Independent Living Skills Inventory ILSI and the Nurses
- Slides: 1
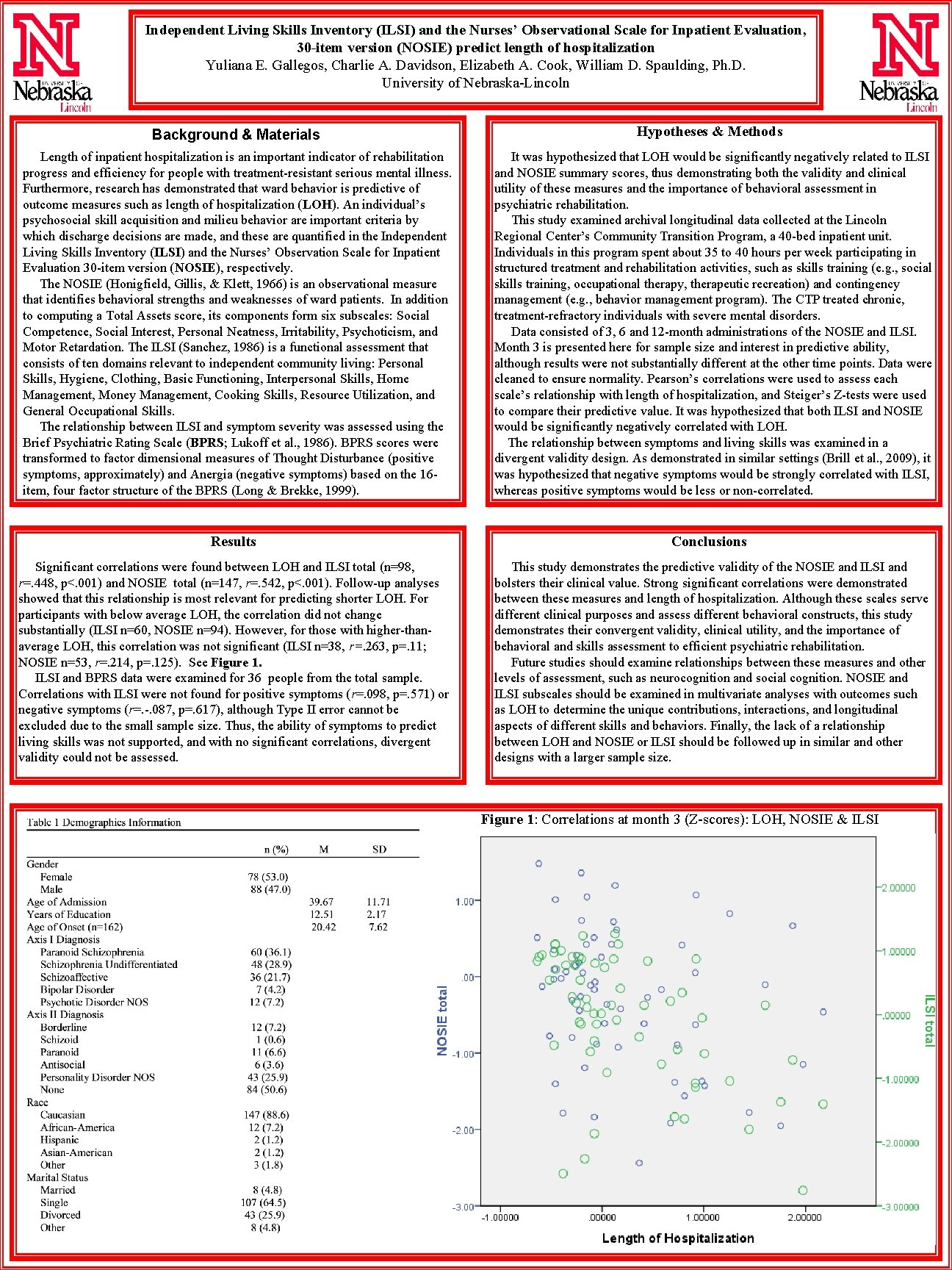
Independent Living Skills Inventory (ILSI) and the Nurses’ Observational Scale for Inpatient Evaluation, 30 -item version (NOSIE) predict length of hospitalization Yuliana E. Gallegos, Charlie A. Davidson, Elizabeth A. Cook, William D. Spaulding, Ph. D. University of Nebraska-Lincoln Background & Materials Hypotheses & Methods Length of inpatient hospitalization is an important indicator of rehabilitation progress and efficiency for people with treatment-resistant serious mental illness. Furthermore, research has demonstrated that ward behavior is predictive of outcome measures such as length of hospitalization (LOH). An individual’s psychosocial skill acquisition and milieu behavior are important criteria by which discharge decisions are made, and these are quantified in the Independent Living Skills Inventory (ILSI) and the Nurses’ Observation Scale for Inpatient Evaluation 30 -item version (NOSIE), respectively. The NOSIE (Honigfield, Gillis, & Klett, 1966) is an observational measure that identifies behavioral strengths and weaknesses of ward patients. In addition to computing a Total Assets score, its components form six subscales: Social Competence, Social Interest, Personal Neatness, Irritability, Psychoticism, and Motor Retardation. The ILSI (Sanchez, 1986) is a functional assessment that consists of ten domains relevant to independent community living: Personal Skills, Hygiene, Clothing, Basic Functioning, Interpersonal Skills, Home Management, Money Management, Cooking Skills, Resource Utilization, and General Occupational Skills. The relationship between ILSI and symptom severity was assessed using the Brief Psychiatric Rating Scale (BPRS; Lukoff et al. , 1986). BPRS scores were transformed to factor dimensional measures of Thought Disturbance (positive symptoms, approximately) and Anergia (negative symptoms) based on the 16 item, four factor structure of the BPRS (Long & Brekke, 1999). It was hypothesized that LOH would be significantly negatively related to ILSI and NOSIE summary scores, thus demonstrating both the validity and clinical utility of these measures and the importance of behavioral assessment in psychiatric rehabilitation. This study examined archival longitudinal data collected at the Lincoln Regional Center’s Community Transition Program, a 40 -bed inpatient unit. Individuals in this program spent about 35 to 40 hours per week participating in structured treatment and rehabilitation activities, such as skills training (e. g. , social skills training, occupational therapy, therapeutic recreation) and contingency management (e. g. , behavior management program). The CTP treated chronic, treatment-refractory individuals with severe mental disorders. Data consisted of 3, 6 and 12 -month administrations of the NOSIE and ILSI. Month 3 is presented here for sample size and interest in predictive ability, although results were not substantially different at the other time points. Data were cleaned to ensure normality. Pearson’s correlations were used to assess each scale’s relationship with length of hospitalization, and Steiger’s Z-tests were used to compare their predictive value. It was hypothesized that both ILSI and NOSIE would be significantly negatively correlated with LOH. The relationship between symptoms and living skills was examined in a divergent validity design. As demonstrated in similar settings (Brill et al. , 2009), it was hypothesized that negative symptoms would be strongly correlated with ILSI, whereas positive symptoms would be less or non-correlated. Results Conclusions Significant correlations were found between LOH and ILSI total (n=98, r=. 448, p<. 001) and NOSIE total (n=147, r=. 542, p<. 001). Follow-up analyses showed that this relationship is most relevant for predicting shorter LOH. For participants with below average LOH, the correlation did not change substantially (ILSI n=60, NOSIE n=94). However, for those with higher-thanaverage LOH, this correlation was not significant (ILSI n=38, r=. 263, p=. 11; NOSIE n=53, r=. 214, p=. 125). See Figure 1. ILSI and BPRS data were examined for 36 people from the total sample. Correlations with ILSI were not found for positive symptoms (r=. 098, p=. 571) or negative symptoms (r=. -. 087, p=. 617), although Type II error cannot be excluded due to the small sample size. Thus, the ability of symptoms to predict living skills was not supported, and with no significant correlations, divergent validity could not be assessed. This study demonstrates the predictive validity of the NOSIE and ILSI and bolsters their clinical value. Strong significant correlations were demonstrated between these measures and length of hospitalization. Although these scales serve different clinical purposes and assess different behavioral constructs, this study demonstrates their convergent validity, clinical utility, and the importance of behavioral and skills assessment to efficient psychiatric rehabilitation. Future studies should examine relationships between these measures and other levels of assessment, such as neurocognition and social cognition. NOSIE and ILSI subscales should be examined in multivariate analyses with outcomes such as LOH to determine the unique contributions, interactions, and longitudinal aspects of different skills and behaviors. Finally, the lack of a relationship between LOH and NOSIE or ILSI should be followed up in similar and other designs with a larger sample size. Figure 1: Correlations at month 3 (Z-scores): LOH, NOSIE & ILSI

