Indications for Not Doing EVAR Edward Woo Associate





- Slides: 38
Indications for Not Doing EVAR Edward Woo Associate Professor Vice Chief/Program Director of Vascular Laboratory Division of Vascular Surgery and Endovascular Therapy University of Pennsylvania Health System Department of Surgery, University of Pennsylvania Health System
Disclosures § Medtronic, Cook, Gore Department of Surgery, University of Pennsylvania Health System
AAA § Affects 5 -9% of men >65 in US – CMS approved screening abd u/s in men >65 § Risk factors – – – FH HTN Chol DM Tobacco Department of Surgery, University of Pennsylvania Health System
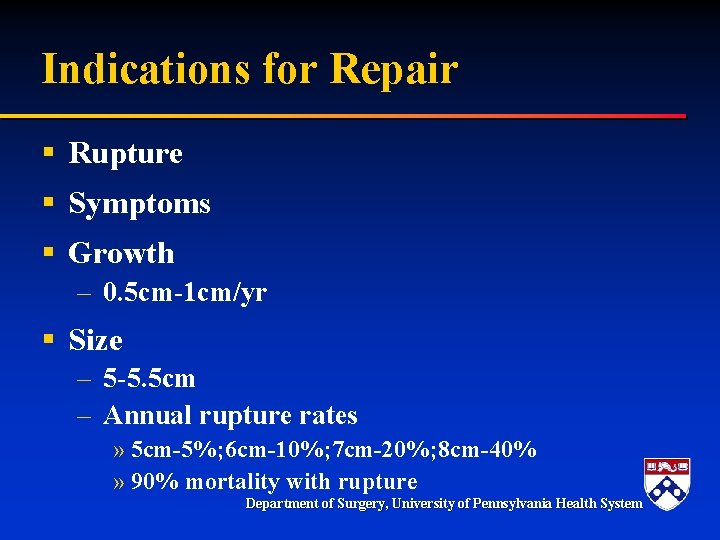
Indications for Repair § Rupture § Symptoms § Growth – 0. 5 cm-1 cm/yr § Size – 5 -5. 5 cm – Annual rupture rates » 5 cm-5%; 6 cm-10%; 7 cm-20%; 8 cm-40% » 90% mortality with rupture Department of Surgery, University of Pennsylvania Health System
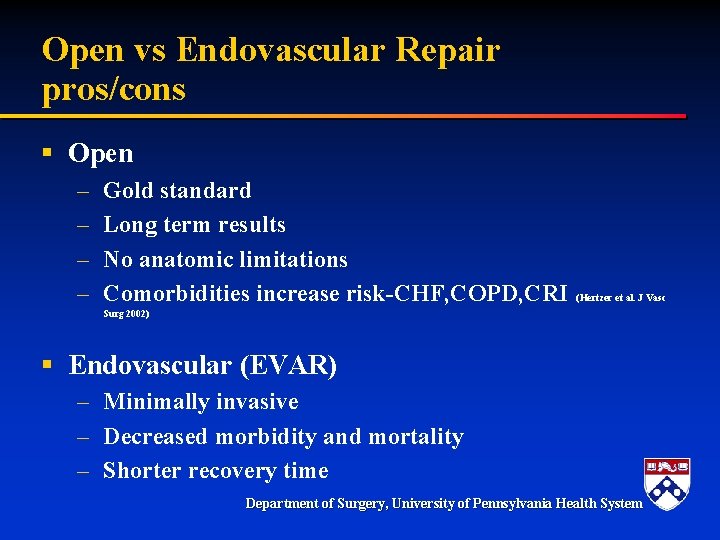
Open vs Endovascular Repair pros/cons § Open – – Gold standard Long term results No anatomic limitations Comorbidities increase risk-CHF, COPD, CRI (Hertzer et al. J Vasc Surg 2002) § Endovascular (EVAR) – Minimally invasive – Decreased morbidity and mortality – Shorter recovery time Department of Surgery, University of Pennsylvania Health System
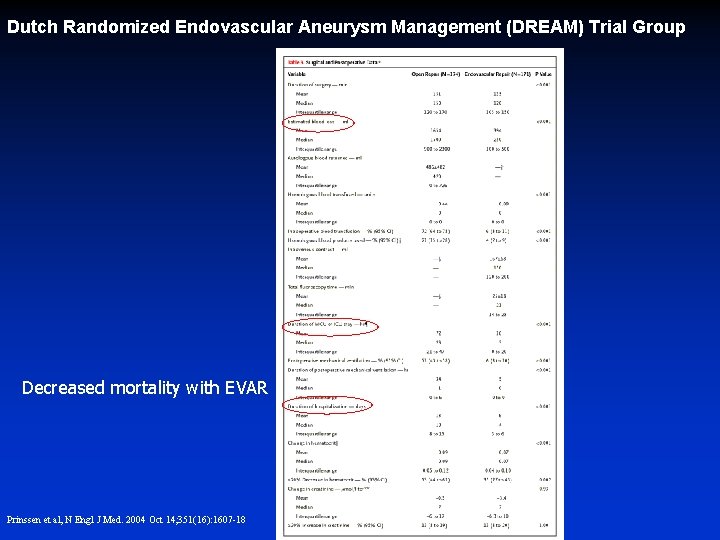
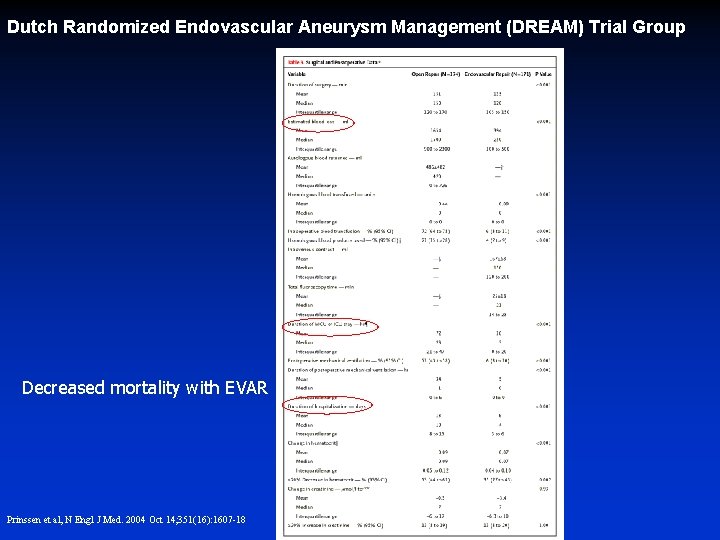
Dutch Randomized Endovascular Aneurysm Management (DREAM) Trial Group Decreased mortality with EVAR Prinssen et al, N Engl J Med. 2004 Oct 14; 351(16): 1607 -18
Why ever perform open AAA repair? Department of Surgery, University of Pennsylvania Health System
Indications for Open Repair § Anatomic Constraints – Proximal – Distal – Other § Endoleak – Recurrent sac growth § Infection – Mycotic AAA – Infected Stent graft § Other Department of Surgery, University of Pennsylvania Health System
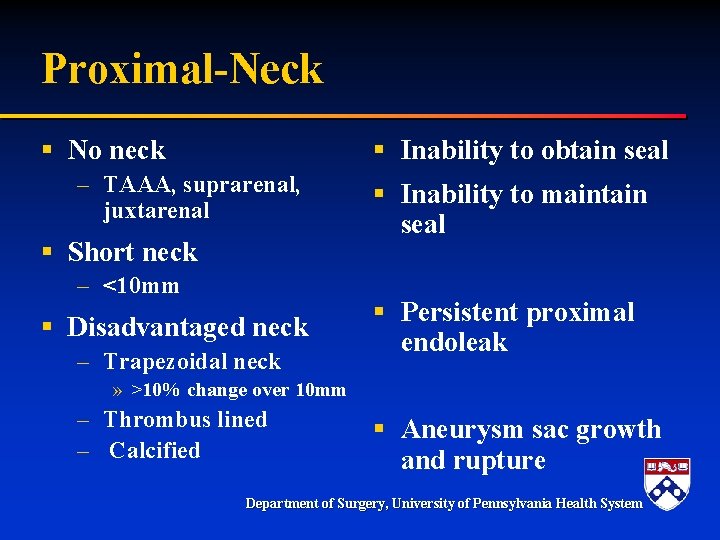
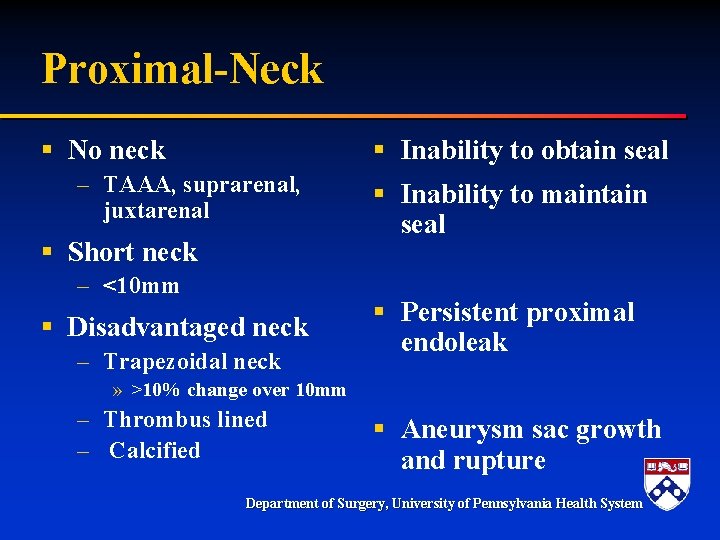
Proximal-Neck § No neck § Inability to obtain seal – TAAA, suprarenal, juxtarenal § Short neck – <10 mm § Disadvantaged neck – Trapezoidal neck § Inability to maintain seal § Persistent proximal endoleak » >10% change over 10 mm – Thrombus lined – Calcified § Aneurysm sac growth and rupture Department of Surgery, University of Pennsylvania Health System
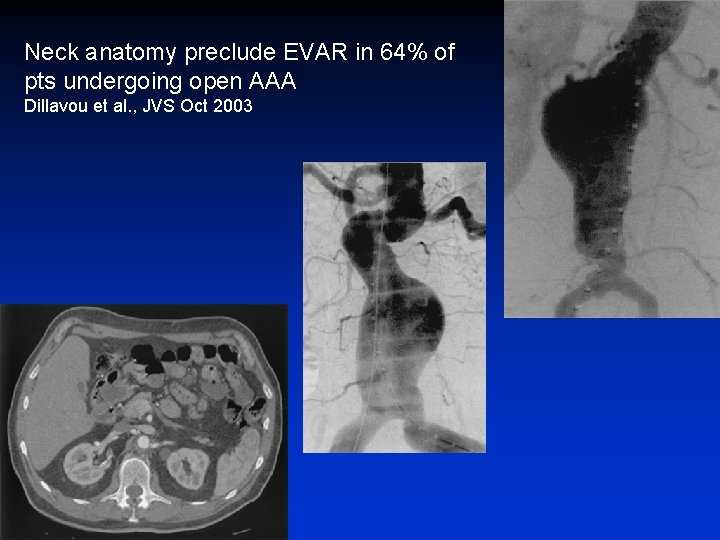
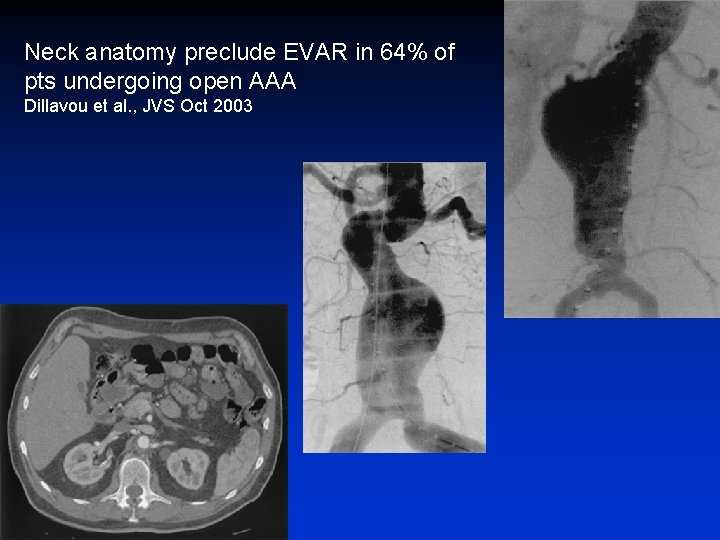
Neck anatomy preclude EVAR in 64% of pts undergoing open AAA Dillavou et al. , JVS Oct 2003
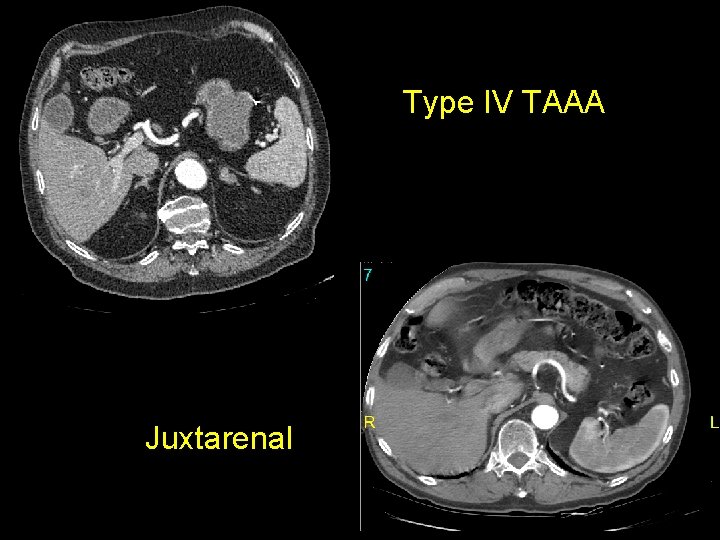
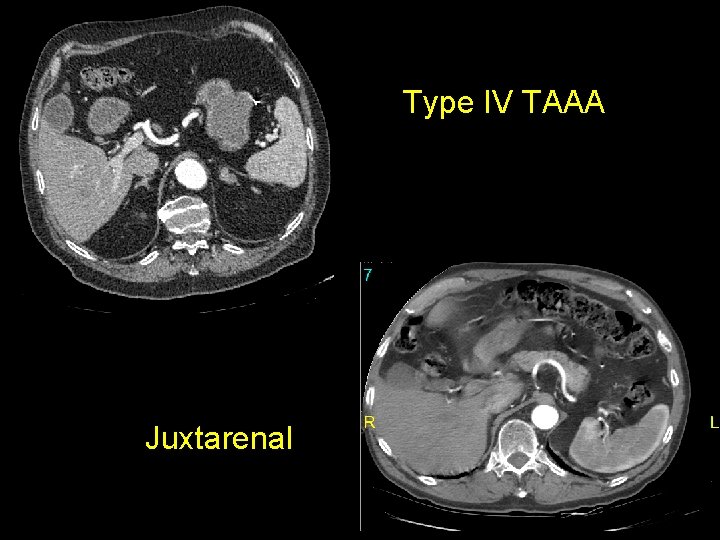
Type IV TAAA Juxtarenal
EVAR Constraints Not Limited to Proximal Neck § Moise et al. Vasc Endovasc Srg 2006 – Early and later experience groups – Proximal and distal landing zones continue to limit EVAR Department of Surgery, University of Pennsylvania Health System
Distal § Aortic length § Narrow/calcified bifurcation § Iliac aneurysms – Preservation of hypogastrics » » Claudication Colonic ischemia Pelvic ischemia-impotence Spinal cord ischemia Department of Surgery, University of Pennsylvania Health System
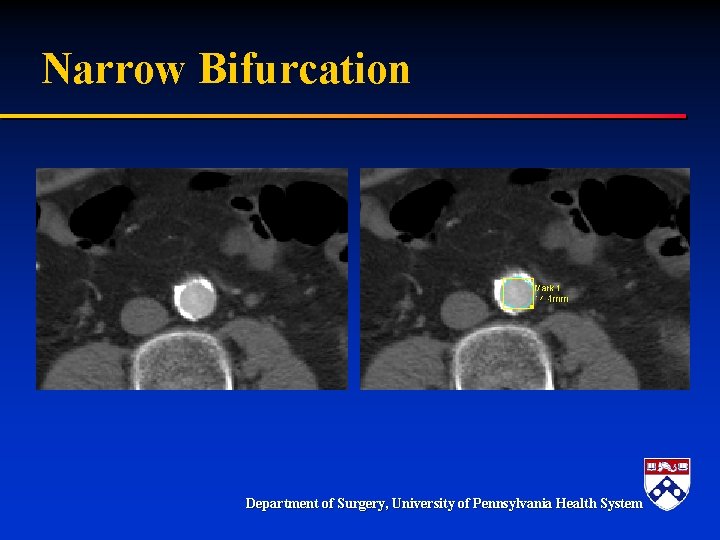
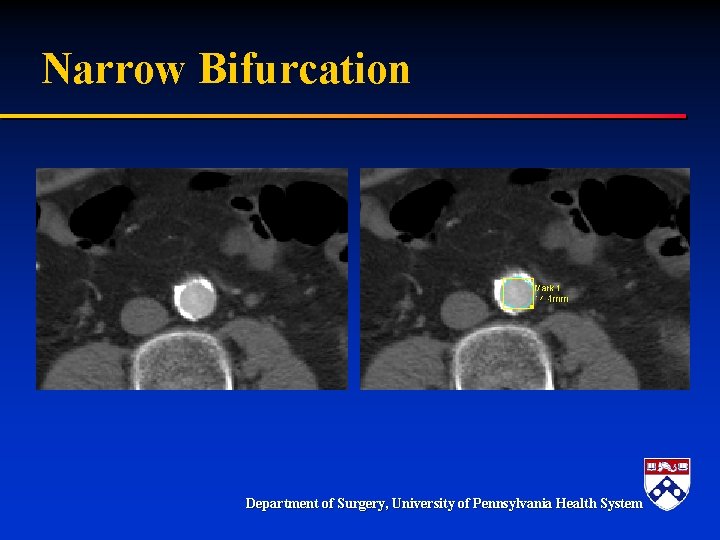
Narrow Bifurcation Department of Surgery, University of Pennsylvania Health System

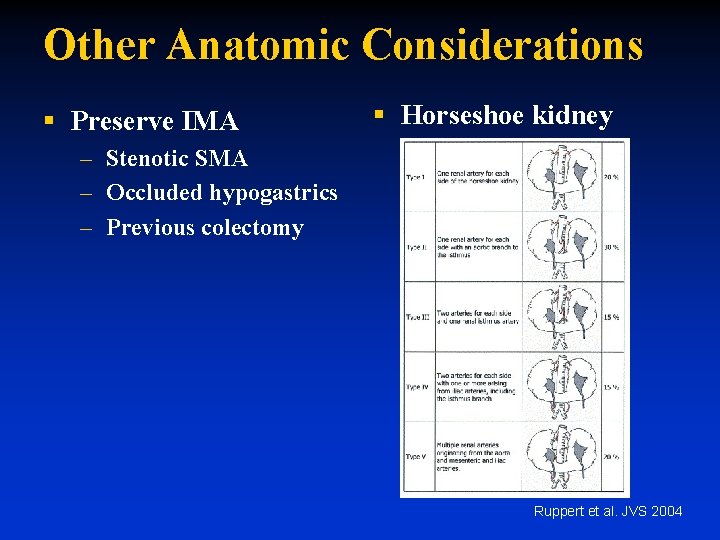
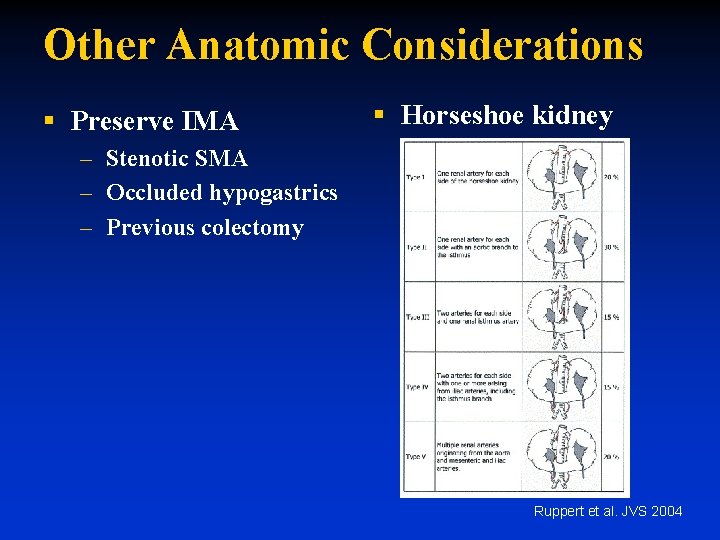
Other Anatomic Considerations § Preserve IMA § Horseshoe kidney – Stenotic SMA – Occluded hypogastrics – Previous colectomy Ruppert et al. JVS 2004
Other Anatomic Considerations § Access – Less common now » Stiffer wires » Smaller devices » Devices less stiff – Female>male § Tortuosity § Uncommon unless at proximal neck
Indications for Open Repair § Anatomic Constraints – Proximal – Distal – Other § Endoleak – Recurrent sac growth § Infection – Mycotic AAA – Infected Stent graft § Other Department of Surgery, University of Pennsylvania Health System
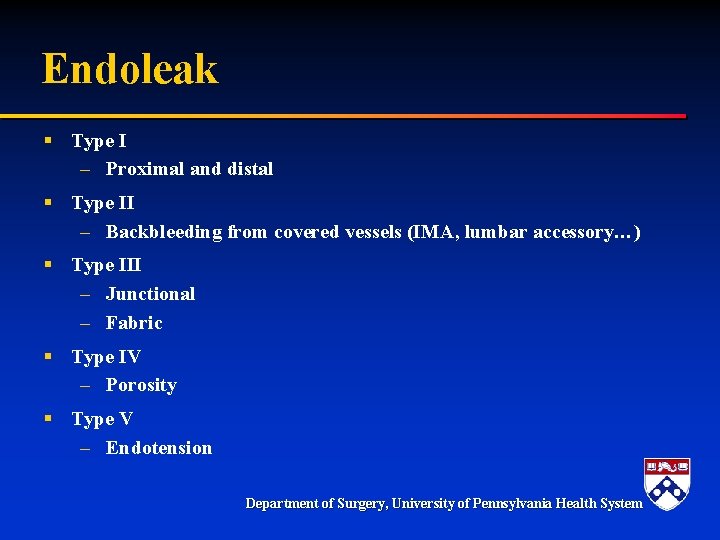
Endoleak § Type I – Proximal and distal § Type II – Backbleeding from covered vessels (IMA, lumbar accessory…) § Type III – Junctional – Fabric § Type IV – Porosity § Type V – Endotension Department of Surgery, University of Pennsylvania Health System
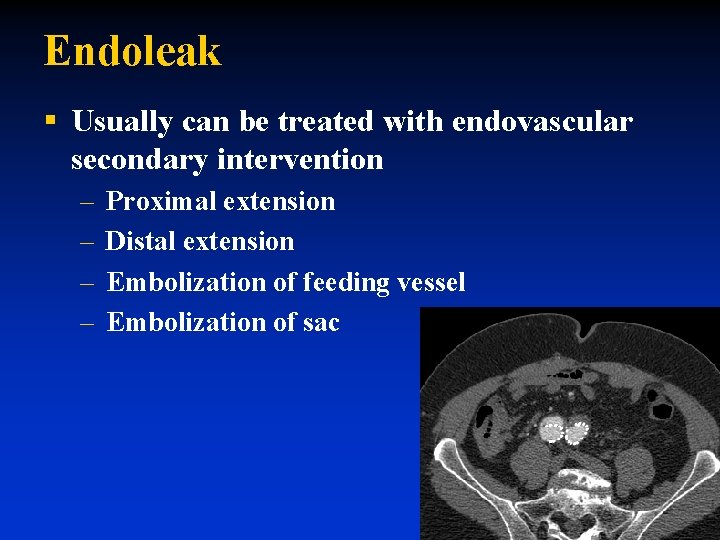
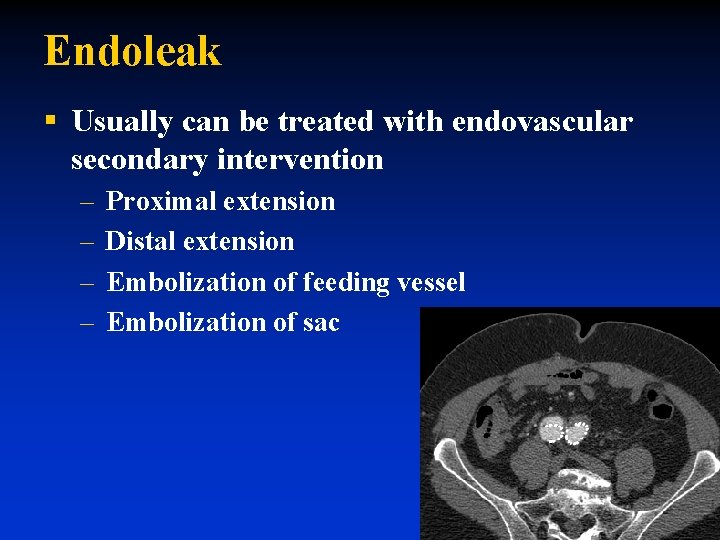
Endoleak § Usually can be treated with endovascular secondary intervention – – Proximal extension Distal extension Embolization of feeding vessel Embolization of sac
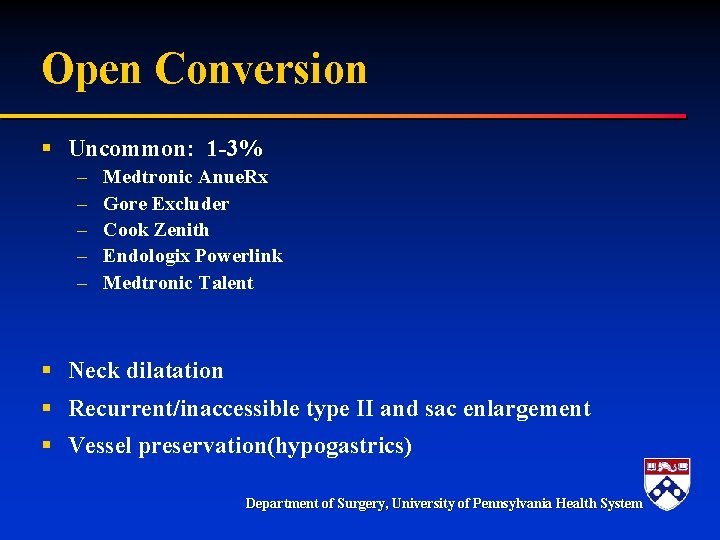
Open Conversion § Uncommon: 1 -3% – – – Medtronic Anue. Rx Gore Excluder Cook Zenith Endologix Powerlink Medtronic Talent § Neck dilatation § Recurrent/inaccessible type II and sac enlargement § Vessel preservation(hypogastrics) Department of Surgery, University of Pennsylvania Health System


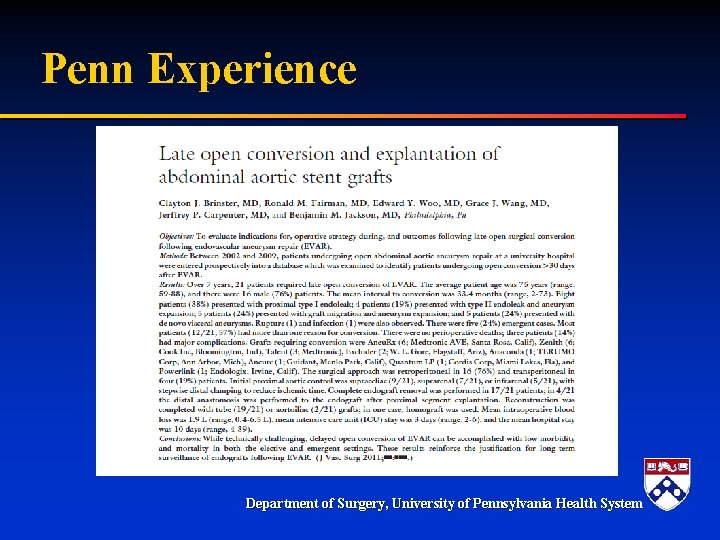
Penn Experience Department of Surgery, University of Pennsylvania Health System
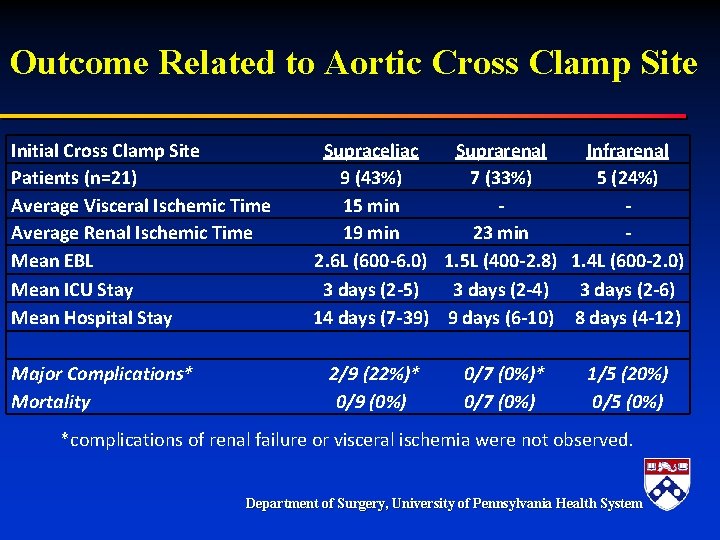
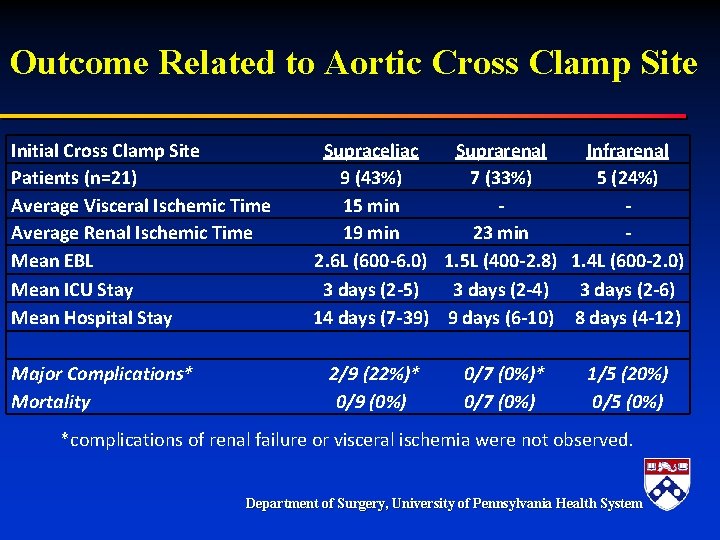
Outcome Related to Aortic Cross Clamp Site Initial Cross Clamp Site Patients (n=21) Average Visceral Ischemic Time Average Renal Ischemic Time Mean EBL Mean ICU Stay Mean Hospital Stay Major Complications* Mortality Supraceliac Suprarenal Infrarenal 9 (43%) 7 (33%) 5 (24%) 15 min 19 min 23 min 2. 6 L (600 -6. 0) 1. 5 L (400 -2. 8) 1. 4 L (600 -2. 0) 3 days (2 -5) 3 days (2 -4) 3 days (2 -6) 14 days (7 -39) 9 days (6 -10) 8 days (4 -12) 2/9 (22%)* 0/9 (0%) 0/7 (0%)* 0/7 (0%) 1/5 (20%) 0/5 (0%) *complications of renal failure or visceral ischemia were not observed. Department of Surgery, University of Pennsylvania Health System
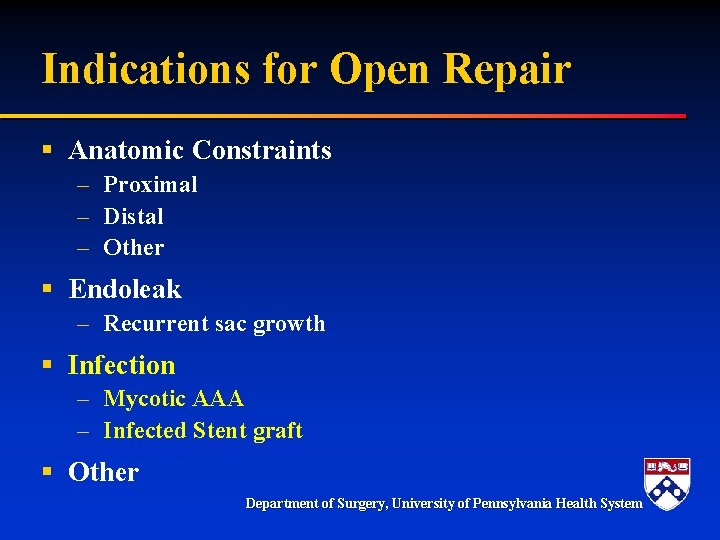
Indications for Open Repair § Anatomic Constraints – Proximal – Distal – Other § Endoleak – Recurrent sac growth § Infection – Mycotic AAA – Infected Stent graft § Other Department of Surgery, University of Pennsylvania Health System
Mycotic aneurysm § Fever, increased WBC, +blood cx’s, saccular aneurysm, rapid enlargement, adjacent abscess § Homograft vs Rifampin/Dacron vs extraanatomic repair § EVAR-bailout or bridge Department of Surgery, University of Pennsylvania Health System

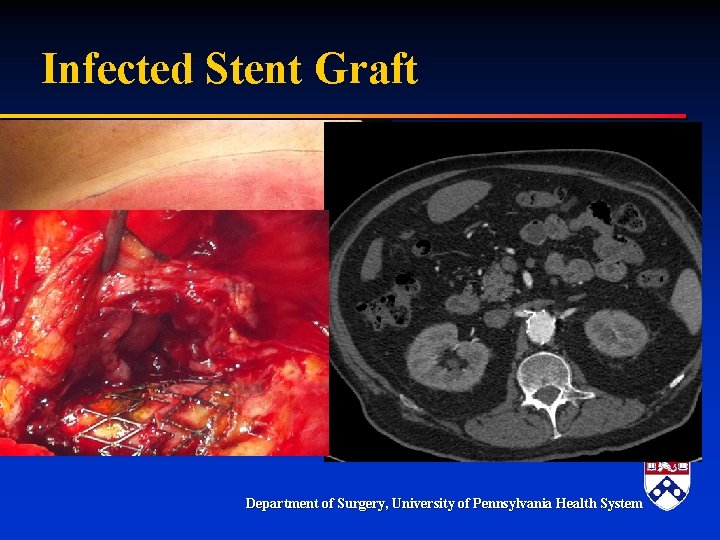
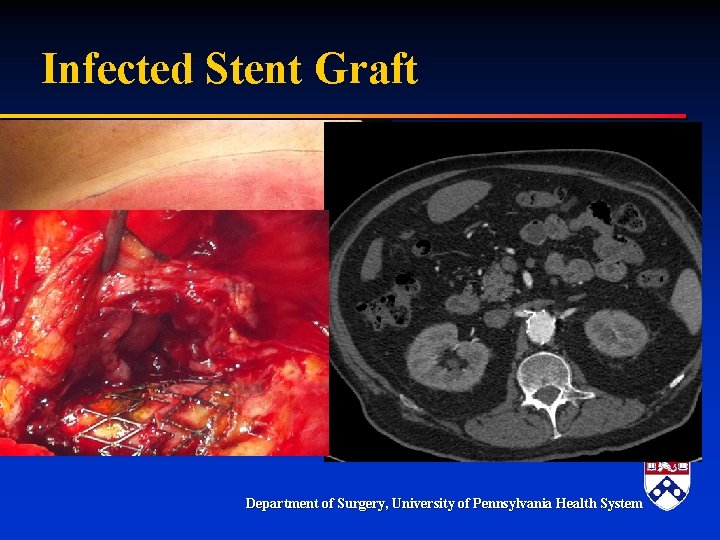
Infected Stent Graft § Uncommon but incidence may be increasing Department of Surgery, University of Pennsylvania Health System
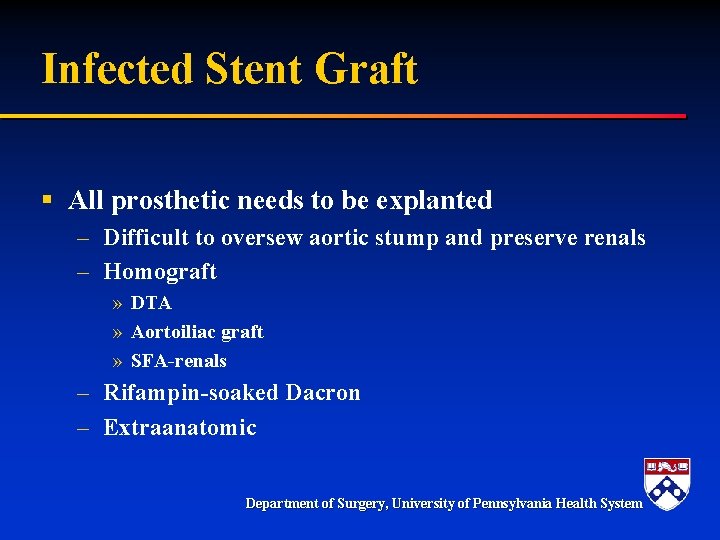
Infected Stent Graft § All prosthetic needs to be explanted – Difficult to oversew aortic stump and preserve renals – Homograft » DTA » Aortoiliac graft » SFA-renals – Rifampin-soaked Dacron – Extraanatomic Department of Surgery, University of Pennsylvania Health System
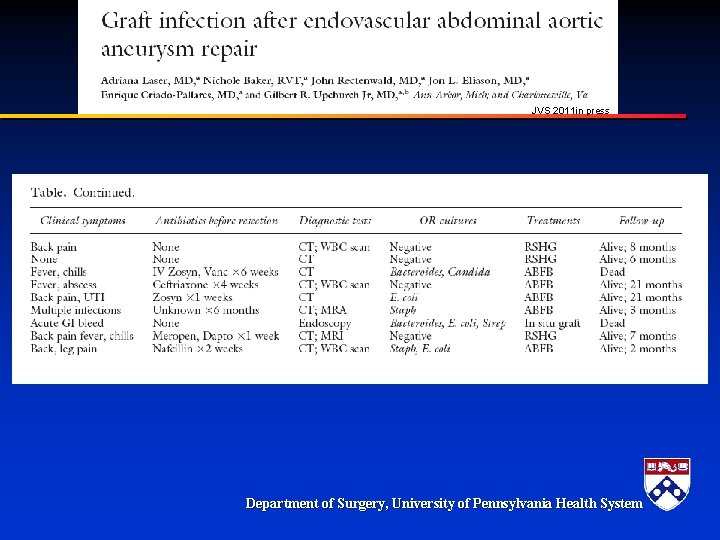
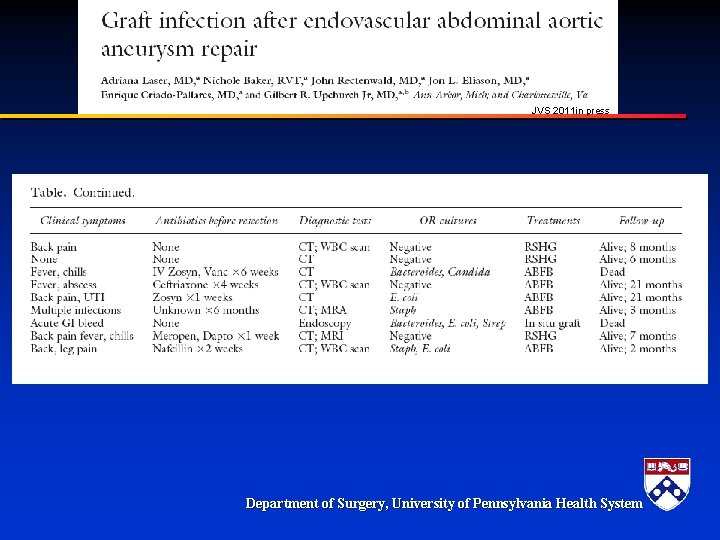
JVS 2011 in press Department of Surgery, University of Pennsylvania Health System

Indications for Open Repair § Anatomic Constraints – Proximal – Distal – Other § Endoleak – Recurrent sac growth § Infection – Mycotic AAA – Infected Stent graft § Other – Renal insufficiency, Age, patient preference… Department of Surgery, University of Pennsylvania Health System
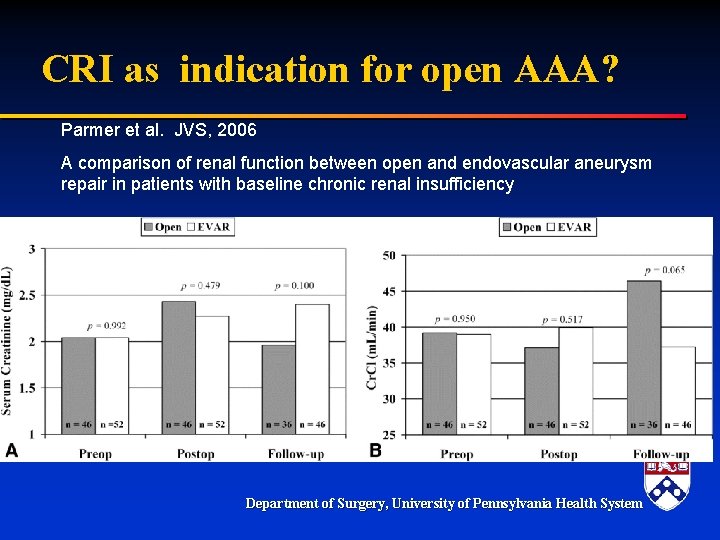
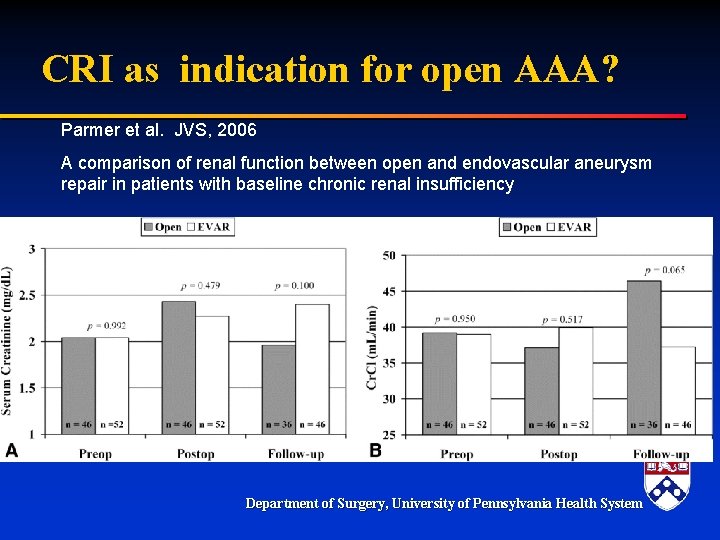
CRI as indication for open AAA? Parmer et al. JVS, 2006 A comparison of renal function between open and endovascular aneurysm repair in patients with baseline chronic renal insufficiency Department of Surgery, University of Pennsylvania Health System
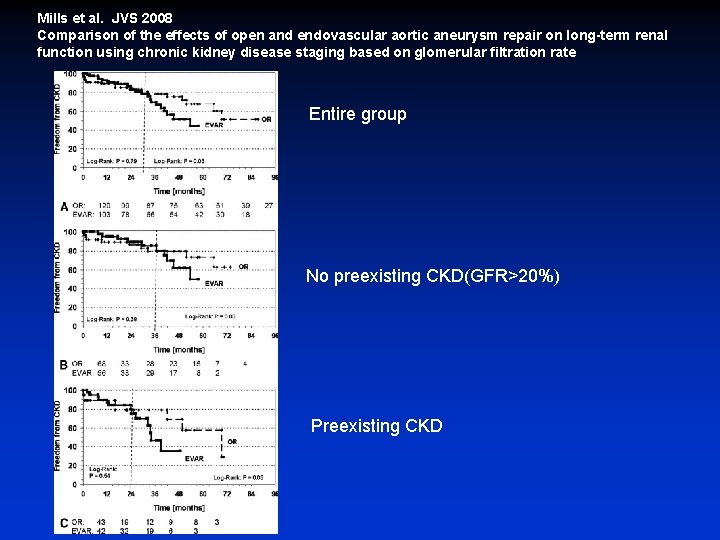
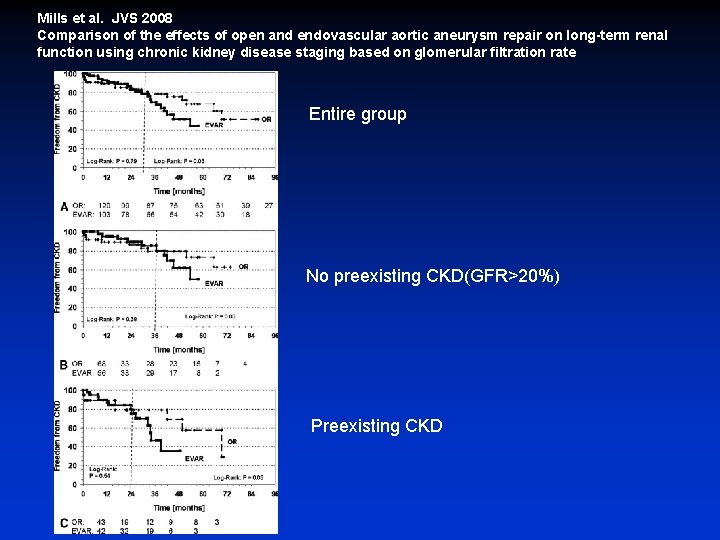
Mills et al. JVS 2008 Comparison of the effects of open and endovascular aortic aneurysm repair on long-term renal function using chronic kidney disease staging based on glomerular filtration rate Entire group No preexisting CKD(GFR>20%) Preexisting CKD
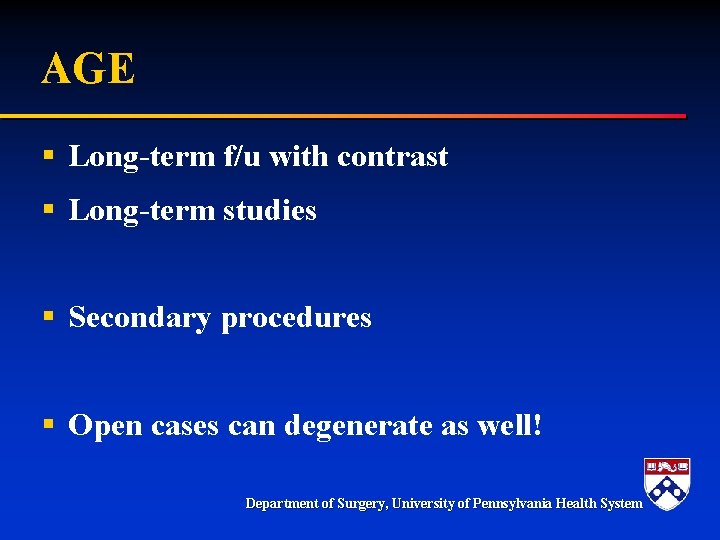
AGE § Long-term f/u with contrast § Long-term studies § Secondary procedures § Open cases can degenerate as well! Department of Surgery, University of Pennsylvania Health System
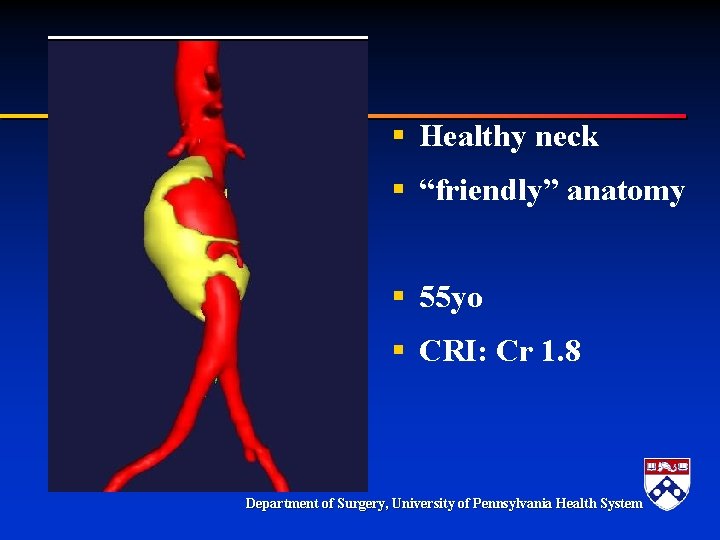
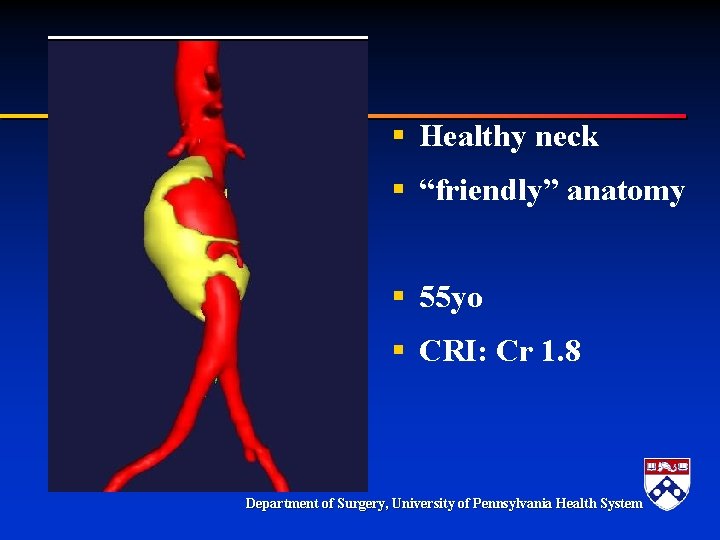
§ Healthy neck § “friendly” anatomy § 55 yo § CRI: Cr 1. 8 Department of Surgery, University of Pennsylvania Health System
Summary § Open AAA indications – – Anatomy Recalcitrant endoleak Infection Other § Can be done with low morbidity and mortality Department of Surgery, University of Pennsylvania Health System