Infectious disease pathology Lecture 3 Mays Ibrahim Arab
Infectious disease pathology Lecture 3 Mays Ibrahim, Arab board of pathology, CABP University of Al-Mustansiriyah, college of medicine

Syphilis � Syphilis is a chronic venereal disease caused by Treponema pallidum spirochete with multiple presentations. � Mode of transmission Sexual contact is the usual mode of spread. Transplacental transmission
� Syphilis 1. is divided into Acquired syphilis a. Primary Syphilis. b. Secondary Syphilis c. Tertiary Syphilis. 2. Congenital syphilis.
Primary syphilis Localized disease Occurs about 3 weeks after contact with an infected individual. Chancre : is a characteristic sign of primary syphilis, and it is a firm, non-tender, raised, red lesion forms on the penis, cervix, vaginal wall, or anus; it will heal after 3 -6 weeks even without therapy(i. e. spontaneously). Diagnosis: Lesional smear( chancre) using dark field microscopy to see the micro organism Tissue biopsy: reveal, ulceration, plasma cells, macrophages, and lymphocytes, with a proliferative endarteritis. 1. 2.

Secondary syphilis 2 to 10 weeks after the primary chancre Disseminated disease with constitutional symptoms. 75% of untreated primary syphilis will get secondary syphilis. due to spread and proliferation of the spirochetes within the skin and mucocutaneous tissues
lesions in secondary syphilis are 1. Maculopapular rash: all over the body including palms and soles of the feet, and affect the mucocutaneous tissues (especially mouth). 2. Condylomata lata: are painless smooth, elevated plaques with a broad-based, in areas of the skin, such as the anogenital region, inner thighs, and axillae


Is highly infectious stage. Lymphadenopathy, mild fever, malaise, and weight loss are common The symptoms of secondary syphilis last several weeks, after which the person enters the latent phase of the disease Tissue biopsy: reveal plasma cell infiltrate and obliterative endarteritis.

Latent phase of syphilis Is a period of time ( 5 years or more) when there are no visible sign or symptoms of syphilis but positive serology. May follow secondary syphilis. Patients are still contagious in the early stage of this phase.
Tertiary syphilis occurs in approximately one third of untreated secondary syphilis patients usually after a latent period of 5 -30 years or more � Have 1. 2. 3. three main manifestations: Cardiovascular syphilis Neurosyphilis Gummas

Cardiovascular syphilis � About 80% of tertiary syphilis. � It affects the followings: Aorta: leading to syphilitic aortitis which will end up with Aneurysm of aortic root and arch (tree barking). Aortic valve: causing valve incompetence. Coronary arteries: narrowing of the coronary artery opening will cause angina pectoris. Heart (very rare): involved by gumma.
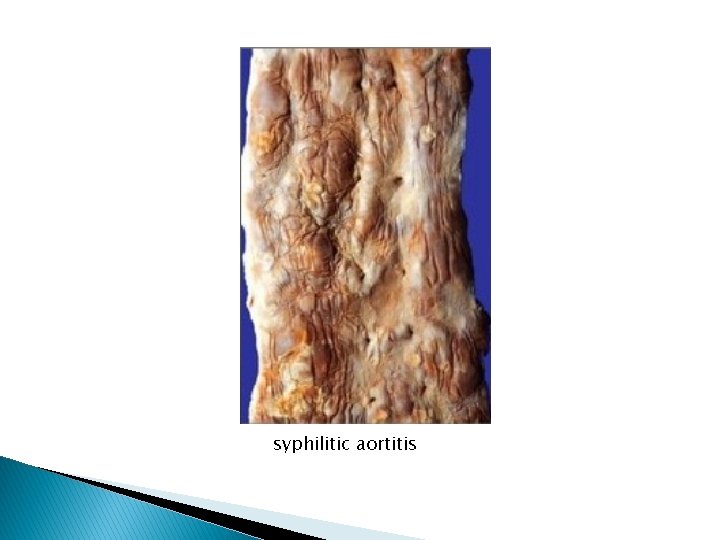
syphilitic aortitis
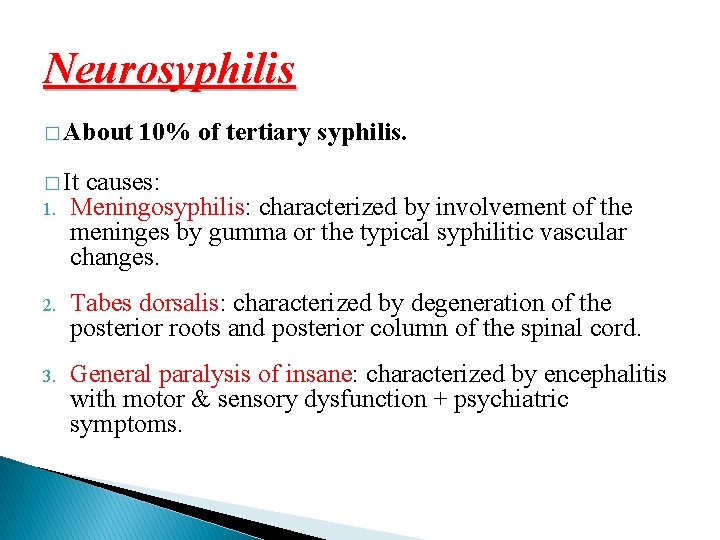
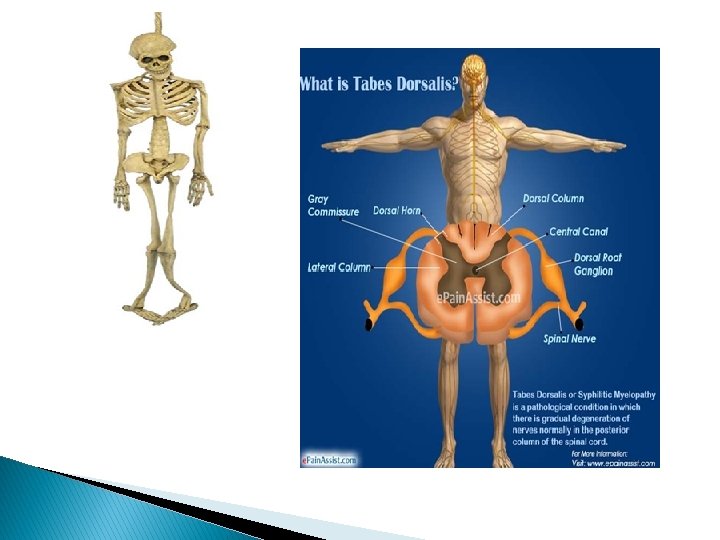
Neurosyphilis � About 10% of tertiary syphilis. � It causes: 1. Meningosyphilis: characterized by involvement of the meninges by gumma or the typical syphilitic vascular changes. 2. Tabes dorsalis: characterized by degeneration of the posterior roots and posterior column of the spinal cord. 3. General paralysis of insane: characterized by encephalitis with motor & sensory dysfunction + psychiatric symptoms.
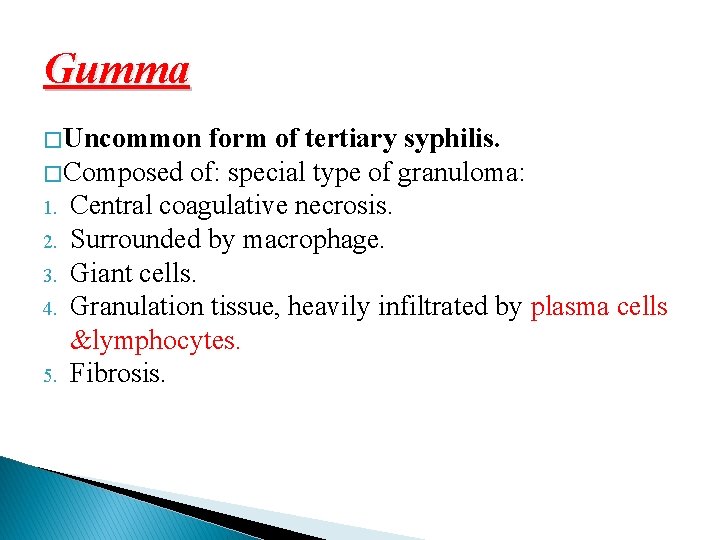
Gumma � Uncommon form of tertiary syphilis. � Composed of: special type of granuloma: 1. Central coagulative necrosis. 2. Surrounded by macrophage. 3. Giant cells. 4. Granulation tissue, heavily infiltrated by plasma cells &lymphocytes. 5. Fibrosis.
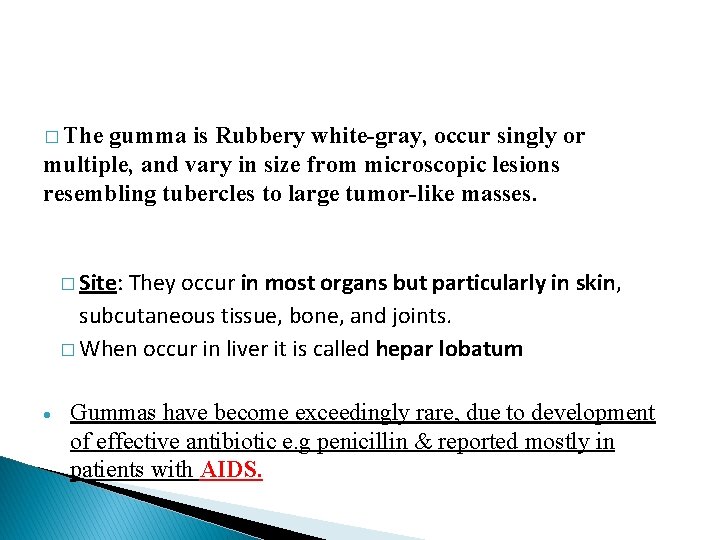
� The gumma is Rubbery white-gray, occur singly or multiple, and vary in size from microscopic lesions resembling tubercles to large tumor-like masses. � Site: They occur in most organs but particularly in skin, subcutaneous tissue, bone, and joints. � When occur in liver it is called hepar lobatum Gummas have become exceedingly rare, due to development of effective antibiotic e. g penicillin & reported mostly in patients with AIDS.
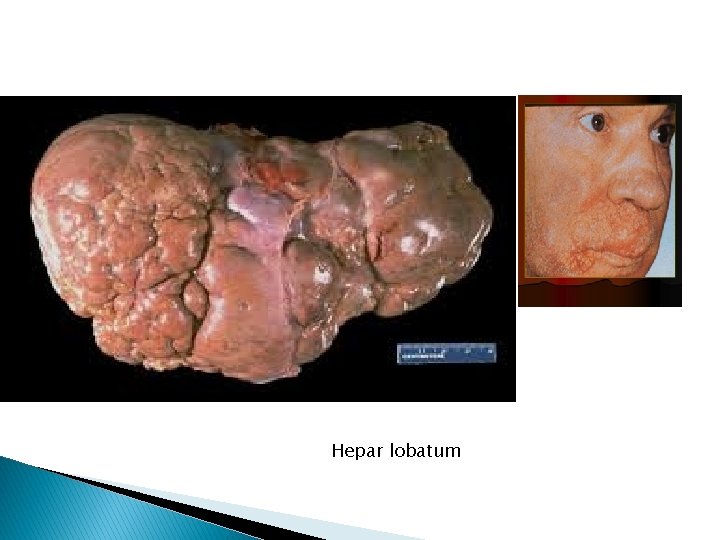
Hepar lobatum
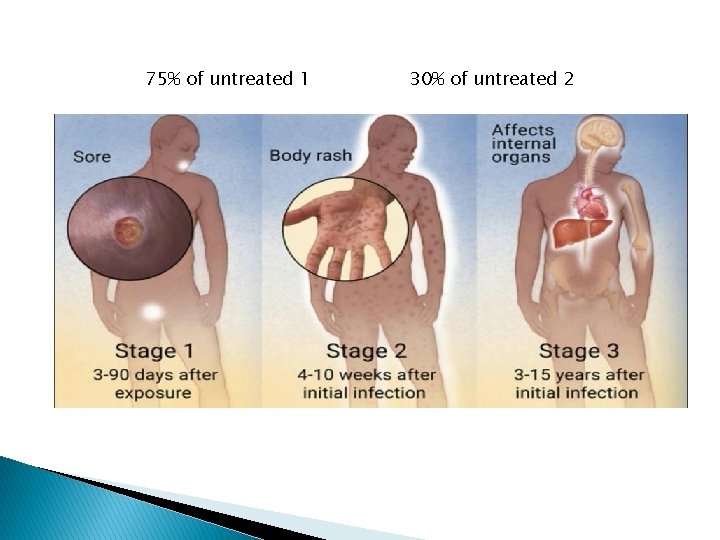
75% of untreated 1 30% of untreated 2

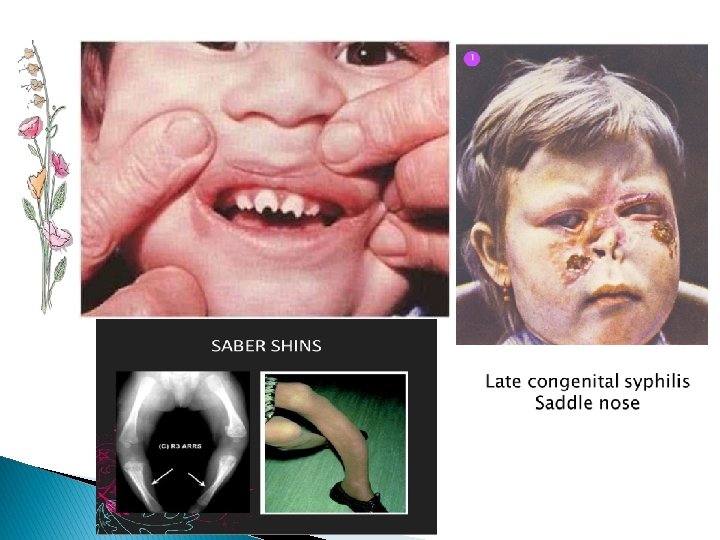
Congenital syphilis � Usually occurs when the mother has primary or secondary syphilis. Mode of transmission: transplacental or trans-vaginaly during birth. � Manifestation of the disease are : � Intrauterine or perinatal death (in 50% of untreated cases). Early (infantile) congenital syphilis: occurs in children between 0 and 2 years old, includes nasal discharge (snuffles), rash with skin sloughing, hepatomegaly, Diffuse lung or liver fibrosis can also occur. Late manifestations it occurs in children at or greater than 2 years of age Notched central incisors known as Hutchinson's teeth saddle nose (collapse of the bony part of nose) Deafness from auditory nerve disease Saber shin is a malformation of the tibia. It presents as a sharp anterior bowing inflammation of the cornea known as interstitial keratitis leading to blindness.
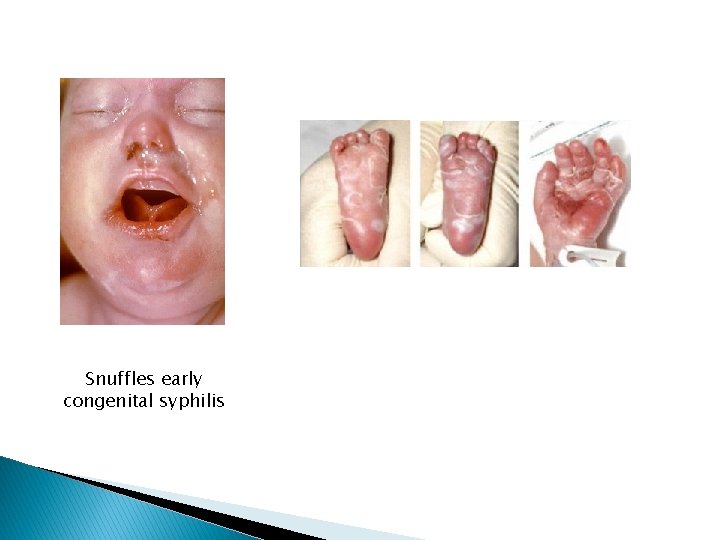
Snuffles early congenital syphilis
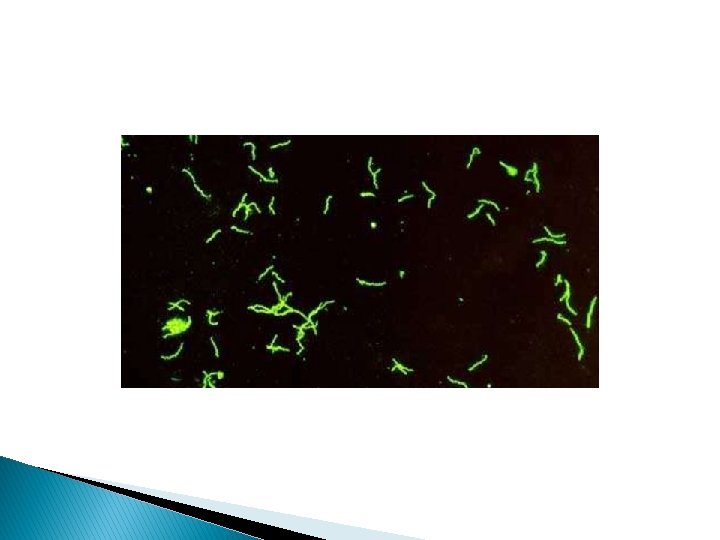
Diagnosis: 1. Visualizing the spirochete in chancre or the rash of secondary syphilis using dark field microscopy. 2. Tissue biopsy 3. Confirmed by the serological test. � Serologic tests for syphilis: 1. Treponemal antibody tests measure antibodies reactive with T. pallidum. 2. Nontreponemal tests (i. e. , VDRL “venereal disease research laboratory test”, RPR “rapid plasma reagin test”) measure antibody to cardiolipin, a found in treponemes and normal tissues.
Parasitic infections � Leishmaniasis � Amoebiasis � Giardiasis � Hydatid cyst � Schistosomiasis (bilhariziasis)
Leishmaniasis � is a chronic inflammatory disease of the skin, mucous membranes, or viscera � caused by intracellular Leishmania species, an obligate intracellular parasites � transmitted by sandfly bites With 3 different clinical presentations � Visceral leishmaniasis: � Cutaneous leishmaniasis � Mucocutaneous leishmaniasis
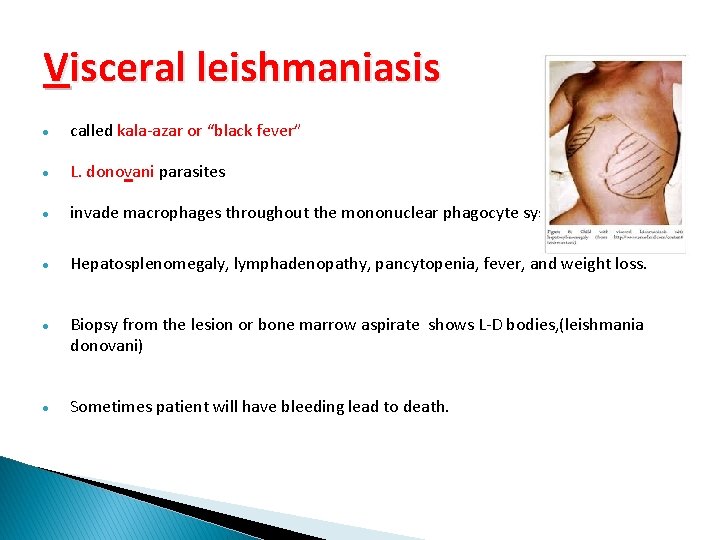
Visceral leishmaniasis called kala-azar or “black fever” L. donovani parasites invade macrophages throughout the mononuclear phagocyte system. Hepatosplenomegaly, lymphadenopathy, pancytopenia, fever, and weight loss. Biopsy from the lesion or bone marrow aspirate shows L-D bodies, (leishmania donovani) Sometimes patient will have bleeding lead to death.
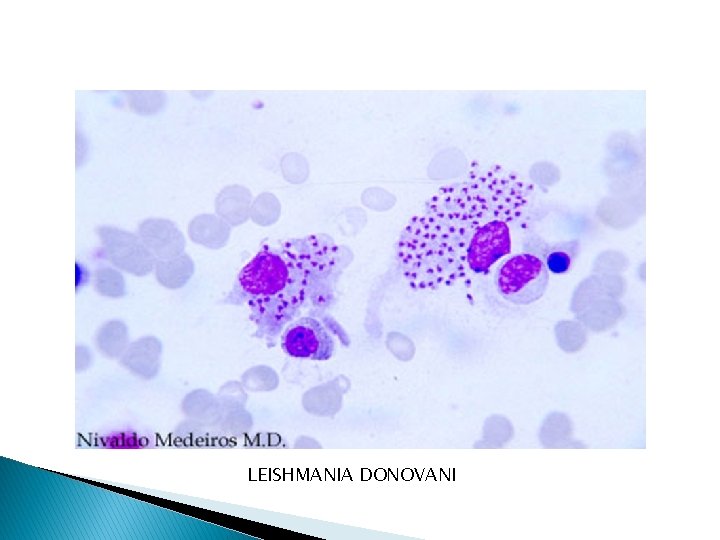
LEISHMANIA DONOVANI
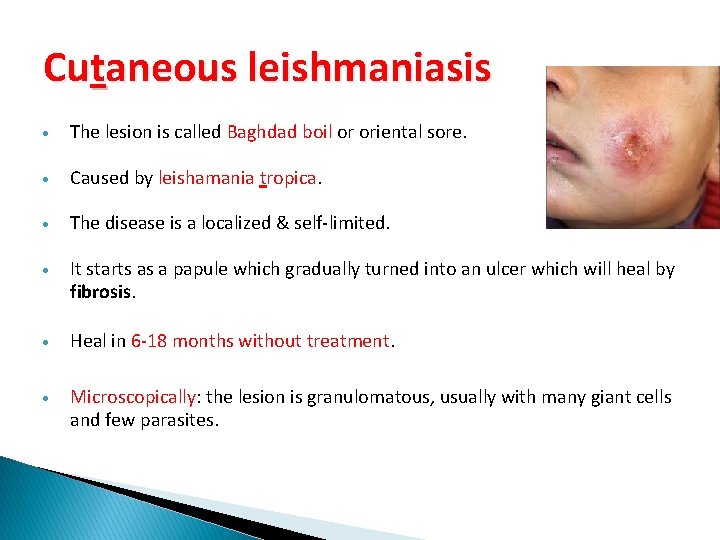
Cutaneous leishmaniasis The lesion is called Baghdad boil or oriental sore. Caused by leishamania tropica. The disease is a localized & self-limited. It starts as a papule which gradually turned into an ulcer which will heal by fibrosis. Heal in 6 -18 months without treatment. Microscopically: the lesion is granulomatous, usually with many giant cells and few parasites.

Mucocutaneous leishmaniasis Caused by leishmania braziliensis The lesions are at the mucocutaneous junction e. g nose, upper lip. The lesion doesn’t heal spontaneously, but it progresses and erodes the skin, mucous membrane and even the cartilage causing a gross disfigurement. Mic. : granuloma formation.
Amoebiasis � Cause: � Site: Entamoeba histolytica. ◦ 1. Colon: amoebic dysentery. ◦ 2. Extraintestinal: liver and lung abscesses.
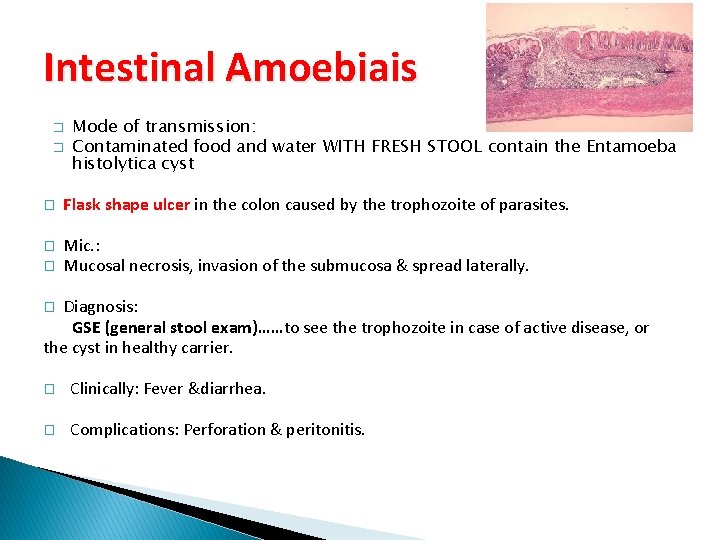
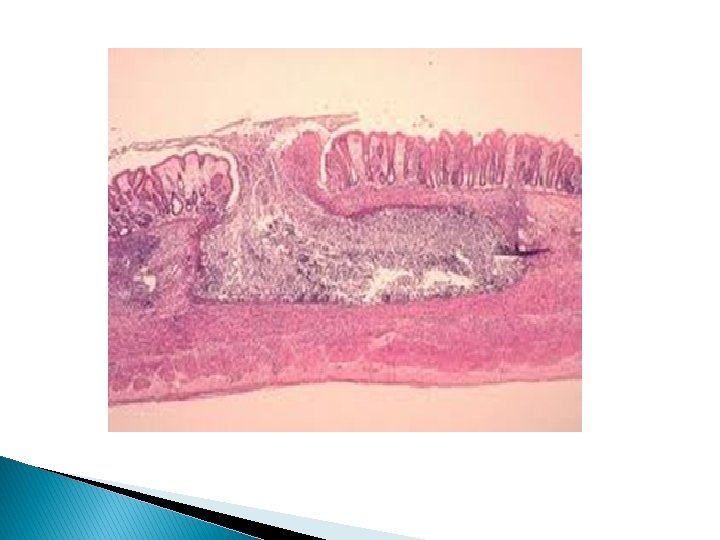
Intestinal Amoebiais � � Mode of transmission: Contaminated food and water WITH FRESH STOOL contain the Entamoeba histolytica cyst � Flask shape ulcer in the colon caused by the trophozoite of parasites. � Mic. : Mucosal necrosis, invasion of the submucosa & spread laterally. � Diagnosis: GSE (general stool exam)……to see the trophozoite in case of active disease, or the cyst in healthy carrier. � � Clinically: Fever &diarrhea. � Complications: Perforation & peritonitis.
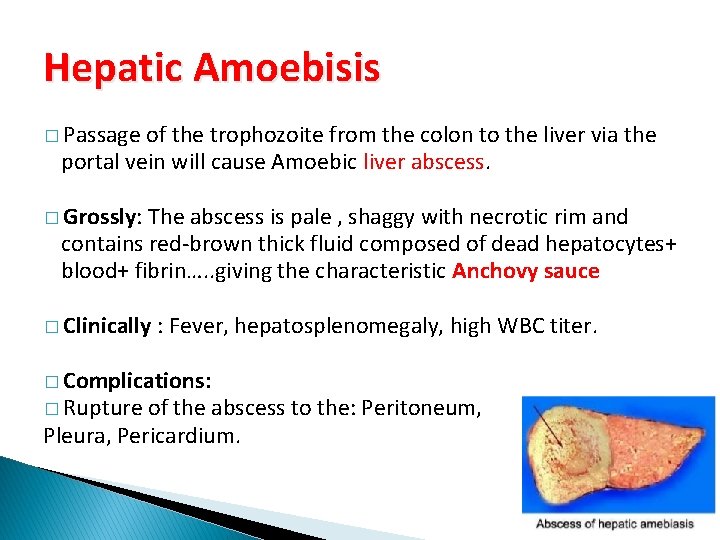
Hepatic Amoebisis � Passage of the trophozoite from the colon to the liver via the portal vein will cause Amoebic liver abscess. � Grossly: The abscess is pale , shaggy with necrotic rim and contains red-brown thick fluid composed of dead hepatocytes+ blood+ fibrin…. . giving the characteristic Anchovy sauce � Clinically : Fever, hepatosplenomegaly, high WBC titer. � Complications: � Rupture of the abscess to the: Peritoneum, Pleura, Pericardium.

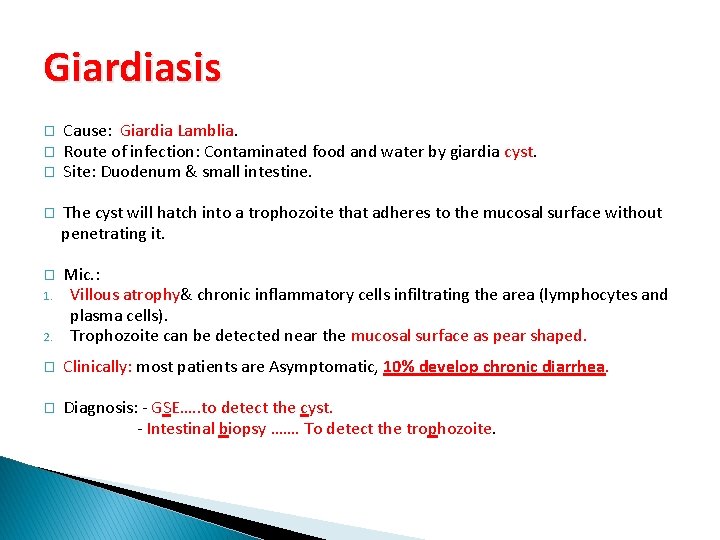
Giardiasis � � � Cause: Giardia Lamblia. Route of infection: Contaminated food and water by giardia cyst. Site: Duodenum & small intestine. � The cyst will hatch into a trophozoite that adheres to the mucosal surface without penetrating it. � 2. Mic. : Villous atrophy& chronic inflammatory cells infiltrating the area (lymphocytes and plasma cells). Trophozoite can be detected near the mucosal surface as pear shaped. � Clinically: most patients are Asymptomatic, 10% develop chronic diarrhea. � Diagnosis: - GSE…. . to detect the cyst. - Intestinal biopsy ……. To detect the trophozoite. 1.
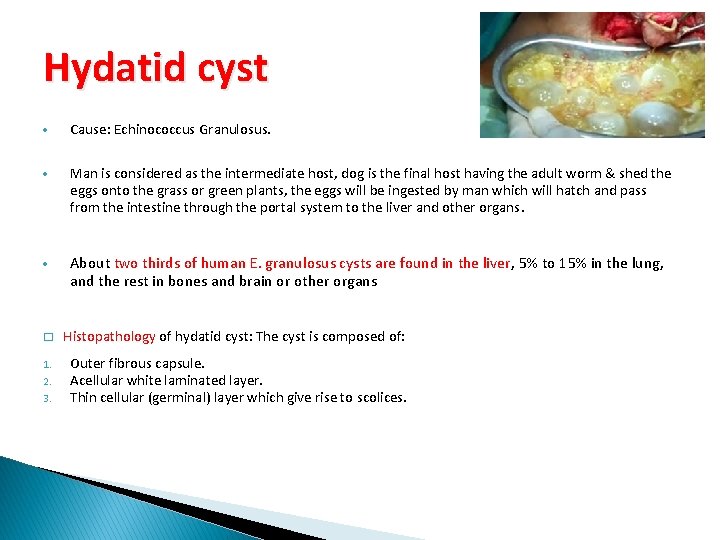
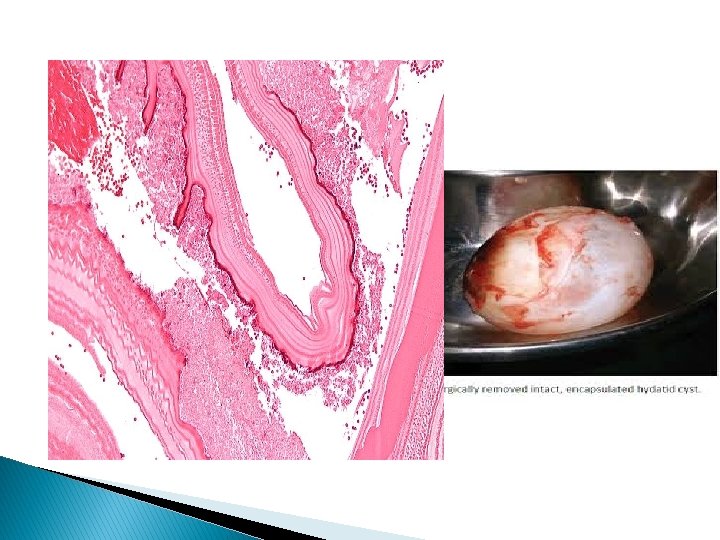
Hydatid cyst Cause: Echinococcus Granulosus. Man is considered as the intermediate host, dog is the final host having the adult worm & shed the eggs onto the grass or green plants, the eggs will be ingested by man which will hatch and pass from the intestine through the portal system to the liver and other organs. About two thirds of human E. granulosus cysts are found in the liver, 5% to 15% in the lung, and the rest in bones and brain or other organs � Histopathology of hydatid cyst: The cyst is composed of: 1. Outer fibrous capsule. Acellular white laminated layer. Thin cellular (germinal) layer which give rise to scolices. 2. 3.
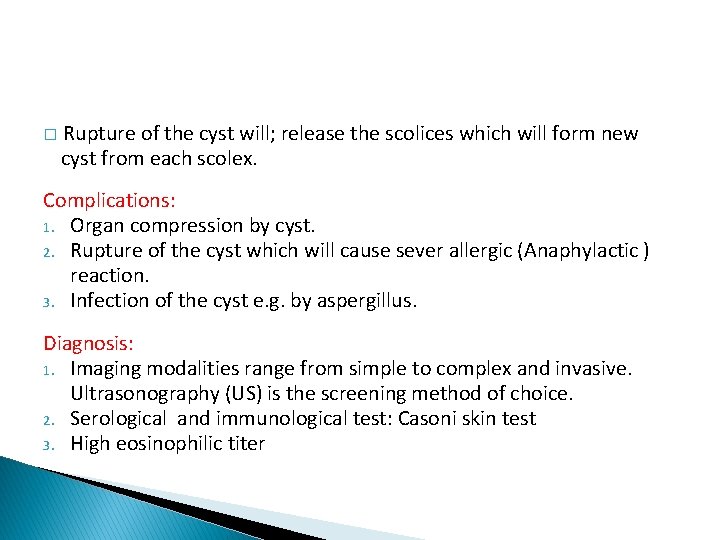
� Rupture of the cyst will; release the scolices which will form new cyst from each scolex. Complications: 1. Organ compression by cyst. 2. Rupture of the cyst which will cause sever allergic (Anaphylactic ) reaction. 3. Infection of the cyst e. g. by aspergillus. Diagnosis: 1. Imaging modalities range from simple to complex and invasive. Ultrasonography (US) is the screening method of choice. 2. Serological and immunological test: Casoni skin test 3. High eosinophilic titer
Schistosomiasis (bilhariziasis) caused by: � Schistosoma hematobium give urinary diseases. � Schistosoma mansoni and schistosoma japanicum give liver and intestinal disease. � � Schistosomiasis is transmitted by freshwater snails that live in the slowmoving water. Infectious schistosome is the larva (cercariae). Larvae (cercariae) penetrate human skin, migrate through the vasculature, to the lungs and the liver where the adult worm live, then to a specific organs where they can stay for many years and can lay thousands of eggs per day If they settle in the urinary bladder (S. haematobium) or portal venous systems (all others).
Clinical presentation Early presentation itchy rash (swimmer’s rash) at site of penetration through the skin. Constitutional symptoms: fever, diarrhea, cough…. etc. Late presentation depending on the organ they affect Urinary bladder: hematuria, bladder hardening due to fibrosis Intestine: abdominal pain, diarrhea, blood in stool. Liver: A granuloma formation around the implanted eggs which will heal by fibrosis , this will cause obstruction of the portal system causing the shift of blood to the systemic circulation ending in esophageal varices and hematamesis (vomiting of blood). � Microscopically: calcified egg deposition and granulomas formation or fibrosis around the eggs. Note: Urinary schistosomiasis is also associated with urinary bladder surface epithelial squamous metaplasia then dysplasia and squamous cell carcinoma. �


- Slides: 44