Infant feeding Ayda khader may 2018 The chapter


- Slides: 85

Infant feeding Ayda khader may. 2018
The chapter aim s to: �explain the structure and function of the female breast �describe the properties and components of breast milk �emphasize the role of the midwife in ensuring breastfeeding success for both mother and baby �discuss the role of breast milk expression and human milk banking �describe the different causes of difficulty with breastfeeding �discuss the use of formula feeding and the various products available �outline the requirements and recommendations of the International Code of Marketing of Breast milk Substitutes and the Baby Friendly Hospital Initiative
Introduction �Breastfeeding for the first 6 months of life is the ideal start for babies. �Breastfeeding improves infant and maternal health and cognitive development �it is the single most important preventive approach for saving children's lives �Low breastfeeding rates have led to a progressive increase in the incidence of illness that has a significant cost to the National Health Service
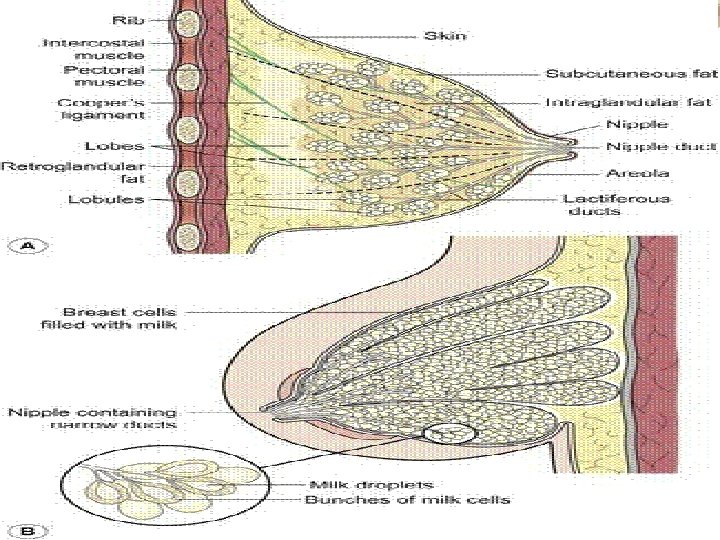
Anatomy and physiology of the breast �The breasts are compound secreting glands, composed of varying proportions of fat, glandular and connective tissue, and arranged in lobes. �Each lobe is divided into lobules consisting of alveoli and ducts.
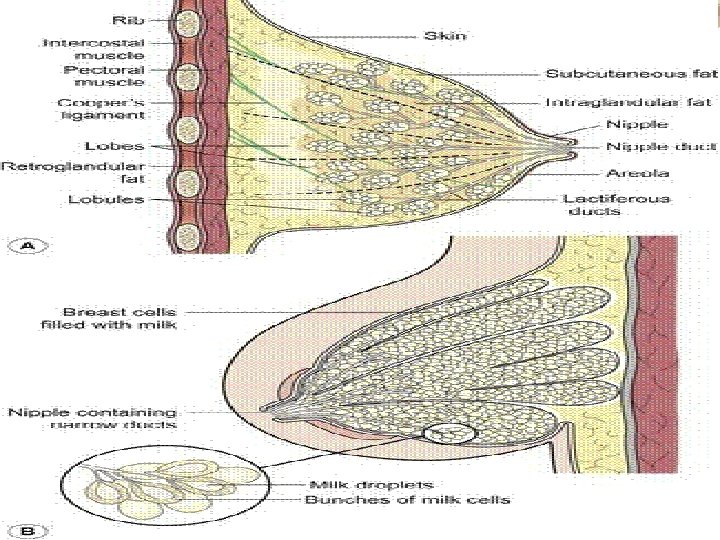
Breast Anatomy § The breast is internally composed of the following parts: 1. Lobes and Lobules �Internally, the mammary gland is composed of 15 -25 lobes that radiates around the nipple. Each lobe consists of about 20 -40 lobules, a smaller milk duct that contains 10 -100 supporting alveoli. 2. Glandular tissues are responsible for milk production and transportation which is composed of: �Alveoli – epithelial grape-like cluster of cells where milk is produced. 6
�Ductules – branch-like tubules extending from the clusters of alveoli and empties to larger ducts called lactiferous ducts. �Lactiferous ducts – widen underneath the areola and nipple to become lactiferous sinuses. �Lactiferous sinuses – collect milk from lactiferous ducts and narrows to an opening in the nipple (nipple pore). 7
3. Connective tissue �Connective tissue supports the breast. Cooper’s ligaments are fibrous bands that attach the breast to the chest wall and keep the breast from sagging. 4. Blood supply � nourishes breast tissue and supplies the nutrients to the breast needed for milk production. � Internal and external mammary arteries & upper intercostals arteries � Venous drainage through corresponding vessels into internal mammary and axillary veins 8
5. Nerves � make the breast sensitive to touch, hence allowing the baby’s suck to stimulate the release of hormones that trigger the let-down or milk ejection reflex (oxytocin) and the production of milk (prolactin). � Largely controlled by hormone activity � The skin is supplied by thoracic nerves � Some sympathetic nerves supply the nipple and areola 9
6. Lymph nodes: � removes waste products � Lymphatic drainage largely into axillary gland � Some into liver and mediastinal gland � The lymphatic vessels of each breast communicate with one another 7. Adipose tissue (fat) – protects the breast from injury. 10
The breast is externally composed of the following parts: 1. Axillary tail � Is breast tissues extending toward the axilla 2. Areola – � circular pigmented area 2. 5 cm in diameter at the center of each breast. � In the areola are small glands called Montgomery's glands which secrete an oily fluid to keep the skin healthy 11
3. Nipple � protruding area at the center of each breast areola at level of 4 th rib � A protuberance of 6 mm in length, composed of pigmented erectile tissues � The surface of nipple is perforated by small orifice of lactiferous ducts � It is covered with epithelium 12
3. Nipple � protruding area at the center of each breast areola at level of 4 th rib � A protuberance of 6 mm in length, composed of pigmented erectile tissues � The surface of nipple is perforated by small orifice of lactiferous ducts � It is covered with epithelium 13
Anatomy and Physiology Breast enlargement �During pregnancy and lactation indicates the mammary glands are becoming functional �Breast size before pregnancy does not determine the amount of milk a woman will produce 14
q Hormones during pregnancy �Estrogen stimulates the ductile systems to grow, then estrogen levels drop after birth �Progesterone increases the size of alveoli and lobes �Prolactin contributes to increasing the breast tissue during pregnancy. 15
q Hormones during breastfeeding �Prolactin levels rise with nipple stimulation �Alveolar cells make milk in response to prolactin when the baby sucks �Oxytocin causes the alveoli to squeeze the newly produced milk into the duct system 16
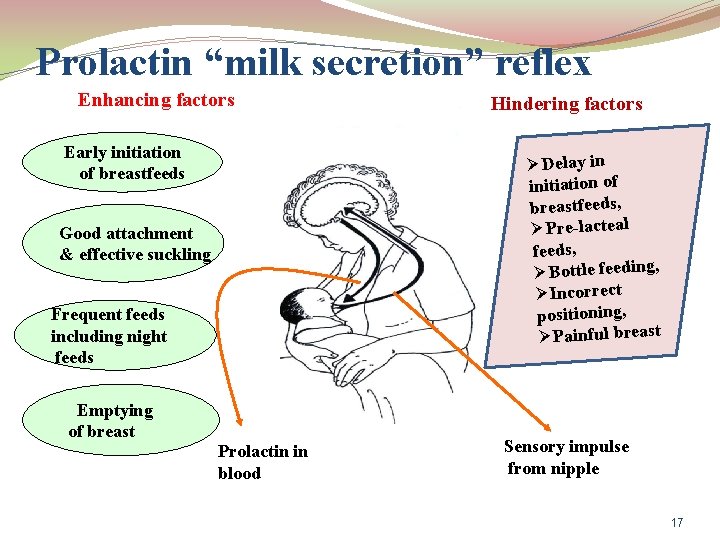
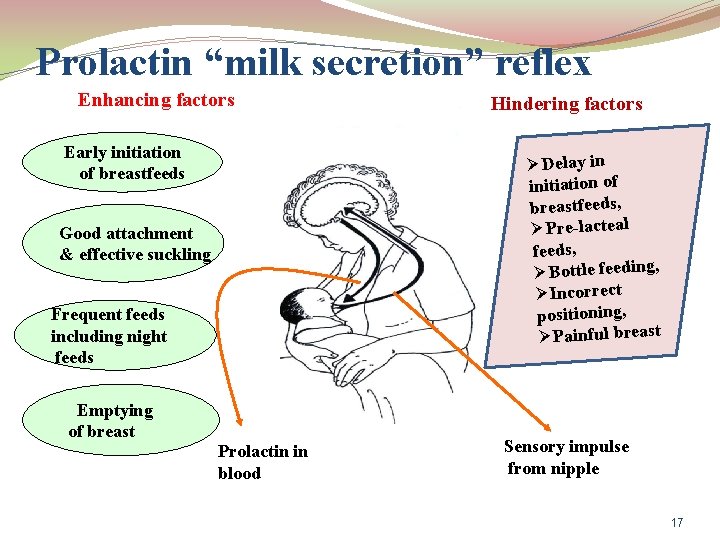
Prolactin “milk secretion” reflex Enhancing factors Early initiation of breastfeeds Hindering factors ØDelay in initiation of breastfeeds, ØPre-lacteal feeds, ØBottle feeding, ØIncorrect positioning, ØPainful breast Good attachment & effective suckling Frequent feeds including night feeds Emptying of breast Prolactin in blood Sensory impulse from nipple 17
Lactation q Lactogenesis I : production start �Initiation of milk production which occurs in second trimester of pregnancy q Lactogenesis II : full production �Postpartum initiation of high volume milk production which occurs as transition from low volume colostrum 18
�Lactogenesis II initiated by falling progesterone levels in the presence of high prolactin levels. Progesterone levels fall 10 fold in first 4 days postpartum. �Breast milk changes in constituents with decreased concentration of secretory Ig. A and lactoferrin. 19
Alveoli secrete milk and contract when stimulated q Oxytocin stimulates milk secretion and is released during the ‘let down’ or milk ejection reflex q After let down, milk travels into the ductules, then to the larger – lactiferous or mammary ducts q 20
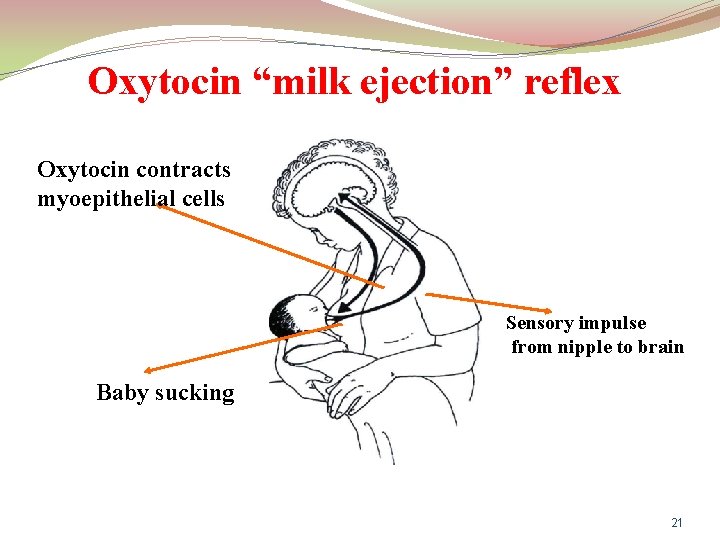
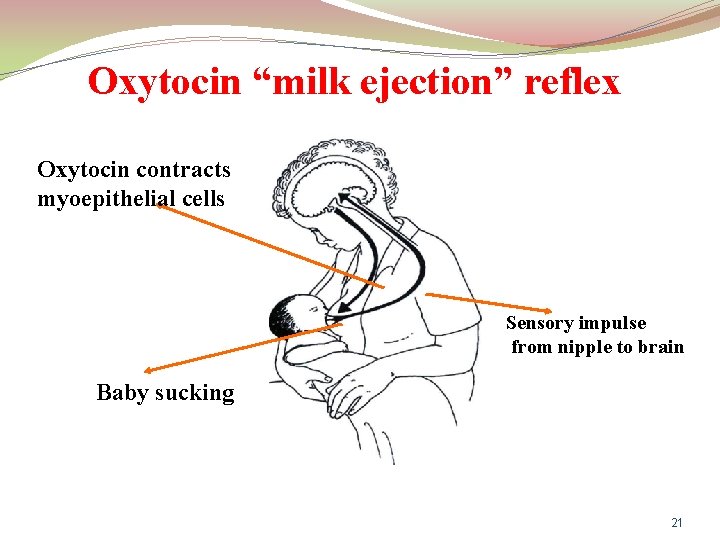
Oxytocin “milk ejection” reflex Oxytocin contracts myoepithelial cells Sensory impulse from nipple to brain Baby sucking 21
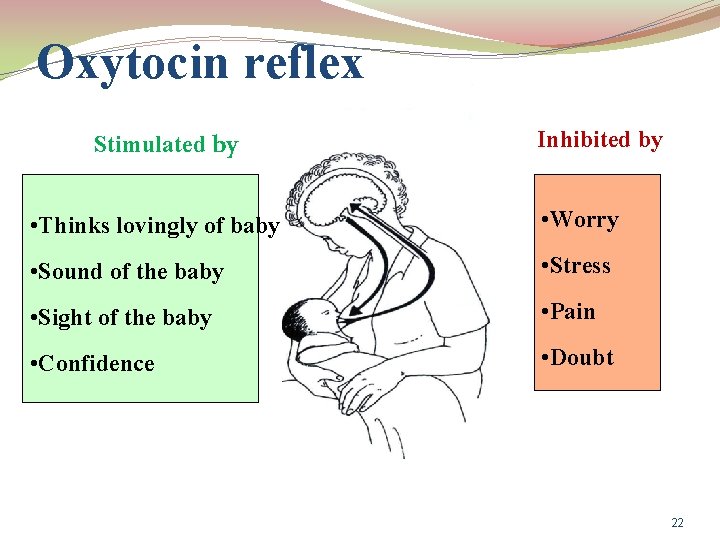
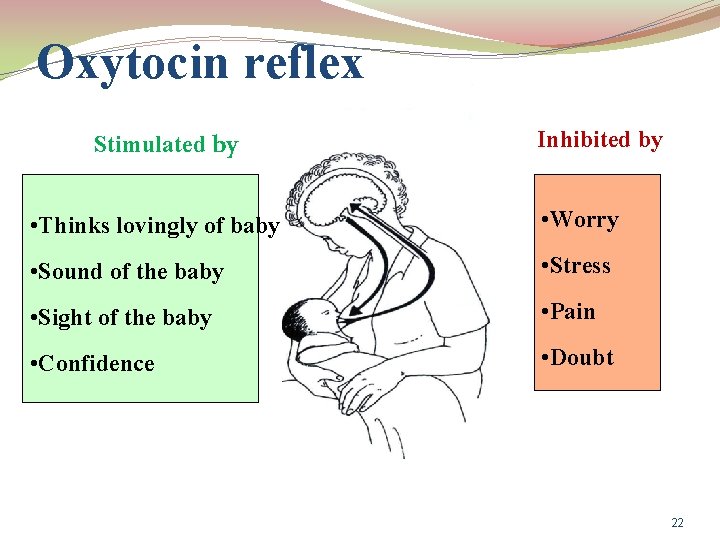
Oxytocin reflex Stimulated by Inhibited by • Thinks lovingly of baby • Worry • Sound of the baby • Stress • Sight of the baby • Pain • Confidence • Doubt 22
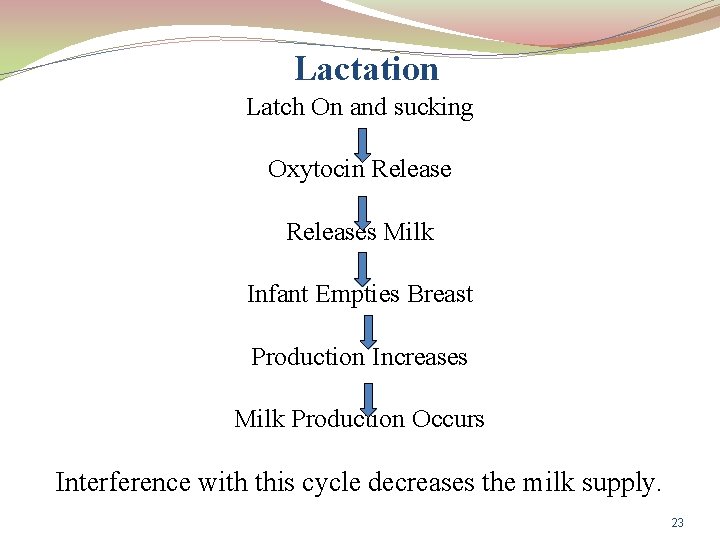
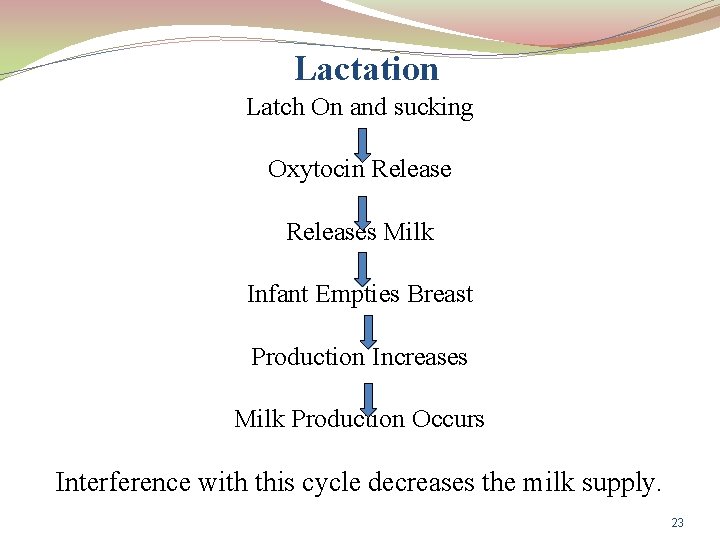
Lactation Latch On and sucking Oxytocin Releases Milk Infant Empties Breast Production Increases Milk Production Occurs Interference with this cycle decreases the milk supply. 23
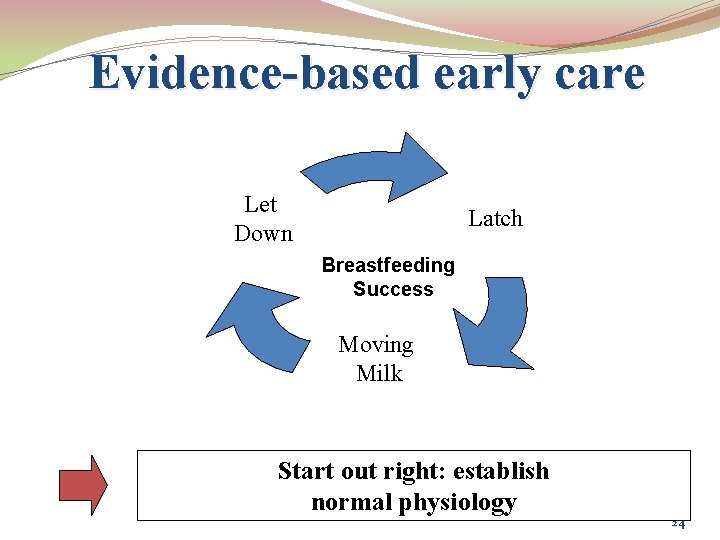
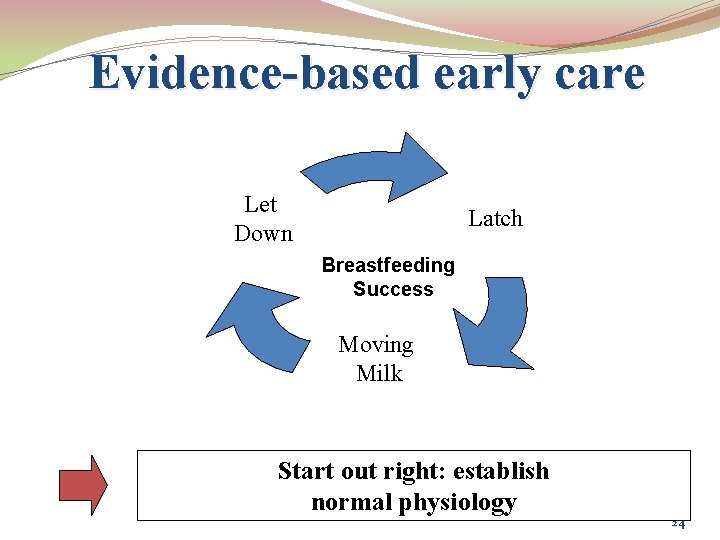
Evidence-based early care Let Down Latch Breastfeeding Success Moving Milk Start out right: establish normal physiology 24
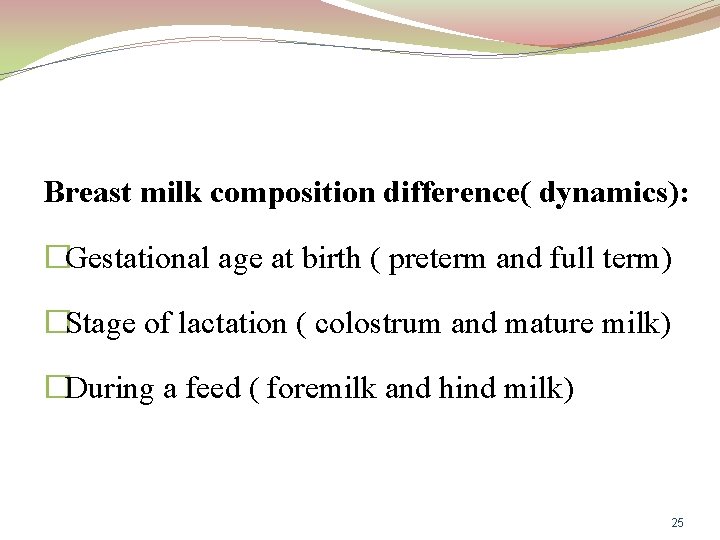
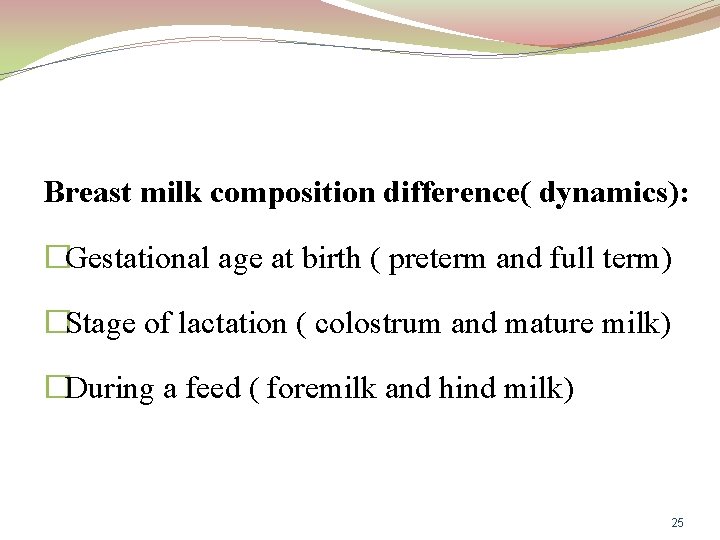
Breast milk composition difference( dynamics): �Gestational age at birth ( preterm and full term) �Stage of lactation ( colostrum and mature milk) �During a feed ( foremilk and hind milk) 25
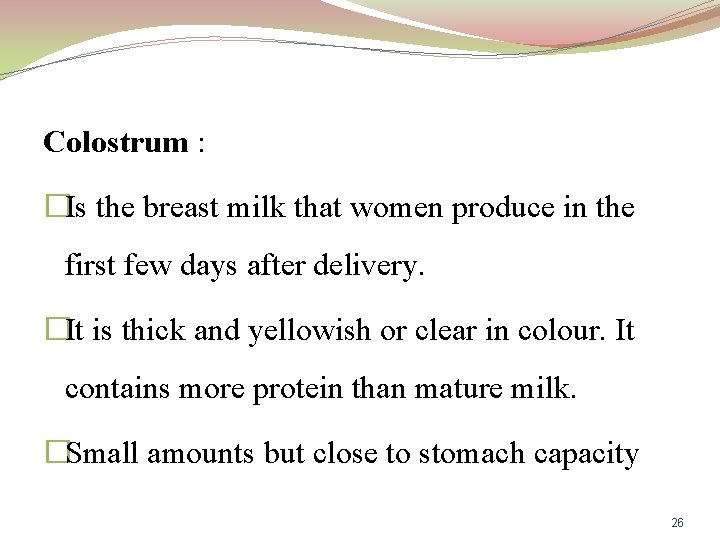
Colostrum : �Is the breast milk that women produce in the first few days after delivery. �It is thick and yellowish or clear in colour. It contains more protein than mature milk. �Small amounts but close to stomach capacity 26
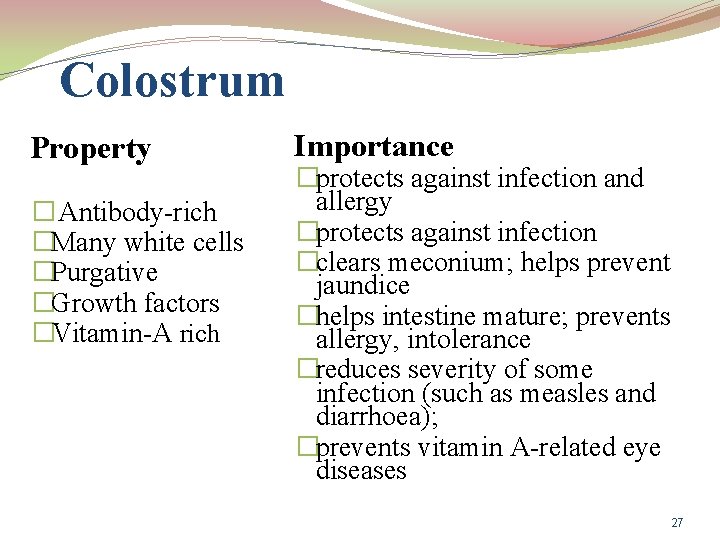
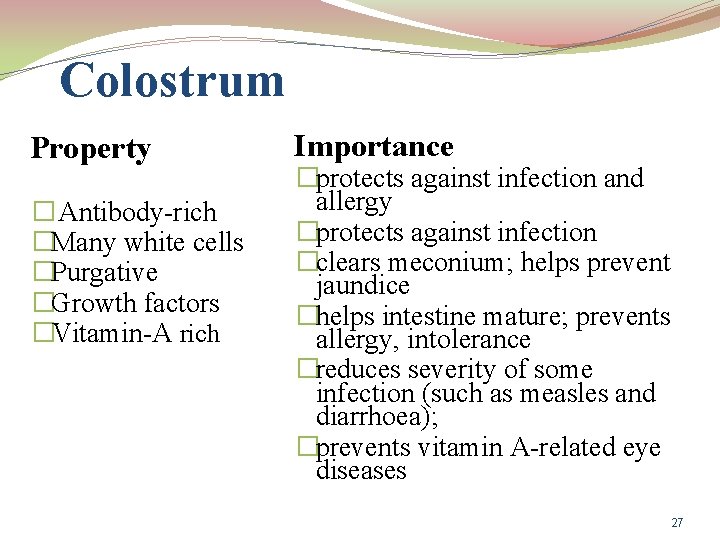
Colostrum Property � Antibody-rich �Many white cells �Purgative �Growth factors �Vitamin-A rich Importance �protects against infection and allergy �protects against infection �clears meconium; helps prevent jaundice �helps intestine mature; prevents allergy, intolerance �reduces severity of some infection (such as measles and diarrhoea); �prevents vitamin A-related eye diseases 27
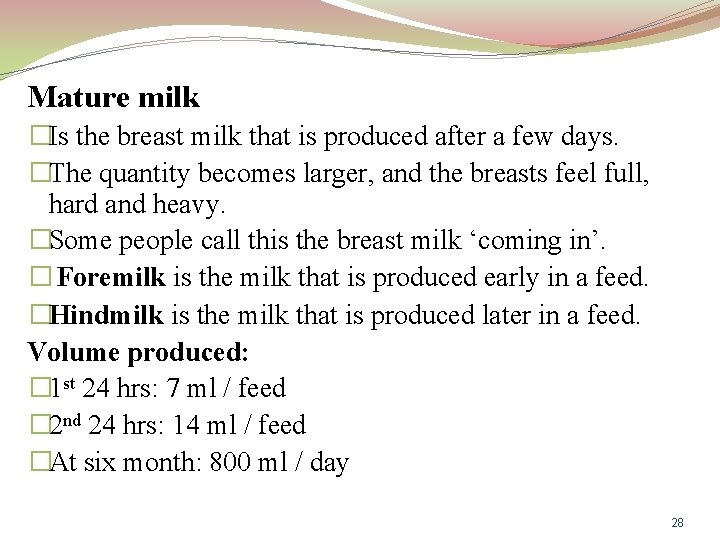
Mature milk �Is the breast milk that is produced after a few days. �The quantity becomes larger, and the breasts feel full, hard and heavy. �Some people call this the breast milk ‘coming in’. � Foremilk is the milk that is produced early in a feed. �Hindmilk is the milk that is produced later in a feed. Volume produced: � 1 st 24 hrs: 7 ml / feed � 2 nd 24 hrs: 14 ml / feed �At six month: 800 ml / day 28
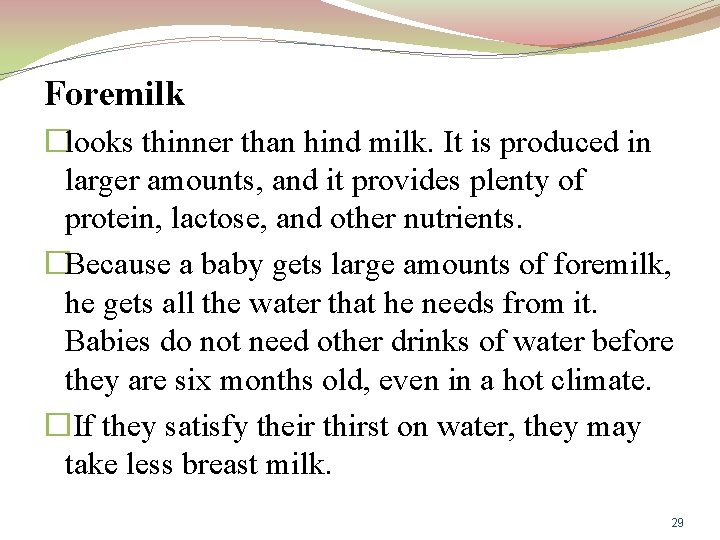
Foremilk �looks thinner than hind milk. It is produced in larger amounts, and it provides plenty of protein, lactose, and other nutrients. �Because a baby gets large amounts of foremilk, he gets all the water that he needs from it. Babies do not need other drinks of water before they are six months old, even in a hot climate. �If they satisfy their thirst on water, they may take less breast milk. 29
Hind milk �Is the milk that is produced later in a feed. �Hind milk looks whiter than foremilk, because it contains more fat. This fat provides much of the energy of a breastfeed. �This is an important reason not to take a baby off a breast too quickly. The baby should be allowed to continue until he has had all that he wants. 30
Breast milk composition Mature milk in 10 days �All necessary nutrient and fluid in 6 month � 88% water � 4. 5% fat �Makes up 1/2 of calories in breast milk �Supplied the energy or rapid growth, more produced at night �Cholesterol is optimal for brain development 31
Breast milk composition cont. . �Secretory IGA => Most important immunoglobulin, breast milk is only source for first 6 weeks � 100 amino acid , mineral and vitamins �Iron supplement at 4 – 6 months �Consider vitamin D 32
Properties of breast milk �Biologic specificity => Longchain omega-3 Fatty Acids � Important for brain and retinal development � Higher IQs 33
Immunologic specificity �Protection against pathogens & allergens �Kills pathogenic organisms or modifies their growth. �Stimulates epithelial maturation for future defence. �First immunization �Protection against common respiratory and intestinal diseases. 34
Immunologic specificity cont. . �Colostrum = Baby’s first vaccination �Less risk of illness such as: Ear infections, pneumonia, crohn’s disease and other bowel illnesses, stomach flu and other intestinal illnesses, ear infections, childhood cancers, diabetes, arthritis, allergies, asthma and eczema. 35
Breastfeeding Best for baby Reduces incidence of allergies Economical - no waste. Antibodies - greater immunity to infections Stool inoffensive - never constipated. Temperature always correct and constant. 36
Breastfeeding Fresh milk - never goes sour in the breast Emotionally bonding Easy once established Digested easily within two to three hours Immediately available Nutritionally balanced Gastroenteritis greatly reduced 37
Exclusive breastfeeding: �The feeding of an infant or young child with breast milk directly from female human breasts rather than from a baby bottle or other container "an infant's consumption of human milk with no supplementation of any type (no water, no juice, no nonhuman milk, and no foods) except for vitamins, minerals, and medications. " 38
Predominant breastfeeding Means breastfeeding the baby but also giving the baby small amount of water or water based drink such as tea Full breastfeeding Means breast feeding either exclusively or predominantly 39
Bottle feeding Means feeding the baby from the bottle, whatever in the bottle including expressed milk Artificial feeding Means feeding a baby on artificial feed, not breastfeeding at all. 40
Human milk varies in its composition: �with the time of day (e. g. fat content is lowest in the morning and highest in the afternoon) �with the stage of lactation (e. g. the fat and protein content of colostrum is higher than in mature milk) �in response to maternal nutrition (e. g. although the total amount of fat is not influenced by diet, the type of fat that appears in the milk will be influenced by what the mother eats) �because of individual variations.
Antenatal preparation �Breasts and nipples are altered by pregnancy �Increased sebum secretion obviates the need for cream to lubricate the nipple. �Women who have inverted and non- protractile (flat) nipples often find that they improve spontaneously during pregnancy �Neither the wearing of Woolwich shells nor Hoffmann's exercises are of any value and should not be recommended
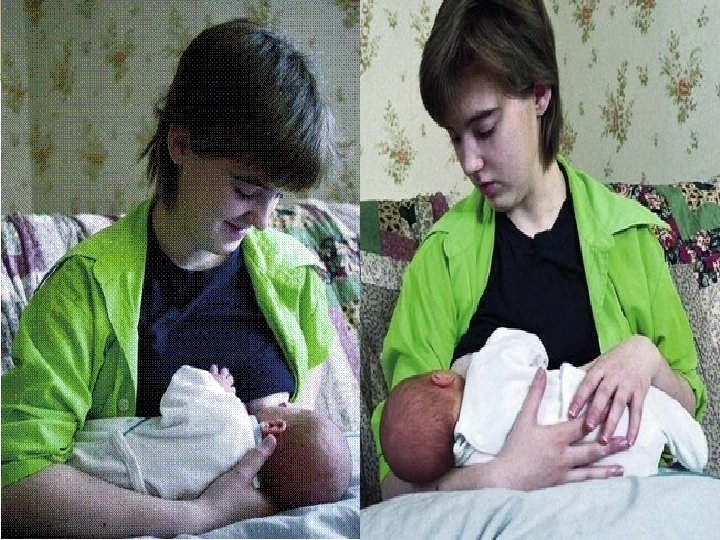
Effective positioning for the mother �A comfortable position is a prerequisite of comfortable breastfeeding. A woman who has recently given birth, especially one new to breastfeeding, may need some help with this.
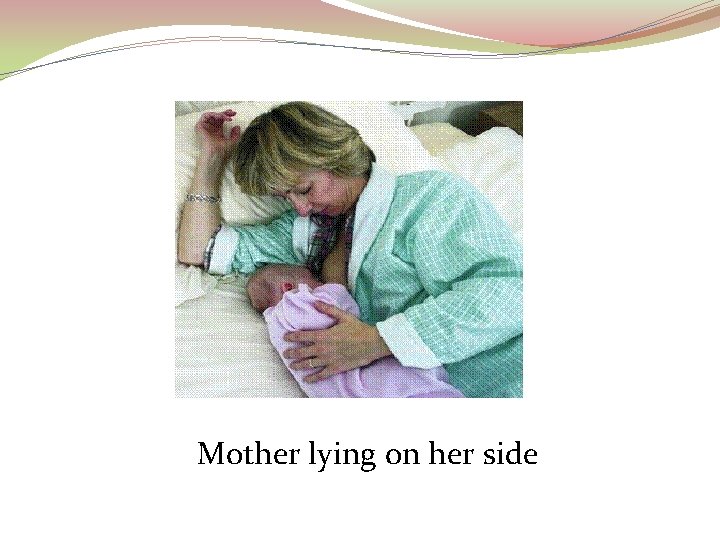
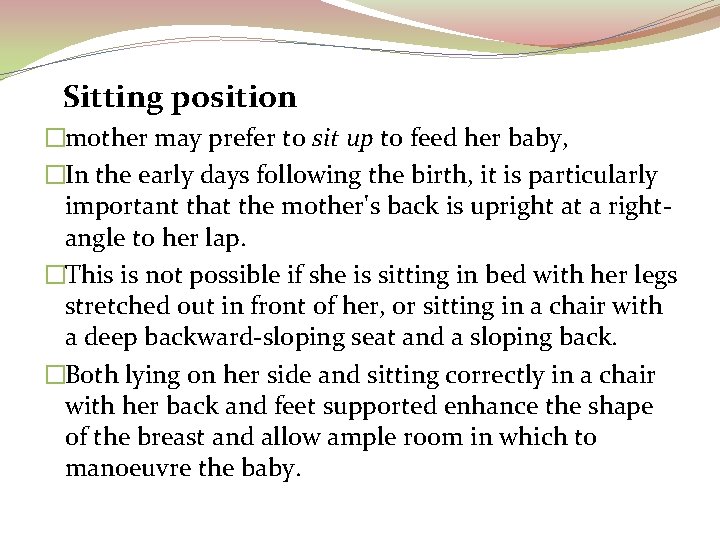
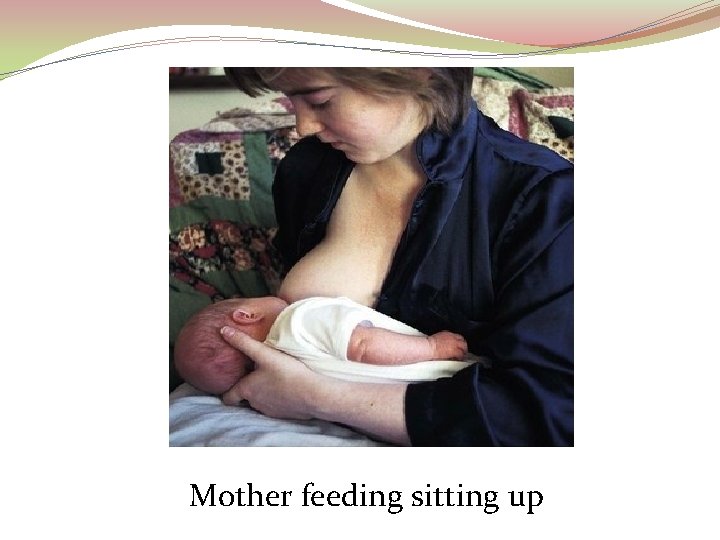
lying on her side �After a caesarean section, or where the perineum is very painful, lying on her side may be the only position a woman can tolerate in the first few days aftr birth, �It is likely that she will need assistance in placing the baby at the breast in this position, because she has only one free hand. �When feeding from the lower breast it may be helpful to raise her body slightly by tucking the end of a pillow under her ribs. � Once the woman can do this unaided, she may find this a comfortable and convenient position for night feeds, enabling her to get more sleep
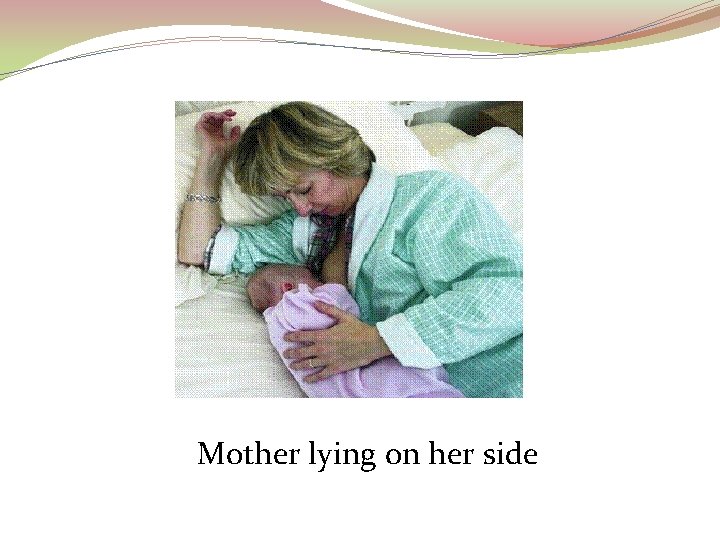
Mother lying on her side
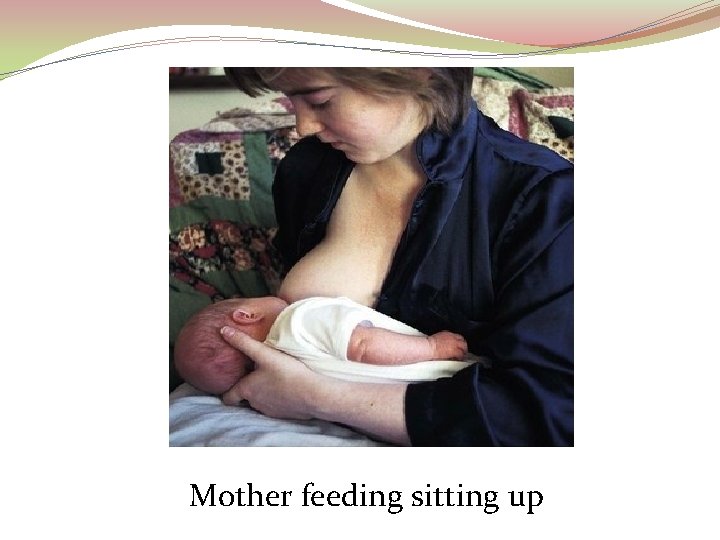
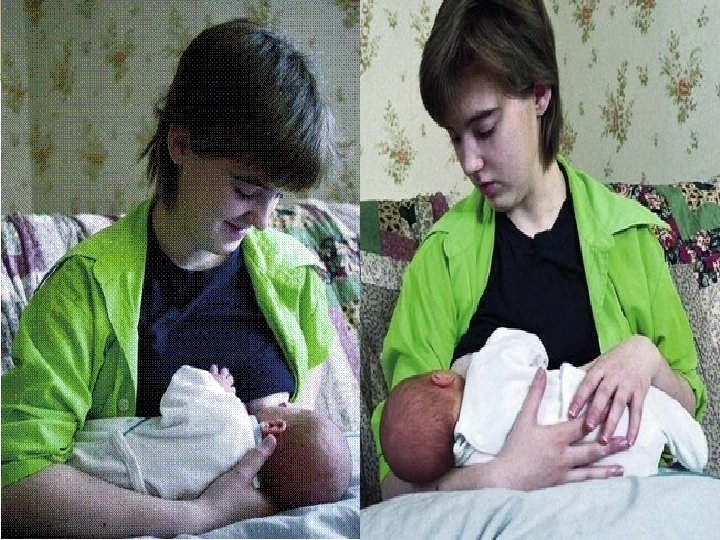
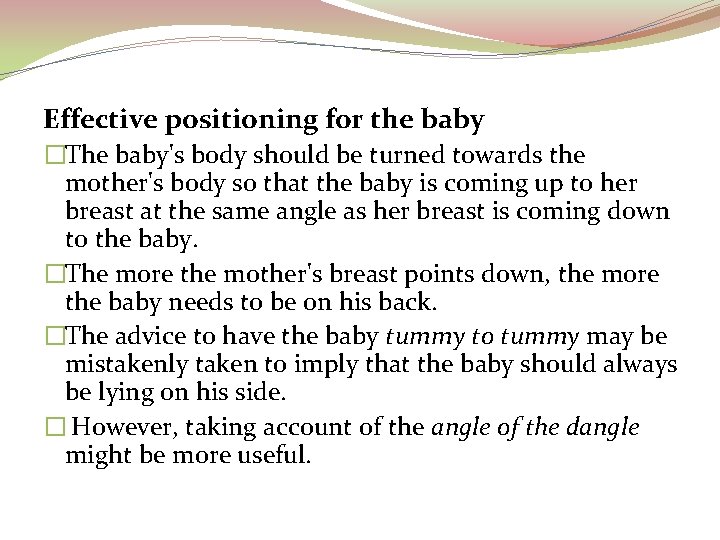
Sitting position �mother may prefer to sit up to feed her baby, �In the early days following the birth, it is particularly important that the mother's back is upright at a rightangle to her lap. �This is not possible if she is sitting in bed with her legs stretched out in front of her, or sitting in a chair with a deep backward-sloping seat and a sloping back. �Both lying on her side and sitting correctly in a chair with her back and feet supported enhance the shape of the breast and allow ample room in which to manoeuvre the baby.
Mother feeding sitting up
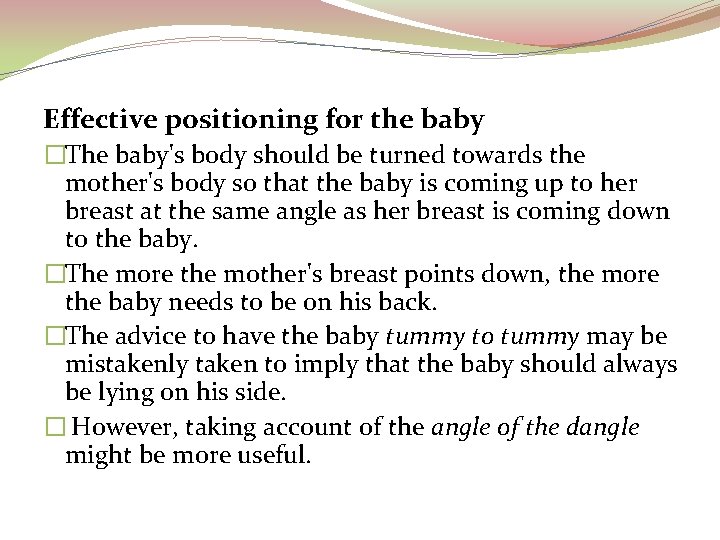
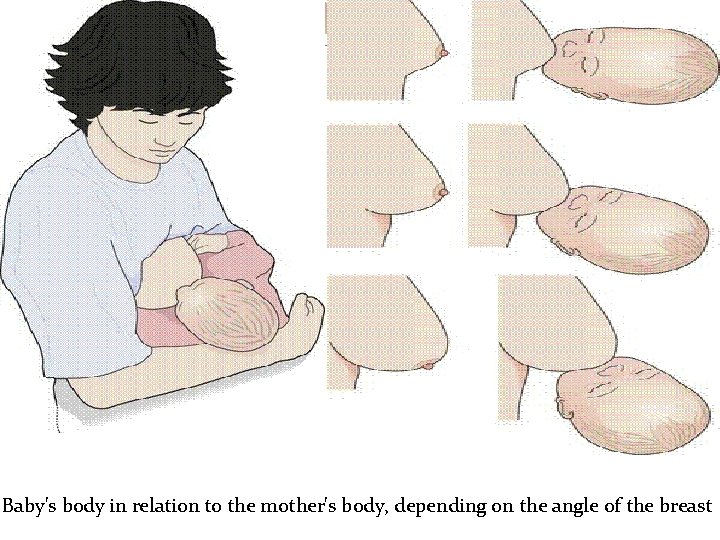
Effective positioning for the baby �The baby's body should be turned towards the mother's body so that the baby is coming up to her breast at the same angle as her breast is coming down to the baby. �The more the mother's breast points down, the more the baby needs to be on his back. �The advice to have the baby tummy to tummy may be mistakenly taken to imply that the baby should always be lying on his side. � However, taking account of the angle of the dangle might be more useful.
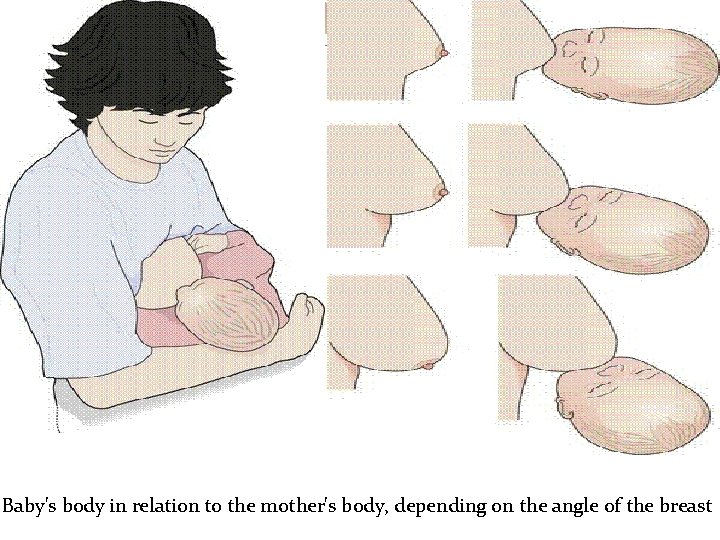
Baby's body in relation to the mother's body, depending on the angle of the breast
Attaching the baby to the breast �The baby should be supported across the shoulders, so that slight extension of the neck can be maintained. �The baby's head may be supported by the extended fingers of the mother's supporting hand or on the mother's forearm �It may be helpful to wrap the baby in a small sheet (Vancouver wrap), so that his hands are by his side. �
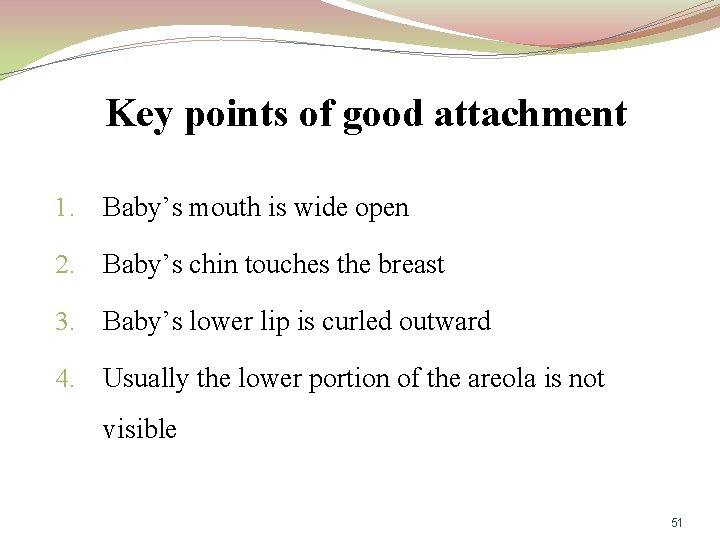
Key points of good attachment 1. Baby’s mouth is wide open 2. Baby’s chin touches the breast 3. Baby’s lower lip is curled outward 4. Usually the lower portion of the areola is not visible 51
�Healthy term babies are equipped with a number of primitive reflexes that enable them to obtain the nourishment they require. �At birth, all reflexes are of brainstem origin, with minimal cortical control. �As the baby matures, higher, cortical pathways develop and the reflexes disappear sequentially: rooting at about 4 months of age and tongue protrusion by about 6 months of age
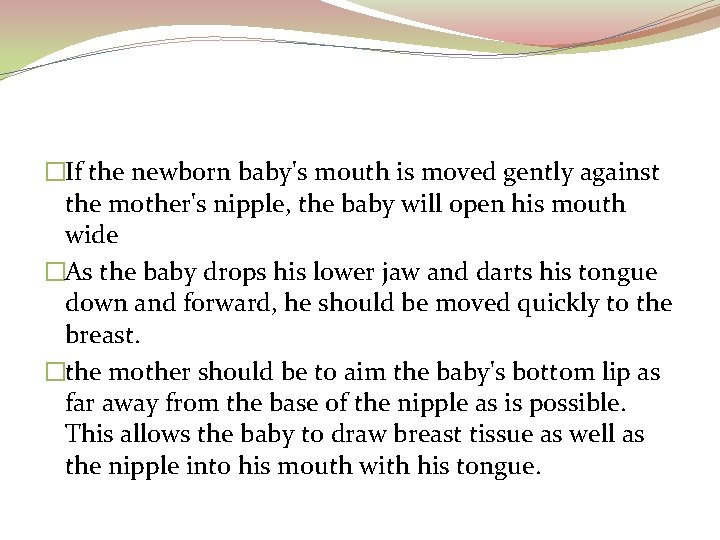
�If the newborn baby's mouth is moved gently against the mother's nipple, the baby will open his mouth wide �As the baby drops his lower jaw and darts his tongue down and forward, he should be moved quickly to the breast. �the mother should be to aim the baby's bottom lip as far away from the base of the nipple as is possible. This allows the baby to draw breast tissue as well as the nipple into his mouth with his tongue.
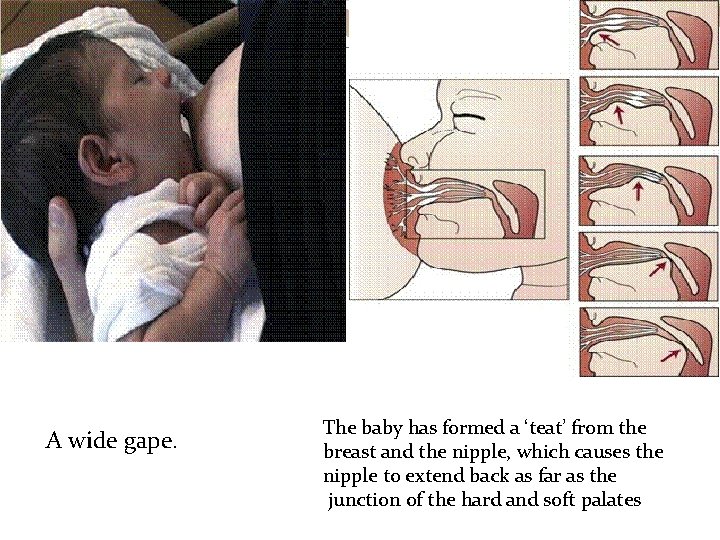
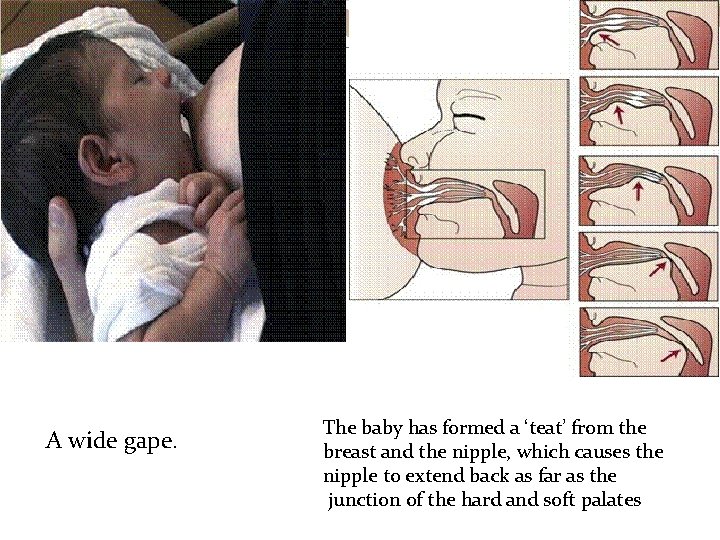
A wide gape. The baby has formed a ‘teat’ from the breast and the nipple, which causes the nipple to extend back as far as the junction of the hard and soft palates
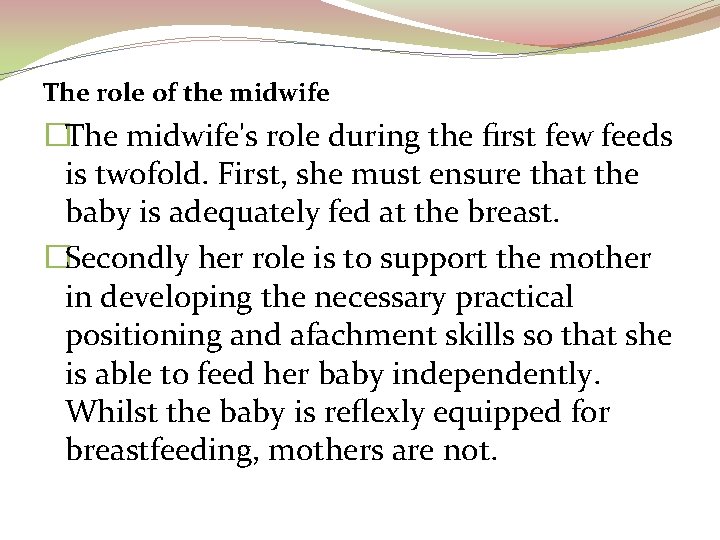
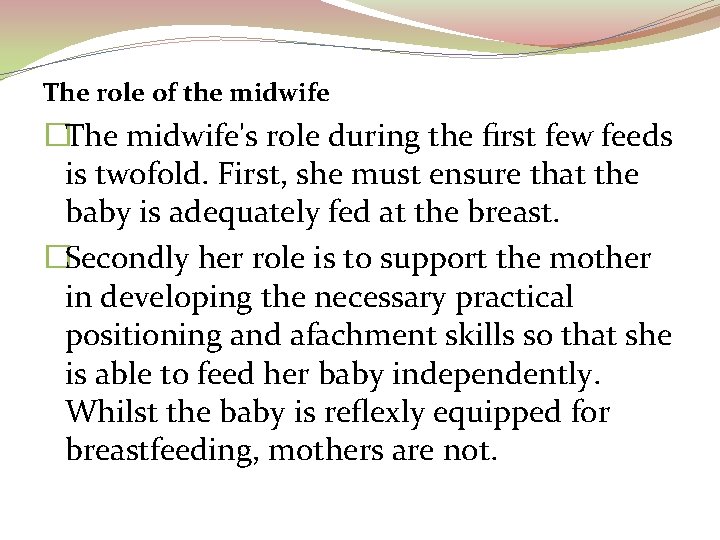
The role of the midwife �The midwife's role during the first few feeds is twofold. First, she must ensure that the baby is adequately fed at the breast. �Secondly her role is to support the mother in developing the necessary practical positioning and afachment skills so that she is able to feed her baby independently. Whilst the baby is reflexly equipped for breastfeeding, mothers are not.
Some mothers will need more help and support than others. Reasons for this include: ü Previous unsuccessful breastfeeding. ü Breastfeeding may have gone well last time by chance rather than knowledge. ü The new baby may behave very differently, or have different needs, from the mother's previous baby/babies. ü The mother may have recently fed (or still be feeding) a toddler and has forgotten quite how much help a new baby requires to breastfeed. ü Their previous baby may have been born at a time when underpinning information now known to be outdated was thought to be correct.
reasons for babies withdrawing from the breast are: �incorrect attachment �the milk flow is very fast and the baby needs to let go and pause �the baby has swallowed air with the generous flow of milk that occurs at the beginning of a feed and requires an opportunity to expel wind.
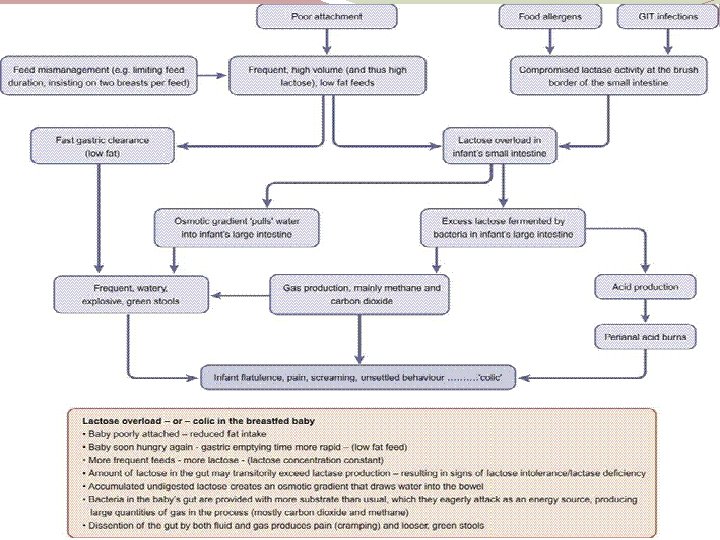
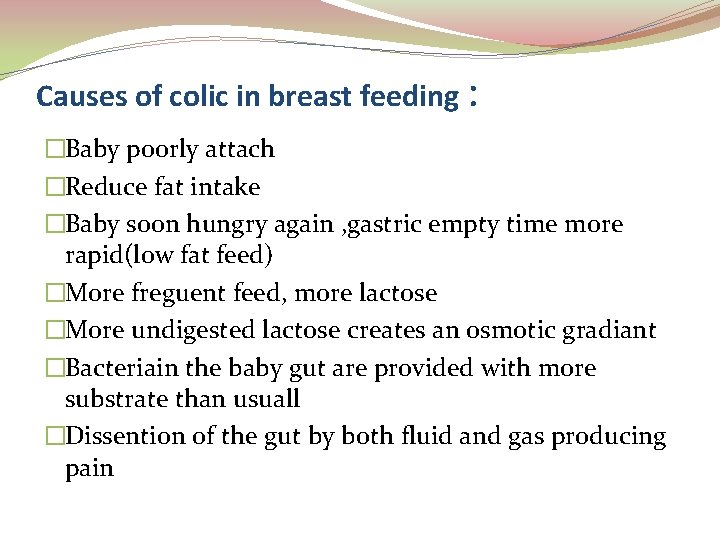
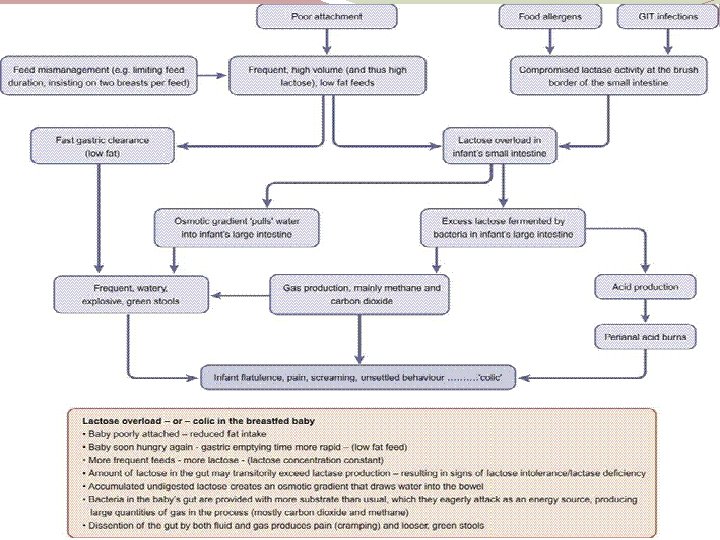
Causes of colic in breast feeding : �Baby poorly attach �Reduce fat intake �Baby soon hungry again , gastric empty time more rapid(low fat feed) �More freguent feed, more lactose �More undigested lactose creates an osmotic gradiant �Bacteriain the baby gut are provided with more substrate than usuall �Dissention of the gut by both fluid and gas producing pain
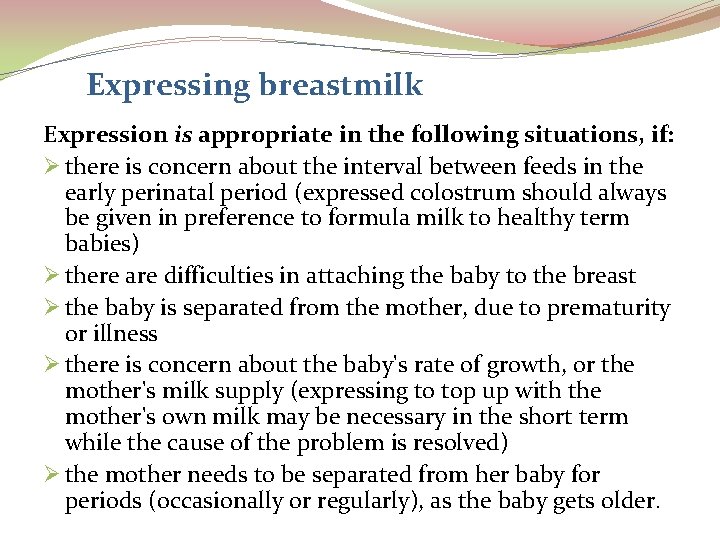
Expressing breastmilk Expression is appropriate in the following situations, if: Ø there is concern about the interval between feeds in the early perinatal period (expressed colostrum should always be given in preference to formula milk to healthy term babies) Ø there are difficulties in attaching the baby to the breast Ø the baby is separated from the mother, due to prematurity or illness Ø there is concern about the baby's rate of growth, or the mother's milk supply (expressing to top up with the mother's own milk may be necessary in the short term while the cause of the problem is resolved) Ø the mother needs to be separated from her baby for periods (occasionally or regularly), as the baby gets older.
Manual expression of milk �Manual expression has several advantages over mechanical pumping and should be taught to all mothers. It is usually the most efficient method of obtaining colostrum. Some mothers will find hand expressing superior to any breast pump. Expressing with a breast pump �If it is possible and practical, the mother should be able to experiment with a variety of breast pumps to discover what will suit her best as not all pumps work well for every woman.
Manually operated pumps �Most manually operated pumps are not efficient enough to allow initiation of full lactation but they can be useful when expressing is required once lactation is established. It is helpful for midwives to explain to mothers that these pumps function most efficiently if the vacuum phase is considerably longer than the release phase. Electrically controlled pumps �Some electrically controlled pumps provide a regular vacuum and release cycle, with variability in the strength of the suction and others also vary the frequency of the cycle. Double pumping is possible with most models, and this has repeatedly been shown to be
Storage of breastmilk advises that expressed milk can be stored for up to: � 5 days in the main part of a fridge, at 4 °C or lower � 2 weeks in the freezer compartment of a refrigerator � 6 months in a domestic freezer, at − 18 °C or lower.
Care of the breasts �Daily washing is all that is necessary for breast hygiene. � Brassieres may be worn in order to provide comfortable support � are useful if the breasts leak and breast pads (or breast shells) are used.
Breast problems Sore and damaged nipples ü The cause is almost always trauma from the baby's mouth and tongue, which results from incorrect attachment of the baby to the breast. ü Correcting this will provide immediate relief from pain and allow rapid healing to take place. ü Epithelial growth factor, contained in fresh human milk and saliva, may aid this process.
�Resting the nipple enables healing to take place but makes the continuation of lactation much more complicated because it is necessary to express the milk and to use some other means of feeding it to the baby. �Nipple shields should be used with caution, and never before the mother has begun to lactate �They make feeding less painful, but often they do not. Their use does not enable the mother to learn how to feed her baby correctly, and their longer-term use may result in reduced milk transfer from mother to baby. �This in turn may result in mastitis in the mother (reduced milk removal), slow weight gain or prolonged feeds in the baby (reduced milk transfer), or both. �If mothers choose to use them, they should be advised to seek help with learning to attach the baby comfortably without a nipple shield as soon as practicable
Other causes of soreness �Infection with Candida albicans (thrush) can occur, although it is not common during the first week after birth. � Sudden development of pain after a period of trouble-free feeding is suggestive of thrush. �The nipple and areola are inflamed and shiny, and pain typically persists throughout the feed. � The baby may show signs of oral or anal thrush. � Both mother and baby should receive concurrent fungicidal treatment, such as miconazole, and it may take several days for the pain in the nipple to disappear
Dermatitis �Sensitivity may develop to topical applications such as creams, ointments or sprays, including those used to treat thrush.
Anatomical variations �Short nipples should not cause problems as the baby is able to form a teat from both the breast and nipple. �Long nipples can lead to poor feeding because although the baby is able to latch on to the nipple, he is unable to draw any breast tissue into his mouth, due to the length of the nipple.
�Abnormally large nipples If the baby is small, his mouth may not be able to get beyond the nipple and onto the breast. Lactation can be initiated by expressing, by hand or by pump, provided the nipple fits into the breast shield. As the baby grows and the breast and nipple become more protractile, breastfeeding may become possible. �Inverted and flat nipples If the nipple is deeply inverted it may be necessary to initiate lactation by expressing and delay attempting to attach the baby to the breast until lactation is established and the breasts have become soft and the breast tissue more elastic.
diffculties with breastfeeding Engorgement This condition occurs around the 3 rd or 4 th day following the baby's birth. ü The breasts become hard, often oedematous, painful and sometimes appear flushed. ü The mother may be pyrexial. ü Engorgement is usually an indication that the baby is not keeping pace with the stage of lactation. ü Engorgement may occur if feeds are delayed or restricted or if the baby is unable to feed efficiently because he is not correctly attached to the breast ü
Deep breast pain �deep breast pain responds to improvement in breastfeeding technique and is likely to be due to raised intraductal pressure caused by inefficient milk removal. � Although it may occur during the feed, it typically occurs afterwards. � This distinguishes it from the sensation of the letdown reflex , which some mothers experience as a fleeting pain. �Very rarely, deep breast pain may be the result of ductal thrush infection
Mastitis � an inflammation of the breast, is the result of milk stasis, not infection, although infection may supervene �one or more adjacent segments of breast tissue are inflamed through milk being forced into the connective tissue of the breast, and appear as wedge-shaped areas of redness and swelling. �If milk is forced back into the bloodstream, the woman's pulse and temperature may rise and in some cases flu-like symptoms, including shivering attacks or rigors, may occur. �The presence or absence of systemic symptoms does not help to distinguish infectious from non-infectious mastitis
Infective mastitis �The main cause of superficial breast infection is damage to the epithelium, allowing bacteria to enter the underlying tissues. � The damage usually results from incorrect attachment of the baby to the breast, which has caused trauma to the nipple. � The motherefore requires urgent assistance to improve her feeding technique, as well as appropriate antibiotics. �Multiplication of bacteria may be enhanced by the use of breast pads or shells. �In spite of antibiotic therapy, abscess formation may occur. Infection may also enter the breast via the milk ducts if milk stasis remains unresolved
Breast abscess A fluctuant swelling develops in a previously inflamed area: namely a breast abscess. Pus may be discharged from the nipple. ü Simple needle aspiration may be effective, or incision and drainage may be necessary ü It may not be possible for the baby to feed from the affected breast for a few days, ü milk removal should continue by expression would reduce the chances of further abscess formation ü A sinus that drains milk may form, but it is likely to heal in time. ü
Blocked ducts �Lumpy areas in the breast are not uncommon, due to distended glandular tissue. If such lumps become very firm and tender and sometimes flushed, they are often described as blocked ducts. �a physical obstruction within the lumen of the duct. � this is very rarely the cause of the symptoms. It is much more likely that milk drainage has been somewhat uneven due to less than optimal attachment and that secreted milk is trying to occupy more space than is actually available, causing the alveoli to distend. � Milk may subsequently be forced out into the connective tissue of the breast where it causes inflammation. �The inflammatory process narrows the lumen of the duct by exerting pressure on it from the outside as the tissue swells, resulting in mastitis or incipient mastitis. �the solution is to improve milk drainage by improved afachment, with possibly milk expression, and to treat the accompanying pain and inflammation.
White spots/epithelial overgrowth �Very occasionally, a ductal opening in the tip of the nipple may become obstructed by epithelial overgrowth. �A white blister is evident on the surface of the nipple, effectively causing a physical obstruction closing off the exit points from one or more milk- producing sections of the breast. �This may sometimes be resolved by the baby feeding. Alternatively, after the baby has fed and the skin is softened, the blister may be removed with a clean fingernail, a rough flannel, or a sterile needle. �True blockages of this sort tend to recur, but once the woman understands how to deal with them, the progression to mastitis can be avoided.
Feeding difficulties due to the baby q Colic in the breastfed baby q. Cleft lip q. Cleft palate q. Tongue tie (Ankyloglossia) q. Blocked nose q. Down syndrome q. Prematurity q. Illness or surgery
Contraindication to breastfeeding Breastfeeding may have to be suspended temporarily following the administration of certain drug , eg, chloramphenicol. Most region have drug centres pharmacy information services where advice may be sought about the saftey of drug for lactating women qcarcinoma q. Breast suergery q. Breast injury q. One breast only q. Human immunodeficiency virus infection
Weaning from the breast �When the mother or the baby decides to stop breastfeeding, �feeds should be tailed off gradually. � Breastfeeds may be omitted, one at a time, and spaced further apart. � Adding supplementary foods should not begin until about 6 months of age. �If the mother uses solid food to give the baby tasters and the experience of different textures before weaning, these should be given after the breastfeed. �Solid foods given to the baby before the breastfeed (weaning) will result in them taking less milk from the breast and less milk being produced. � Allowing the baby to lead the process of weaning may make the transition much easier.
The baby friendly hospital initiative �The Baby Friendly Hospital Initiative (BFI) was an initiative launched worldwide in 1991 (and in the UK in 1994) by WHO and UNICEF to encourage hospitals to promote practices supportive of breastfeeding. � It was focused around the 10 steps to successful breastfeeding with which all hospitals who wish to achieve Baby Friendly status must comply �Evidence for the 10 steps is contained in the WHO/UNICEF document of the same name �This has subsequently been extended to community-based facilities, neonatal units and university training programmes for midwifery and health visiting, all of which can be BFI- accredited in their own right. �In addition, all accredited Baby Friendly facilities must fully implement the International Code on the Marketing of Breastmilk Substitutes
The 1 0 steps t o successful breast feeding 1) 2) 3) 4) 5) Have a written breastfeeding policy that is routinely communicated to all healthcare staff. Train all healthcare staff in skills necessary to implement this policy. Inform all pregnant women about the benefits and management of breastfeeding. Help mothers initiate breastfeeding soon after birth. Show mothers how to breastfeed and how to maintain lactation even if they should be separated from their infants.
6) Give newborn infants no food or drink other than breastmilk, unless medically indicated. 7) Practice rooming-in: allow mothers and infants to remain together 24 hours a day. 8) Encourage breastfeeding on demand. 9) Give no artificial teats or dummies to breastfeeding infants. 10) Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from hospital or clinic.

Thanks