In the Name of God Pathology of Bone
In the Name of God Pathology of Bone Lesions Hana Saffar, MD, APCP Canter Institute, IKHC, TUMS NOV 2019
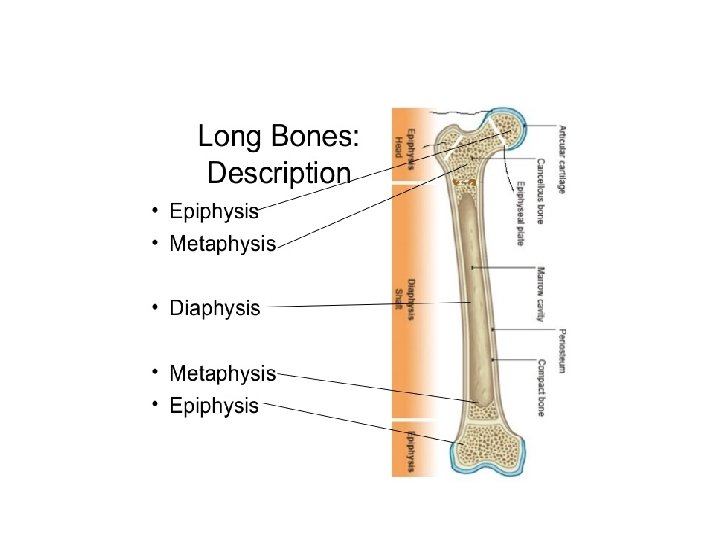
Topographic features of bone
Based on gross appearance bones are divided to: • Flat: trunk, craniofacial such as skull, scapula, clavicle, pelvic, sternum • Tubular: (long and short): bones of extremities and rib • Epiphysioid bones: carpal and tarsal and patella bones
Based on overall organization of type I collagen bones are divided to: • Woven: collagen fibers are haphazardly organized and form irregular network • Lamellar bone : collage fibrillary network has an orderly parallel organization
Extracellular matrix Perform mechanical function of skeleton • Collagen • Proteoglycans • Minerals
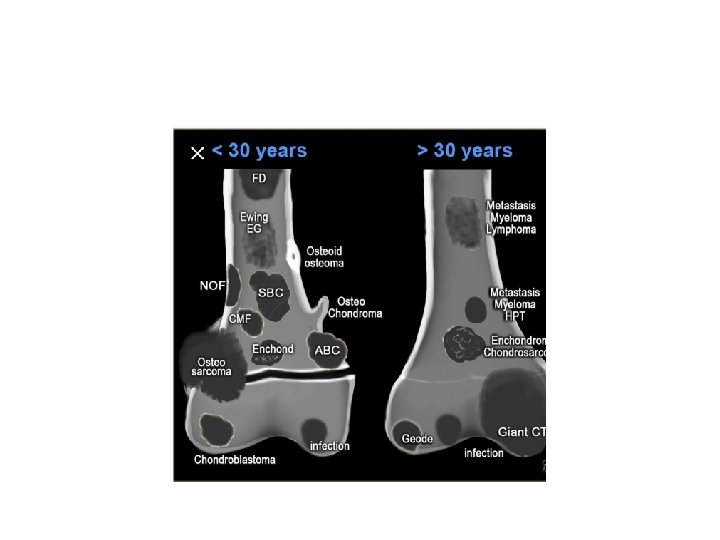
Location of lesion Location, location: access to imaging is essential for musculoskeletal pathologists
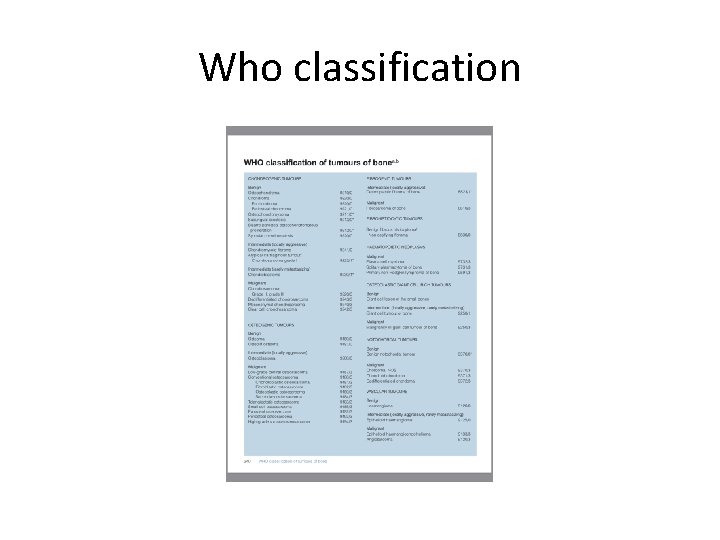
Who classification
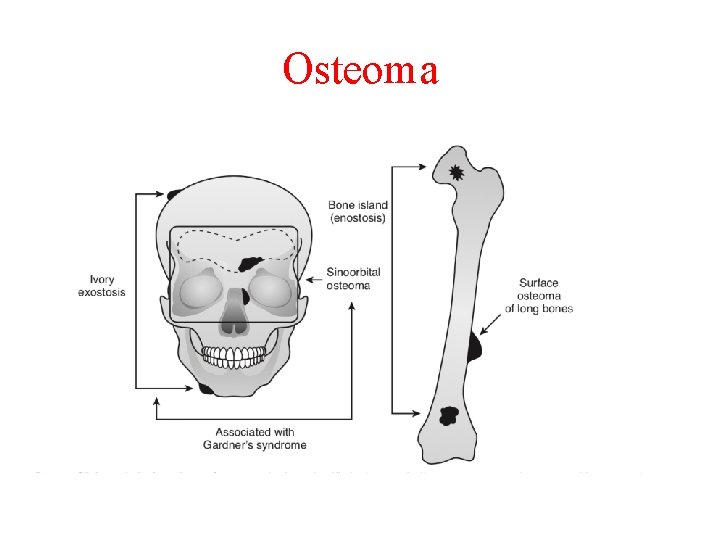
Osteoma and bone island They can be divided into: • Calvarial and mandibular ivory exostosis • Osteoma of paranasal sinuses • Enostoses or bone island • Surface osteoma of long bones
Osteoma • Some authors consider these lesions to be hamartomatous or dysplastic • But for those affecting orbit and facial bones and paranasal sinuses benign bone forming nature is considered
Osteoma • The etiology of sporadic cases is unknown • Multiple osteoma could be seen in setting of Gardner syndrome • Multiple enostosis are seen in setting of osteopoikilosis, however most cases are hamartomatous
Osteoma
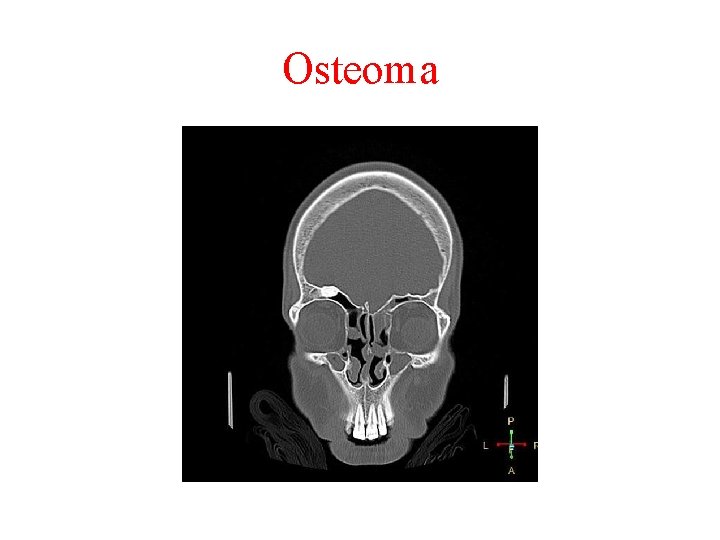
Osteoma location: • Most of the times in bones with membranous ossification like calvarial, facial and jaw bones • Intramedullary lesions originate in epi and metaphyseal of long bones, pelvic and vertebral bones
Osteoma Clinic and radiology: • Usually asymptomatic, sometimes local swelling • Osteomas are usually homogenously ossified and well limited
Osteoma Gross findings : • Well-circumscribed with broad attachment to underlying bone • Most osteomas are smaller than 2 cm
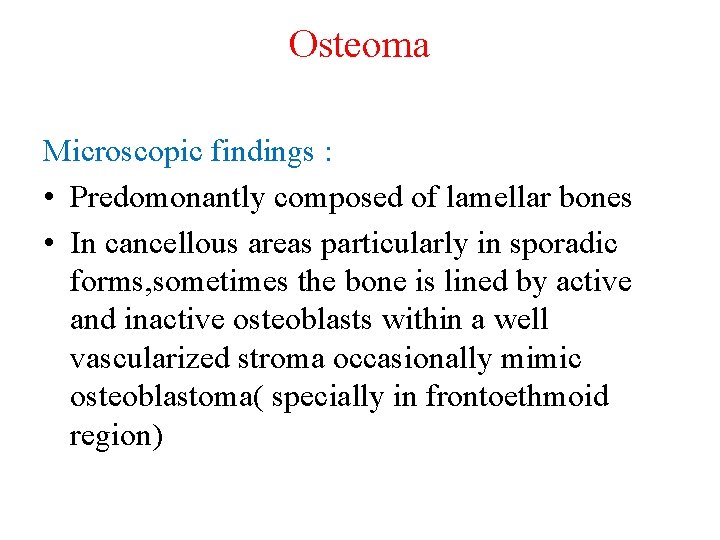
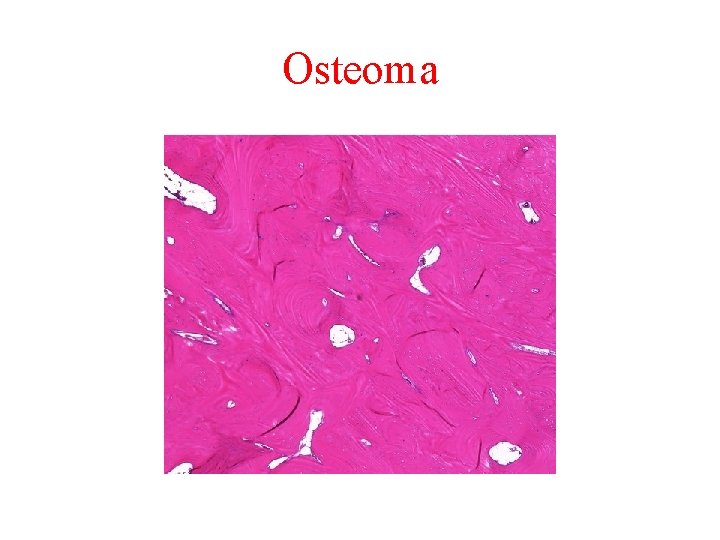
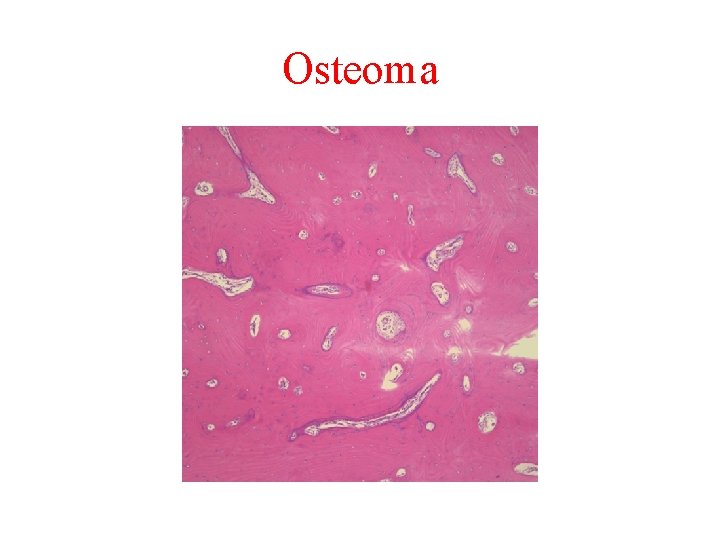
Osteoma Microscopic findings : • Predomonantly composed of lamellar bones • In cancellous areas particularly in sporadic forms, sometimes the bone is lined by active and inactive osteoblasts within a well vascularized stroma occasionally mimic osteoblastoma( specially in frontoethmoid region)
Osteoma Behaviour : • Asymptomatic cases generally do not require treatment
Osteoma
Osteoma
Osteoma
Osteoid osteoma Definition: benign tumor which is consists of a well-demarcated osteoblastic mass called a Nidus that is surrounded by a distinct zone of reactive bone sclerosis. • The zone of sclerosis is not an integral part of the tumor and represents a secondary reversible change that gradually disappears after removal of nidus.
Osteoid osteoma • This zone should be specifically excluded in taking measurement of these lesions. • Size of nidus is usually less than 1 cm.
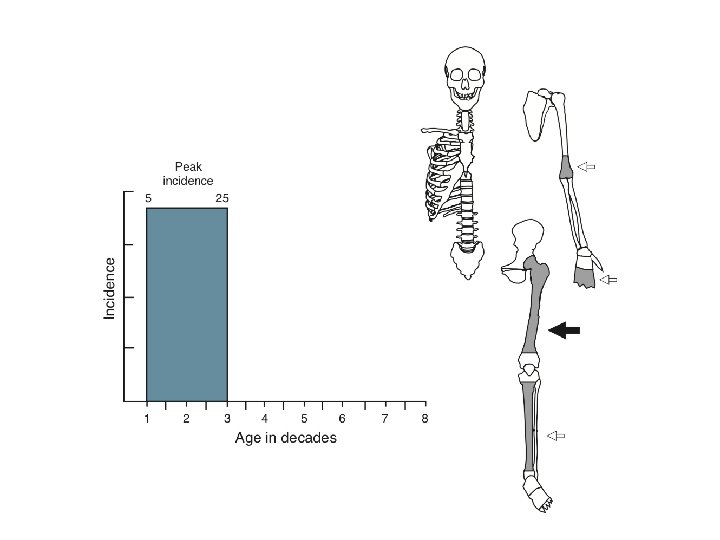
Osteoid osteoma Incidence: 10 -20% of all benign bone tumors • Usually occur in teenagers and young adults ( pick incidence is in second decade of life) • Male/ Female ratio: 2/1
Osteoid osteoma Clinical symptoms: • Pain that is worse at night and is revealed by Aspirin and NSAIDS (in 80%of cases) • Arthritis when the lesion is close to joints • Painful swelling of adjacent soft tissue when the lesion is superficial • In vertebral lesions clinically may mimic neuropathy • In small bones of hand feet may mimic osteomyelitis
Osteoid osteoma Cause of pain: • Presence of nerves within nidus • Large amounts of PGE 2 and prostacyclin released from nidus (more accepted)
Osteoid osteoma • Conventional radiolgraphic feature reveals a well-demarcated lytic lesion (nidus) surrounded by a distinct zone of sclerosis
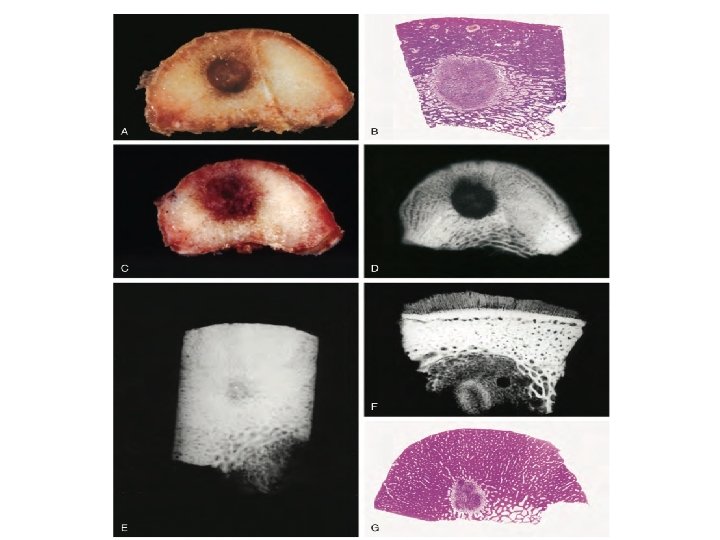
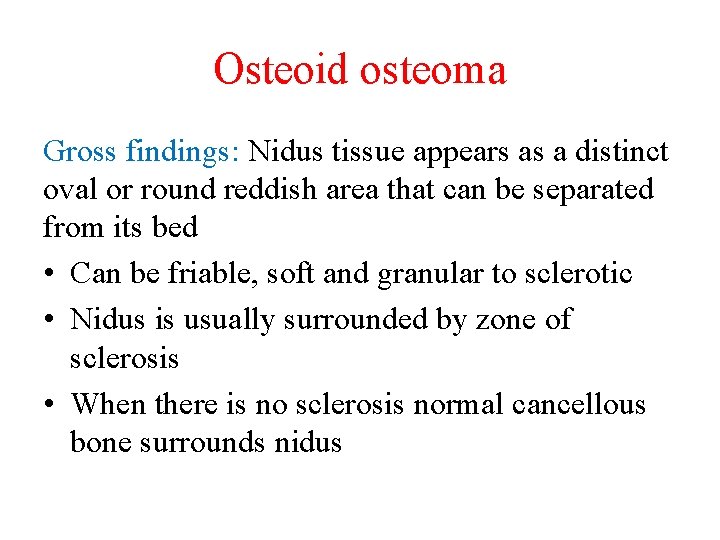
Osteoid osteoma Gross findings: Nidus tissue appears as a distinct oval or round reddish area that can be separated from its bed • Can be friable, soft and granular to sclerotic • Nidus is usually surrounded by zone of sclerosis • When there is no sclerosis normal cancellous bone surrounds nidus
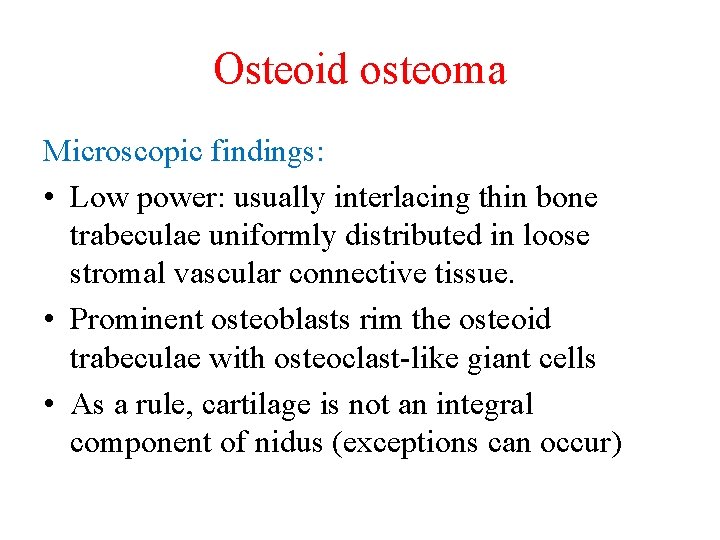
Osteoid osteoma Microscopic findings: • Low power: usually interlacing thin bone trabeculae uniformly distributed in loose stromal vascular connective tissue. • Prominent osteoblasts rim the osteoid trabeculae with osteoclast-like giant cells • As a rule, cartilage is not an integral component of nidus (exceptions can occur)
Osteoid osteoma • Genetics: only 3 cases have shown clonal chromosome abberations • IHC: Nuclear staining for RUNX 2 and OSTERX
Osteoid osteoma Differential diagnosis: • Acute and chronic osteomyelitis • Bone abscess • Intracortical hemangioma • Bone island • Stress fracture • Ewing sarcoma • Intracortical osteosarcoma
• Reactive bone formation can be distinguished by its parallel or radially oriented bone trabeculae with gradual maturation to lamellar bone
Osteoid osteoma Treatment and behavior: • Sometimes spontaneously regress • Removal of nidus and surrounding bone by en bloc resection Other modalities include curettage and bone graft, recurrence is uncommon Its important to consider whether the lesion was missed on surgery or the pathologist failed to identify it
Benign ostaoblastoma Definition: a benign bone-forming neoplasm, greater than 2 cm which is identical to osteoblastoma and produces woven spicules bordered by prominent osteoblasts
Benign ostaoblastoma Main differences with osteoid osteoma: • Higher growth potential (more than 2 cm) • Lacks distinct nocturnal pain • Secondary peripheral sclerosis may be minimal or absent • There are cases with composite features (1. 5 cm size for nidus would be helpful)
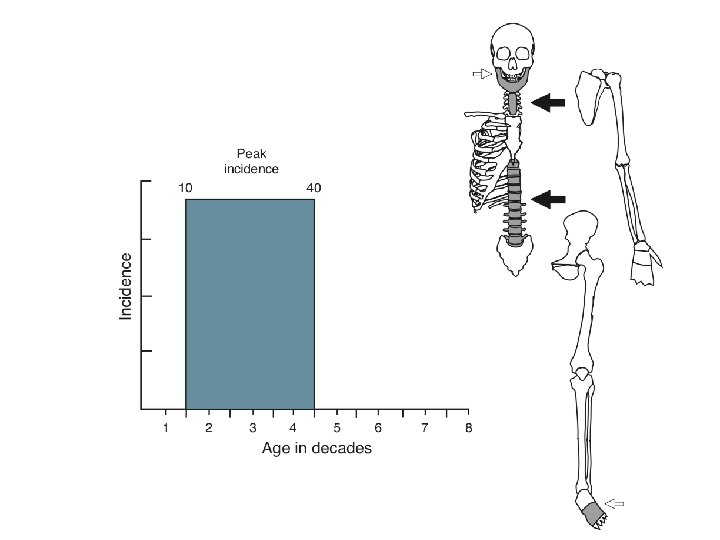
Benign ostaoblastoma Incidence: less than 1% of all primary bone tumors • Pick incidence is in the second and third decade of life • Male/ Female: 2/1
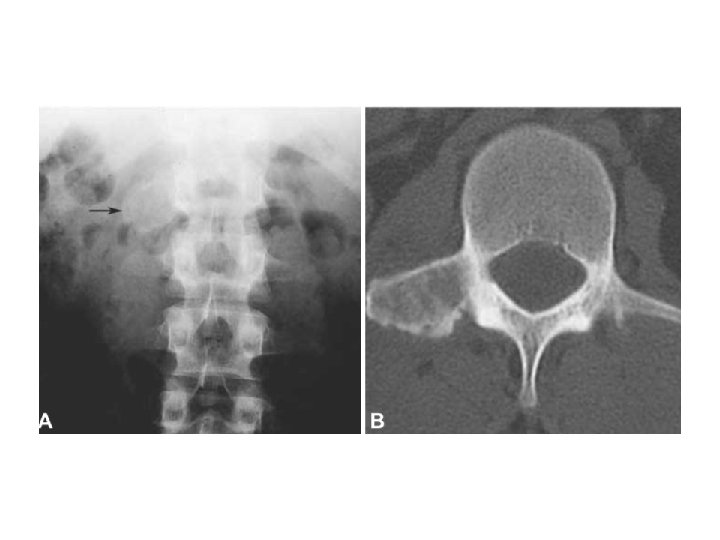
Benign ostaoblastoma Radiologic imaging: • Similar to those of osteoid osteoma, round or oval well-demarcated metaphyseal lytic defect surrounded by zone of reactive sclerosis • The sclerotic zone is usually less extensive compared with osteoid osteoma
Benign ostaoblastoma Gross finding: • Similar to that of osteoid osteoma • The tissue is granular, friable and reddish and may bleed when curetted • The bone contour can be markedly expanded specially in small bones • Features of ABC could be seen
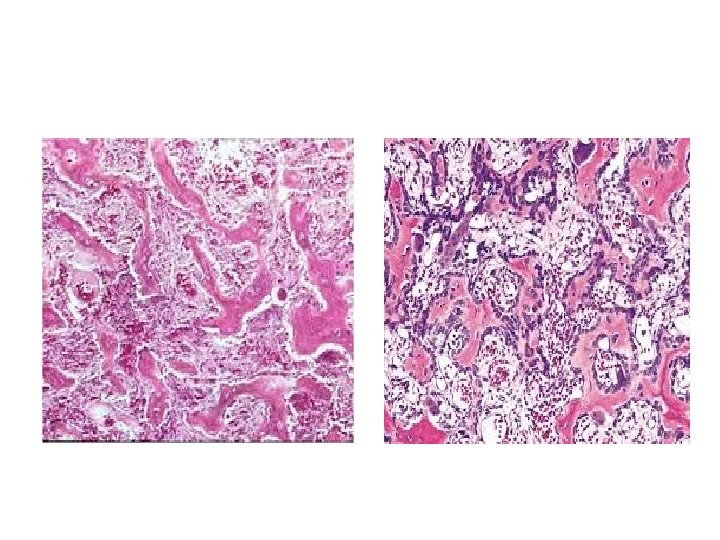
Benign ostaoblastoma Microscopic findings: • Similar to that of osteoid osteoma • Nidus is consists of an interlacing network of bone trabeculae evenly distributed in a loose fibroblastic stroma with prominent vasculature • Lacelike osteoids are rarely seen • Prominent osteoblastic rimming and osteoclastlike giant cells are seen • Few scattered mitotic figures could be seen
Benign ostaoblastoma • When the tumor extends beyond cortex, the shell of reactive bone could be seen in periphery • As a rule cartilage should not be present (exceptions can occur) • Features of ABC are seen mainly in large expanded lesions • In rare instances stromal cells show atypia called atypical or pseudosarcomatous differentiation (atypia is degenerative type like ancient schwannoma)
Benign ostaoblastoma Differential diagnosis: • Osteosarcoma • Osteoid osteoma • ABC (share similar anatomic locations, reactive bone formation in solid portions of ABC could be challenging )
Benign ostaoblastoma Treatment and behavior: • Higher growth potential than osteoid osteoma • The preferred treatment is surgical en bloc excision • Radiotherapy can be used in the cases of incomplete resection • Recurrence rate may be as high as 25% • Malignant transformation has reported rarely
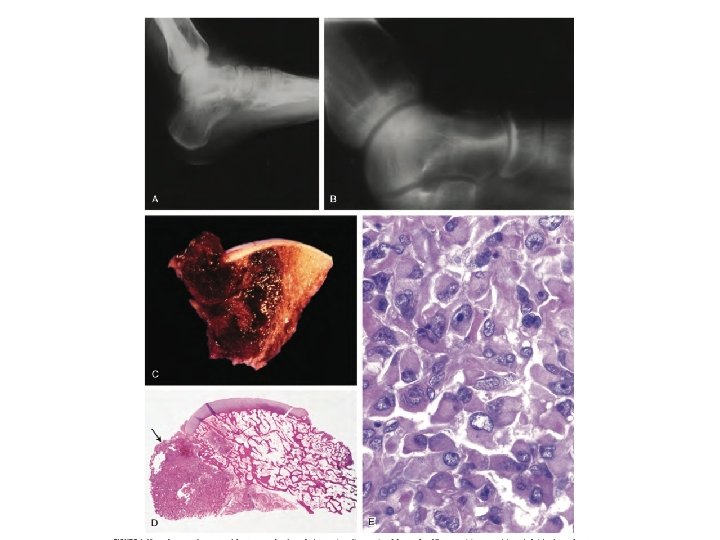
Aggressive osteoblastoma • A rare tumor that represents a borderline lesion between benign osteoblastoma and osteosarcoma • These tumors are likely to recur, do not metastasize and are characterized by epithelioid osteoblasts in microscopy • They are not precursors of conventional osteosarcoma
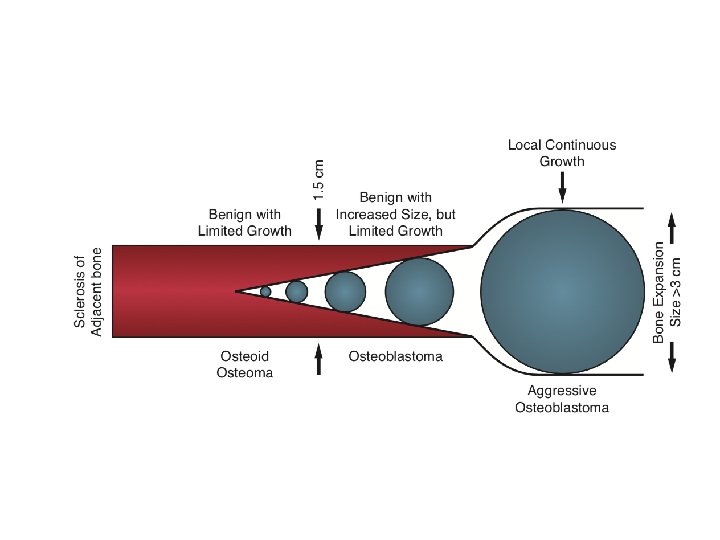
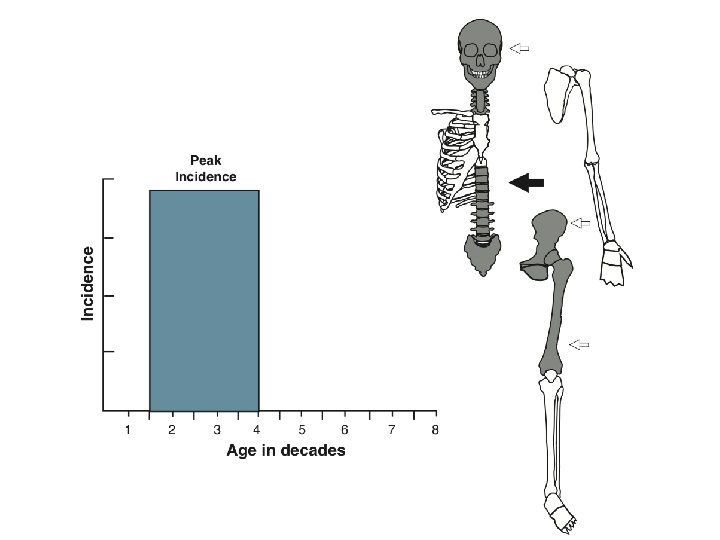
Aggressive osteoblastoma Radiologic findings: share many features with conventional osteoblastoma • They are usually larger and more than 4 cm • Gross findings: • Similar to that of conventional osteoblastoma
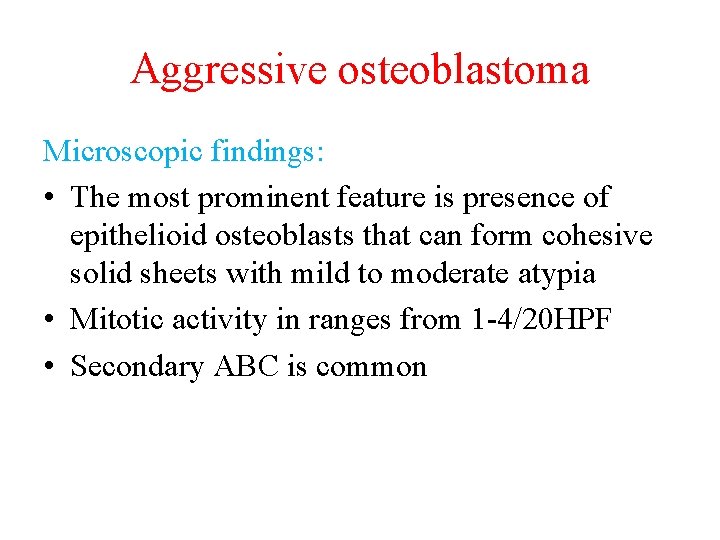
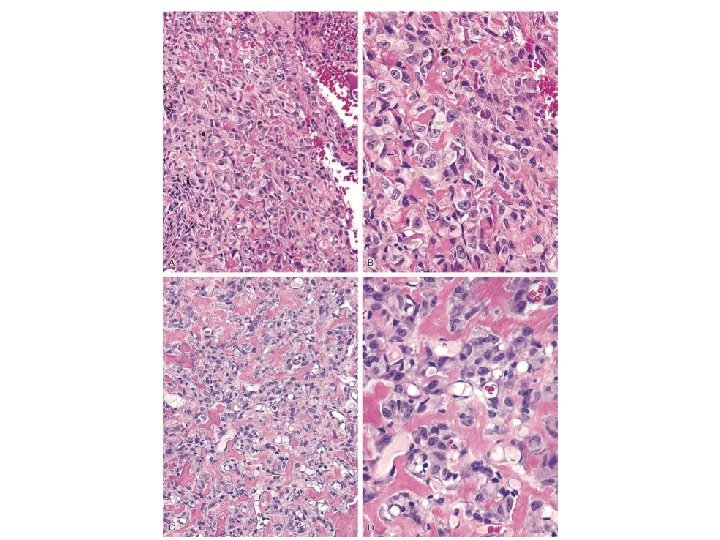
Aggressive osteoblastoma Microscopic findings: • The most prominent feature is presence of epithelioid osteoblasts that can form cohesive solid sheets with mild to moderate atypia • Mitotic activity in ranges from 1 -4/20 HPF • Secondary ABC is common
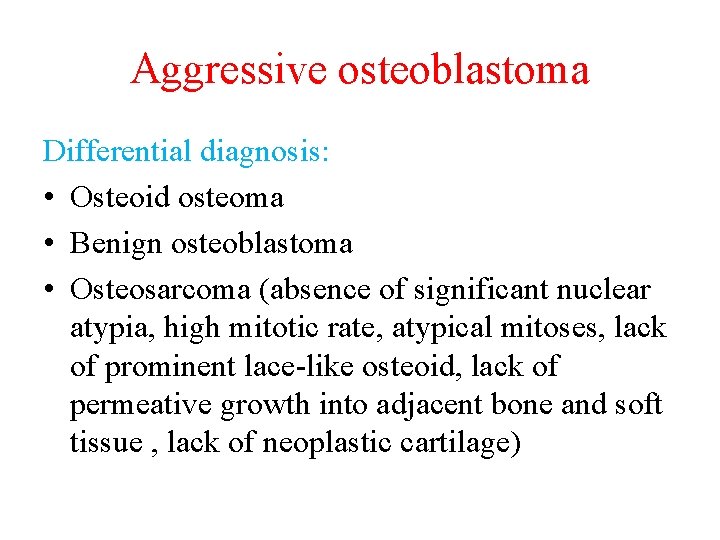
Aggressive osteoblastoma Differential diagnosis: • Osteoid osteoma • Benign osteoblastoma • Osteosarcoma (absence of significant nuclear atypia, high mitotic rate, atypical mitoses, lack of prominent lace-like osteoid, lack of permeative growth into adjacent bone and soft tissue , lack of neoplastic cartilage)

- Slides: 61