INFECTION PREVENTION AND CONTROL BEGINS WITH YOU BREAKING
INFECTION PREVENTION AND CONTROL BEGINS WITH YOU
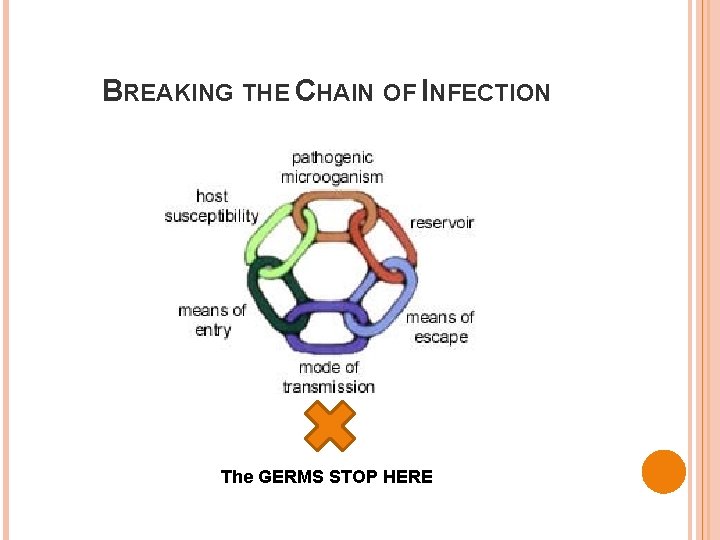
BREAKING THE CHAIN OF INFECTION The GERMS STOP HERE
HAND HYGIENE 10 Greatest Carriers of Germs are the Fingers
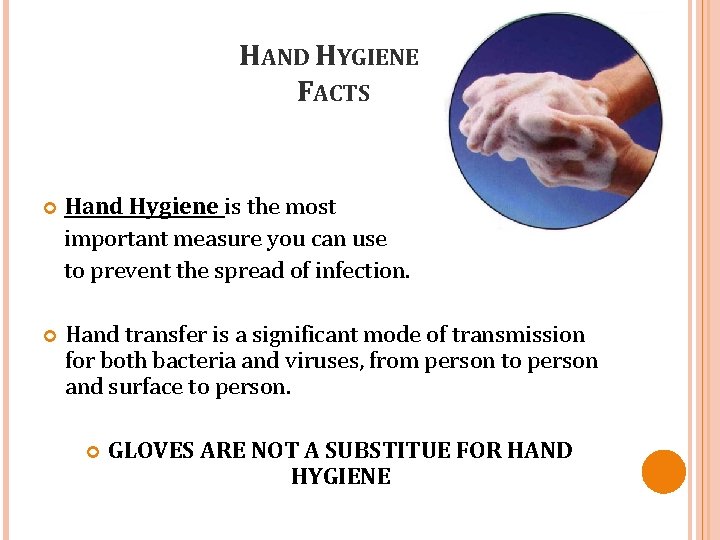
HAND HYGIENE FACTS Hand Hygiene is the most important measure you can use to prevent the spread of infection. Hand transfer is a significant mode of transmission for both bacteria and viruses, from person to person and surface to person. GLOVES ARE NOT A SUBSTITUE FOR HAND HYGIENE
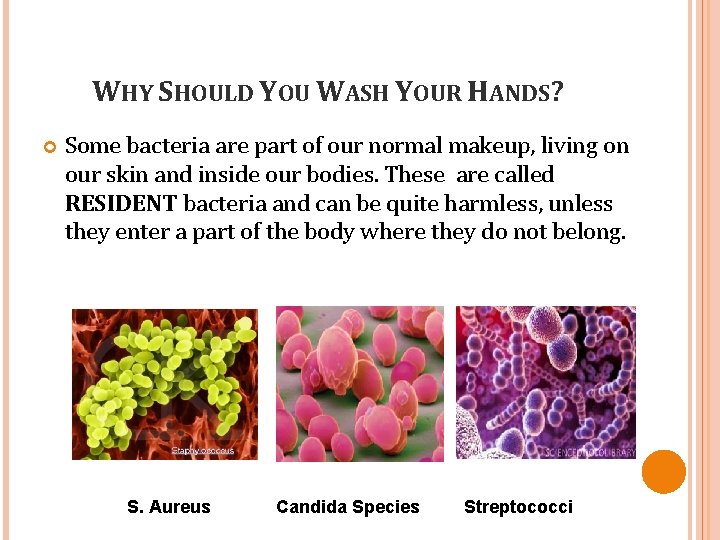
WHY SHOULD YOU WASH YOUR HANDS? Some bacteria are part of our normal makeup, living on our skin and inside our bodies. These are called RESIDENT bacteria and can be quite harmless, unless they enter a part of the body where they do not belong. S. Aureus Candida Species Streptococci

WHY SHOULD YOU WASH YOUR HANDS? Other bacteria are picked up when touching a contaminated patient or surface. These are called TRANSIENT bacteria and can be carried on your hands or equipment from one patient to another or another surface. Clostridium difficile MRSA VRE
TRANSIENT FLORA Ø Ø Ø ALL THE OTHER MICROBES YOU PICK UP INADVERTENTLY: While raising bedside rails or casually leaning against them while chatting… When taking a pulse or blood pressure… When leaving your notebook and pen on a bedside table… When opening a door, using the phone, typing at the keyboard… When shaking someone’s hand. . .
HAND HYGIENE Alcohol hand antiseptics (waterless hand rub) remove microbes from healthcare providers hands. If hands are visibly soiled, soap and water hand washing is required. � The effectiveness of alcohol-based products may be reduced in the presence of substantial organic matter *If patient has been diagnosed with C difficile soap and water hand washing is required.
IT’S ALL ABOUT THE HANDS Skin around fingernails harbors high concentration of bacteria. Fact: Microbial count is higher underneath the fingernails than anywhere else on your hands Keep your natural nails short (fingertip length) Remove chipped nail polish No cosmetically enhanced nails Fact: More likely to harbor harmful microorganisms
WHEN DO YOU PERFORM HAND HYGIENE? Wash your hands: � Before and After patient contact � After gloves are removed � Between tasks on the same patient to prevent cross- contamination of different body sites
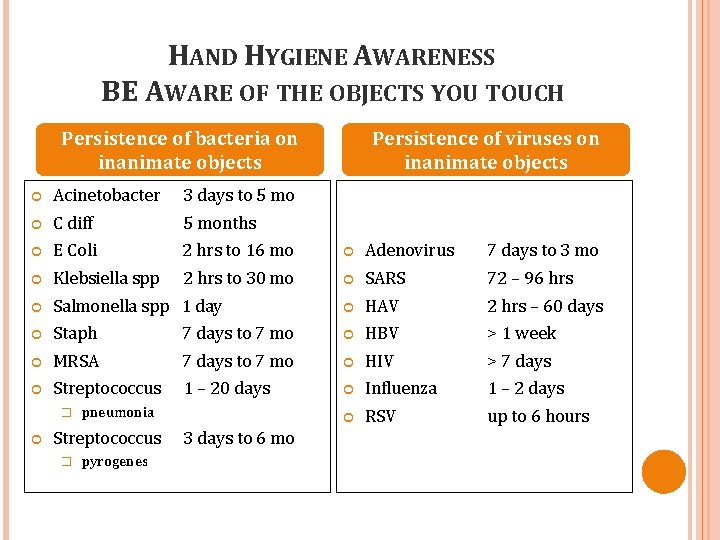
HAND HYGIENE AWARENESS BE AWARE OF THE OBJECTS YOU TOUCH Persistence of bacteria on inanimate objects Persistence of viruses on inanimate objects Acinetobacter 3 days to 5 mo C diff 5 months E Coli 2 hrs to 16 mo Adenovirus 7 days to 3 mo Klebsiella spp 2 hrs to 30 mo SARS 72 – 96 hrs Salmonella spp 1 day HAV 2 hrs – 60 days Staph 7 days to 7 mo HBV > 1 week MRSA 7 days to 7 mo HIV > 7 days Streptococcus 1 – 20 days Influenza 1 – 2 days RSV up to 6 hours � pneumonia Streptococcus � pyrogenes 3 days to 6 mo
STANDARD PRECAUTIONS Standard precautions are meant to reduce the risk of transmission of bloodborne and other pathogens from both recognized and unrecognized sources. Apply standard precaution to all: � Patients � Contaminated equipment and surfaces Use good judgment to determine when personal protective equipment (ppe) in necessary
STANDARD PRECAUTIONS Wear gloves if likely to contact: � Blood � Body fluids � Secretions � Excretions � Mucous membranes � Contaminated items or surfaces

STANDARD PRECAUTIONS Wear protective fluid resistant Yellow impervious gown or Yellow fluid proof apron when likely to soil skin or clothes with blood or body fluids, examples are: � Washing instrumentation � Isolation precaution patients
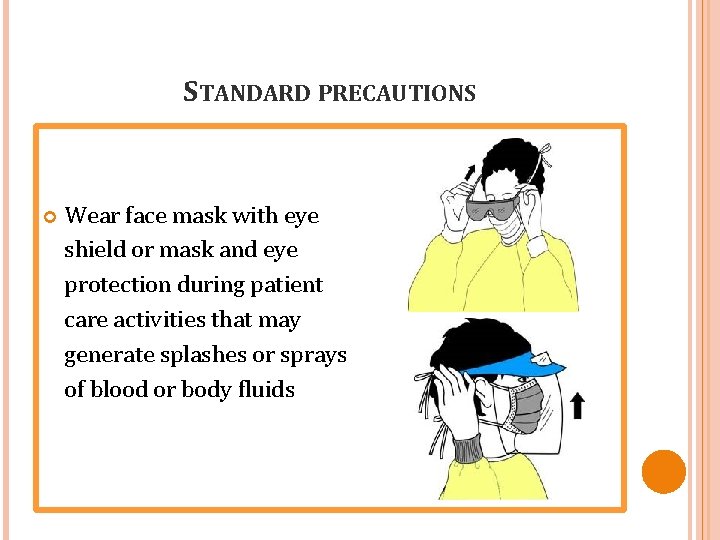
STANDARD PRECAUTIONS Wear face mask with eye shield or mask and eye protection during patient care activities that may generate splashes or sprays of blood or body fluids
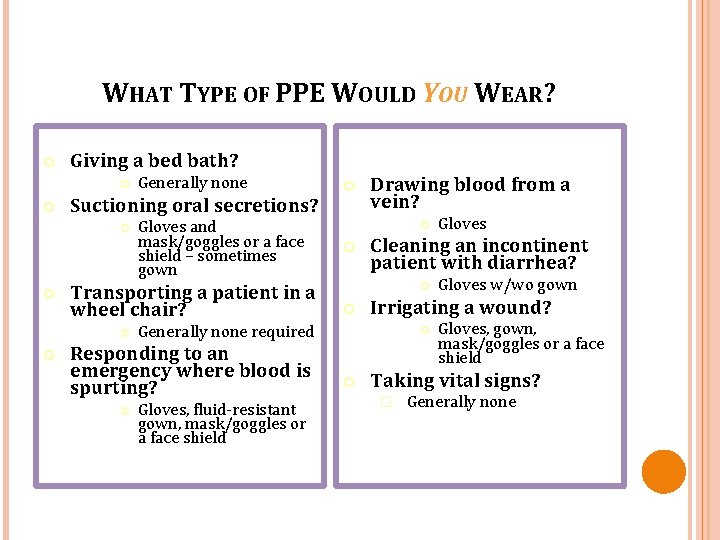
WHAT TYPE OF PPE WOULD YOU WEAR? Giving a bed bath? Suctioning oral secretions? Gloves and mask/goggles or a face shield – sometimes gown Transporting a patient in a wheel chair? Generally none Drawing blood from a vein? Gloves, fluid-resistant gown, mask/goggles or a face shield Gloves w/wo gown Irrigating a wound? Gloves Cleaning an incontinent patient with diarrhea? Generally none required Responding to an emergency where blood is spurting? Gloves, gown, mask/goggles or a face shield Taking vital signs? � Generally none
STANDARD PRECAUTIONS Remove gloves, gown, mask and eye protection before leaving the work area. � Each are a One time use Gloves, gown, mask are NOT worn in halls, elevators, cafeteria, or gift Shoppe.
PPE FOR EXPANDED PRECAUTIONS • Expanded Precautions include – Contact Precautions – Droplet Precautions – Airborne Infection Isolation

USE OF PPE FOR EXPANDED PRECAUTIONS • Contact Precautions – Gown and gloves for contact with patient or environment of care (e. g. , medical equipment, environmental surfaces) examples are MDRO’s � * In some instances these are required for entering patient’s environment • • Droplet Precautions – Surgical masks within 3 feet of patient, transmitted when coughing sneezing, laughing ect. Airborne Infection Isolation – Particulate respirator, examples are TB, measles, chicken pox and disseminated shingles. � * Negative pressure isolation room also required
TRANSMISSION BASED PRECAUTIONS “CONTACT Direct Contact Transmission Infectious organisms on the skin, in a body substance, or on the hands of one person are acquired directly by another person Indirect Contact Transmission Infectious organisms are acquired indirectly from contact with contaminated objects or surfaces
TRANSMISSION BASED PRECAUTIONS “DROPLET” n n n Direct contact of conjunctivae or mucous membranes with large droplet > 5 microns Droplets land on surfaces close to patient and are acquired indirectly by HCWs Droplets are NOT a form of airborne transmission but of indirect contact
TRANSMISSION BASED PRECAUTIONS “AIRBORNE” Infectious droplet nuclei =< 5 microns aerosolized during coughing, speaking or singing, travel on air currents and are inhaled
TUBERCULOSIS What is Tuberculosis? Infectious disease caused by bacteria. Usually affects lungs. Other body parts can be affected. Tuberculosis Transmission Spread through air (droplet nuclei). Sneezing, coughing, speaking, singing by individual with TB disease. Sharing the same air space with persons with infectious TB disease.
TUBERCULOSIS If you suspect a patient has TB they are to be placed in a Negative Airflow room � *Door must remain closed to ensure negative pressure ppe = N-95 Respirator for staff entering the room If a patient is to be transported to other areas a surgical mask shall be worn by the patient during transport. � *Transport is not preferred. Notify the Infection Control nurse and the Community Health Department Tests to anticipate the patient will receive are: � � � TST Sputum Cultures for AFB Chest X-Ray
TUBERCULOSIS Annual TB testing via tuberculin skin test (TST) will be conducted for all employees at MRHC Employees with a documented history of positive TST will not undergo testing. Instead they will complete an annual TB evaluation. Fit mask testing for direct care employees is completed on hire and if physical changes occur such: � Weight loss, weight gain � Employee cannot remember mask they wear � Facial hair � Facial surgery

STANDARD PRECAUTIONS Clean re-useable equipment between patients to prevent transfer of microorganisms to other patients, staff or environment, examples: Stethoscope, BP monitor, bladder scanner ect…

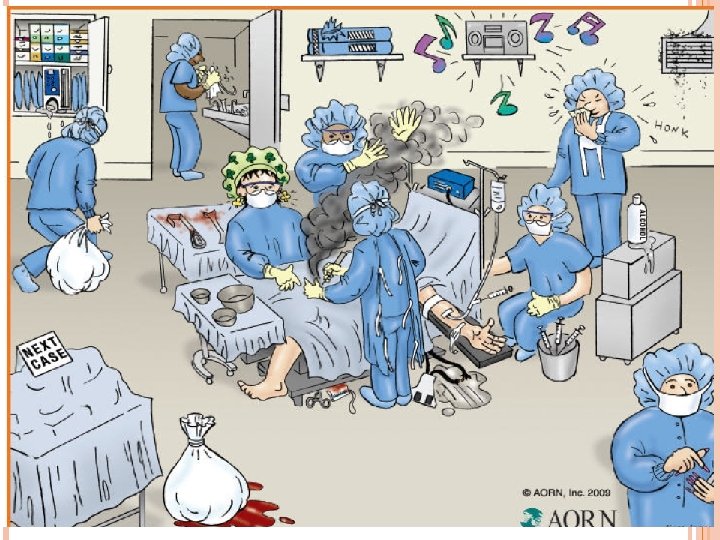
WHAT DO THESE CHARACTERS HAVE IN COMMON?
BLOODBORNE PATHOGENS Microorganisms present in human blood that can cause disease in humans. Examples: � Hepatitis B Virus (HBV) � Human Immunodeficiency Virus (HIV) � Hepatitis C Virus (HBC � DID YOU KNOW These are present for a lifetime once contracted. • All can be contracted with exposure to blood and body fluids. •
PREVENTING BLOODBORNE PATHOGEN TRANSMISSION How to protect yourself � Be Aware Are Sharps containers overfilled? Are you using safety devices? � Be Prepared Use safety devices as they are intended Explain the procedure to the patient to gain there cooperation and avoid potential movement during the procedure. Ask for assistance with patients that might be uncooperative � Dispose of with Care Avoid recap needles Dispose of used needles in sharps containers
NEEDLE STICK FACTS One out of five healthcare workers sustain a needle stick injury every year Safety devices prevent needle sticks Safety devices are the law, employers must provide them
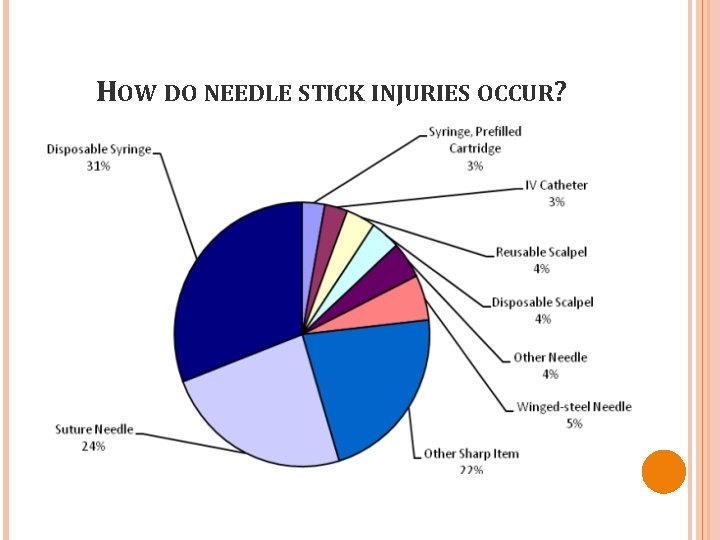
HOW DO NEEDLE STICK INJURIES OCCUR?
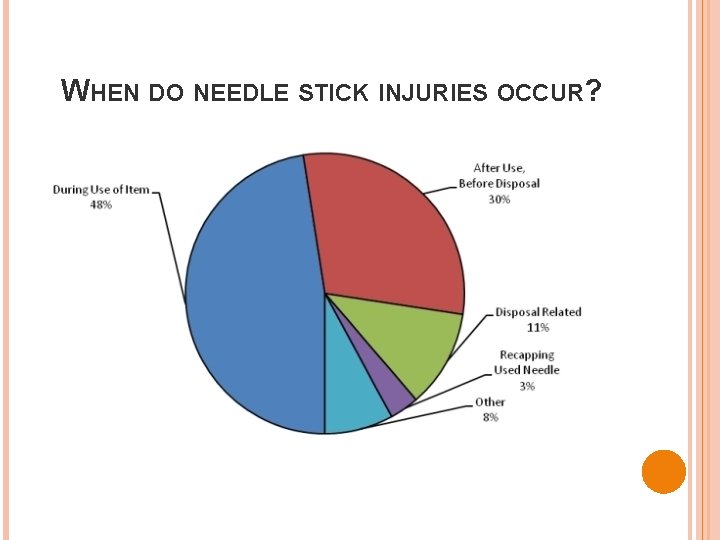
WHEN DO NEEDLE STICK INJURIES OCCUR?
NEEDLE STICK FACTS Serious or fatal infections like HIV, Hepatitis B and C have been acquired from needle sticks HIV Risk of HIV infection from sharps injury is about 0. 3% or 1 in 300 Hep B Risk of Hep B infection from sharps injury is 6 to 30% depending on hep B antigen status of source individual Hep C Risk of Hep C infection from sharps injury is approximately 1. 8%

WHAT TO DO IF YOU HAVE A BLOOD OR BODY FLUID EXPOSURE? Immediately report your injury to your supervisor; do not wait until the end of your shift Do not apply pressure to the wound, allow it to bleed freely Wash the wound with soap and water Identify the patient involved so that they can be evaluated for an infection Go to the ER to seek a medical assessment, take source patient information with you Follow the directions for any necessary blood tests, vaccinations or medications to prevent infection Document the incident in Quantros Follow up with the Infection Control nurse to review source patient and employee laboratory results.
SHARPS WASTE IS HAZARDOUS Injury may result from attempting to insert a sharp in an overfilled container Containers become overfilled when items are discarded inappropriately � (i. e. : dressing, wrapper, tubing, tape, empty sterile H 2 O or saline vials, syringes without a needle, whether used for blood draw or not)
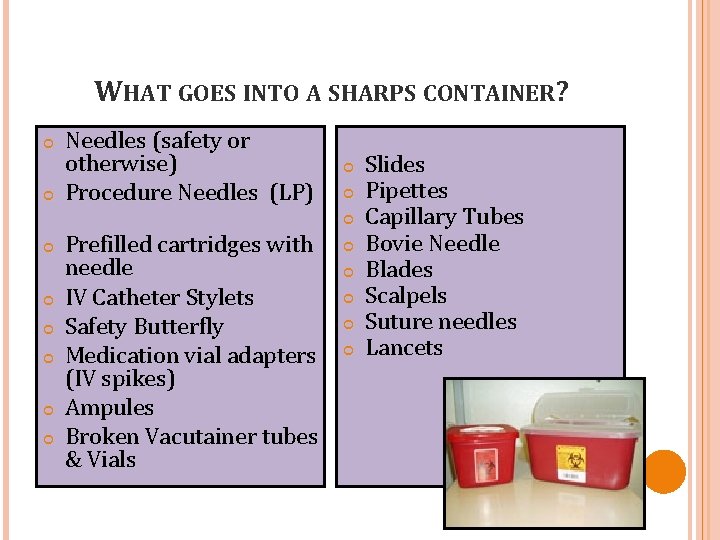
WHAT GOES INTO A SHARPS CONTAINER? Needles (safety or otherwise) Procedure Needles (LP) Prefilled cartridges with needle IV Catheter Stylets Safety Butterfly Medication vial adapters (IV spikes) Ampules Broken Vacutainer tubes & Vials Slides Pipettes Capillary Tubes Bovie Needle Blades Scalpels Suture needles Lancets
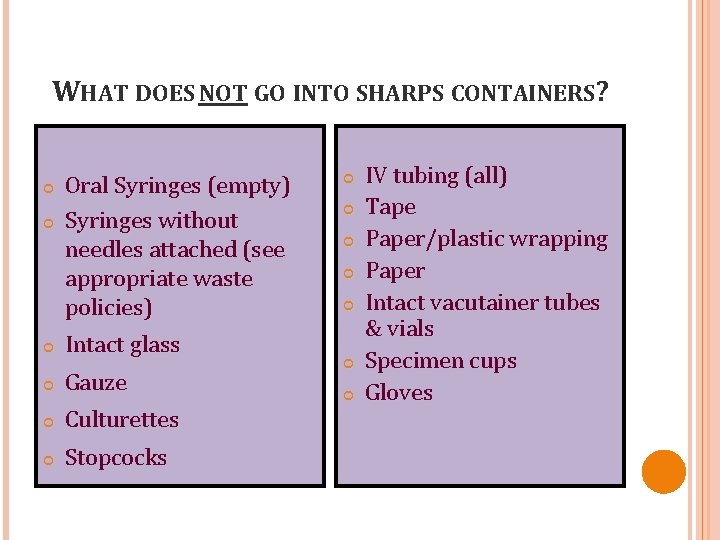
WHAT DOES NOT GO INTO SHARPS CONTAINERS? Oral Syringes (empty) Syringes without needles attached (see appropriate waste policies) Intact glass Gauze Culturettes Stopcocks IV tubing (all) Tape Paper/plastic wrapping Paper Intact vacutainer tubes & vials Specimen cups Gloves
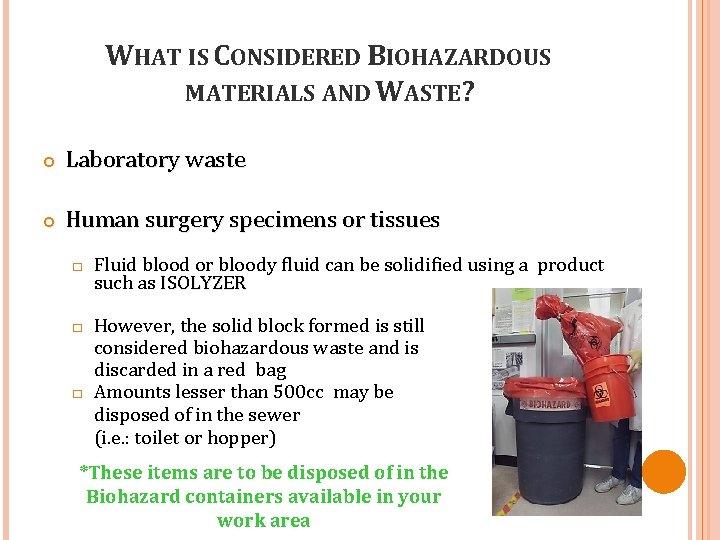
WHAT IS CONSIDERED BIOHAZARDOUS MATERIALS AND WASTE? Laboratory waste Human surgery specimens or tissues � � � Fluid blood or bloody fluid can be solidified using a product such as ISOLYZER However, the solid block formed is still considered biohazardous waste and is discarded in a red bag Amounts lesser than 500 cc may be disposed of in the sewer (i. e. : toilet or hopper) *These items are to be disposed of in the Biohazard containers available in your work area
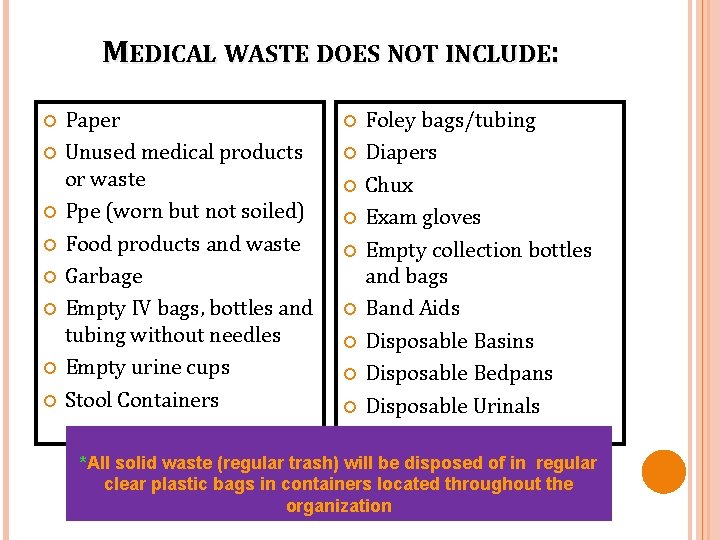
MEDICAL WASTE DOES NOT INCLUDE: Paper Unused medical products or waste Ppe (worn but not soiled) Food products and waste Garbage Empty IV bags, bottles and tubing without needles Empty urine cups Stool Containers Foley bags/tubing Diapers Chux Exam gloves Empty collection bottles and bags Band Aids Disposable Basins Disposable Bedpans Disposable Urinals *All solid waste (regular trash) will be disposed of in regular clear plastic bags in containers located throughout the organization
ADDITIONAL PRECAUTIONS Bag all unused linen Eat and drink only in designated areas Follow appropriate cleaning and disinfecting procedures Use only hospital approved disinfectant Eliminate cardboard in patient care areas
INFECTION PREVENTION AND CONTROL Policies located in Policy Tech Exposure Control Plan located in Policy Tech “Up to Date” clinical resource in the Medical Library for Education to you, patients and families.
MRHC is dedicated to keeping you healthy. Offered to all employees at no cost are: • Hepatitis B Vaccination (series of 3 vaccinations) • Annual TB testing • N-95 Fit mask testing for direct care providers • Annual Influenza Vaccinations
INFECTION PREVENTION AND CONTROL BEGINS WITH YOU Questions?
Thank you!
- Slides: 48