Infectious and Inflammatory Processes of the Temporal Bone
Infectious and Inflammatory Processes of the Temporal Bone Neelmini Emmanuel, MD 1 and John L. Go, MD, FACR 1, 2, 3 Division of Neuroradiology 1 and Departments of Radiology 2 and Otolaryngology Keck School of Medicine University of Southern California House Ear Clinic 3 of St. Vincent Medical Center Los Angeles, CA
Purpose n This exhibit will familiarize the attendees with the infectious and inflammatory disorders of the temporal bone
Design: This exhibit will divide and explore the infectious and inflammatory disorders of the temporal bone by region and disease entities within each region : n Pinna and External Auditory Canal (EAC) otitis externa n Chronic otitis externa n EAC cholesteatoma/keratos is obturans n n n Acute n Middle ear cavity (MEC) n Acute otitis media n Chronic otitis media n Cholesteatoma Mastoid region n Petrous apex n n n Simple mastoiditis Coalescent mastoiditis Complications of mastoiditis Petrous apicitis Cholesterol granuloma Inner Ear n n Labyrinthitis ossificans
Pinna and EAC n Otitis externa may be subdivided into acute and chronic otitis externa. Acute otitis externa is inflammation of the soft tissue of the external auditory canal. With repeated episodes of inflammation and periostitis, concentric narrowing of the external auditory canal may form. This is commonly referred to as surfer’s ear, and is an example of chronic otitis externa. Soft tissue may fill the external auditory canal, leading to medial meatal fibrosis. n Malignant otitis externa refers to inflammation away from the external auditory canal, typically inferior to the EAC. The fissures of Santorini represent small channels containing veins draining the EAC. Thrombophlebitis of these veins leads to extension of infection below the EAC.
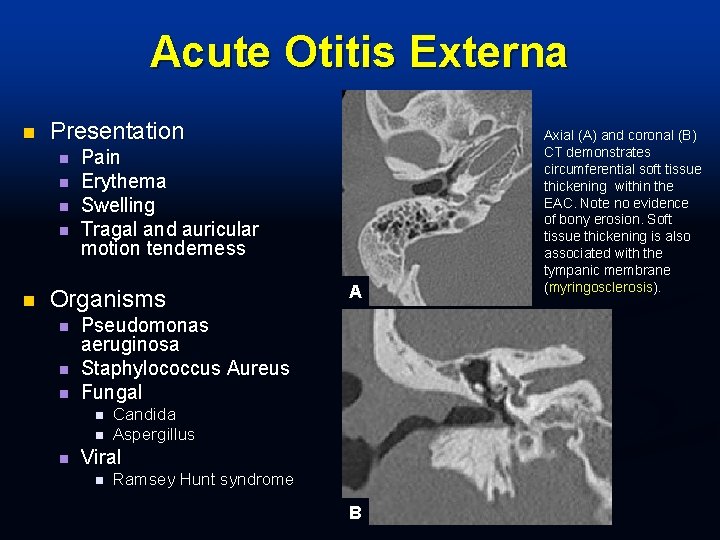
Acute Otitis Externa n Presentation n n Pain Erythema Swelling Tragal and auricular motion tenderness Organisms n n n Pseudomonas aeruginosa Staphylococcus Aureus Fungal n n n A Candida Aspergillus Viral n Ramsey Hunt syndrome B Axial (A) and coronal (B) CT demonstrates circumferential soft tissue thickening within the EAC. Note no evidence of bony erosion. Soft tissue thickening is also associated with the tympanic membrane (myringosclerosis).
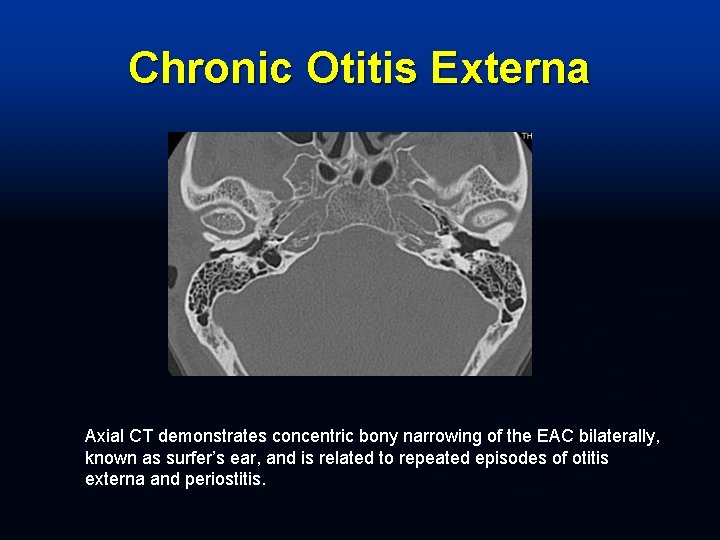
Chronic Otitis Externa Axial CT demonstrates concentric bony narrowing of the EAC bilaterally, known as surfer’s ear, and is related to repeated episodes of otitis externa and periostitis.
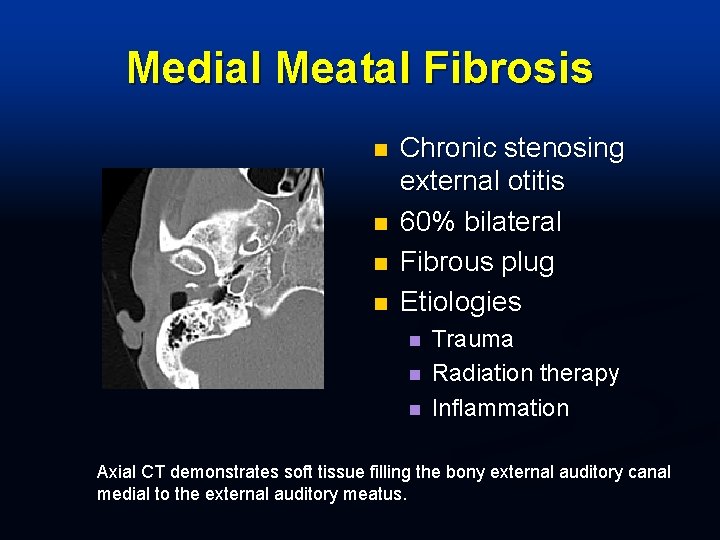
Medial Meatal Fibrosis n n Chronic stenosing external otitis 60% bilateral Fibrous plug Etiologies n n n Trauma Radiation therapy Inflammation Axial CT demonstrates soft tissue filling the bony external auditory canal medial to the external auditory meatus.
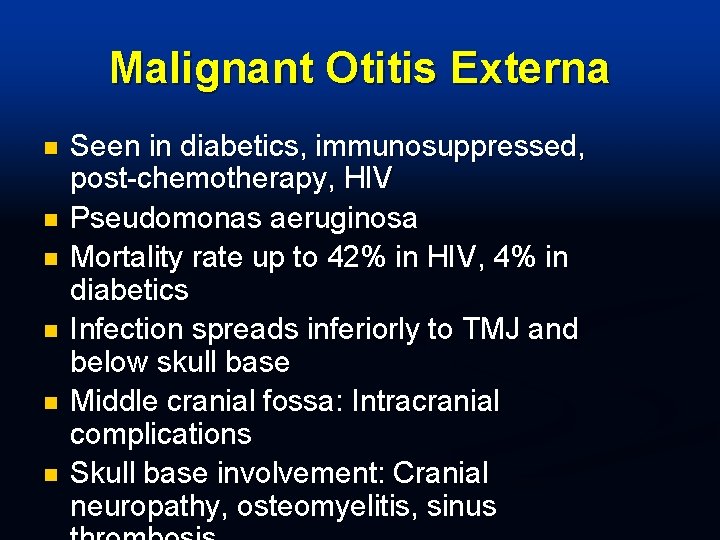
Malignant Otitis Externa n n n Seen in diabetics, immunosuppressed, post-chemotherapy, HIV Pseudomonas aeruginosa Mortality rate up to 42% in HIV, 4% in diabetics Infection spreads inferiorly to TMJ and below skull base Middle cranial fossa: Intracranial complications Skull base involvement: Cranial neuropathy, osteomyelitis, sinus

Malignant Otitis Externa A B Non-contrast axial CT at the level of the left EAC (A) and 1 cm inferior (B) demonstrating soft tissue mass filling EAC with bony erosion of EAC. Note inflammatory changes associated with the parotid, masticator and parapharyangeal spaces (red arrow).
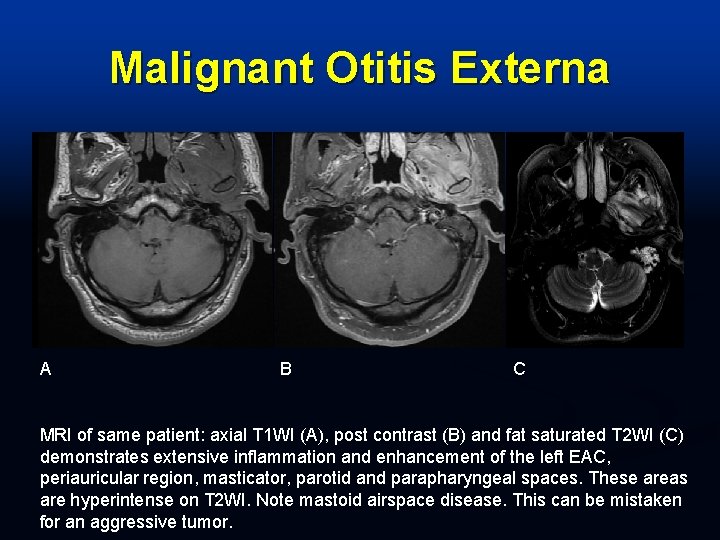
Malignant Otitis Externa A B C MRI of same patient: axial T 1 WI (A), post contrast (B) and fat saturated T 2 WI (C) demonstrates extensive inflammation and enhancement of the left EAC, periauricular region, masticator, parotid and parapharyngeal spaces. These areas are hyperintense on T 2 WI. Note mastoid airspace disease. This can be mistaken for an aggressive tumor.
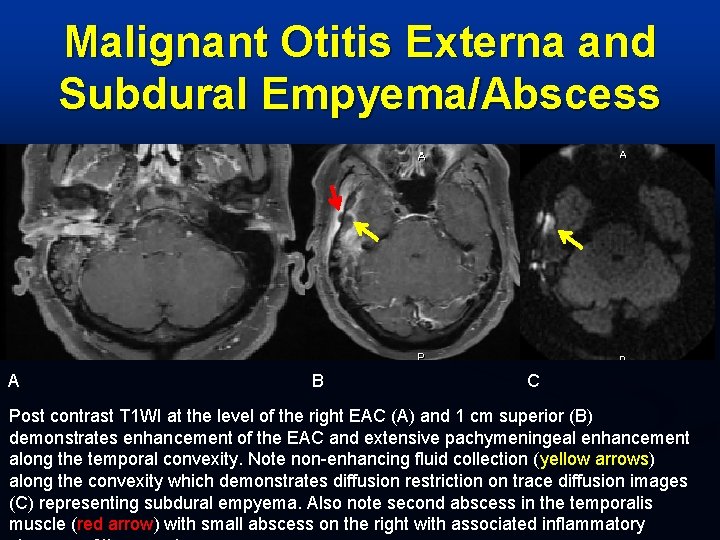
Malignant Otitis Externa and Subdural Empyema/Abscess A B C Post contrast T 1 WI at the level of the right EAC (A) and 1 cm superior (B) demonstrates enhancement of the EAC and extensive pachymeningeal enhancement along the temporal convexity. Note non-enhancing fluid collection (yellow arrows) along the convexity which demonstrates diffusion restriction on trace diffusion images (C) representing subdural empyema. Also note second abscess in the temporalis muscle (red arrow) with small abscess on the right with associated inflammatory
EAC Cholesteatoma 10% of acquired cholesteatomas occur in the external auditory canal n Represent a ball of keratinized, desquamated epithelial cells n May be associated with prior perforation of the tympanic membrane n Soft tissue mass associated with adjacent bony destruction n
EAC Cholesteatoma n CT n n Soft tissue mass with associated bony destruction MRI T 1 WI: iso- to hypointense in signal intensity n T 2 WI: mild to moderate hyperintense signal intensity n Post contrast imaging: No enhancement n Diffusion imaging: restricted diffusion n
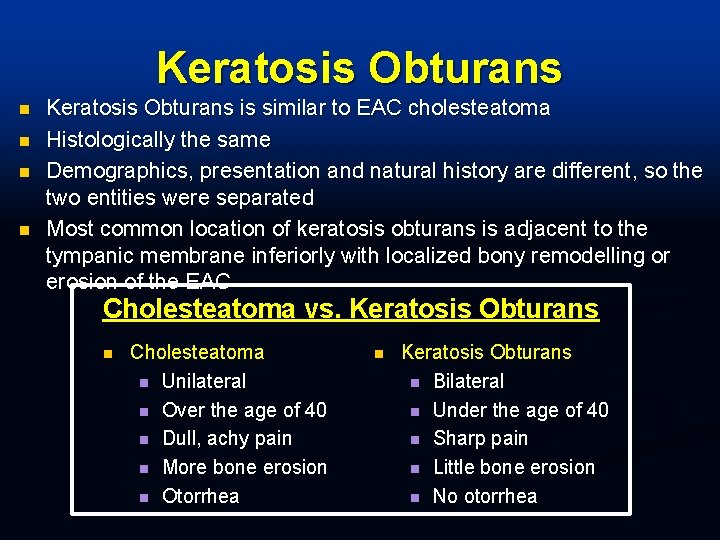
Keratosis Obturans n n Keratosis Obturans is similar to EAC cholesteatoma Histologically the same Demographics, presentation and natural history are different, so the two entities were separated Most common location of keratosis obturans is adjacent to the tympanic membrane inferiorly with localized bony remodelling or erosion of the EAC Cholesteatoma vs. Keratosis Obturans n Cholesteatoma n Unilateral n Over the age of 40 n Dull, achy pain n More bone erosion n Otorrhea n Keratosis Obturans n Bilateral n Under the age of 40 n Sharp pain n Little bone erosion n No otorrhea
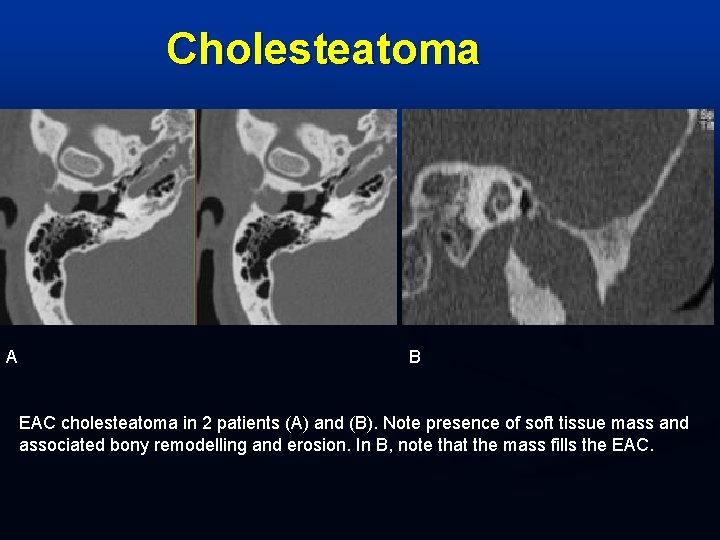
Cholesteatoma A B EAC cholesteatoma in 2 patients (A) and (B). Note presence of soft tissue mass and associated bony remodelling and erosion. In B, note that the mass fills the EAC.
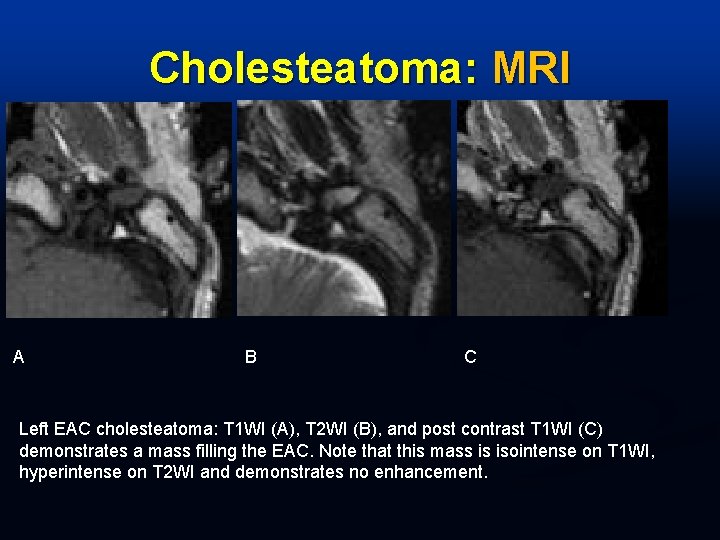
Cholesteatoma: MRI A B C Left EAC cholesteatoma: T 1 WI (A), T 2 WI (B), and post contrast T 1 WI (C) demonstrates a mass filling the EAC. Note that this mass is isointense on T 1 WI, hyperintense on T 2 WI and demonstrates no enhancement.
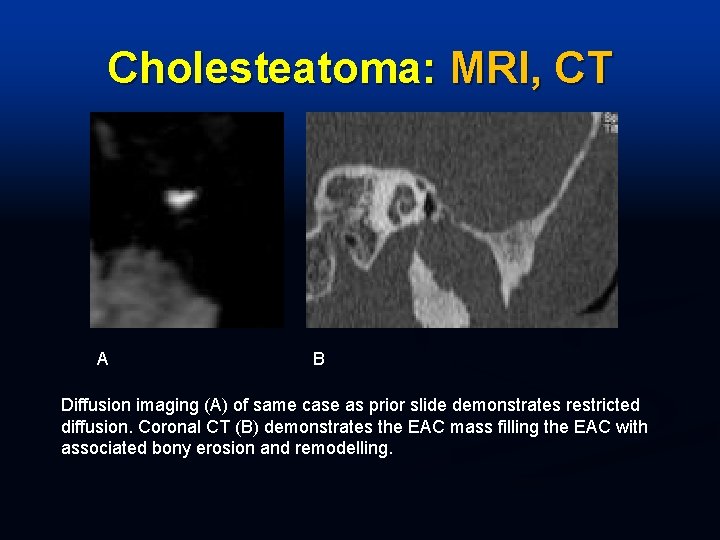
Cholesteatoma: MRI, CT A B Diffusion imaging (A) of same case as prior slide demonstrates restricted diffusion. Coronal CT (B) demonstrates the EAC mass filling the EAC with associated bony erosion and remodelling.
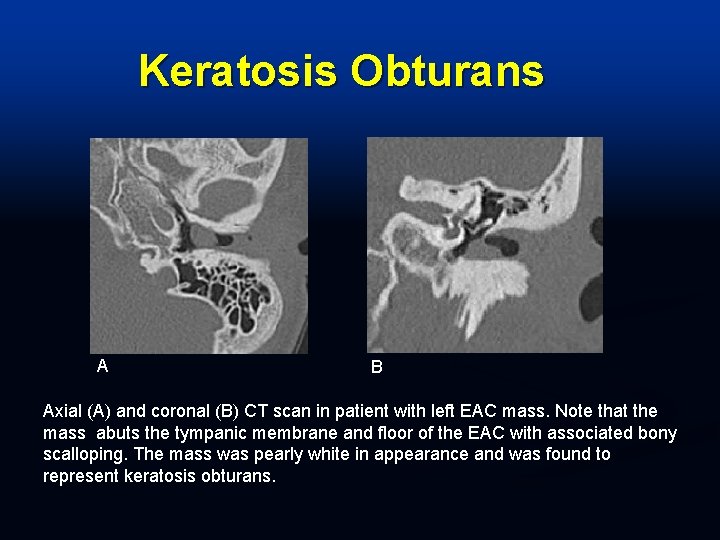
Keratosis Obturans A B Axial (A) and coronal (B) CT scan in patient with left EAC mass. Note that the mass abuts the tympanic membrane and floor of the EAC with associated bony scalloping. The mass was pearly white in appearance and was found to represent keratosis obturans.
n Middle Ear Cavity n n n Acute otitis media (AOM) Chronic otitis media (COM) Cholesteatoma Tympanosclerosis Inflammation within the middle ear cavity may represent acute otitis media, chronic otitis media, or cholesteatoma. n Effusion within the middle ear cavity does not equal acute OM. n Effusion within the middle ear cavity with signs of infection (otalgia, fever, elevated WBC, ESR or CRP) is indicative of infection. n
Acute Otitis Media n Bacterial infection Streptococcus pneumoniae n Haemophilus influenzae n n Less common, higher incidence of meningitis Proteus n Pseudomonas n n Mycotic infections: unusual
Acute Otitis Media: Imaging n CT imaging Fluid within the MEC n No ossicular erosion n n MR imaging: Fluid signal intensity on MRI Hypointense on T 1 -weighted images n Hyperintense on T 2 -weighted images n No enhancement n No diffusion abnormality n
Chronic Otitis Media Unresolved inflammatory process n TM perforation commonly associated with retraction pockets n Pseudomonas and Staphylococcus infection most common organisms n Highly vascularized granulation tissue present n
Chronic Otitis Media: Imaging n CT imaging Fluid/soft tissue in MEC n Ossicular erosion or disruption may be present n n MR imaging Post contrast images demonstrate enhancement n Diffusion imaging: negative n
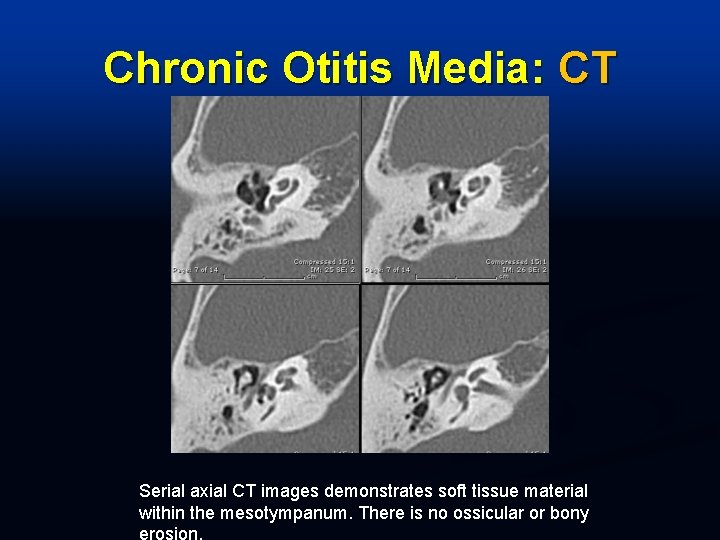
Chronic Otitis Media: CT Serial axial CT images demonstrates soft tissue material within the mesotympanum. There is no ossicular or bony
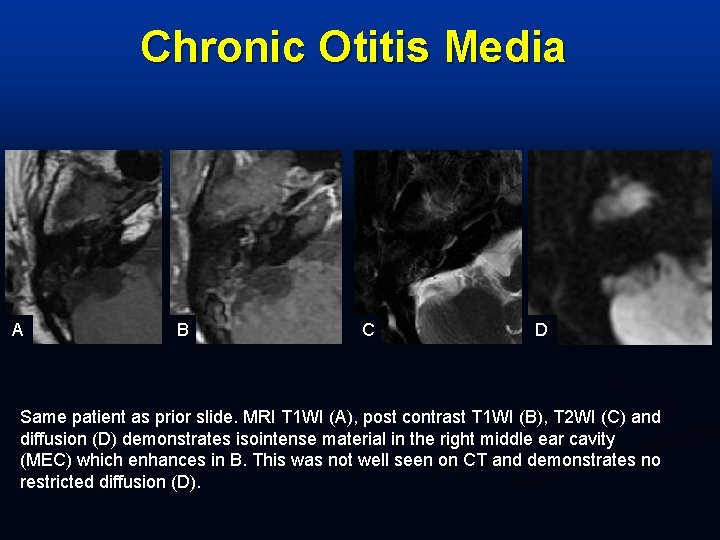
Chronic Otitis Media A B C D Same patient as prior slide. MRI T 1 WI (A), post contrast T 1 WI (B), T 2 WI (C) and diffusion (D) demonstrates isointense material in the right middle ear cavity (MEC) which enhances in B. This was not well seen on CT and demonstrates no restricted diffusion (D).
Middle Ear Cavity Cholesteatoma Imaging similar to epidermoid n CT imaging n n n Soft tissue mass with ossicular/bony erosion MR imaging Hypointense on T 1 -weighted images n Hyperintense on T 2 -weighted images n Post contrast images, no enhancement n Diffusion imaging: Positive n
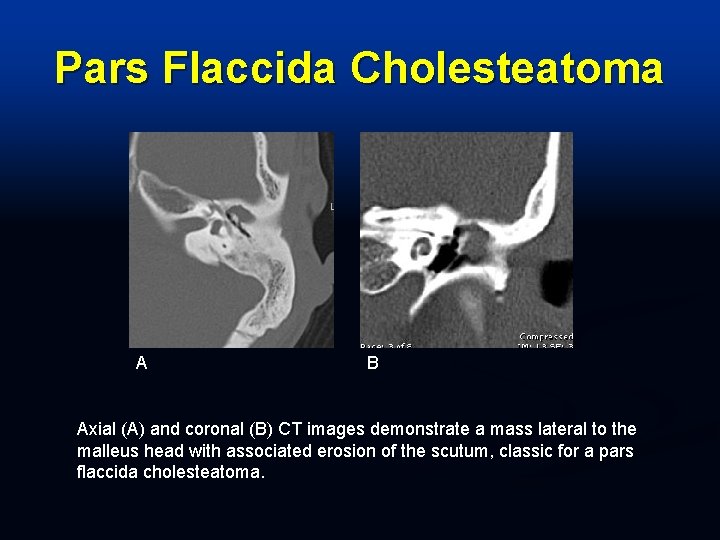
Pars Flaccida Cholesteatoma A B Axial (A) and coronal (B) CT images demonstrate a mass lateral to the malleus head with associated erosion of the scutum, classic for a pars flaccida cholesteatoma.
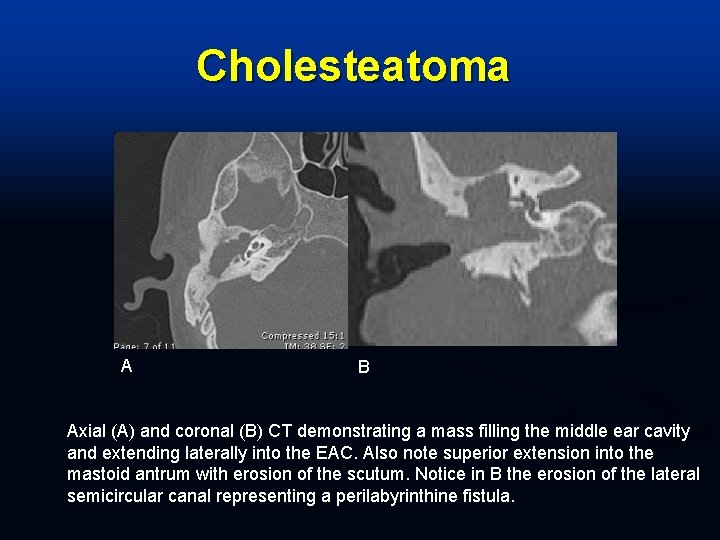
Cholesteatoma A B Axial (A) and coronal (B) CT demonstrating a mass filling the middle ear cavity and extending laterally into the EAC. Also note superior extension into the mastoid antrum with erosion of the scutum. Notice in B the erosion of the lateral semicircular canal representing a perilabyrinthine fistula.
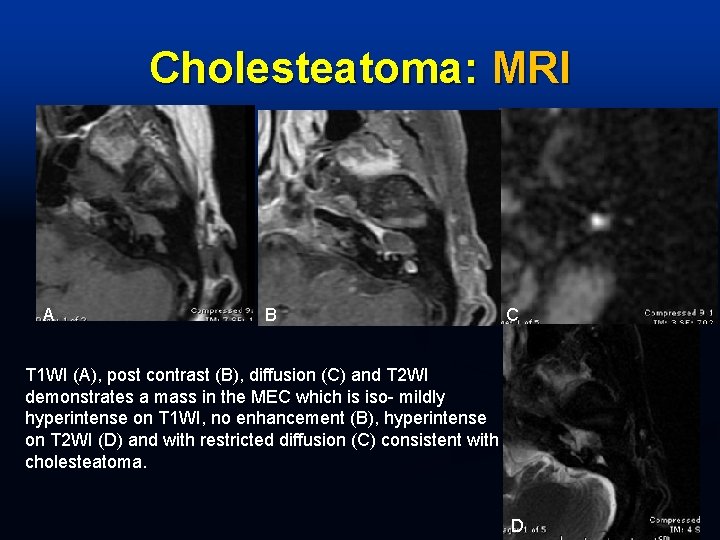
Cholesteatoma: MRI A B C T 1 WI (A), post contrast (B), diffusion (C) and T 2 WI demonstrates a mass in the MEC which is iso- mildly hyperintense on T 1 WI, no enhancement (B), hyperintense on T 2 WI (D) and with restricted diffusion (C) consistent with cholesteatoma. D
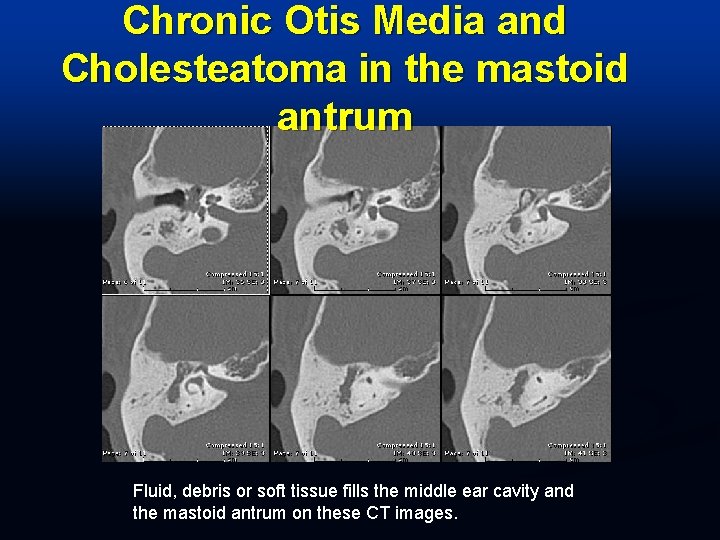
Chronic Otis Media and Cholesteatoma in the mastoid antrum Fluid, debris or soft tissue fills the middle ear cavity and the mastoid antrum on these CT images.
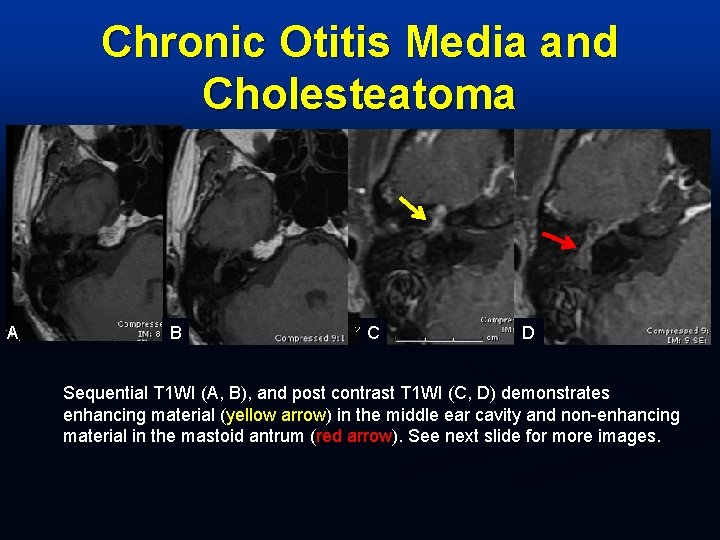
Chronic Otitis Media and Cholesteatoma A B C D Sequential T 1 WI (A, B), and post contrast T 1 WI (C, D) demonstrates enhancing material (yellow arrow) in the middle ear cavity and non-enhancing material in the mastoid antrum (red arrow). See next slide for more images.
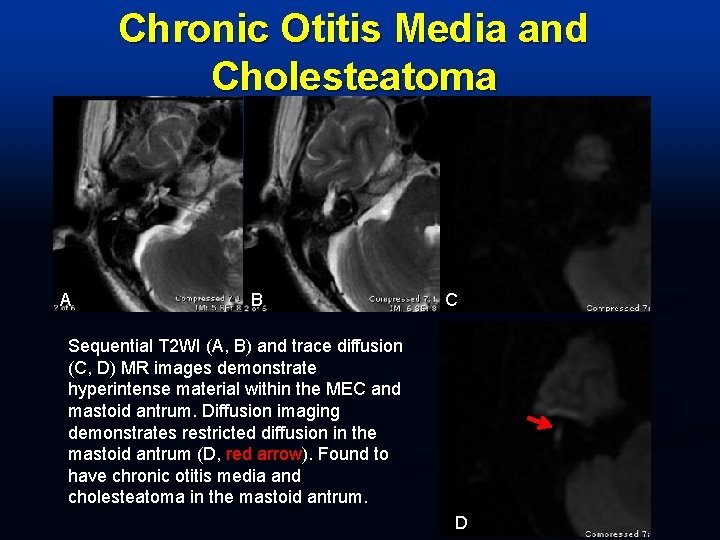
Chronic Otitis Media and Cholesteatoma A B C Sequential T 2 WI (A, B) and trace diffusion (C, D) MR images demonstrate hyperintense material within the MEC and mastoid antrum. Diffusion imaging demonstrates restricted diffusion in the mastoid antrum (D, red arrow). Found to have chronic otitis media and cholesteatoma in the mastoid antrum. D
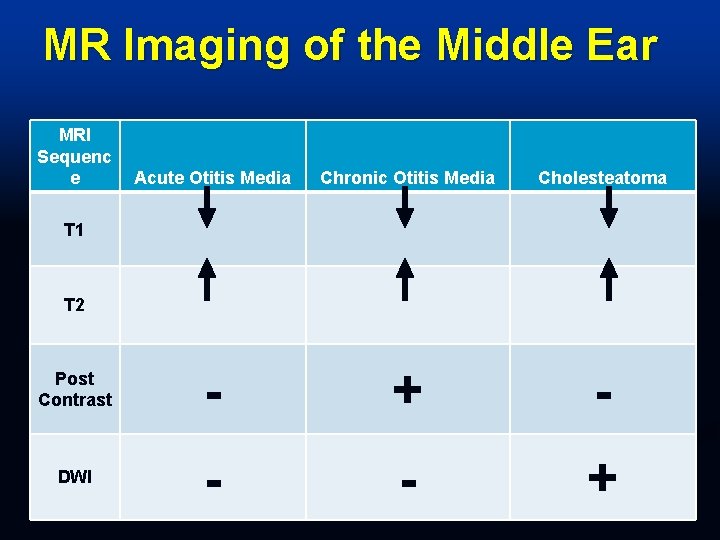
MR Imaging of the Middle Ear MRI Sequenc e Acute Otitis Media Chronic Otitis Media Cholesteatoma Post Contrast - + - DWI - - + T 1 T 2
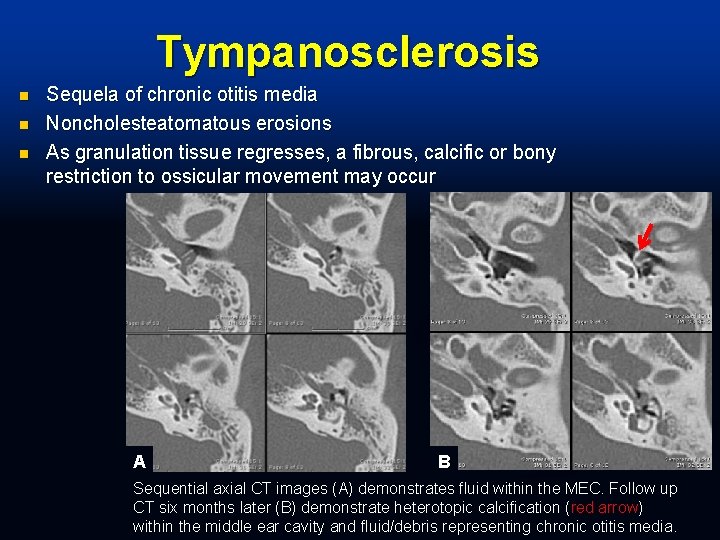
Tympanosclerosis n n n Sequela of chronic otitis media Noncholesteatomatous erosions As granulation tissue regresses, a fibrous, calcific or bony restriction to ossicular movement may occur A B Sequential axial CT images (A) demonstrates fluid within the MEC. Follow up CT six months later (B) demonstrate heterotopic calcification (red arrow) within the middle ear cavity and fluid/debris representing chronic otitis media.
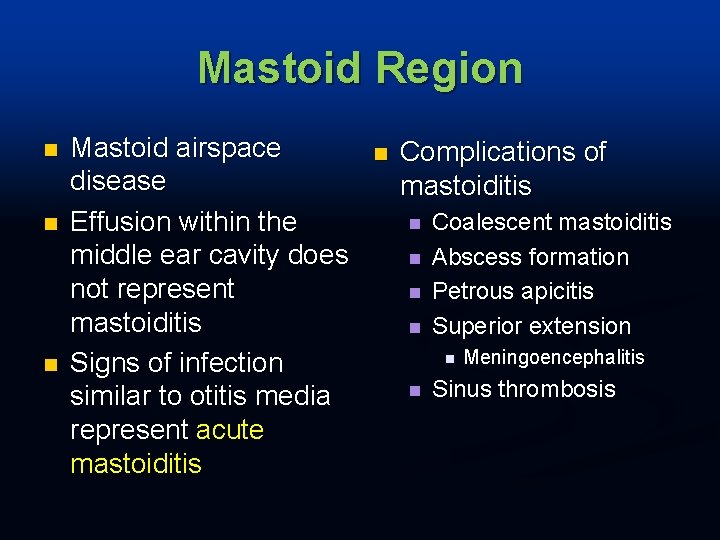
Mastoid Region n Mastoid airspace disease Effusion within the middle ear cavity does not represent mastoiditis Signs of infection similar to otitis media represent acute mastoiditis n Complications of mastoiditis n n Coalescent mastoiditis Abscess formation Petrous apicitis Superior extension n n Meningoencephalitis Sinus thrombosis
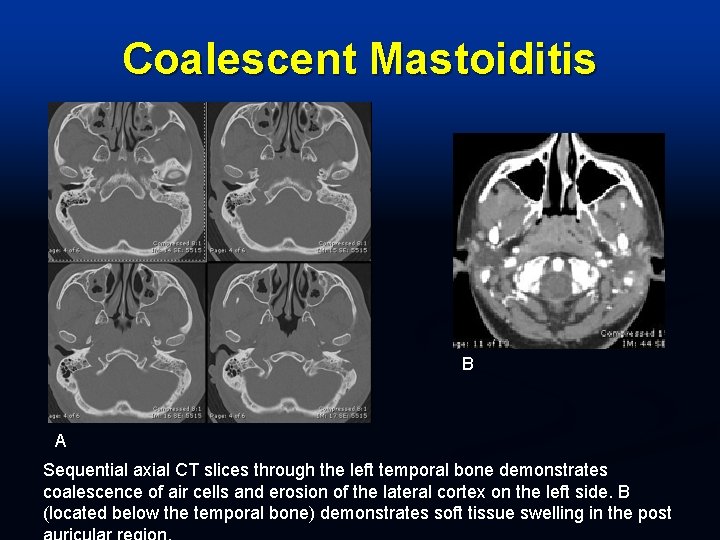
Coalescent Mastoiditis B A Sequential axial CT slices through the left temporal bone demonstrates coalescence of air cells and erosion of the lateral cortex on the left side. B (located below the temporal bone) demonstrates soft tissue swelling in the post
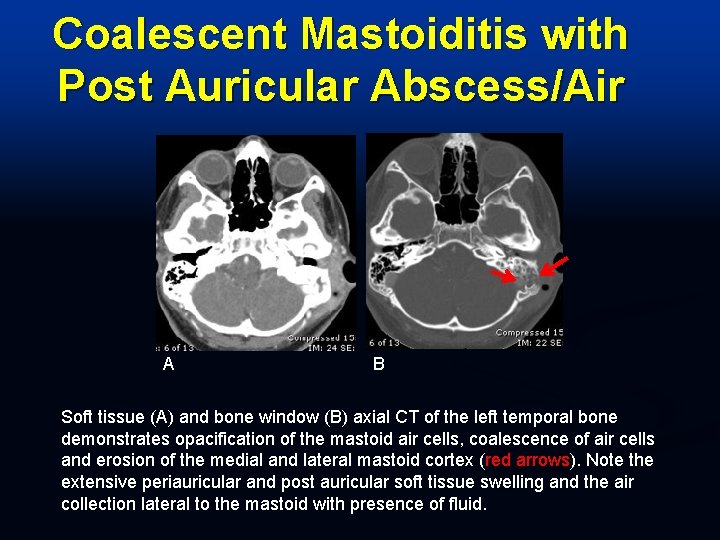
Coalescent Mastoiditis with Post Auricular Abscess/Air A B Soft tissue (A) and bone window (B) axial CT of the left temporal bone demonstrates opacification of the mastoid air cells, coalescence of air cells and erosion of the medial and lateral mastoid cortex (red arrows). Note the extensive periauricular and post auricular soft tissue swelling and the air collection lateral to the mastoid with presence of fluid.
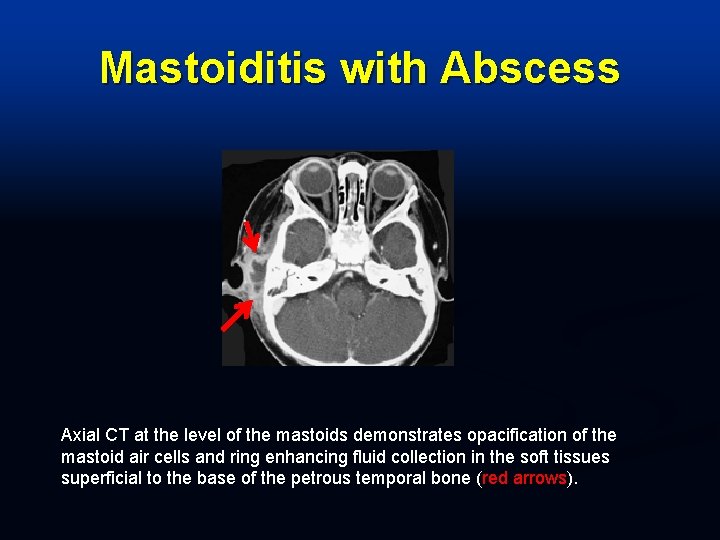
Mastoiditis with Abscess Axial CT at the level of the mastoids demonstrates opacification of the mastoid air cells and ring enhancing fluid collection in the soft tissues superficial to the base of the petrous temporal bone (red arrows).
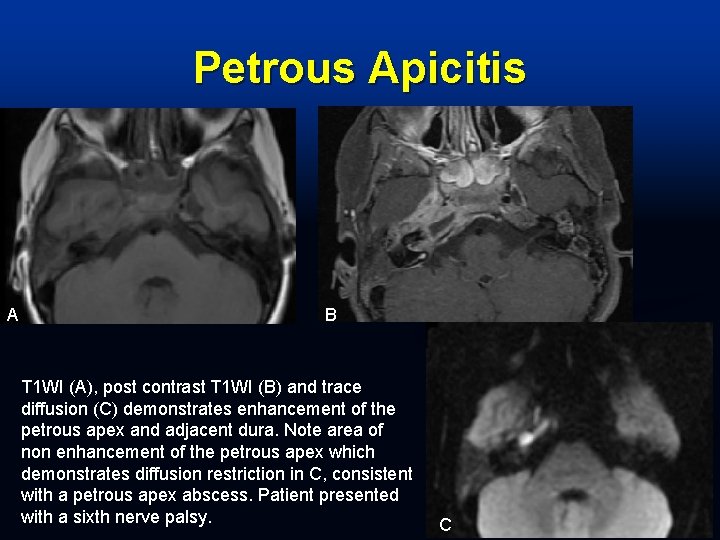
Petrous Apicitis A B T 1 WI (A), post contrast T 1 WI (B) and trace diffusion (C) demonstrates enhancement of the petrous apex and adjacent dura. Note area of non enhancement of the petrous apex which demonstrates diffusion restriction in C, consistent with a petrous apex abscess. Patient presented with a sixth nerve palsy. C
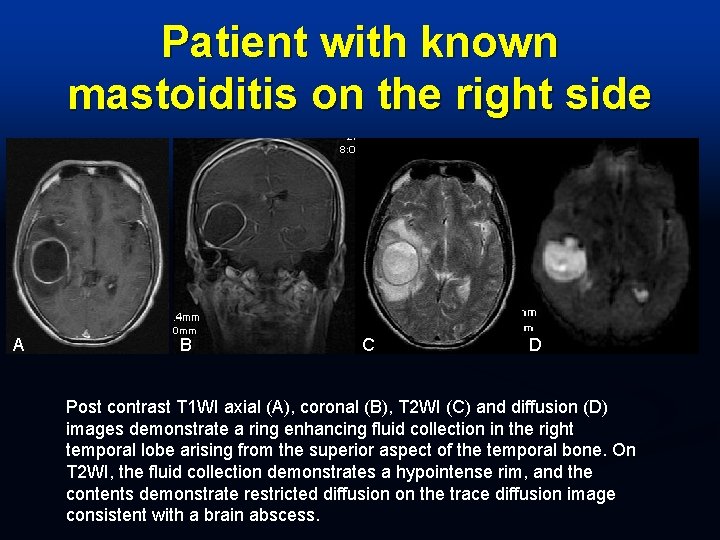
Patient with known mastoiditis on the right side A B C D Post contrast T 1 WI axial (A), coronal (B), T 2 WI (C) and diffusion (D) images demonstrate a ring enhancing fluid collection in the right temporal lobe arising from the superior aspect of the temporal bone. On T 2 WI, the fluid collection demonstrates a hypointense rim, and the contents demonstrate restricted diffusion on the trace diffusion image consistent with a brain abscess.
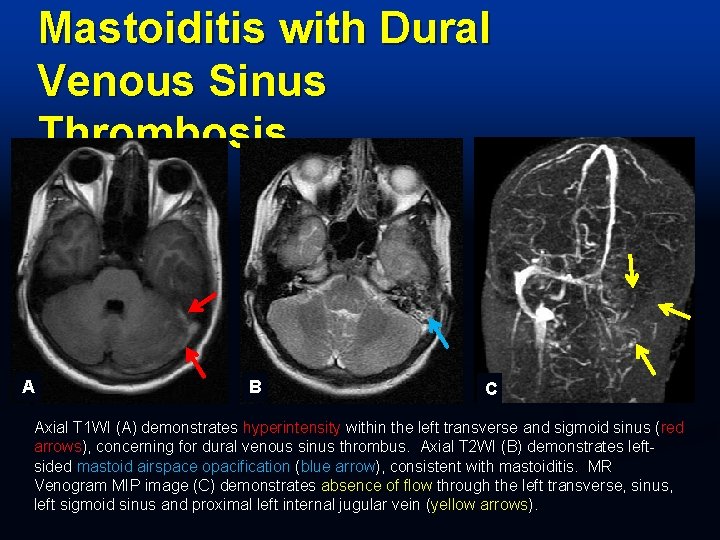
Mastoiditis with Dural Venous Sinus Thrombosis A B C Axial T 1 WI (A) demonstrates hyperintensity within the left transverse and sigmoid sinus (red arrows), concerning for dural venous sinus thrombus. Axial T 2 WI (B) demonstrates leftsided mastoid airspace opacification (blue arrow), consistent with mastoiditis. MR Venogram MIP image (C) demonstrates absence of flow through the left transverse, sinus, left sigmoid sinus and proximal left internal jugular vein (yellow arrows).
Cholesterol Granuloma Expansile lesion, most common petrous apex n May occur in the MEC or mastoids n CT imaging n Expansile without bone destruction n Typically posterior to ICA n n MRI Hyperintense on both T 1 - and T 2 -weighted images n No enhancement n
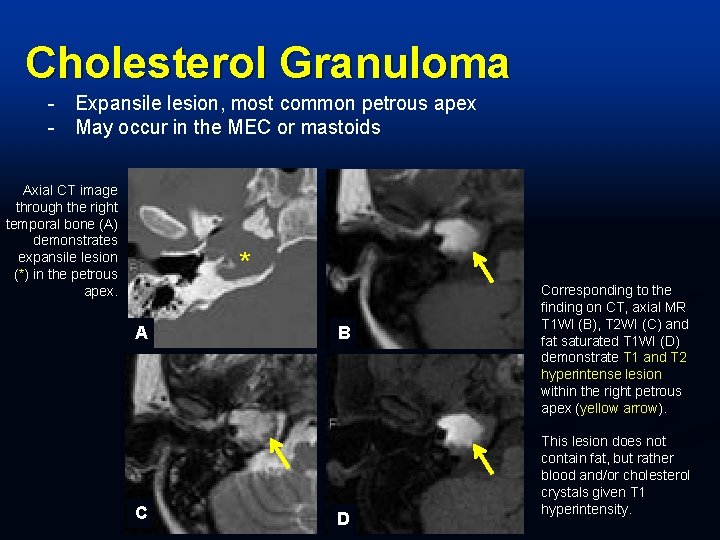
Cholesterol Granuloma - Expansile lesion, most common petrous apex - May occur in the MEC or mastoids Axial CT image through the right temporal bone (A) demonstrates expansile lesion (*) in the petrous apex. * A C B D Corresponding to the finding on CT, axial MR T 1 WI (B), T 2 WI (C) and fat saturated T 1 WI (D) demonstrate T 1 and T 2 hyperintense lesion within the right petrous apex (yellow arrow). This lesion does not contain fat, but rather blood and/or cholesterol crystals given T 1 hyperintensity.
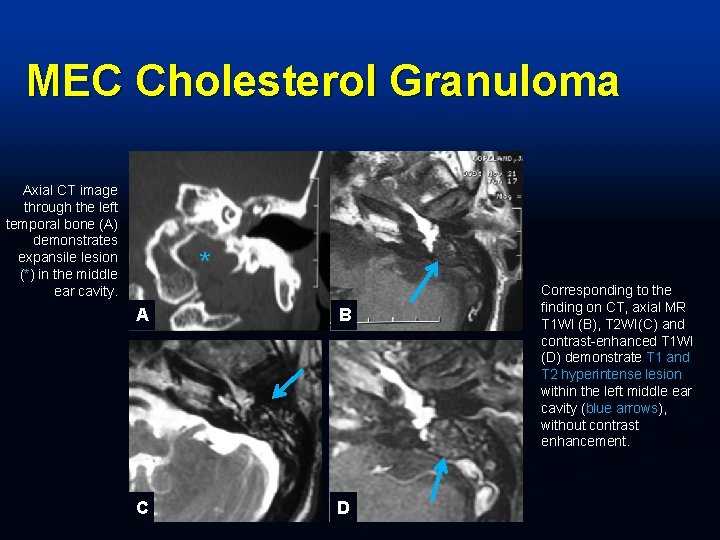
MEC Cholesterol Granuloma Axial CT image through the left temporal bone (A) demonstrates expansile lesion (*) in the middle ear cavity. * A B C D Corresponding to the finding on CT, axial MR T 1 WI (B), T 2 WI(C) and contrast-enhanced T 1 WI (D) demonstrate T 1 and T 2 hyperintense lesion within the left middle ear cavity (blue arrows), without contrast enhancement.
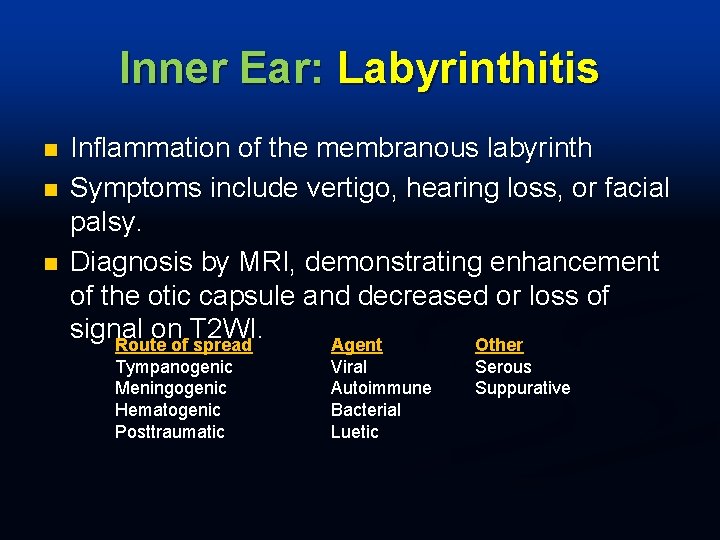
Inner Ear: Labyrinthitis n n n Inflammation of the membranous labyrinth Symptoms include vertigo, hearing loss, or facial palsy. Diagnosis by MRI, demonstrating enhancement of the otic capsule and decreased or loss of signal on T 2 WI. Route of spread Agent Other Tympanogenic Meningogenic Hematogenic Posttraumatic Viral Autoimmune Bacterial Luetic Serous Suppurative
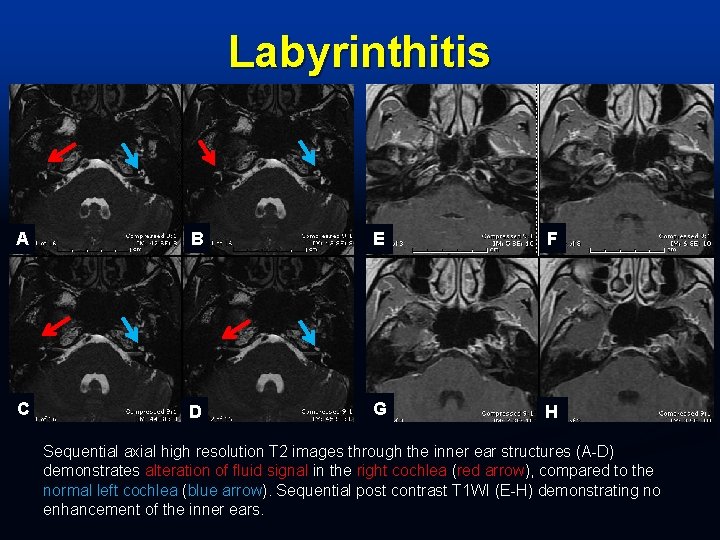
Labyrinthitis A B E F C D G H Sequential axial high resolution T 2 images through the inner ear structures (A-D) demonstrates alteration of fluid signal in the right cochlea (red arrow), compared to the normal left cochlea (blue arrow). Sequential post contrast T 1 WI (E-H) demonstrating no enhancement of the inner ears.
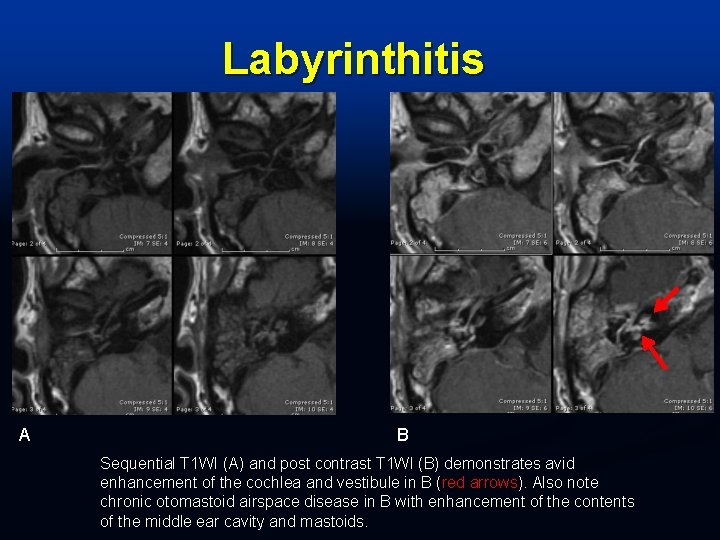
Labyrinthitis A B Sequential T 1 WI (A) and post contrast T 1 WI (B) demonstrates avid enhancement of the cochlea and vestibule in B (red arrows). Also note chronic otomastoid airspace disease in B with enhancement of the contents of the middle ear cavity and mastoids.
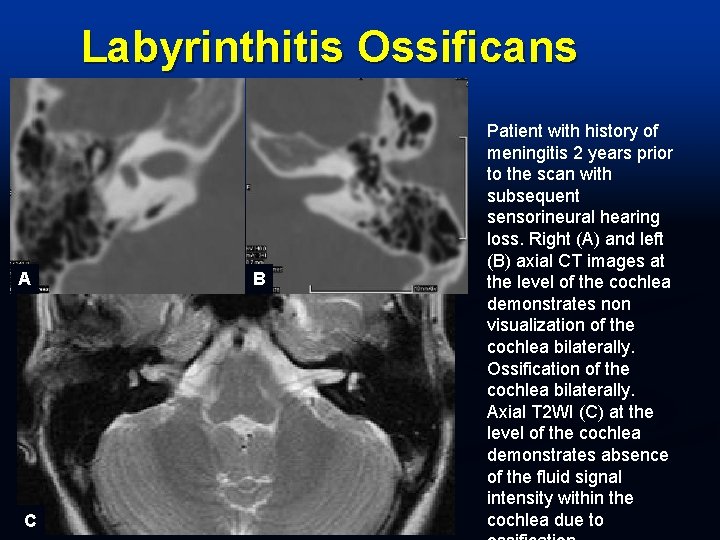
Labyrinthitis Ossificans A C B Patient with history of meningitis 2 years prior to the scan with subsequent sensorineural hearing loss. Right (A) and left (B) axial CT images at the level of the cochlea demonstrates non visualization of the cochlea bilaterally. Ossification of the cochlea bilaterally. Axial T 2 WI (C) at the level of the cochlea demonstrates absence of the fluid signal intensity within the cochlea due to
Conclusion n Infectious and inflammatory disorders may primarily or secondarily involve the temporal bone. This exhibit has systematically described the underlying pathophysiology and imaging findings of these conditions in the various areas of the temporal bone and utility of different imaging modalities in evaluating these entities.
References Aralaşmak A, Dinçer E, Arslan G, Cevikol C, Karaali K. Posttraumatic labyrinthitis ossificans with perilymphatic fistulization. Diagn Interv Radiol. 2009 Dec; 15(4): 239 -41. Booth TN, Roland P, Kutz JW Jr, Lee K, Isaacson B. High-resolution 3 -D T 2 -weighted imaging in the diagnosis of labyrinthitis ossificans: emphasis on subtle cochlear involvement. Pediatr Radiol. 2013 Dec; 43(12): 1584 -90. Dubrulle F, Kohler R, Vincent C, Puech P, Ernst O. Differential diagnosis and prognosis of T 1 -weighted post-gadolinium intralabyrinthine hyperintensities. Eur Radiol. 2010 Nov; 20(11): 2628 -36. Lemmerling MM, De Foer B, Verbist BM, Vande. Vyver V. Imaging of inflammatory and infectious diseases in the temporal bone. Neuroimaging Clin N Am. 2009 Aug; 19(3): 321 -37. Migirov L. Computed tomographic versus surgical findings in complicated acute otomastoiditis. Ann Otol Rhinol Laryngol. 2003 Aug; 112(8): 675 -7. Minks DP, Porte M, Jenkins N. Acute mastoiditis--the role of radiology. Clin Radiol. 2013 Apr; 68(4): 397 -405. Park SY, Jung YH, Oh JH. Clinical characteristics of keratosis obturans and external auditory canal cholesteatoma. Otolaryngol Head Neck Surg. 2015 Feb; 152(2): 326 -30. Petrovic BD, Futterer SF, Hijaz T, Russell EJ, Karagianis AG. Frequency and diagnostic utility of intralabyrinthine FLAIR hyperintensity in the evaluation of internal auditory canal and inner ear pathology. Acad Radiol. 2010 Aug; 17(8): 992 -1000. Saat R, Laulajainen-Hongisto AH, Mahmood G, Lempinen LJ, Aarnisalo AA, Markkola AT, Jero JP. MR imaging features of acute mastoiditis and their clinical relevance. AJNR Am J Neuroradiol. 2015 Feb; 36(2): 361 -7. Scrafton DK, Qureishi A, Nogueira C, Mortimore S. Luc's abscess as an unlucky complication of mastoiditis. Ann R Coll Surg Engl. 2014 Jul; 96(5). Shemesh S, Marom T, Raichman DB, Tamir SO. Dural enhancement and thickening in acute mastoiditis. Neuroradiol J. 2015 Apr; 28(2): 137 -9.
- Slides: 50