Infectious Endocarditis Chris Goddard CNP Infectious Disease UCMC



- Slides: 106
Infectious Endocarditis Chris Goddard, CNP Infectious Disease UCMC
Me Went to Archbishop Moeller HS ’ 04 Undergrad @ Kent State University – major in nursing and minor in psych ‘ 09 UCMC neuroscience nurse for ~5 years Acute Care of Gero/Adult ‘ 14 ~6 years with Infectious Disease at UCMC Adjunct faculty at UC Co. N and NKU Co. N 674 diagnostic codes entered in last year
My general cardiac knowledge male female
My general cardiac knowledge Male Female
My general cardiac knowledge Female Male ego Situationally appropriate humor, superior intelligence
Infective Endocarditis Presentation Febrile illness – r/o Cotton Fever Myalgia’s and arthralagia’s Persistent bacteremia Characteristic lesion of microbial infection of the endothelial surface of the heart Variable in size Amorphous mass of fibrin & platelets Abundant organisms Few inflammatory cells
Infective Endocarditis Case rate may vary between 2 -3 cases /100, 000 to as high as 15 -30/100, 000 depending on incidence of i. v. drug abuse and age of the population 55 -75% of patients with native valve endocarditis (NVE) have underlying valve abnormalities MVP Rheumatic Congenital i. v. drug abuse
GENERAL CONSIDERATIONS In IVDU’s incidence is 150 -2000 per 100, 000 person years. Due to IVDU the average has shifted down and more likely to see Right sided endocarditis (and more like TV) Incidence rate is 2 -3 fold higher in men Poor dental hygiene, hemodialysis & DM associated with increased risk
CHANGING EPIDEMIOLOGY Degenerative valve disease Prosthetic valves; intra-vascular devices Hemodialysis, diabetes, HIV, drug abuse S. aureus, MRSA, HCA- and CA-infections Antibiotic resistance
Infective Endocarditis Adult population MVP – prominent predisposing factor High prevalence in population viridans group streptococci (oral flora) 20% in young women Accounts for 7 – 30% NVE in cases not related to drug abuse or nosocomial infection Relative risk in MVP ~3. 5 – 8. 2, largely confined to patients with murmur, but also increased in men and patients >45 years old MVP with murmur – MVP w/o murmur – incidence IE 52/100/000 pt. years incidence IE 4. 6/100, 000 pt. years
Infective Endocarditis Adult population Rheumatic Heart Disease 20 – 25% of cases of IE in 1970’s & 80’s 7 – 18% of cases in recent reported series Mitral site more common in women Aortic site more common in men Congenital Heart Disease 10 – 20% of cases in young adults 8% of cases in older adults PDA, VSD, bicuspid aortic valve (esp. in men>60)
Infective Endocarditis Pediatric population The vast majority (75 -90%) of cases after the neonatal period are associated with an underlying congenital abnormality Aortic valve VSD Tetralogy of Fallot Microbiology Neonates: S. aureus, coag – staph, group B strep Older children: 40% strep, S. aureus
Infective Endocarditis Intravenous Drug Abuse Risk is 2 – 5% per pt. /year Tendency to involve right-sided valves Distribution in clinical series 46 – 78% tricuspid 24 – 32% mitral 8 – 19% aortic Underlying valve normal in 75 – 93% S. aureus predominant organism (>50%, 60 -70% of tricuspid cases)
Infective Endocarditis Intravenous Drug Abuse Increased frequency of gram negative infection such as P. aeruginosa & fungal infections High concordance of HIV positivity & IE (27 -73%) HIV status does not in itself modify clinical picture Survival is decreased if CD 4 count < 200/mm 3
Infective Endocarditis in the 21 st Century International Collaboration on Endocarditis (ICE) was established in 1999. From June 2000 through September 2005, 2781 adult patients with definite IE (by modified Duke criteria) were enrolled from 58 sites in 25 countries. The median age of the cohort was 58. Most patients (72%) had native-valve IE, and 23% of episodes were categorized as healthcare associated
Infective Endocarditis in the 21 st Century The most common predisposing factors were native-valve disease (32%), an invasive procedure during the previous 60 days (27%), congenital heart disease (12%), and active intravenous drug use (10%). Staphylococcus aureus was the most common causative organism (31%), followed by viridans group streptococci (VGS; 17%).
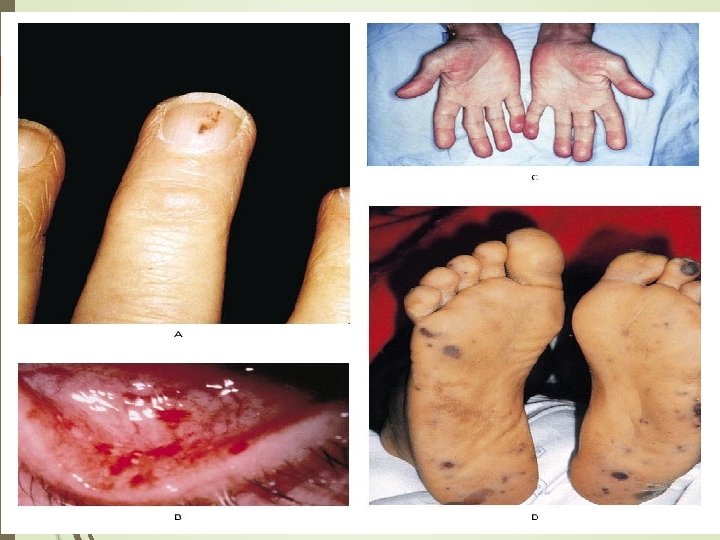
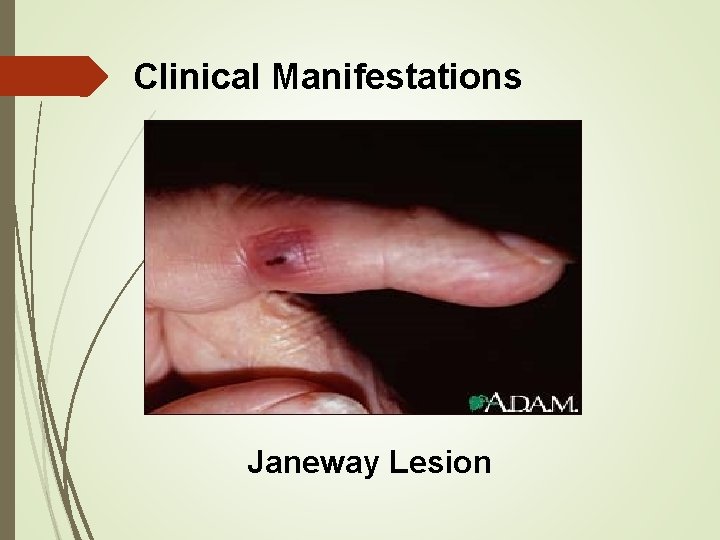
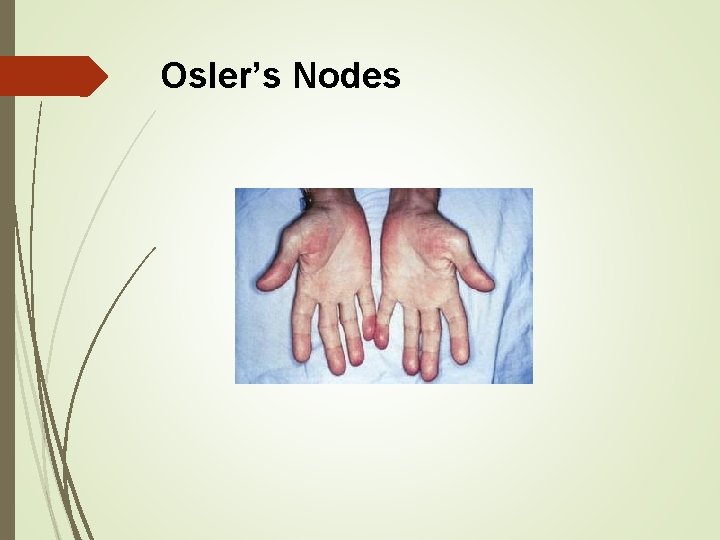
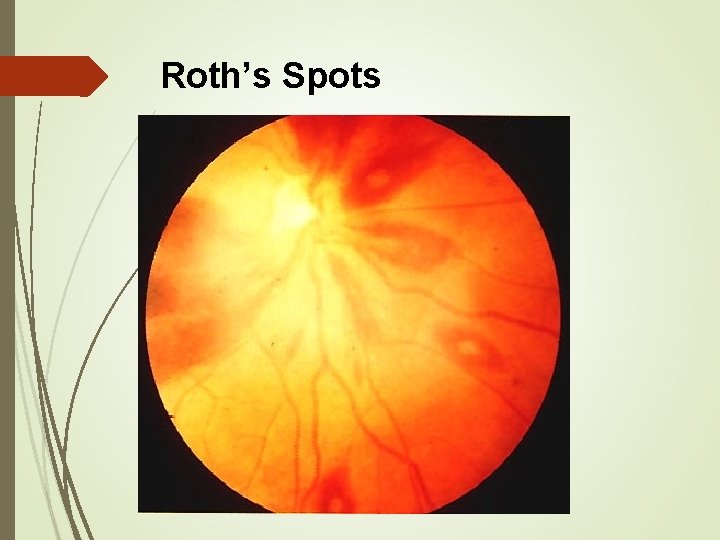
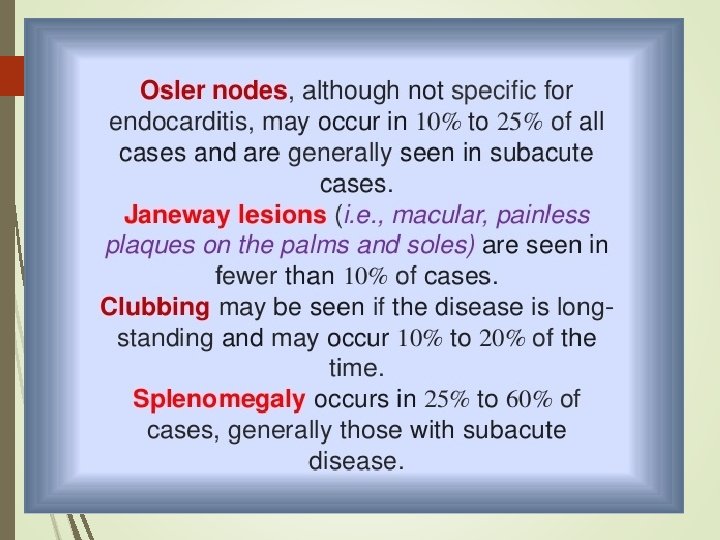
Infective Endocarditis in the 21 st Century Most patients (77%) presented 1 month after symptom onset, and few exhibited the classic findings of splinter hemorrhages (8%), Janeway lesions (5%), Osler nodes (3%), or Roth spots (2%). Serious complications included congestive heart failure (32%), nonstroke embolic events (23%), stroke (17%), and intracardiac abscess (14%
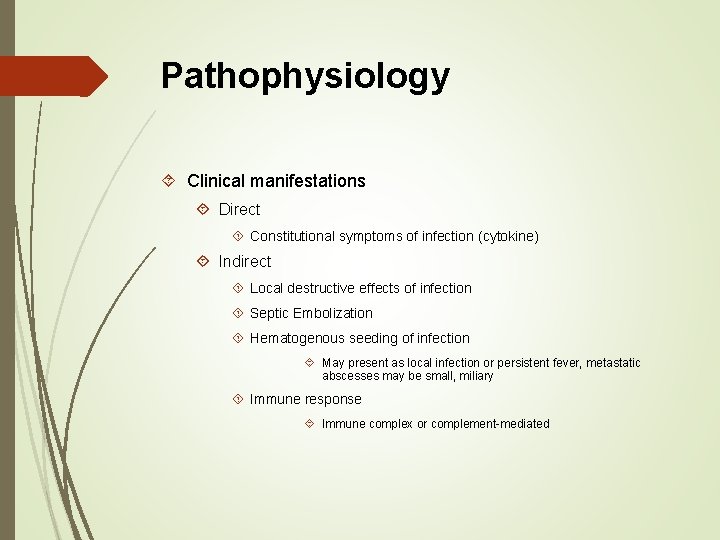
Pathophysiology Clinical manifestations Direct Constitutional symptoms of infection (cytokine) Indirect Local destructive effects of infection Septic Embolization Hematogenous seeding of infection May present as local infection or persistent fever, metastatic abscesses may be small, miliary Immune response Immune complex or complement-mediated
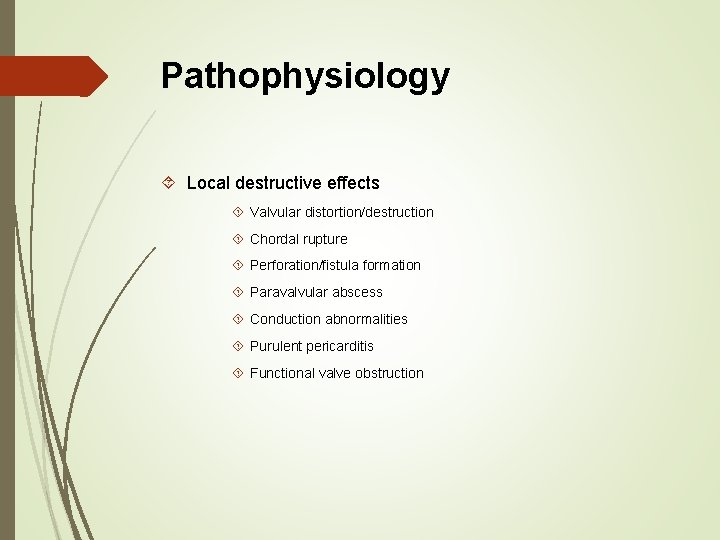
Pathophysiology Local destructive effects Valvular distortion/destruction Chordal rupture Perforation/fistula formation Paravalvular abscess Conduction abnormalities Purulent pericarditis Functional valve obstruction
Staph aureus Bacteremia Prevalence if IE is variable 13 -25% Factors associated with increased probability include: Community acquisition, absence of a primary focus, presence of metastatic sequelae, & fever or bacteremia >3 days after removal of catheter
Common Clinical Findings History of cardiac risk factors or IVDA Fever, malaise, night sweats New regurgitant murmur, heart failure Less common: Janeway lesions, Osler nodes, Roth spots – absent in 80 -90% Splenomegaly
Clinical Situations Constituting High Risk for Complications for IE Prosthetic cardiac valves Left-sided IE S aureus IE Fungal IE Previous IE Prolonged clinical symptoms ( 3 months) Cyanotic congenital heart disease Patients with systemic to pulmonary shunts Poor clinical response to antimicrobial therapy
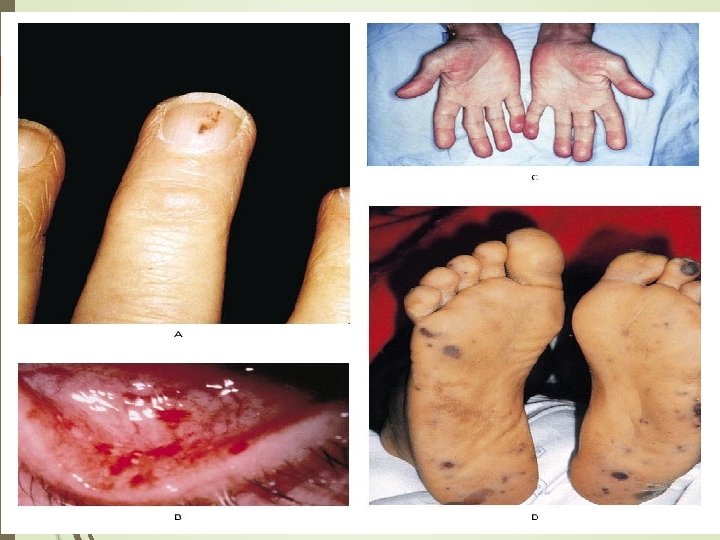
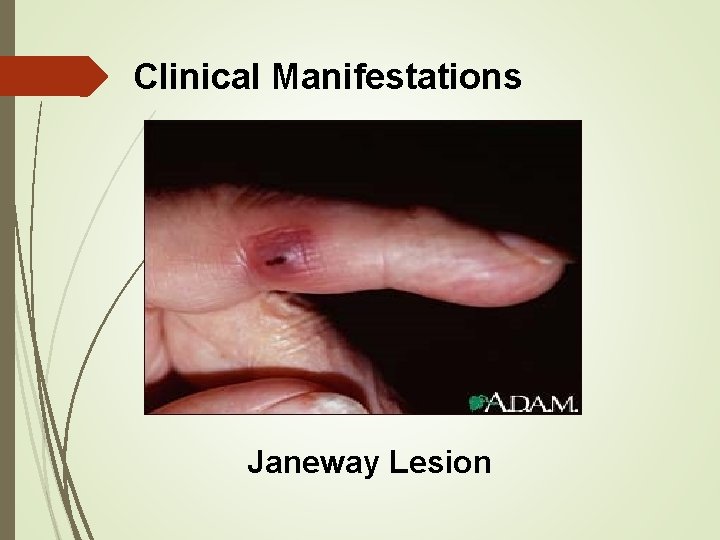
Clinical Manifestations Janeway Lesion

Splinter Hemorrhage
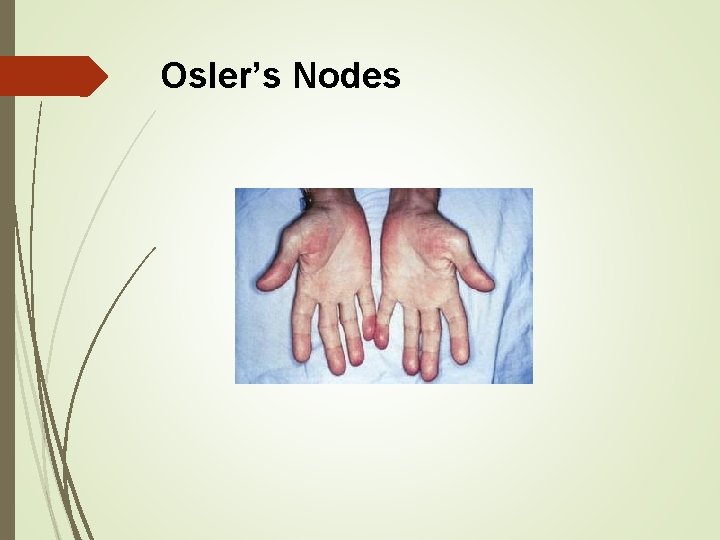
Osler’s Nodes
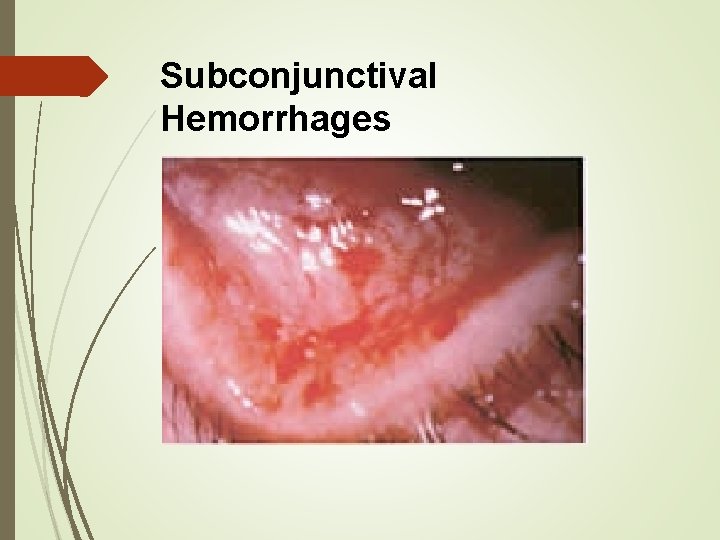
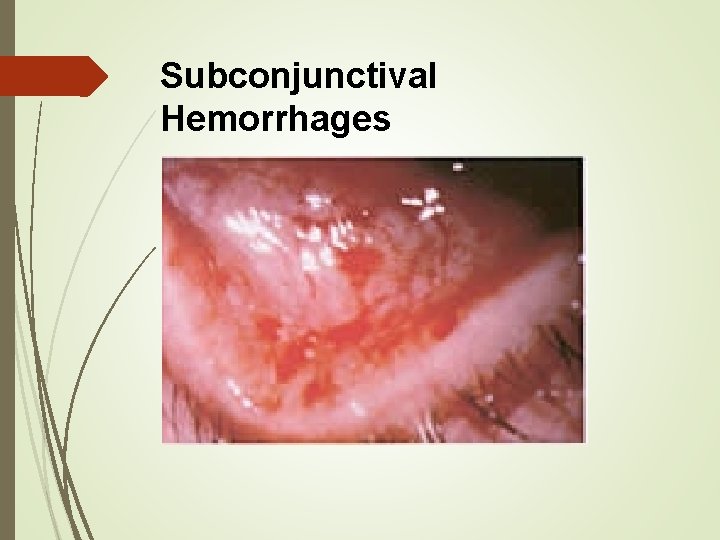
Subconjunctival Hemorrhages
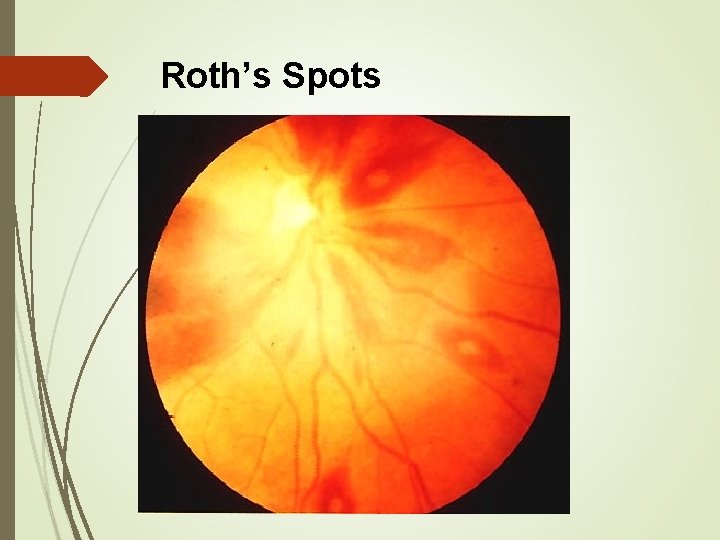
Roth’s Spots
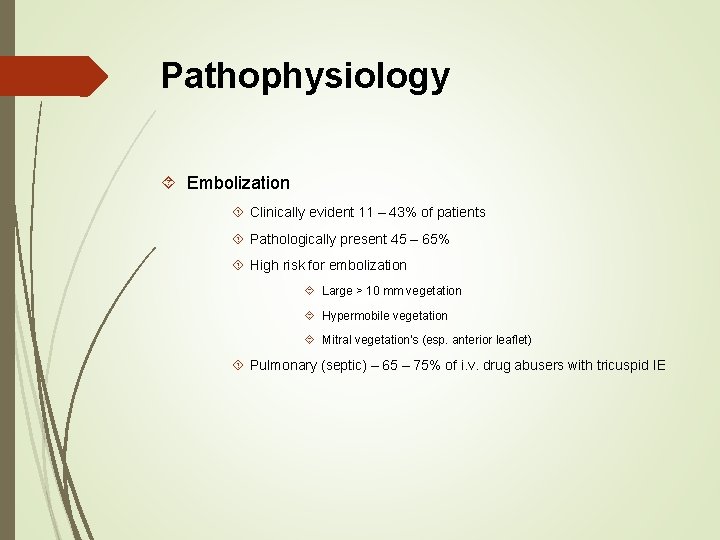
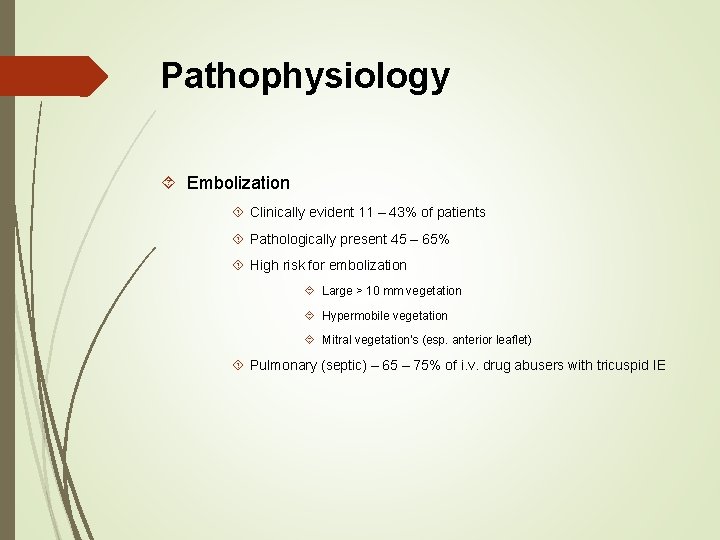
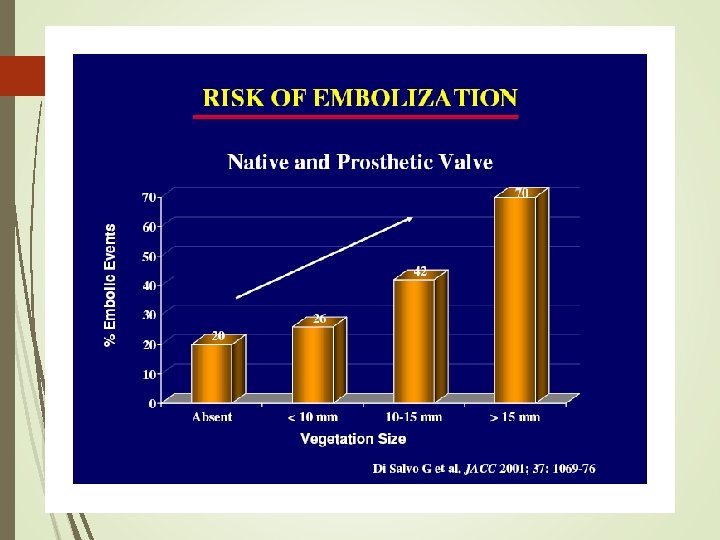
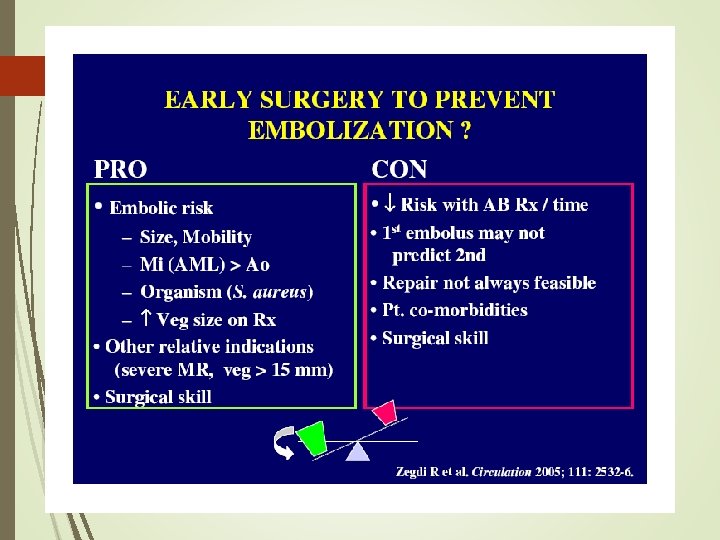
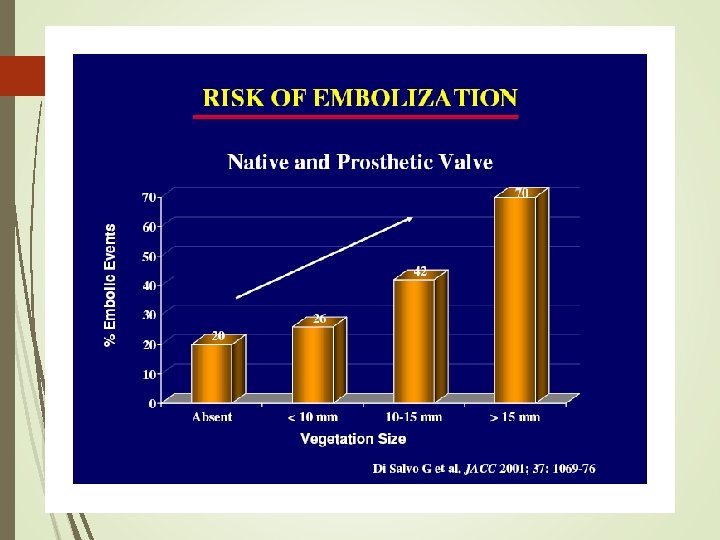
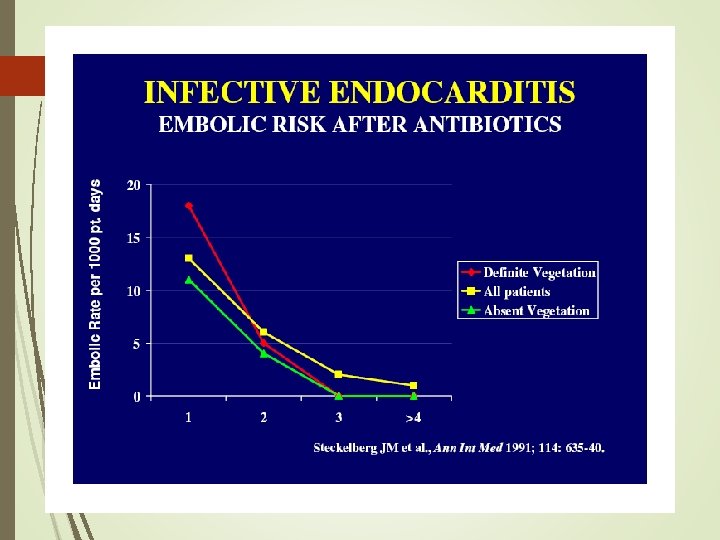
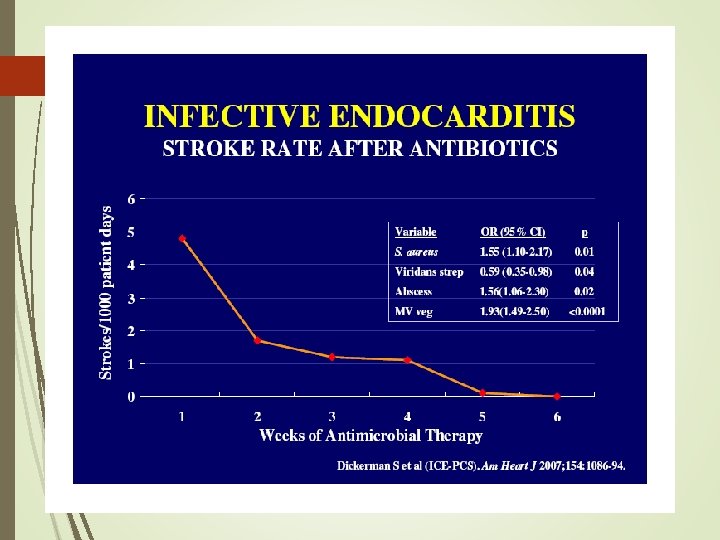
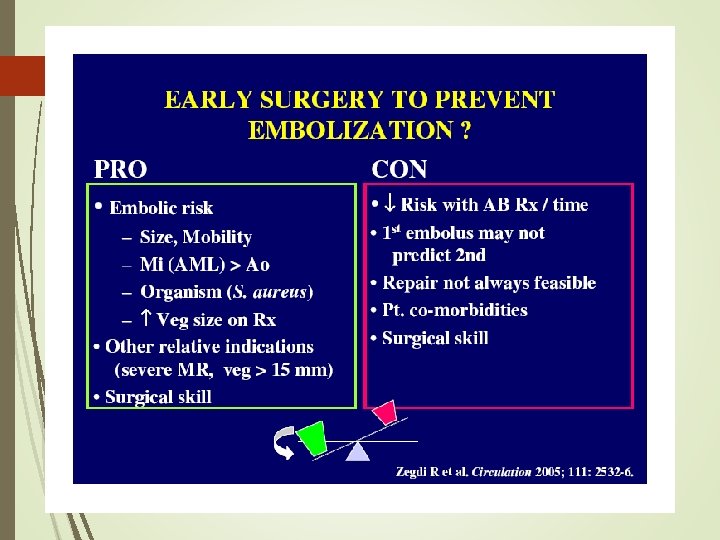
Pathophysiology Embolization Clinically evident 11 – 43% of patients Pathologically present 45 – 65% High risk for embolization Large > 10 mm vegetation Hypermobile vegetation Mitral vegetation's (esp. anterior leaflet) Pulmonary (septic) – 65 – 75% of i. v. drug abusers with tricuspid IE
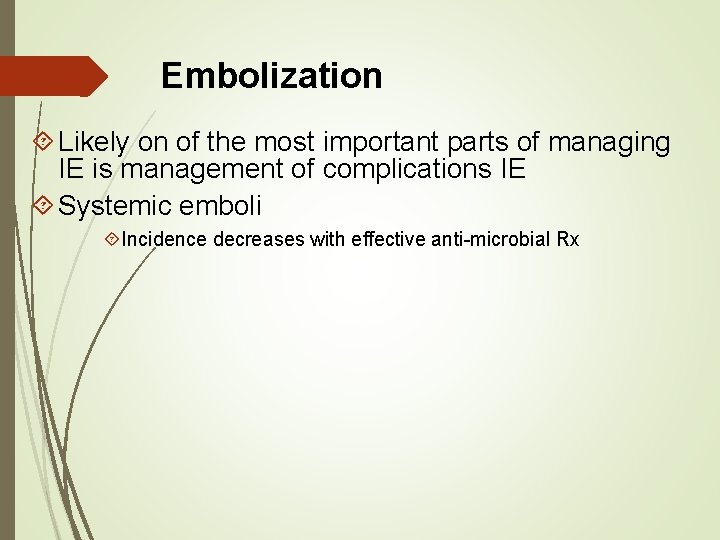
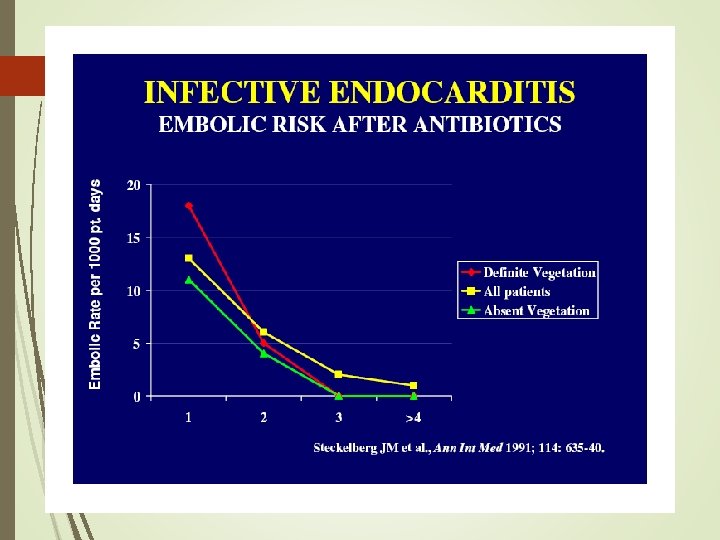
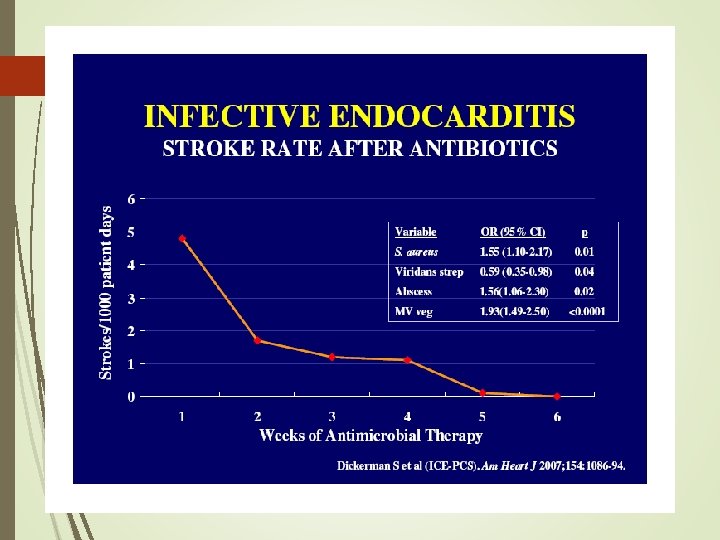
Embolization Likely on of the most important parts of managing IE is management of complications IE Systemic emboli Incidence decreases with effective anti-microbial Rx
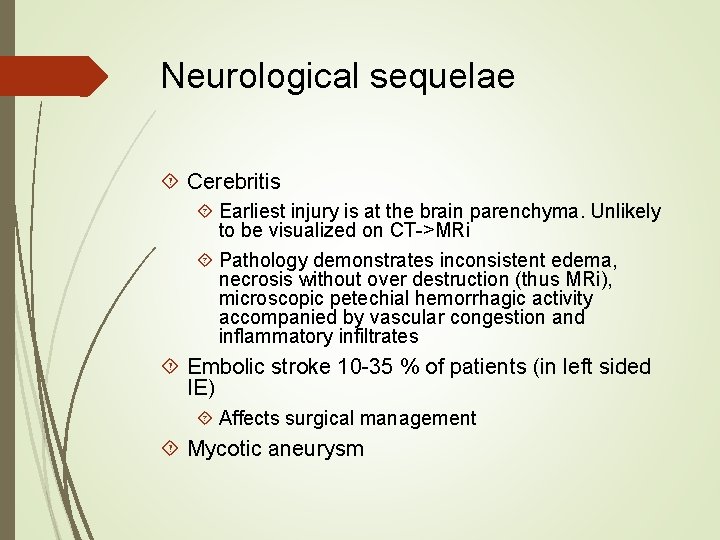
Neurological sequelae Cerebritis Earliest injury is at the brain parenchyma. Unlikely to be visualized on CT->MRi Pathology demonstrates inconsistent edema, necrosis without over destruction (thus MRi), microscopic petechial hemorrhagic activity accompanied by vascular congestion and inflammatory infiltrates Embolic stroke 10 -35 % of patients (in left sided IE) Affects surgical management Mycotic aneurysm
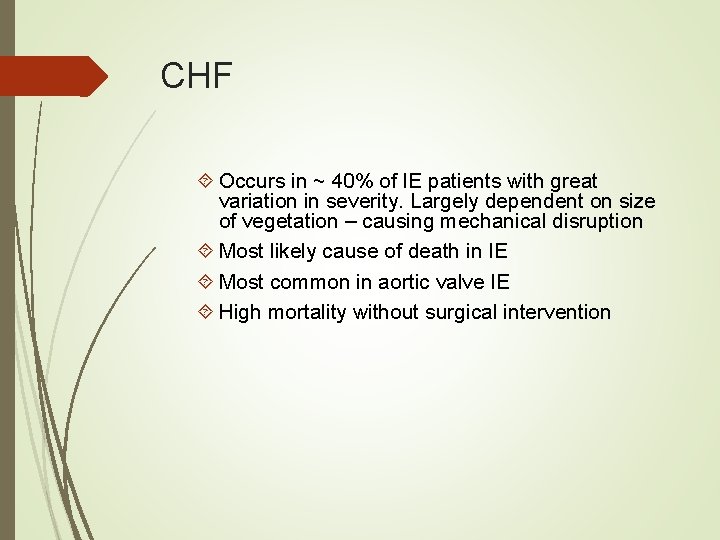
CHF Occurs in ~ 40% of IE patients with great variation in severity. Largely dependent on size of vegetation – causing mechanical disruption Most likely cause of death in IE Most common in aortic valve IE High mortality without surgical intervention
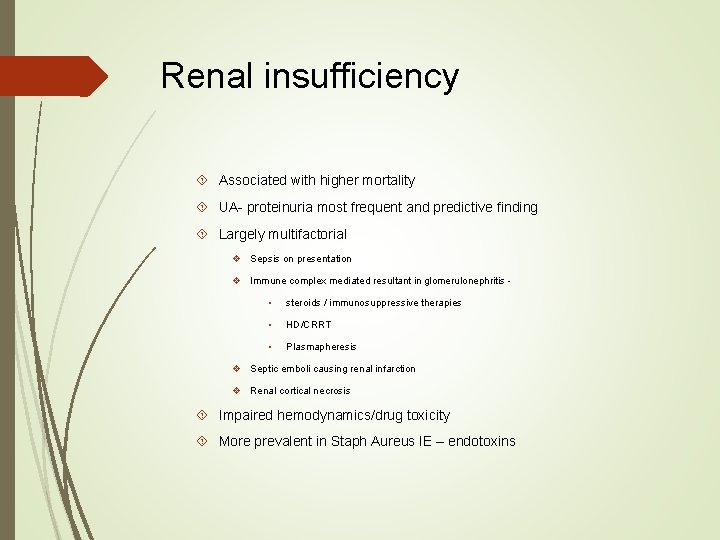
Renal insufficiency Associated with higher mortality UA- proteinuria most frequent and predictive finding Largely multifactorial v Sepsis on presentation v Immune complex mediated resultant in glomerulonephritis • steroids / immunosuppressive therapies • HD/CRRT • Plasmapheresis v Septic emboli causing renal infarction v Renal cortical necrosis Impaired hemodynamics/drug toxicity More prevalent in Staph Aureus IE – endotoxins
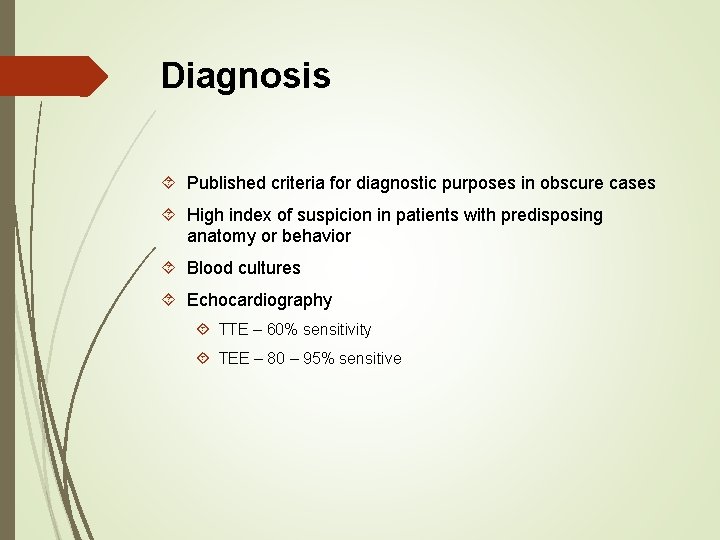
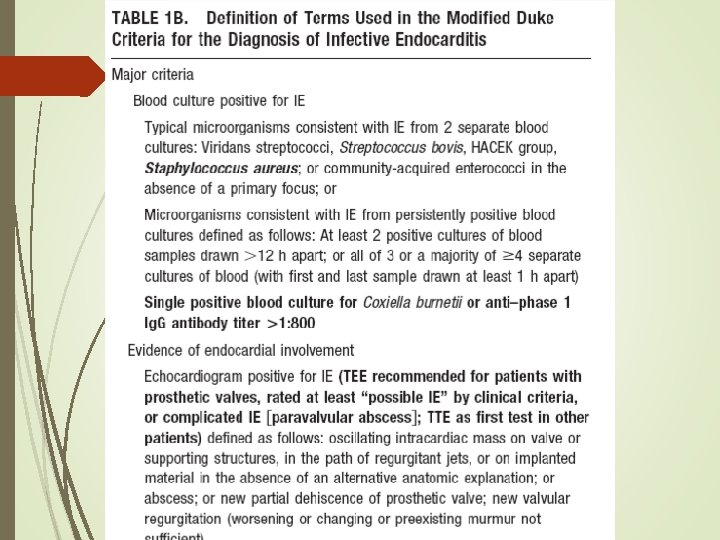
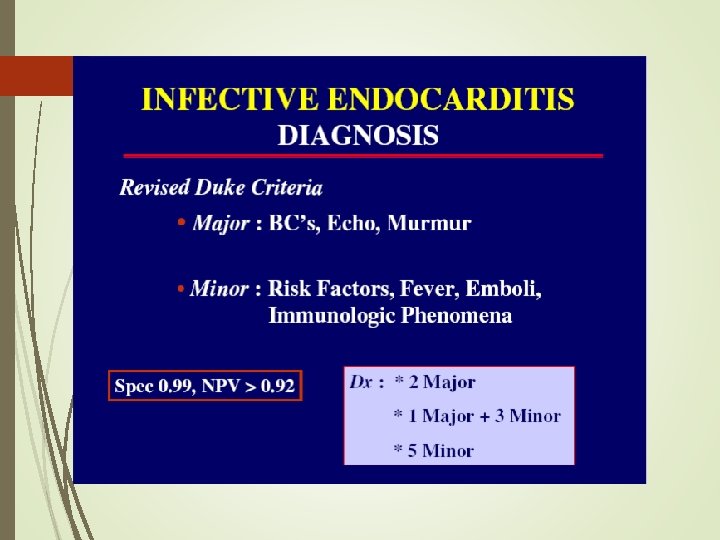
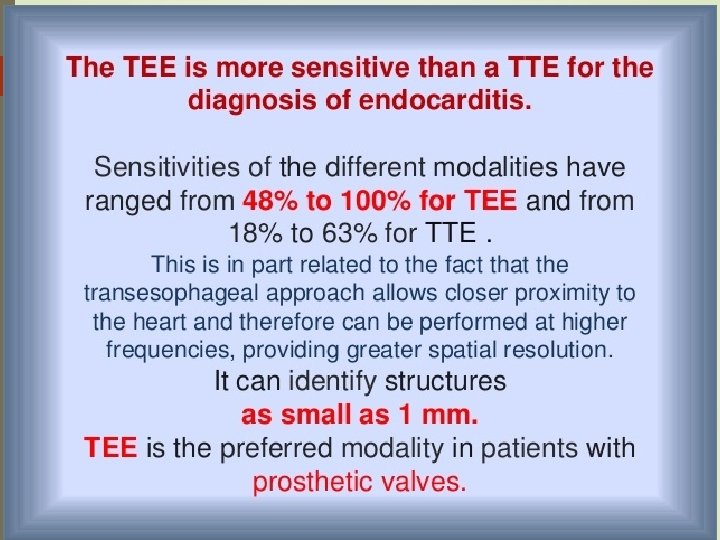
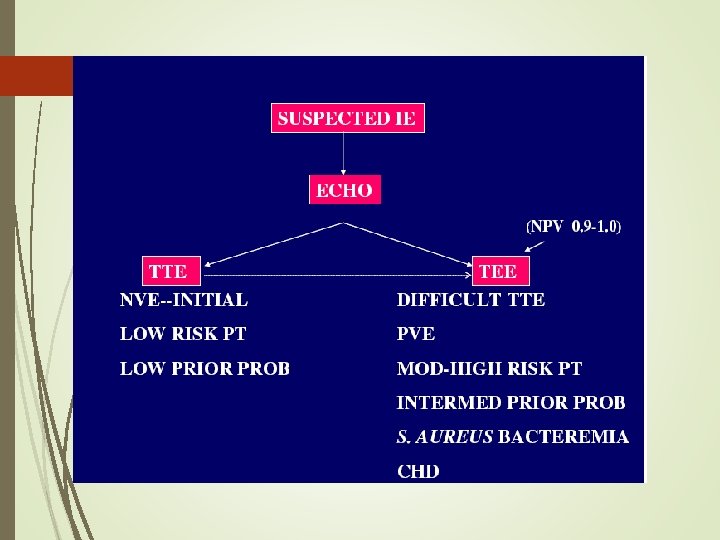
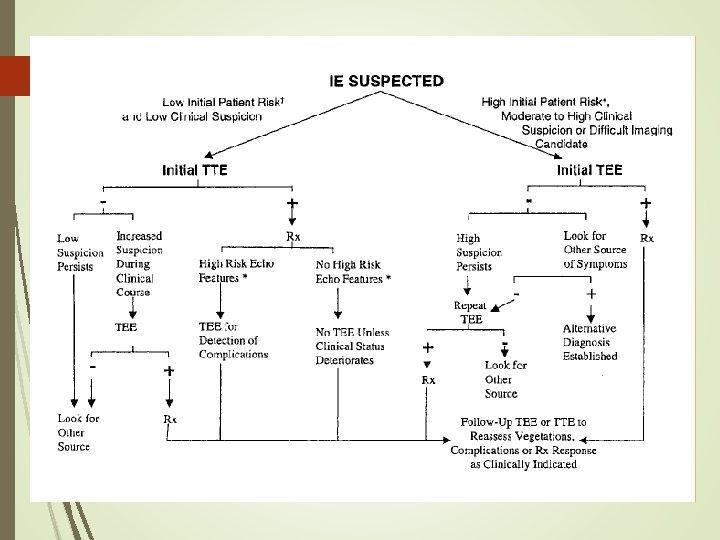
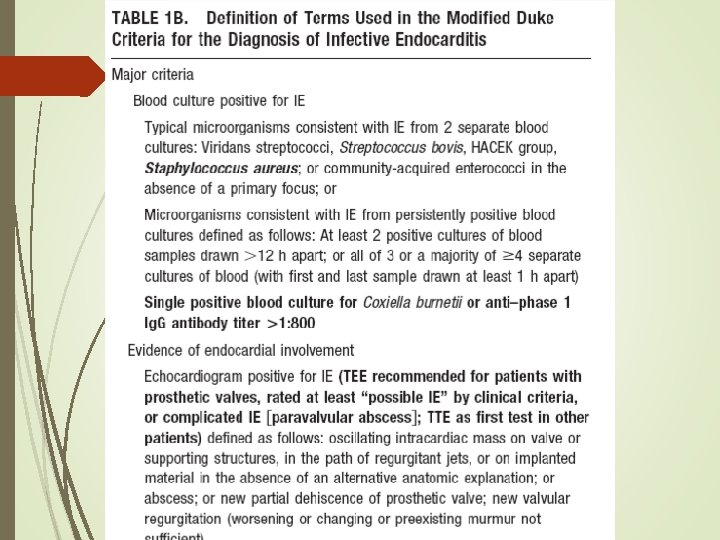
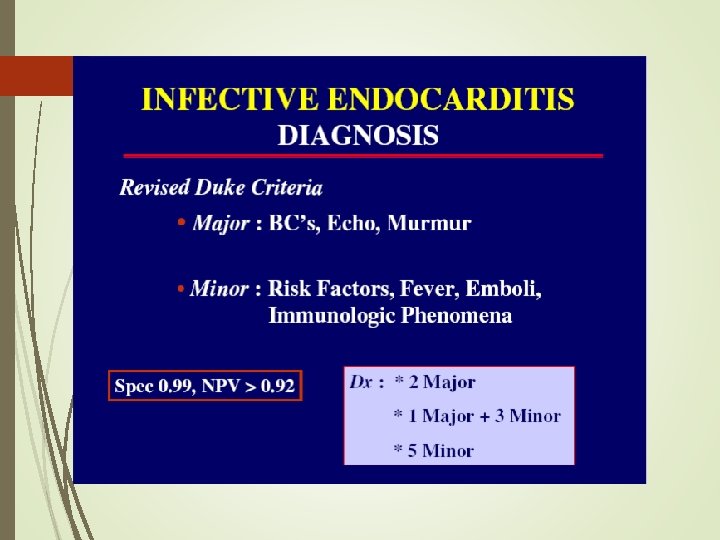
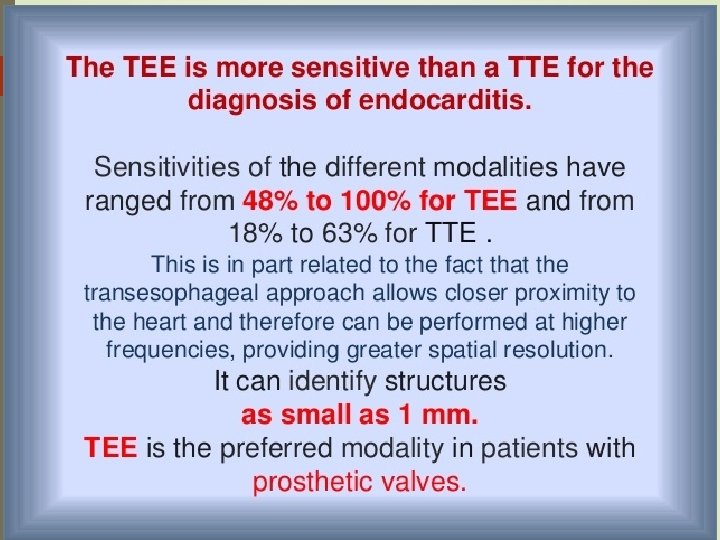
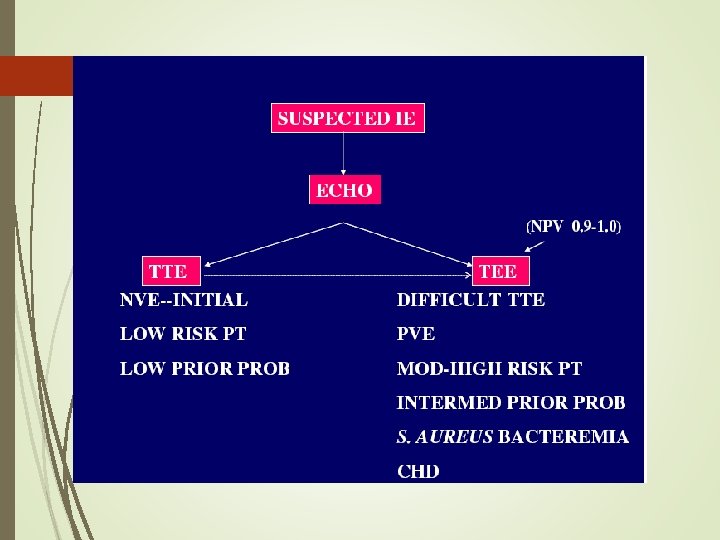
Diagnosis Published criteria for diagnostic purposes in obscure cases High index of suspicion in patients with predisposing anatomy or behavior Blood cultures Echocardiography TTE – 60% sensitivity TEE – 80 – 95% sensitive
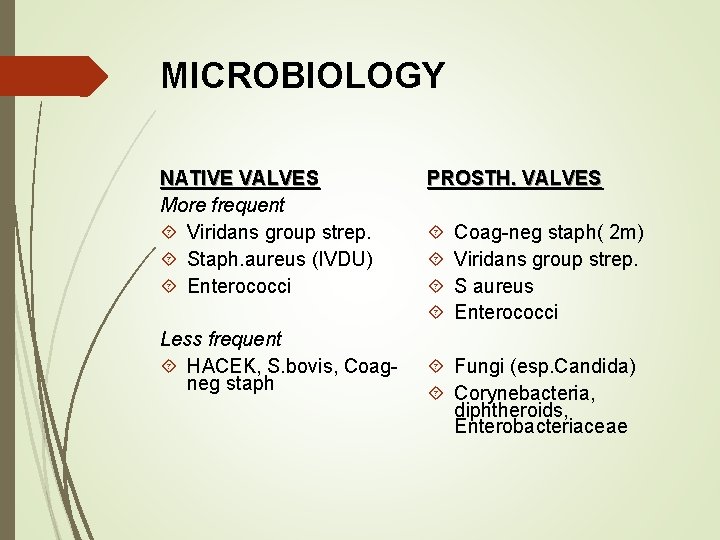
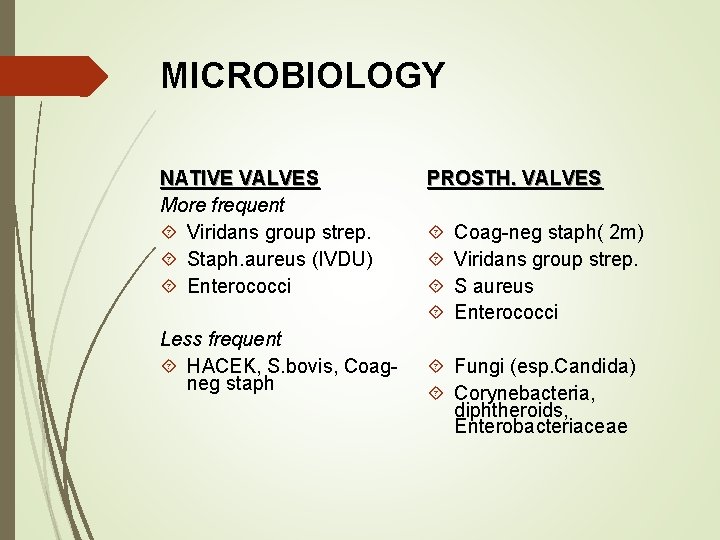
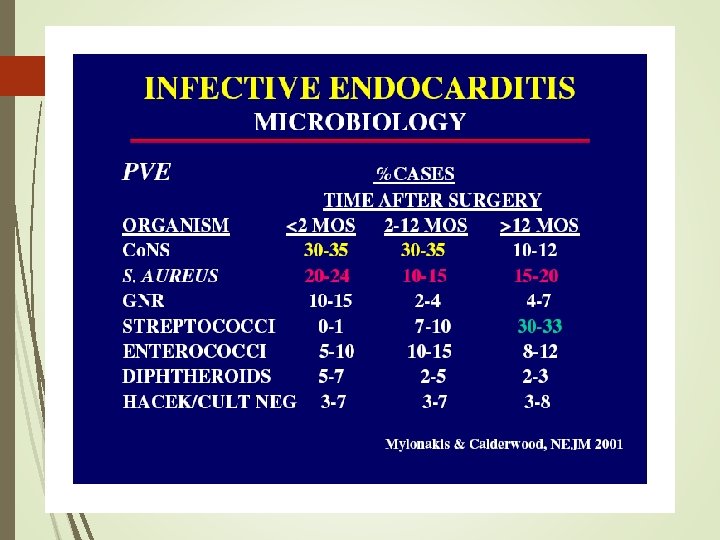
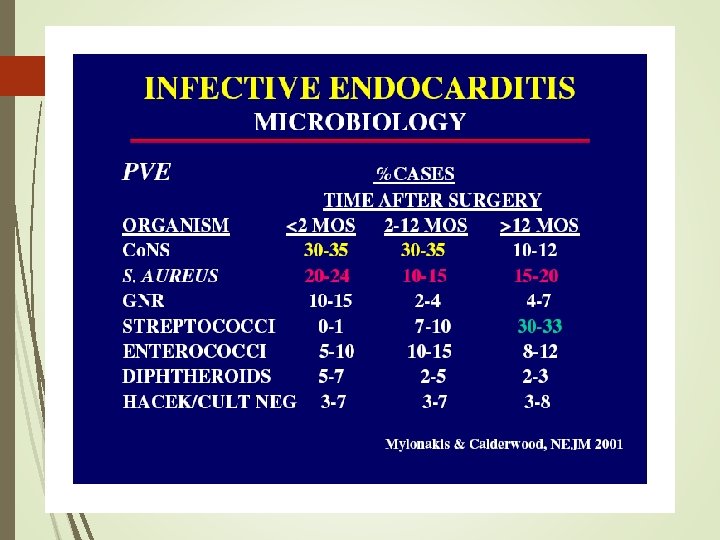
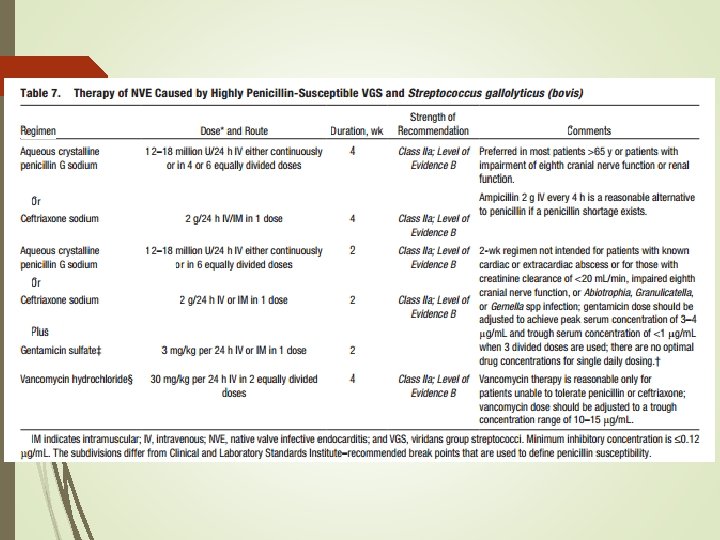
MICROBIOLOGY NATIVE VALVES More frequent Viridans group strep. Staph. aureus (IVDU) Enterococci Less frequent HACEK, S. bovis, Coagneg staph PROSTH. VALVES Coag-neg staph( 2 m) Viridans group strep. S aureus Enterococci Fungi (esp. Candida) Corynebacteria, diphtheroids, Enterobacteriaceae
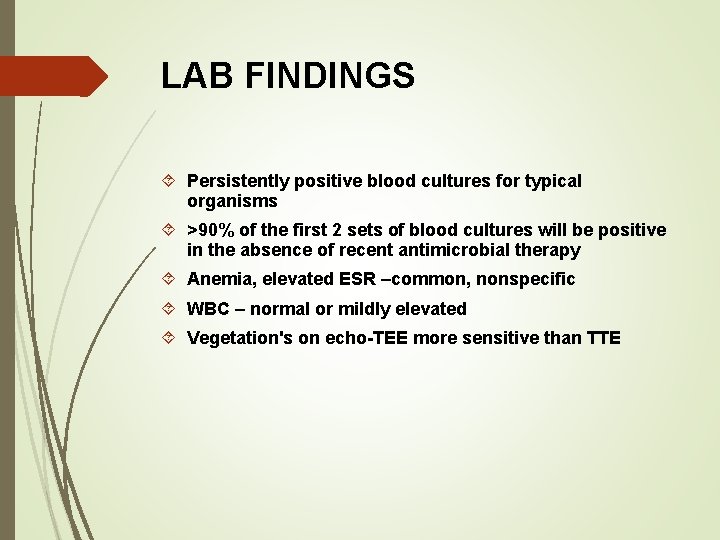
LAB FINDINGS Persistently positive blood cultures for typical organisms >90% of the first 2 sets of blood cultures will be positive in the absence of recent antimicrobial therapy Anemia, elevated ESR –common, nonspecific WBC – normal or mildly elevated Vegetation's on echo-TEE more sensitive than TTE
OTHER LAB FINDINGS Polyclonal hypergammaglobulinemia Hypocomplementemia False positive rheumatoid factor, Lyme serology or syphilis serology – immunologic activation Microhematuria , elevated creatinine & urinary sediment findings suggest glomerulonephritis – deposition of circulating immune complexes
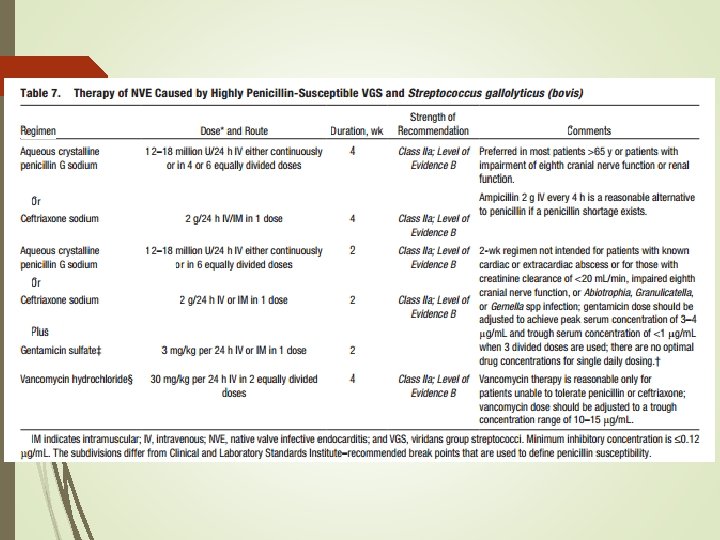
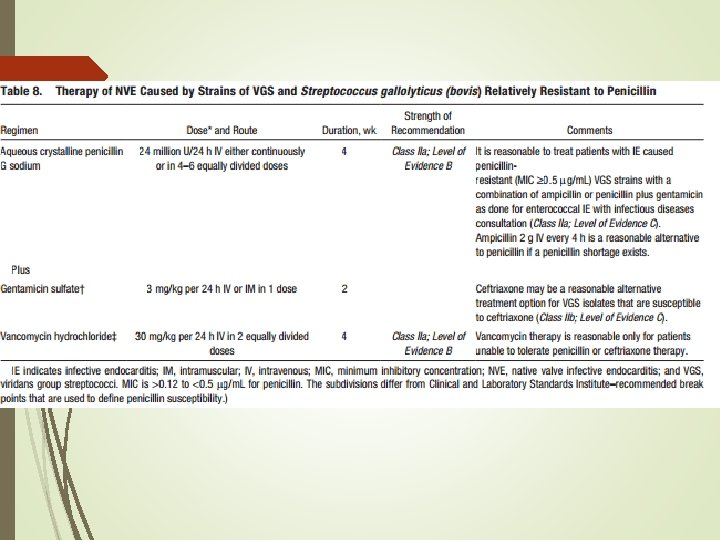
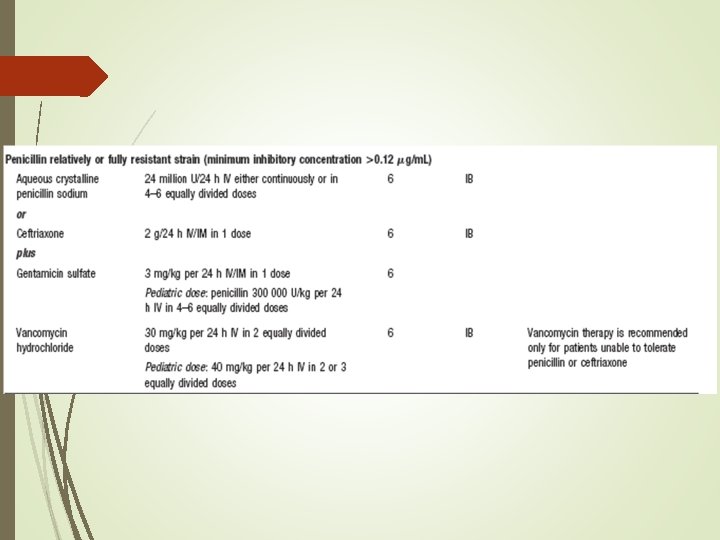
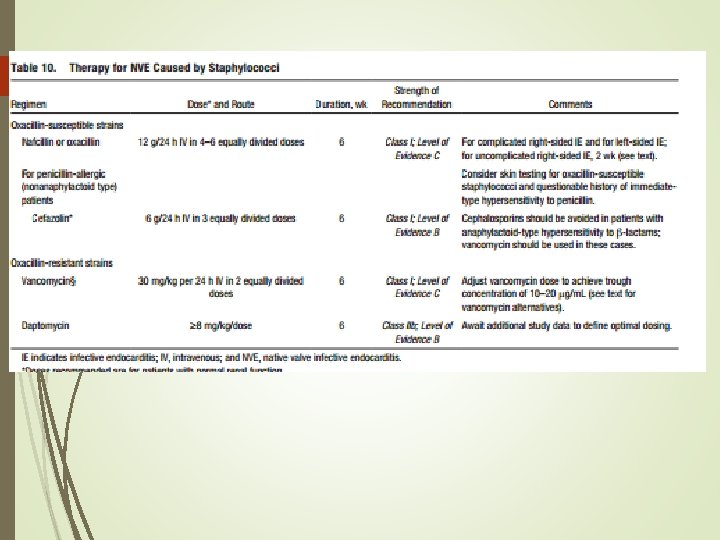
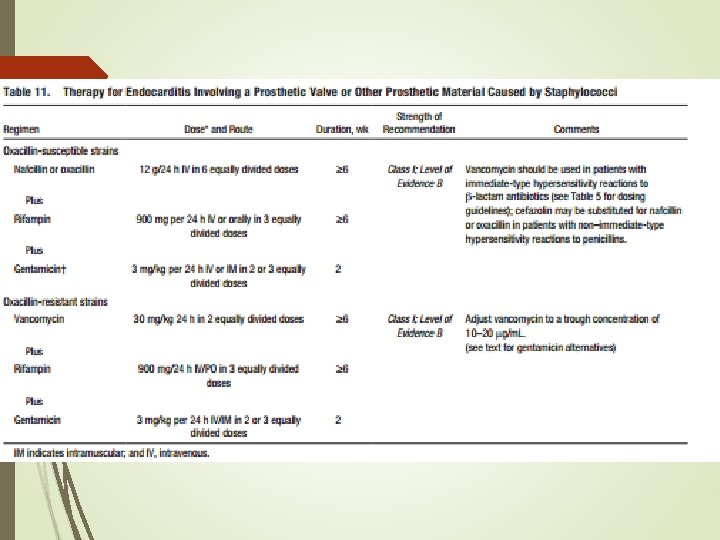
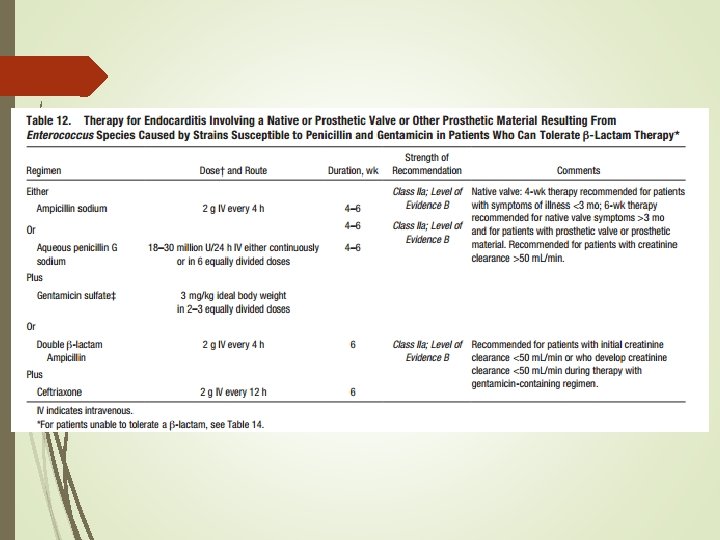
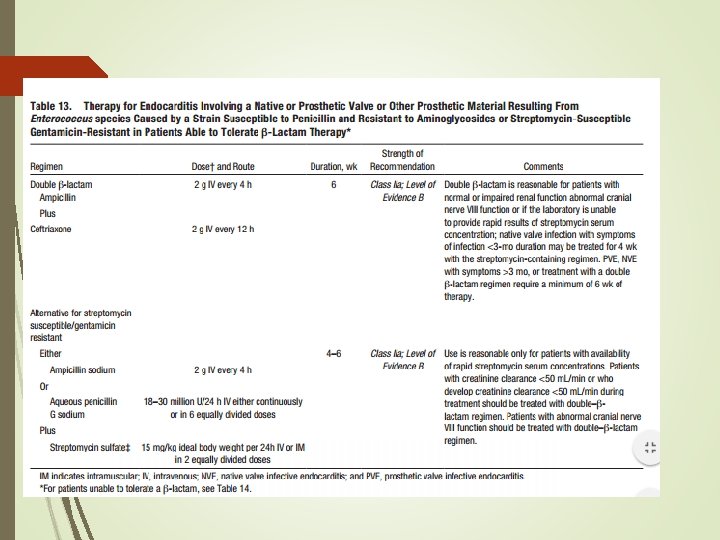
Antimicrobial- Susceptibility Testing Helpful in defining optimal antibiotic dosing, especially streptococcal infection. MIC is needed for dosing considerations Susceptibility of Staph: for oxacillin, vancomycin, rifampin & gentamicin Enterococcal IE - Determine MIC’s of amp & vanc/dapto plus MIC’s of gentamicin & streptomycin for synergy
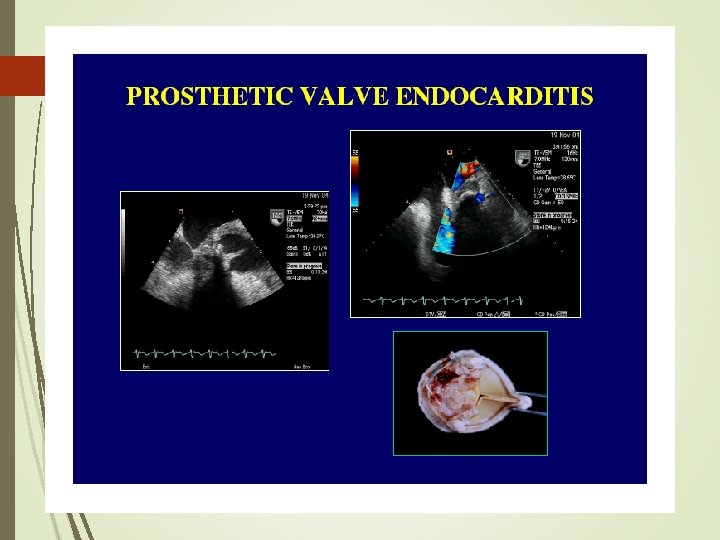
IMAGING Echo demonstrates valvular veg in <60 -95% patients TEE – more sensitive for detection valvular vegetation's or perforations esp in pts with prosthetic valves Myocardial abscesses CXR – right sided IE – multiple migratory pulmonary infiltrates and septic emboli
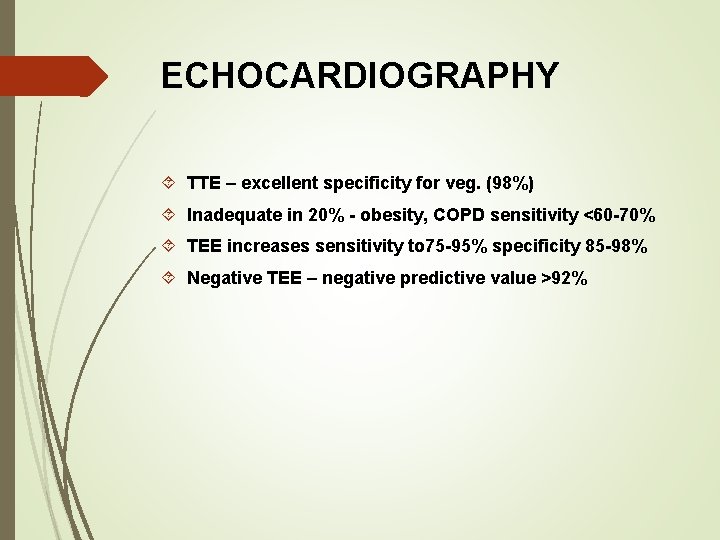
ECHOCARDIOGRAPHY TTE – excellent specificity for veg. (98%) Inadequate in 20% - obesity, COPD sensitivity <60 -70% TEE increases sensitivity to 75 -95% specificity 85 -98% Negative TEE – negative predictive value >92%
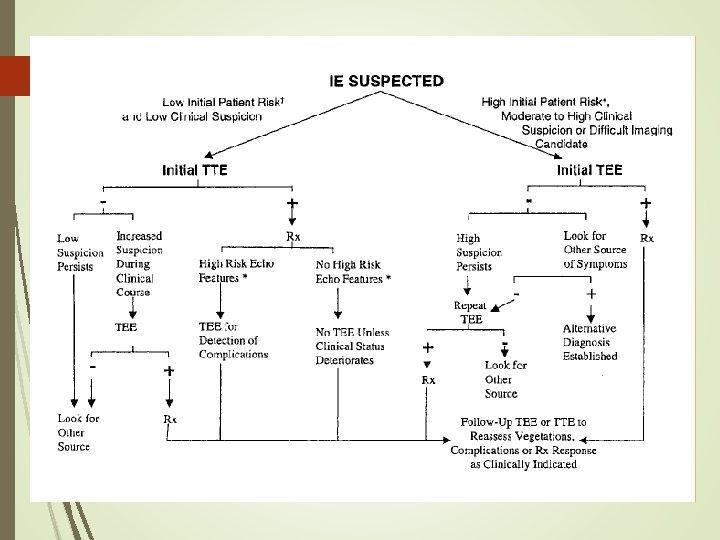
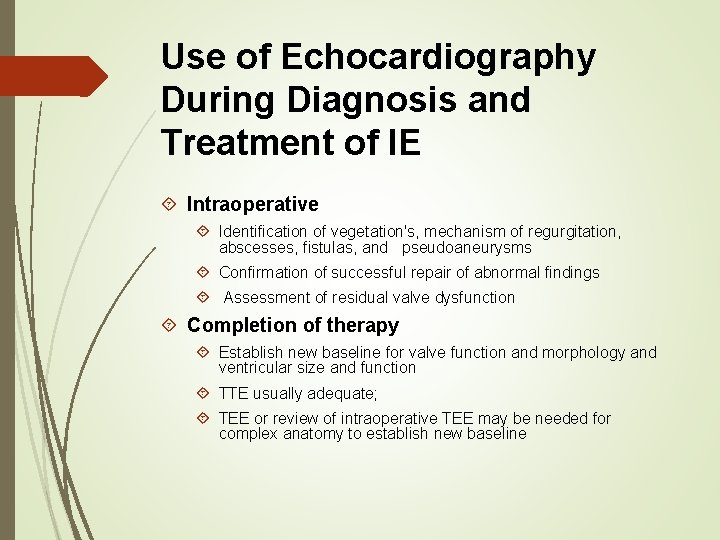
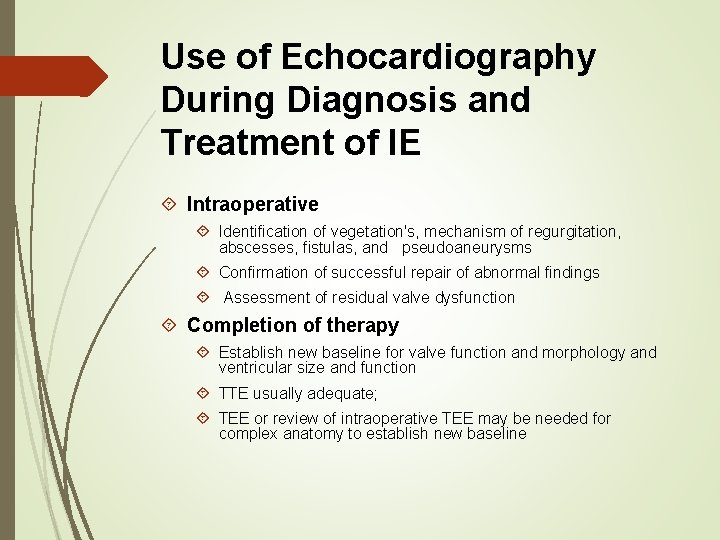
Use of Echocardiography During Diagnosis and Treatment of IE Intraoperative Identification of vegetation's, mechanism of regurgitation, abscesses, fistulas, and pseudoaneurysms Confirmation of successful repair of abnormal findings Assessment of residual valve dysfunction Completion of therapy Establish new baseline for valve function and morphology and ventricular size and function TTE usually adequate; TEE or review of intraoperative TEE may be needed for complex anatomy to establish new baseline
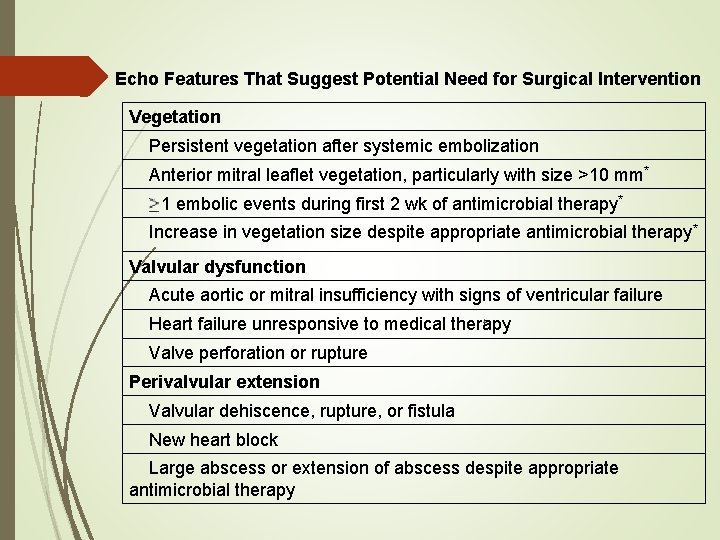
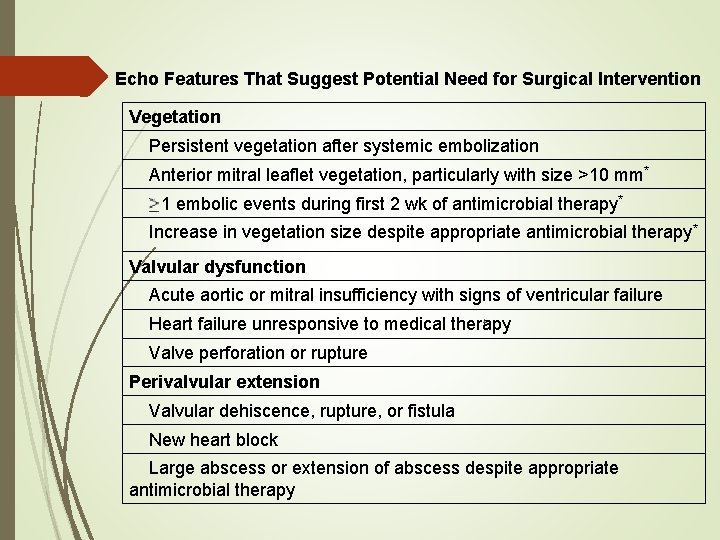
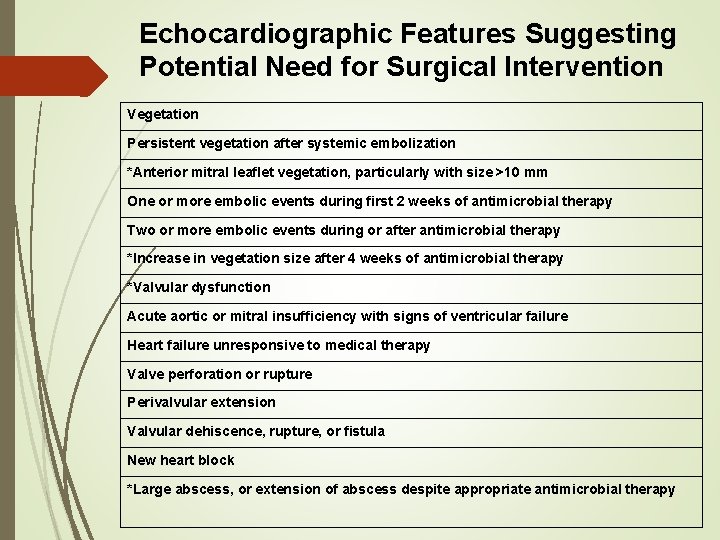
Echo Features That Suggest Potential Need for Surgical Intervention Vegetation Persistent vegetation after systemic embolization Anterior mitral leaflet vegetation, particularly with size >10 mm* 1 embolic events during first 2 wk of antimicrobial therapy* Increase in vegetation size despite appropriate antimicrobial therapy* Valvular dysfunction Acute aortic or mitral insufficiency with signs of ventricular failure Heart failure unresponsive to medical therapy Valve perforation or rupture Perivalvular extension Valvular dehiscence, rupture, or fistula New heart block Large abscess or extension of abscess despite appropriate antimicrobial therapy
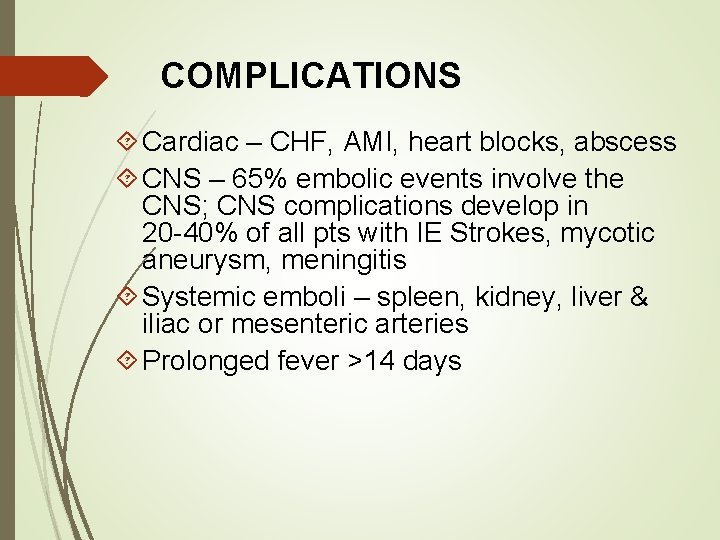
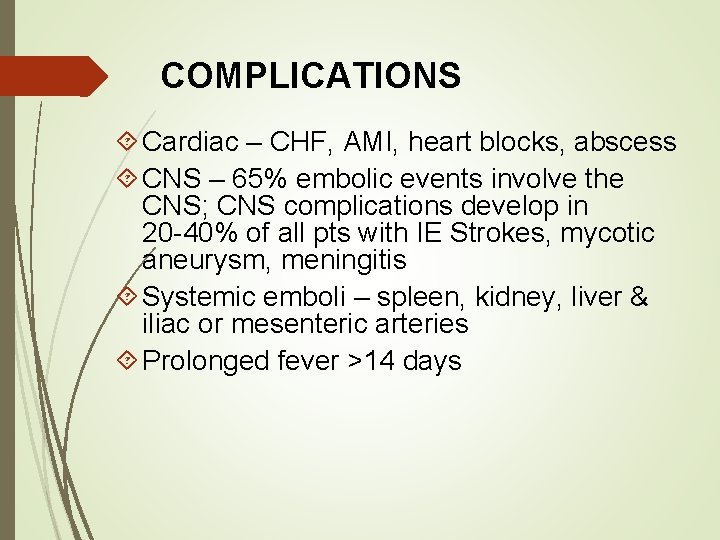
COMPLICATIONS Cardiac – CHF, AMI, heart blocks, abscess CNS – 65% embolic events involve the CNS; CNS complications develop in 20 -40% of all pts with IE Strokes, mycotic aneurysm, meningitis Systemic emboli – spleen, kidney, liver & iliac or mesenteric arteries Prolonged fever >14 days
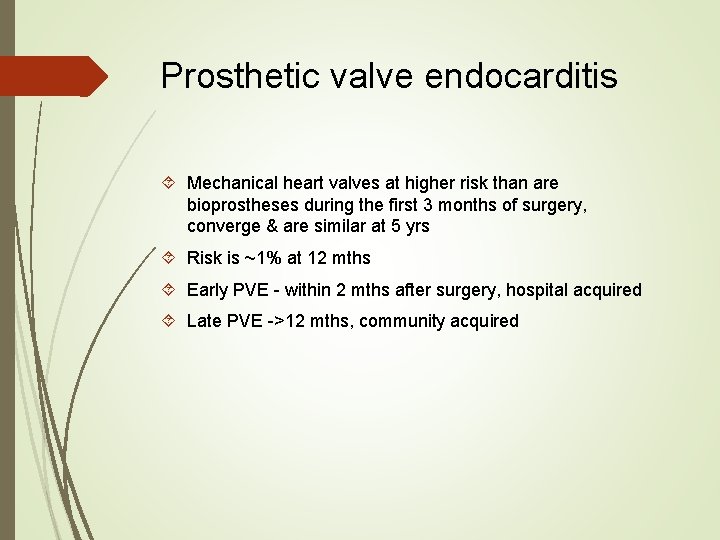
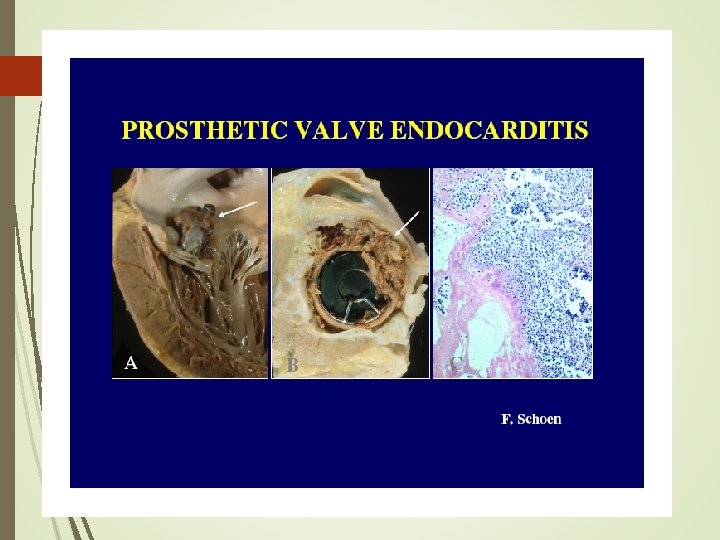
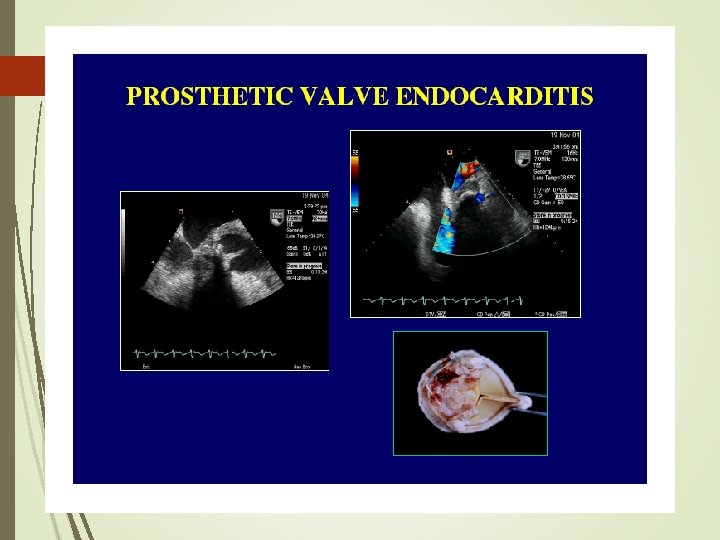
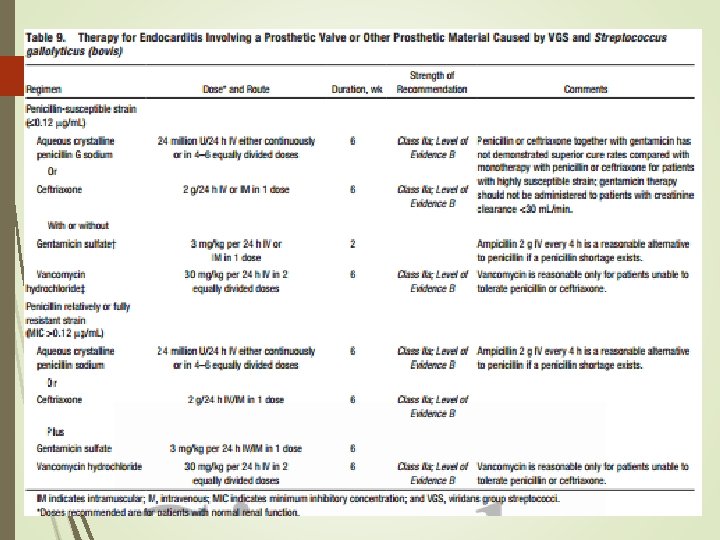
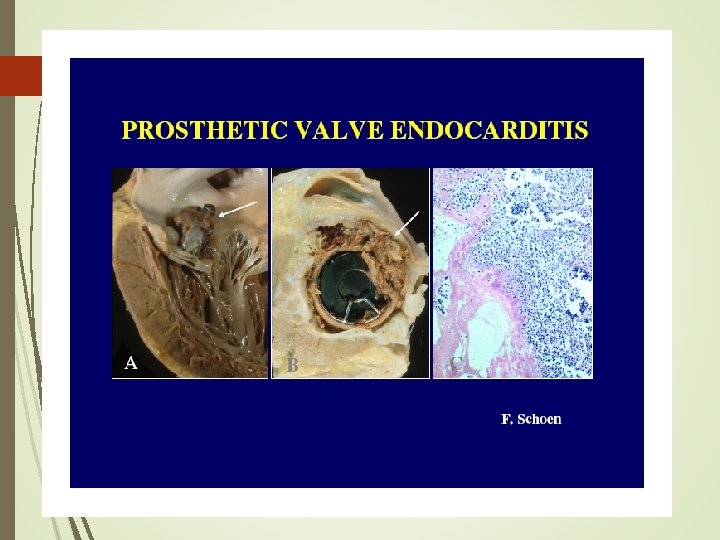
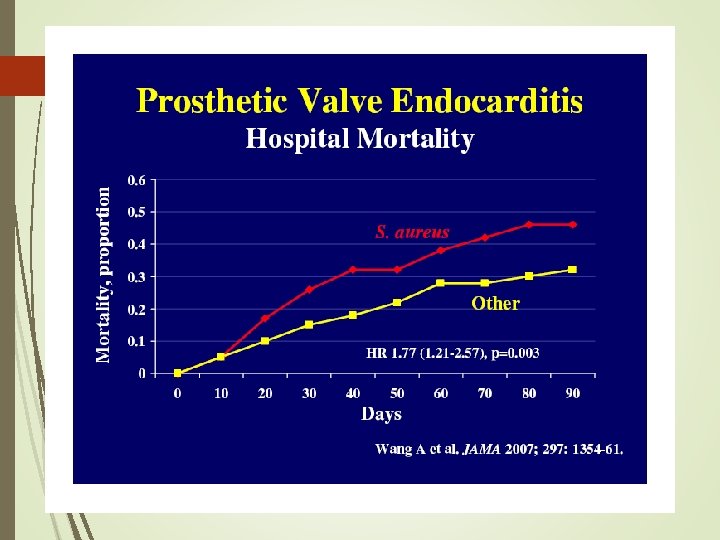
Prosthetic valve endocarditis Mechanical heart valves at higher risk than are bioprostheses during the first 3 months of surgery, converge & are similar at 5 yrs Risk is ~1% at 12 mths Early PVE - within 2 mths after surgery, hospital acquired Late PVE ->12 mths, community acquired
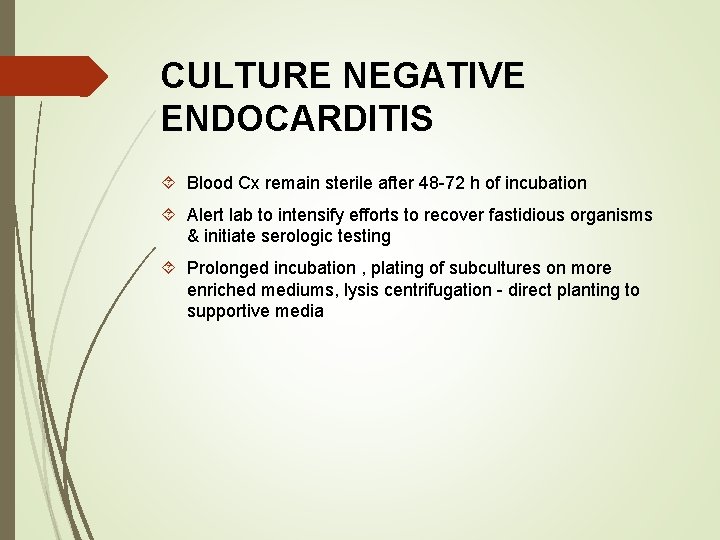
CULTURE NEGATIVE ENDOCARDITIS Blood Cx remain sterile after 48 -72 h of incubation Alert lab to intensify efforts to recover fastidious organisms & initiate serologic testing Prolonged incubation , plating of subcultures on more enriched mediums, lysis centrifugation - direct planting to supportive media
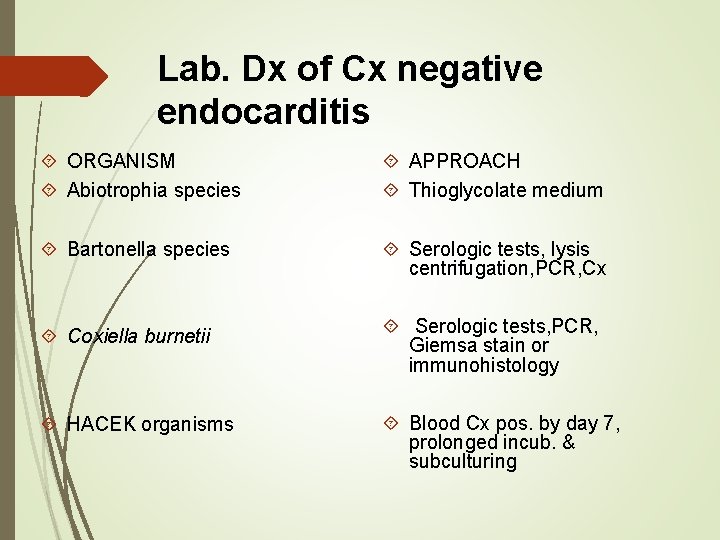
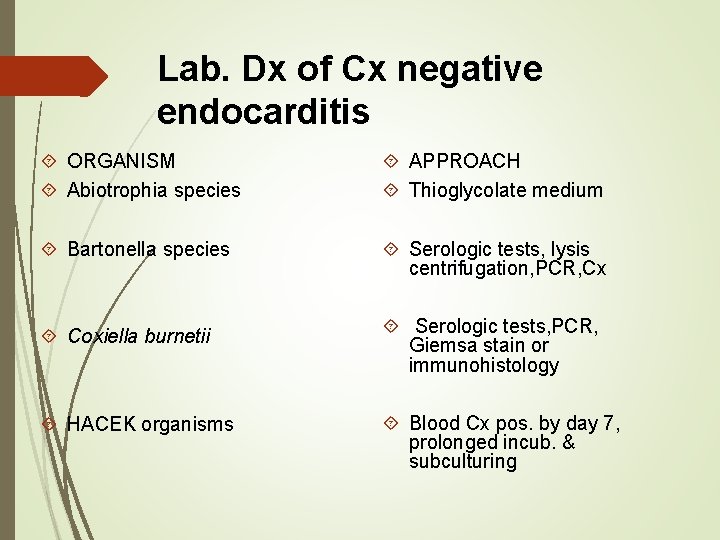
Lab. Dx of Cx negative endocarditis ORGANISM Abiotrophia species APPROACH Thioglycolate medium Bartonella species Serologic tests, lysis centrifugation, PCR, Cx Coxiella burnetii Serologic tests, PCR, Giemsa stain or immunohistology HACEK organisms Blood Cx pos. by day 7, prolonged incub. & subculturing
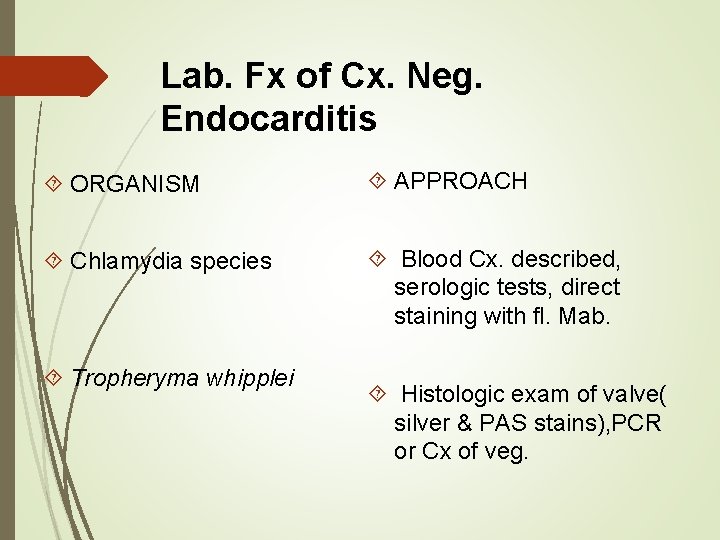
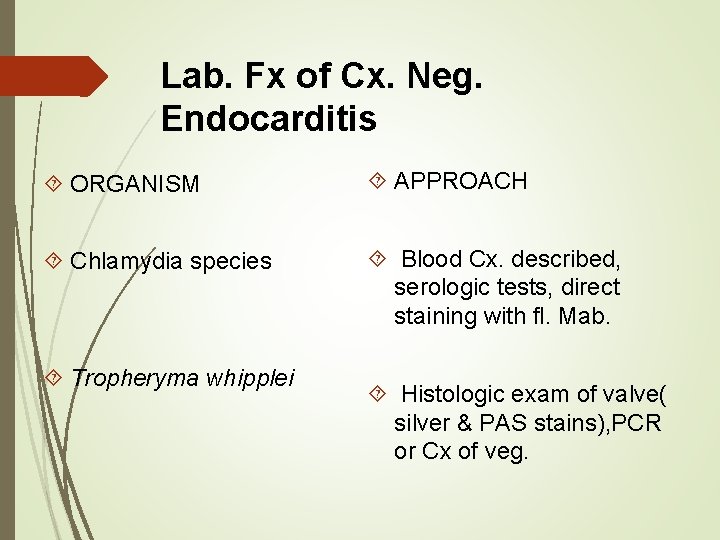
Lab. Fx of Cx. Neg. Endocarditis ORGANISM APPROACH Chlamydia species Blood Cx. described, serologic tests, direct staining with fl. Mab. Tropheryma whipplei Histologic exam of valve( silver & PAS stains), PCR or Cx of veg.
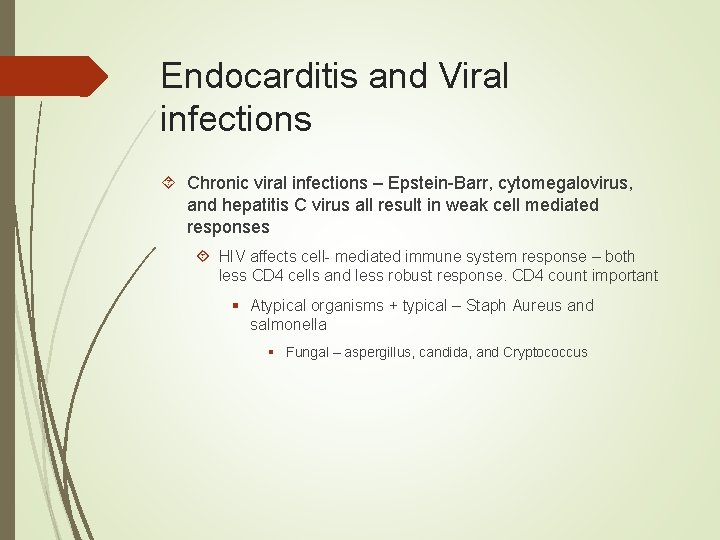
Endocarditis and Viral infections Chronic viral infections – Epstein-Barr, cytomegalovirus, and hepatitis C virus all result in weak cell mediated responses HIV affects cell- mediated immune system response – both less CD 4 cells and less robust response. CD 4 count important § Atypical organisms + typical – Staph Aureus and salmonella § Fungal – aspergillus, candida, and Cryptococcus
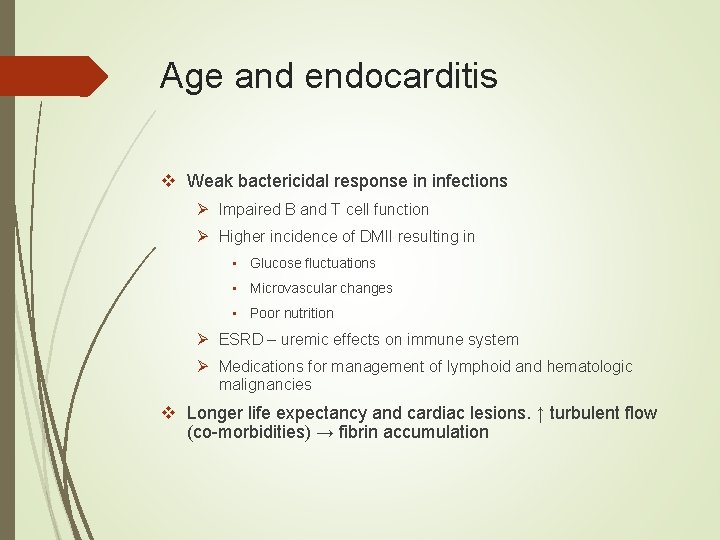
Age and endocarditis v Weak bactericidal response in infections Ø Impaired B and T cell function Ø Higher incidence of DMII resulting in • Glucose fluctuations • Microvascular changes • Poor nutrition Ø ESRD – uremic effects on immune system Ø Medications for management of lymphoid and hematologic malignancies v Longer life expectancy and cardiac lesions. ↑ turbulent flow (co-morbidities) → fibrin accumulation
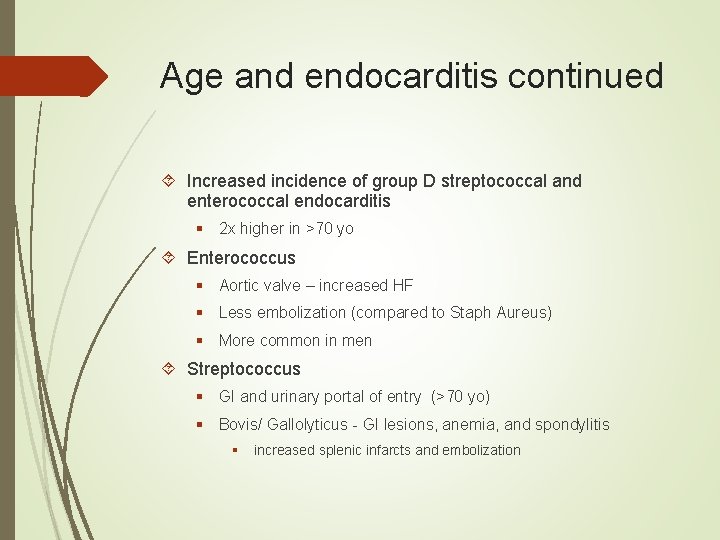
Age and endocarditis continued Increased incidence of group D streptococcal and enterococcal endocarditis § 2 x higher in >70 yo Enterococcus § Aortic valve – increased HF § Less embolization (compared to Staph Aureus) § More common in men Streptococcus § GI and urinary portal of entry (>70 yo) § Bovis/ Gallolyticus - GI lesions, anemia, and spondylitis § increased splenic infarcts and embolization

Fungal endocarditis Candida – most likely C Albicans § Surgery required § Micafungin, liposomal ampho B, addition of flucytosine? § No fluconazole monotherapy, suppression Aspergillus § Again surgery required for cure § Voriconazole, ampho B + flucytosine 2 nd Histoplasmosis § Ampho B induction then itraconazole treatment → suppression Cryptococcus § Ampho B + fluccytosine → fluconazole
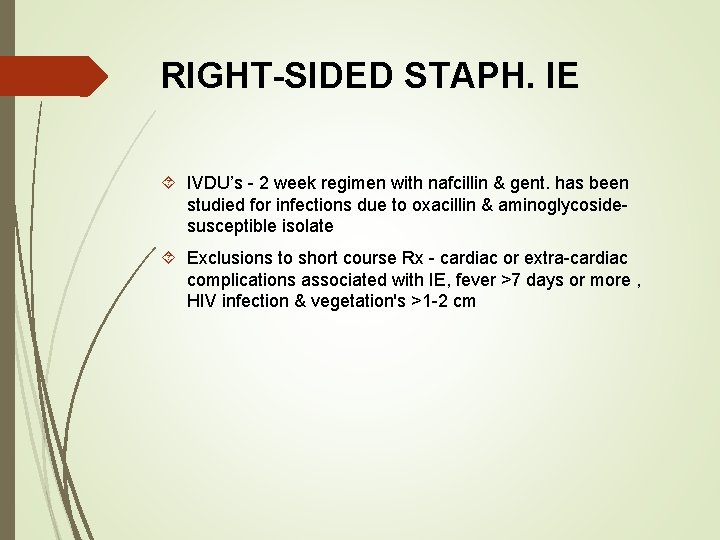
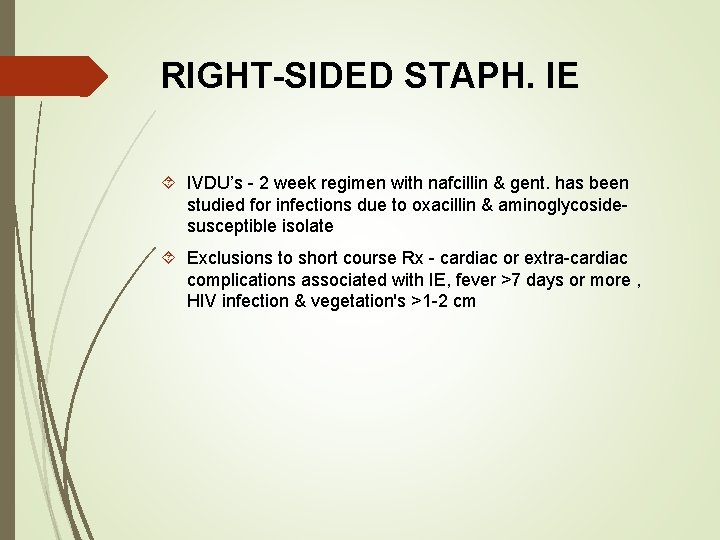
RIGHT-SIDED STAPH. IE IVDU’s - 2 week regimen with nafcillin & gent. has been studied for infections due to oxacillin & aminoglycosidesusceptible isolate Exclusions to short course Rx - cardiac or extra-cardiac complications associated with IE, fever >7 days or more , HIV infection & vegetation's >1 -2 cm
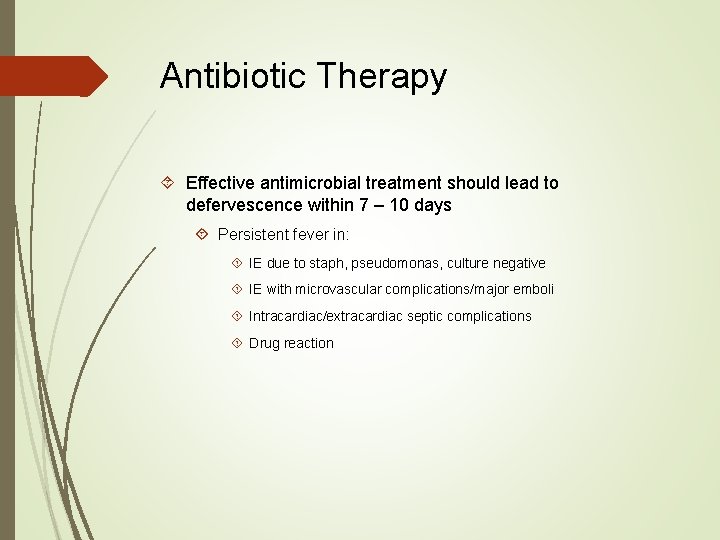
Antibiotic Therapy Effective antimicrobial treatment should lead to defervescence within 7 – 10 days Persistent fever in: IE due to staph, pseudomonas, culture negative IE with microvascular complications/major emboli Intracardiac/extracardiac septic complications Drug reaction
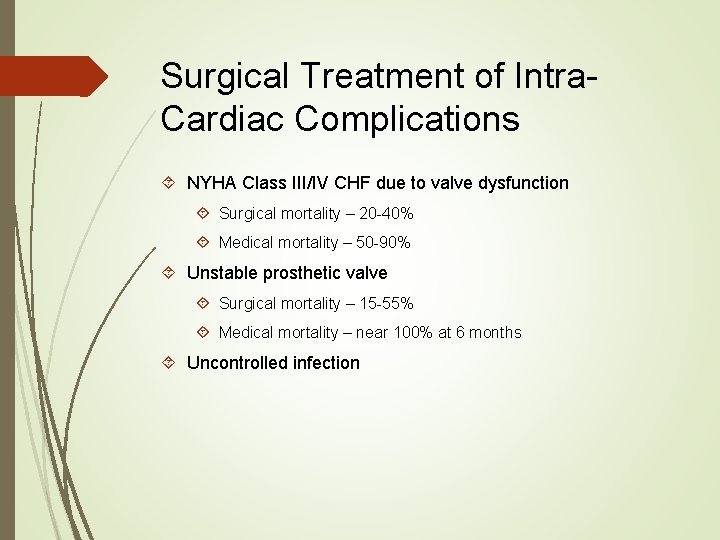
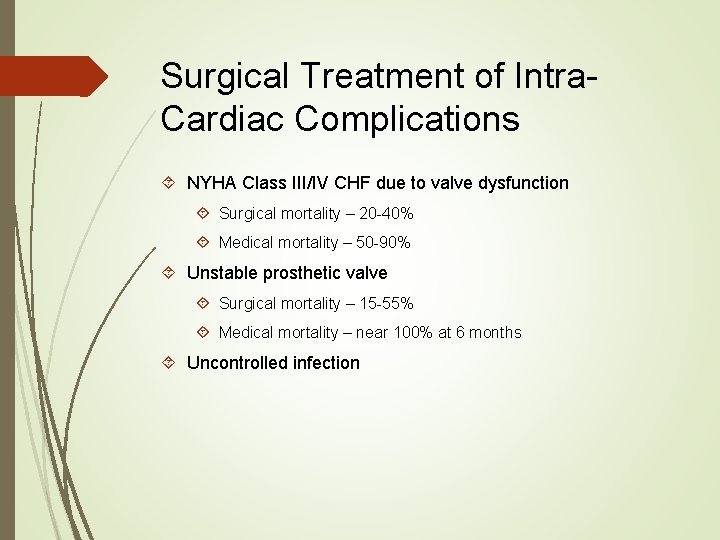
Surgical Treatment of Intra. Cardiac Complications NYHA Class III/IV CHF due to valve dysfunction Surgical mortality – 20 -40% Medical mortality – 50 -90% Unstable prosthetic valve Surgical mortality – 15 -55% Medical mortality – near 100% at 6 months Uncontrolled infection
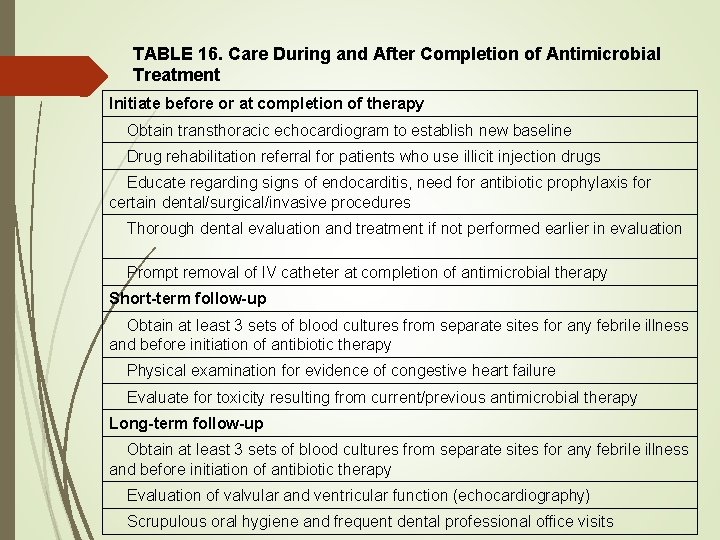
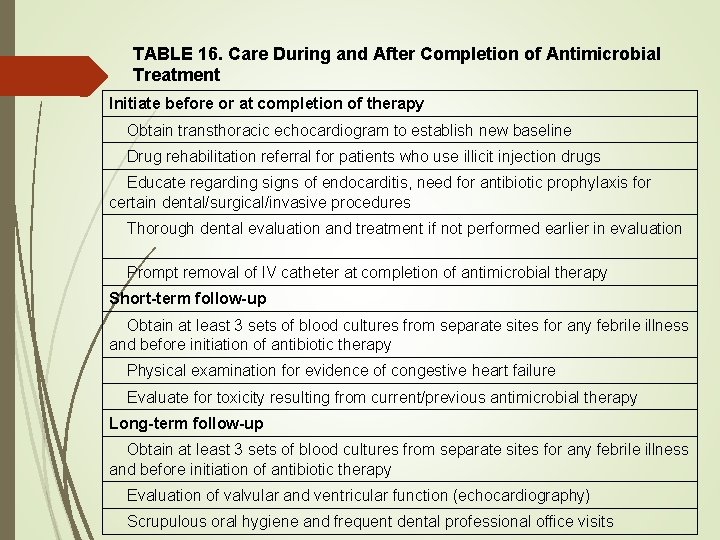
TABLE 16. Care During and After Completion of Antimicrobial Treatment Initiate before or at completion of therapy Obtain transthoracic echocardiogram to establish new baseline Drug rehabilitation referral for patients who use illicit injection drugs Educate regarding signs of endocarditis, need for antibiotic prophylaxis for certain dental/surgical/invasive procedures Thorough dental evaluation and treatment if not performed earlier in evaluation Prompt removal of IV catheter at completion of antimicrobial therapy Short-term follow-up Obtain at least 3 sets of blood cultures from separate sites for any febrile illness and before initiation of antibiotic therapy Physical examination for evidence of congestive heart failure Evaluate for toxicity resulting from current/previous antimicrobial therapy Long-term follow-up Obtain at least 3 sets of blood cultures from separate sites for any febrile illness and before initiation of antibiotic therapy Evaluation of valvular and ventricular function (echocardiography) Scrupulous oral hygiene and frequent dental professional office visits
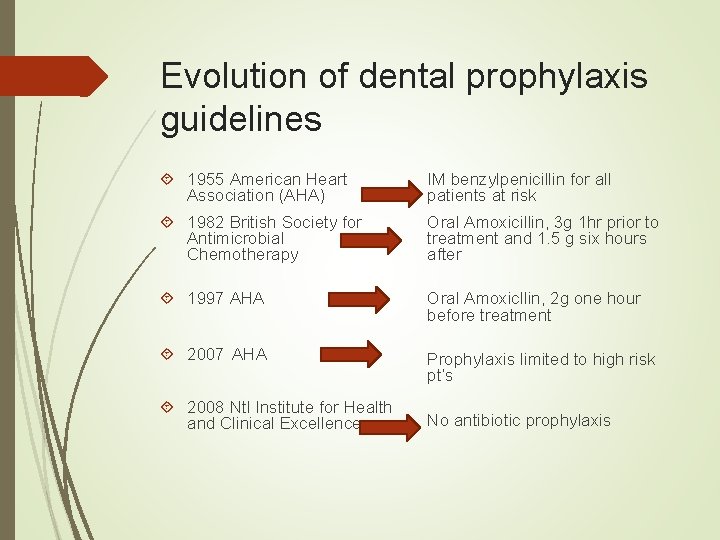
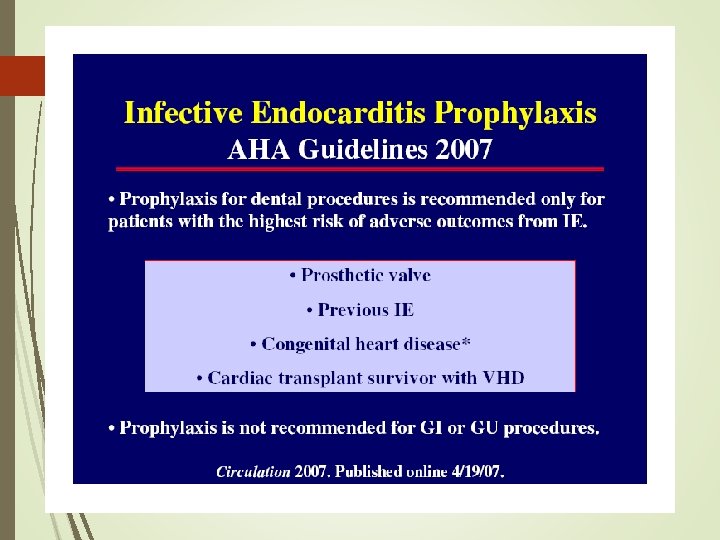
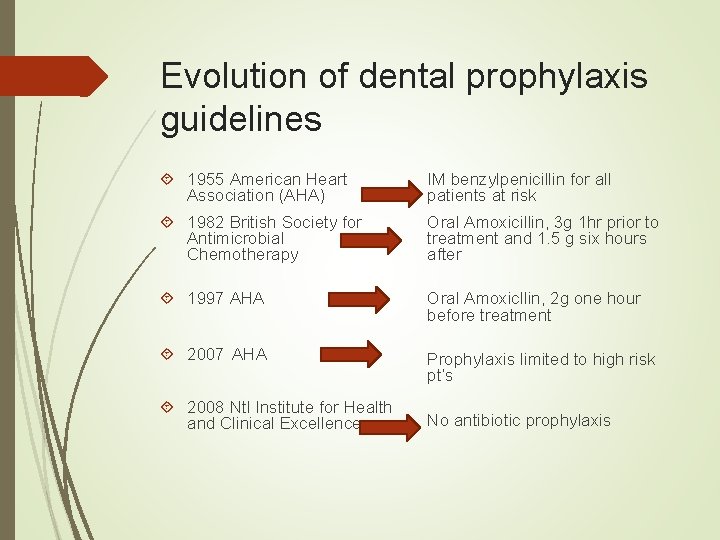
Evolution of dental prophylaxis guidelines 1955 American Heart Association (AHA) IM benzylpenicillin for all patients at risk 1982 British Society for Antimicrobial Chemotherapy Oral Amoxicillin, 3 g 1 hr prior to treatment and 1. 5 g six hours after 1997 AHA Oral Amoxicllin, 2 g one hour before treatment 2007 AHA Prophylaxis limited to high risk pt’s 2008 Ntl Institute for Health and Clinical Excellence No antibiotic prophylaxis
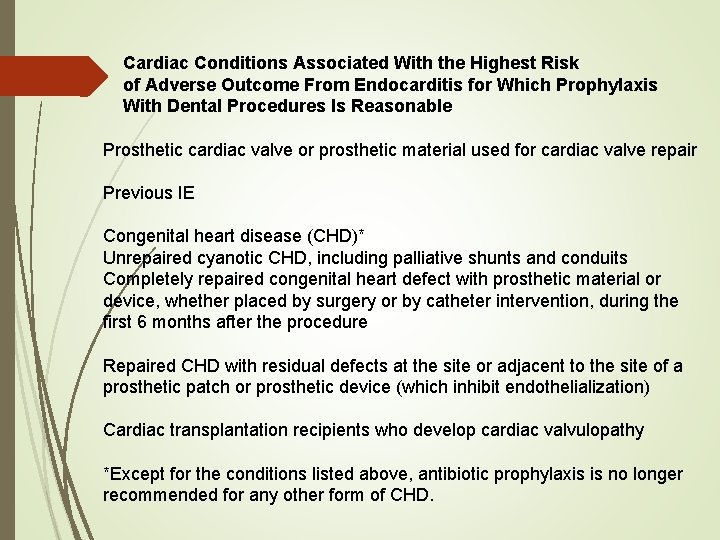
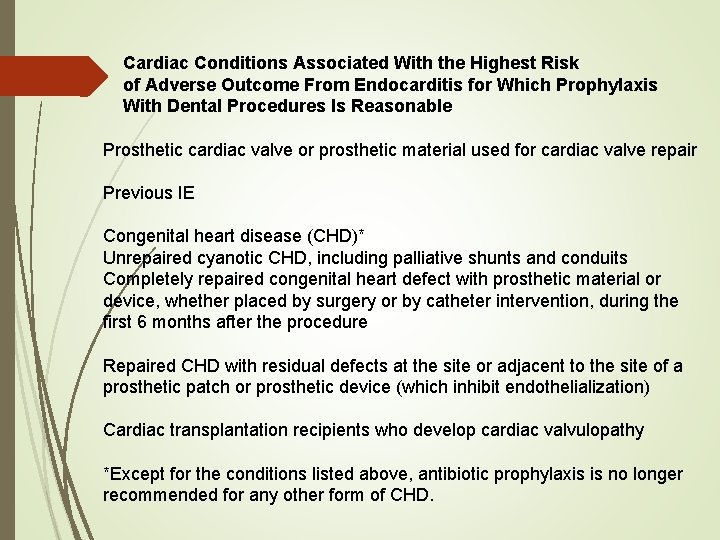
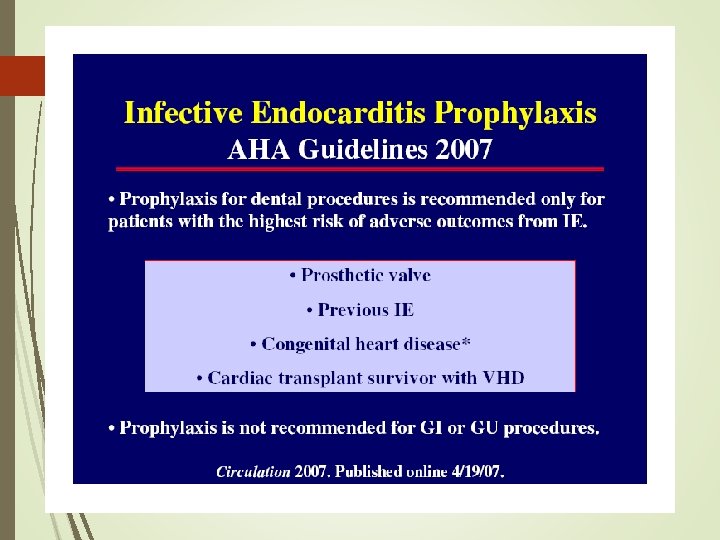
Cardiac Conditions Associated With the Highest Risk of Adverse Outcome From Endocarditis for Which Prophylaxis With Dental Procedures Is Reasonable Prosthetic cardiac valve or prosthetic material used for cardiac valve repair Previous IE Congenital heart disease (CHD)* Unrepaired cyanotic CHD, including palliative shunts and conduits Completely repaired congenital heart defect with prosthetic material or device, whether placed by surgery or by catheter intervention, during the first 6 months after the procedure Repaired CHD with residual defects at the site or adjacent to the site of a prosthetic patch or prosthetic device (which inhibit endothelialization) Cardiac transplantation recipients who develop cardiac valvulopathy *Except for the conditions listed above, antibiotic prophylaxis is no longer recommended for any other form of CHD.
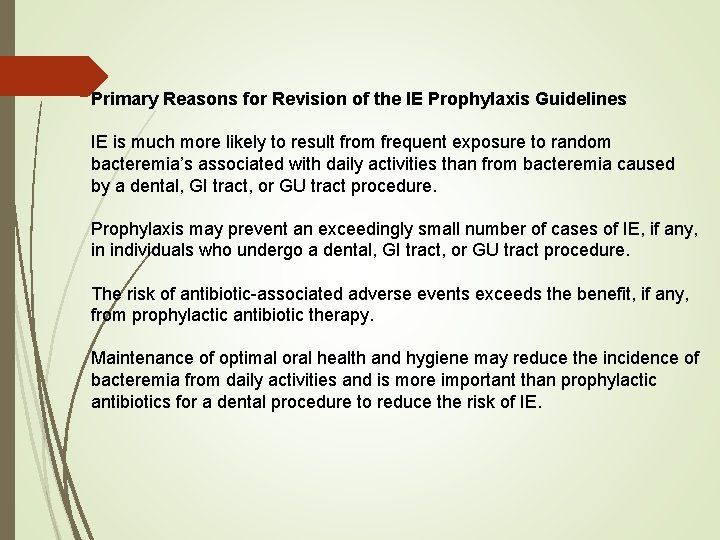
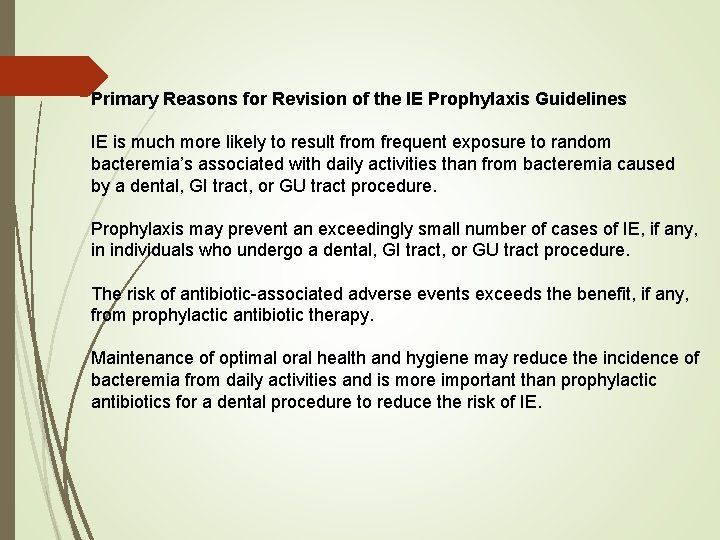
Primary Reasons for Revision of the IE Prophylaxis Guidelines IE is much more likely to result from frequent exposure to random bacteremia’s associated with daily activities than from bacteremia caused by a dental, GI tract, or GU tract procedure. Prophylaxis may prevent an exceedingly small number of cases of IE, if any, in individuals who undergo a dental, GI tract, or GU tract procedure. The risk of antibiotic-associated adverse events exceeds the benefit, if any, from prophylactic antibiotic therapy. Maintenance of optimal oral health and hygiene may reduce the incidence of bacteremia from daily activities and is more important than prophylactic antibiotics for a dental procedure to reduce the risk of IE.
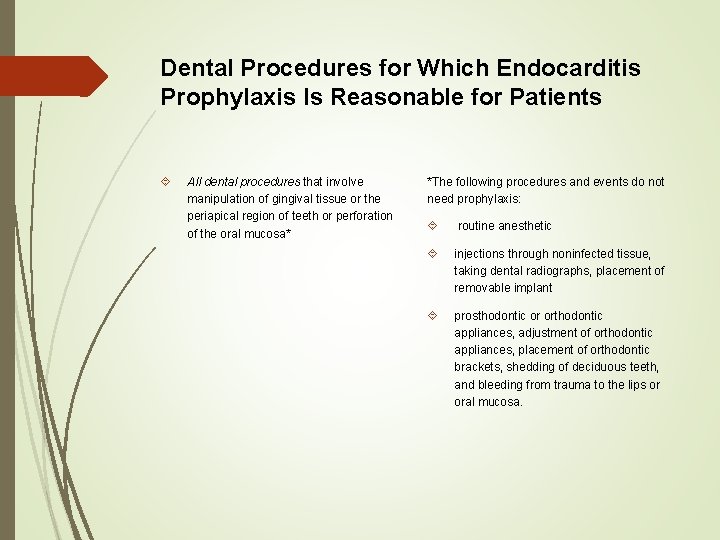
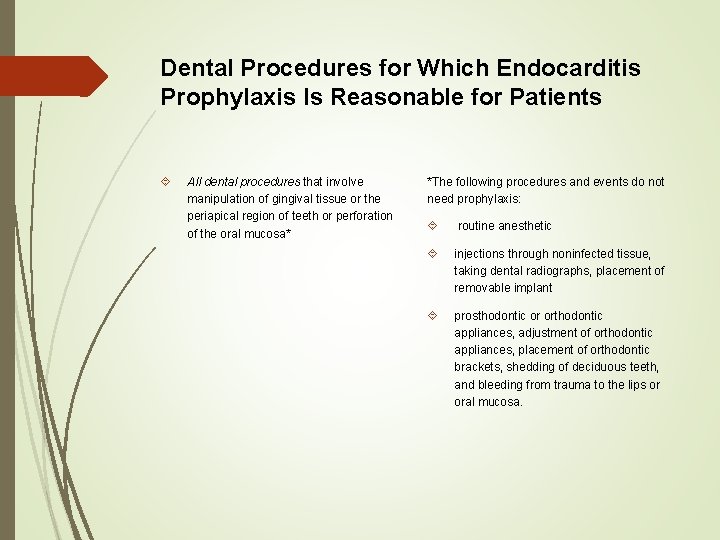
Dental Procedures for Which Endocarditis Prophylaxis Is Reasonable for Patients All dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa* *The following procedures and events do not need prophylaxis: routine anesthetic injections through noninfected tissue, taking dental radiographs, placement of removable implant prosthodontic or orthodontic appliances, adjustment of orthodontic appliances, placement of orthodontic brackets, shedding of deciduous teeth, and bleeding from trauma to the lips or oral mucosa.
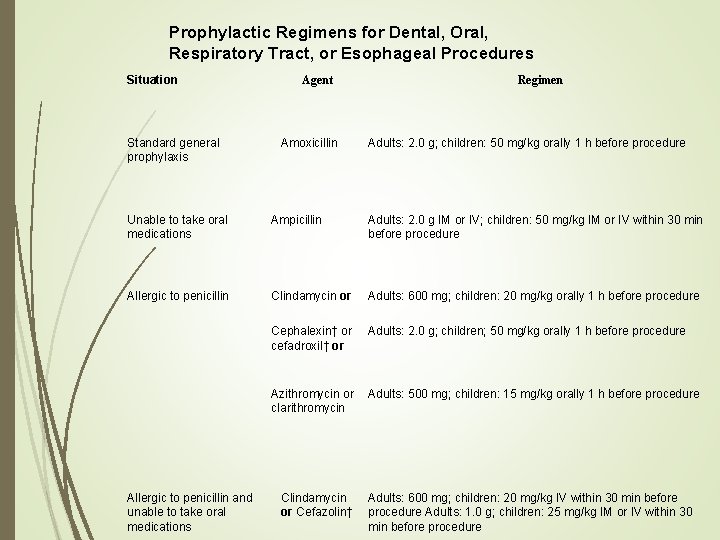
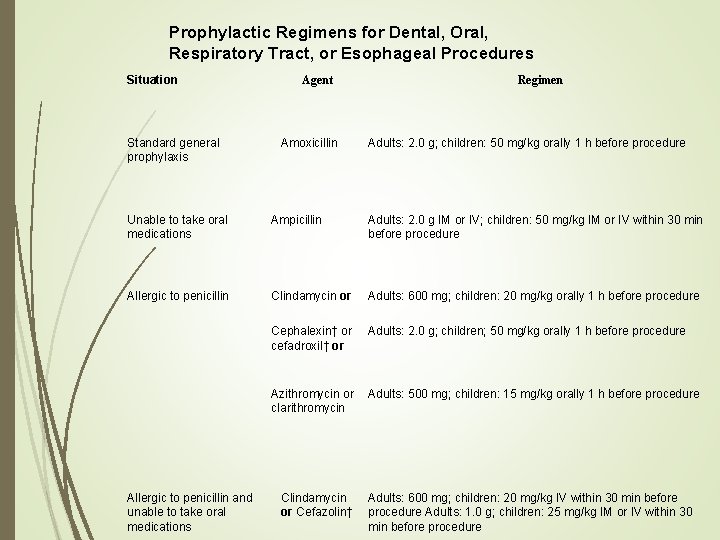
Prophylactic Regimens for Dental, Oral, Respiratory Tract, or Esophageal Procedures Situation Standard general prophylaxis Agent Amoxicillin Regimen Adults: 2. 0 g; children: 50 mg/kg orally 1 h before procedure Unable to take oral medications Ampicillin Adults: 2. 0 g IM or IV; children: 50 mg/kg IM or IV within 30 min before procedure Allergic to penicillin Clindamycin or Adults: 600 mg; children: 20 mg/kg orally 1 h before procedure Cephalexin† or cefadroxil† or Adults: 2. 0 g; children; 50 mg/kg orally 1 h before procedure Azithromycin or clarithromycin Adults: 500 mg; children: 15 mg/kg orally 1 h before procedure Allergic to penicillin and unable to take oral medications Clindamycin or Cefazolin† Adults: 600 mg; children: 20 mg/kg IV within 30 min before procedure Adults: 1. 0 g; children: 25 mg/kg IM or IV within 30 min before procedure
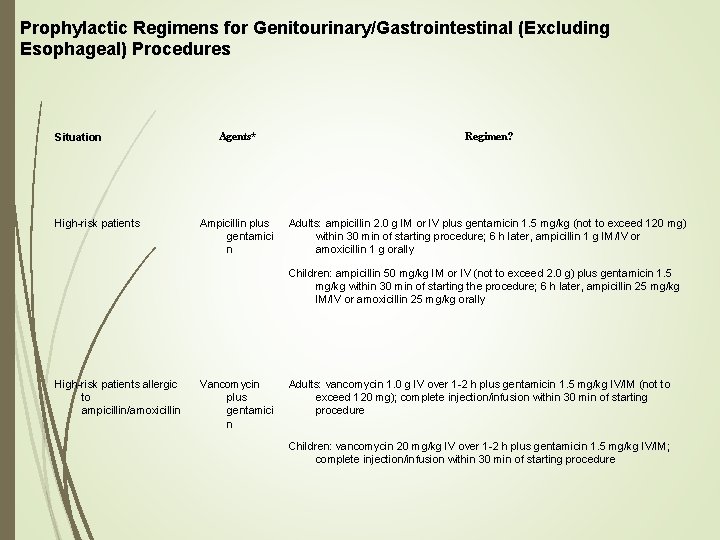
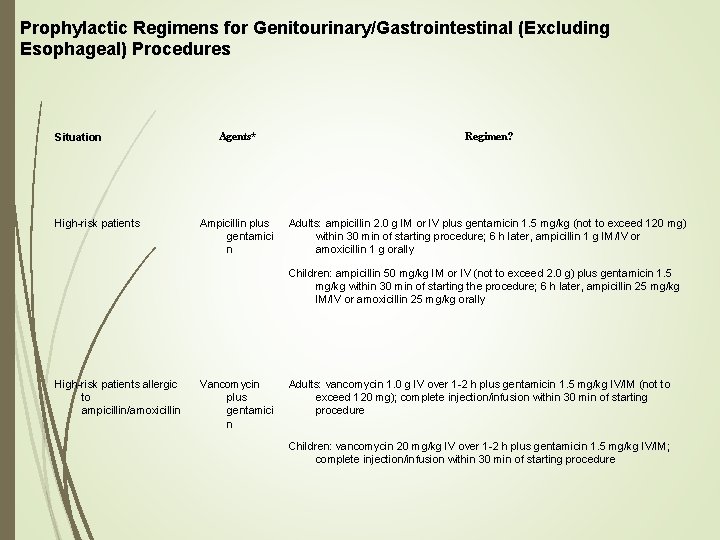
Prophylactic Regimens for Genitourinary/Gastrointestinal (Excluding Esophageal) Procedures Situation High-risk patients Agents* Regimen? Ampicillin plus gentamici n Adults: ampicillin 2. 0 g IM or IV plus gentamicin 1. 5 mg/kg (not to exceed 120 mg) within 30 min of starting procedure; 6 h later, ampicillin 1 g IM/IV or amoxicillin 1 g orally Children: ampicillin 50 mg/kg IM or IV (not to exceed 2. 0 g) plus gentamicin 1. 5 mg/kg within 30 min of starting the procedure; 6 h later, ampicillin 25 mg/kg IM/IV or amoxicillin 25 mg/kg orally High-risk patients allergic to ampicillin/amoxicillin Vancomycin plus gentamici n Adults: vancomycin 1. 0 g IV over 1 -2 h plus gentamicin 1. 5 mg/kg IV/IM (not to exceed 120 mg); complete injection/infusion within 30 min of starting procedure Children: vancomycin 20 mg/kg IV over 1 -2 h plus gentamicin 1. 5 mg/kg IV/IM; complete injection/infusion within 30 min of starting procedure
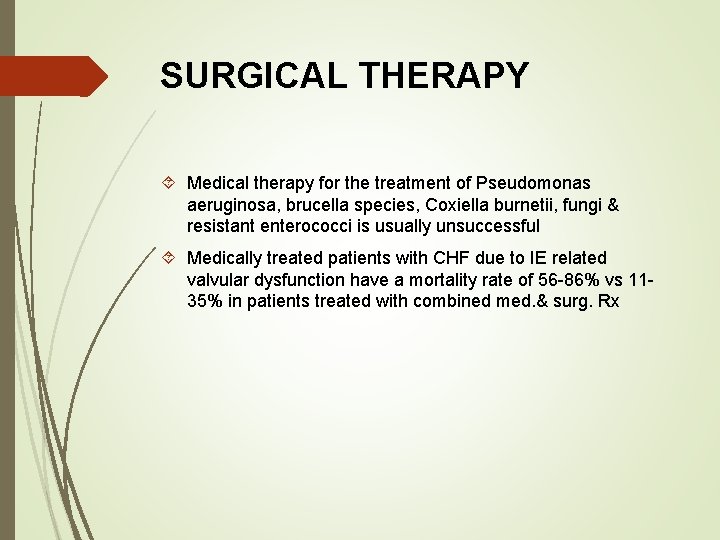
SURGICAL THERAPY Medical therapy for the treatment of Pseudomonas aeruginosa, brucella species, Coxiella burnetii, fungi & resistant enterococci is usually unsuccessful Medically treated patients with CHF due to IE related valvular dysfunction have a mortality rate of 56 -86% vs 1135% in patients treated with combined med. & surg. Rx
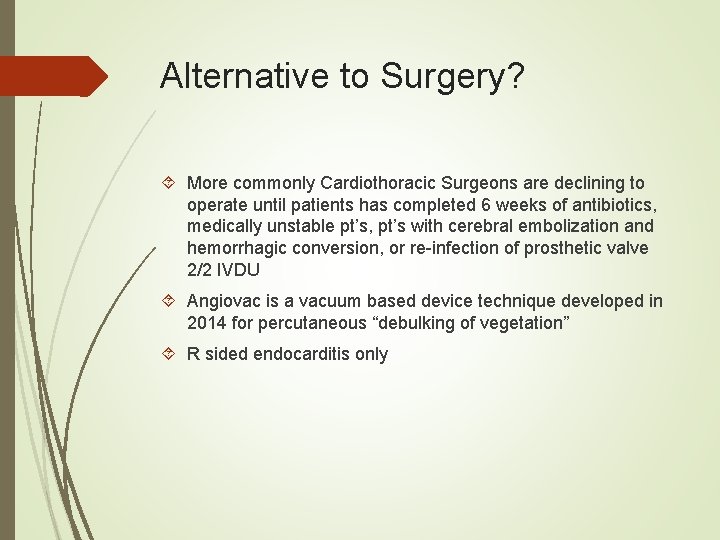
Alternative to Surgery? More commonly Cardiothoracic Surgeons are declining to operate until patients has completed 6 weeks of antibiotics, medically unstable pt’s, pt’s with cerebral embolization and hemorrhagic conversion, or re-infection of prosthetic valve 2/2 IVDU Angiovac is a vacuum based device technique developed in 2014 for percutaneous “debulking of vegetation” R sided endocarditis only
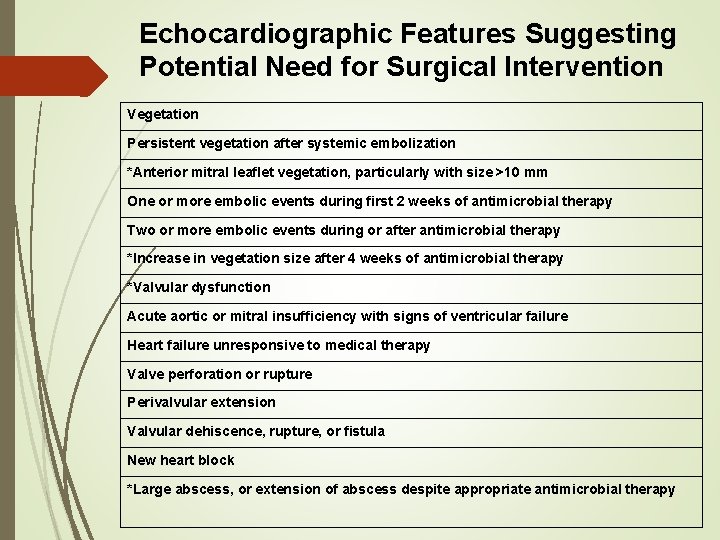
Echocardiographic Features Suggesting Potential Need for Surgical Intervention Vegetation Persistent vegetation after systemic embolization *Anterior mitral leaflet vegetation, particularly with size >10 mm One or more embolic events during first 2 weeks of antimicrobial therapy Two or more embolic events during or after antimicrobial therapy *Increase in vegetation size after 4 weeks of antimicrobial therapy *Valvular dysfunction Acute aortic or mitral insufficiency with signs of ventricular failure Heart failure unresponsive to medical therapy Valve perforation or rupture Perivalvular extension Valvular dehiscence, rupture, or fistula New heart block *Large abscess, or extension of abscess despite appropriate antimicrobial therapy
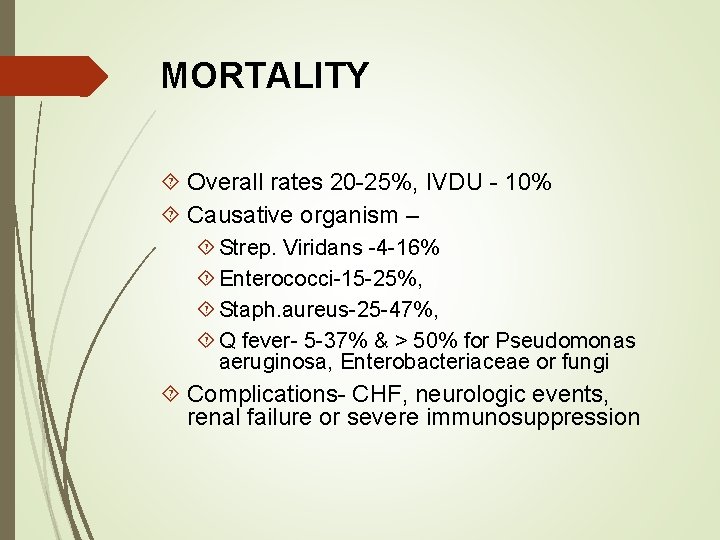
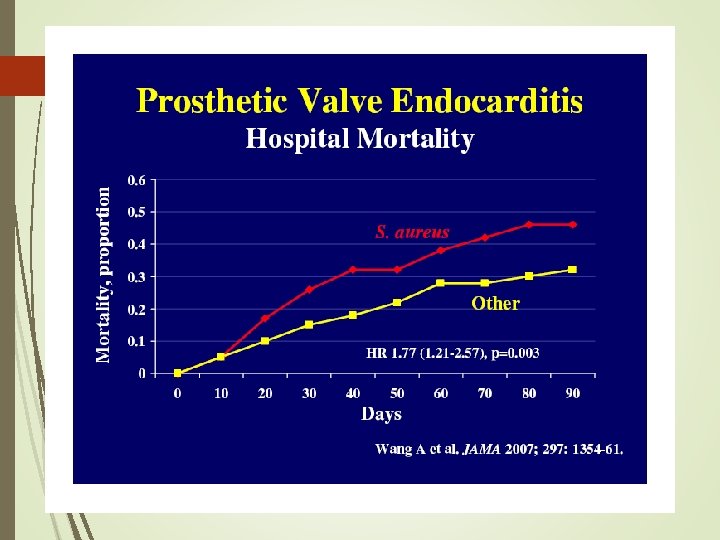
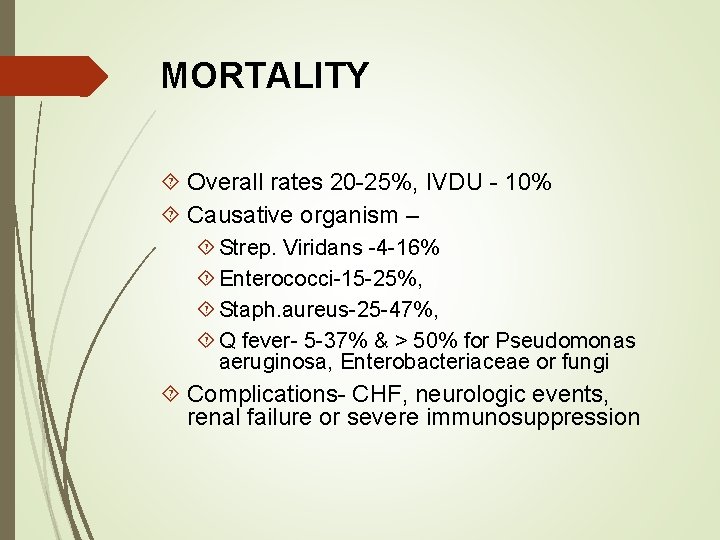
MORTALITY Overall rates 20 -25%, IVDU - 10% Causative organism – Strep. Viridans -4 -16% Enterococci-15 -25%, Staph. aureus-25 -47%, Q fever- 5 -37% & > 50% for Pseudomonas aeruginosa, Enterobacteriaceae or fungi Complications- CHF, neurologic events, renal failure or severe immunosuppression

RELAPSE Occurs within 2 months of discontinuation of antimicrobial Rx <2% for native valve IE due to pcn-susc. viridans strep 8 -20% with enterococcal IE 10 -15 % with PVE
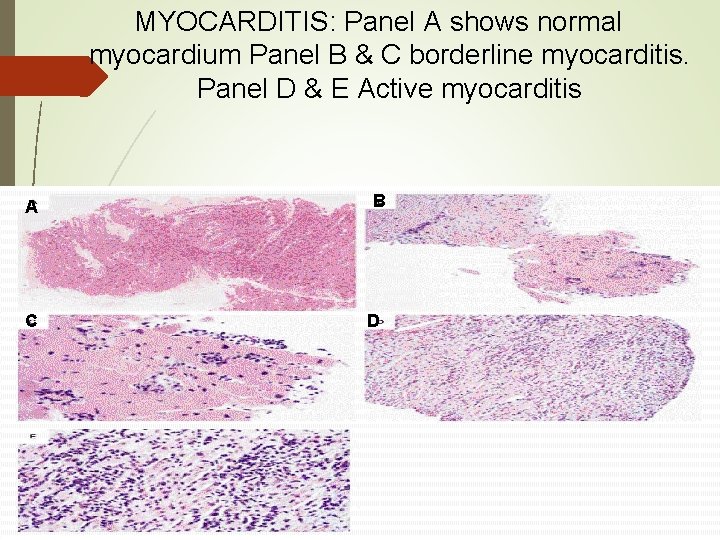
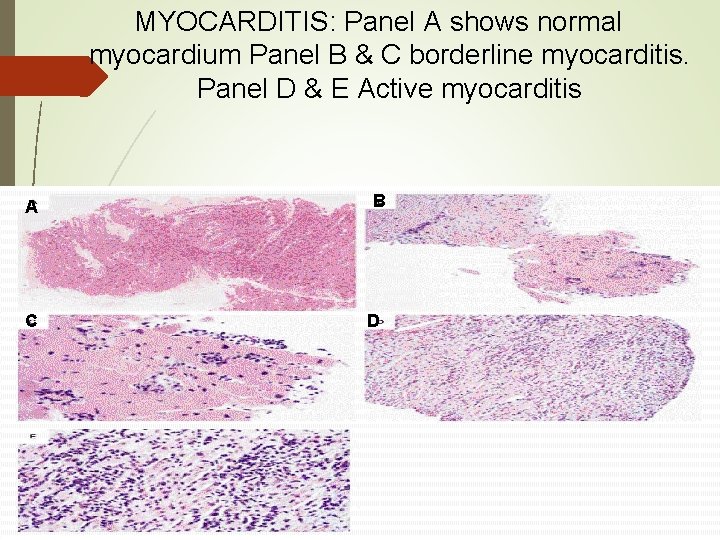
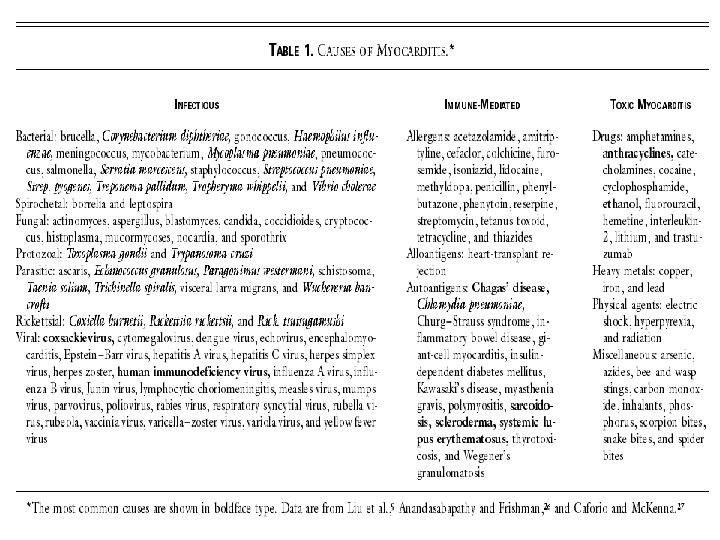
MYOCARDITIS: Panel A shows normal myocardium Panel B & C borderline myocarditis. Panel D & E Active myocarditis A C B D
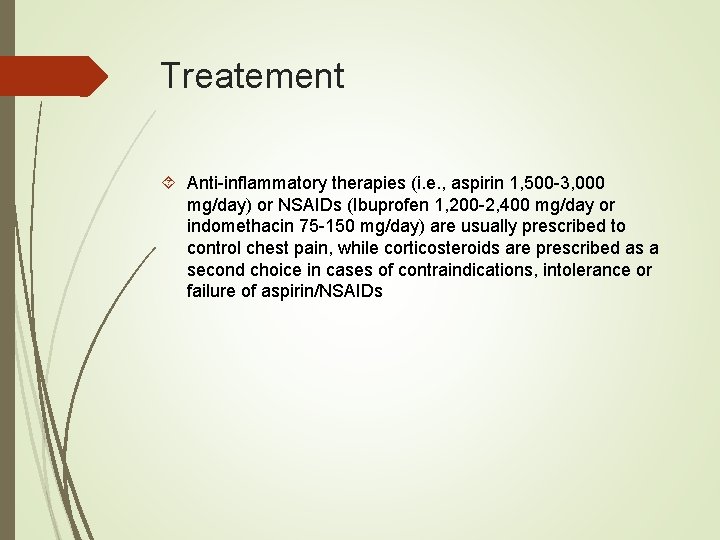
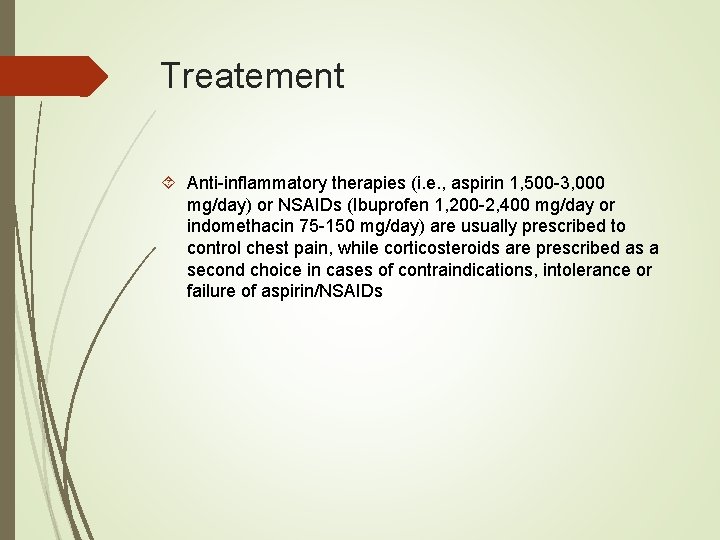
Treatement Anti-inflammatory therapies (i. e. , aspirin 1, 500 -3, 000 mg/day) or NSAIDs (Ibuprofen 1, 200 -2, 400 mg/day or indomethacin 75 -150 mg/day) are usually prescribed to control chest pain, while corticosteroids are prescribed as a second choice in cases of contraindications, intolerance or failure of aspirin/NSAIDs
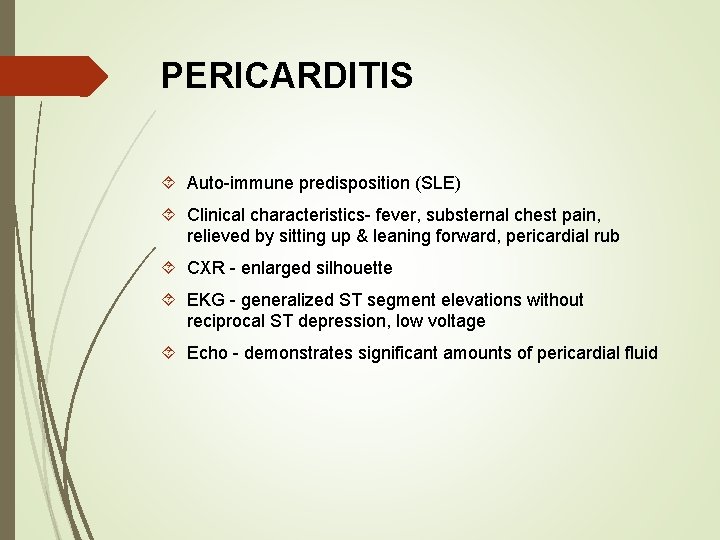
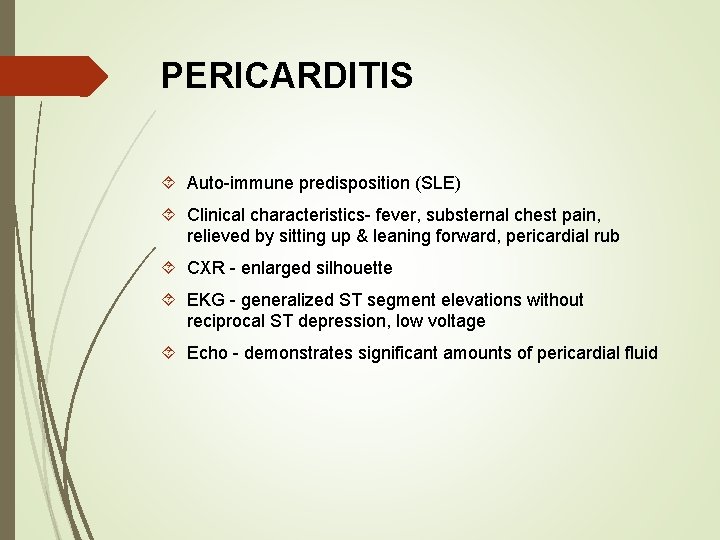
PERICARDITIS Auto-immune predisposition (SLE) Clinical characteristics- fever, substernal chest pain, relieved by sitting up & leaning forward, pericardial rub CXR - enlarged silhouette EKG - generalized ST segment elevations without reciprocal ST depression, low voltage Echo - demonstrates significant amounts of pericardial fluid
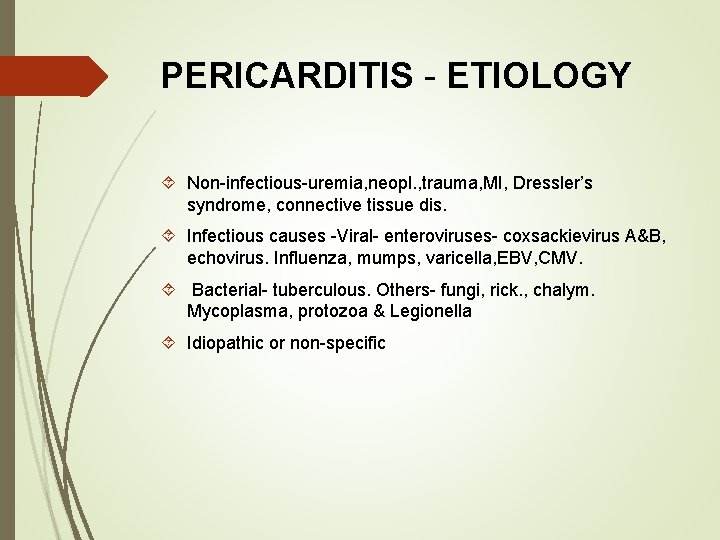
PERICARDITIS - ETIOLOGY Non-infectious-uremia, neopl. , trauma, MI, Dressler’s syndrome, connective tissue dis. Infectious causes -Viral- enteroviruses- coxsackievirus A&B, echovirus. Influenza, mumps, varicella, EBV, CMV. Bacterial- tuberculous. Others- fungi, rick. , chalym. Mycoplasma, protozoa & Legionella Idiopathic or non-specific
DIAGNOSIS OF PERICARDITIS Cultures - viral cx of pharynx, fecal sp. & pericardial fluid Serologic testing - acute & convalescent sera for antibodies to potential pathogens (cox. B virus or other enteroviruses) Pericardial drainage & biopsy -fluid & tissue can be cx for virus & tissue examined by histologic & immunofluorescent tech.
CONSTRICTIVE PERICARDITIS Treatment duration based on CRP ~3 months NSAIDS’s + colchicine – NSAID’s discontinuation if pain is no longer present after two weeks colchicine Avoid steroids due to reoccurrence Cardiac tamponade – pericardiocentesis
Future avenues for IE treatment Oritavancin & Dalbavancin – lipoglycopeptide Excreted extremely slowly (~<5% in urine and <1% stool at 14 days) Well tolerated with no clinically consequential changes in renal, hepatic, or hematological indices
Long-term implications Median survival is ~5 years post IE (based on studies in early 2000’s) Early surgical intervention with sever HF, overall better outcomes with later (3 months) surgery IVDU is the diagnosis that needs most attention Left sided IE and HF management and CKD management
Case report Unbelievably adorable 2 yo with PMhx of CHD s/p pulmonic valve creation ~2 years prior 1. 5 weeks of intermittent (low grade) fevers, no other signs of overt illness Social history: daughter of a brilliant and charming father who works in infectious disease NP and mother is notably attractive and brilliant
Organism: strept mitis Treated with ceftriaxone BID + gent synergism for 2 weeks, valve replacement and 4 more weeks of CTX monotherapy, completing a 6 week course. Acute antibiotic treatment course to be followed by lifetime embarrassment and doting over by father