Infections of the Skin Lice Scabies Pinworm Ringworm
Infections of the Skin Lice, Scabies, Pinworm, Ringworm, Impetigo

Bacterial p. 694 (9 th ed) p. 227 -228 (10 th ed) • IMPETIGO CONTAGIOSA— • Appearance: maculovesicular lesion; ruptures easily; crusts form; itchy! • Etiology: Staphylococci • Management: carefully remove crusts with Burrow (bleach)solution; apply topical antibiotic ointment; may need PO or IV antibiotics. • Contagious!--CONTACT precautions indicated if hospitalized.

Bacterial • MRSA: http: //www. cdc. gov/mrsa / • Appearance: often appears as atopic dermatitis in nares and under fingernails Furuncle or Carbuncle • Etiology: Methicillin Resistant Staph Aureus • Management: provide washcloths & towels separate from other family members. Soak in tub with ½ c bleach w/ 5 inches of water. Apply mupirocin (Bactroban) to nares bid for 2 -4 wks. May require I&D and hospitalization

Viral Infections p. 696 9 th ed. p. 229 10 th ed. • Warts • Herpes Simplex type 1 • Herpes Simplex type 2 • Herpes zoster, Shingles • Molluscum contagiosum

Fungal infections p. 228 -30 10 th ed. • Dermatophytoses—Ringworm also referred to as Tinea Capitis, or Tinea Corporis, or Tinea cruris, or Tinea Pedis • Appearance: ring-like shape, scaly, unilateral, non-pruritic except tinea cruris • Etiology: filamentous fungi— Trichophyton, Microsporum, & Epidermophyton • Management: Oral GRISEOFULVIN, topical antifungal creams e. g. clotrimazole; nystatin, or miconazole, wet compresses or soaks
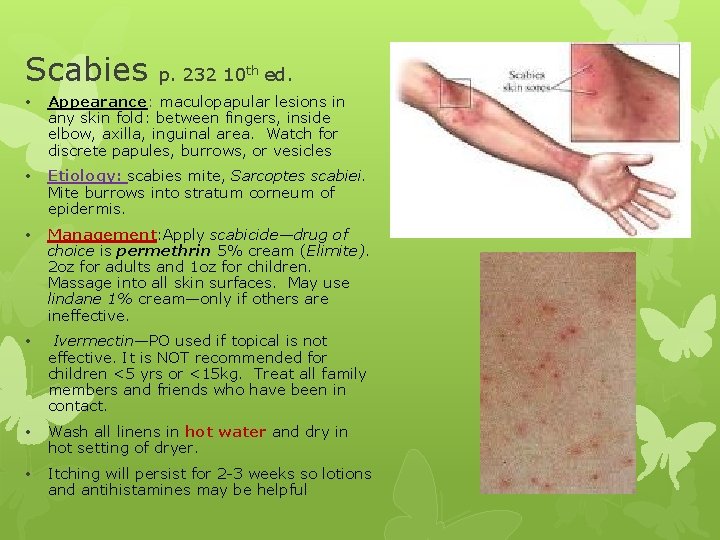
Scabies p. 232 10 th ed. • Appearance: maculopapular lesions in any skin fold: between fingers, inside elbow, axilla, inguinal area. Watch for discrete papules, burrows, or vesicles • Etiology: scabies mite, Sarcoptes scabiei. Mite burrows into stratum corneum of epidermis. • Management: Apply scabicide—drug of choice is permethrin 5% cream (Elimite). 2 oz for adults and 1 oz for children. Massage into all skin surfaces. May use lindane 1% cream—only if others are ineffective. • Ivermectin—PO used if topical is not effective. It is NOT recommended for children <5 yrs or <15 kg. Treat all family members and friends who have been in contact. • Wash all linens in hot water and dry in hot setting of dryer. • Itching will persist for 2 -3 weeks so lotions and antihistamines may be helpful

ENTEROBIASIS— Pinworms p. 620 -1 9 th ed. P. 225 -6 10 th ed. • Appearance: Etiology: nematode Enterobius vermicularis. Crowded conditions, in classrooms and daycare centers favor transmission. • Manifestations: gen’l irritability, restlessnes, poor sleep, bed-wetting, distractibility, short attention span, peranal dermatitis and pruritis, • Diagnosis: Tape test: clear, transparent tape is placed around the end of a tongue depressor. Press firmly against perianal region early in the morning before bath or BM. Place specimen in jar or plastic bag for examination. • Treatment: Anthelmintics are med of choice. (If pyrantel pamoate is RX, teach parents that BM & emesis will be bright red. ) Treat ALL family members with oral med and repeat dose in 2 weeks to eradicate eggs. • Wear pajamas and underwear to sleep, take a bath every day, and wash (not shake) all bedding in HOT water and nightclothes (pajamas) after treatment to help prevent reinfection. .
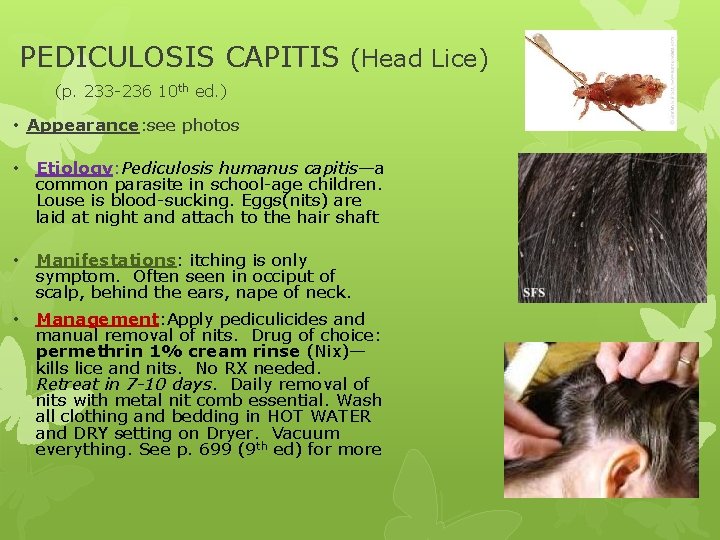
PEDICULOSIS CAPITIS (Head Lice) (p. 233 -236 10 th ed. ) • Appearance: see photos • Etiology: Pediculosis humanus capitis—a common parasite in school-age children. Louse is blood-sucking. Eggs(nits) are laid at night and attach to the hair shaft • Manifestations: itching is only symptom. Often seen in occiput of scalp, behind the ears, nape of neck. • Management: Apply pediculicides and manual removal of nits. Drug of choice: permethrin 1% cream rinse (Nix)— kills lice and nits. No RX needed. Retreat in 7 -10 days. Daily removal of nits with metal nit comb essential. Wash all clothing and bedding in HOT WATER and DRY setting on Dryer. Vacuum everything. See p. 699 (9 th ed) for more

Aren’t you glad to have healthy skin? ? The End
- Slides: 9