Infection Control for SARS How is SARS spread




- Slides: 17

Infection Control for SARS
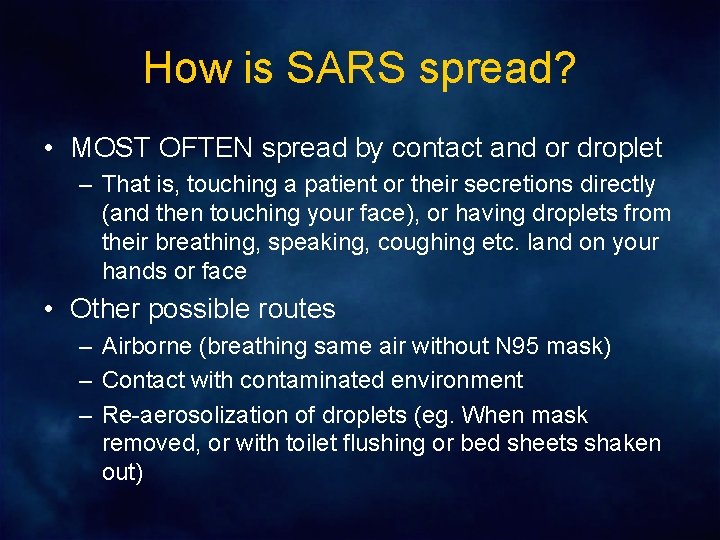
How is SARS spread? • MOST OFTEN spread by contact and or droplet – That is, touching a patient or their secretions directly (and then touching your face), or having droplets from their breathing, speaking, coughing etc. land on your hands or face • Other possible routes – Airborne (breathing same air without N 95 mask) – Contact with contaminated environment – Re-aerosolization of droplets (eg. When mask removed, or with toilet flushing or bed sheets shaken out)
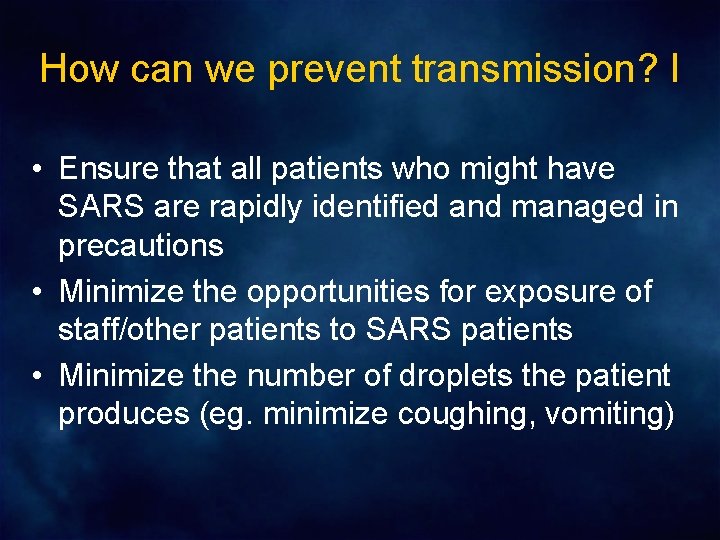
How can we prevent transmission? I • Ensure that all patients who might have SARS are rapidly identified and managed in precautions • Minimize the opportunities for exposure of staff/other patients to SARS patients • Minimize the number of droplets the patient produces (eg. minimize coughing, vomiting)
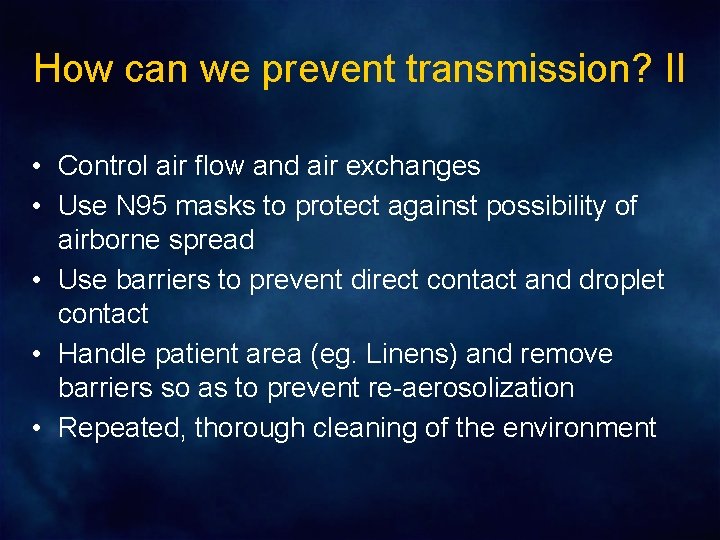
How can we prevent transmission? II • Control air flow and air exchanges • Use N 95 masks to protect against possibility of airborne spread • Use barriers to prevent direct contact and droplet contact • Handle patient area (eg. Linens) and remove barriers so as to prevent re-aerosolization • Repeated, thorough cleaning of the environment
Keys to prevention of SARS transmission: Obsession Paranoia Self-discipline

Identification / Management of Patients • Fever surveillance in patients – All patients with fever assessed for SARS risk, maintained in SARS precautions • Fever/symptom surveillance in staff – Occupational health assessment of staff with fever, myalgias, new cough
Managing Known SARS patients Room Placement / Entry • Airborne isolation rooms or SARS unit (negative pressure, at least 6 air exchanges per hour) • Only essential staff enter room/unit • Minimize time in room • Minimize time within six feet of patient – HCW position to avoid droplets in front of patient’s face • Minimize amount of direct contact with patient • Do not go into patient’s bathroom unless essential for patient care
Managing Known SARS Patients Reducing Droplets • Medical management to reduce cough • Medical management to reduce nausea and prevent vomiting • No nebulizer treatments • Supply oxygen dry; by nasal prongs if possible • Patient to wear surgical mask at all times when HCW are in the room • Handle bed linens to avoid creating aerosols
Managing Known SARS Patients Protective Barriers - 1 • N 95 mask • Face shield (fluid shield mask worn upside down) • Cap/Hair cover • Gown • Double Glove

Managing Known SARS Patients Protective Barriers - 2 • N 95 mask – Ensure mask fits on face – Comfortable enough so that does not need adjustment while garbed • Ensure overlap between gloves and gown cuff • Double glove – Wear first pair for direct contact with patient, then remove – If top pair of gloves contaminated (eg. cleaning vomit), remove and replace
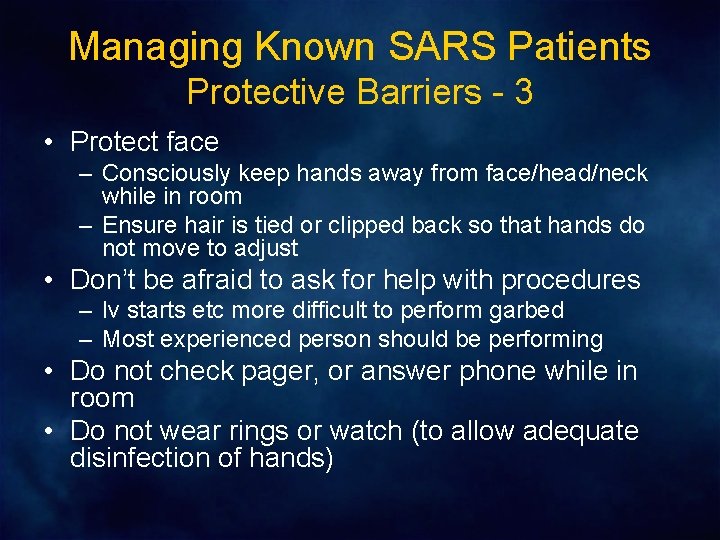
Managing Known SARS Patients Protective Barriers - 3 • Protect face – Consciously keep hands away from face/head/neck while in room – Ensure hair is tied or clipped back so that hands do not move to adjust • Don’t be afraid to ask for help with procedures – Iv starts etc more difficult to perform garbed – Most experienced person should be performing • Do not check pager, or answer phone while in room • Do not wear rings or watch (to allow adequate disinfection of hands)
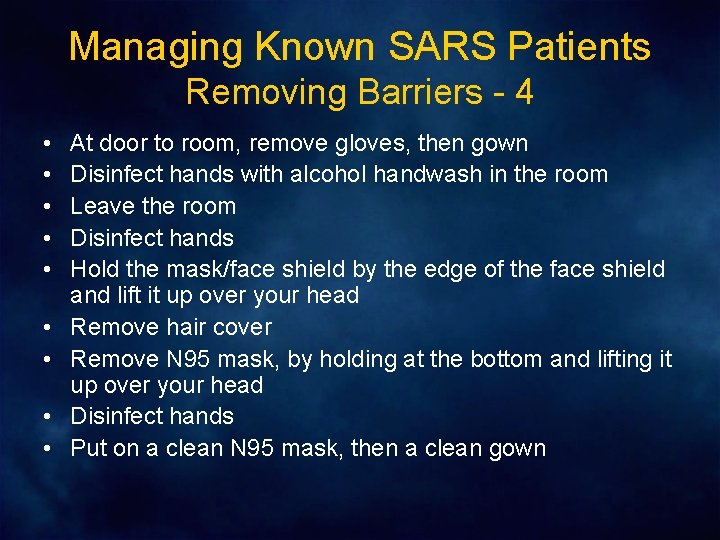
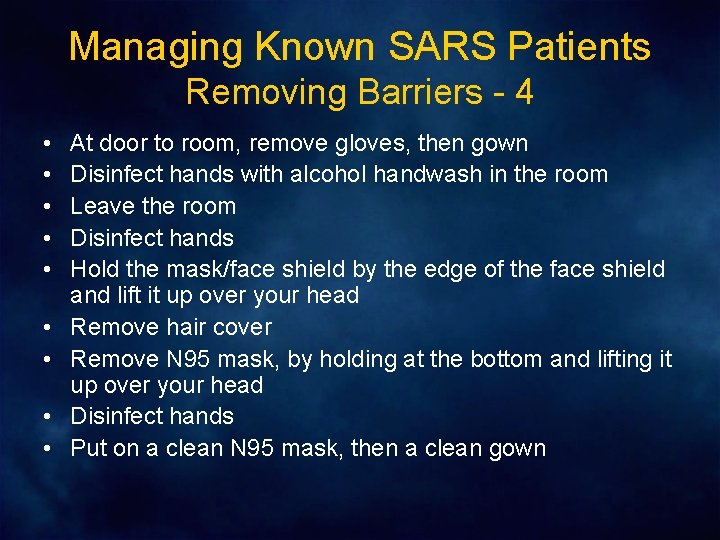
Managing Known SARS Patients Removing Barriers - 4 • • • At door to room, remove gloves, then gown Disinfect hands with alcohol handwash in the room Leave the room Disinfect hands Hold the mask/face shield by the edge of the face shield and lift it up over your head Remove hair cover Remove N 95 mask, by holding at the bottom and lifting it up over your head Disinfect hands Put on a clean N 95 mask, then a clean gown

High risk activities • • Intubation Noninvasive positive pressure ventilation Manual bagging Nebulized medication administration Use of Venturi mask Tracheal and oropharyngeal suction Nasopharyngeal aspiration / throat swab Percussion chest physiotherapy
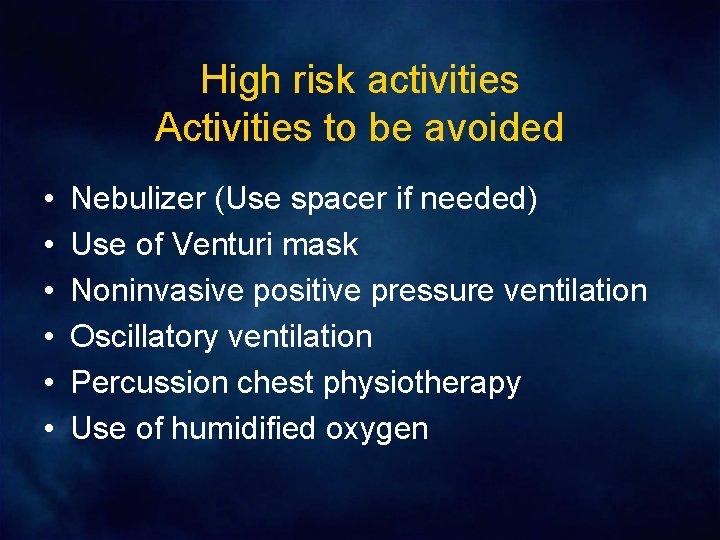
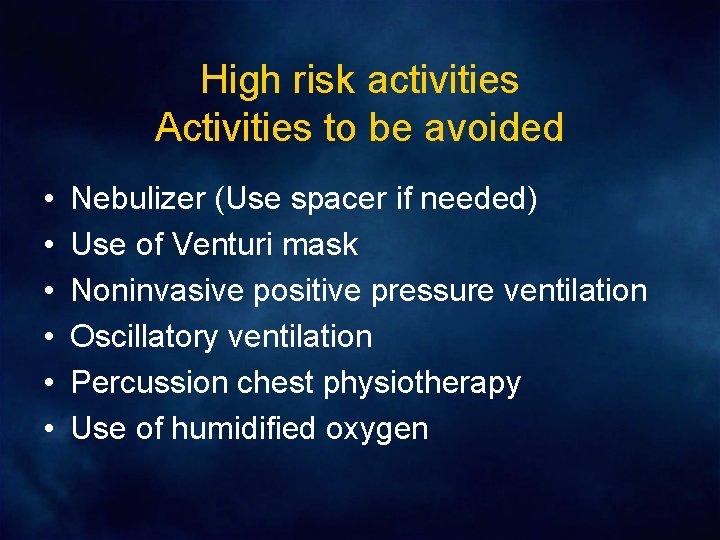
High risk activities Activities to be avoided • • • Nebulizer (Use spacer if needed) Use of Venturi mask Noninvasive positive pressure ventilation Oscillatory ventilation Percussion chest physiotherapy Use of humidified oxygen
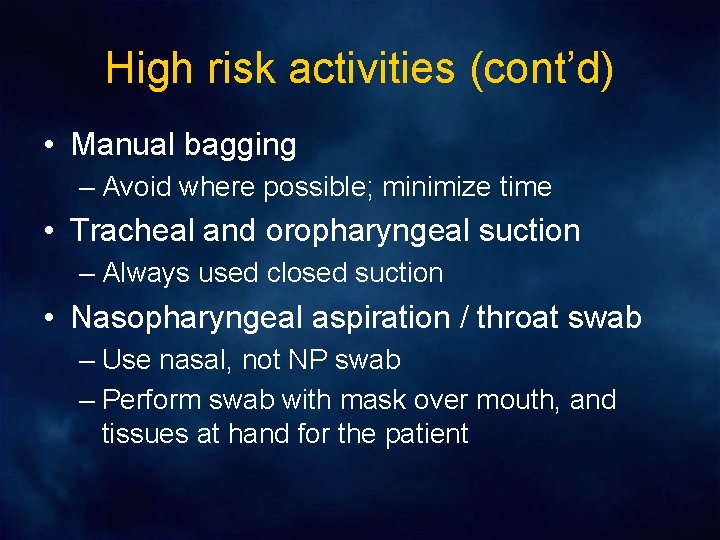
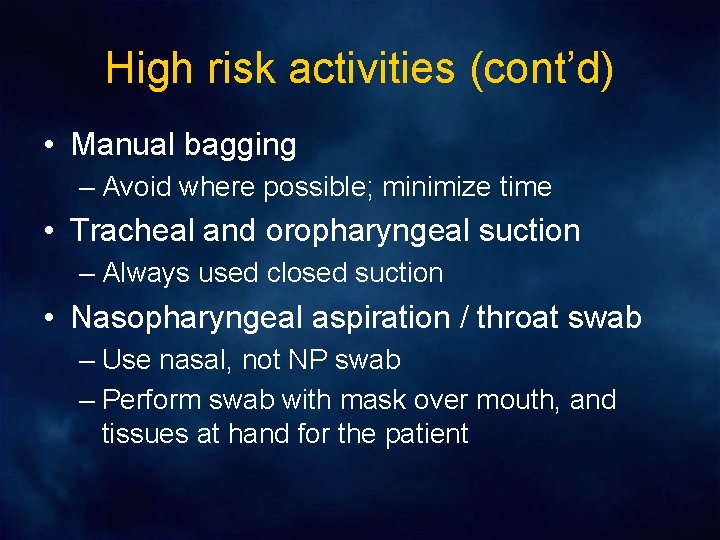
High risk activities (cont’d) • Manual bagging – Avoid where possible; minimize time • Tracheal and oropharyngeal suction – Always used closed suction • Nasopharyngeal aspiration / throat swab – Use nasal, not NP swab – Perform swab with mask over mouth, and tissues at hand for the patient
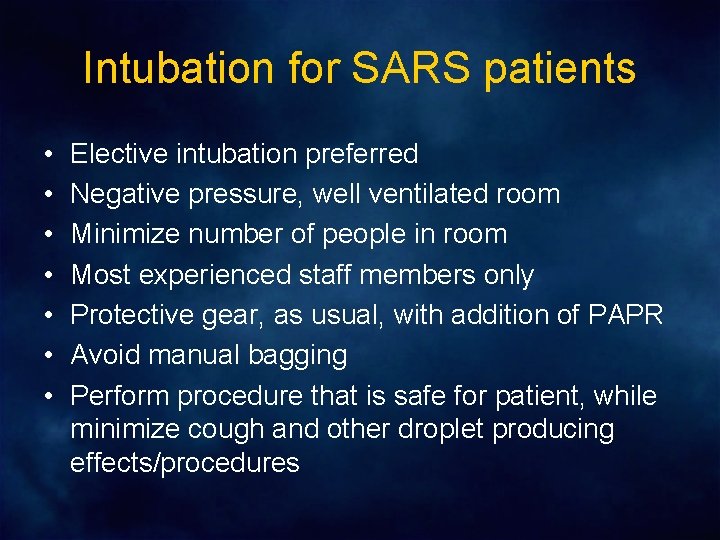
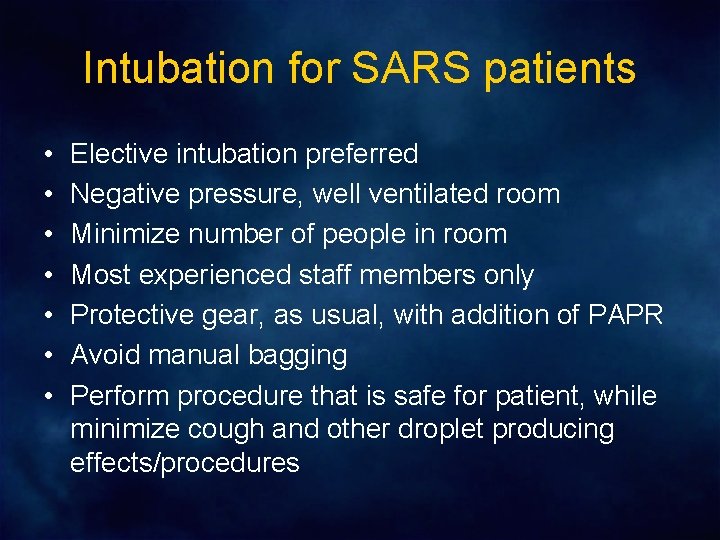
Intubation for SARS patients • • Elective intubation preferred Negative pressure, well ventilated room Minimize number of people in room Most experienced staff members only Protective gear, as usual, with addition of PAPR Avoid manual bagging Perform procedure that is safe for patient, while minimize cough and other droplet producing effects/procedures
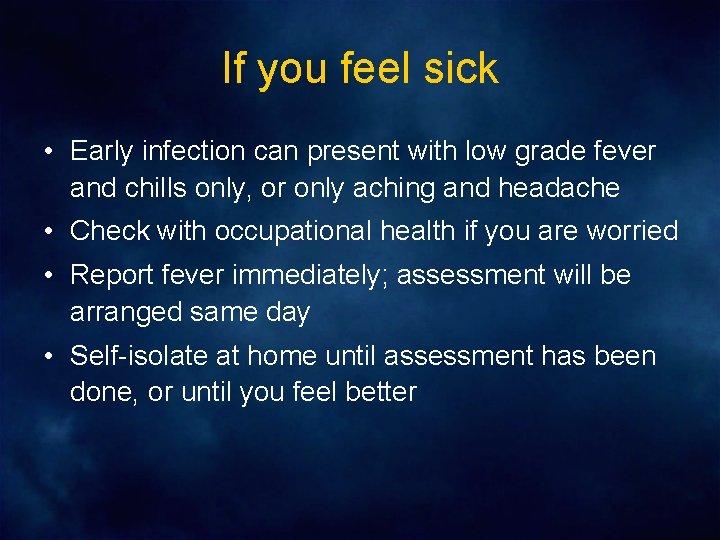
If you feel sick • Early infection can present with low grade fever and chills only, or only aching and headache • Check with occupational health if you are worried • Report fever immediately; assessment will be arranged same day • Self-isolate at home until assessment has been done, or until you feel better