Indications for CTOPCI Clinical Rationale and Appropriateness J








- Slides: 21
Indications for CTO-PCI: Clinical Rationale and Appropriateness J. Aaron Grantham, MD, FACC, FSCAI Associate Professor of Medicine University of Missouri Kansas City Saint Luke’s Mid America Heart Institute Kansas City, MO www. ctofundamentals. org

J. Aaron Grantham, MD Consulting: Abbott Vascular Grant Support: Abbott Vascular. Medtronic, Inc. , Asahi Intecc Co. Honoraria: Boston Scientific Corporation, Bridge. Point Off-Label: No FDA approved stent for CTO-PCI. Will not recommend one in particular.
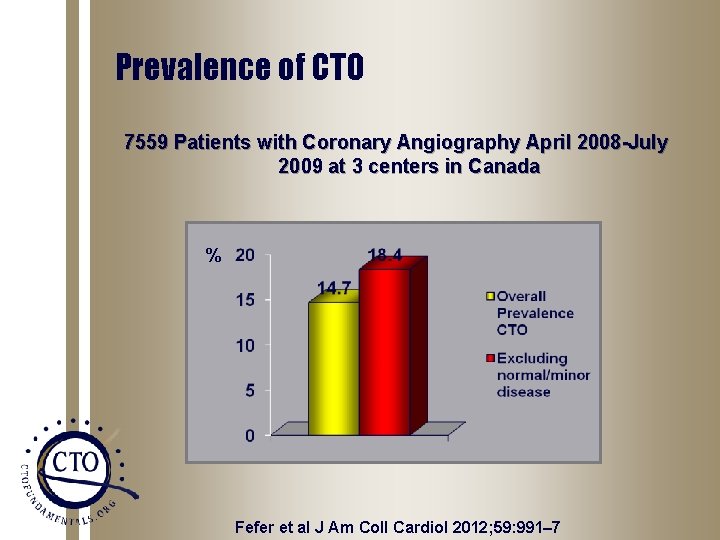
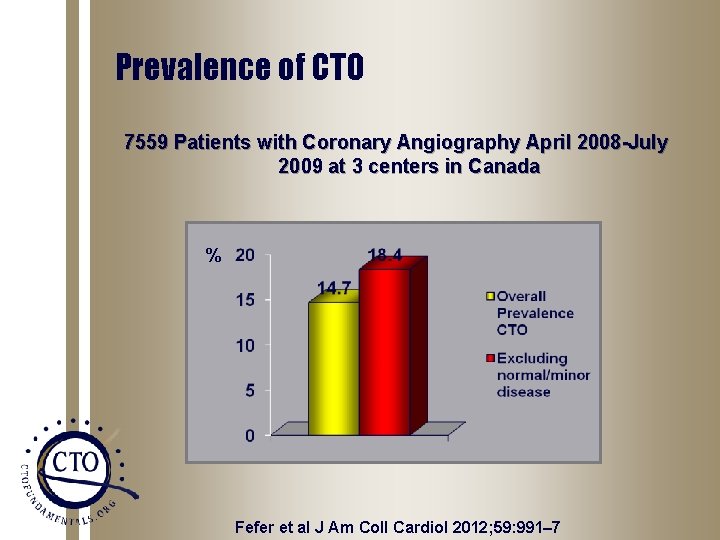
Prevalence of CTO 7559 Patients with Coronary Angiography April 2008 -July 2009 at 3 centers in Canada % Fefer et al J Am Coll Cardiol 2012; 59: 991– 7

CTO-PCI Variability CTO PCI attempt rate variability in Canada Fefer et al J Am Coll Cardiol 2012; 59: 991– 7
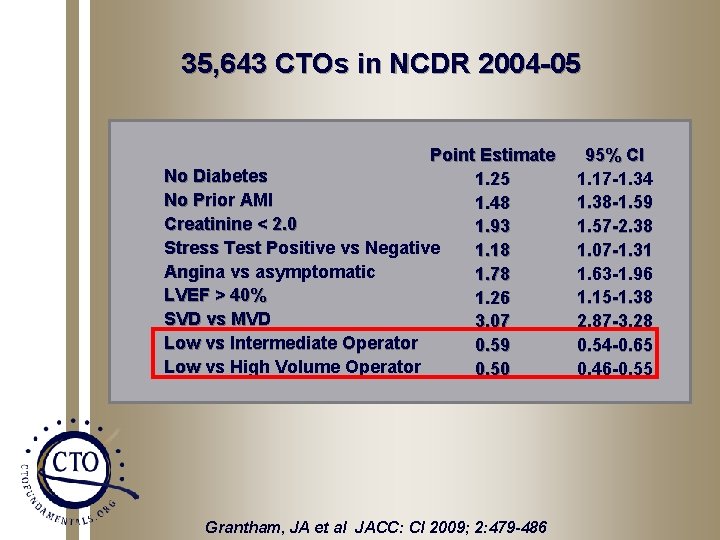
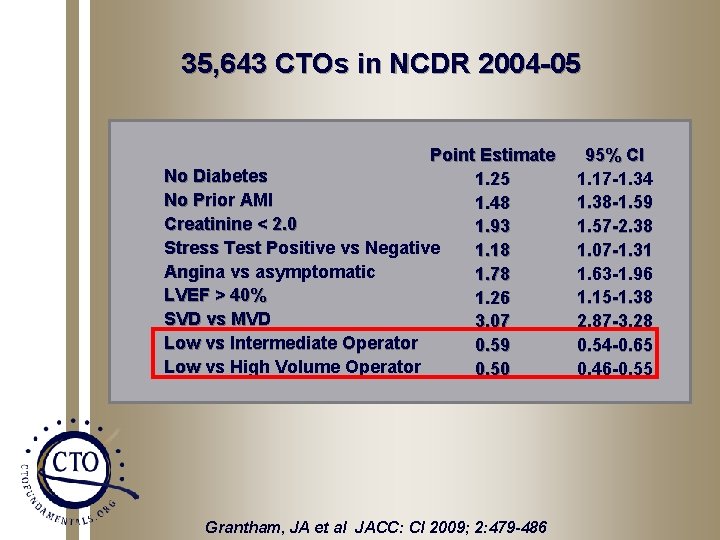
35, 643 CTOs in NCDR 2004 -05 Point Estimate No Diabetes 1. 25 No Prior AMI 1. 48 Creatinine < 2. 0 1. 93 Stress Test Positive vs Negative 1. 18 Angina vs asymptomatic 1. 78 LVEF > 40% 1. 26 SVD vs MVD 3. 07 Low vs Intermediate Operator 0. 59 Low vs High Volume Operator 0. 50 Grantham, JA et al JACC: CI 2009; 2: 479 -486 95% CI 1. 17 -1. 34 1. 38 -1. 59 1. 57 -2. 38 1. 07 -1. 31 1. 63 -1. 96 1. 15 -1. 38 2. 87 -3. 28 0. 54 -0. 65 0. 46 -0. 55
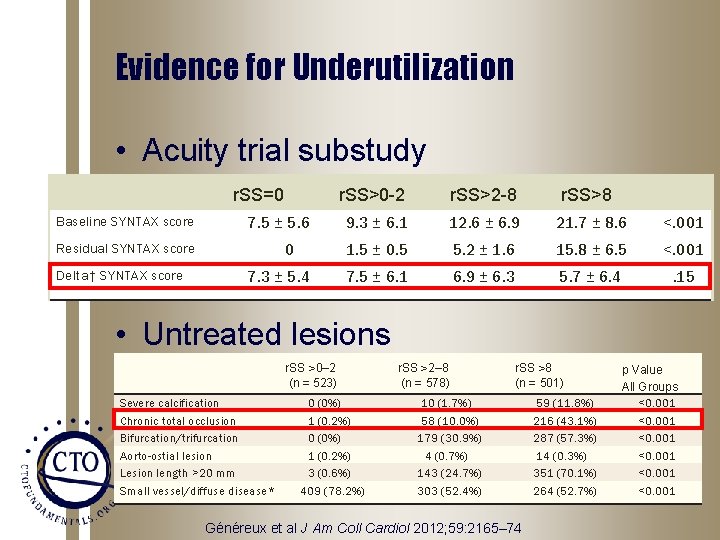
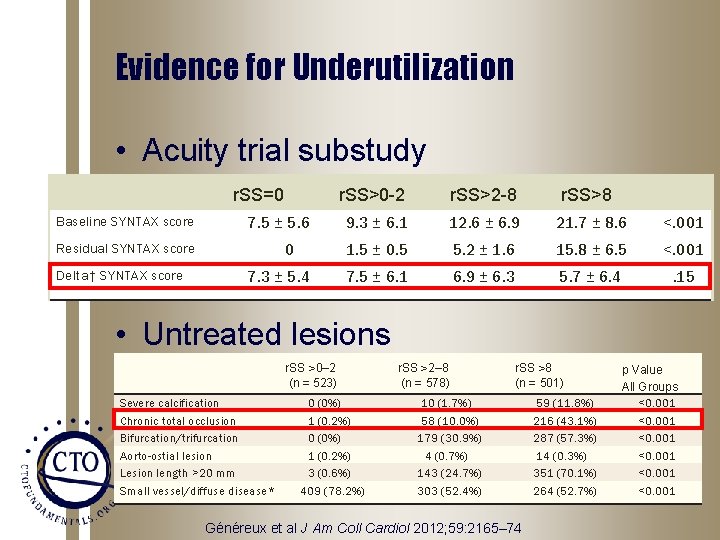
Evidence for Underutilization • Acuity trial substudy r. SS=0 r. SS>0 -2 r. SS>2 -8 r. SS>8 r. SS=0 r. SS>0 -2 r. SS>2 -8 r. SS>8 Baseline SYNTAX score 7. 5 ± 5. 6 Residual SYNTAX score Delta† SYNTAX score 0 7. 3 ± 5. 4 9. 3 ± 6. 1 12. 6 ± 6. 9 21. 7 ± 8. 6 <. 001 1. 5 ± 0. 5 5. 2 ± 1. 6 15. 8 ± 6. 5 <. 001 7. 5 ± 6. 1 6. 9 ± 6. 3 5. 7 ± 6. 4 . 15 • Untreated lesions r. SS >0– 2 (n = 523) Severe calcification Chronic total occlusion Bifurcation/trifurcation Aorto-ostial lesion Lesion length >20 mm Small vessel/diffuse disease* 0 (0%) 1 (0. 2%) 3 (0. 6%) 409 (78. 2%) r. SS >2– 8 (n = 578) r. SS >8 (n = 501) 10 (1. 7%) 58 (10. 0%) 179 (30. 9%) 4 (0. 7%) 143 (24. 7%) 303 (52. 4%) Généreux et al J Am Coll Cardiol 2012; 59: 2165– 74 59 (11. 8%) 216 (43. 1%) 287 (57. 3%) 14 (0. 3%) 351 (70. 1%) 264 (52. 7%) p Value All Groups <0. 001

There is no evidence for CTO-PCI Evidence for Quality of Life Benefit Long-term survival free from angina in success vs. failure Joyal D et al. Am Heart J 2010; 160: 179 -87
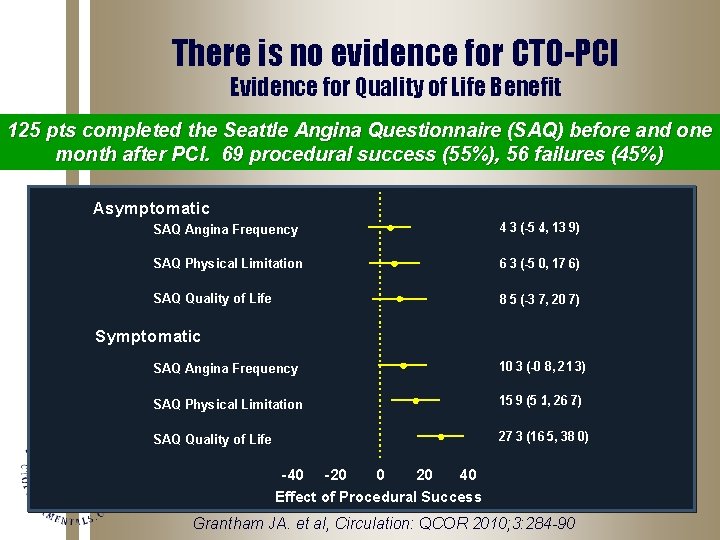
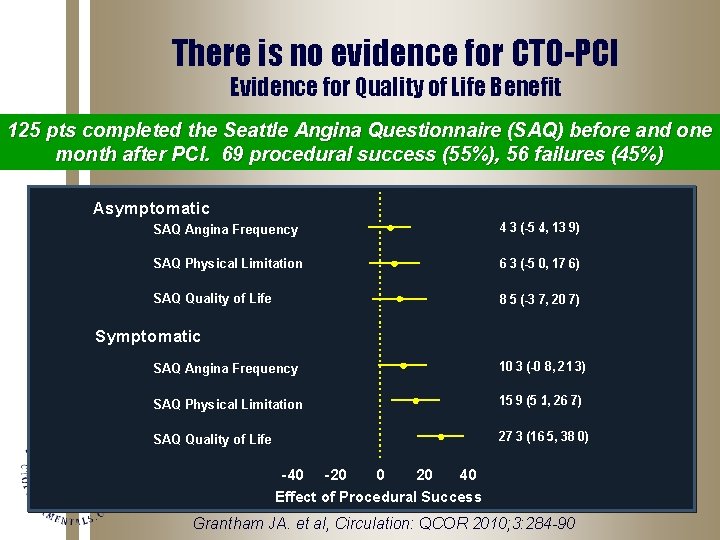
There is no evidence for CTO-PCI Evidence for Quality of Life Benefit 125 pts completed the Seattle Angina Questionnaire (SAQ) before and one month after PCI. 69 procedural success (55%), 56 failures (45%) Asymptomatic SAQ Angina Frequency 43. (-5 4. , 13 9. ) SAQ Physical Limitation 63. (-5 0. , 17 6. ) SAQ Quality of Life 85. (-3 7. , 20 7. ) Symptomatic SAQ Angina Frequency 10 3. (-0 8. , 21 3. ) SAQ Physical Limitation 15 9. (5 1. , 26 7. ) SAQ Quality of Life 27 3. (16 5. , 38 0. ) - 40 -20 0 20 40 Effect of Procedural Success Grantham JA. et al, Circulation: QCOR 2010; 3: 284 -90
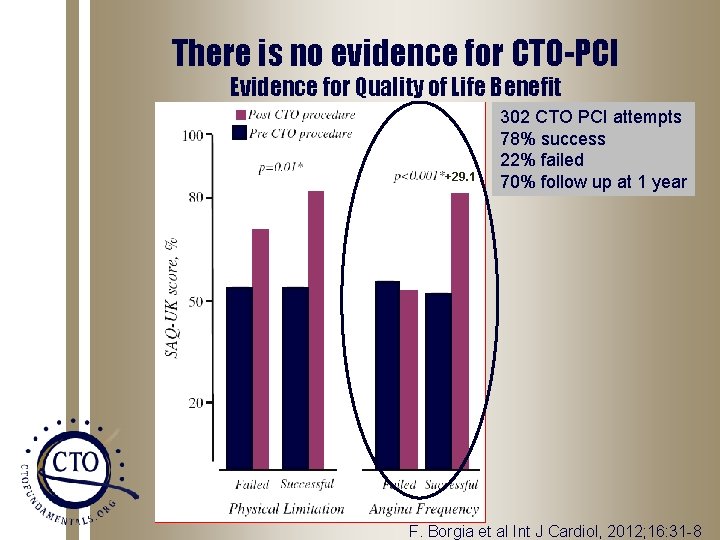
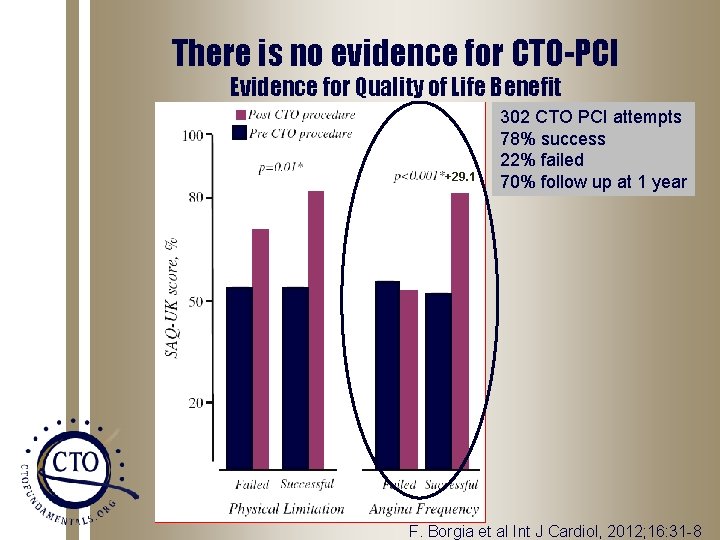
There is no evidence for CTO-PCI Evidence for Quality of Life Benefit +29. 1 302 CTO PCI attempts 78% success 22% failed 70% follow up at 1 year F. Borgia et al Int J Cardiol, 2012; 16: 31 -8
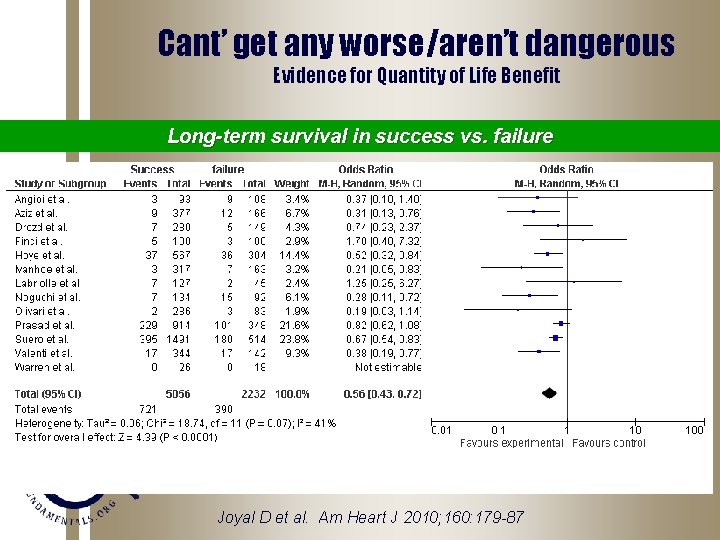
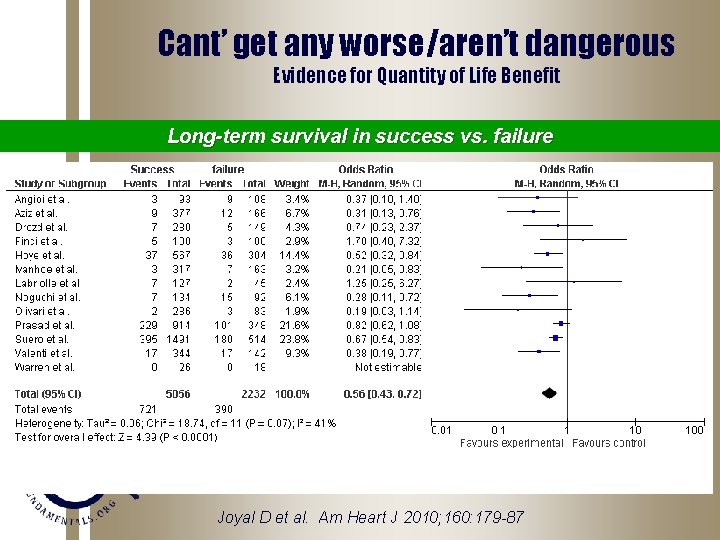
Cant’ get any worse/aren’t dangerous Evidence for Quantity of Life Benefit Long-term survival in success vs. failure Joyal D et al. Am Heart J 2010; 160: 179 -87

Cant’ get any worse/aren’t dangerous Cardiac Death Rate Evidence for Quantity of Life Benefit 7110 1331 718 545 252 0% 1 - 5% 5 -10% 11 -20% >20% % Ischemic Burden Hachamovitch et al Circulation. 2003; 107: 2900 -2907
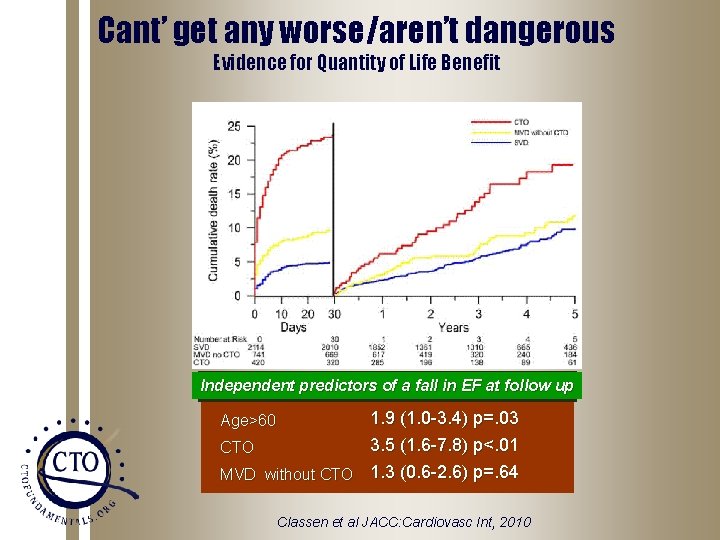
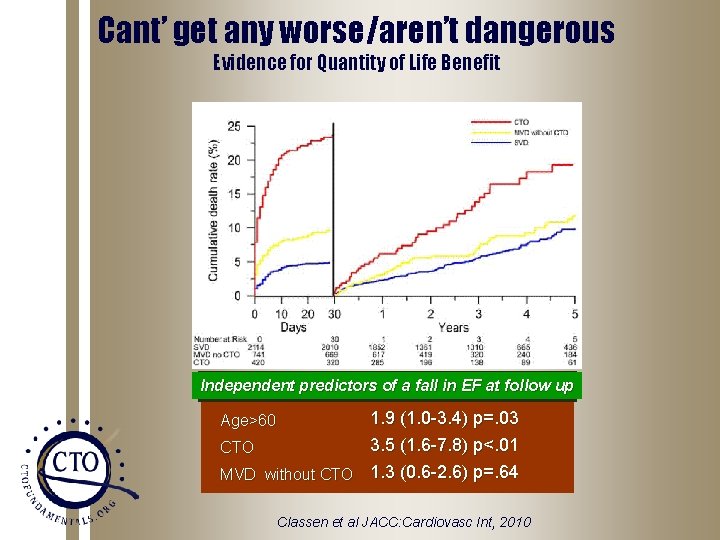
Cant’ get any worse/aren’t dangerous Evidence for Quantity of Life Benefit Independent predictors of a fall in EF at follow up 1. 9 (1. 0 -3. 4) p=. 03 3. 5 (1. 6 -7. 8) p<. 01 CTO MVD without CTO 1. 3 (0. 6 -2. 6) p=. 64 Age>60 Classen et al JACC: Cardiovasc Int, 2010

Cant’ get anyworse/aren’t dangerous Evidence for Quantity of Life Benefit 718 pts AICD for primary prevention. 162 with incomplete revascularization. 44% due to CTO, 56% non CTO residual disease. • Appropriate ICD therapy (12% vs 7% 1 yr. 33% vs 15% at 3 yr) Nombelo et al Circ Arrhythm Electrophysiol 2012; 5: 147 -54

CTO-PCI and AUC Single vessel CTO Class 0 Class I/II Class III/IV High Risk Max Rx U A A Int Risk Max Rx U U A Low Risk Max Rx I U U High Risk No Rx U U A Int Risk No Rx I U U Low Risk No Rx I I I Modified from Patel et al J Am Coll Cardiol 2009; 53: 530 -553
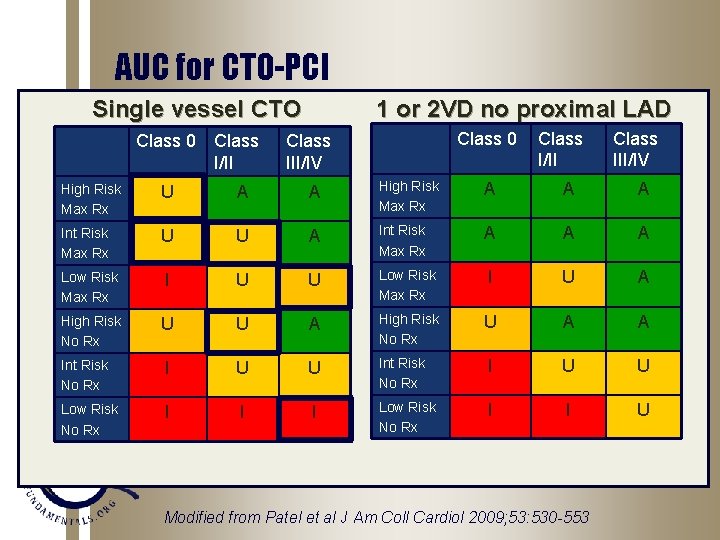
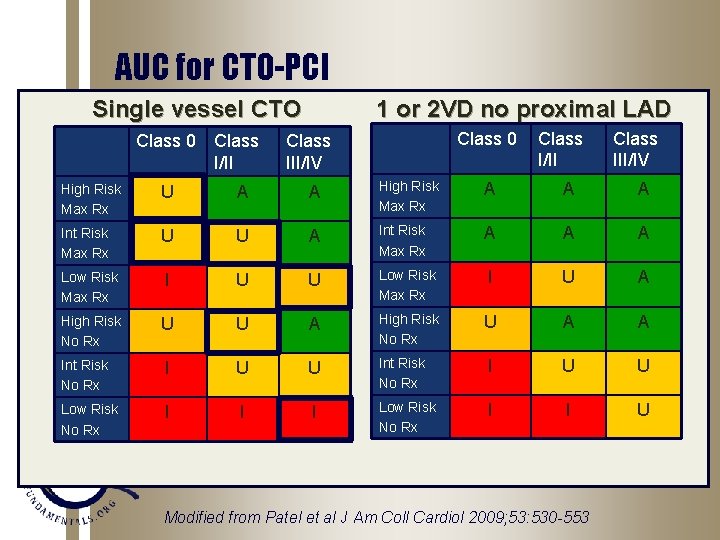
AUC for CTO-PCI Single vessel CTO 1 or 2 VD no proximal LAD Class 0 Class I/II High Risk Max Rx A A Int Risk Max Rx A A A U U Low Risk Max Rx I U A U U A High Risk No Rx U A A Int Risk No Rx I U U Low Risk No Rx I I I Low Risk No Rx I I U Class 0 Class I/II Class III/IV High Risk Max Rx U A A Int Risk Max Rx U U Low Risk Max Rx I High Risk No Rx Modified from Patel et al J Am Coll Cardiol 2009; 53: 530 -553 Class III/IV
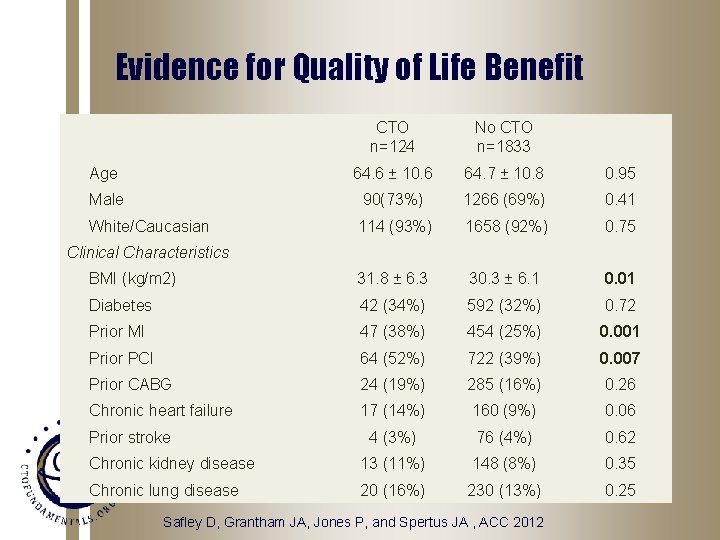
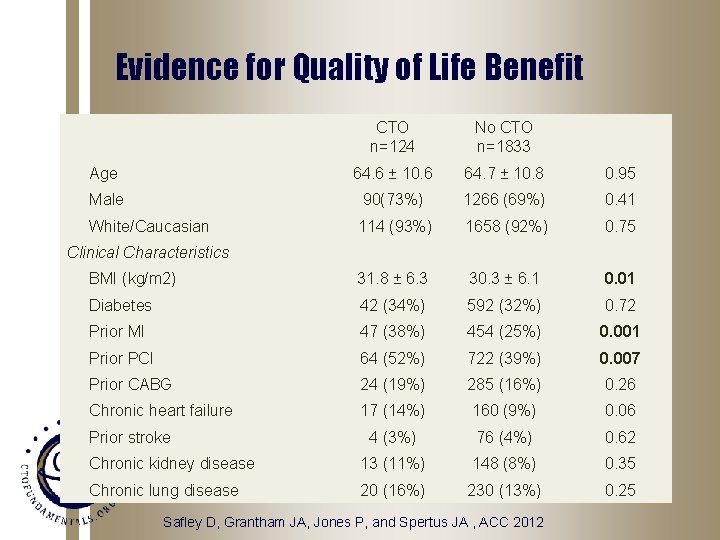
Evidence for Quality of Life Benefit CTO n=124 No CTO n=1833 Age 64. 6 ± 10. 6 64. 7 ± 10. 8 0. 95 Male 90(73%) 1266 (69%) 0. 41 114 (93%) 1658 (92%) 0. 75 BMI (kg/m 2) 31. 8 ± 6. 3 30. 3 ± 6. 1 0. 01 Diabetes 42 (34%) 592 (32%) 0. 72 Prior MI 47 (38%) 454 (25%) 0. 001 Prior PCI 64 (52%) 722 (39%) 0. 007 Prior CABG 24 (19%) 285 (16%) 0. 26 Chronic heart failure 17 (14%) 160 (9%) 0. 06 4 (3%) 76 (4%) 0. 62 Chronic kidney disease 13 (11%) 148 (8%) 0. 35 Chronic lung disease 20 (16%) 230 (13%) 0. 25 White/Caucasian Clinical Characteristics Prior stroke Safley D, Grantham JA, Jones P, and Spertus JA , ACC 2012
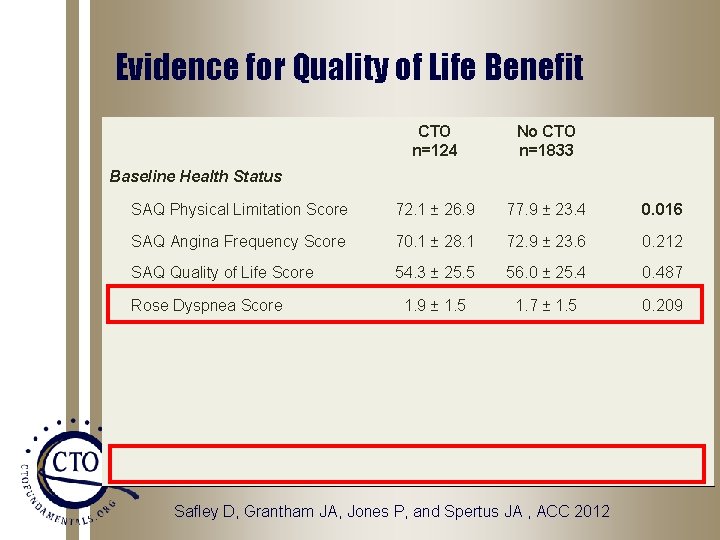
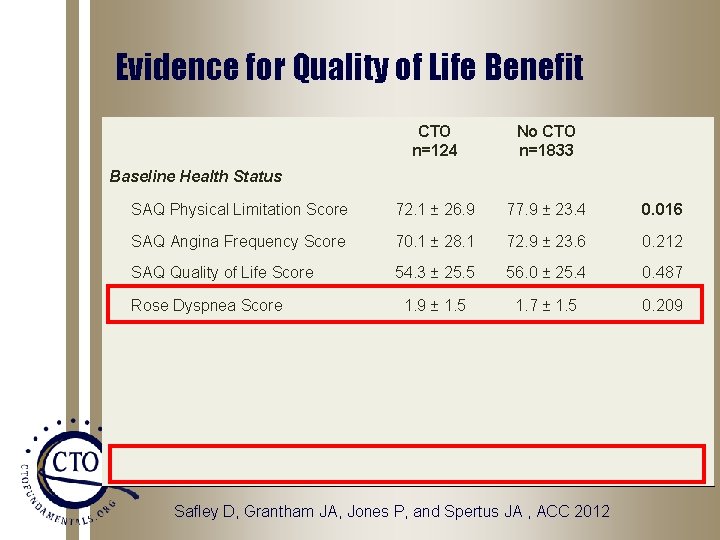
Evidence for Quality of Life Benefit CTO n=124 No CTO n=1833 SAQ Physical Limitation Score 72. 1 ± 26. 9 77. 9 ± 23. 4 0. 016 SAQ Angina Frequency Score 70. 1 ± 28. 1 72. 9 ± 23. 6 0. 212 SAQ Quality of Life Score 54. 3 ± 25. 5 56. 0 ± 25. 4 0. 487 Rose Dyspnea Score 1. 9 ± 1. 5 1. 7 ± 1. 5 0. 209 6 -Month Health Status SAQ Physical Limitation Score 96. 2 ± 12. 8 95. 7 ± 12. 9 0. 742 SAQ Angina Frequency Score 91. 0 ± 19. 0 93. 2 ± 15. 1 0. 126 SAQ Quality of Life Score 80. 6 ± 21. 4 80. 5 ± 19. 9 0. 951 1. 0 ± 1. 4 0. 9 ± 1. 3 0. 497 Baseline Health Status Rose Dyspnea Score Safley D, Grantham JA, Jones P, and Spertus JA , ACC 2012
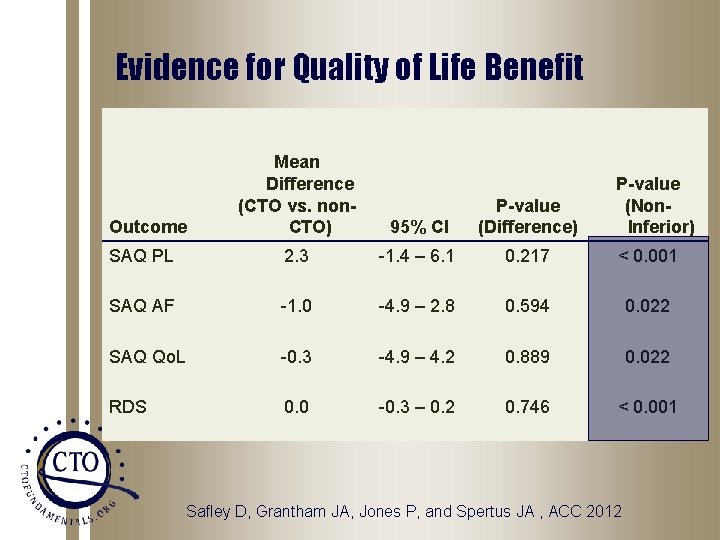
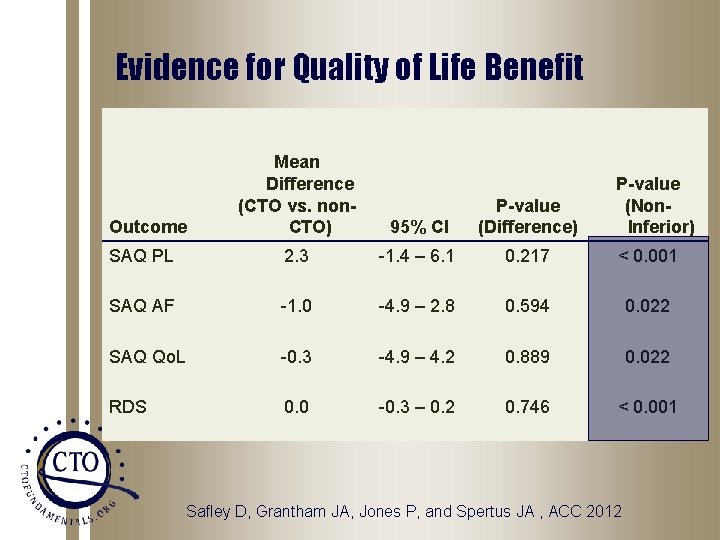
Evidence for Quality of Life Benefit Mean Difference (CTO vs. non. CTO) 95% CI P-value (Difference) SAQ PL 2. 3 -1. 4 – 6. 1 0. 217 < 0. 001 SAQ AF -1. 0 -4. 9 – 2. 8 0. 594 0. 022 SAQ Qo. L -0. 3 -4. 9 – 4. 2 0. 889 0. 022 RDS 0. 0 -0. 3 – 0. 2 0. 746 < 0. 001 Outcome P-value (Non. Inferior) Safley D, Grantham JA, Jones P, and Spertus JA , ACC 2012
AUC CTO • AUC supports CTO revascularization but…. • Violates principle of treating patient not the angiogram. • AUC for CTO should be same for non CTO disease

CTO-PCI Benefits • CTOs are commonly discovered • They are treated according to institutional and operator capabilities, not patient needs • The benefits include symptom relief and potentially survival advantage – Ischemic burden, double jeopardy, arrhythmogenesis

 Clinical rationale
Clinical rationale Developmentally appropriate practices definition
Developmentally appropriate practices definition Randuca
Randuca Rationale and problem statement
Rationale and problem statement Technical rationale
Technical rationale Background and rationale
Background and rationale Formuö
Formuö Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Personlig tidbok
Personlig tidbok A gastrica
A gastrica Vad är densitet
Vad är densitet Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Debattartikel struktur
Debattartikel struktur Autokratiskt ledarskap
Autokratiskt ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon