Infections of the central nervous system Anna Piekarska

- Slides: 79
Infections of the central nervous system Anna Piekarska MD, Ph. D
Contents 1. Bacterial meningitis 2. Non purulent bacterial meningitis 3. Viral meningitis 4. Viral encephalitis 5. Differential diagnosis between bacterial and viral CNS infections
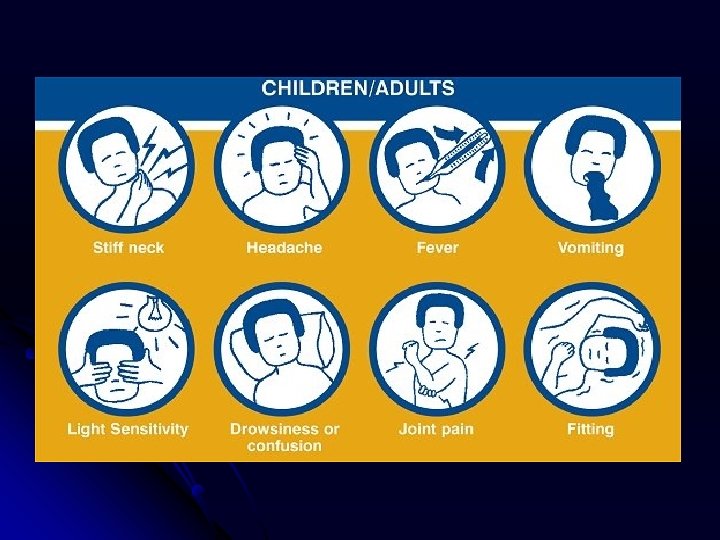
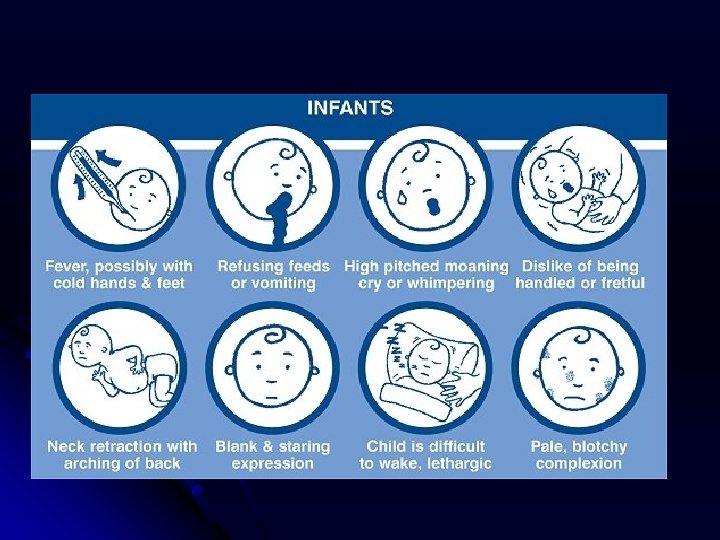
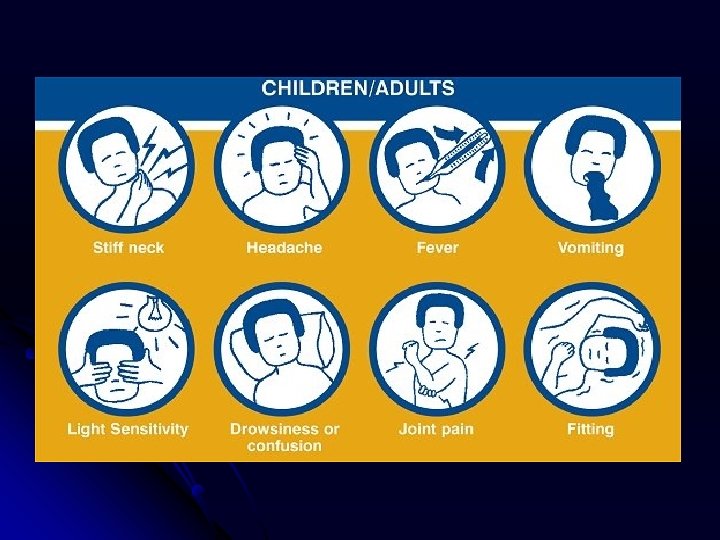
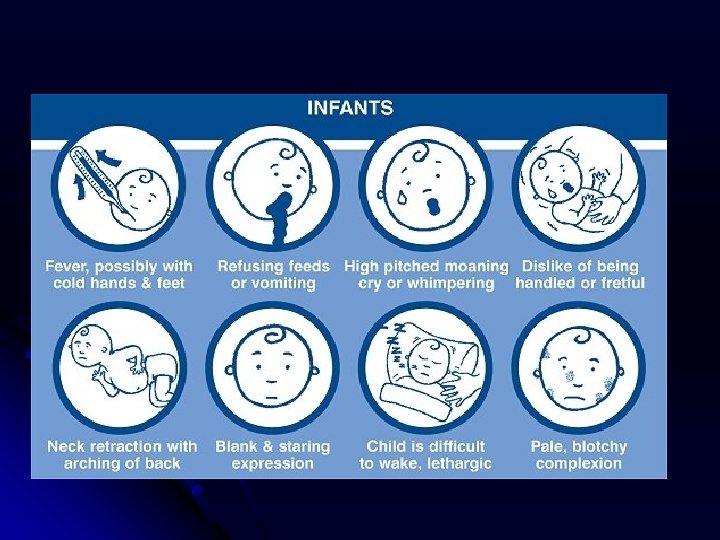
Clinical features of bacterial meningitis Headache over 12 -36 h l Fever over 38°C l Meningism l Nusea and vomiting l Alteration of consciousness l Hematology and biochemistry of the blood is abnormal l
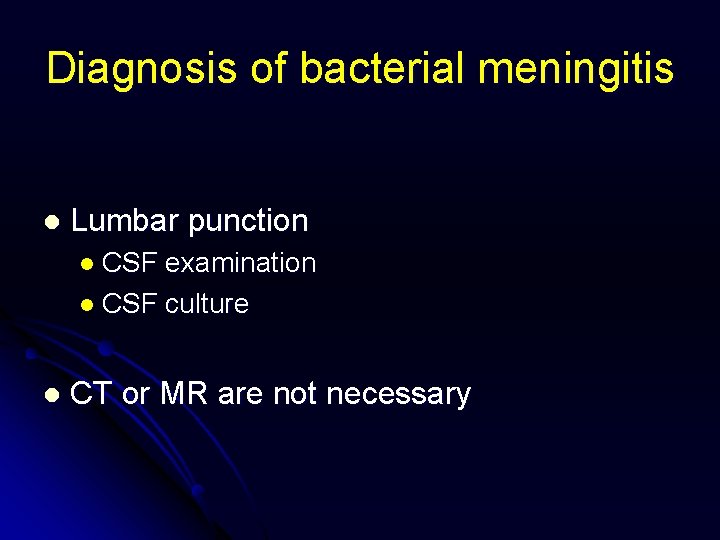
Diagnosis of bacterial meningitis l Lumbar punction l CSF examination l CSF culture l CT or MR are not necessary
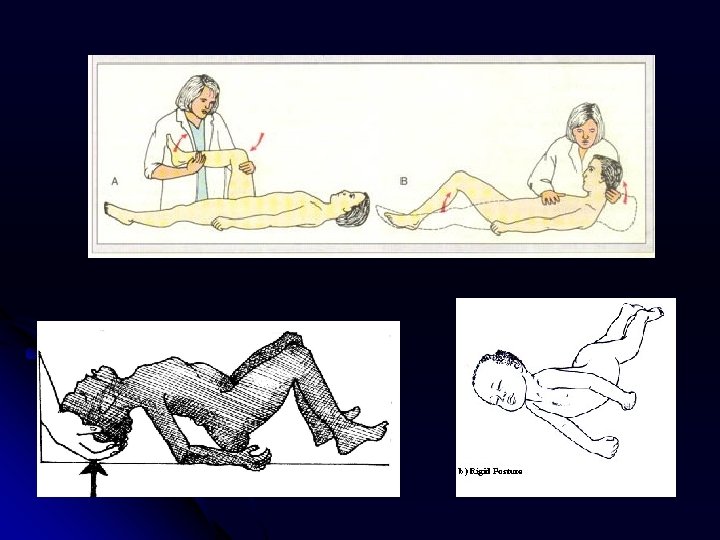
Indications to the lumbar punction Headache + Fever + Meningism
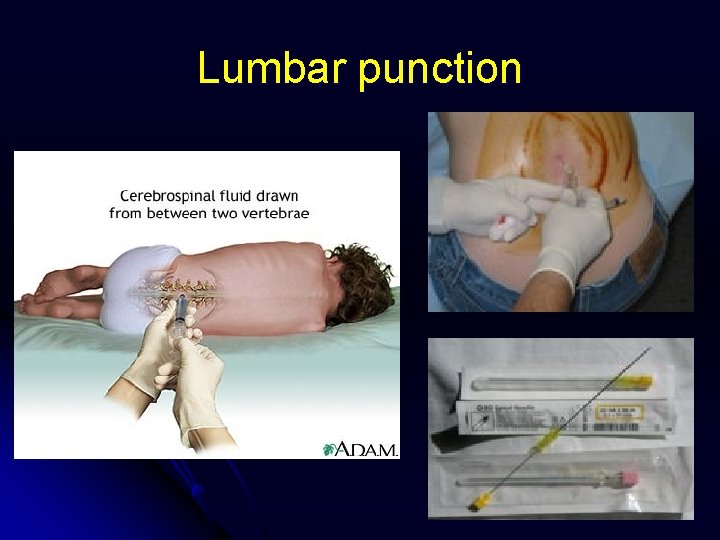
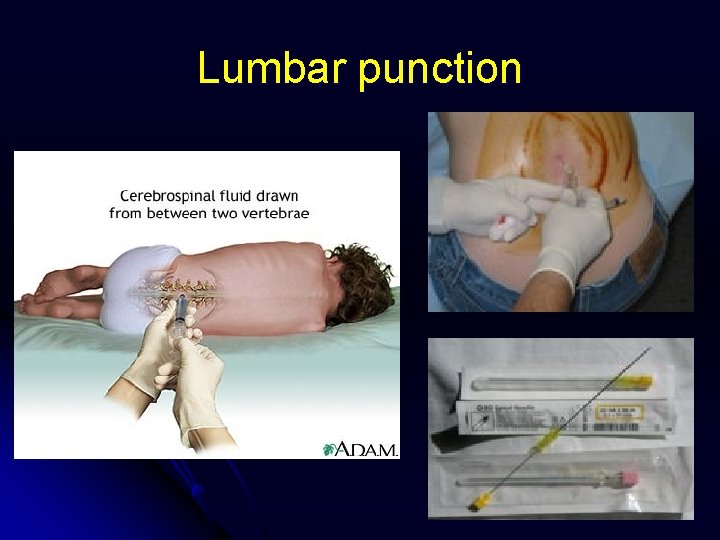
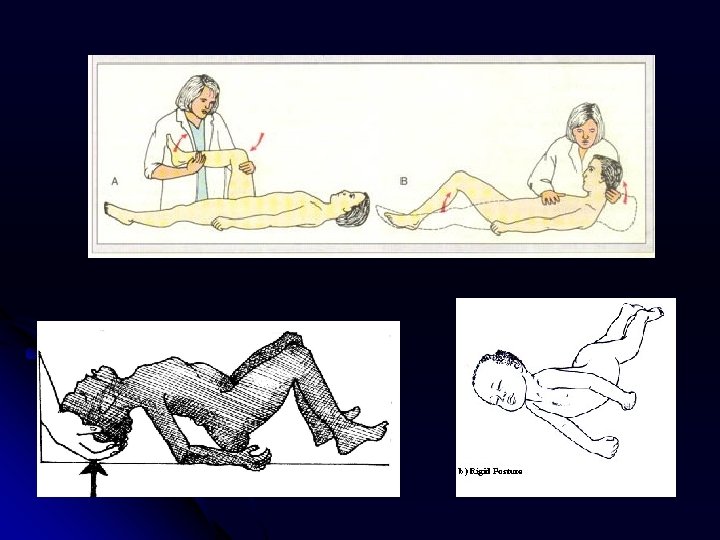
Lumbar punction
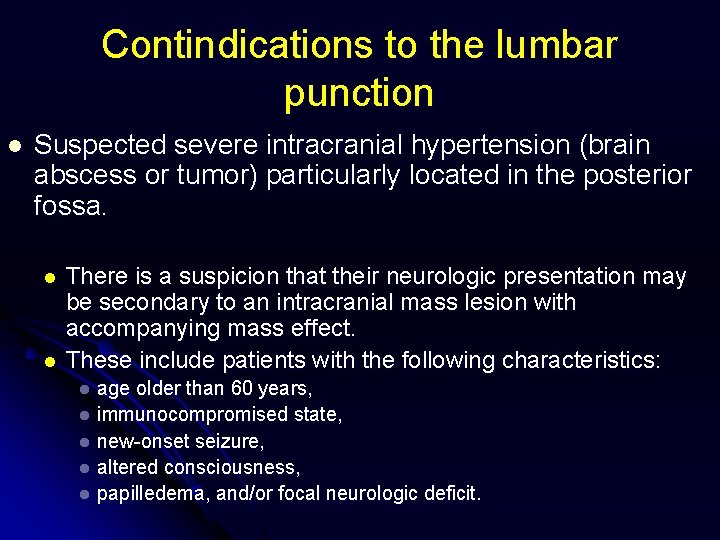
Contindications to the lumbar punction l Suspected severe intracranial hypertension (brain abscess or tumor) particularly located in the posterior fossa. l l There is a suspicion that their neurologic presentation may be secondary to an intracranial mass lesion with accompanying mass effect. These include patients with the following characteristics: age older than 60 years, l immunocompromised state, l new-onset seizure, l altered consciousness, l papilledema, and/or focal neurologic deficit. l
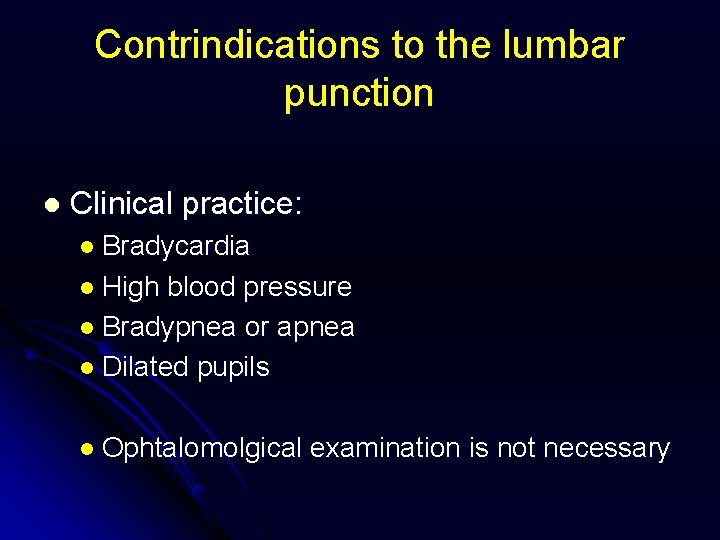
Contrindications to the lumbar punction l Clinical practice: l Bradycardia l High blood pressure l Bradypnea or apnea l Dilated pupils l Ophtalomolgical examination is not necessary
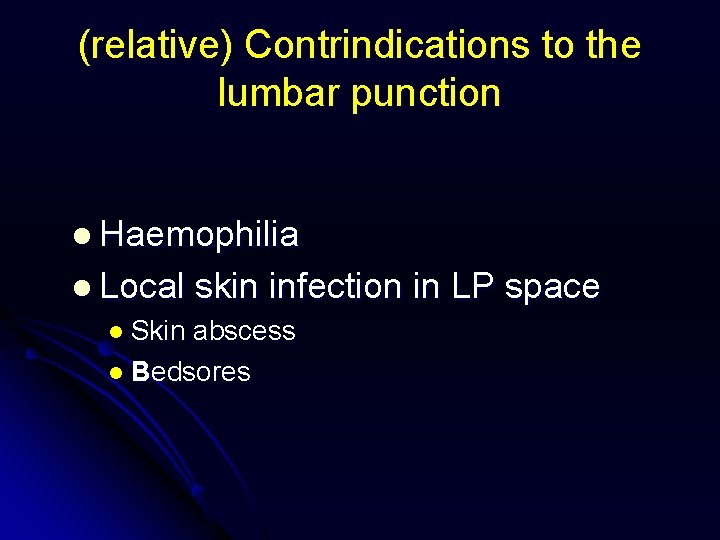
(relative) Contrindications to the lumbar punction l Haemophilia l Local skin infection l Skin abscess l Bedsores in LP space
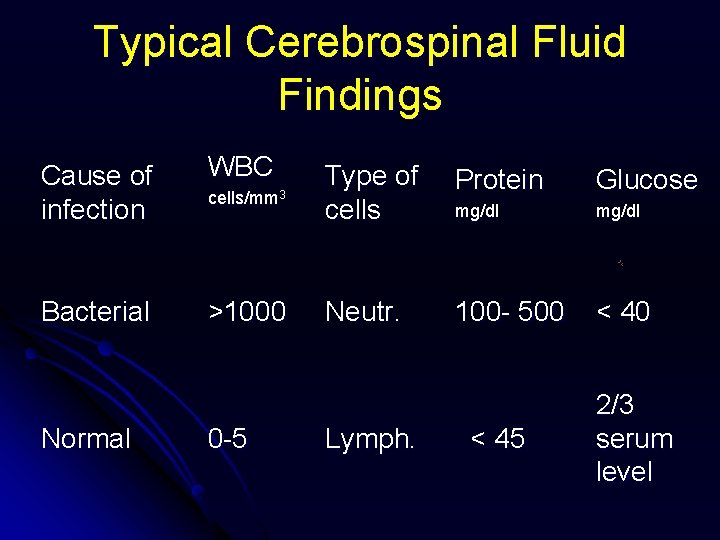
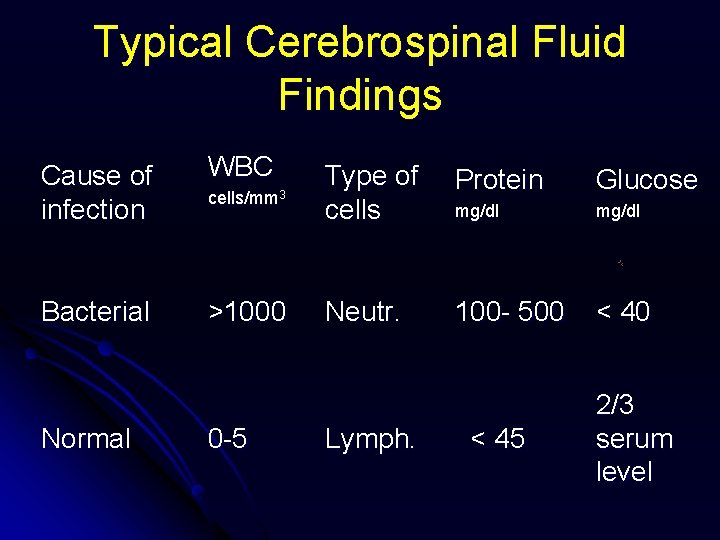
Typical Cerebrospinal Fluid Findings Cause of infection WBC cells/mm 3 Type of cells Protein Glucose mg/dl Bacterial >1000 Neutr. 100 - 500 < 40 Normal 0 -5 Lymph. < 45 2/3 serum level
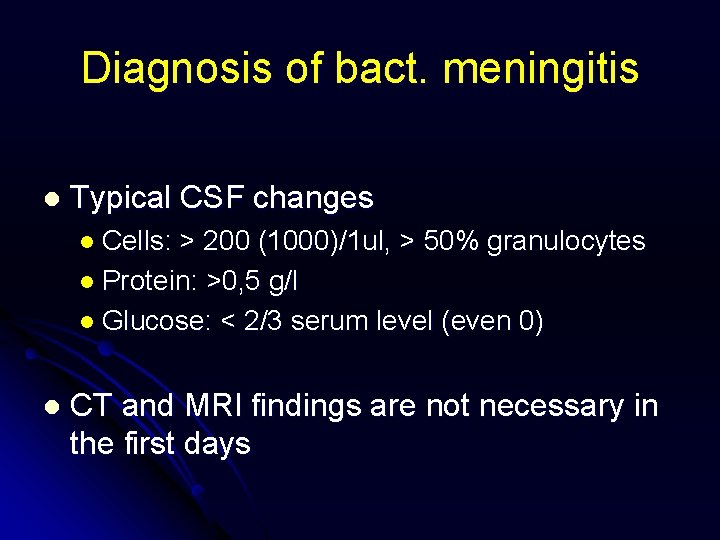
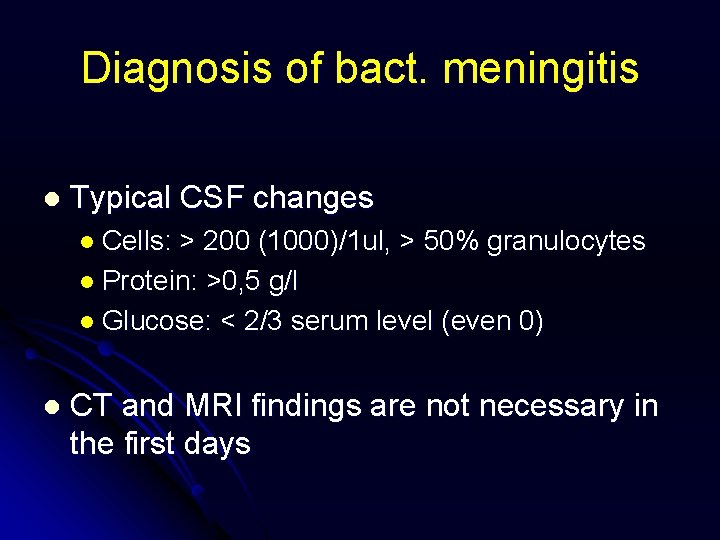
Diagnosis of bact. meningitis l Typical CSF changes l Cells: > 200 (1000)/1 ul, > 50% granulocytes l Protein: >0, 5 g/l l Glucose: < 2/3 serum level (even 0) l CT and MRI findings are not necessary in the first days
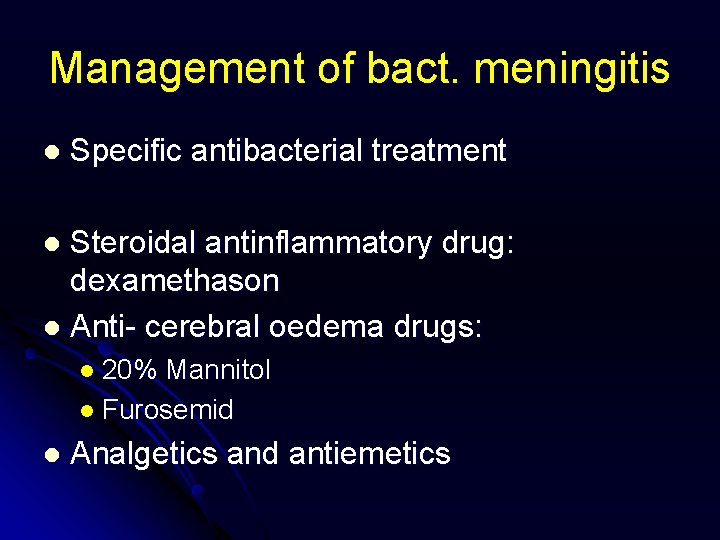
Management of bact. meningitis l Specific antibacterial treatment Steroidal antinflammatory drug: dexamethason l Anti- cerebral oedema drugs: l l 20% Mannitol l Furosemid l Analgetics and antiemetics
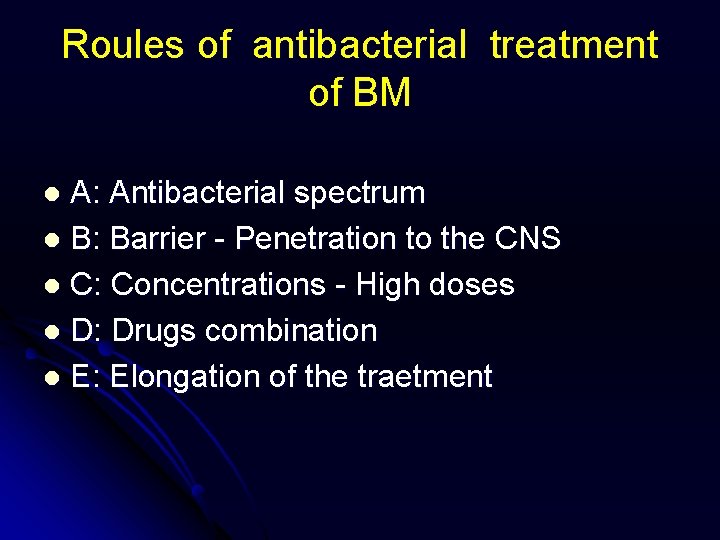
Roules of antibacterial treatment of BM A: Antibacterial spectrum l B: Barrier - Penetration to the CNS l C: Concentrations - High doses l D: Drugs combination l E: Elongation of the traetment l
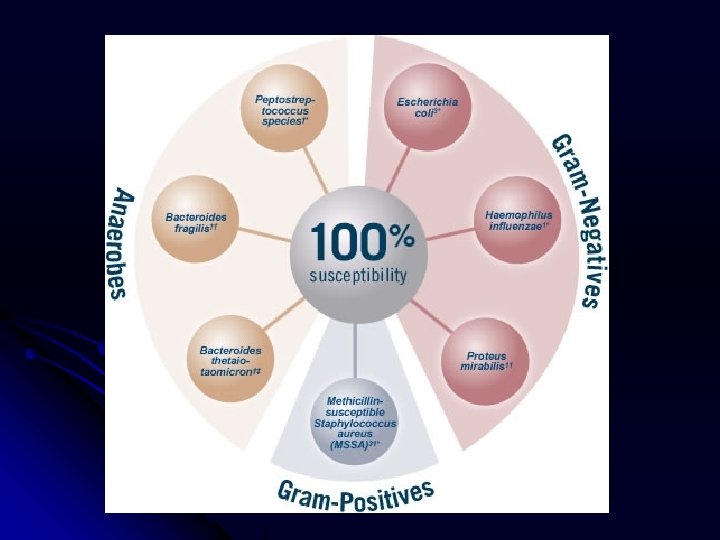
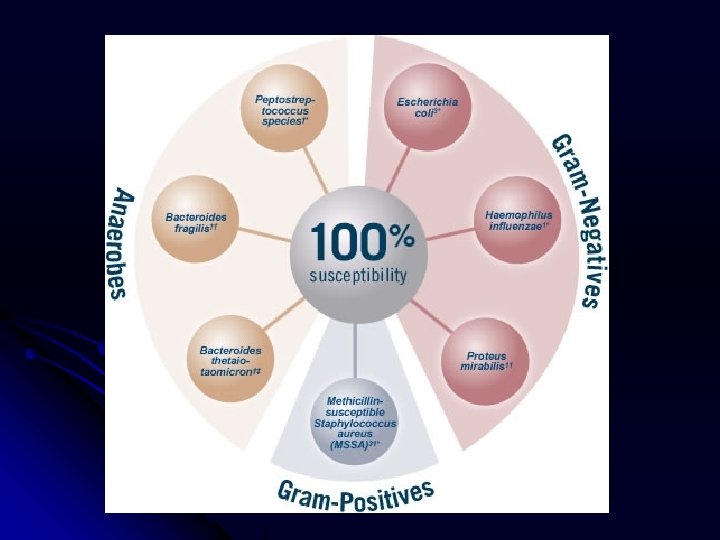
Bacterial meningitis l List of pathogens l Gram – positive: l Streptococcus spp. l Staphylococcus spp. l Gram – negative: l Neisseria meningitidis l Haemophilus influenze l E. coli l Pseudomonas l Proteus aeruginosa spp. l Klebsiella pneumoniae
Epidemiology of bact. meningitis l Newborns l Gram-negative l Children 1 m- 2 y l Haemophilus influenzae type b l Strept. / Neisseria l Adults with immuodepresion
Antibiotics in BM Penicillin 24 MU/d + Ceftriaxon 2, 0 - 4, 0 g/g l Ceftriaxon 2, 0 -4, 0 g/d + Amikacin 1, 5 g/d l P/C or C/A + Metronidazol 1, 5 g/d l Chloramfenicol 3, 0 g/d l Meropenem 1, 5 - 3, 0 g/d l Vancomycin 3, 0 g/d l Trimetoprim+ sulfametoxazol 960 mg 2 x/d as supporting treatment l
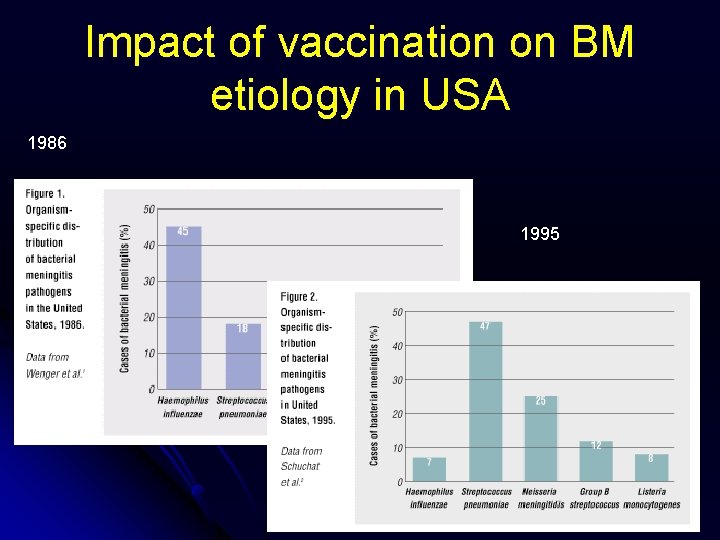
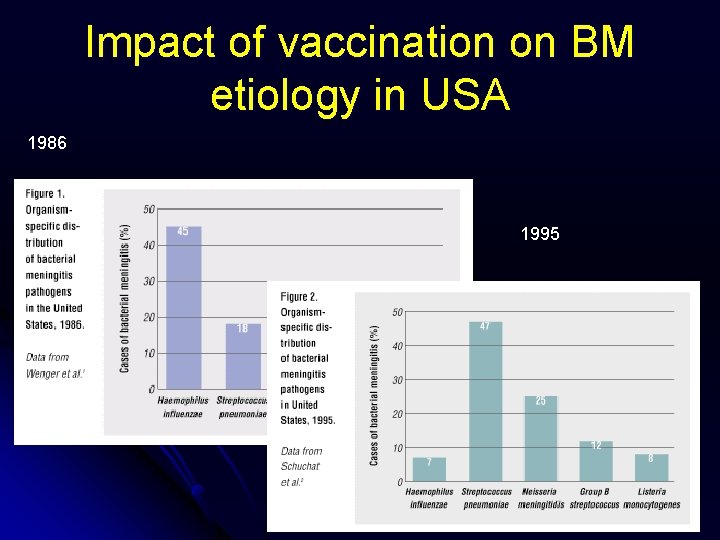
Impact of vaccination on BM etiology in USA 1986 1995
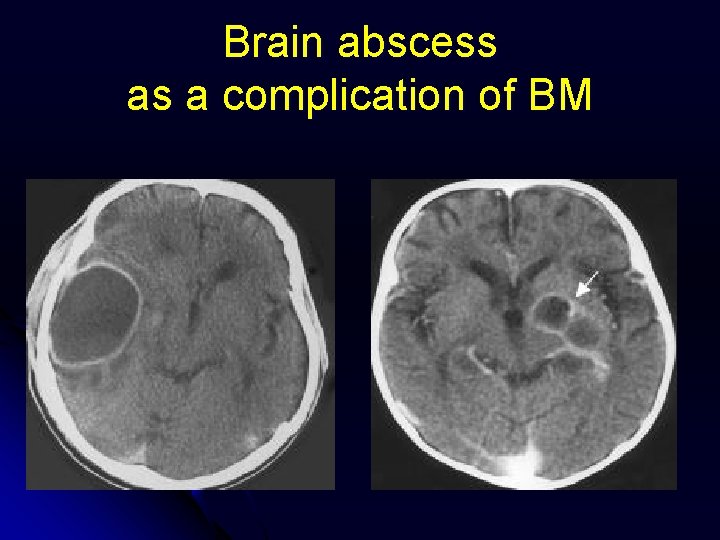
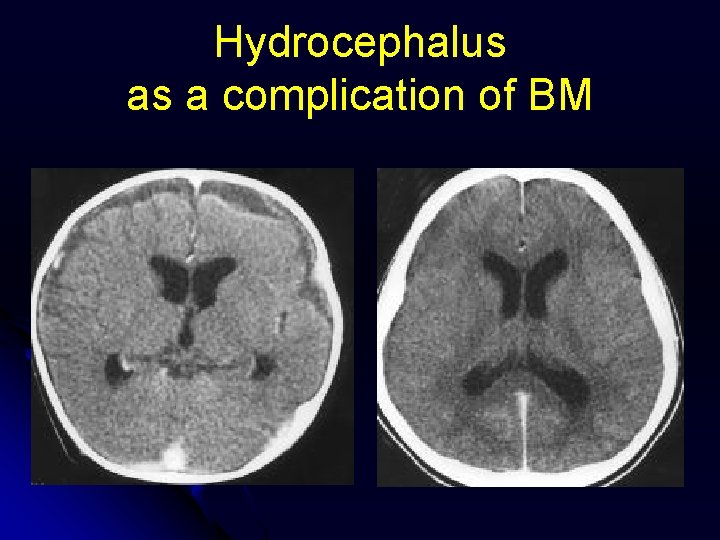
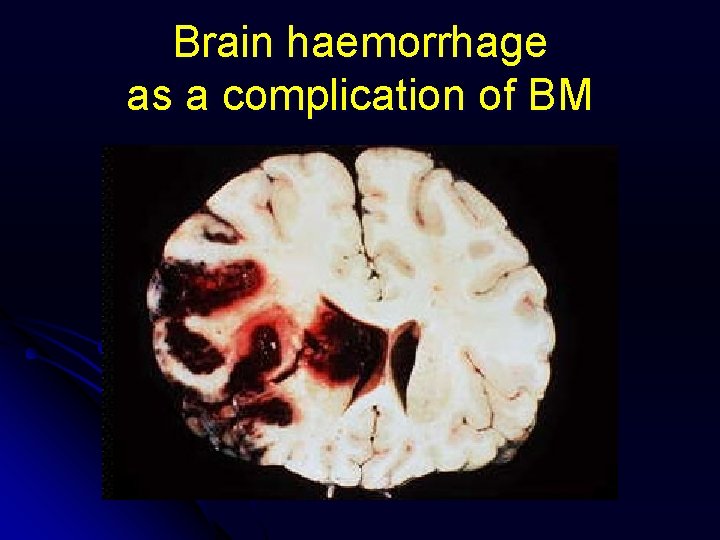
Complications of BM l Early l l l Death Sepsis and septic shock Brain abscess Hydrocephalus Late l Permanent neurological sequeles: deafness, l focal neuroligical signs l l Psychotic symptoms: Loss of memory l Afasia l Altered personality l Behavior disorders l

Comlications of BM
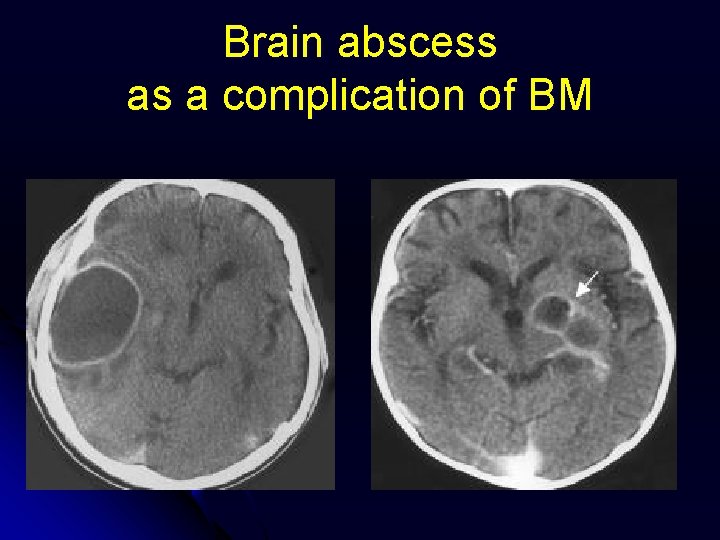
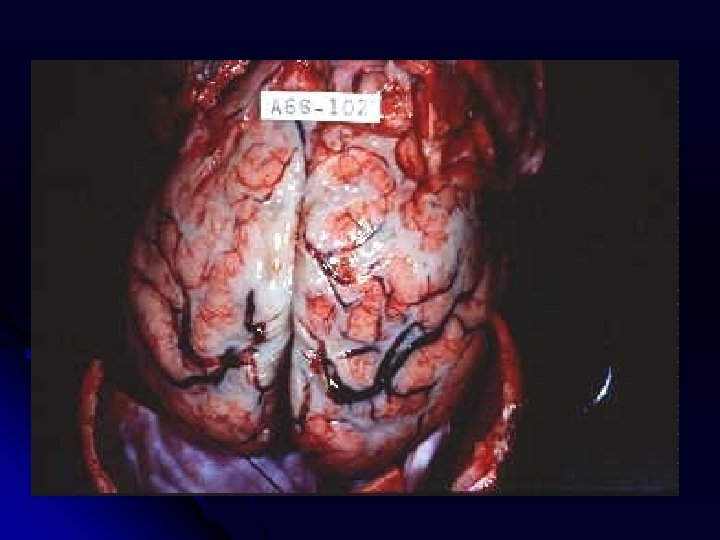
Brain abscess as a complication of BM
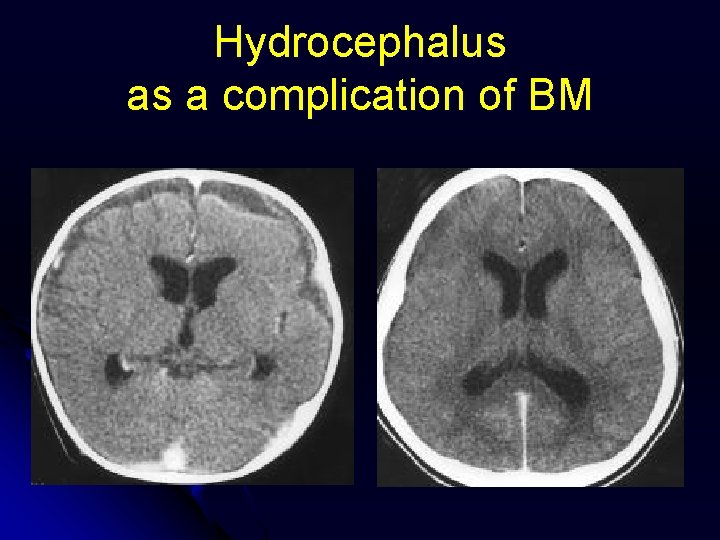
Hydrocephalus as a complication of BM
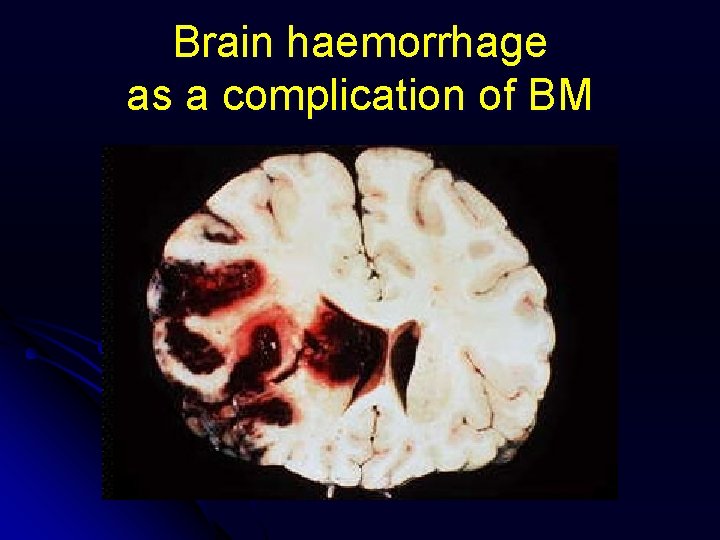
Brain haemorrhage as a complication of BM
Bacterial non-purulent neuroinfections Tuberculosis l Listeriosis l Borreliosis l Leptospirosis l Syphylis l Brucellosis l
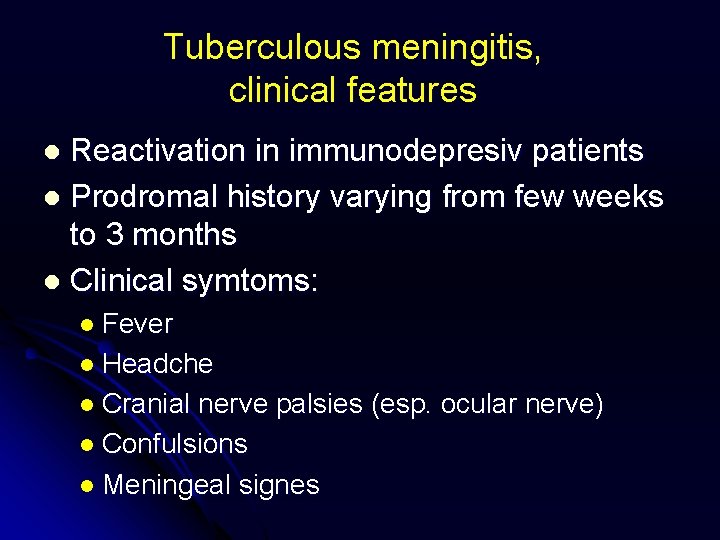
Tuberculous meningitis, clinical features Reactivation in immunodepresiv patients l Prodromal history varying from few weeks to 3 months l Clinical symtoms: l l Fever l Headche l Cranial nerve palsies (esp. ocular nerve) l Confulsions l Meningeal signes
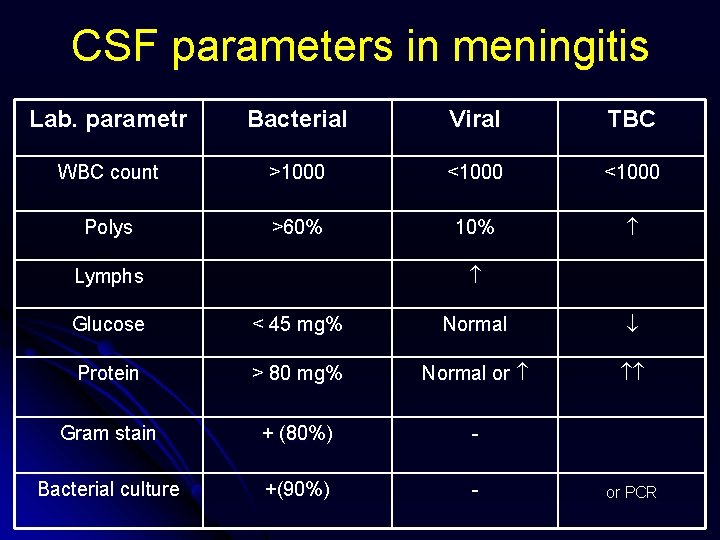
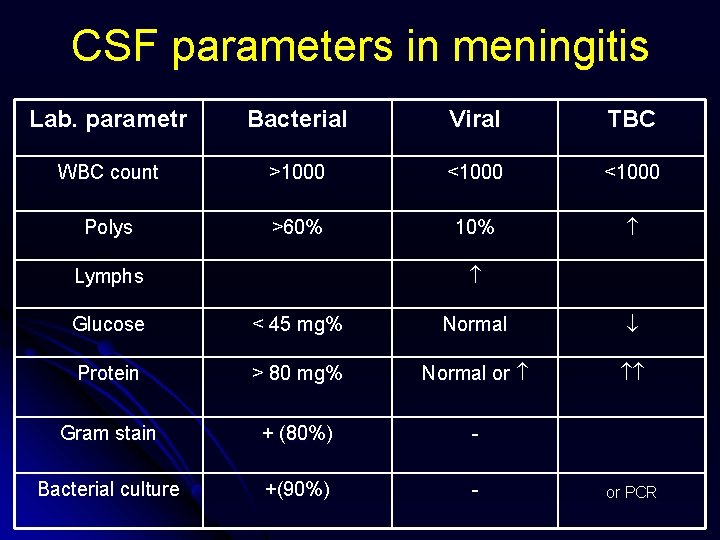
CSF parameters in meningitis Lab. parametr Bacterial Viral TBC WBC count >1000 <1000 Polys >60% 10% Lymphs Glucose < 45 mg% Normal Protein > 80 mg% Normal or Gram stain + (80%) - Bacterial culture +(90%) - or PCR
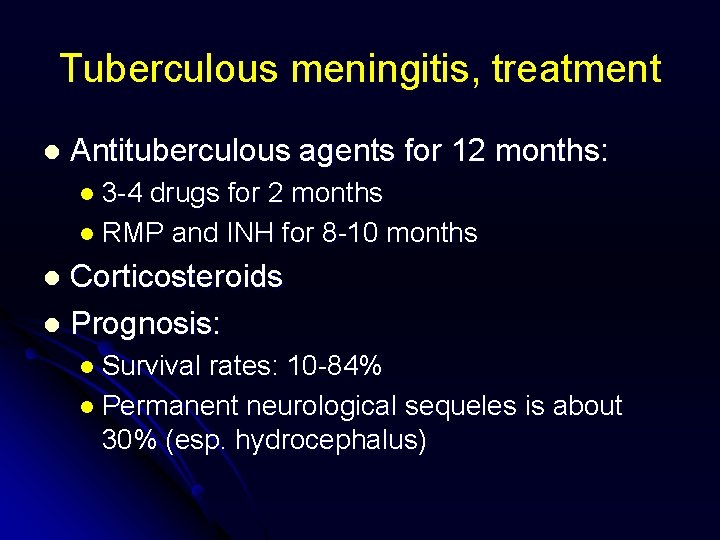
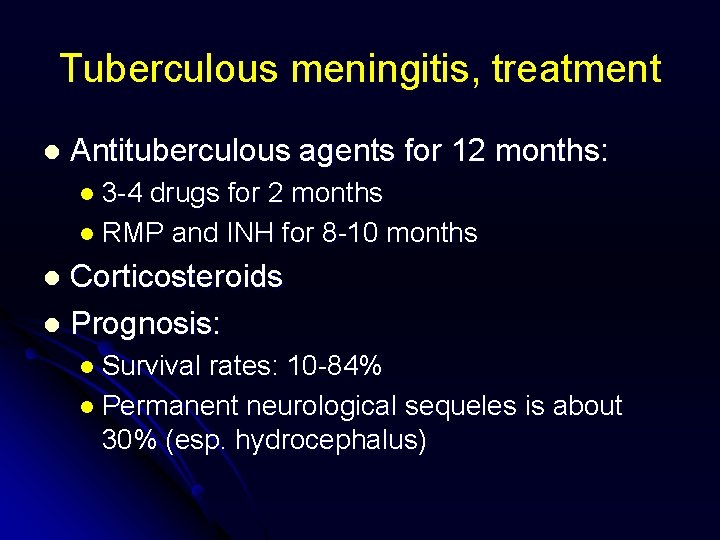
Tuberculous meningitis, treatment l Antituberculous agents for 12 months: l 3 -4 drugs for 2 months l RMP and INH for 8 -10 months Corticosteroids l Prognosis: l l Survival rates: 10 -84% l Permanent neurological sequeles is about 30% (esp. hydrocephalus)
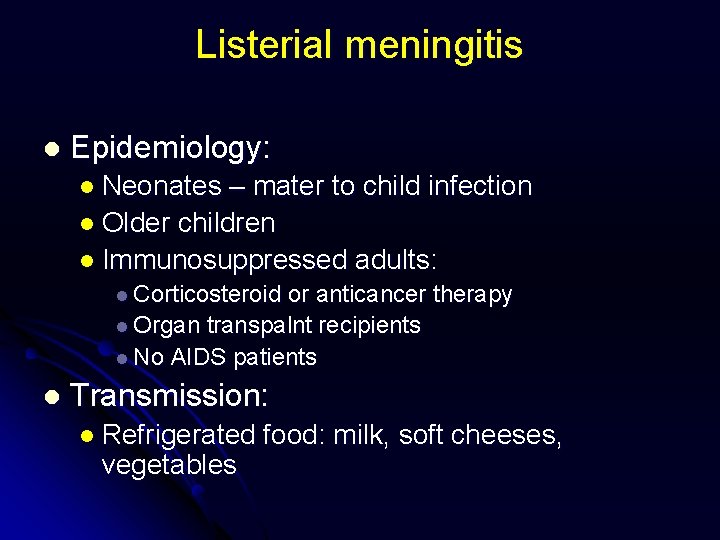
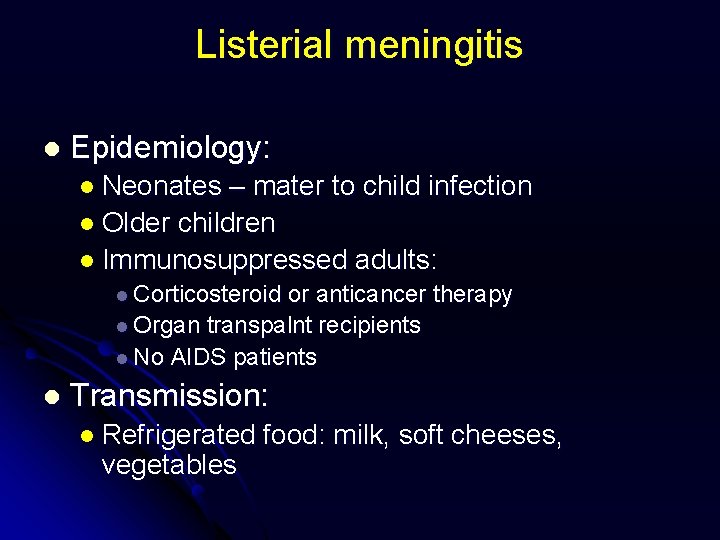
Listerial meningitis l Epidemiology: l Neonates – mater to child infection l Older children l Immunosuppressed adults: l Corticosteroid or anticancer therapy l Organ transpalnt recipients l No AIDS patients l Transmission: l Refrigerated vegetables food: milk, soft cheeses,
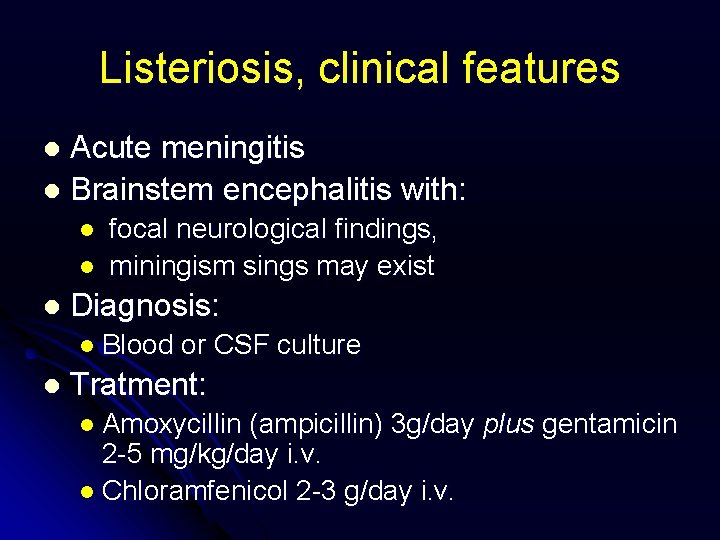
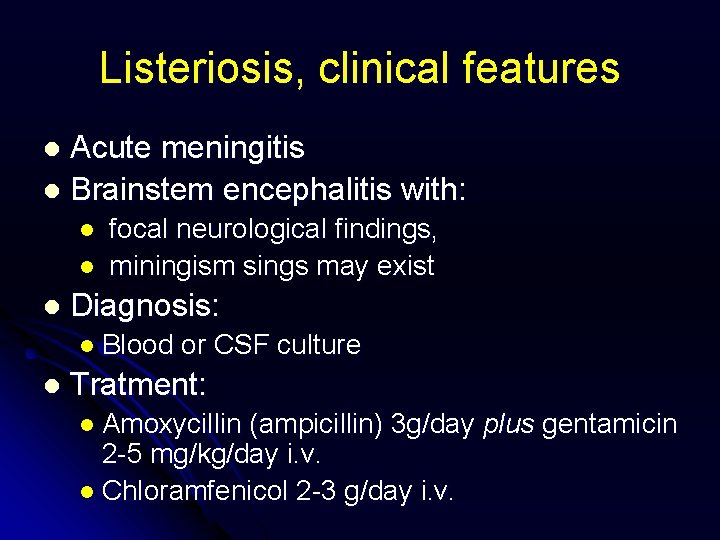
Listeriosis, clinical features Acute meningitis l Brainstem encephalitis with: l l focal neurological findings, miningism sings may exist Diagnosis: l Blood l or CSF culture Tratment: l Amoxycillin (ampicillin) 3 g/day plus gentamicin 2 -5 mg/kg/day i. v. l Chloramfenicol 2 -3 g/day i. v.
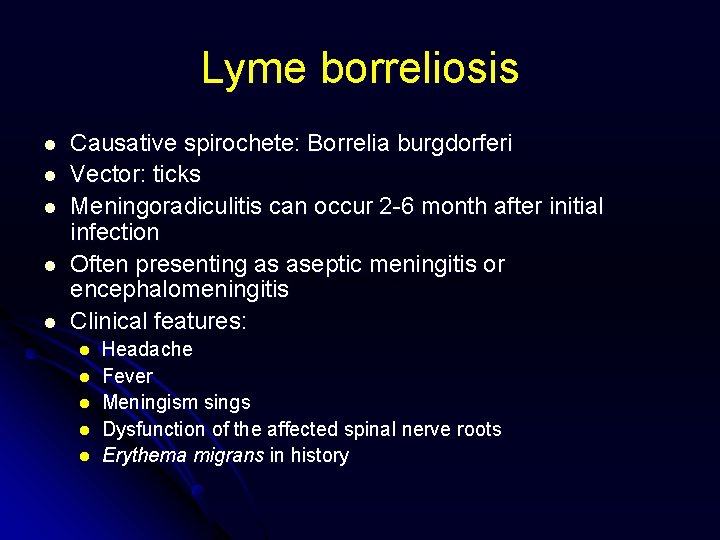
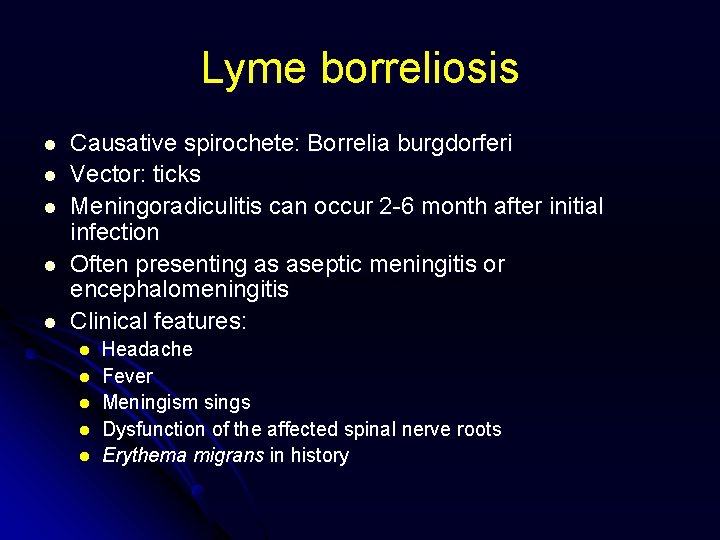
Lyme borreliosis l l l Causative spirochete: Borrelia burgdorferi Vector: ticks Meningoradiculitis can occur 2 -6 month after initial infection Often presenting as aseptic meningitis or encephalomeningitis Clinical features: l l l Headache Fever Meningism sings Dysfunction of the affected spinal nerve roots Erythema migrans in history
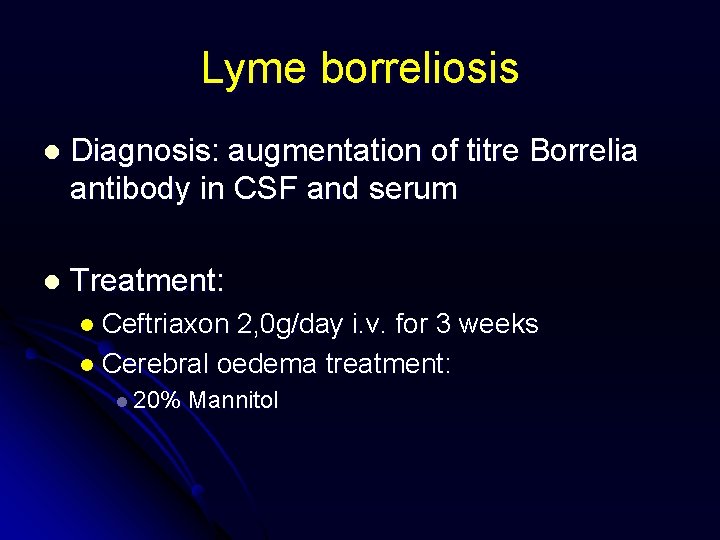
Lyme borreliosis l Diagnosis: augmentation of titre Borrelia antibody in CSF and serum l Treatment: l Ceftriaxon 2, 0 g/day i. v. for 3 weeks l Cerebral oedema treatment: l 20% Mannitol
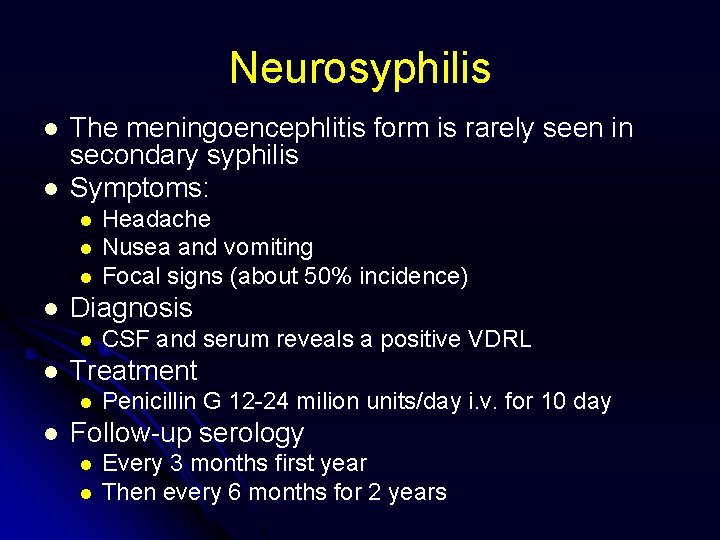
Neurosyphilis l l The meningoencephlitis form is rarely seen in secondary syphilis Symptoms: l l Diagnosis l l CSF and serum reveals a positive VDRL Treatment l l Headache Nusea and vomiting Focal signs (about 50% incidence) Penicillin G 12 -24 milion units/day i. v. for 10 day Follow-up serology l l Every 3 months first year Then every 6 months for 2 years
Leptospirosis l l l LPS is seen in summer months, usually in association with water and animal (mouss, rat) exposure LPS involve the CNS as aseptic meningitis in 968% of LPS cases Symptoms l l Headache Muscular pain and tenderness Nusea and vomiting Renal faillure
Leptospirosis l Diagnosis l Isolation of the organism from the: l Urine l Blood l CSF l Treatment l Penicillin 10 milion units/day l Or tetracycline 2 -4 g/day
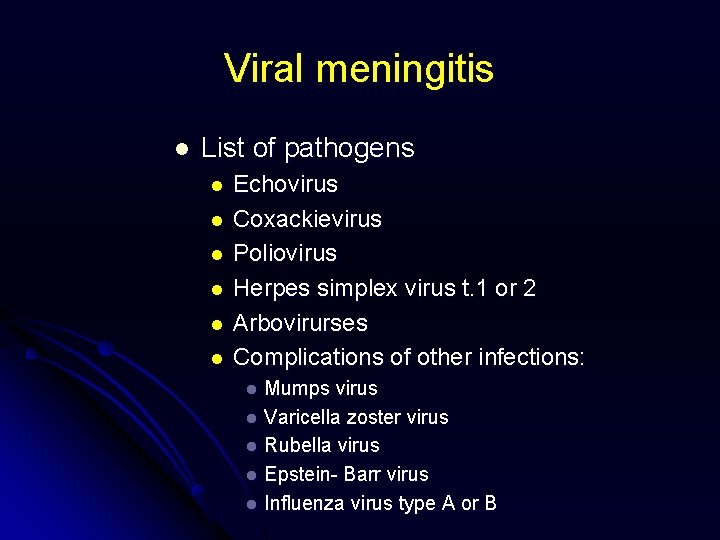
Viral meningitis l List of pathogens l l l Echovirus Coxackievirus Poliovirus Herpes simplex virus t. 1 or 2 Arbovirurses Complications of other infections: Mumps virus l Varicella zoster virus l Rubella virus l Epstein- Barr virus l Influenza virus type A or B l
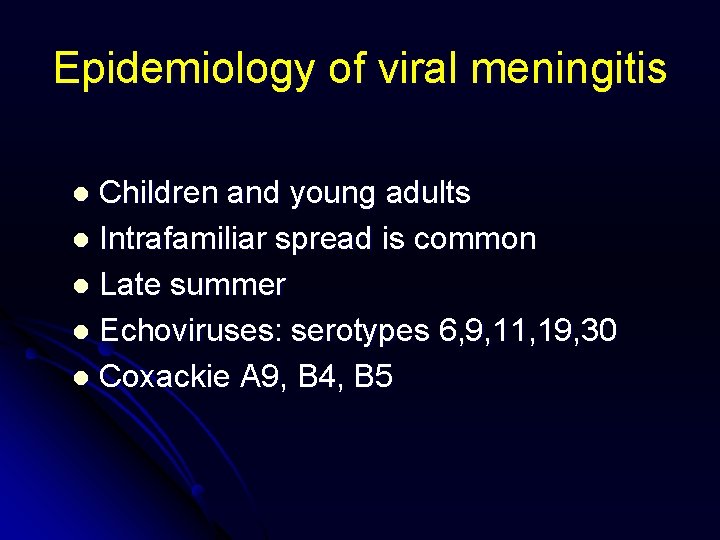
Epidemiology of viral meningitis Children and young adults l Intrafamiliar spread is common l Late summer l Echoviruses: serotypes 6, 9, 11, 19, 30 l Coxackie A 9, B 4, B 5 l
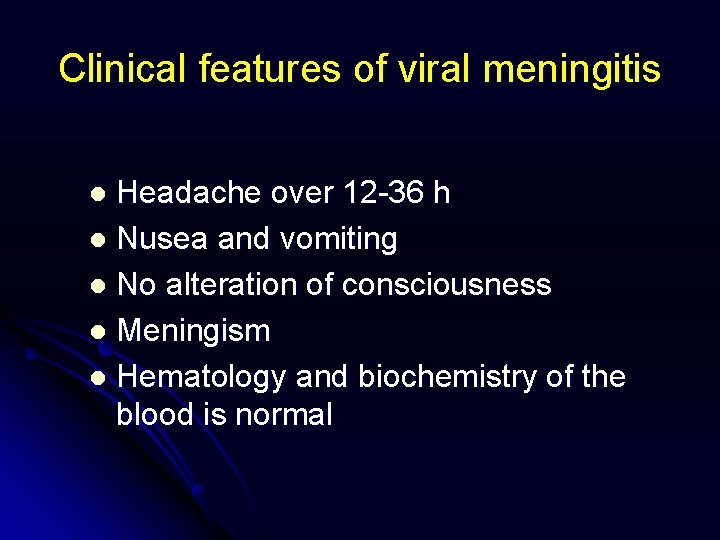
Clinical features of viral meningitis Headache over 12 -36 h l Nusea and vomiting l No alteration of consciousness l Meningism l Hematology and biochemistry of the blood is normal l
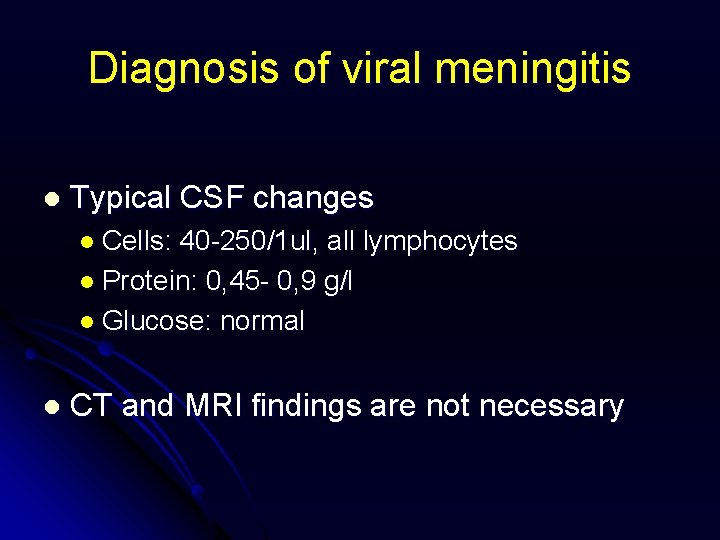
Diagnosis of viral meningitis l Typical CSF changes l Cells: 40 -250/1 ul, all lymphocytes l Protein: 0, 45 - 0, 9 g/l l Glucose: normal l CT and MRI findings are not necessary
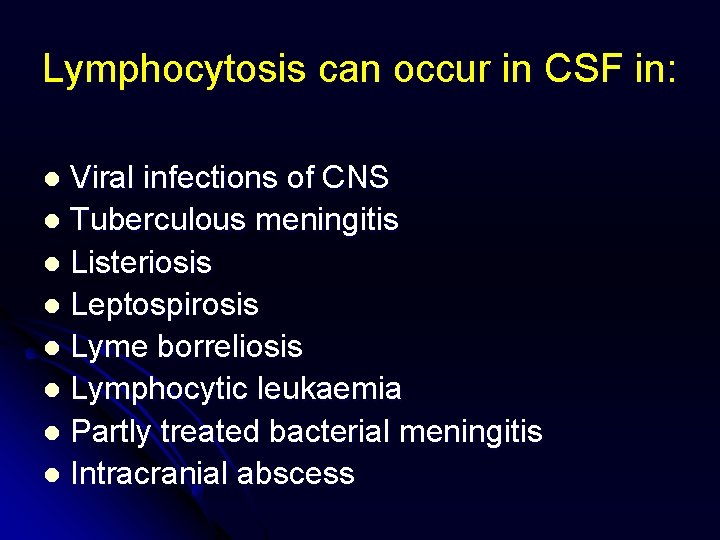
Lymphocytosis can occur in CSF in: Viral infections of CNS l Tuberculous meningitis l Listeriosis l Leptospirosis l Lyme borreliosis l Lymphocytic leukaemia l Partly treated bacterial meningitis l Intracranial abscess l
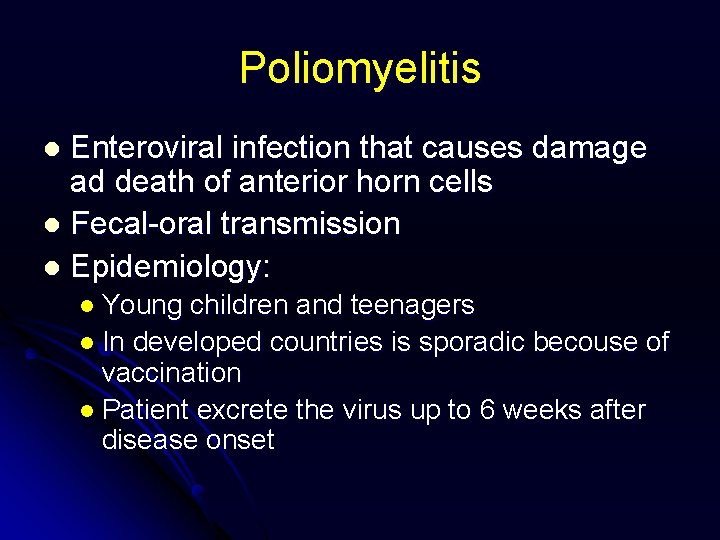
Poliomyelitis Enteroviral infection that causes damage ad death of anterior horn cells l Fecal-oral transmission l Epidemiology: l l Young children and teenagers l In developed countries is sporadic becouse of vaccination l Patient excrete the virus up to 6 weeks after disease onset
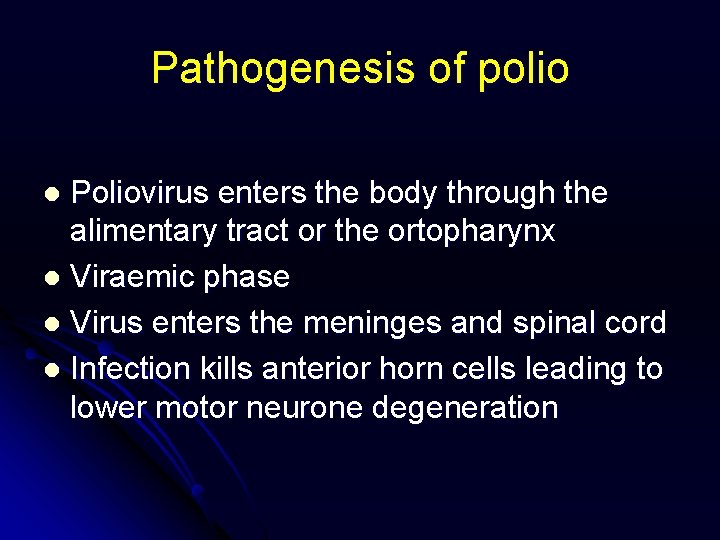
Pathogenesis of polio Poliovirus enters the body through the alimentary tract or the ortopharynx l Viraemic phase l Virus enters the meninges and spinal cord l Infection kills anterior horn cells leading to lower motor neurone degeneration l
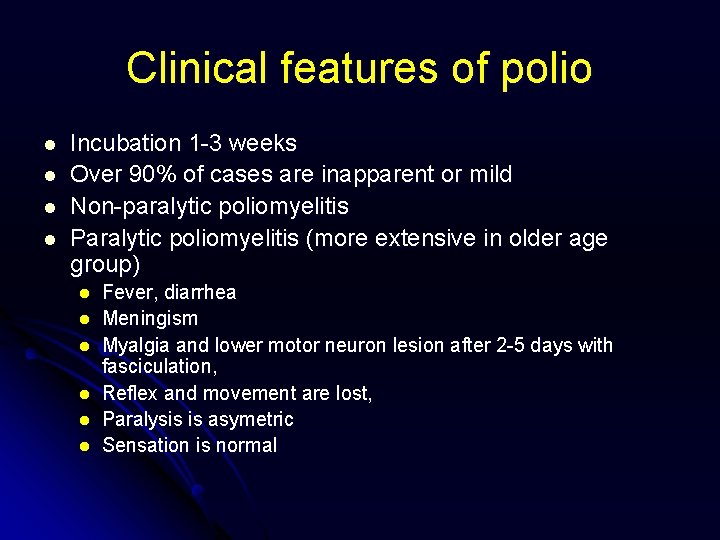
Clinical features of polio l l Incubation 1 -3 weeks Over 90% of cases are inapparent or mild Non-paralytic poliomyelitis Paralytic poliomyelitis (more extensive in older age group) l l l Fever, diarrhea Meningism Myalgia and lower motor neuron lesion after 2 -5 days with fasciculation, Reflex and movement are lost, Paralysis is asymetric Sensation is normal
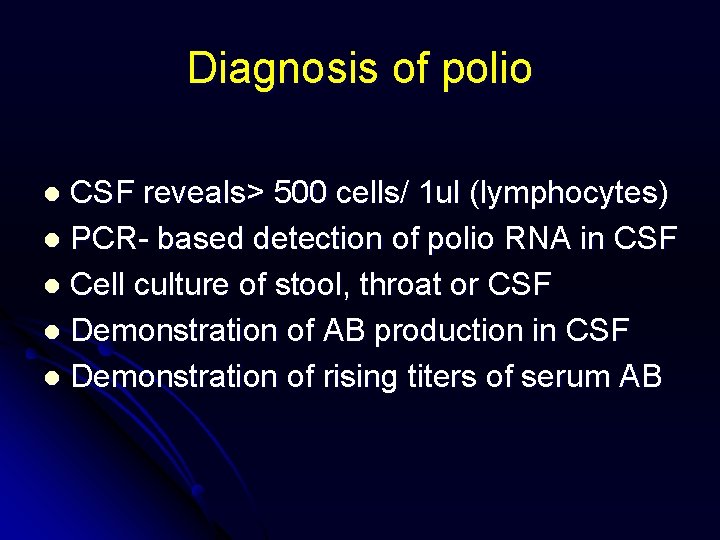
Diagnosis of polio CSF reveals> 500 cells/ 1 ul (lymphocytes) l PCR- based detection of polio RNA in CSF l Cell culture of stool, throat or CSF l Demonstration of AB production in CSF l Demonstration of rising titers of serum AB l
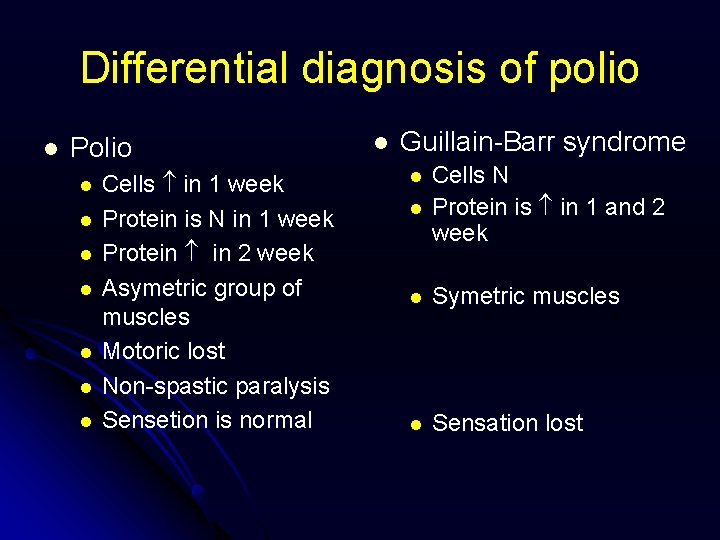
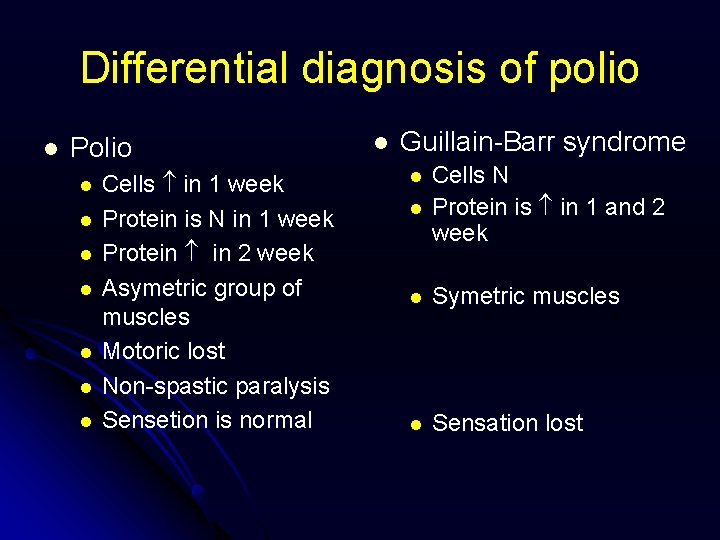
Differential diagnosis of polio l Polio l l l l Cells in 1 week Protein is N in 1 week Protein in 2 week Asymetric group of muscles Motoric lost Non-spastic paralysis Sensetion is normal l Guillain-Barr syndrome l Cells N Protein is in 1 and 2 week l Symetric muscles l Sensation lost l
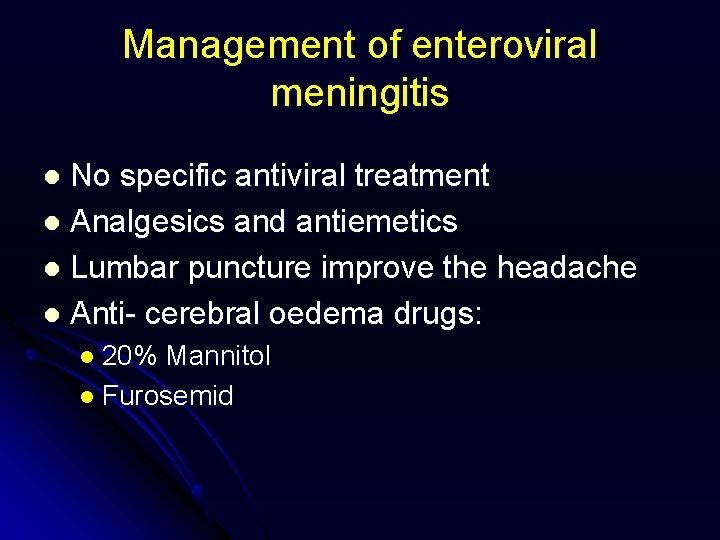
Management of enteroviral meningitis No specific antiviral treatment l Analgesics and antiemetics l Lumbar puncture improve the headache l Anti- cerebral oedema drugs: l l 20% Mannitol l Furosemid
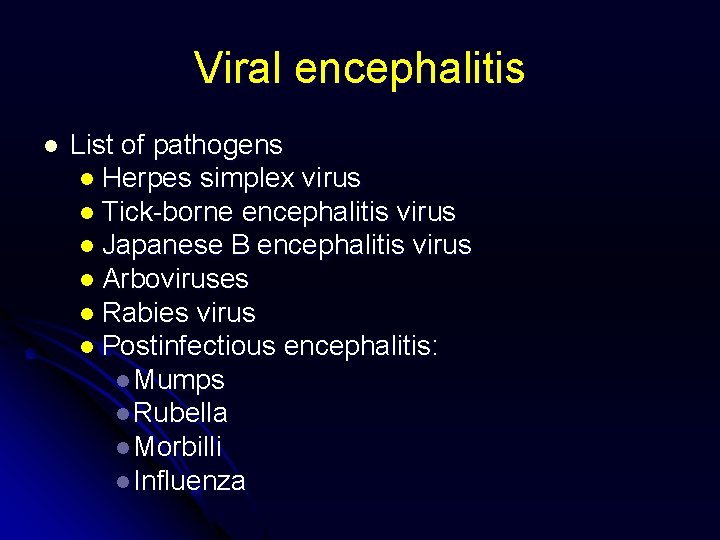
Viral encephalitis l List of pathogens l Herpes simplex virus l Tick-borne encephalitis virus l Japanese B encephalitis virus l Arboviruses l Rabies virus l Postinfectious encephalitis: l Mumps l Rubella l Morbilli l Influenza
Clinical features of viral encephalitis l l l l Irritability Altered personality Drowsiness Ataxia Excessively brisk tendon reflexes Upgoing plantar responses Sings of cerebral or brainstem failure l l l slugish, absent pupil reflexes, intermittent breathing patterns Sings of brain swelling l l focal neurological signs, papilloedema Signs of meningitis may coexist
Diagnosis of viral encephalitis Clinical features l CSF l CT and MRI findings l Encephalographic changes l Demonstration of specific antibodies in CSF l PCR- based DNA or RNA detection techniques l
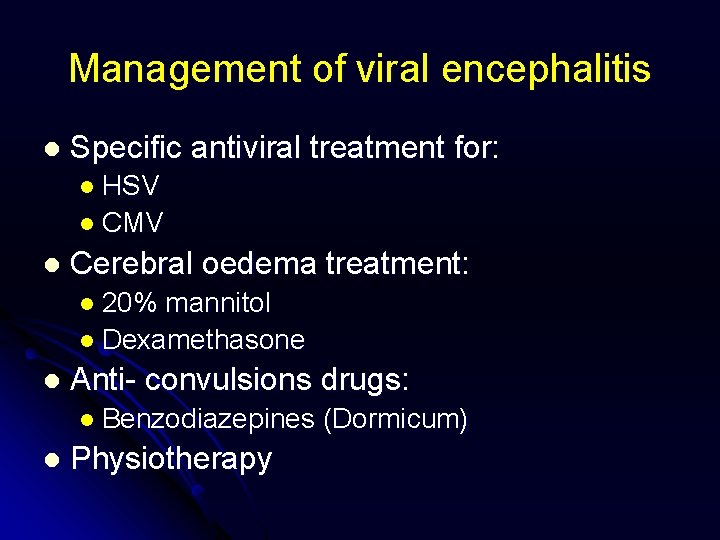
Management of viral encephalitis l Specific antiviral treatment for: l HSV l CMV l Cerebral oedema treatment: l 20% mannitol l Dexamethasone l Anti- convulsions drugs: l Benzodiazepines l Physiotherapy (Dormicum)
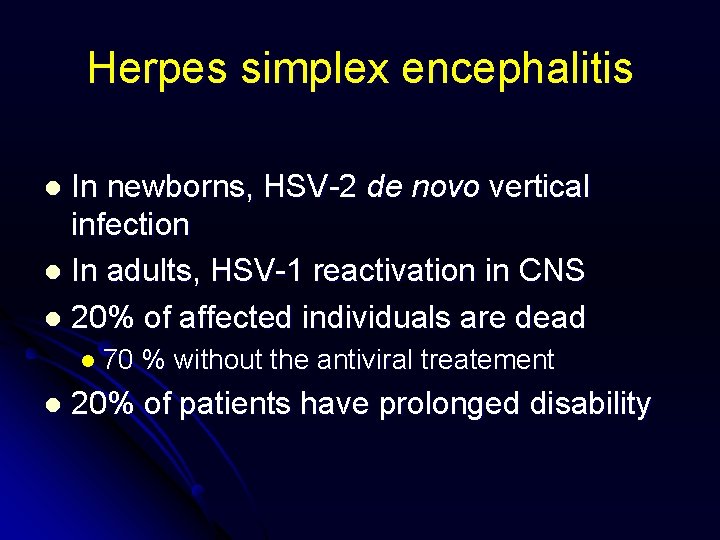
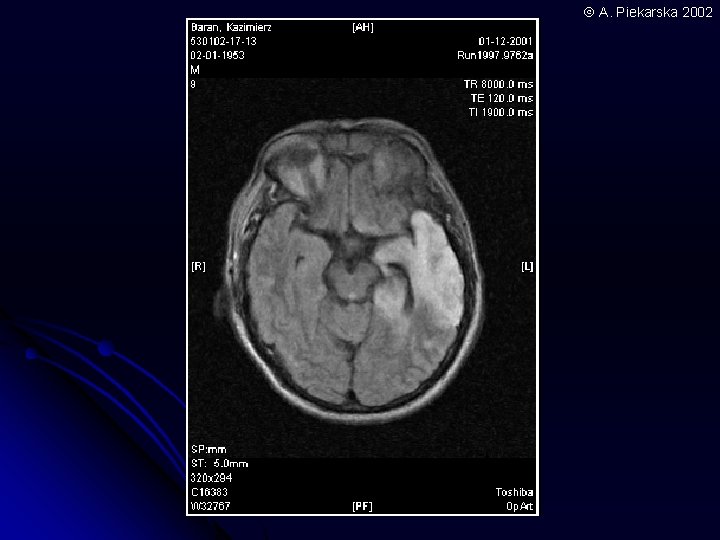
Herpes simplex encephalitis In newborns, HSV-2 de novo vertical infection l In adults, HSV-1 reactivation in CNS l 20% of affected individuals are dead l l 70 l % without the antiviral treatement 20% of patients have prolonged disability
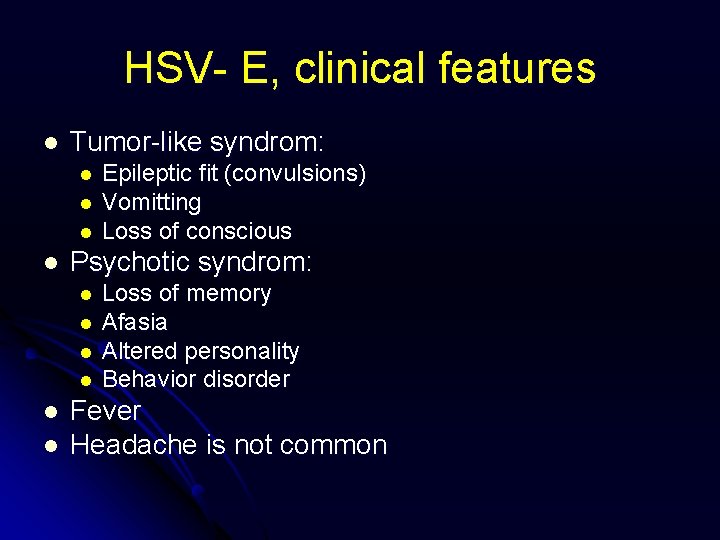
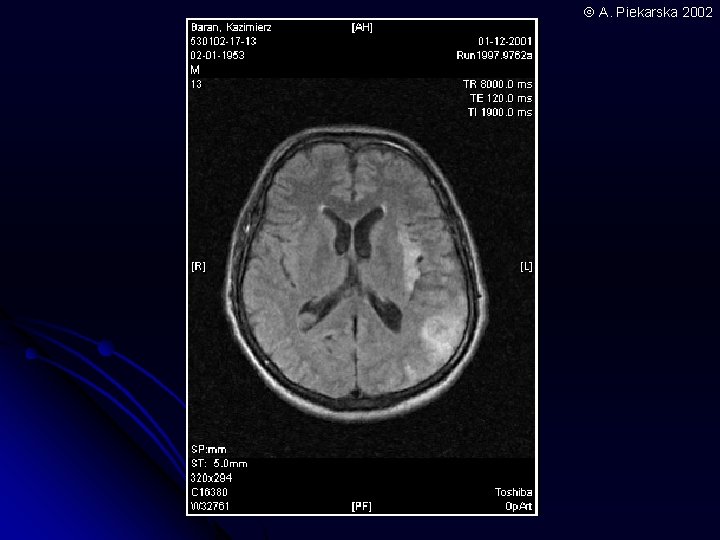
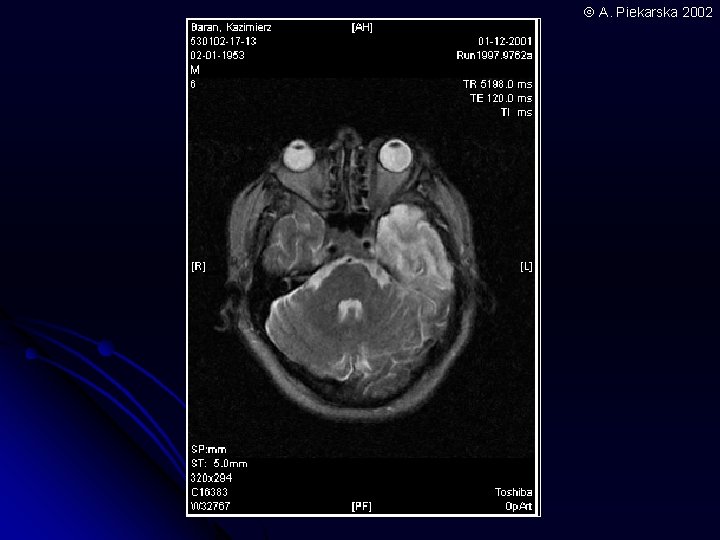
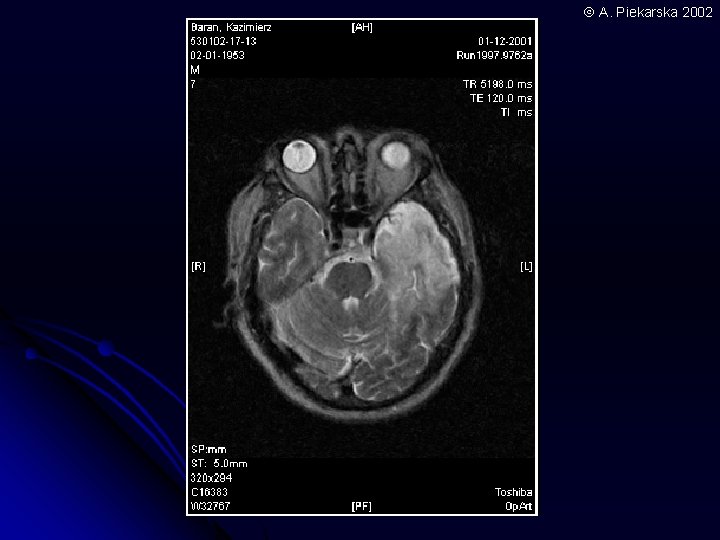
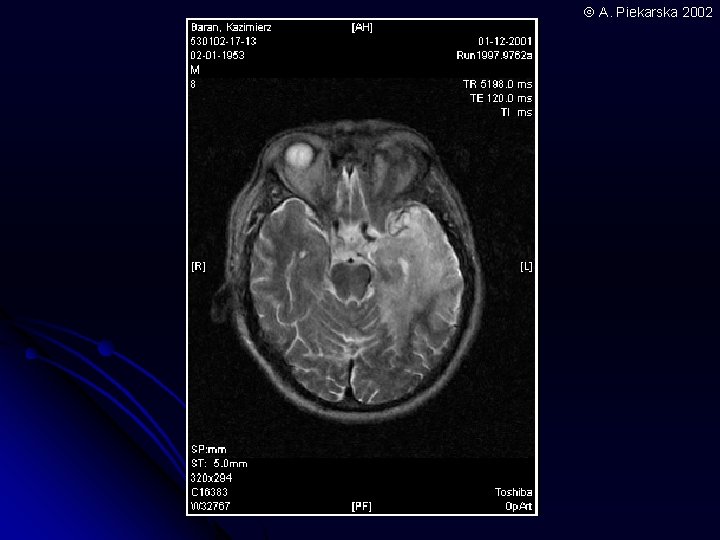
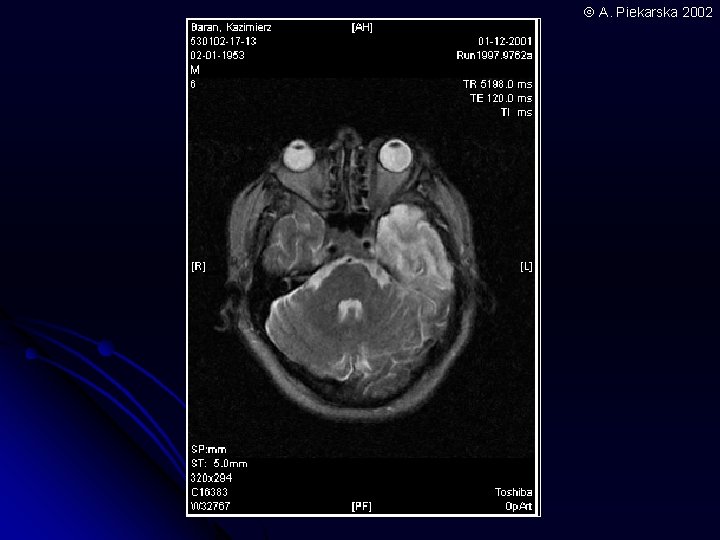
HSV- E, clinical features l Tumor-like syndrom: l l Psychotic syndrom: l l l Epileptic fit (convulsions) Vomitting Loss of conscious Loss of memory Afasia Altered personality Behavior disorder Fever Headache is not common
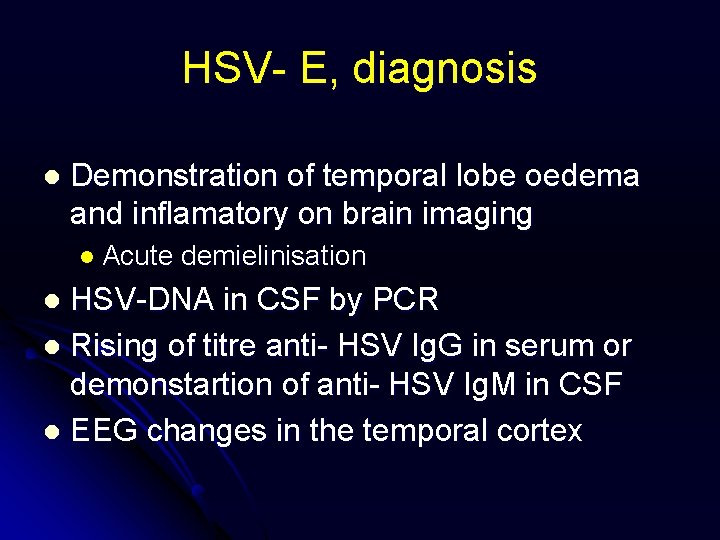
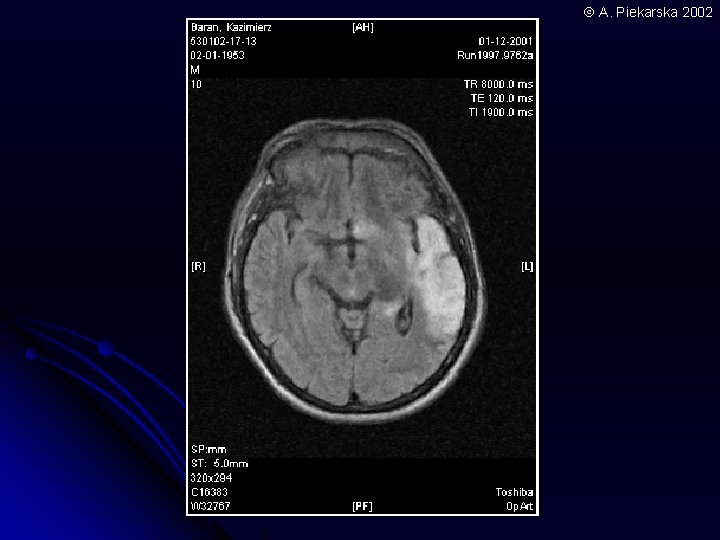
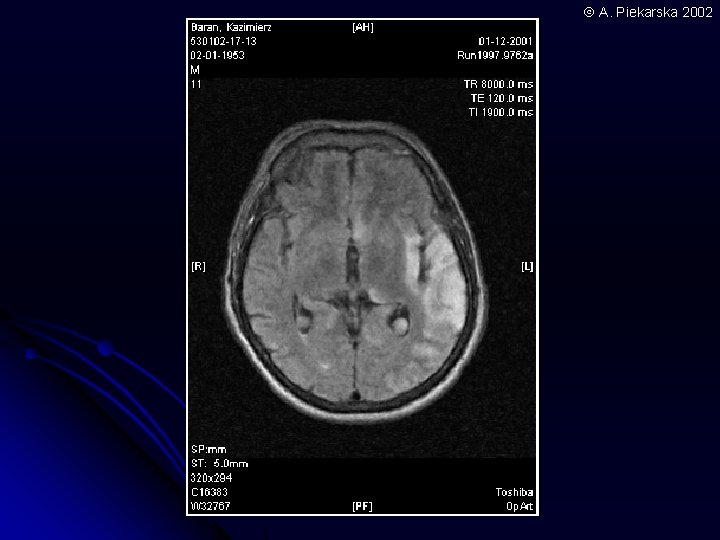
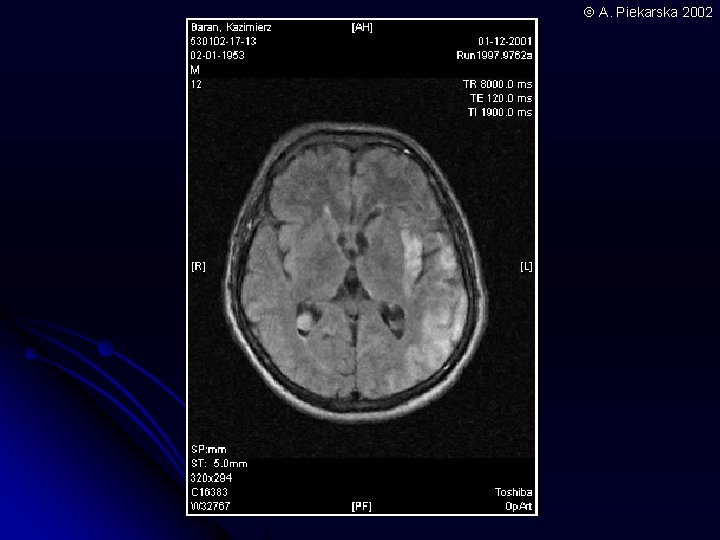
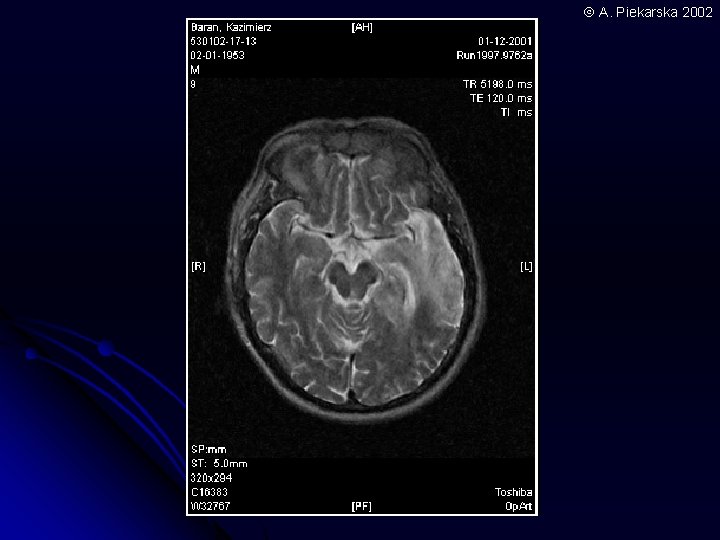
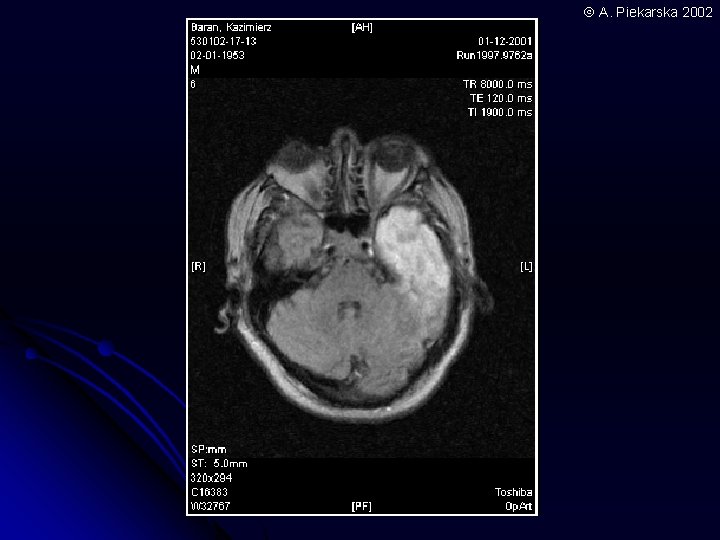
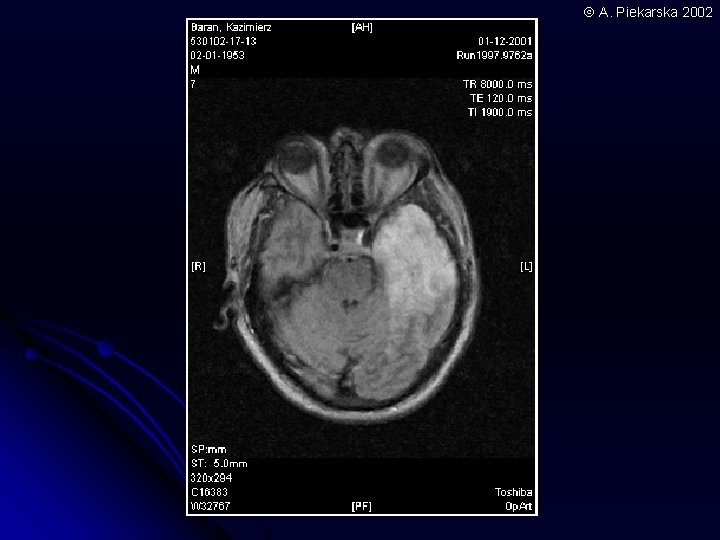
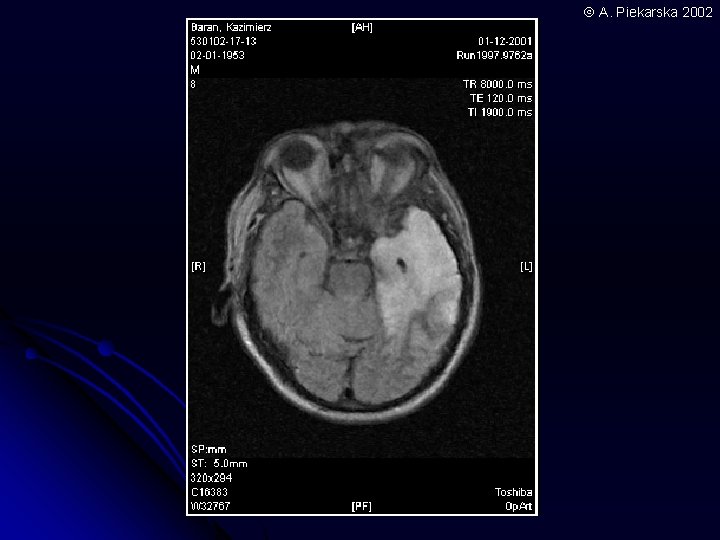
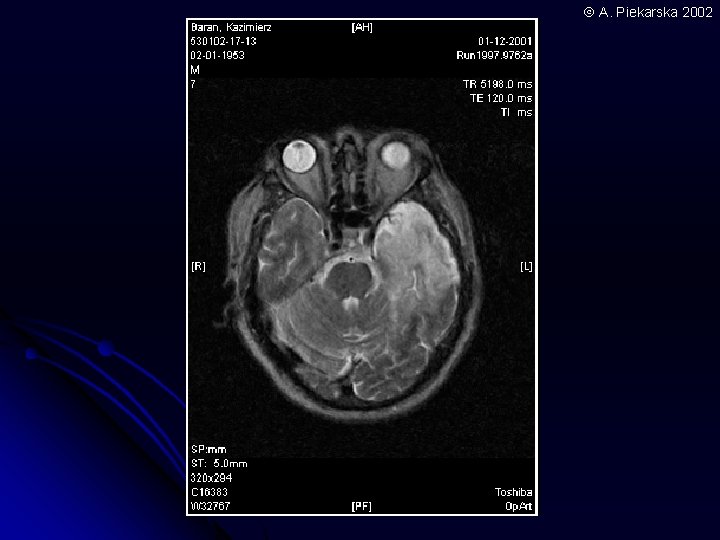
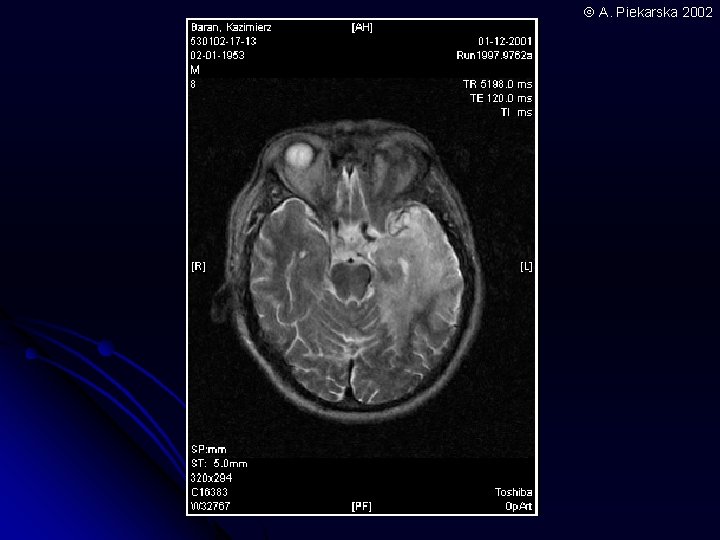
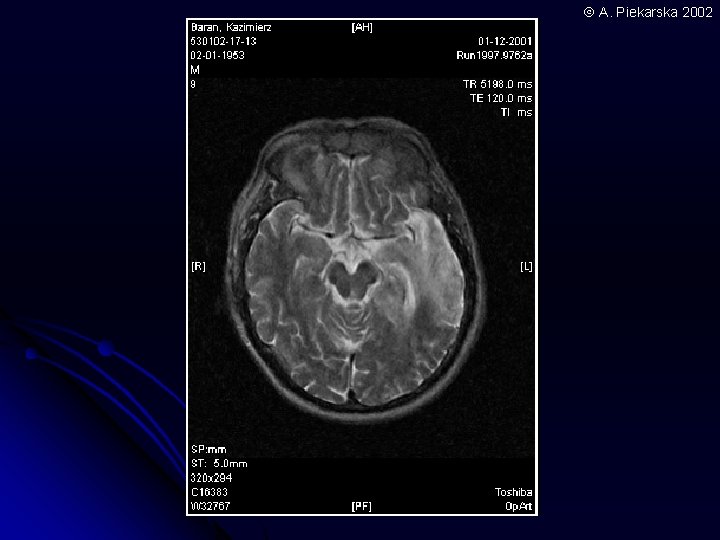
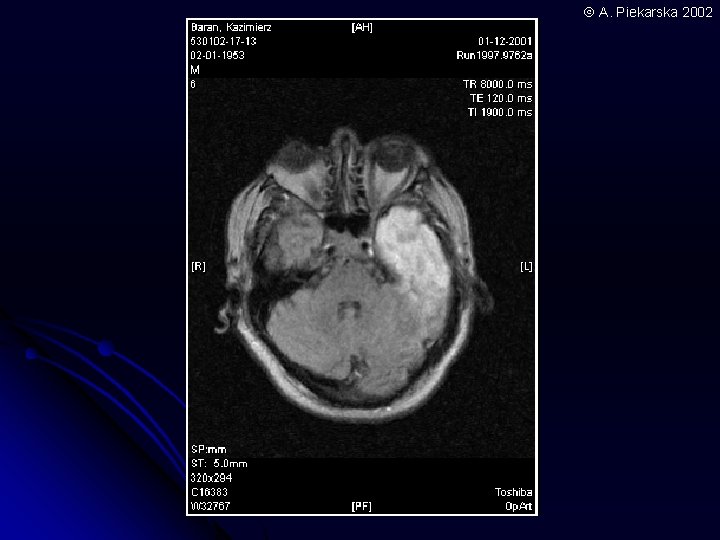
HSV- E, diagnosis l Demonstration of temporal lobe oedema and inflamatory on brain imaging l Acute demielinisation HSV-DNA in CSF by PCR l Rising of titre anti- HSV Ig. G in serum or demonstartion of anti- HSV Ig. M in CSF l EEG changes in the temporal cortex l
HSV-E, treatment Aciclovir 10 mg/kg every 8 hour i. v per 3 -6 weeks l Cerebral oedema treatment: l l 20% l mannitol Neuroleptics
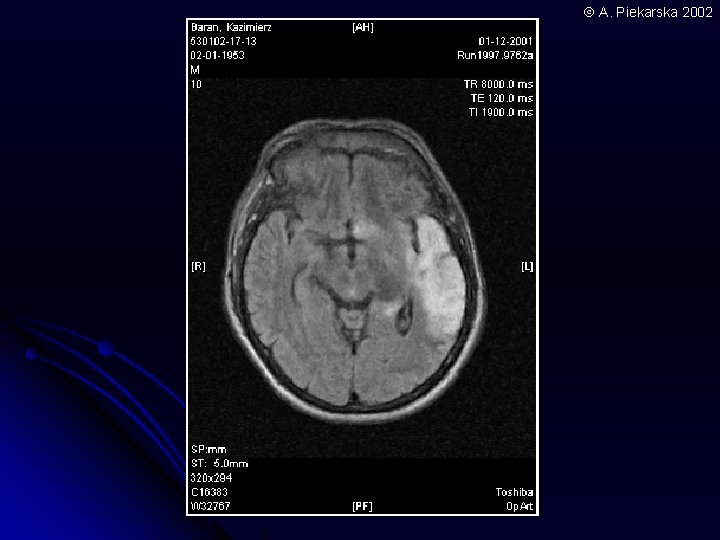
A. Piekarska 2002
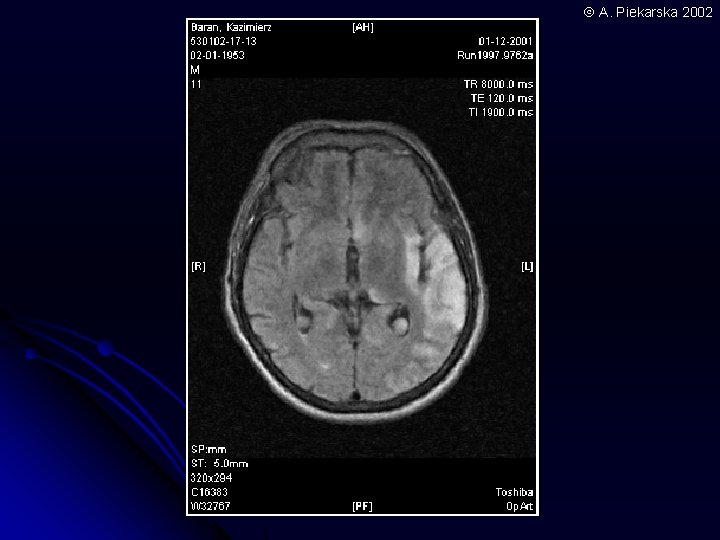
A. Piekarska 2002
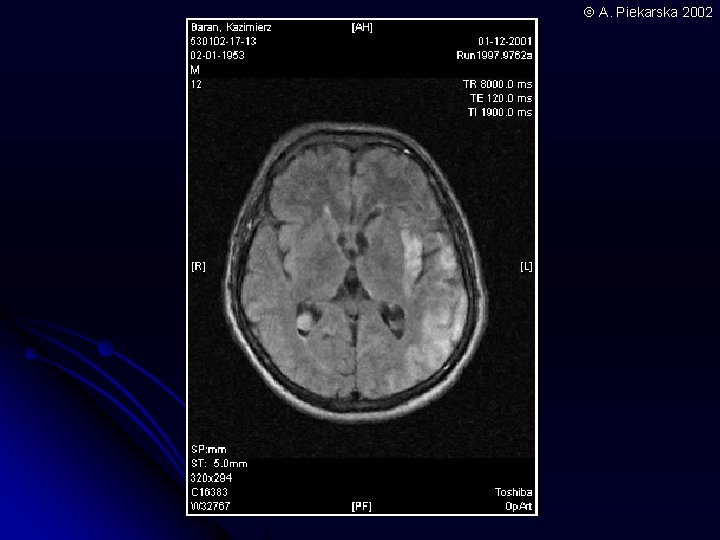
A. Piekarska 2002
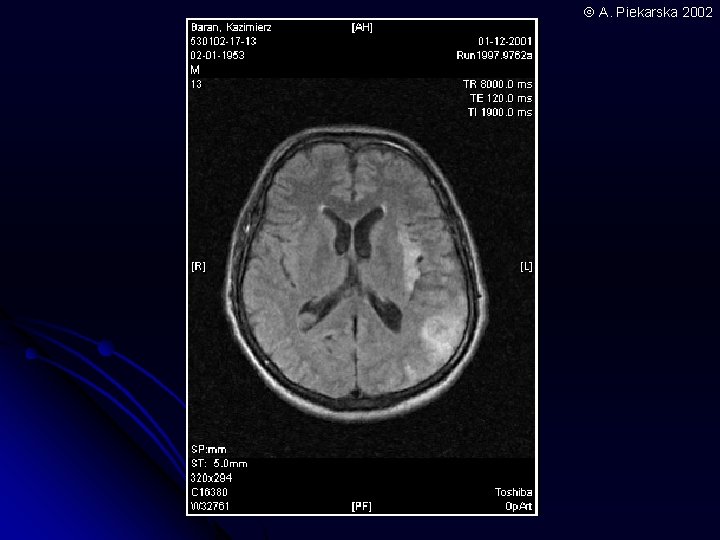
A. Piekarska 2002
A. Piekarska 2002
A. Piekarska 2002
A. Piekarska 2002
A. Piekarska 2002
A. Piekarska 2002
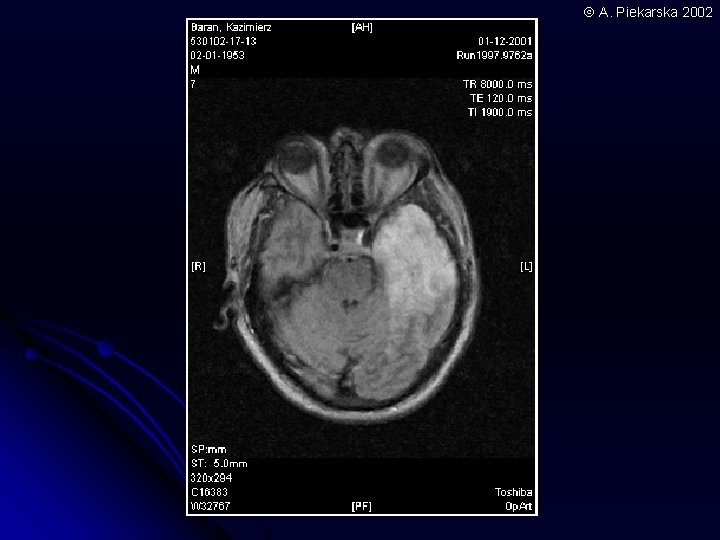
A. Piekarska 2002
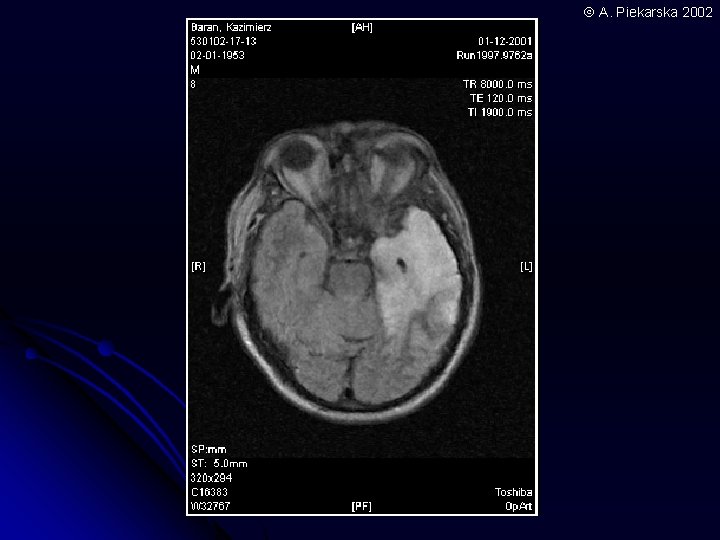
A. Piekarska 2002
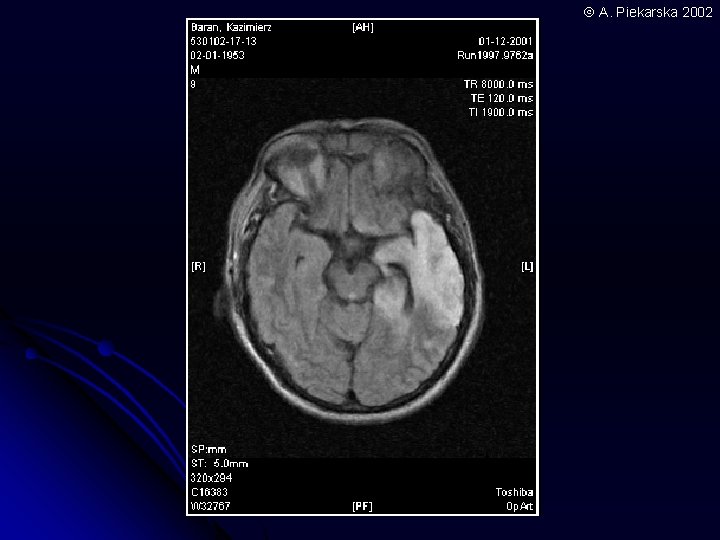
A. Piekarska 2002
Rabies Uniformly fatal in unimmunized individuals l Virus is occured in saliva of inected animals l l Skunk, raccoon, fox, wolf l Chiropter, squirrel l Virus replicate in bited muscles and migrate to neurons and gray substance of brain and to salivary glands, where is excrete
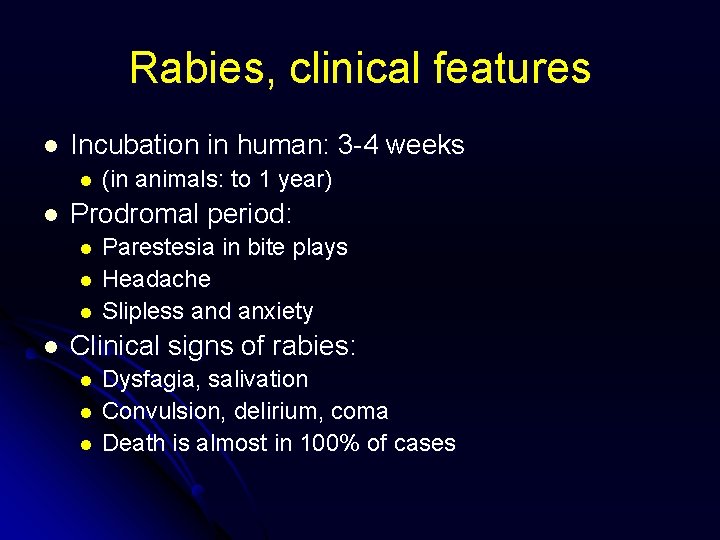
Rabies, clinical features l Incubation in human: 3 -4 weeks l l Prodromal period: l l (in animals: to 1 year) Parestesia in bite plays Headache Slipless and anxiety Clinical signs of rabies: l l l Dysfagia, salivation Convulsion, delirium, coma Death is almost in 100% of cases
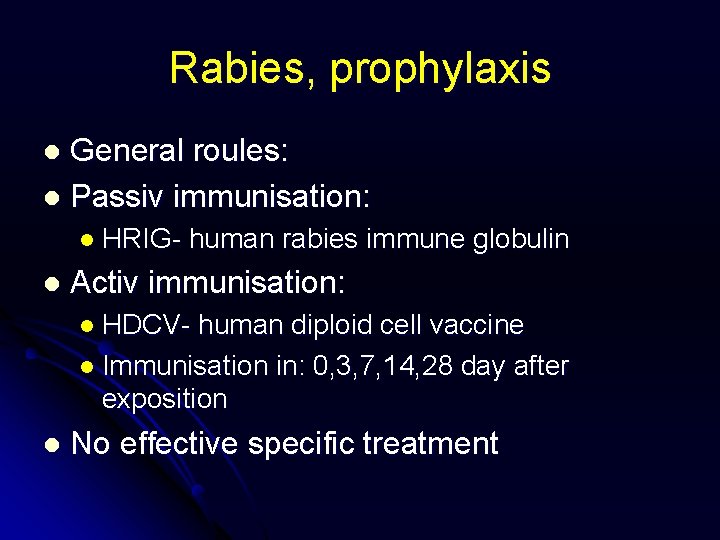
Rabies, prophylaxis General roules: l Passiv immunisation: l l HRIG- l human rabies immune globulin Activ immunisation: l HDCV- human diploid cell vaccine l Immunisation in: 0, 3, 7, 14, 28 day after exposition l No effective specific treatment
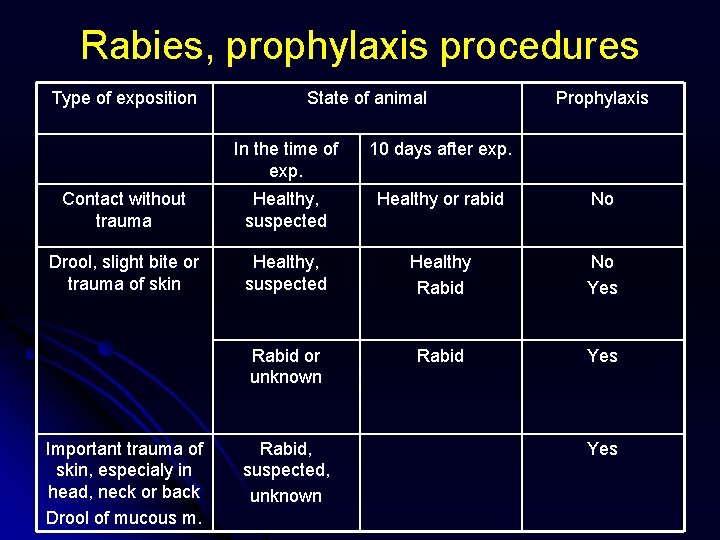
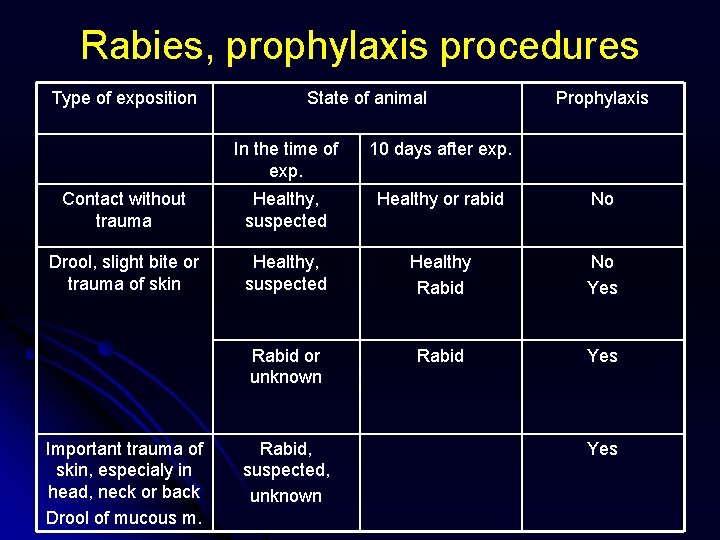
Rabies, prophylaxis procedures Type of exposition State of animal Prophylaxis In the time of exp. 10 days after exp. Contact without trauma Healthy, suspected Healthy or rabid No Drool, slight bite or trauma of skin Healthy, suspected Healthy Rabid No Yes Rabid or unknown Rabid Yes Important trauma of skin, especialy in head, neck or back Drool of mucous m. Rabid, suspected, unknown Yes
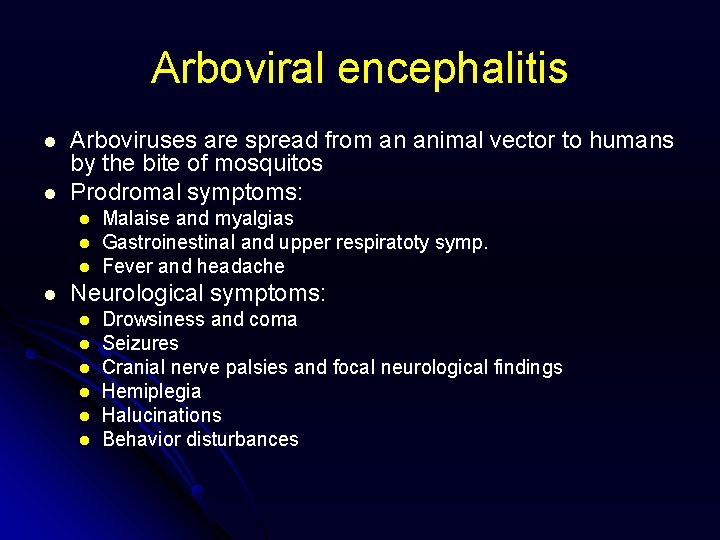
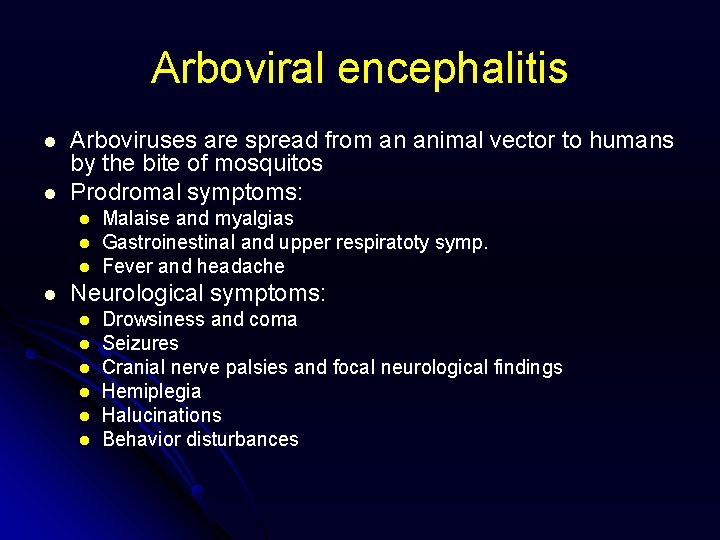
Arboviral encephalitis l l Arboviruses are spread from an animal vector to humans by the bite of mosquitos Prodromal symptoms: l l Malaise and myalgias Gastroinestinal and upper respiratoty symp. Fever and headache Neurological symptoms: l l l Drowsiness and coma Seizures Cranial nerve palsies and focal neurological findings Hemiplegia Halucinations Behavior disturbances
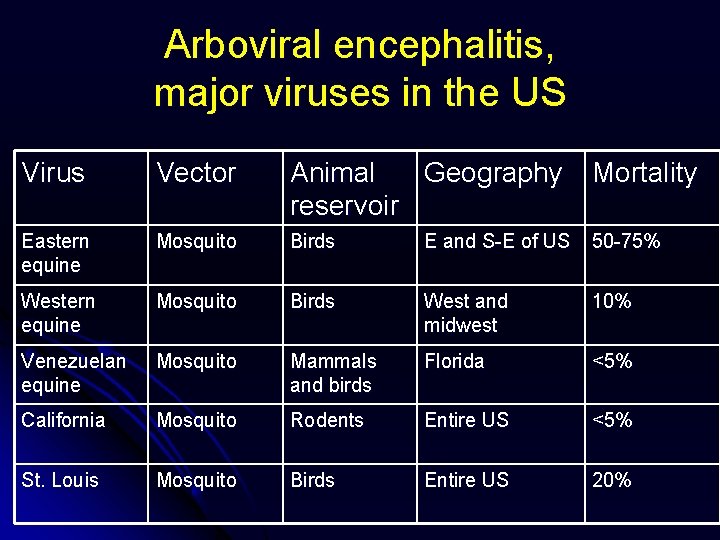
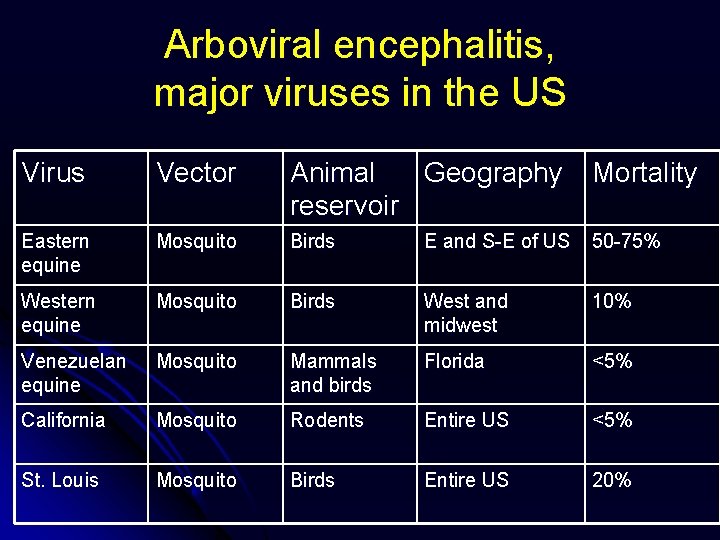
Arboviral encephalitis, major viruses in the US Virus Vector Animal Geography reservoir Mortality Eastern equine Mosquito Birds E and S-E of US 50 -75% Western equine Mosquito Birds West and midwest 10% Venezuelan equine Mosquito Mammals and birds Florida <5% California Mosquito Rodents Entire US <5% St. Louis Mosquito Birds Entire US 20%
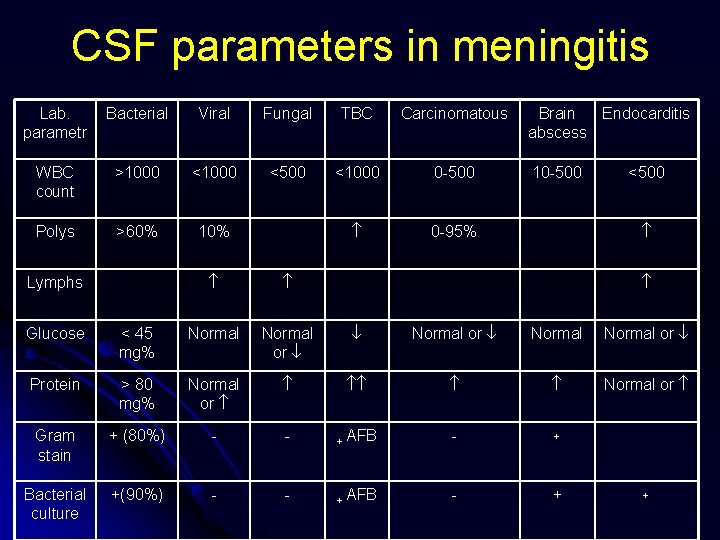
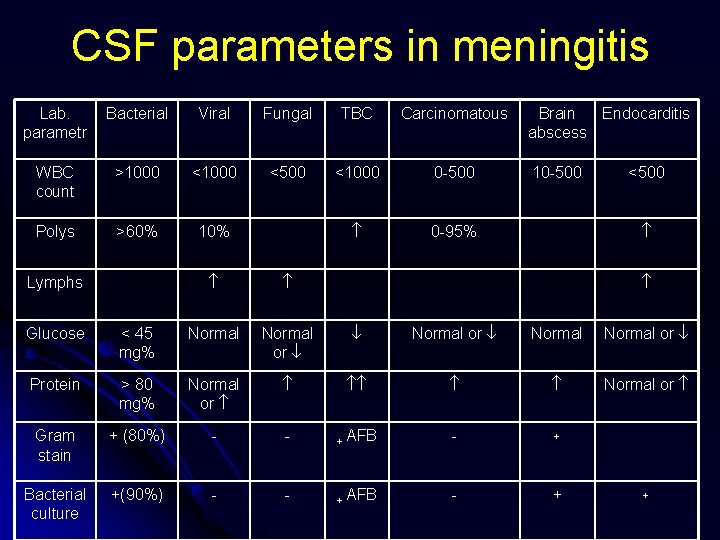
CSF parameters in meningitis Lab. parametr Bacterial Viral Fungal TBC Carcinomatous WBC count >1000 <500 <1000 0 -500 Polys >60% 10% 0 -95% Lymphs Brain Endocarditis abscess 10 -500 <500 Glucose < 45 mg% Normal or Normal or Protein > 80 mg% Normal or Gram stain + (80%) - - + AFB - + Bacterial culture +(90%) - - + AFB - + +
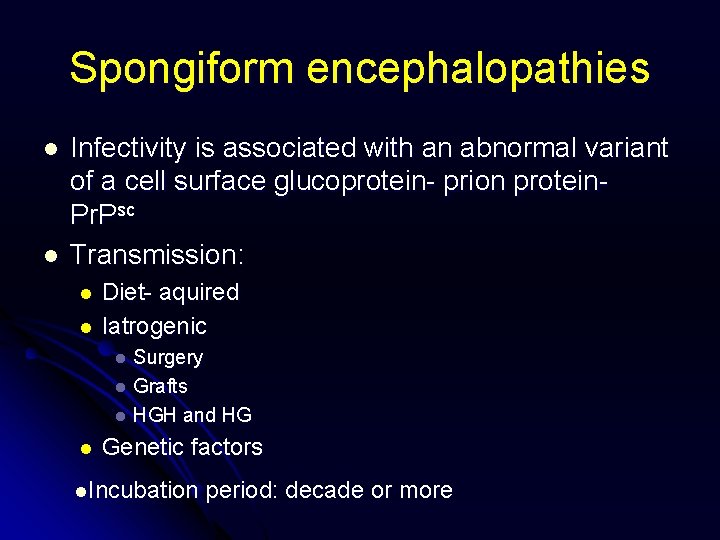
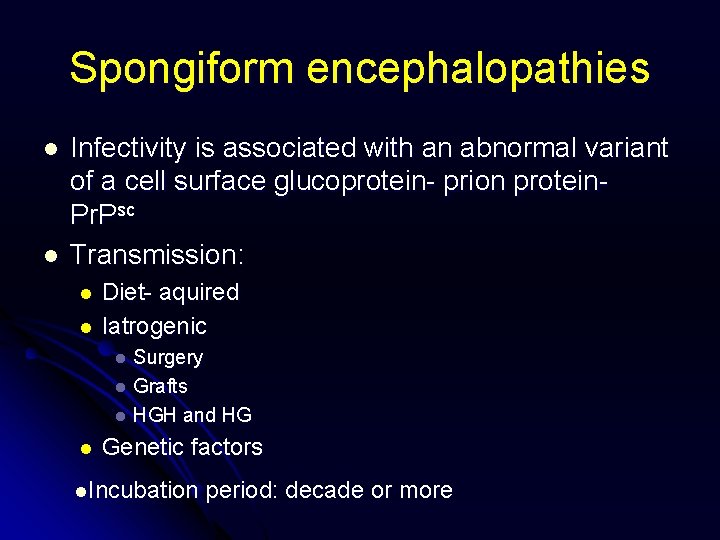
Spongiform encephalopathies l l Infectivity is associated with an abnormal variant of a cell surface glucoprotein- prion protein. Pr. Psc Transmission: l l Diet- aquired Iatrogenic Surgery l Grafts l HGH and HG l l Genetic factors l. Incubation period: decade or more
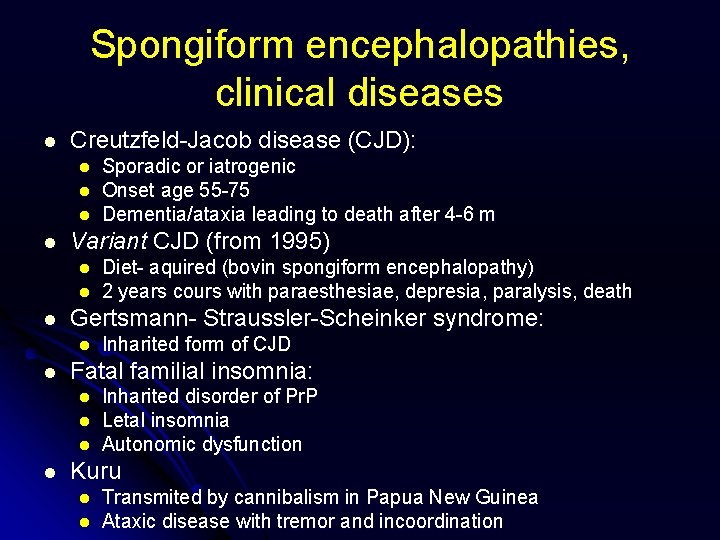
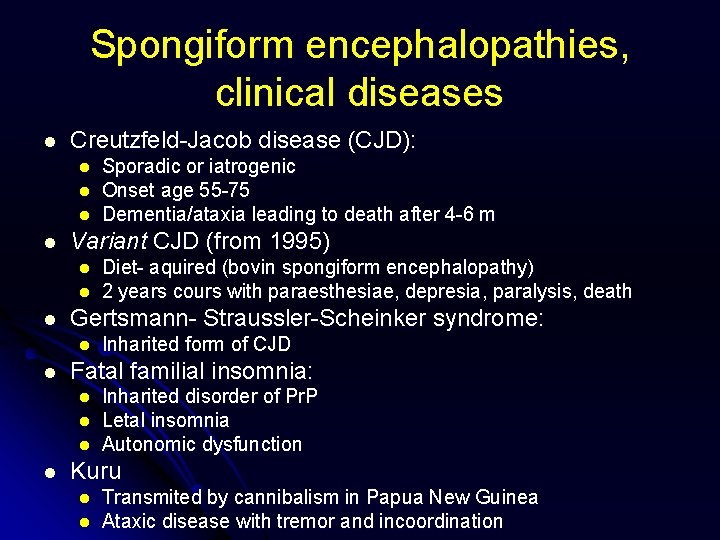
Spongiform encephalopathies, clinical diseases l Creutzfeld-Jacob disease (CJD): l l Variant CJD (from 1995) l l l Inharited form of CJD Fatal familial insomnia: l l Diet- aquired (bovin spongiform encephalopathy) 2 years cours with paraesthesiae, depresia, paralysis, death Gertsmann- Straussler-Scheinker syndrome: l l Sporadic or iatrogenic Onset age 55 -75 Dementia/ataxia leading to death after 4 -6 m Inharited disorder of Pr. P Letal insomnia Autonomic dysfunction Kuru l l Transmited by cannibalism in Papua New Guinea Ataxic disease with tremor and incoordination