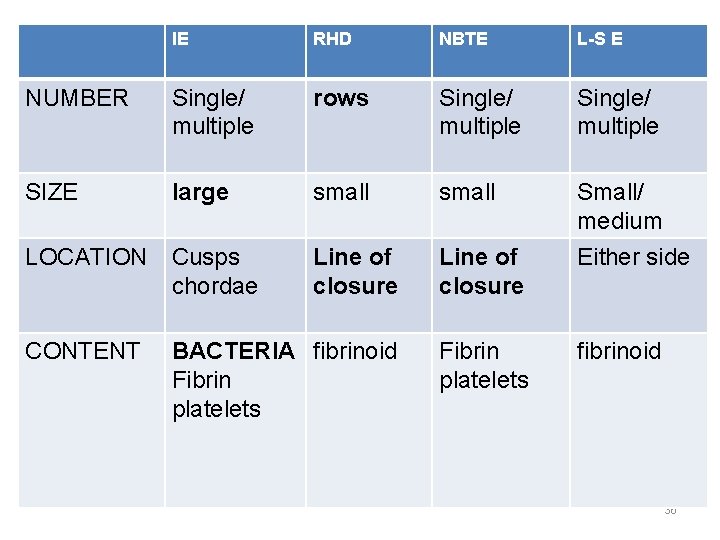
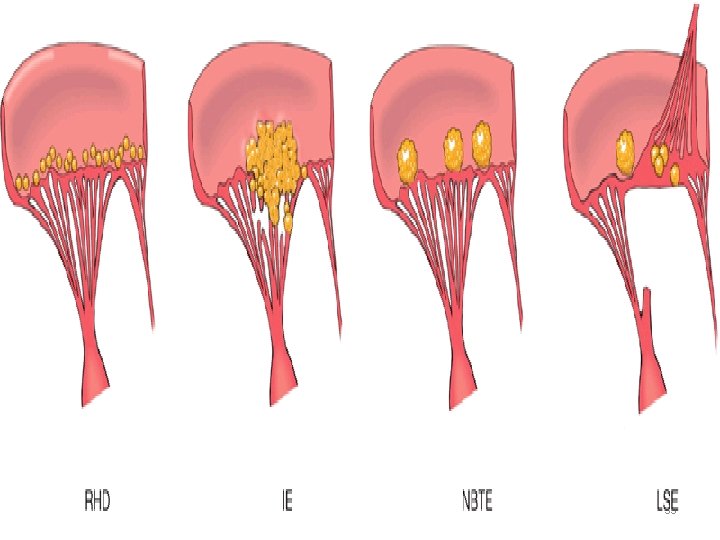
CARDIAC VEGETATIONS • • Rheumatic heart disease IE NBTE Libman-Sacks endocarditis (SLE) 27
Nonbacterial thrombotic endocarditis (NBTE) Marantic • • • Malignancy, DIC, uremia, burns, valvular heart disease, intracardiac catheter 28
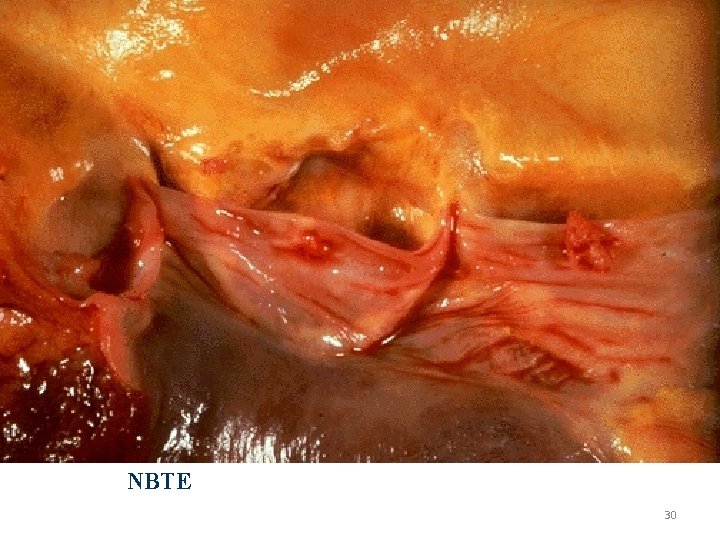
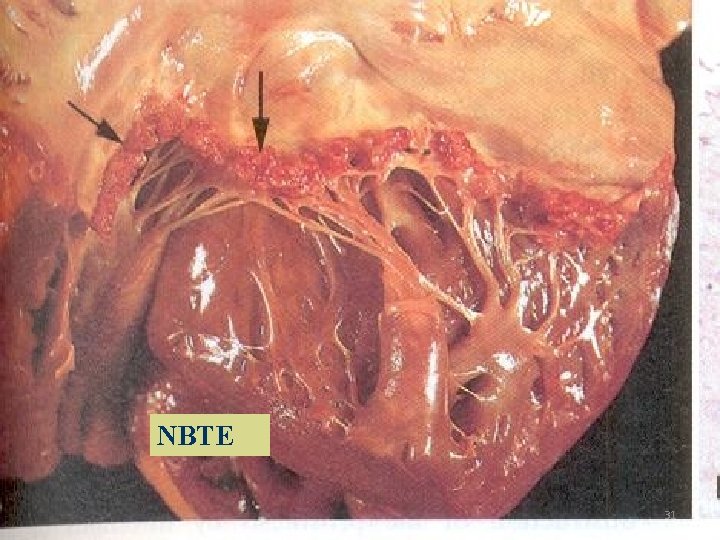
NBTE • Small masses of fibrin & platelets • No organisms 29
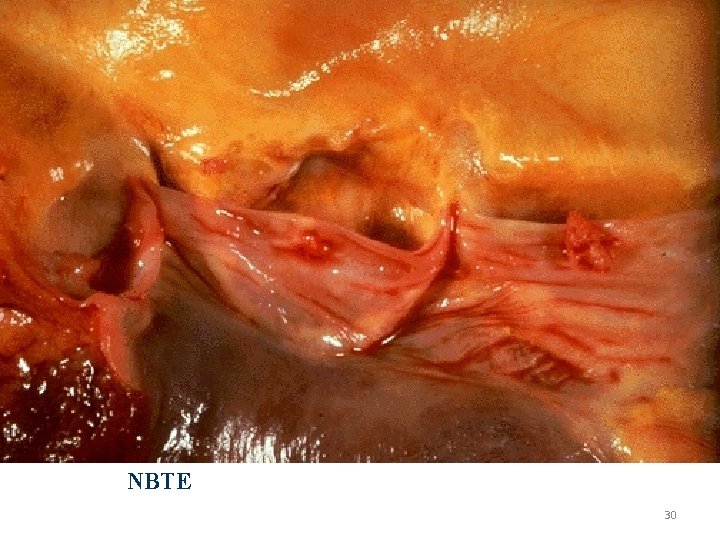
NBTE 30
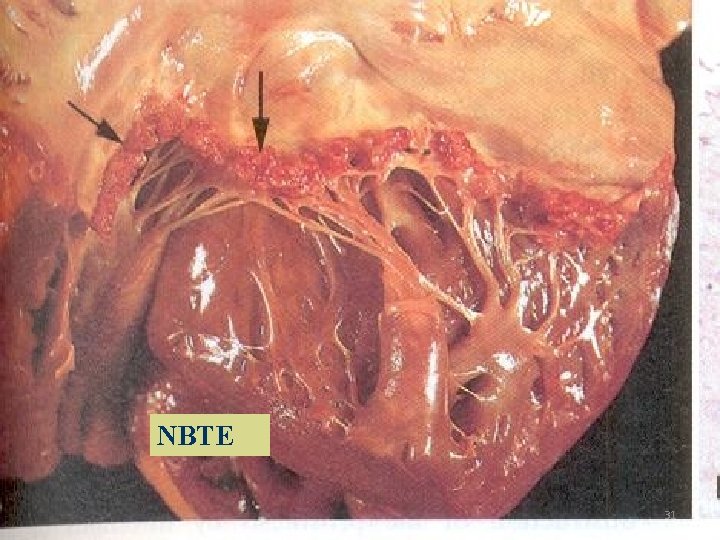
NBTE 31
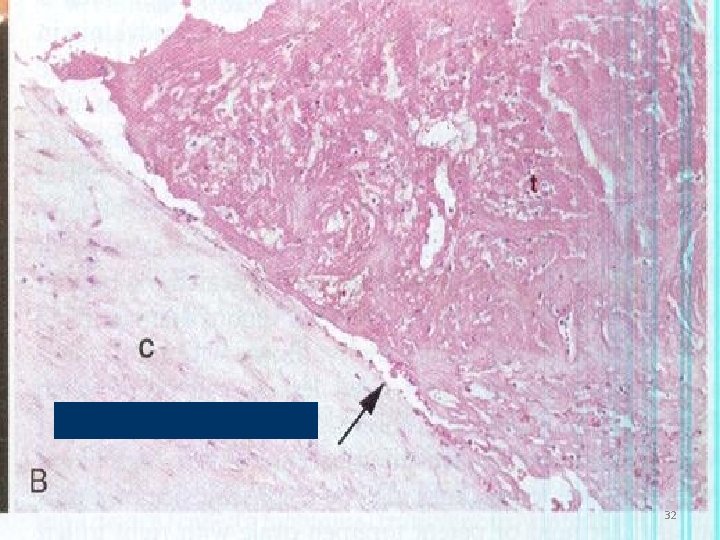
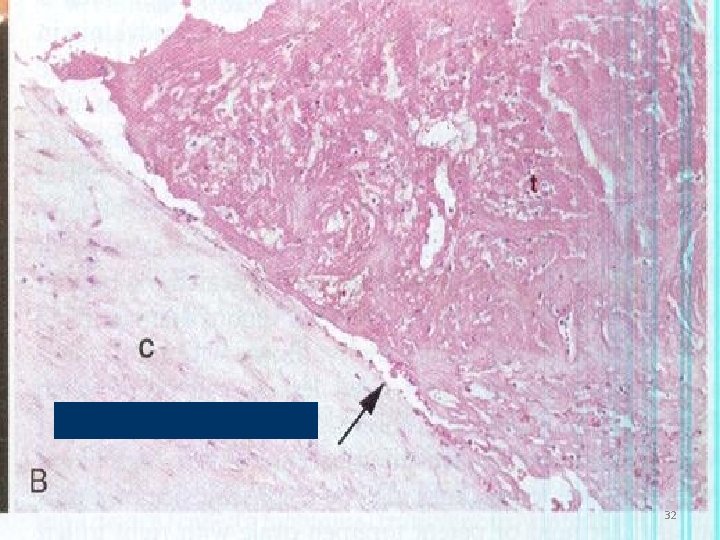
VALVE CUSP 32
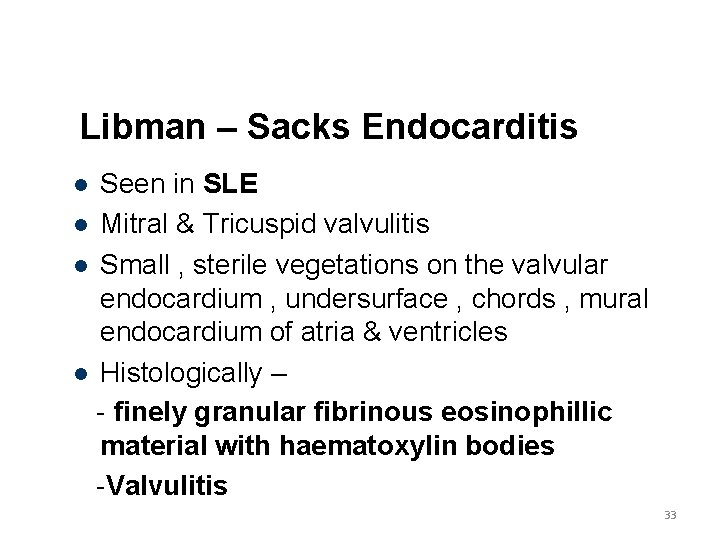
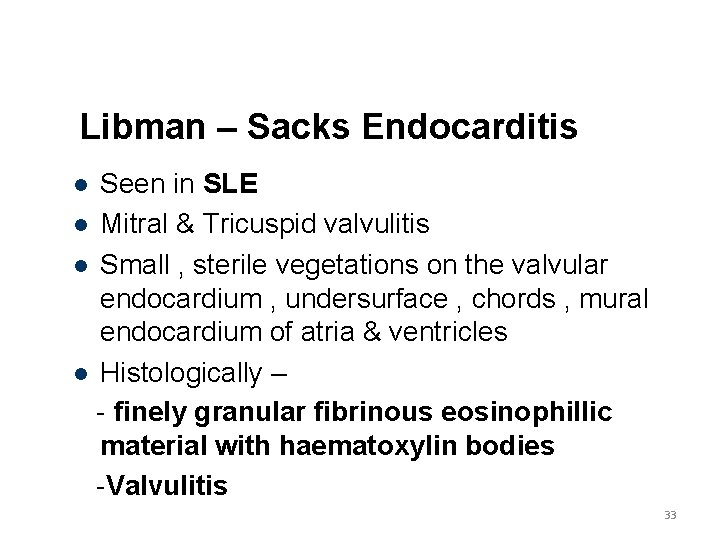
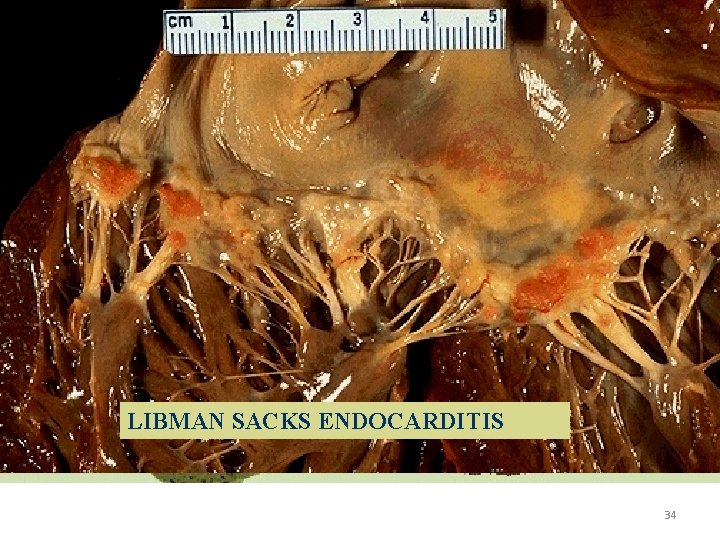
Libman – Sacks Endocarditis Seen in SLE Mitral & Tricuspid valvulitis Small , sterile vegetations on the valvular endocardium , undersurface , chords , mural endocardium of atria & ventricles Histologically – - finely granular fibrinous eosinophillic material with haematoxylin bodies -Valvulitis 33
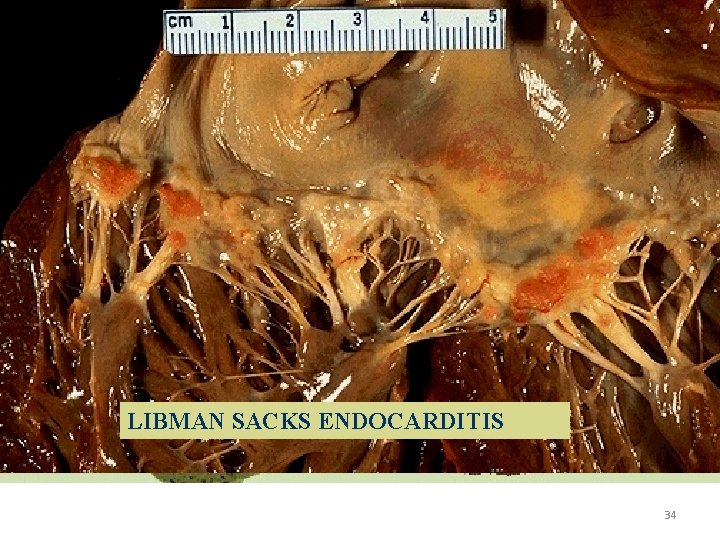
LIBMAN SACKS ENDOCARDITIS 34
35
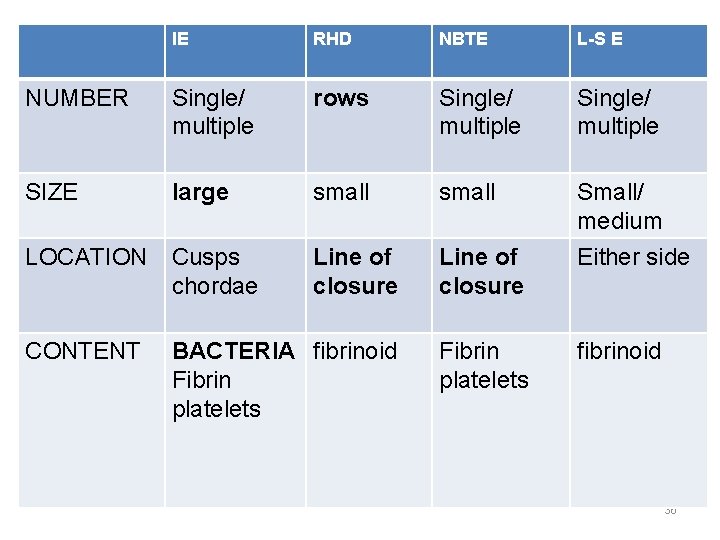
IE RHD NBTE L-S E NUMBER Single/ multiple rows Single/ multiple SIZE large small LOCATION Cusps chordae Line of closure Small/ medium Either side CONTENT BACTERIA fibrinoid Fibrin platelets fibrinoid 36
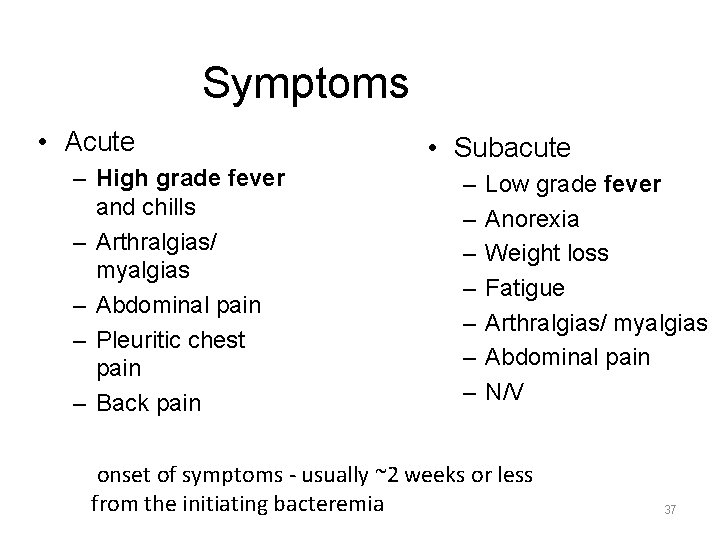
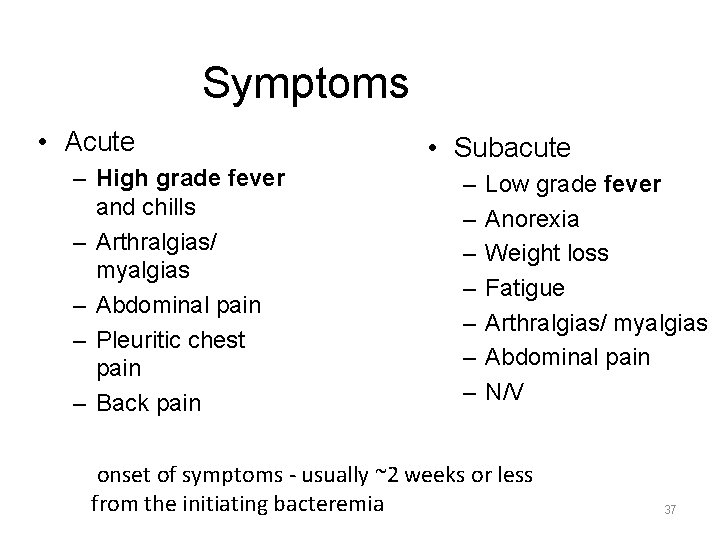
Symptoms • Acute – High grade fever and chills – Arthralgias/ myalgias – Abdominal pain – Pleuritic chest pain – Back pain • Subacute – – – – Low grade fever Anorexia Weight loss Fatigue Arthralgias/ myalgias Abdominal pain N/V onset of symptoms - usually ~2 weeks or less from the initiating bacteremia 37
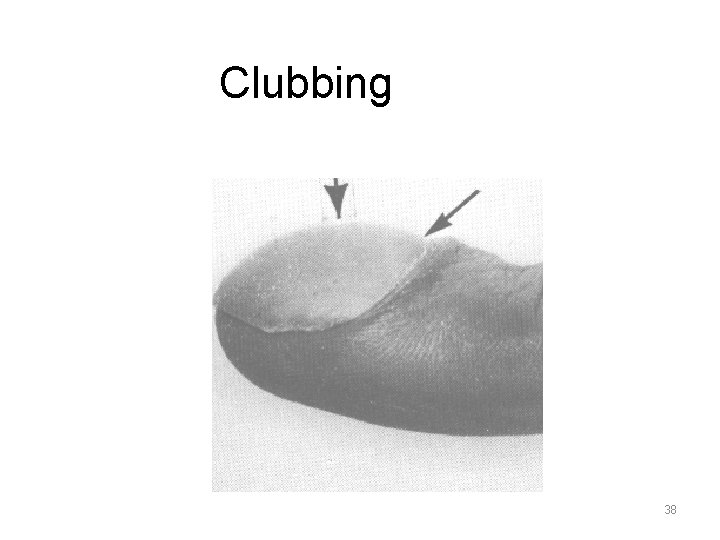
Clubbing 38

petechiae 39
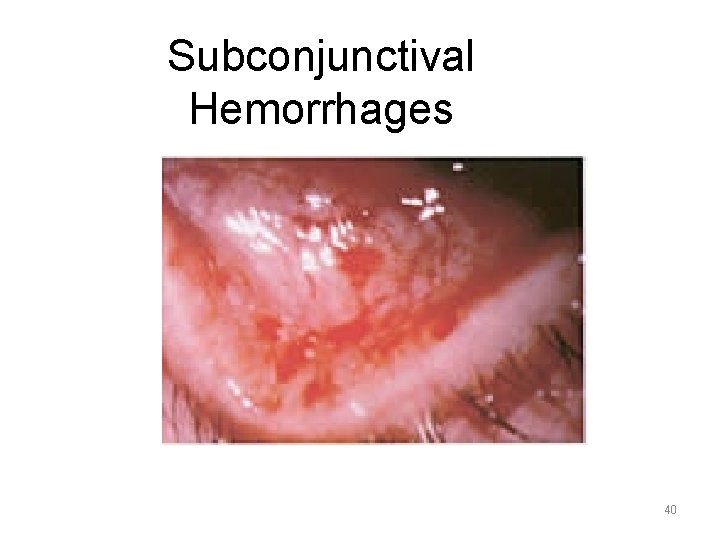
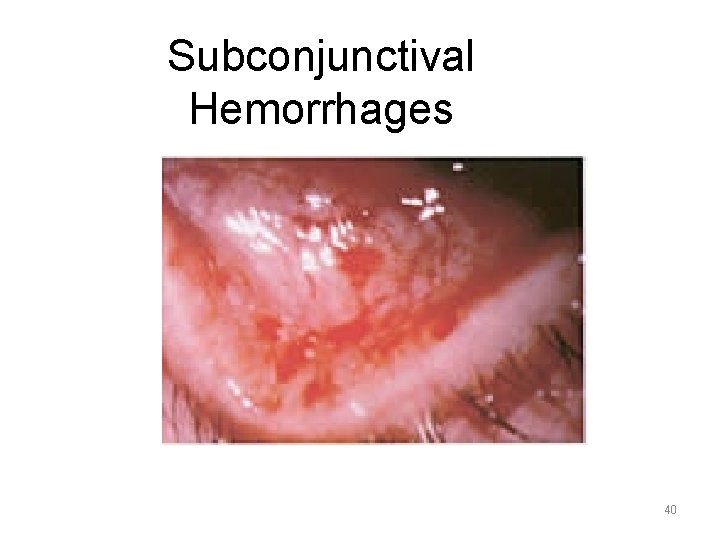
Subconjunctival Hemorrhages 40
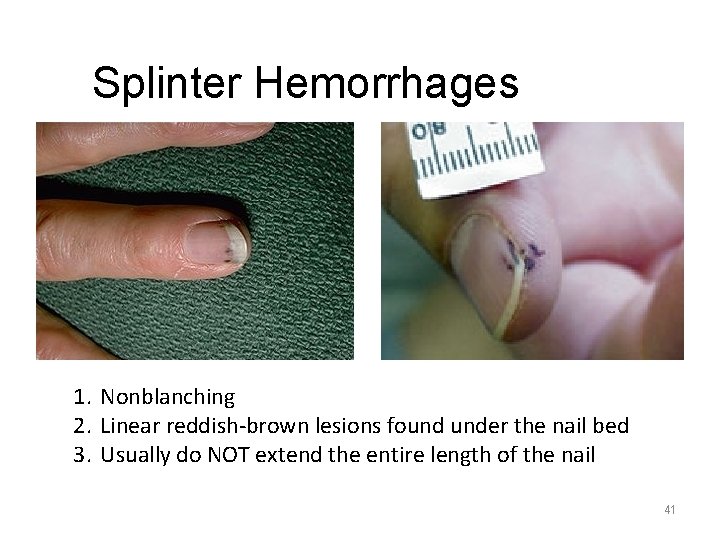
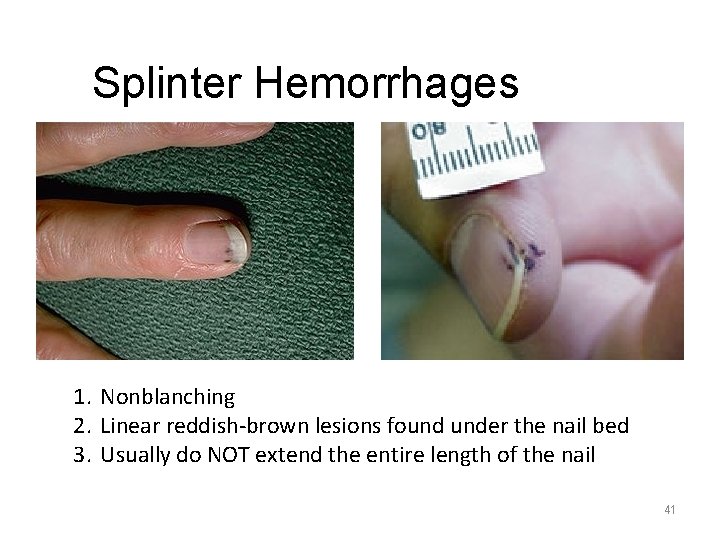
Splinter Hemorrhages 1. Nonblanching 2. Linear reddish-brown lesions found under the nail bed 3. Usually do NOT extend the entire length of the nail 41
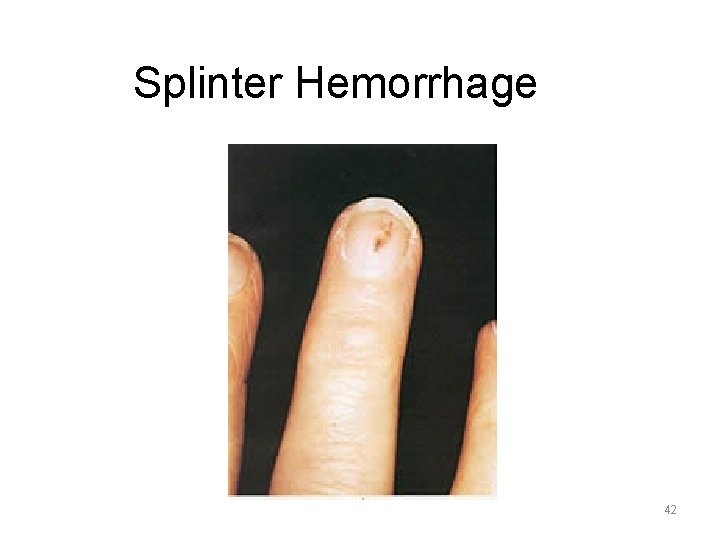
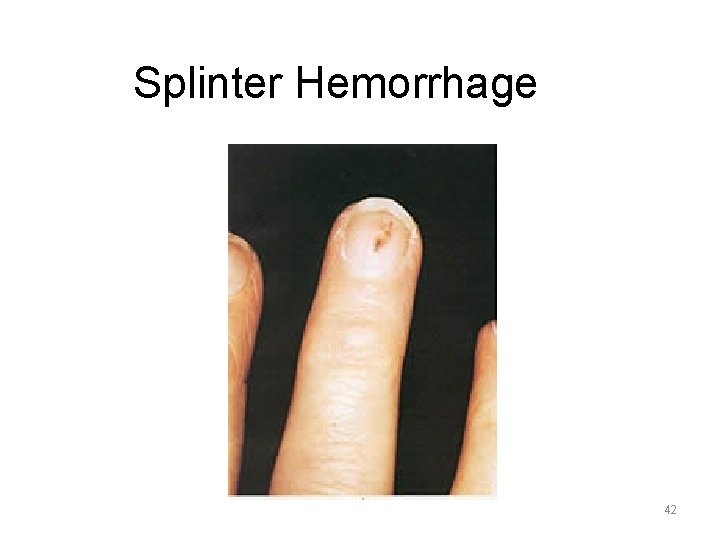
Splinter Hemorrhage 42
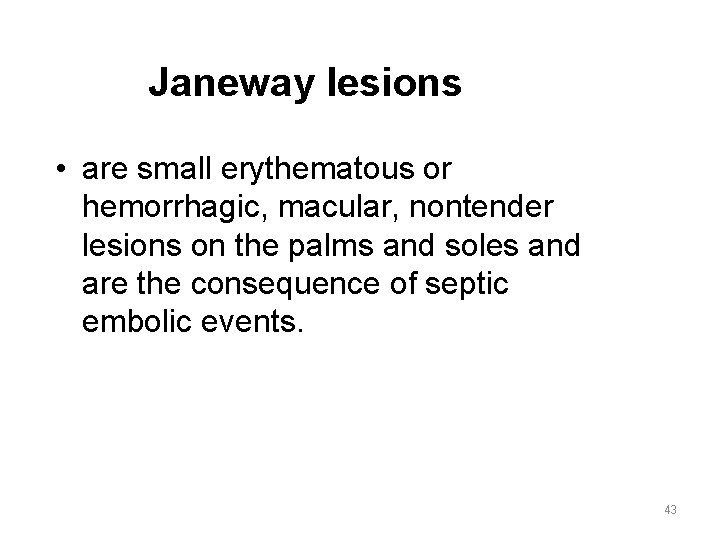
Janeway lesions • are small erythematous or hemorrhagic, macular, nontender lesions on the palms and soles and are the consequence of septic embolic events. 43

Janeway Lesions 44

Janeway Lesions 45
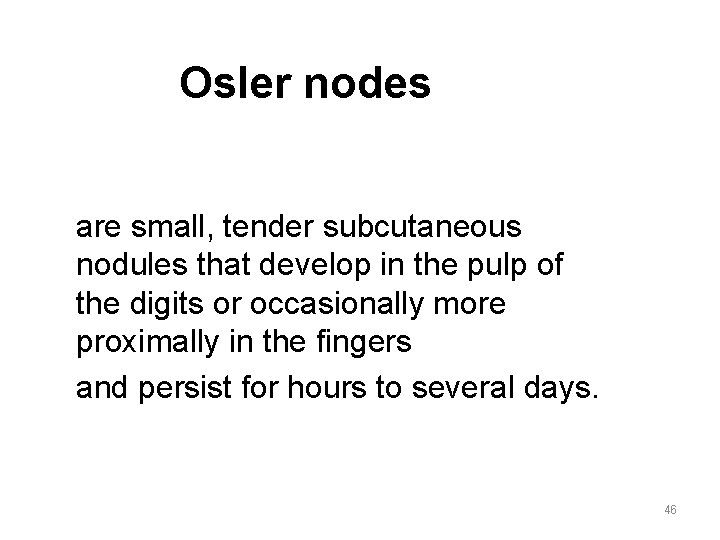
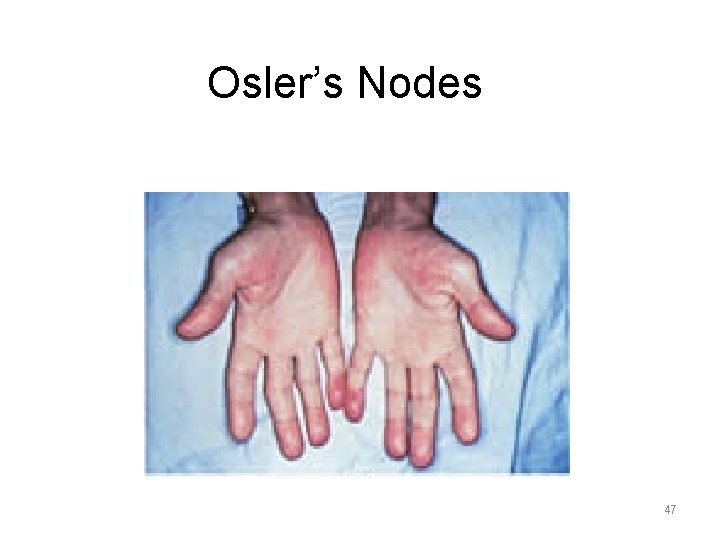
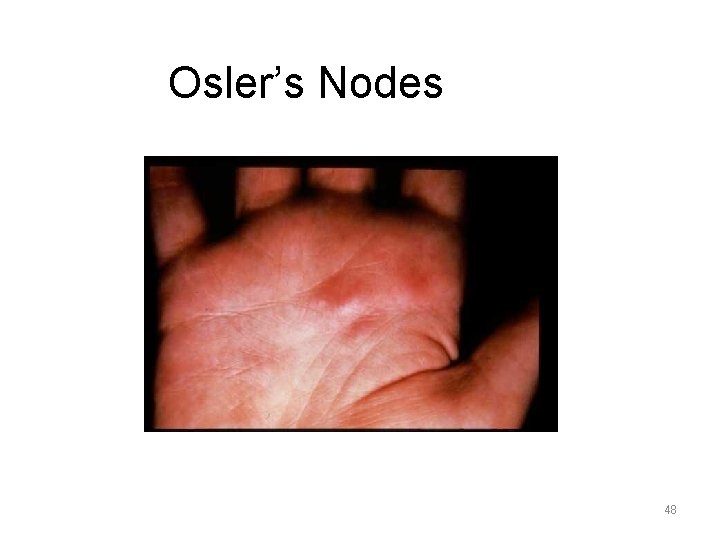
Osler nodes are small, tender subcutaneous nodules that develop in the pulp of the digits or occasionally more proximally in the fingers and persist for hours to several days. 46
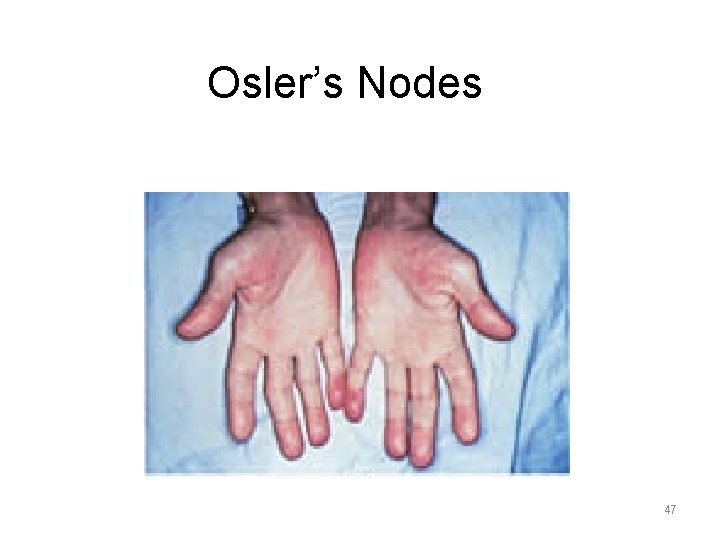
Osler’s Nodes 47
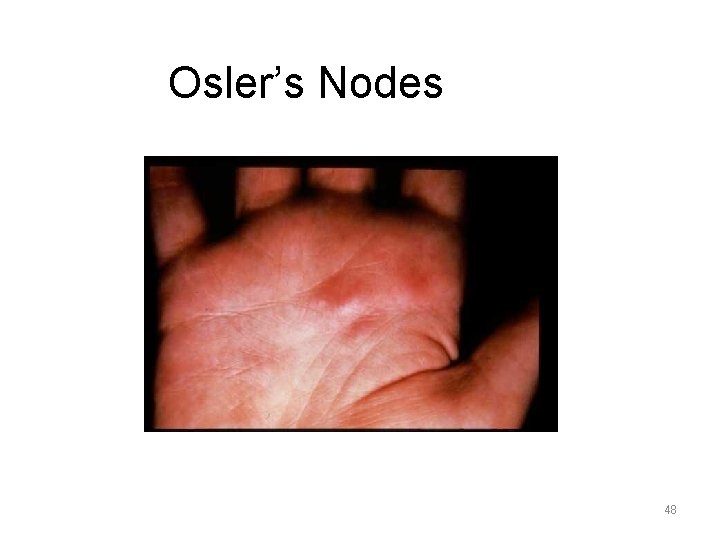
Osler’s Nodes 48
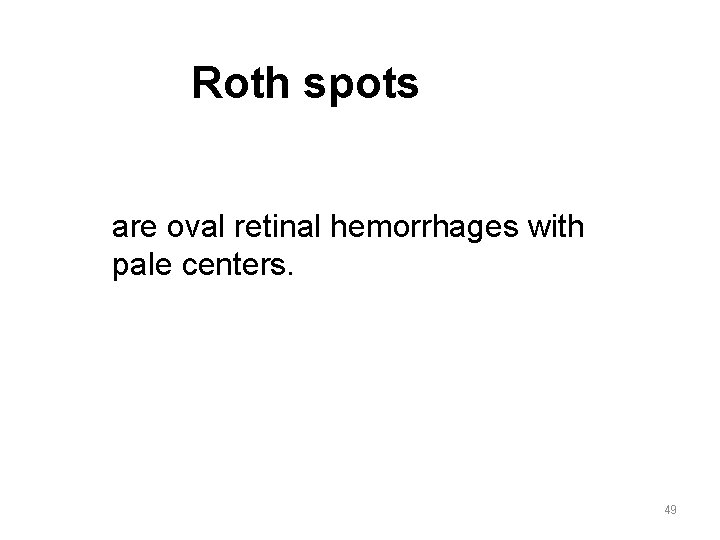
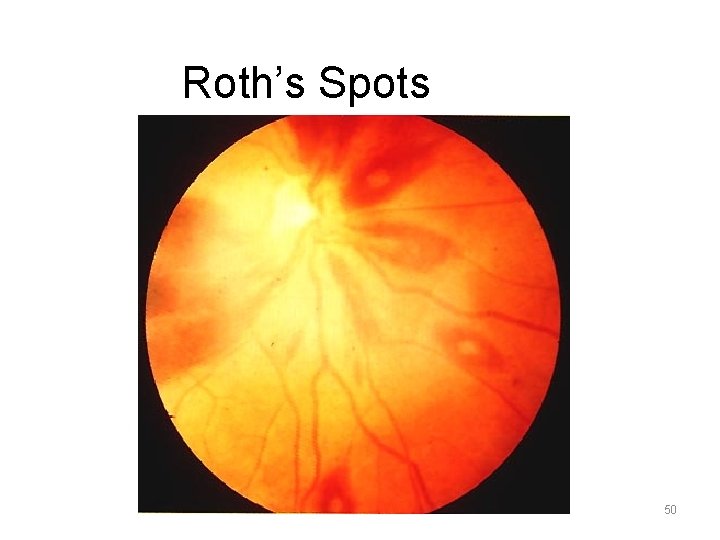
Roth spots are oval retinal hemorrhages with pale centers. 49
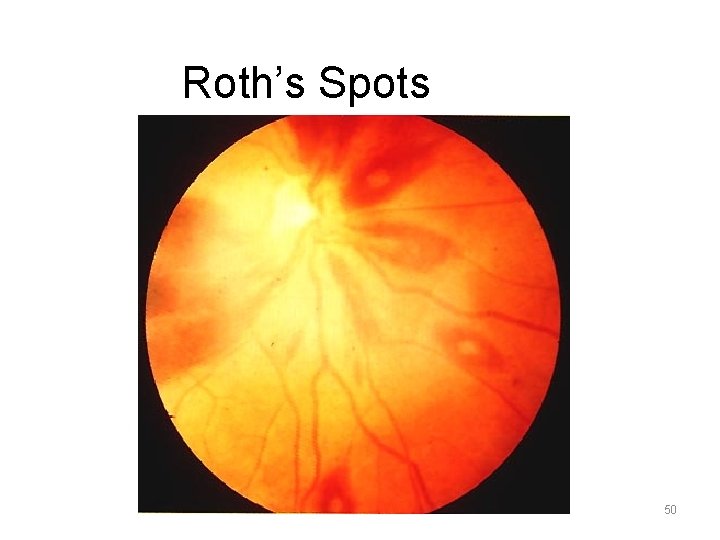
Roth’s Spots 50
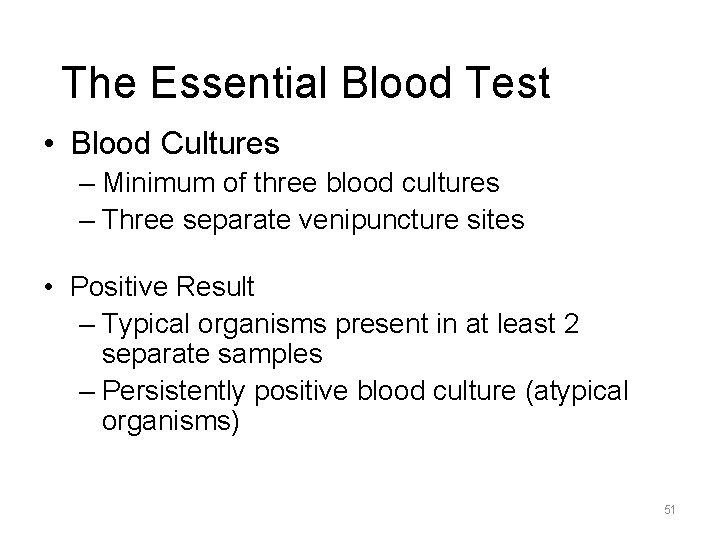
The Essential Blood Test • Blood Cultures – Minimum of three blood cultures – Three separate venipuncture sites • Positive Result – Typical organisms present in at least 2 separate samples – Persistently positive blood culture (atypical organisms) 51
Additional Labs • • • CBC ESR and CRP Complement levels (C 3, C 4, Urinalysis RFT 52
Imaging • Chest x-ray – Look for multiple focal infiltrates and calcification of heart valves • EKG – Rarely diagnostic – Look for evidence of ischemia, conduction delay, and arrhythmias • Echocardiography 53
Complications – Embolic – Local spread of infection – Metastatic spread of infection – Formation of immune complexes – glomerulonephritis and arthritis 54
Local Spread of Infection Cardiac complications • Extensive valvular damage perforation, insufficiency, dehiscence of artificial valve • Paravalvular abscess , ring abscess – Most common in aortic valve, IVDA, and S. aureus – May extend into adjacent conduction tissue causing arrythmias – Higher rates of embolization and mortality 55
Cardiac complications • Pericarditis • Fistulous intracardiac connections • Cardiac failure 56
Metastatic Spread of Infection • Metastatic abscess – Kidneys, spleen, lungs, brain, soft tissues • • • Meningitis and/or encephalitis Vertebral osteomyelitis Septic arthritis Septic infarcts Mycotic aneurysms 57
Organs • Neurologic manifestations Cerebral emboli, cerebritis, brain abscess, hemorrhage, . • Peripheral embolization Ischemia, infarction, mycotic aneurysms • Pulmonary infarction • Glomerulonephritis, Renal insufficiency • Congestive heart failure 58
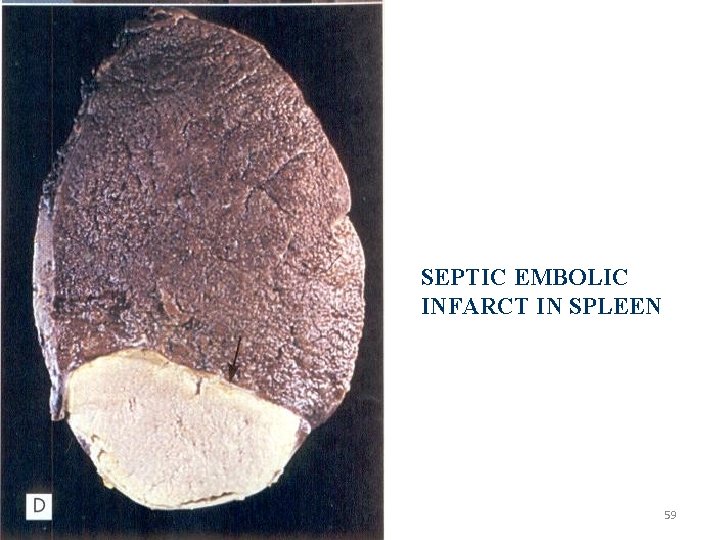
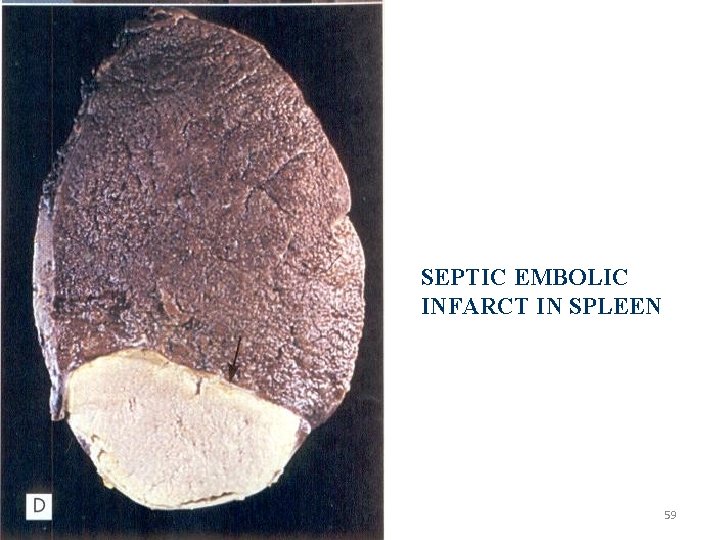
SEPTIC EMBOLIC INFARCT IN SPLEEN 59
Diagnostic Criteria PATHOLOGIC CRITERIA • Microorganisms, demonstrated by culture or histologic examination, in a vegetation, embolus from a vegetation, or intracardiac abscess • Histologic confirmation of active endocarditis in vegetation or intracardiac abscess 60
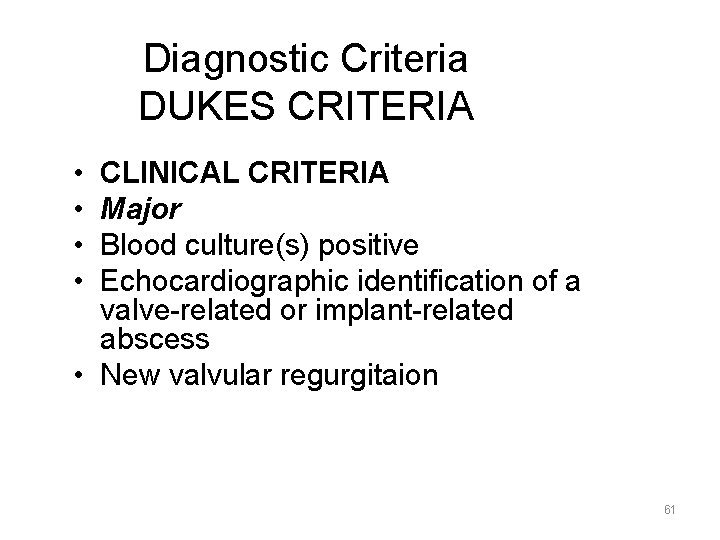
Diagnostic Criteria DUKES CRITERIA • • CLINICAL CRITERIA Major Blood culture(s) positive Echocardiographic identification of a valve-related or implant-related abscess • New valvular regurgitaion 61
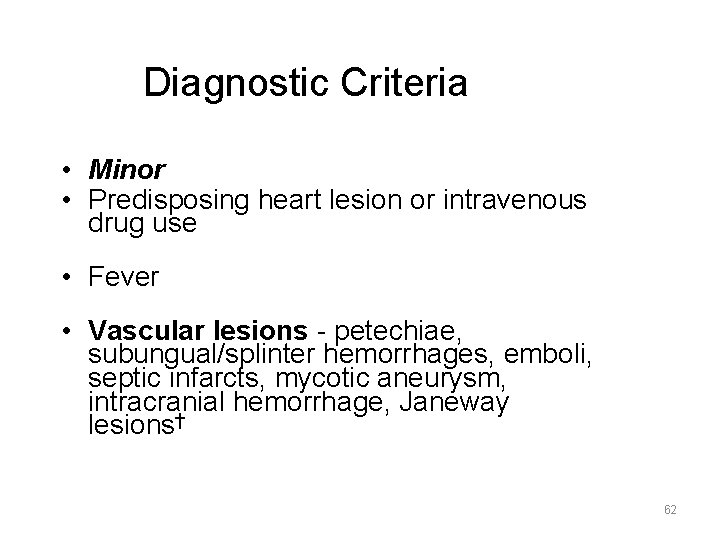
Diagnostic Criteria • Minor • Predisposing heart lesion or intravenous drug use • Fever • Vascular lesions - petechiae, subungual/splinter hemorrhages, emboli, septic infarcts, mycotic aneurysm, intracranial hemorrhage, Janeway lesions† 62

• Immunological phenomena, including glomerulonephritis, Osler nodes, Roth spots, rheumatoid factor • Microbiologic evidence, including a single culture positive for an unusual organism • Echocardiographic findings consistent with but not diagnostic of endocarditis, including worsening or changing of a preexistent murmur 63
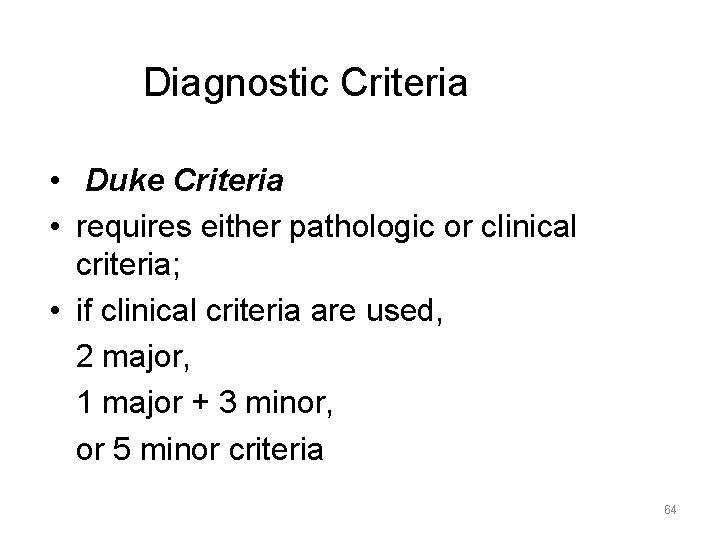
Diagnostic Criteria • Duke Criteria • requires either pathologic or clinical criteria; • if clinical criteria are used, 2 major, 1 major + 3 minor, or 5 minor criteria 64