Infectious Diseases Pearls Randall S Edson MD MACP




















- Slides: 59

Infectious Diseases Pearls Randall S. Edson, MD, MACP Professor of Medicine Mayo Clinic College of Medicine Internal Medicine Program Director, CPMC San Francisco, CA Division of INFECTIOUS DISEASES © 2011 MFMER | slide-1

Disclosures, etc No financial disclosures or discussion of off-label drugs, etc. © 2011 MFMER | slide-2
Coming clean…………. . Went through express lane with > 12 items Forgot to return shopping cart to corral on one occasion Deliberately avoids using the stairs at all costs, despite ubiquitous signage and propaganda
Public Service Announcement © 2012 MFMER | 3220467 -4

Learning objectives Recognize important travel-acquired infections Understand the approach to the diagnosis of LTB Diagnose CNS infection based on pattern recognition Review updated guidelines for UTI management Diagnose a mystery rash © 2011 MFMER | slide-5

25 yr old ♂ with three week history: fever, sore throat, fatigue, sweats. Grad student; just returned from 3 week trip to Southern Africa. Ate local food, swam in fresh water, took brief course of ciprofloxacin for traveler’s diarrhea Exam: Appears ill; T 38. 80; oral ulcers, exudative pharyngitis, post-cervical nodes, rash Lab: HCT 38%; WBC 12, 000(↑lymphs, “atypical”); mild ↑AST; Mono spot neg; HIV Ab negative

© 2012 MFMER | 3220467 -7
Which of the following would most likely establish diagnosis? a. b. c. d. e. EBV serology CMV serology Dengue serology PCR for HIV RNA Rickettsia africae serology
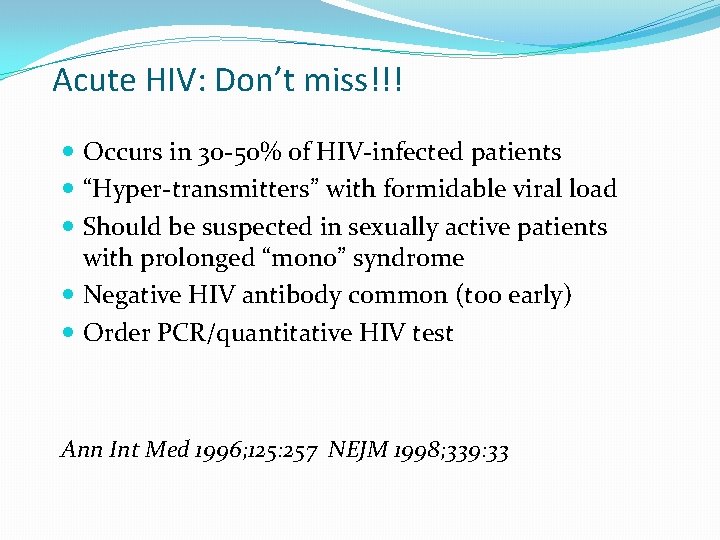
Acute HIV: Don’t miss!!! Occurs in 30 -50% of HIV-infected patients “Hyper-transmitters” with formidable viral load Should be suspected in sexually active patients with prolonged “mono” syndrome Negative HIV antibody common (too early) Order PCR/quantitative HIV test Ann Int Med 1996; 125: 257 NEJM 1998; 339: 33
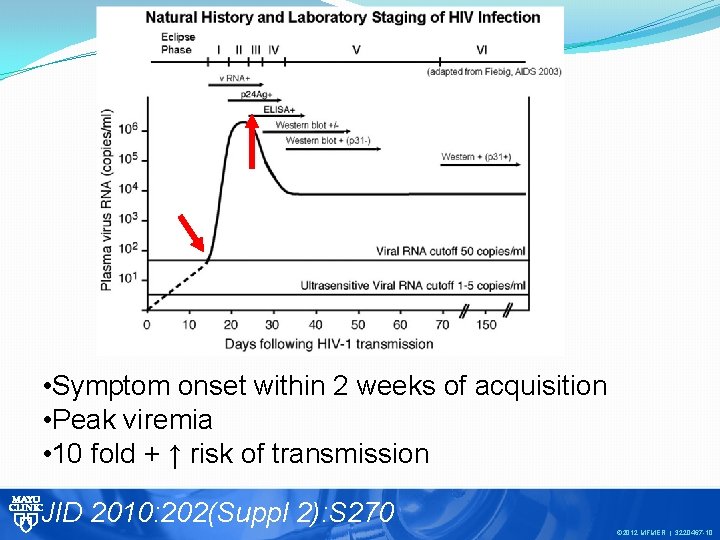
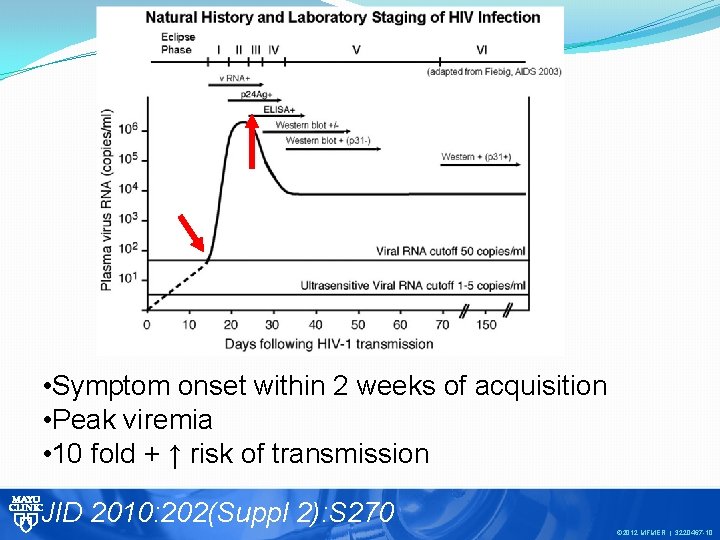
• Symptom onset within 2 weeks of acquisition • Peak viremia • 10 fold + ↑ risk of transmission JID 2010: 202(Suppl 2): S 270 © 2012 MFMER | 3220467 -10
What’s in your travel kit? ? >50, 000 new cases of HIV/year in US © 2012 MFMER | 3220467 -11
STD in Returning Travelers Casual sex: 5 -51% of short term travelers, ↑ among long term travelers Meta analysis: 20% have casual sex abroad; 50% unprotected* Not usually addressed in pre-travel consults * Intern J of Inf. Dis 2010; 14(10): e 842 -51 CID 2001; 32: 1063 J Travel Med 2009; 16: 79
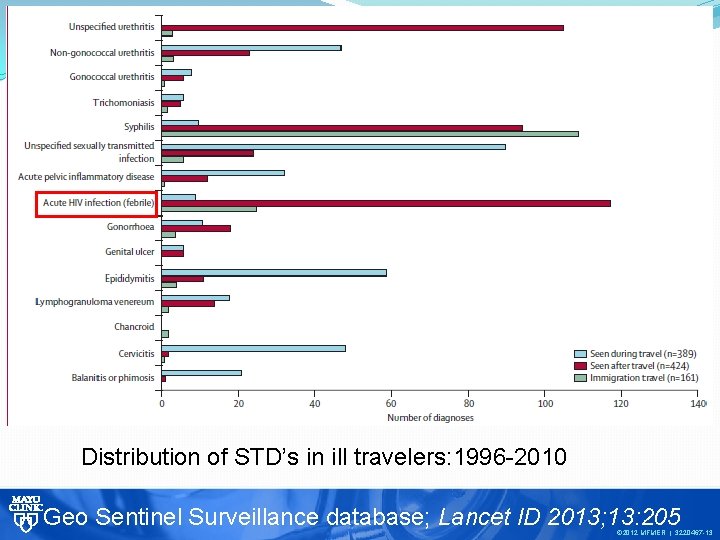
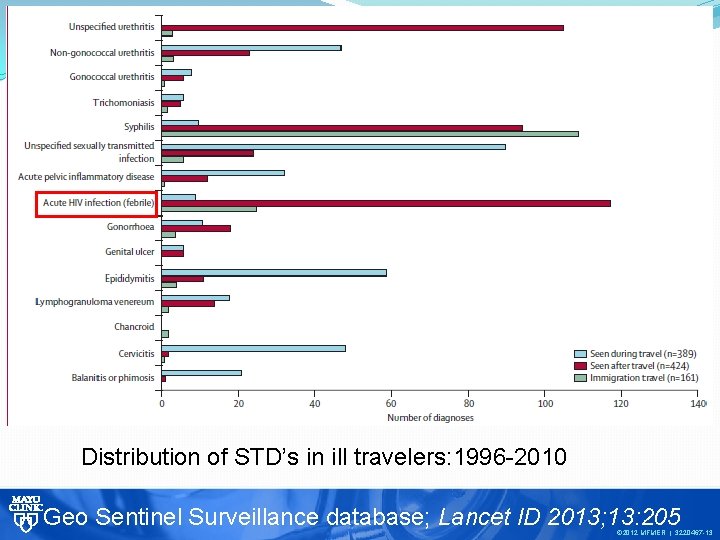
Distribution of STD’s in ill travelers: 1996 -2010 Geo Sentinel Surveillance database; Lancet ID 2013; 13: 205 © 2012 MFMER | 3220467 -13
Pre-employment evaluation 28 yr. old ♀ respiratory tech about to begin work at your hospital Mild asthma, controlled with occasional albuterol; otherwise healthy Immigrated to US from Philippines 3 years ago Cervical cytology, all adult immunizations current; received BCG as a child © 2012 MFMER | 317742414
Your hospital requires screening for LTB Which of the following would be the most appropriate screening test for latent TB? a) b) c) d) Chest x-ray Interferon-γ release assay PPD(5 TU) PPD(10 TU) © 2012 MFMER | 317742415
TB and Latent TB 1/3 of world population infected with TB Latent TB develops in ≈ 30% exposed Estimated cases of LTB in US ≈11 million Lifetime risk of reactivation 5 -10% Most clinical TB in US occurs in immigrants from high prevalence countries Herrera et al. Clin Inf Dis 2011; 52(8): 1031
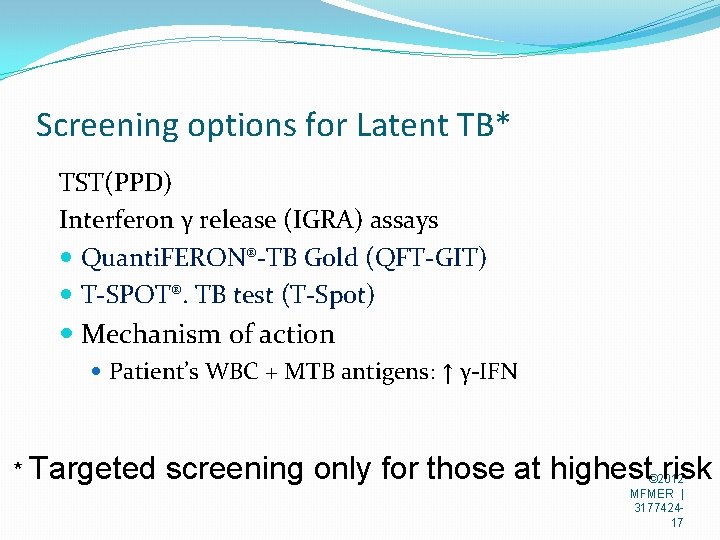
Screening options for Latent TB* TST(PPD) Interferon γ release (IGRA) assays Quanti. FERON®-TB Gold (QFT-GIT) T-SPOT®. TB test (T-Spot) Mechanism of action Patient’s WBC + MTB antigens: ↑ γ-IFN * Targeted screening only for those at highest risk © 2012 MFMER | 317742417
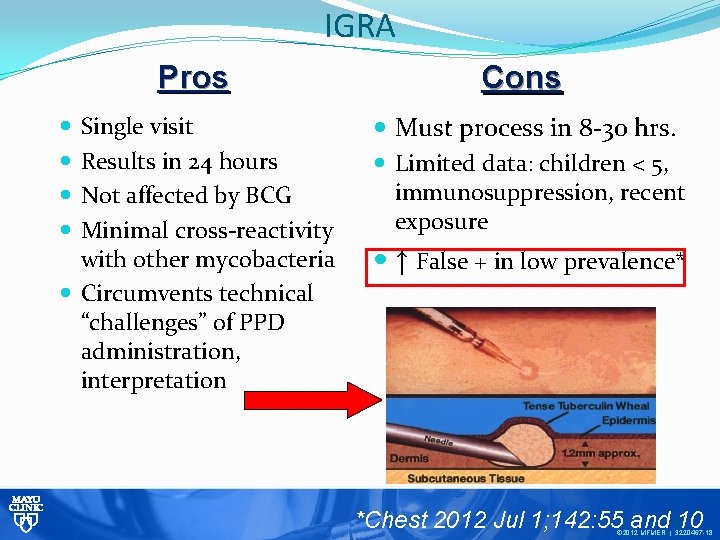
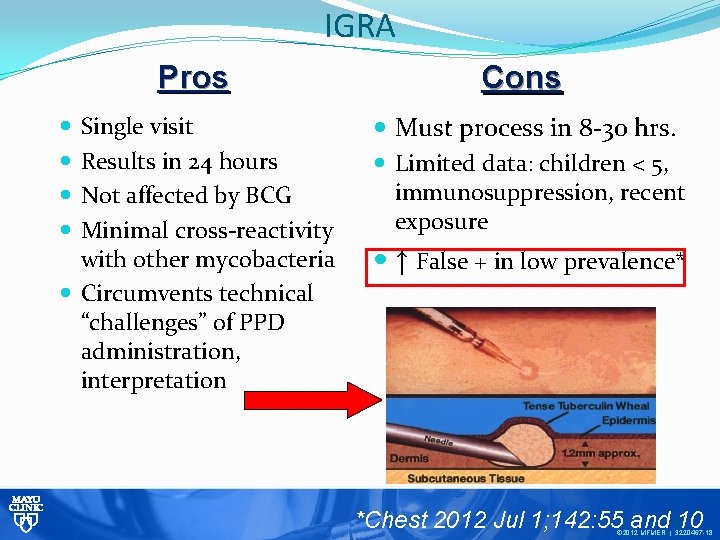
IGRA Pros Cons Single visit Results in 24 hours Not affected by BCG Minimal cross-reactivity with other mycobacteria Circumvents technical “challenges” of PPD administration, interpretation Must process in 8 -30 hrs. Limited data: children < 5, immunosuppression, recent exposure ↑ False + in low prevalence* *Chest 2012 Jul 1; 142: 55 and © 10 © 2012 MFMER | 3220467 -18
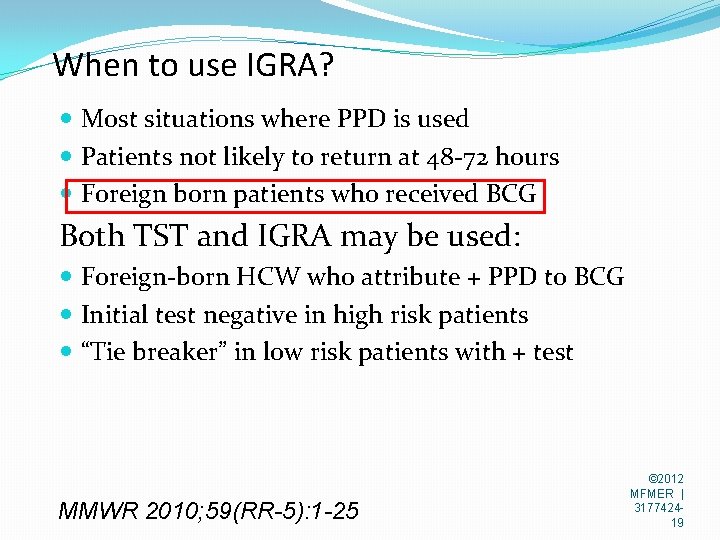
When to use IGRA? Most situations where PPD is used Patients not likely to return at 48 -72 hours Foreign born patients who received BCG Both TST and IGRA may be used: Foreign-born HCW who attribute + PPD to BCG Initial test negative in high risk patients “Tie breaker” in low risk patients with + test MMWR 2010; 59(RR-5): 1 -25 © 2012 MFMER | 317742419

Game changer in the treatment of latent TB 900 mg INH plus 900 mg of Rifapentine once weekly for three months Equally effective as 9 months of daily INH ≈ $40 total Perfect situation for Directly Observed Therapy (DOT) Rifapentine is expensive: ≈ $325 for 3 month course © 2012 MFMER | 3220467 -20

55 yr. old ♂ farmer with fever and confusion 8/2012: difficulty with concentration, spatial perception; co-workers noted distraction and trouble with word finding. Day 2: severe HA DM 2, s/p bariatric surgery, hypertension Sexually active, farms and road maintenance Exam: T 38. 50; drowsy; mild neck stiffness CSF: WBC 165 cells/µL(mostly lymphs) Protein 150 mg/d. L; glucose 61 mg/d. L Gram stain: no organisms seen

Develops significant weakness and cogwheeling several hours later Which one of the following tests would most likely establish the correct diagnosis? a. b. c. d. MRI of head with gadolinium CSF PCR for Herpes simplex virus CSF Ig. M for West Nile virus CSF serology for enterovirus

4891 cases, 2293(51%) Neuro-invasive, 223 deaths; 70% from 10 states; highest number to date since 2003 © 2012 MFMER | 3220467 -23

Unintended consequence of foreclosure © 2012 MFMER | 3220467 -24
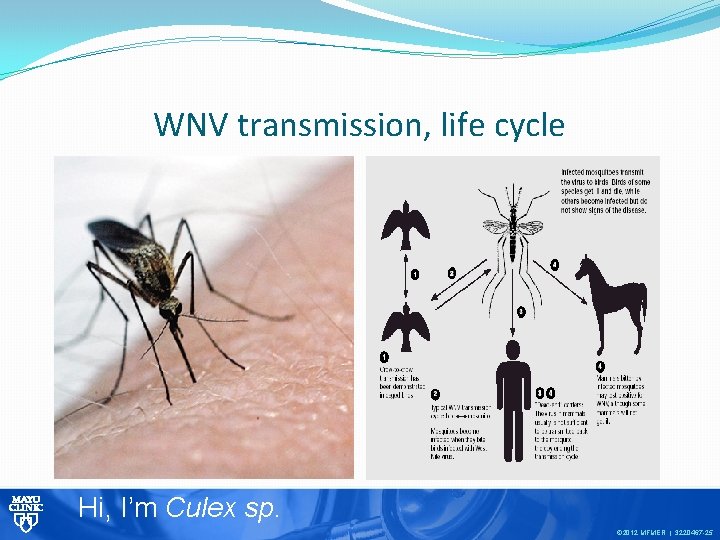
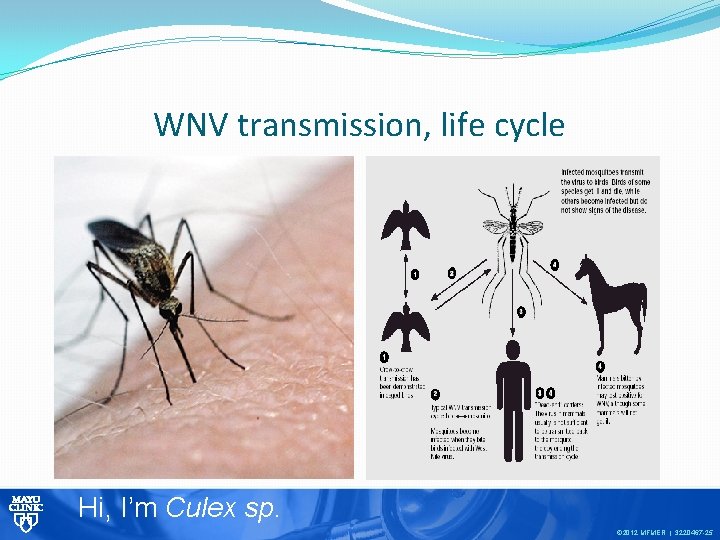
WNV transmission, life cycle Hi, I’m Culex sp. © 2012 MFMER | 3220467 -25
Flavivirus West Nile Virus 101 St Louis Encephalitis; Yellow fever; JE Acquisition: mosquito, transfusion, transplant Peak incidence: Late August, early September Incubation: 2 to 14 days 80% asymptomatic 20% WN fever; < 1% Neuro-invasive
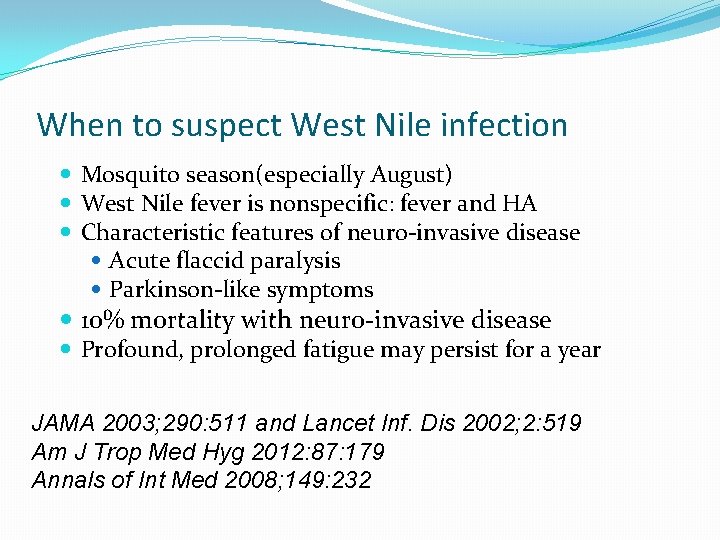
When to suspect West Nile infection Mosquito season(especially August) West Nile fever is nonspecific: fever and HA Characteristic features of neuro-invasive disease Acute flaccid paralysis Parkinson-like symptoms 10% mortality with neuro-invasive disease Profound, prolonged fatigue may persist for a year JAMA 2003; 290: 511 and Lancet Inf. Dis 2002; 2: 519 Am J Trop Med Hyg 2012: 87: 179 Annals of Int Med 2008; 149: 232

Diagnostic time course of West Nile Virus Serum or CSF Ig. M best diagnostic test Ig. M antibodies may persist for a year www. mayomedicallaboratories. com/articles/communique/2008 © 2012 MFMER | 3220467 -28
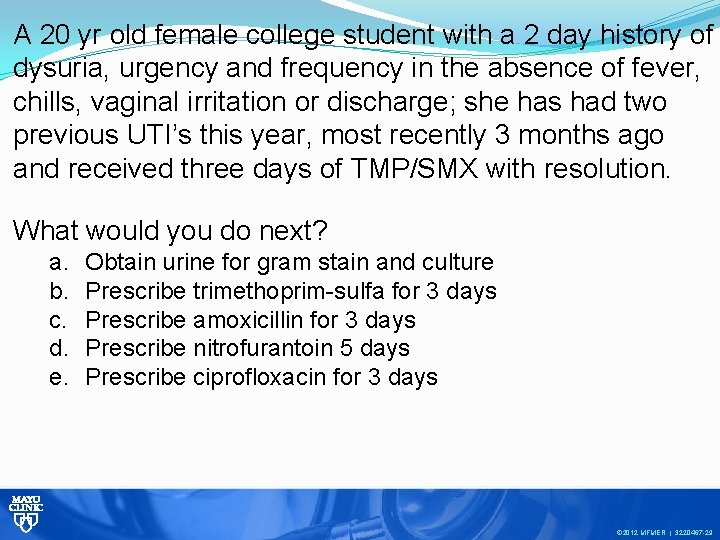
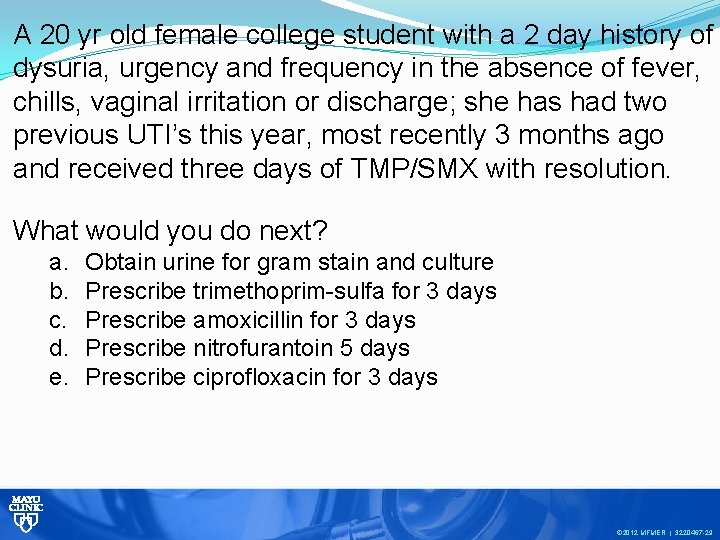
A 20 yr old female college student with a 2 day history of dysuria, urgency and frequency in the absence of fever, chills, vaginal irritation or discharge; she has had two previous UTI’s this year, most recently 3 months ago and received three days of TMP/SMX with resolution. What would you do next? a. b. c. d. e. Obtain urine for gram stain and culture Prescribe trimethoprim-sulfa for 3 days Prescribe amoxicillin for 3 days Prescribe nitrofurantoin 5 days Prescribe ciprofloxacin for 3 days © 2012 MFMER | 3220467 -29
When words fail…………… © 2012 MFMER | 3220467 -30

NEJM 2012; 366: 1028 -37 and Clin Inf Dis 2011; 52(5): e 103 -e 120 © 2012 MFMER | 3220467 -31

Key facts in UTI management E. coli increasingly resistant to TMP/SMX, FQ Avoid TMP/SMX if local resistance is ≥ 20% or used w/n last 3 months Avoid FQ if local resistance is ≥ 10% Mayo Antibiogram 2011

More key facts in UTI management Do not treat asymptomatic bacteriuria(AB) even with pyuria except: Pregnancy; post renal transplant Prior to urologic instrumentation Unintended consequences of AB Rx ↑ frequency of subsequent symptomatic UTI 1 Asymptomatic bacteriuria may be “protective” Alarming increase in community-acquired multidrug resistant E. coli 2 1 Clin Infect Dis 2012; 55: 771 2 Mayo Clin Proc 2012; 87(8): 753
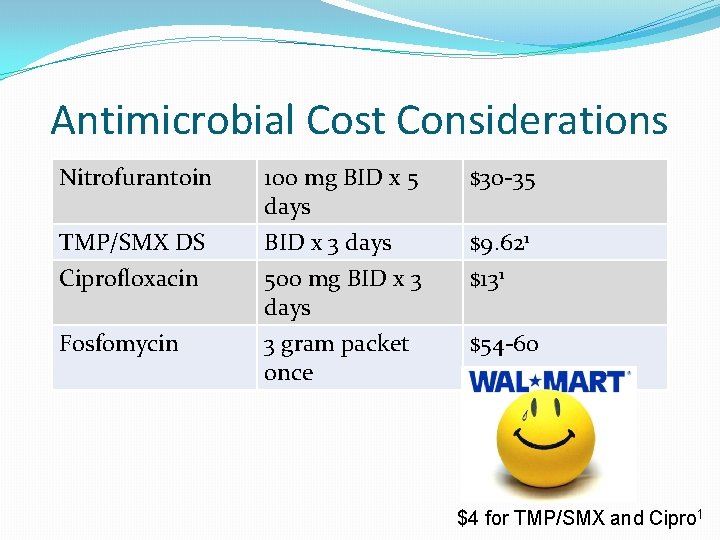
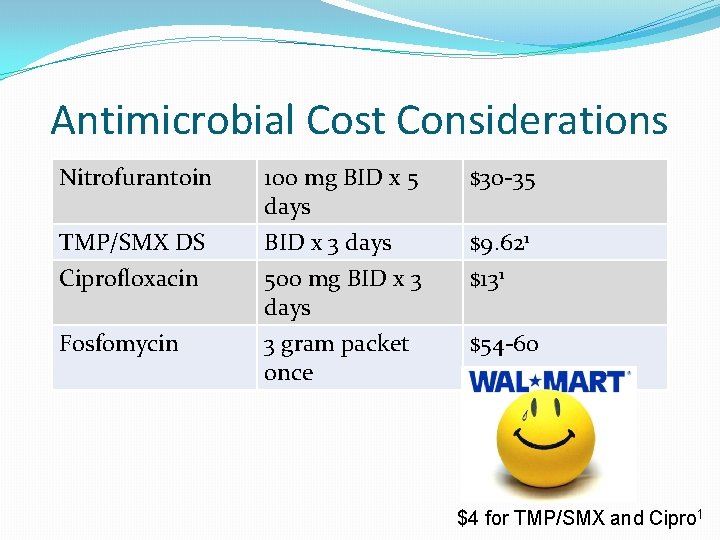
Antimicrobial Cost Considerations Nitrofurantoin 100 mg BID x 5 days $30 -35 TMP/SMX DS Ciprofloxacin BID x 3 days 500 mg BID x 3 days $9. 621 $131 Fosfomycin 3 gram packet once $54 -60 $4 for TMP/SMX and Cipro 1
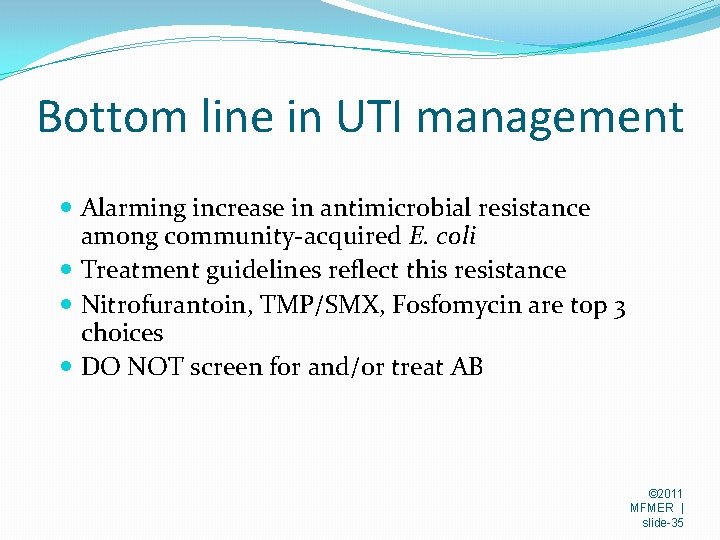
Bottom line in UTI management Alarming increase in antimicrobial resistance among community-acquired E. coli Treatment guidelines reflect this resistance Nitrofurantoin, TMP/SMX, Fosfomycin are top 3 choices DO NOT screen for and/or treat AB © 2011 MFMER | slide-35
67 yr old man with a rash Developed painless nodular, pustular rash 2 weeks ago Did not respond to several oral antibiotics and five infusions of vancomycin Swab culture: rare Pseudomonas fluorescence Treated with ciprofloxacin without improvement Examination Vital signs normal, afebrile Rash on dorsum of left forearm

© 2012 MFMER | 3220467 -37

What would you do next? a. b. c. d. Begin anti-mycobacterial Rx Start trimethoprim-sulfa for suspected Nocardia Start antifungal Rx Send to Derm for biopsy
Most likely diagnosis? a. b. c. d. e. Squamous cell carcinoma Blastomycosis Nocardiosis Non-tuberculous mycobacterial infection Dermatophyte
Additional history 5 days before rash onset cleared brush, had exposure to mud, thorns; recalls many scratches, wearing shortsleeve shirt Has cattle, dogs, cats
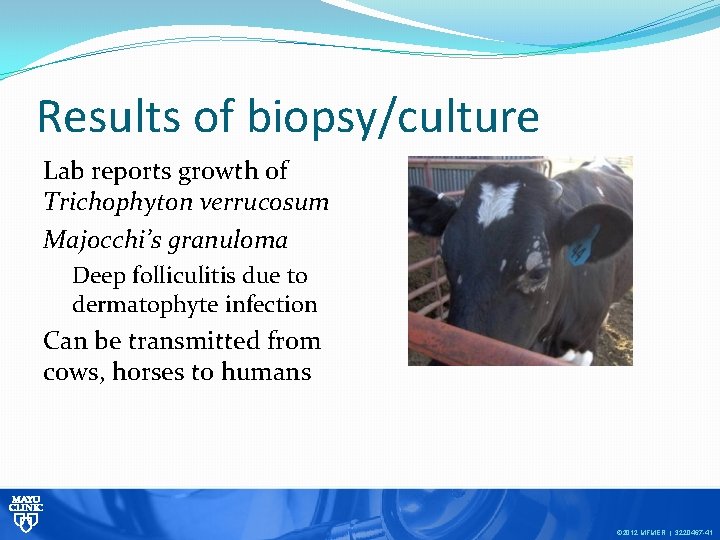
Results of biopsy/culture Lab reports growth of Trichophyton verrucosum Majocchi’s granuloma Deep folliculitis due to dermatophyte infection Can be transmitted from cows, horses to humans © 2012 MFMER | 3220467 -41

Trichophyton verrucosum © 2012 MFMER | 3220467 -42
Clinical bottom line The occupational and exposure history can be critical in broadening the differential diagnosis
56 year old ♂ with chronic cough, sweats 3 month history of productive cough, sweats, weight loss. No response to several AB courses PMH: MS, COPD SH: divorced, disabled miner; 50 pack year smoking history; former daily marijuana smoker, now using marijuana “chocolates. ” Lives in wooded area of Michigan’s UP Recently moved into old house with obvious mold; spent several weeks using leaf blower; several local dogs ill with respiratory symptoms
MBF © 2012 MFMER | 3220467 -45
Malignancy suspected; second opinion sought Physical examination Appears cachectic(“hunter-gatherer diet”) Afebrile Many missing teeth and periodontal disease Few rales at right lung base CBC, electrolytes, etc. all normal
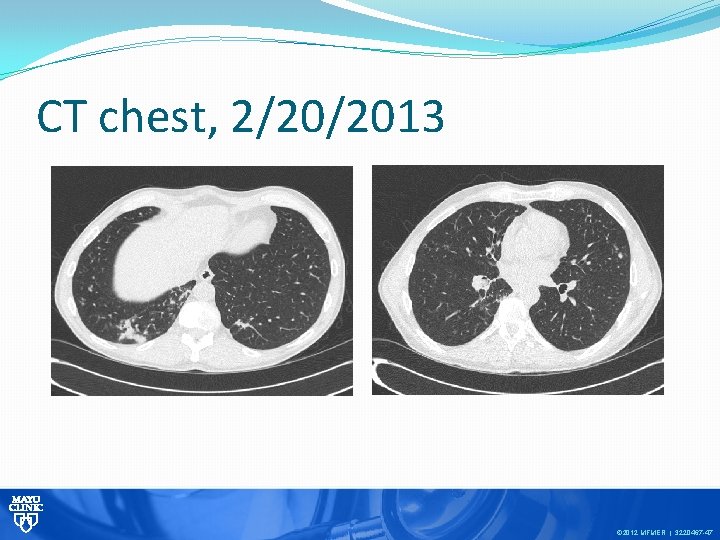
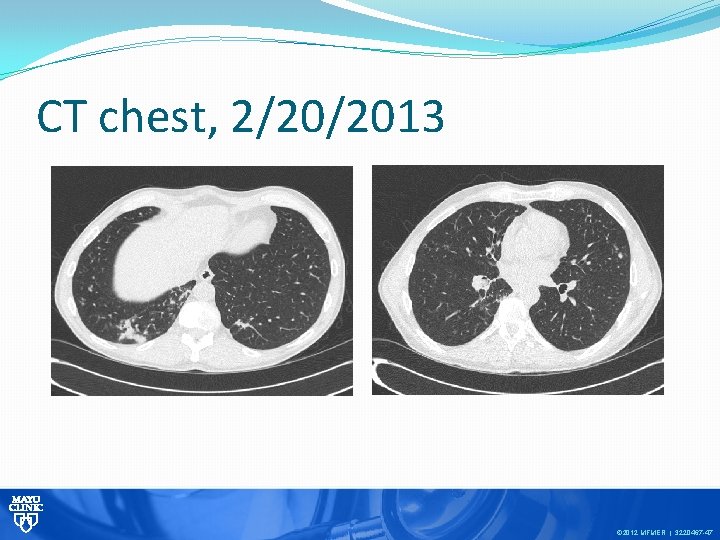
CT chest, 2/20/2013 © 2012 MFMER | 3220467 -47
Bronchoscopy done on 2/20/13 Mucopurulent secretions noted in right lower lung. A diagnostic result was received……. .

Direct smear from BAL fluid © 2012 MFMER | 3220467 -49
What is the most likely diagnosis? a. b. c. d. Bronchogenic CA with post-obstructive pneumonia Mixed aerobic/anaerobic pneumonitis Pulmonary blastomycosis Pulmonary nocardiosis
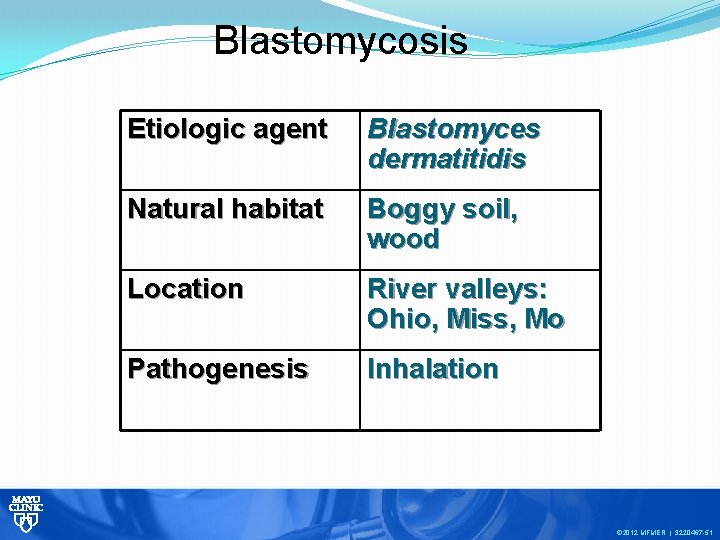
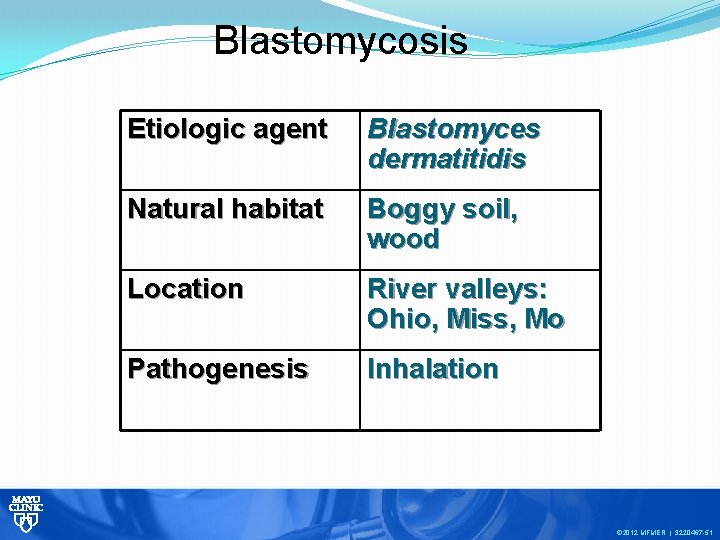
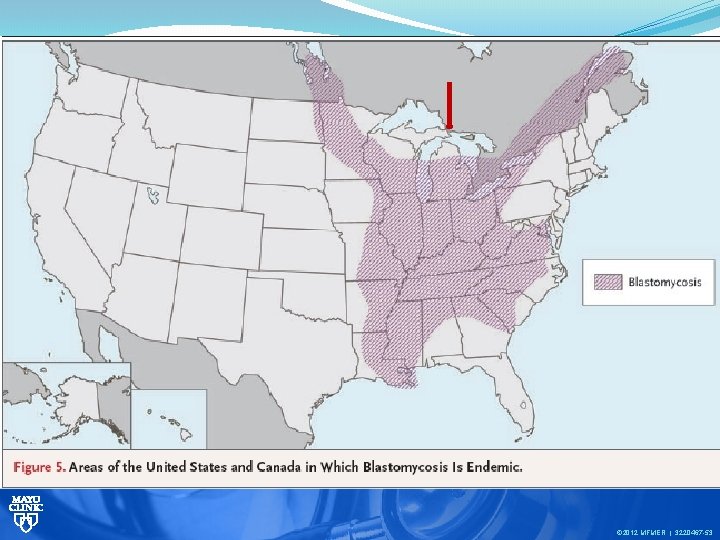
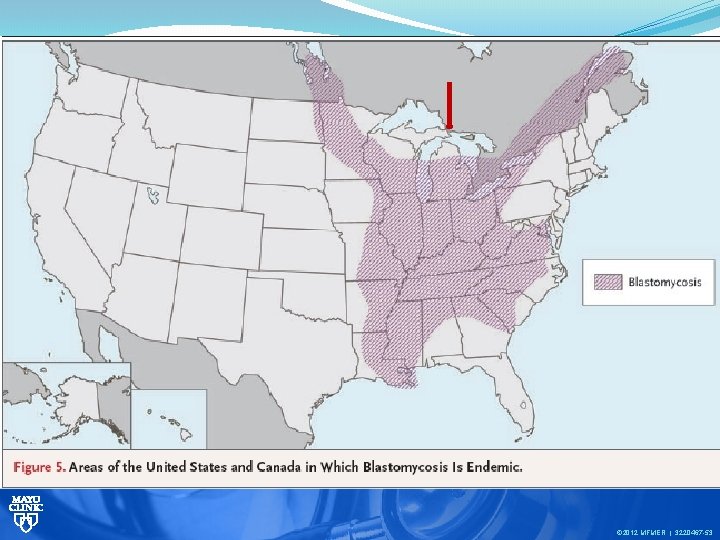
Blastomycosis Etiologic agent Blastomyces dermatitidis Natural habitat Boggy soil, wood Location River valleys: Ohio, Miss, Mo Pathogenesis Inhalation © 2012 MFMER | 3220467 -51
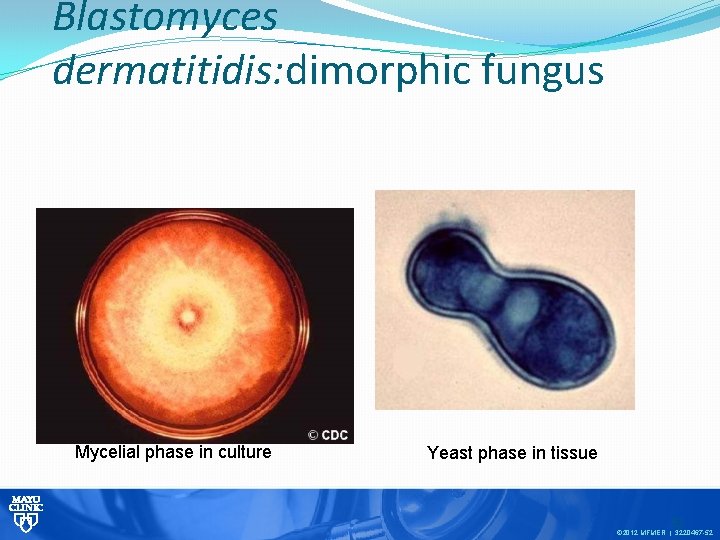
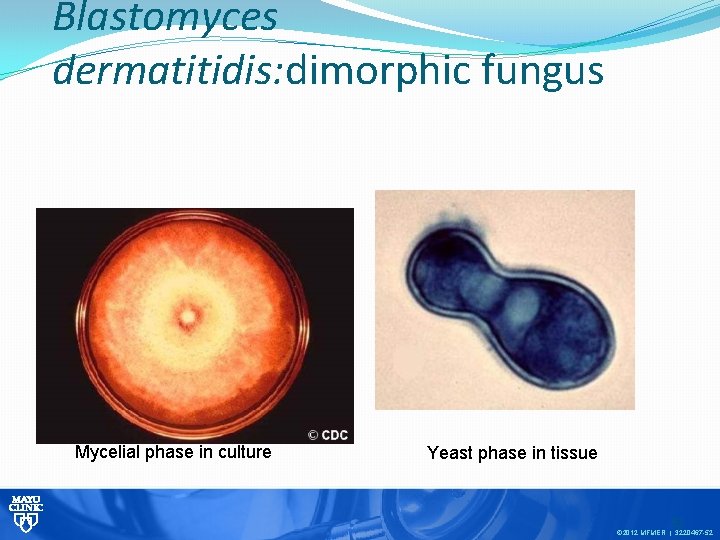
Blastomyces dermatitidis: dimorphic fungus Mycelial phase in culture Yeast phase in tissue 52 © 2012 MFMER | 3220467 -52
© 2012 MFMER | 3220467 -53

NEJM 1986; 314(9): 529 -34 “Leave it to Beaver” © 2012 MFMER | 3220467 -54
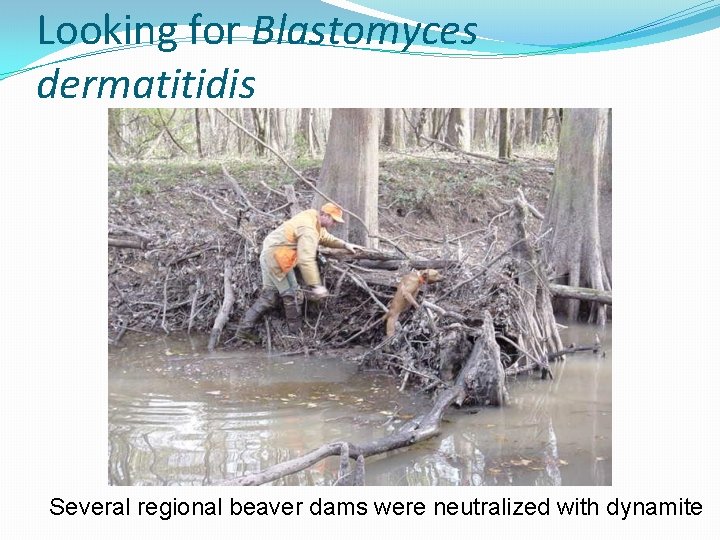
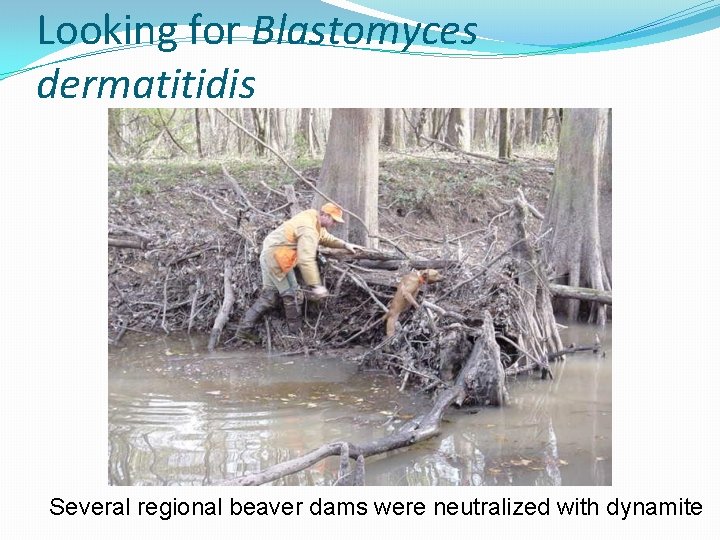
Looking for Blastomyces dermatitidis Several regional beaver dams were neutralized with dynamite
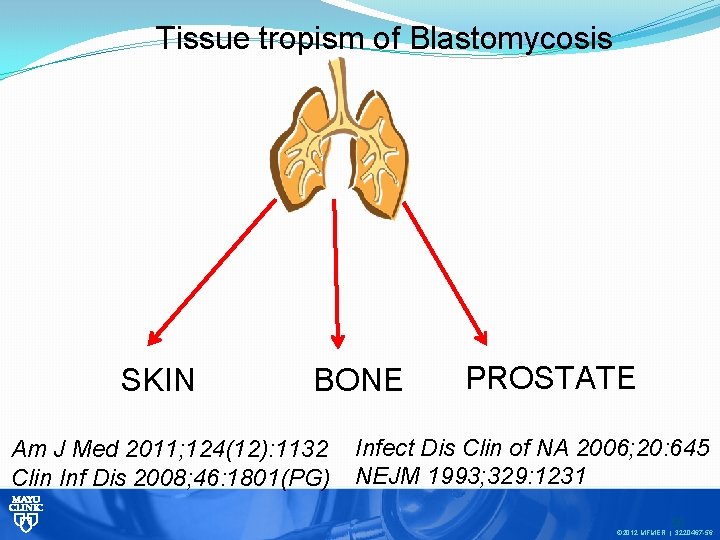
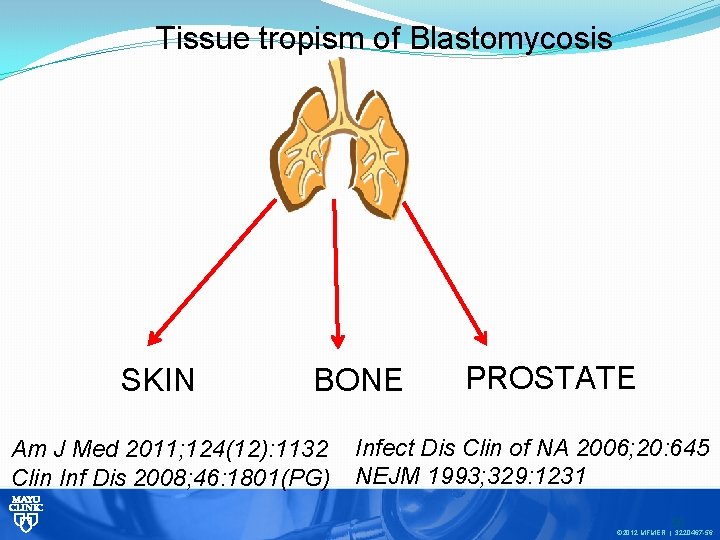
Tissue tropism of Blastomycosis SKIN BONE Am J Med 2011; 124(12): 1132 Clin Inf Dis 2008; 46: 1801(PG) PROSTATE Infect Dis Clin of NA 2006; 20: 645 NEJM 1993; 329: 1231 56 © 2012 MFMER | 3220467 -56

Cutaneous manifestation of disseminated Blastomycosis © 2012 MFMER | 3220467 -57
Blastomycosis: making the diagnosis Direct smear from clinical specimen Culture Serology Previous CF test had poor sensitivity, specificity Newly approved EIA has excellent sensitivity, specificity Urine antigen: high sensitivity, poor specificity
Don’t forget to do your part © 2011 MFMER | slide-59
 Icd 10 morbus hansen
Icd 10 morbus hansen Epidemiological triad of malaria
Epidemiological triad of malaria Portugol
Portugol Edson shiguemi hirata
Edson shiguemi hirata Edson paschoalin
Edson paschoalin Plastic packing pearls
Plastic packing pearls Pearls of sicily lido di noto
Pearls of sicily lido di noto Np cca points
Np cca points Like a sunset's crimson splendour meaning
Like a sunset's crimson splendour meaning Inrs
Inrs Gensvarsmodeller
Gensvarsmodeller Analisis pearls
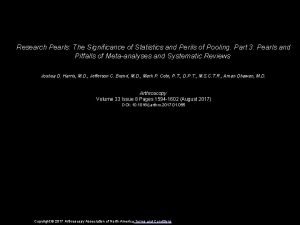
Analisis pearls Stat pearls impact factor
Stat pearls impact factor Symbolism in the pearl
Symbolism in the pearl Pharmacy clinical pearls
Pharmacy clinical pearls I am a small and skinny chap
I am a small and skinny chap Natural pearls are found in which creature
Natural pearls are found in which creature Magma coral bells
Magma coral bells Gdma2 medical abbreviation
Gdma2 medical abbreviation Analisa pearls
Analisa pearls Infectious disease
Infectious disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious disease quality controls
Infectious disease quality controls Noncellular infectious protein particles are called
Noncellular infectious protein particles are called Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious nucleic acid
Infectious nucleic acid Infectious mononucleosis
Infectious mononucleosis Periods of infectious disease
Periods of infectious disease Infectious stunting syndrome
Infectious stunting syndrome Infectious disease board review
Infectious disease board review Hennepin county infectious disease manual
Hennepin county infectious disease manual Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Lead poisoning
Lead poisoning What is the smallest infectious agent
What is the smallest infectious agent Mebosha
Mebosha Snc set symbol
Snc set symbol Stages of infectious disease
Stages of infectious disease Dr randall mcshine
Dr randall mcshine Randall neustaedter
Randall neustaedter Is randall woodfield still alive
Is randall woodfield still alive Randall library database
Randall library database Dick świr marcinko
Dick świr marcinko Randall tyle
Randall tyle Randall neustaedter
Randall neustaedter Chris randall wvu
Chris randall wvu Randall bone
Randall bone Get up and bar the door translation
Get up and bar the door translation Randall pearce
Randall pearce Excess property thermodynamics
Excess property thermodynamics Randall oreilly
Randall oreilly Ballad of birmingham theme
Ballad of birmingham theme Randall reed md
Randall reed md Iab qualification
Iab qualification Chremamorphism
Chremamorphism Randall marcinko
Randall marcinko Randall munroe
Randall munroe Randall waller instagram
Randall waller instagram Hipositratüri
Hipositratüri Randall eisenberg
Randall eisenberg Randall
Randall