Incorporating Shared Decision Making into Office Visits Ann













- Slides: 31
Incorporating Shared Decision Making into Office Visits Ann Tseng, MD Daisuke Yamashita, MD Eric Wiser, MD Marcel Tam, MD Emily Barclay, MS

Disclosures • We have nothing to disclose!
CPCI – the impetus for shared decision making • 4 yr (2012 -2016) multipayer initiative designed to strengthen primary care. • CMS collaborated with State health plans and commercial payers • 7 regions: Arkansas, Colorado, New Jersey, Oregon, Cincinnati-Dayton region, Greater Tulsa area, Upstate NY
CPCI Five Functions • Risk-stratified care management • Access and Continuity • Planned Care of Chronic Conditions and Preventative Care • Patient and Caregiver Engagement • Coordination or Care across the Medical Neighborhood
Milestone VII • Identify a priority condition, decision, or test that would benefit from shared decision making and the use of a decision aid • Make a decision aid available to appropriate patients • Generate a metric for the proportion of patients who received the decision aid for this priority area
Shared Decision Making (SDM) • Fully informs patients about risks and benefits or various treatment options • Engages patient in the decision making process • Facilitates the incorporation of patient preferences and values into the medical plan
Potential of SDM • Patients who are more empowered to manage their health and treatment • Reductions in unwarranted variation of care • Increased awareness among patients regarding potential adverse consequences from a medical decision or treatment option

What is a Decision Aid? • Interventions designed to support patients' decision – making the choice explicit – providing information about treatment or screening options and their associated outcomes, compared to usual care and/or alternative intervention
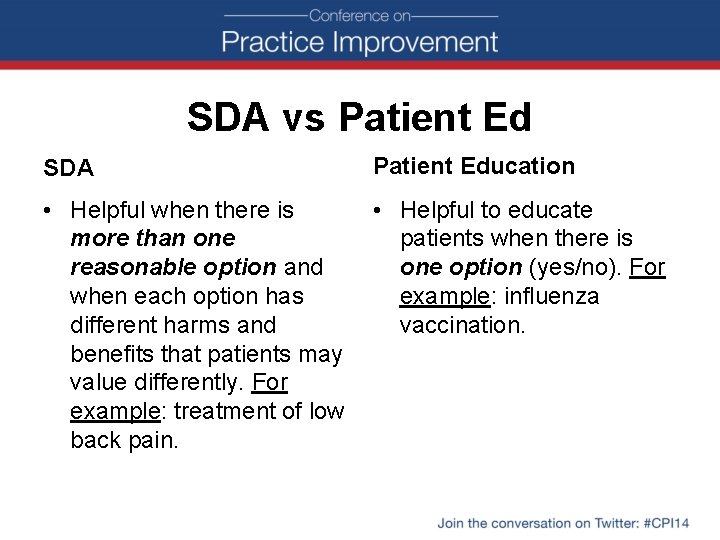
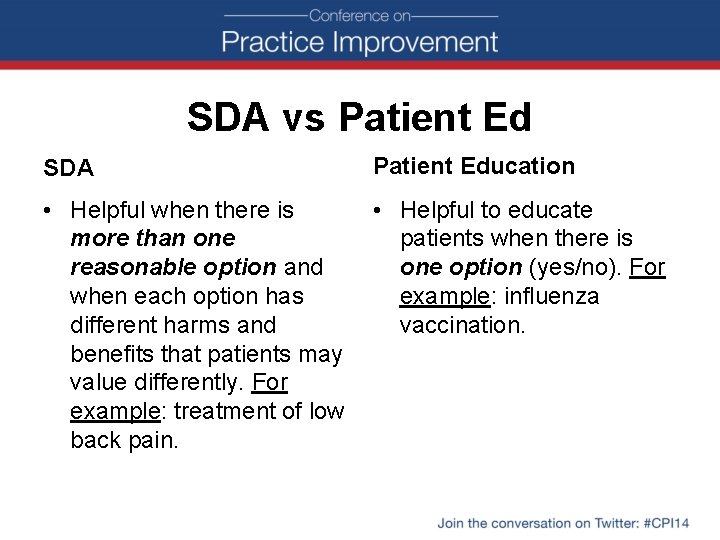
SDA vs Patient Ed SDA Patient Education • Helpful when there is more than one reasonable option and when each option has different harms and benefits that patients may value differently. For example: treatment of low back pain. • Helpful to educate patients when there is one option (yes/no). For example: influenza vaccination.
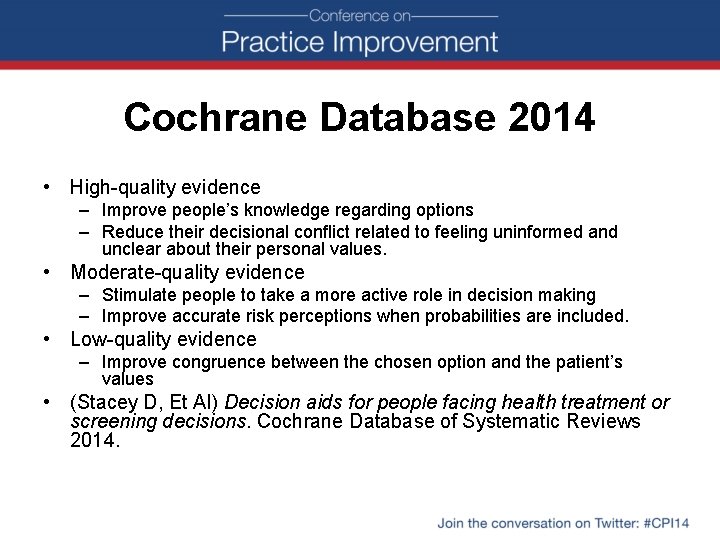
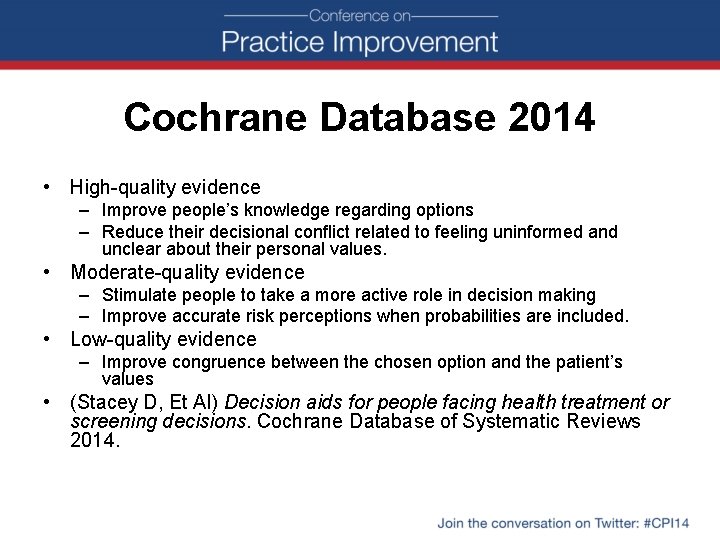
Cochrane Database 2014 • High-quality evidence – Improve people’s knowledge regarding options – Reduce their decisional conflict related to feeling uninformed and unclear about their personal values. • Moderate-quality evidence – Stimulate people to take a more active role in decision making – Improve accurate risk perceptions when probabilities are included. • Low-quality evidence – Improve congruence between the chosen option and the patient’s values • (Stacey D, Et Al) Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2014.

Evidence (Cont. ) • Reduced proportions of people who remained undecided post-intervention • Patients were either more satisfied with patientprovider communication or had no impact • Secondary Outcomes: – reduced the number of people of choosing major elective invasive surgery in favor of more conservative options – reduced the number of people choosing menopausal hormone therapy
The problem… • Office Visits are 15 -20 min, but SDM tools are LONG and BULKY! • Copyrights on some SDM products

So we made our own SDM tool…

Development of SDM Tool • Collaboration with three clinics in two departments to create tool. • Tool validated and edited through three different patient advisory councils. • Ongoing edits and updates made based on clinician and patient feedback.

Walking you through our attached tool…
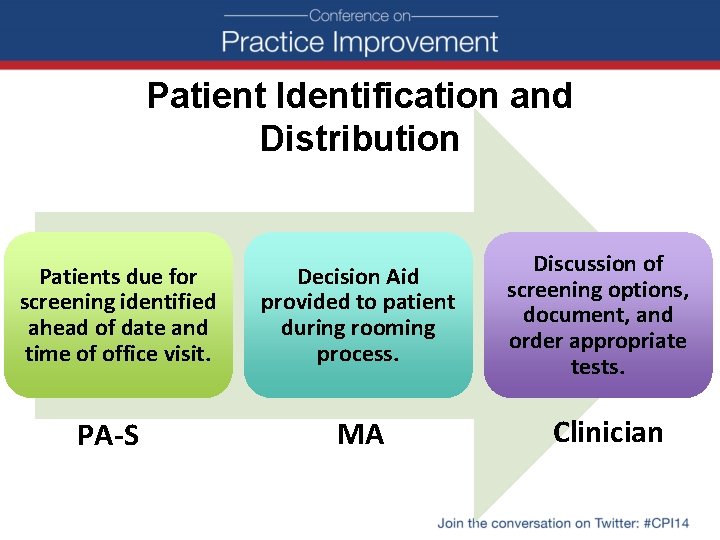
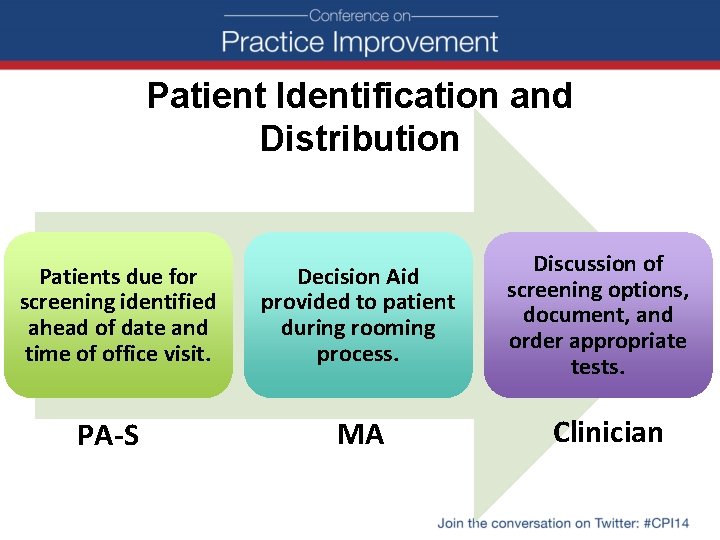
Patient Identification and Distribution Patients due for screening identified ahead of date and time of office visit. PA-S Decision Aid provided to patient during rooming process. MA Discussion of screening options, document, and order appropriate tests. Clinician

Continuous Follow-Up & Feedback Engaging leadership Quarterly reports to measure rates of screening and tool use Champions at MA, clinician, PA-S level Feedback continually provided by clinicians and patients using tool.

Validating our SDM tool
International Patient Decision Aid Standards (IPDAS) • Most well-known group for validating decision aids • International – led by researchers in UK, Canada • The original publication validating their work: BMJ. 2006 Aug 26; 333(7565): 417. Epub 2006 Aug 14. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process.
IPDAS Checklist (Abbreviated) • 30 criteria (median importance of “ 9” on a scale of 1 -9) in the sections of: Content Development Process Effectiveness • Multistakeholder group voted on criteria • Full 64 point checklist also exists (original)
IPDAS checklist performance Meets (on the abbreviated checklist): • 13/19 content criteria • 6/9 development process criteria – (includes field testing from patients, other clinicians) • 2/2 effectiveness criteria

How we could improve our tool (from IPDAS checklist) • Including info about event rates if no screening • Report “readability levels” • Report any affiliations by the authors
DATA!

Data Interpretation • 3 sets of reports thus far: April 2014 (encompassing last 3 years) June 2014 (encompassing last 3 years) October 2014 (encompassing last 3 years)

Clinic Wide Data Month Shared Decision Colon Cancer % Screening % April 2014 5. 50% 55. 42% July 2014 8% 59. 62% October 2014 11% 60%
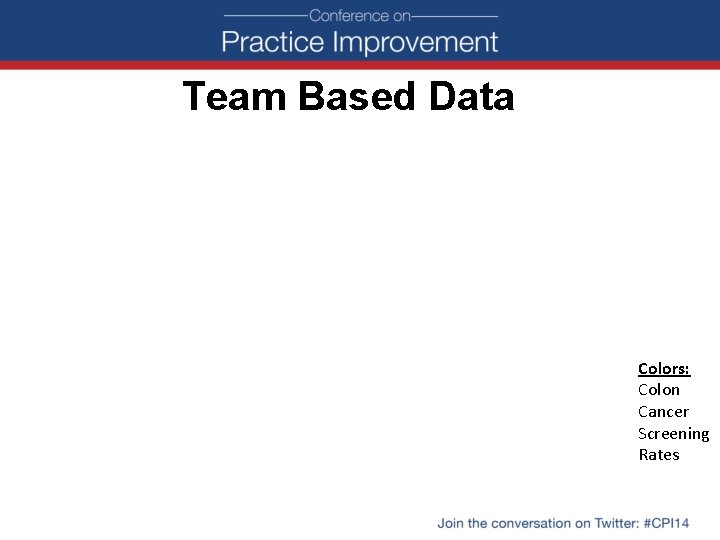
Team Based Data Colors: Colon Cancer Screening Rates
Limitations to Data • We don’t distribute tool if patient is UTD • Captures data based on dot phrases • Encompasses pre-intervention data (all months that have data points)

Successes of incorporating SDM into office visits • Improved colorectal cancer screening rates. • Increased patient satisfaction. • Ability to get buy-in from leadership in three different clinics. • Ongoing collaboration on a number of screening and health maintenance efforts as a result of shared decision aid development process.

Challenges of SDM • Sustainability of shared decision making workflow. • Change fatigue. • Inability to track who has received a shared decision aid in our Epic EHR. • Lack of time during office visits to adequately discuss options using aid during standard visit.
How Have We Combatted These Challenges? • Clinic quality improvement champions. • Constant socialization of shared decision making processes, tools, and outcomes. • Standardization of tool and workflow. • Currently only using tool during extended office visits such as annual exams. • Patient involvement in development of workflow and tools.
Where does SDM go from here? • We can give the tool out, but what happens with it? • Improving our colorectal tool • 2 nd tool for breast Cancer and 3 rd in 2015 - CPCI requirement • Group visits for future tools (? )