Infections and Neuroimmune Disorders Hayley Gans MD Stanford

- Slides: 22
Infections and Neuroimmune Disorders Hayley Gans, MD Stanford University Medical Center Inflammatory Brain Disorder Conference May 14 th 2021
• No conflicts of interest
Infections and central nervous system • Neurotrophic • Neuroinflammatory • Neuroinfection & neuroimmunology is a growing sub-specialty of the nervous system. • Despite remarkable diagnostic and therapeutic advancements during the past 30 years through the prevention of infectious diseases by vaccine and the development of safe, effective antimicrobial agents, neurologic infections remain a major cause of permanent neurologic disability worldwide. • Immune-system-to-brain communication
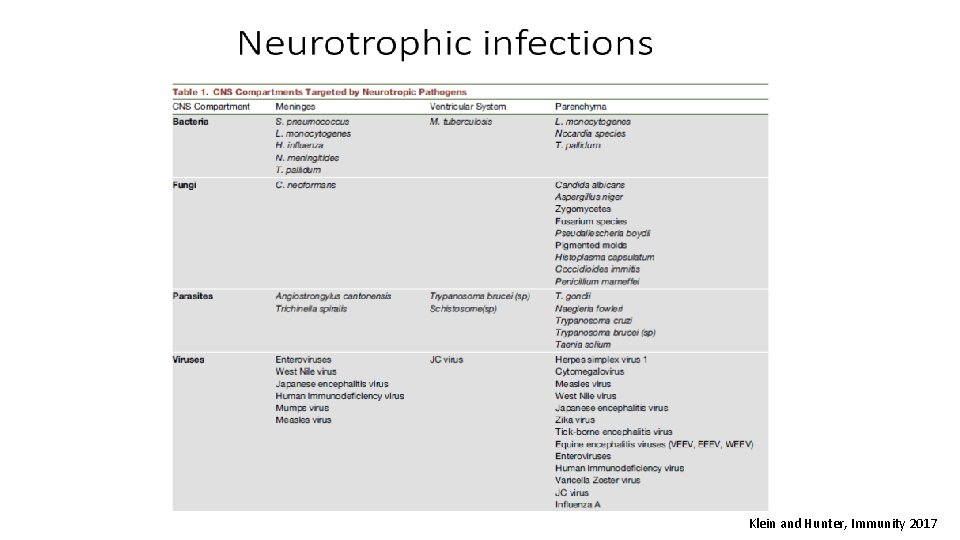
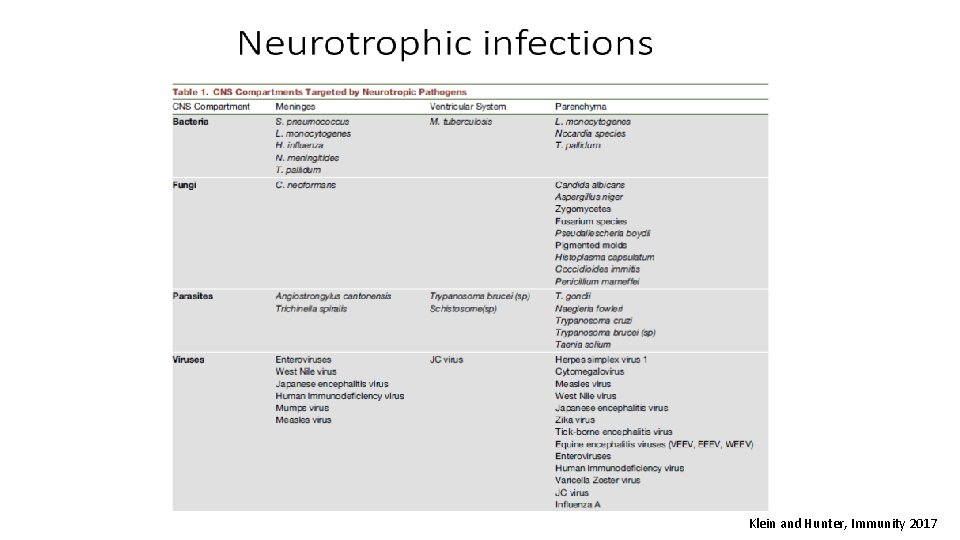
Klein and Hunter, Immunity 2017
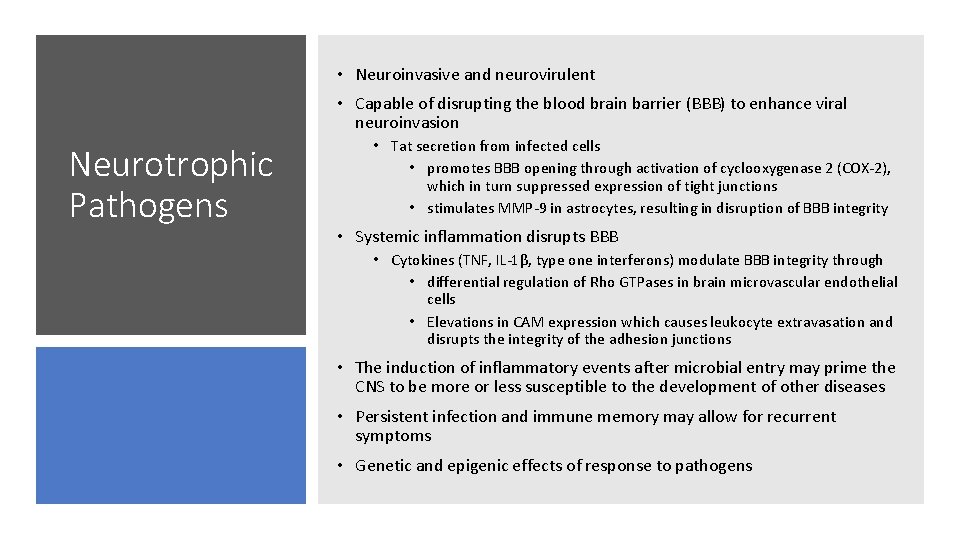
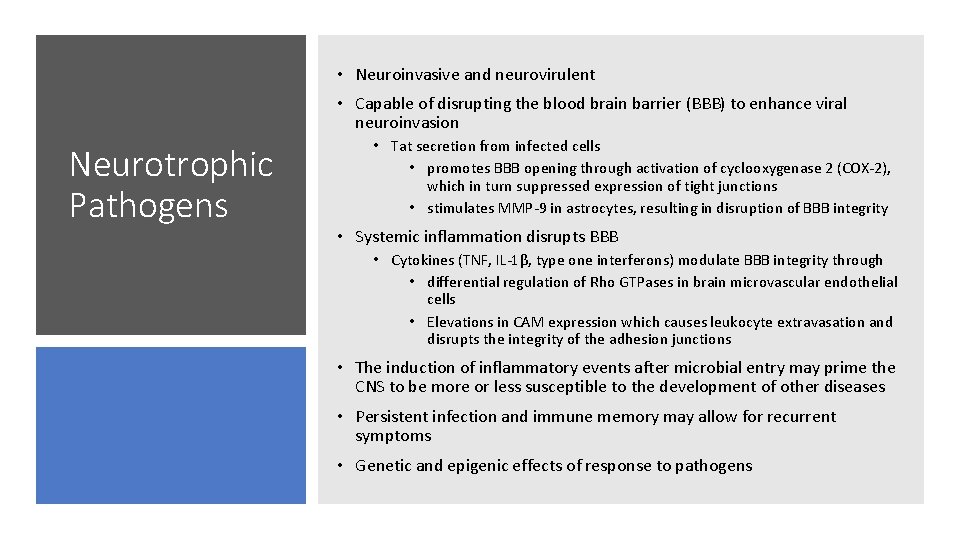
• Neuroinvasive and neurovirulent • Capable of disrupting the blood brain barrier (BBB) to enhance viral neuroinvasion Neurotrophic Pathogens • Tat secretion from infected cells • promotes BBB opening through activation of cyclooxygenase 2 (COX-2), which in turn suppressed expression of tight junctions • stimulates MMP-9 in astrocytes, resulting in disruption of BBB integrity • Systemic inflammation disrupts BBB • Cytokines (TNF, IL-1β, type one interferons) modulate BBB integrity through • differential regulation of Rho GTPases in brain microvascular endothelial cells • Elevations in CAM expression which causes leukocyte extravasation and disrupts the integrity of the adhesion junctions • The induction of inflammatory events after microbial entry may prime the CNS to be more or less susceptible to the development of other diseases • Persistent infection and immune memory may allow for recurrent symptoms • Genetic and epigenic effects of response to pathogens
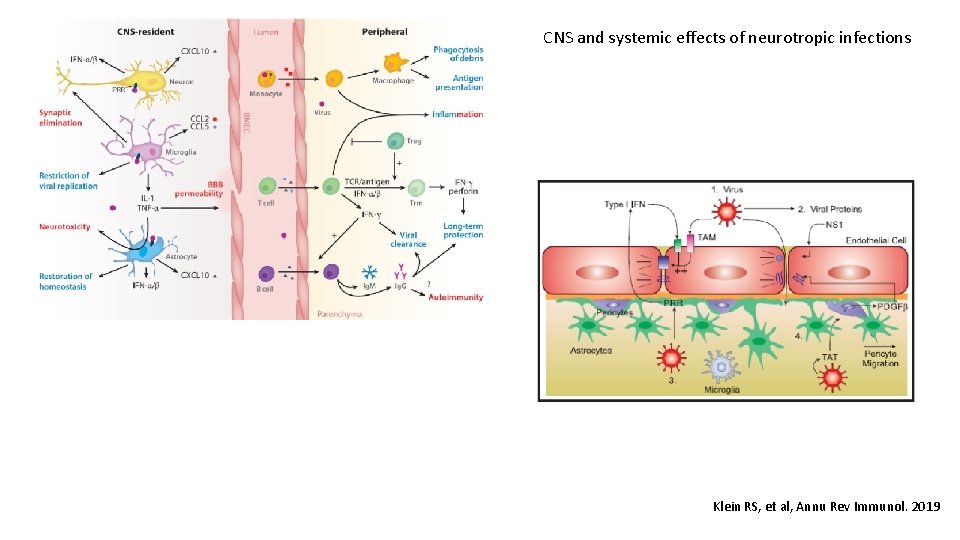
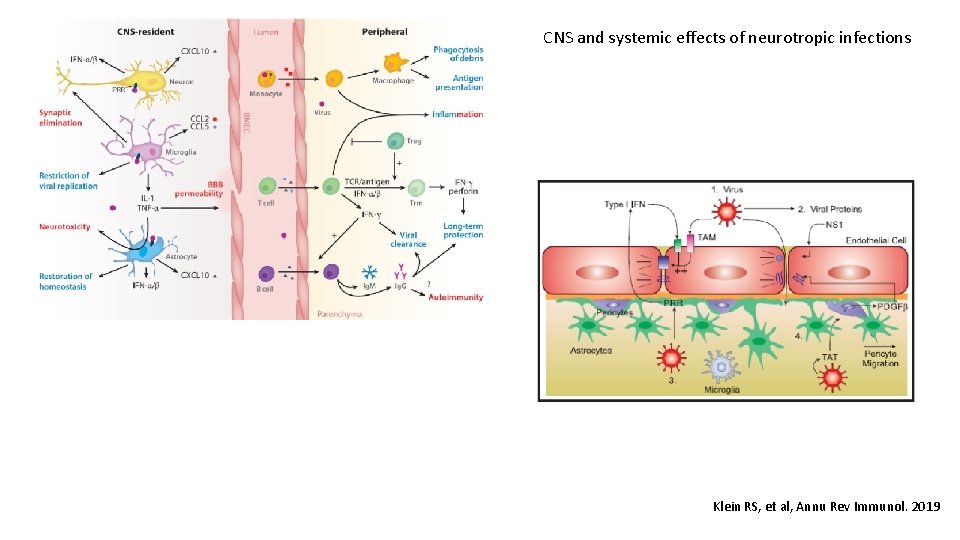
CNS and systemic effects of neurotropic infections Klein RS, et al, Annu Rev Immunol. 2019
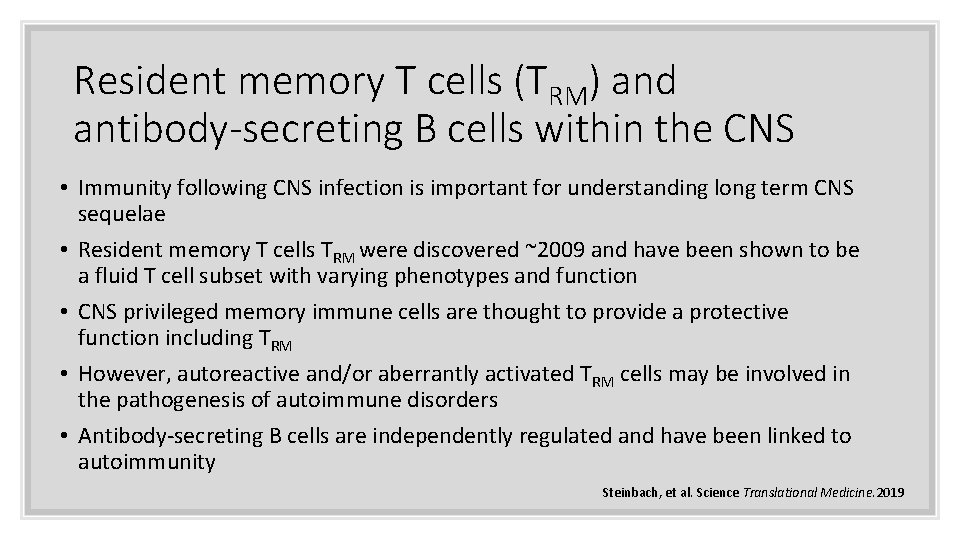
Resident memory T cells (TRM) and antibody-secreting B cells within the CNS • Immunity following CNS infection is important for understanding long term CNS sequelae • Resident memory T cells TRM were discovered ~2009 and have been shown to be a fluid T cell subset with varying phenotypes and function • CNS privileged memory immune cells are thought to provide a protective function including TRM • However, autoreactive and/or aberrantly activated TRM cells may be involved in the pathogenesis of autoimmune disorders • Antibody-secreting B cells are independently regulated and have been linked to autoimmunity Steinbach, et al. Science Translational Medicine. 2019
Neuroimmunology • Neuroimmune disorders are a heterogeneous group of severe neurological conditions primarily characterized by inflammatory responses in the CNS • Distinct manifestations in childhood, adolescent and adulthood • Each entity rare but as a group are not uncommon • Heightened immune responses against the CNS • cell- mediated, humorally mediated, infection triggered and genetically defined mechanisms • Immune activity as causal or secondary is not fully understood • Unifying aspect is that the disease course can be modulated by immune- targeted therapies. Wells, et al, Nat Rev Neurol 14. 2018
Neuroimmune disorders • Acute disseminated encephalomyelitis (ADEM), acute flaccid myelitis (AFM), , neuromyelitis optica spectrum disorder (NMOSD), optic neuritis (ON), and transverse myelitis (TM), Guillain-Barré syndrome (GBS) • Antibodies against N-methyl-D-aspartate receptor (NMDAR), voltage-gated potassium channel complex proteins, glutamic acid decarboxylase acid, gammaaminobutyric acid (GABA) B, MOG antibody disease (MOGAD)
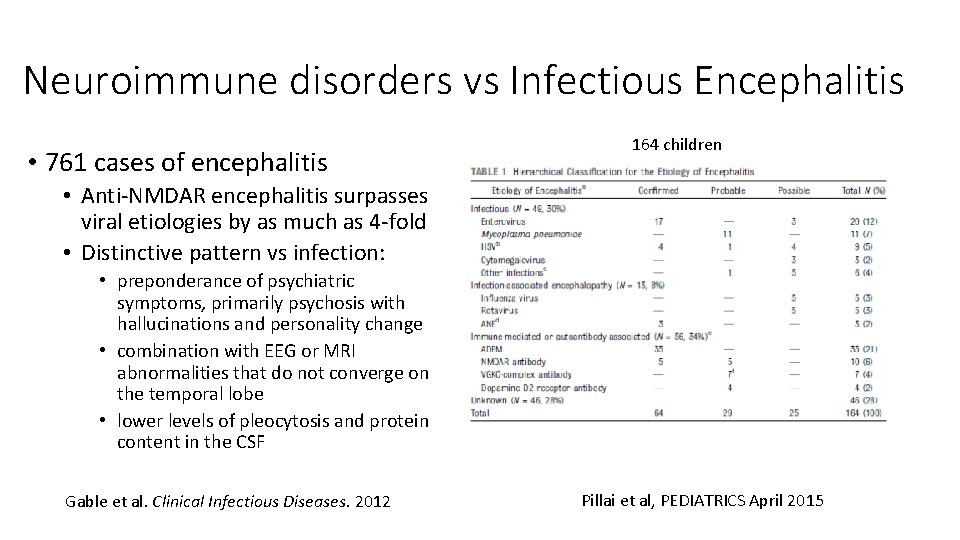
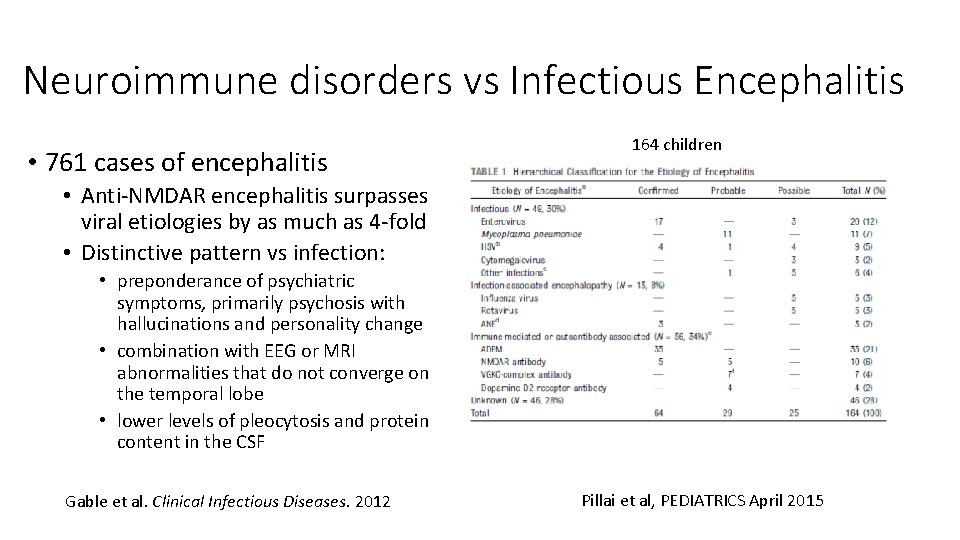
Neuroimmune disorders vs Infectious Encephalitis • 761 cases of encephalitis 164 children • Anti-NMDAR encephalitis surpasses viral etiologies by as much as 4 -fold • Distinctive pattern vs infection: • preponderance of psychiatric symptoms, primarily psychosis with hallucinations and personality change • combination with EEG or MRI abnormalities that do not converge on the temporal lobe • lower levels of pleocytosis and protein content in the CSF Gable et al. Clinical Infectious Diseases. 2012 Pillai et al, PEDIATRICS April 2015
Infections Associated with Neuroimmune Disease • Anti-NMDA antibody induced encephalitis • herpes simplex virus, varicella-zoster, Epstein-Barr, measles virus, mumps, group A hemolytic streptococcus, toxoplasma, Chlamydophila pneumoniae, Bordetella pertussis, Bordetella parapertussis, mycoplasma pneumoniae • ADEM • coronavirus, coxsackie, cytomegalovirus, Epstein-Barr, herpes simplex, hepatitis A, HIV, influenza, measles, rubella, varicella zoster, and West Nile virus. Other associated organisms associated include Borrelia burgdorferi, chlamydia, Leptospira, Mycoplasma pneumoniae, rickettsia, and beta hemolytic Streptococcus • GBS • Campylobacter, cytomegalovirus, Epstein-Barr virus, Mycoplasma pneumoniae, and influenza-like illnesses, HIV • Pediatric acute-onset neuropsychiatric syndrome (PANS) or childhood acute neuropsychiatric symptoms (CANS) • beta hemolytic Streptococcus: PANDAS • Mycoplasma pneumoniae, influenza, Epstein-Barr virus, Lyme disease
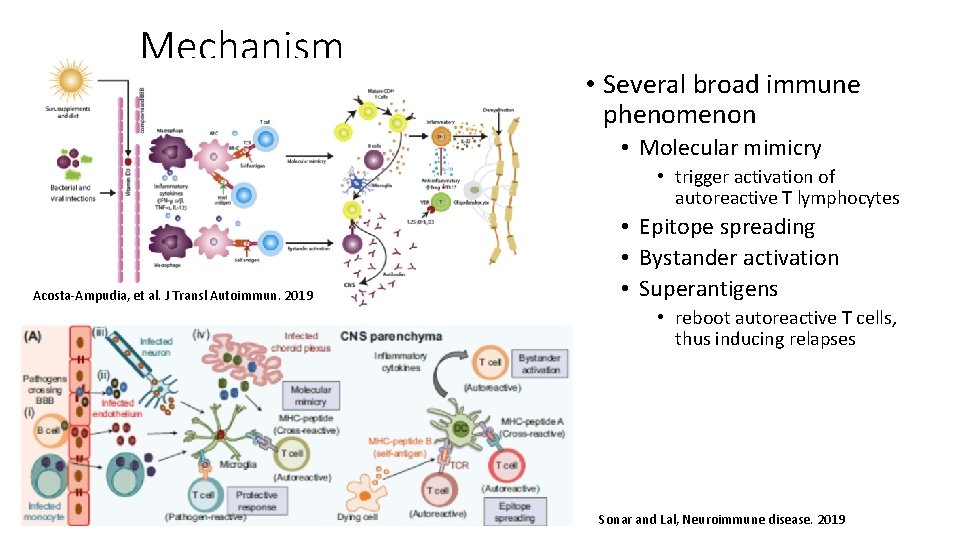
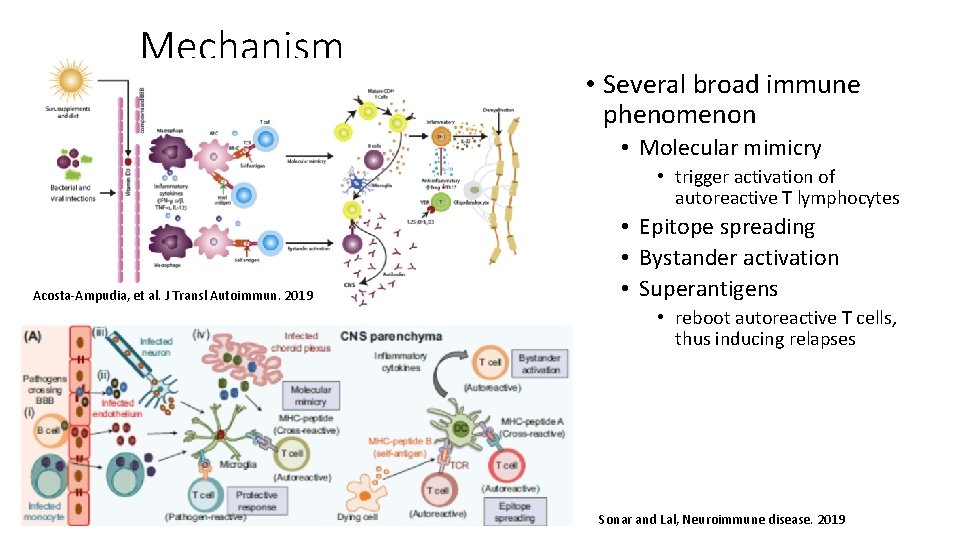
Mechanism • Several broad immune phenomenon • Molecular mimicry • trigger activation of autoreactive T lymphocytes Acosta-Ampudia, et al. J Transl Autoimmun. 2019 • Epitope spreading • Bystander activation • Superantigens • reboot autoreactive T cells, thus inducing relapses Sonar and Lal, Neuroimmune disease. 2019
• Immune activation against neuronal antigens • Involvement of both the autoantibodies and autoreactive T cells • Strong association of human leukocyte antigen (HLA) polymorphism supporting role for both CD 4 and CD 8 T cells Mechanisms • Pathogen-derived molecules show molecular mimicry to the myelin and other CNS antigens • L 2 protein of human papillomavirus 7, DNA polymerase of EBV and HSV, and hemagglutinin of influenza virus mimic human MBP 85– 99 epitope • DNA polymerase of HBV mimics human MBP 66– 75 • Human CMV capsid protein UL 86 981– 1003 mimics the rat MOG • immunodominant glycoproteins of C. jejuni, lipooligosaccharides (LOS), and lipopolysaccharide (LPS) closely resemble the neuronal gangliosides such as GM 1, GD 1 a, GM 1/GD 1 complex and induce cross-reactive autoantibodies and effector T cells • M. pneumoniae and H. influenzae thought to cause GBS through the molecular mimicry of bacterial glycolipids with myelin galactocerebroside (Gal-C) • group A β-hemolytic streptococcus (GABHS) : generates antibodies against epitopes on the basal ganglia
• Interleukin-6 (IL-6), interleukin-17 A (IL-17 A), and C-X-C motif chemokine 13 (CXCL 13) elevations Mechanism • negatively regulate the tight junction molecules, and prompt leukocyte migrating across the blood-brain barrier • Stimulate B cell differentiation, enhance the survival of plasmablasts, and promote antibody production • And IL-17 A may trigger a positive-feedback loop for IL-6 signaling through signal transducer and activator of transcription 3 (STAT 3) and nuclear factor (NF)-κB • IL-17 promotes blood-brain barrier breakdown, Ig. G deposition, microglial activation, and loss of excitatory synaptic proteins • Initial infection may set up subsequent IL-17 expression from primed autoreactive Th 17 cells during flare-ups caused by other pathogens including the influenza virus, mycoplasma, and staphylococcus aureus that are able to induce a robust Th 17 cellular response.
PANDAS/PANS natural history • Prospective study in PANDAS patients; 40 matched case-controls • Initial diagnosis showed association of cases with GABHS • Exacerbations not associated with GABHS • 715 children with chronic tic disorder followed prospectively • Did not detect any significant association of any of the 4 GAS exposure definitions with tic exacerbations (odds ratios ranging between 1. 006 and 1. 235, all p values >0. 3) • Specific workup or active management of GAS infections is unlikely to help modify the course of tics in CTD and is therefore not recommended • Prospective randomized study of 31 children with PANS receiving azithromycin or placebo for 4 weeks with standard neuropsychiatric medication • Greater reduction in the Clinical Global Impression-Severity Scale (CGI-S) for OCD symptoms in the azithromycin group • Other neuropsychiatric outcomes did not differ • 12 children with new-onset PANDAS followed for 3 years • All positive for GABHS and treated with resolution of symptoms • 6 had recurrences, all positive and treated for GABHS with resolution • Kurlan, Pediatrics. 2008 • Martino et al, Neurology. 2021 • Murphy et al, J Child Adolesc Psychopharmacol. 2017 • Murphy and Pichichero, Arch Pediatr Adolesc Med. 2002
PANDAS and prophylaxis • 40 children with PANDAS followed in an 8 -mo. prospective, randomized cross-over trial of 4 months of prophylaxis • Equal number of infections in both the active and placebo phases of the study. • There was no significant change seen in either the obsessive-compulsive or tic symptom severity between the two phases. • 23 children with PANDAS followed for a year, randomized, double-blind study • Significant decreases in streptococcal infections and neuropsychiatric exacerbations during the study year compared with baseline year Garvey, et al: Biol Psychiatry. 1999 Snider, et al: Biol Psychiatry. 2005
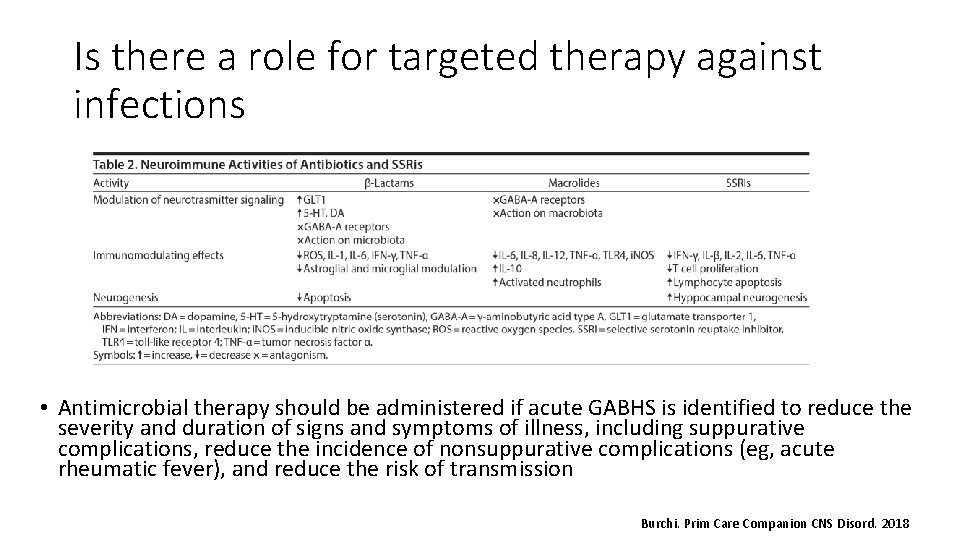
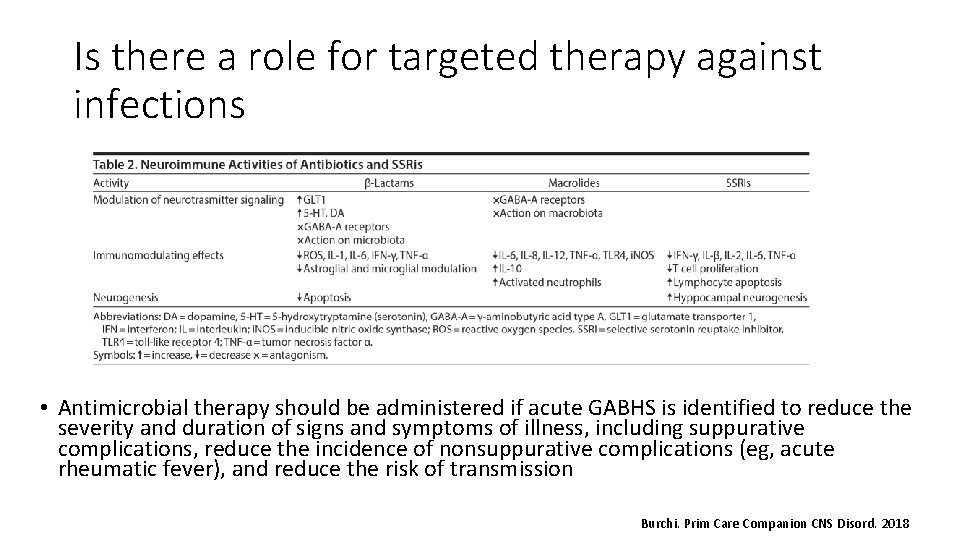
Is there a role for targeted therapy against infections • Antimicrobial therapy should be administered if acute GABHS is identified to reduce the severity and duration of signs and symptoms of illness, including suppurative complications, reduce the incidence of nonsuppurative complications (eg, acute rheumatic fever), and reduce the risk of transmission Burchi. Prim Care Companion CNS Disord. 2018
Should Immunosuppression be delayed • Is there risk for worsening a CNS infection if present • In era of molecular diagnostics, potential to r/o infection in timely fashion does exist • Corticosteroids are of proven benefit when combined with antiinfectious therapies for the specific brain infections (pneumococcus, tuberculosis, HSV) • HSV has been shown to reactivate in vitro in the presence of dexamethasone • HSV induced anti- NMDA receptor encephalitis showed no viral reaction in the 93% who received immunosuppression and no anti-viral therapy Wells, etc al. Nat Rev Neurol 14, 2018. PMID: 29925924
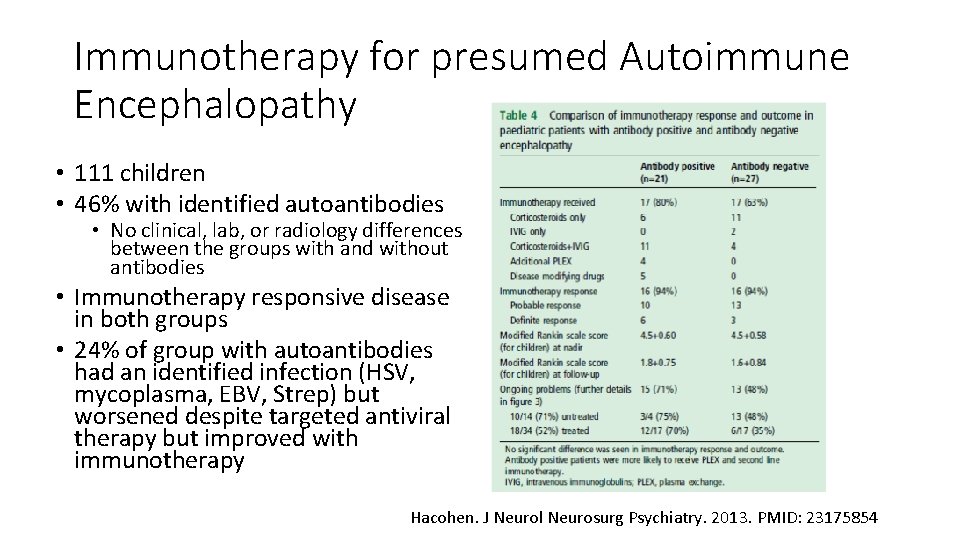
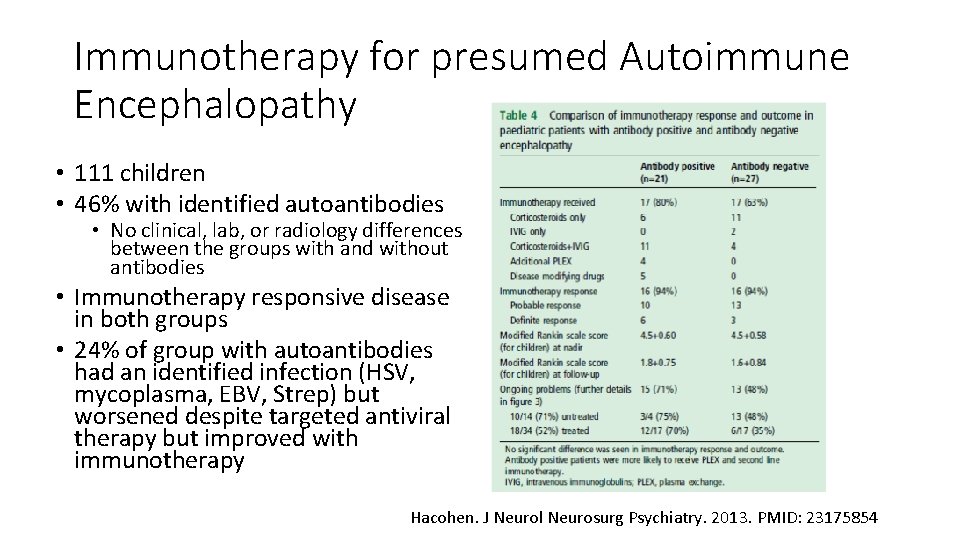
Immunotherapy for presumed Autoimmune Encephalopathy • 111 children • 46% with identified autoantibodies • No clinical, lab, or radiology differences between the groups with and without antibodies • Immunotherapy responsive disease in both groups • 24% of group with autoantibodies had an identified infection (HSV, mycoplasma, EBV, Strep) but worsened despite targeted antiviral therapy but improved with immunotherapy Hacohen. J Neurol Neurosurg Psychiatry. 2013. PMID: 23175854
• Common pathway for infectious induced neuroimmune disorders is immune dysregulation • Molecular diagnostics may be helpful in ruling out infectious that would worsen with immunotherapy Summary • While some entities may be ‘improved” with anti-microbial directed therapy, prospective, controlled studies in comparison to immunosuppression do not exist, and it is unclear if it is the immunosuppressive qualities of antimicrobial therapy was the effective therapeutic • Acute infections should be treated • Early effective immunosuppression is associated with better long-term prognosis; thus, delay is not substantiated by the potential infectious risk if autoimmune disease is substantiated • Specific immune abnormalities are hall marks of different neuroimmune disorders that may direct immunotherapy modalities which requires

Questions Thanks
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Klein RS, Hunter CA. Protective and Pathological Immunity during Central Nervous System Infections. Immunity. 2017; 46(6): 891 -909. Klein RS, Garber C, Funk KE, et al. Neuroinflammation During RNA Viral Infections. Annual Review of Immunology. 2019; 37(1): 73 -95. Sonar SA, Lal G. Overview of Mechanisms Underlying Neuroimmune Diseases. In: Springer International Publishing; 2019: 3 -62. Steinbach K, Vincenti I, Egervari K, et al. Brain-resident memory T cells generated early in life predispose to autoimmune disease in mice. Science Translational Medicine. 2019; 11(498): eaav 5519. Wells E, Hacohen Y, Waldman A, et al. Neuroimmune disorders of the central nervous system in children in the molecular era. Nature Reviews Neurology. 2018; 14(7): 433 -445. Acosta-Ampudia Y, Monsalve DM, Ramirez-Santana C. Identifying the culprits in neurological autoimmune diseases. J Transl Autoimmun. 2019; 2: 100015. Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis. 2012; 54(7): 899 -904. Pillai SC, Hacohen Y, Tantsis E, et al. Infectious and autoantibody-associated encephalitis: clinical features and long-term outcome. Pediatrics. 2015; 135(4): e 974 -984. Kurlan R, Johnson D, Kaplan EL. Streptococcal Infection and Exacerbations of Childhood Tics and Obsessive-Compulsive Symptoms: A Prospective Blinded Cohort Study. PEDIATRICS. 2008; 121(6): 1188 -1197. Martino D, Schrag A, Anastasiou Z, et al. Association of Group A Streptococcus Exposure and Exacerbations of Chronic Tic Disorders. Neurology. 2021; 96(12): e 1680 -e 1693. Murphy ML, Pichichero ME. Prospective identification and treatment of children with pediatric autoimmune neuropsychiatric disorder associated with group A streptococcal infection (PANDAS). Arch Pediatr Adolesc Med. 2002; 156(4): 356 -361. Murphy TK, Brennan EM, Johnco C, et al. A Double-Blind Randomized Placebo-Controlled Pilot Study of Azithromycin in Youth with Acute-Onset Obsessive–Compulsive Disorder. Journal of Child and Adolescent Psychopharmacology. 2017; 27(7): 640 -651. Garvey MA, Perlmutter SJ, Allen AJ, et al. A pilot study of penicillin prophylaxis for neuropsychiatric exacerbations triggered by streptococcal infections. Biol Psychiatry. 1999; 45(12): 1564 -1571. Snider LA, Lougee L, Slattery M, Grant P, Swedo SE. Antibiotic prophylaxis with azithromycin or penicillin for childhood-onset neuropsychiatric disorders. Biol Psychiatry. 2005; 57(7): 788 -792. Burchi E, Pallanti S. Antibiotics for PANDAS? Limited Evidence: Review and Putative Mechanisms of Action. Prim Care Companion CNS Disord. 2018; 20(3). Hacohen Y, Wright S, Waters P, et al. Paediatric autoimmune encephalopathies: clinical features, laboratory investigations and outcomes in patients with or without antibodies to known central nervous system autoantigens. Journal of Neurology, Neurosurgery & Psychiatry. 2013; 84(7): 748 -755.