Indiana State Dept of Health Newborn Screening Refreshers
Indiana State Dept. of Health - Newborn Screening Refreshers, Best Practices, and Program Updates
Mission of ISDH Newborn Screening Program • Ensure that every newborn in Indiana receives state-mandated screening for all designated genetic conditions • Maintain a centralized program to ensure that infants who test positive for screened condition(s) receive appropriate diagnosis and treatment and that their parents receive genetic counseling • Promote genetic services, public awareness, and education concerning genetic conditions
Goals of Presentation • Increase education for facilities to ensure that babies born in Indiana are receiving care that aligns with ISDH Newborn Screening Program’s mission • Inform facilities of changes that have been made within NBS • Decrease the number of repeat newborn screens • Increase the turnaround time for newborn screening results • Decrease the number of babies lost to follow-up • Increase reporting and communication with facilities and Newborn Screening Program
REMINDERS AND BEST PRACTICES IN NEWBORN SCREENING
Why Do Newborn Screening? • Required by law (Indiana Code 16 -14 -17) • Early detection & treatment of newborn screening disorders – Lessens severity – Improves quality and quantity of life years • Lack of early detection & treatment can lead to: – Severe intellectual disability – Inadequate growth & development – Death

Birthing Facility’s Role Entity Role(s) in the Heelstick Process ISDH • • • Birthing Facility • • Ensure that mandated newborn screening (NBS) is properly conducted Ensure appropriate diagnosis management of affected newborns Designate & contract with NBS Lab Alert parents about NBS Conduct Newborn Screening If family refuses NBS based on religious reasons, have parent(s) sign religious waiver & submit religious waiver to ISDH Notify ISDH (through INSTEP monthly summary reports) if an infant has not received a screen

Newborn Screening Log • All birthing facilities and midwives should maintain a newborn screening log that documents the following info for all infants: – Specimen collection date – Specimen submission date – Date NBS results were received – Results of NBS
Introduction to Indiana’s Newborn Screening Process • Three parts: – Heelstick – Pulse Oximetry – Universal Newborn Hearing Screen
Heelstick Screening • Performed on a blood specimen taken from the heel of an infant shortly after birth • Used to screen for certain genetic conditions – Metabolic conditions – Endocrine conditions – Cystic fibrosis – Hemoglobinopathies
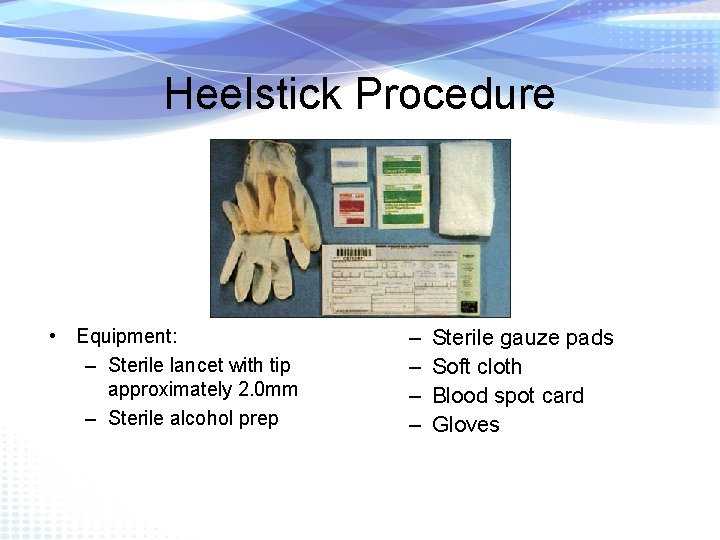
Heelstick Procedure • Equipment: – Sterile lancet with tip approximately 2. 0 mm – Sterile alcohol prep – – Sterile gauze pads Soft cloth Blood spot card Gloves
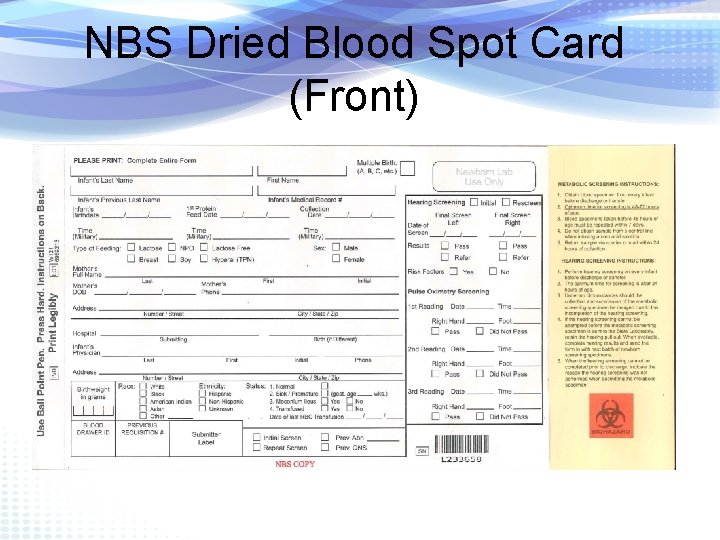
NBS Dried Blood Spot Card (Front)

NBS Dried Blood Spot Card (Back)
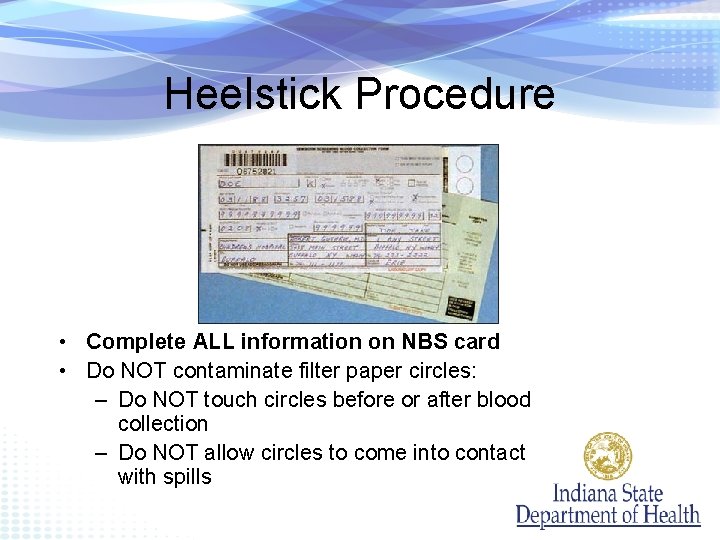
Heelstick Procedure • Complete ALL information on NBS card • Do NOT contaminate filter paper circles: – Do NOT touch circles before or after blood collection – Do NOT allow circles to come into contact with spills
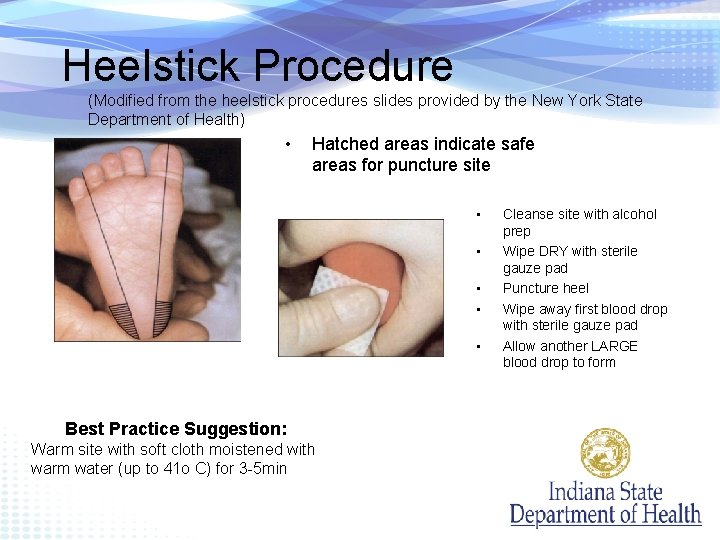
Heelstick Procedure (Modified from the heelstick procedures slides provided by the New York State Department of Health) • Hatched areas indicate safe areas for puncture site • • • Best Practice Suggestion: Warm site with soft cloth moistened with warm water (up to 41 o C) for 3 -5 min Cleanse site with alcohol prep Wipe DRY with sterile gauze pad Puncture heel Wipe away first blood drop with sterile gauze pad Allow another LARGE blood drop to form
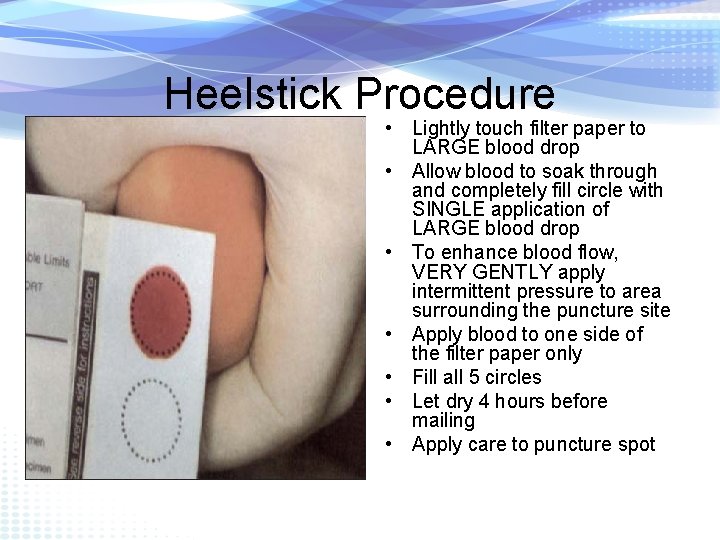
Heelstick Procedure • Lightly touch filter paper to LARGE blood drop • Allow blood to soak through and completely fill circle with SINGLE application of LARGE blood drop • To enhance blood flow, VERY GENTLY apply intermittent pressure to area surrounding the puncture site • Apply blood to one side of the filter paper only • Fill all 5 circles • Let dry 4 hours before mailing • Apply care to puncture spot
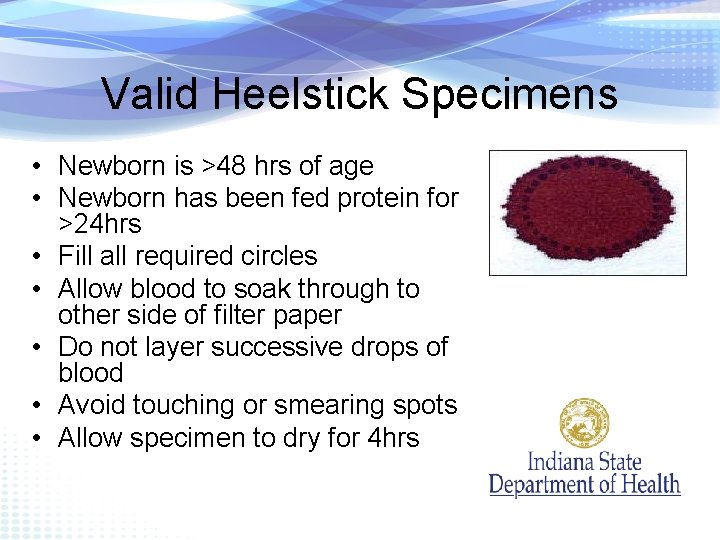
Valid Heelstick Specimens • Newborn is >48 hrs of age • Newborn has been fed protein for >24 hrs • Fill all required circles • Allow blood to soak through to other side of filter paper • Do not layer successive drops of blood • Avoid touching or smearing spots • Allow specimen to dry for 4 hrs
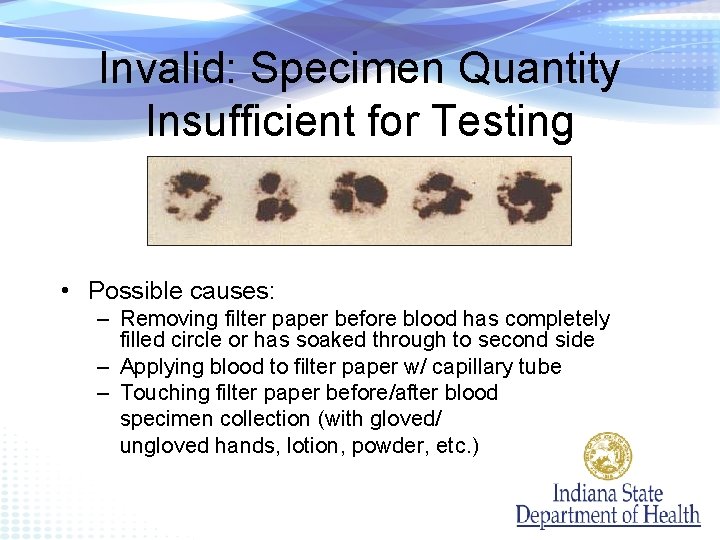
Invalid: Specimen Quantity Insufficient for Testing • Possible causes: – Removing filter paper before blood has completely filled circle or has soaked through to second side – Applying blood to filter paper w/ capillary tube – Touching filter paper before/after blood specimen collection (with gloved/ ungloved hands, lotion, powder, etc. )
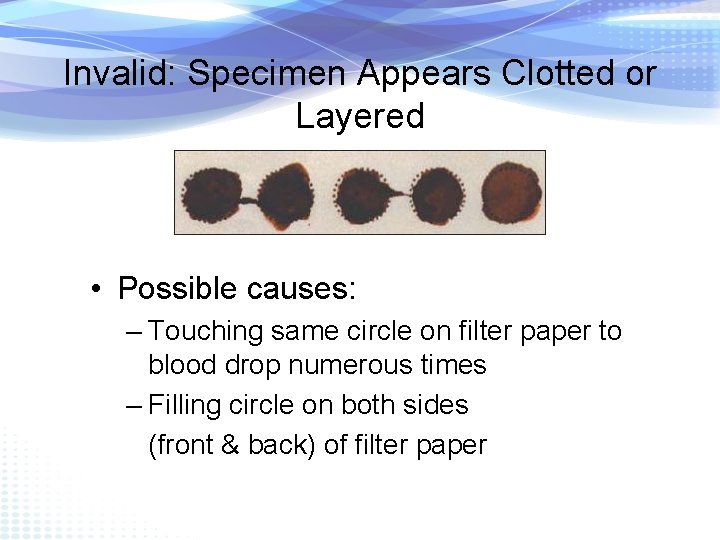
Invalid: Specimen Appears Clotted or Layered • Possible causes: – Touching same circle on filter paper to blood drop numerous times – Filling circle on both sides (front & back) of filter paper
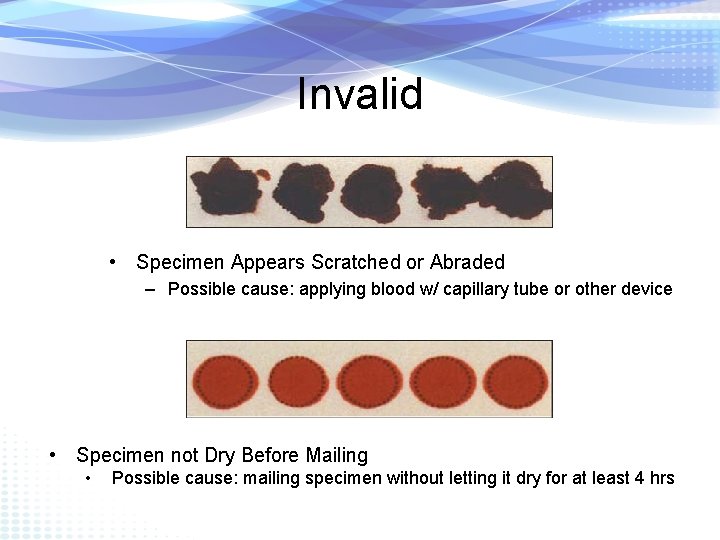
Invalid • Specimen Appears Scratched or Abraded – Possible cause: applying blood w/ capillary tube or other device • Specimen not Dry Before Mailing • Possible cause: mailing specimen without letting it dry for at least 4 hrs
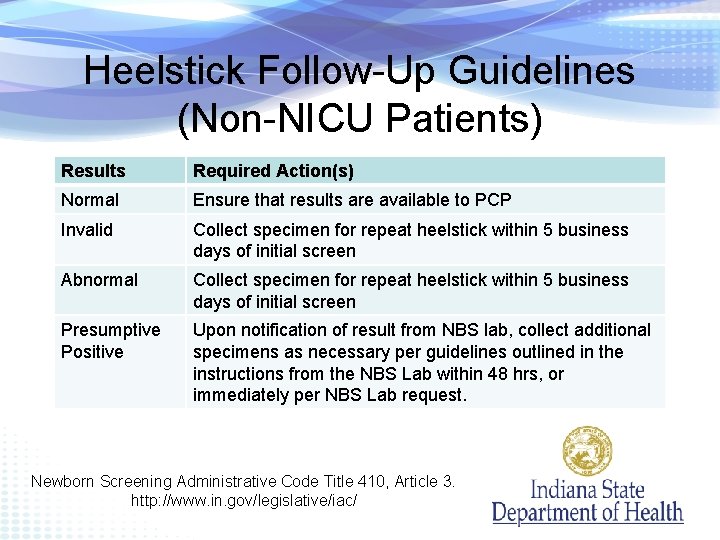
Heelstick Follow-Up Guidelines (Non-NICU Patients) Results Required Action(s) Normal Ensure that results are available to PCP Invalid Collect specimen for repeat heelstick within 5 business days of initial screen Abnormal Collect specimen for repeat heelstick within 5 business days of initial screen Presumptive Positive Upon notification of result from NBS lab, collect additional specimens as necessary per guidelines outlined in the instructions from the NBS Lab within 48 hrs, or immediately per NBS Lab request. Newborn Screening Administrative Code Title 410, Article 3. http: //www. in. gov/legislative/iac/
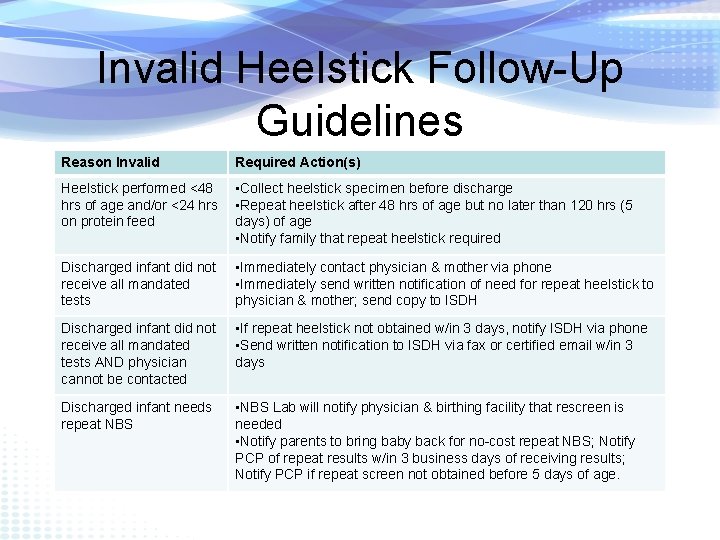
Invalid Heelstick Follow-Up Guidelines Reason Invalid Required Action(s) Heelstick performed <48 hrs of age and/or <24 hrs on protein feed • Collect heelstick specimen before discharge • Repeat heelstick after 48 hrs of age but no later than 120 hrs (5 days) of age • Notify family that repeat heelstick required Discharged infant did not receive all mandated tests • Immediately contact physician & mother via phone • Immediately send written notification of need for repeat heelstick to physician & mother; send copy to ISDH Discharged infant did not receive all mandated tests AND physician cannot be contacted • If repeat heelstick not obtained w/in 3 days, notify ISDH via phone • Send written notification to ISDH via fax or certified email w/in 3 days Discharged infant needs repeat NBS • NBS Lab will notify physician & birthing facility that rescreen is needed • Notify parents to bring baby back for no-cost repeat NBS; Notify PCP of repeat results w/in 3 business days of receiving results; Notify PCP if repeat screen not obtained before 5 days of age.
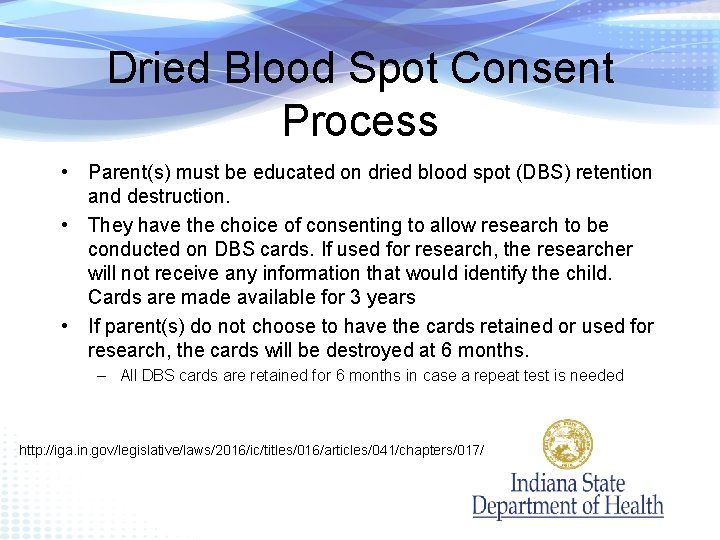
Dried Blood Spot Consent Process • Parent(s) must be educated on dried blood spot (DBS) retention and destruction. • They have the choice of consenting to allow research to be conducted on DBS cards. If used for research, the researcher will not receive any information that would identify the child. Cards are made available for 3 years • If parent(s) do not choose to have the cards retained or used for research, the cards will be destroyed at 6 months. – All DBS cards are retained for 6 months in case a repeat test is needed http: //iga. in. gov/legislative/laws/2016/ic/titles/016/articles/041/chapters/017/

Pulse Oximetry Screening for Critical Congenital Heart Disease (CCHD)
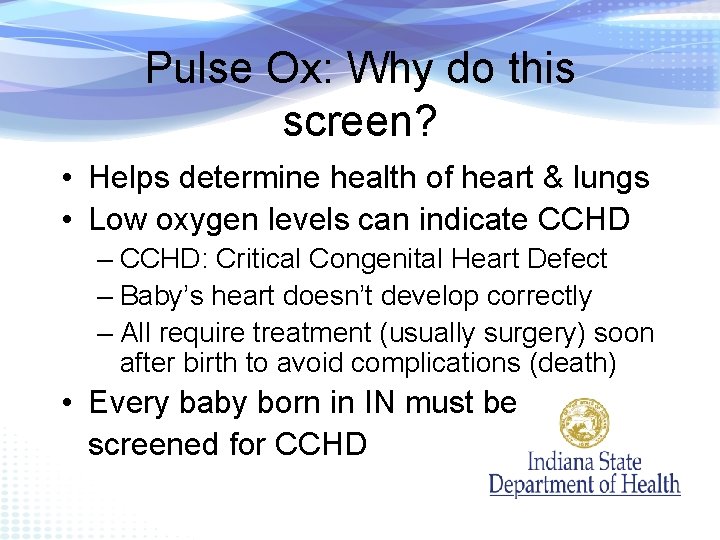
Pulse Ox: Why do this screen? • Helps determine health of heart & lungs • Low oxygen levels can indicate CCHD – CCHD: Critical Congenital Heart Defect – Baby’s heart doesn’t develop correctly – All require treatment (usually surgery) soon after birth to avoid complications (death) • Every baby born in IN must be screened for CCHD
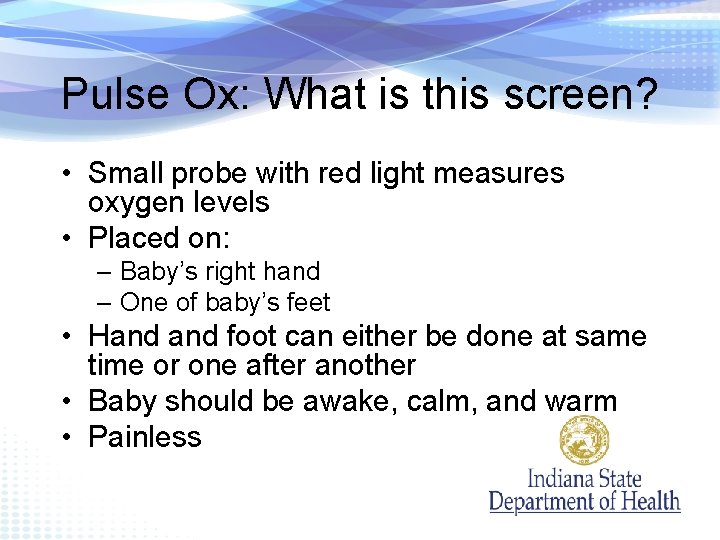
Pulse Ox: What is this screen? • Small probe with red light measures oxygen levels • Placed on: – Baby’s right hand – One of baby’s feet • Hand foot can either be done at same time or one after another • Baby should be awake, calm, and warm • Painless
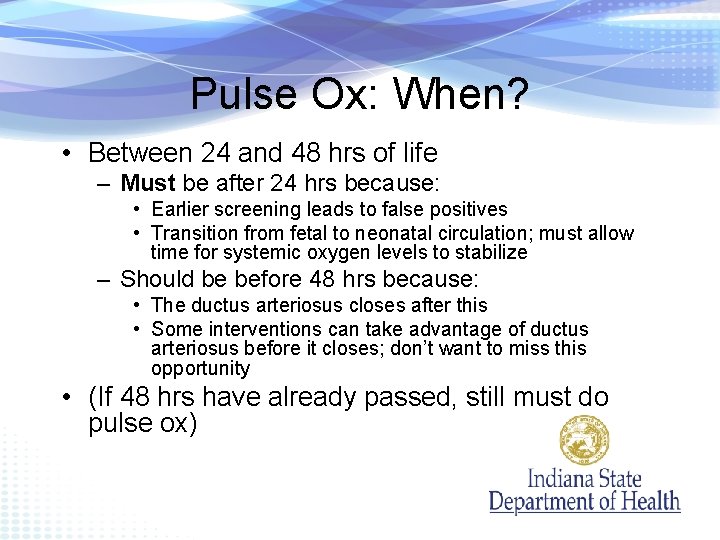
Pulse Ox: When? • Between 24 and 48 hrs of life – Must be after 24 hrs because: • Earlier screening leads to false positives • Transition from fetal to neonatal circulation; must allow time for systemic oxygen levels to stabilize – Should be before 48 hrs because: • The ductus arteriosus closes after this • Some interventions can take advantage of ductus arteriosus before it closes; don’t want to miss this opportunity • (If 48 hrs have already passed, still must do pulse ox)
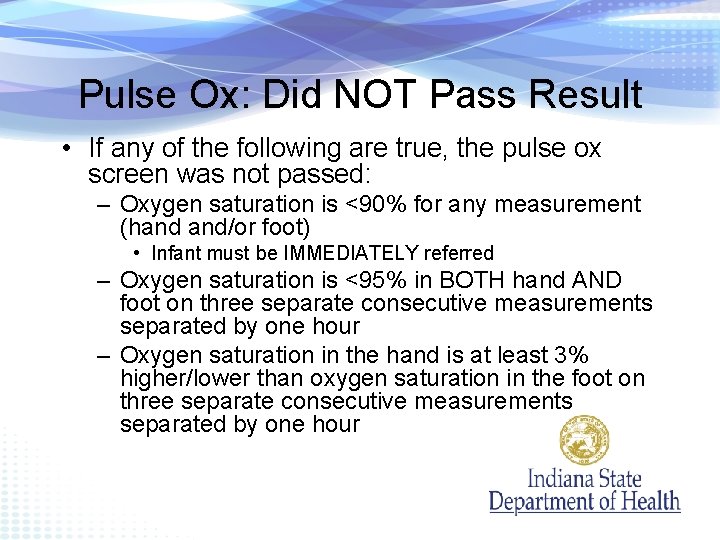
Pulse Ox: Did NOT Pass Result • If any of the following are true, the pulse ox screen was not passed: – Oxygen saturation is <90% for any measurement (hand and/or foot) • Infant must be IMMEDIATELY referred – Oxygen saturation is <95% in BOTH hand AND foot on three separate consecutive measurements separated by one hour – Oxygen saturation in the hand is at least 3% higher/lower than oxygen saturation in the foot on three separate consecutive measurements separated by one hour
Pulse Ox: Pass Result • Both must be true for a pass: – Oxygen saturations are 95% or higher in the hand or foot AND – Difference between oxygen saturation in the hand foot is 3% or less.
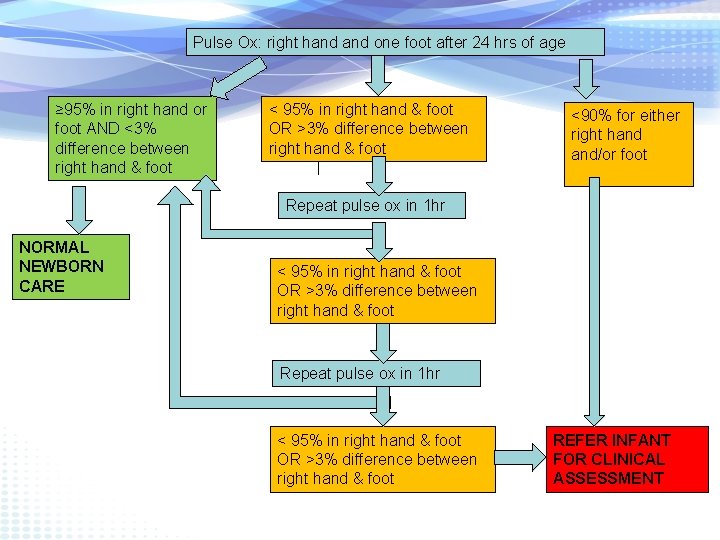
Pulse Ox: right hand one foot after 24 hrs of age ≥ 95% in right hand or foot AND <3% difference between right hand & foot < 95% in right hand & foot OR >3% difference between right hand & foot <90% for either right hand and/or foot Repeat pulse ox in 1 hr NORMAL NEWBORN CARE < 95% in right hand & foot OR >3% difference between right hand & foot Repeat pulse ox in 1 hr < 95% in right hand & foot OR >3% difference between right hand & foot REFER INFANT FOR CLINICAL ASSESSMENT
Failed Pulse Ox • Clinical assessment: – Medical evaluation – Echocardiogram – Referral to pediatric cardiology • Immediately if symptomatic • In timely manner if asymptomatic
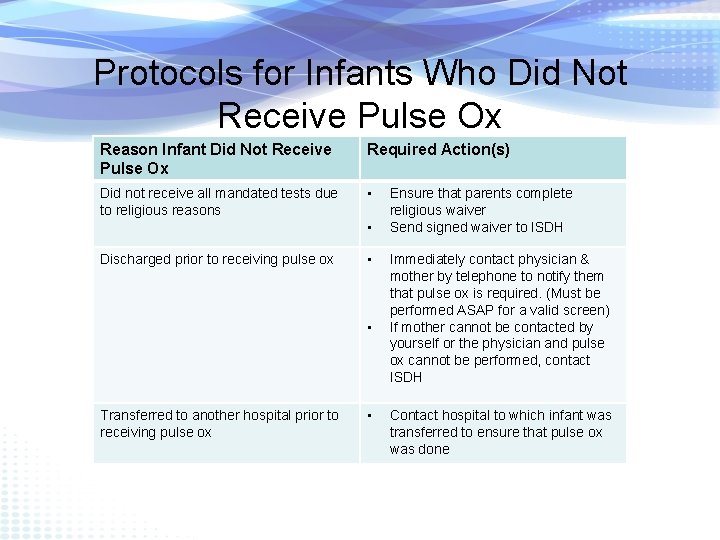
Protocols for Infants Who Did Not Receive Pulse Ox Reason Infant Did Not Receive Pulse Ox Required Action(s) Did not receive all mandated tests due to religious reasons • • Discharged prior to receiving pulse ox • • Transferred to another hospital prior to receiving pulse ox • Ensure that parents complete religious waiver Send signed waiver to ISDH Immediately contact physician & mother by telephone to notify them that pulse ox is required. (Must be performed ASAP for a valid screen) If mother cannot be contacted by yourself or the physician and pulse ox cannot be performed, contact ISDH Contact hospital to which infant was transferred to ensure that pulse ox was done
Early Hearing Detection and Intervention (EHDI) Universal Newborn Hearing Screening
Why Screen a Newborn’s Hearing? • Up to 3 babies in 1000 have permanent hearing loss. It is the most common congenital condition • Another 6 per 1000 babies acquire late-onset hearing loss during childhood • In Indiana, 134 babies were identified in 2015 – nearly 100 more that were born in other years were also identified in 2015
Why UNHS? • Before newborn hearing screening became routine, most children were not identified with hearing loss until the age of 2 or 3 • Today, many babies are identified by a few weeks of age when appropriate intervention programs can maximize their long term speech and language, cognitive and social skills
Why UNHS? • Average of identification: – 1980 s: 30 months – 2003: 6 months – 2007: 3 months • When does a child begin to learn language?

EHDI Goals • 1 -3 -6!! – Screen by 1 month – Confirmatory evaluation by 3 months (Identify!) – Early intervention by 6 months
EHDI Process • Babies are required by law to have a hearing screening (preferably before 1 month of age) – The only acceptable reason (by law) for a baby to not receive a hearing screening is a religious objection
Screening Procedure • Screening may occur twice (max) • Both ears screened each time • Both ears must pass on the same screen • If both ears do not pass either screen, they are referred immediately for a diagnostic hearing evaluation
Infant Hearing Screening • Otoacoustic Emissions (OAE) • Measures “echo” from the inner ear • Tests for sensory hearing loss
Infant Hearing Screening • Automated Auditory Brainstem Response (AABR) • Measures brainwaves associated with hearing • Screens for all types of hearing loss
EHDI Process • Hospitals/birthing centers are required to report UNHS data to ISDH/EHDI: – Number of live births – Babies that did not pass UNHS – Babies that did not receive UNHS – Babies that passed but are at risk
EHDI Best Practices • The newborn or infant's hearing should be screened after six (6) hours of age and prior to discharge as follows: – (1) Preterm newborns or infants (born prior to thirty-five (35) weeks gestational age) who stay in the nursery greater than five (5) days should have hearing screening when the newborn or infant is medically stable, but prior to discharge.
EHDI Best Practices • (2) Newborns or infants who reside for greater than five (5) days in the neonatal intensive care unit (NICU), especially those who have complicated birth factors, are considered to be at significantly greater risk for types of neural hearing loss, such as auditory neuropathy/dysynchrony. These newborns or infants should receive hearing screening or diagnostic testing, or both, as recommended by the department.
EHDI Best Practices • (3)When possible, inpatient diagnostic testing shall be made available to longstay newborns or infants
Reporting to ISDH 1. Mail NBS card to laboratory 2. Monthly Summary Report a) Paper copy or Online (INSTEP): i. Indiana Newborn Screening Tracking & Education Program (INSTEP) b) To register for INSTEP, please contact: i. ISDH Genomics and Newborn Screening i. ISDHNBS@isdh. in. gov ii. P: (888) 815 -0006 iii. F: (317) 234 -2995
Mail NBS Card to IU Laboratory • • • Create account with IU laboratory – Barb Lesko Send completed blood spot card to IU Newborn Screening Lab within 24 hours of collection. Address: Newborn Screening Laboratory PO Box 770 Indianapolis, IN 46206 Phone: 1(800) 245 -9137 – Request more supplies Barb Lesko: (317) 491 – 6682 – Questions or concerns – Sending NBS cards through neighboring hospitals/clinics – Establishing account
Contact Information Newborn Screening EHDI Genomics and Newborn Screening Early Hearing Detection & Intervention (EHDI) Program ISDHNBS@isdh. in. gov P: (888) 815 -0006 F: (317) 234 -2995 Alyssa Rex, Follow-up Coordinator ARex@isdh. IN. gov P: 855. 875. 5193 F: 317. 925. 2888 USPS: Indiana State Dept. of Health – Maternal and Child Health Attn: Newborn Screening 2 N. Meridian St. Indianapolis, IN 46204
Requesting Lab Results • Fax the lab on your letterhead and include: – Baby’s name – Baby’s DOB – Mom’s name – Birth Facility • Fax: (317) 491 -6679
Opting Out • Every person has the right to opt out of newborn screening due to religious beliefs – Complete Religious Waiver • Mail or Fax: Indiana State Department of Health Attn: Genomics and Newborn Screening 2 North Meridian Indianapolis, IN 46204 Fax: (317) 234 – 2995 - Update INSTEP exception
NBS UPDATES
New. STEPs 360 • Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC) – Recommended Universal Screening Panel (RUSP) – Standardized best practices in NBS • Objectives: – Specimen received by lab 24 hours after collection – Presumptive Positive results reported within 5 -7 days after birth – All results within 7 days after birth
Weekend Courier • Spring 2017, the IU NBS laboratory will be adding a Sunday courier pickup to increase the turnaround time for NBS specimens • In addition, the laboratory will be extending the laboratory hours from 5 days/week to 6 days/week • These changes will result in faster NBS results and quicker care for newborns born with a genetic condition
Quality Indicators and Training • Best practices on your end that can help the NBS lab meet the timeliness expectations: – Allow blood spot to dry 4 hours before putting in envelop • Coordinate heelstick time with courier pick-up time • Quality checks: – NBS Lab will be tracking time of receipt (blood spot card) – NBS Lab tracking invalid blood spot results – Show facility performance monthly (webinars, newsletters, ISDH website) • Training: – Monthly webinars – ISDH NBS team able to offer focused training as needed or as indicated by quality checks
Q&A • Any questions? !?
- Slides: 54