In the name of GOD Myoma in pregnancy

- Slides: 23
In the name of GOD
Myoma in pregnancy Sedigheh Borna, MD perinatologist Medical university of Tehran Vali_asr Hospital Obstetrics/Gynecology Department
• Myomas are the most frequently recorded benign smooth muscle tumor of the uterus, affecting 20%– 60% of women of reproductive age and may negatively affect fertility and outcome of pregnancy • As most fibroids are asymptomatic, the true prevalence of fibroids may be greatly higher • The incidence of fibroids in pregnancy reported ranges from 0. 1 to 10. 7% of all pregnancies and increases as the female chooses to postpone pregnancy later on • It was found that 10%– 40% of prepartum complications which happened in pregnancy with fibroid have been associated with the
EFFECTS OF PREGNANCY ON FIBROID • Changes in size – increases • Fibroid is an estrogen dependant tumor. Increased vascularity , Edema , Hypertrophy and hyperplasia of the fibromuscular tissues. • Pregnancy is a progesterone predominant state. • Actually, most fibroids do not increase in size during pregnancy. • 69% - had no increase in fibroid volume throughout pregnancy • 31% - noted increase in fibroid volume, greatest increase before 10 th week of gestation and a reduction to baseline value 4 weeks after delivery • Larger fibroids (>5 cm) more likely to grow Smaller fibroids More likely to remain stable. The mean increase in fibroid volume during pregnancy • 12% very few fibroids increase by >25%. • Changes in position • Changes in shape - becomes flattened • Degenerative changes specially, red degeneration • Torsion of pedunculated subserous fibroid 10% • Infection and polypoidal changes are more in puerperium.
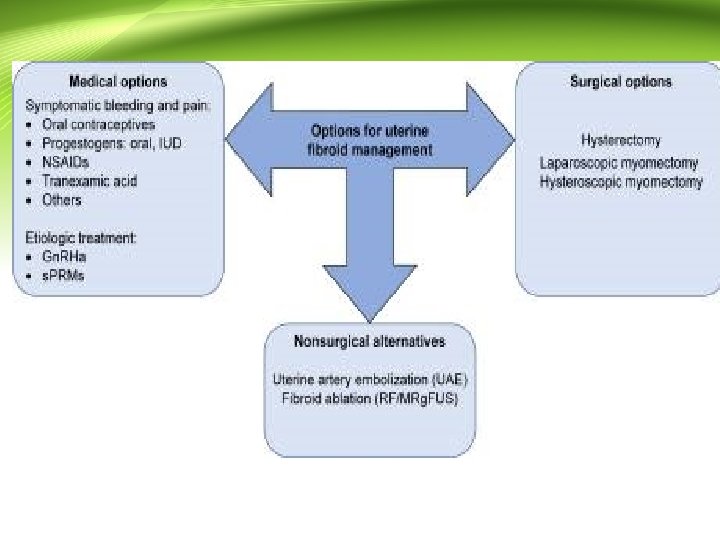
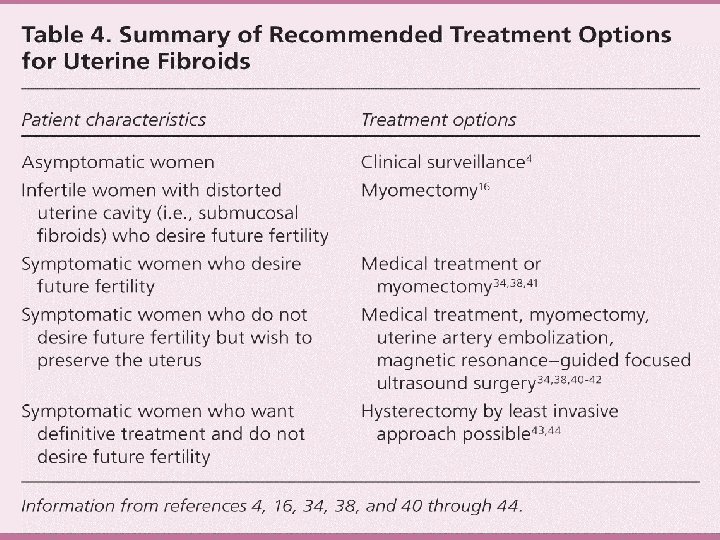
Treatment: ACOG • Certain signs and symptoms may signal the need for treatment: • Heavy or painful menstrual periods that cause anemia or that disrupt a woman’s normal activities • Bleeding between periods • Uncertainty whether the growth is a fibroid or another type of tumor, such as an ovarian tumor • Rapid increase in growth of the fibroid • Infertility • Pelvic pain
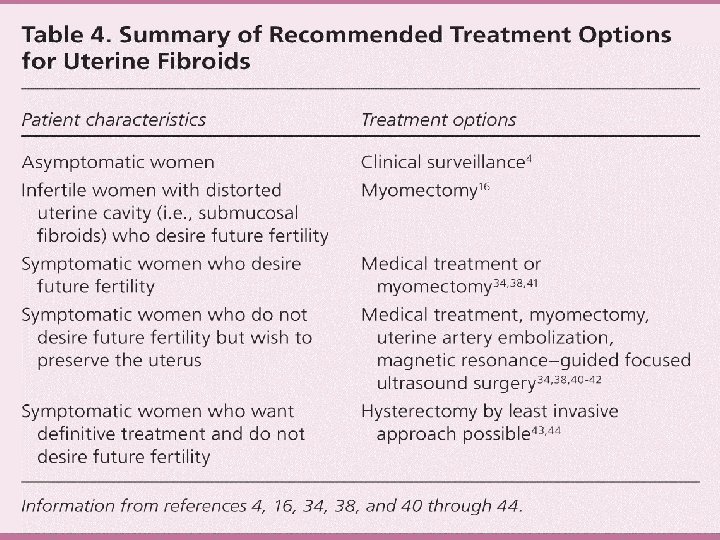
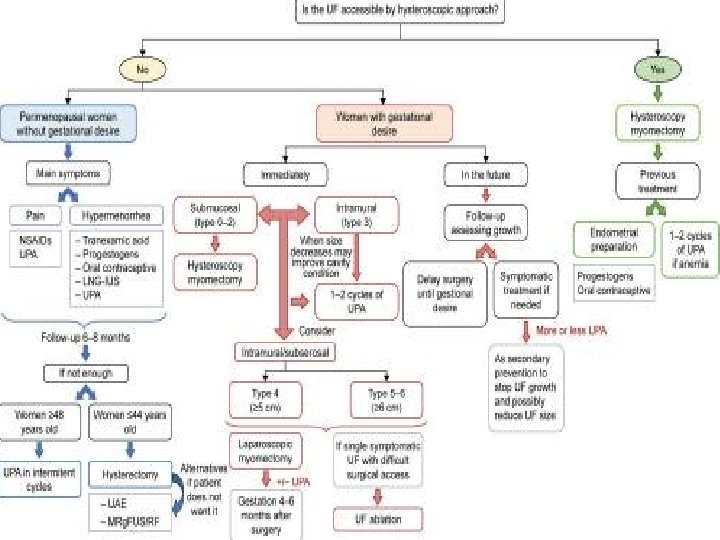
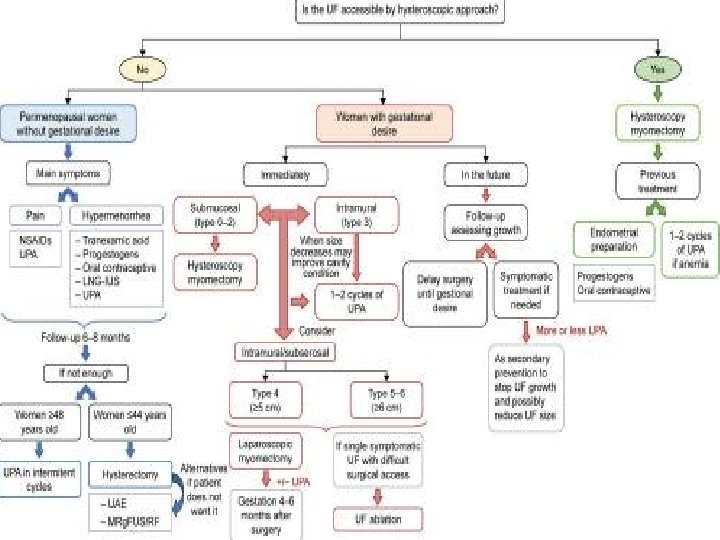
• Management of uterine fibroids should be tailored to and location of fibroids; • the patient's age, symptoms, • desire to preserve fertility, • and access to therapy; • and the physician's experience.
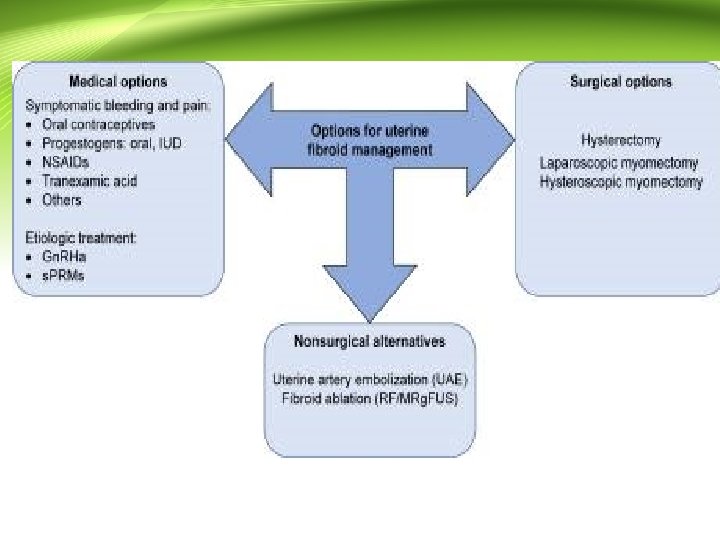
Medical therapy • Most medical therapies for uterine leiomyomas preclude conception, cause adverse effects when employed longterm, and result in rapid symptom rebound when discontinued. • Therefore, medical treatment of leiomyomas in infertile patients attempting to become pregnant is usually unsuccessful • One medical treatment of uterine leiomyoma is a selective progesterone modulator, ulipristal. • It is associated with rapid decrease in uterine bleeding, slight reduction in myoma size, and minimal menopausal symptoms. • If needed , ulipristal can be administered for another three months after two menstrual periods. • use 5 mg orally per day for three months, and the longest treatment has been four courses.
Miscellaneous techniques • Myoma coagulation or myolysis is associated with adhesion formation and may increase the risk of uterine rupture in pregnancy. • • The efficacy and safety of other procedures, especially in young women who wish to conceive, have not been proven. • These techniques include occlusion of uterine vessels either via laparoscopy or a vaginally-placed clamp, High intensity focused ultrasound (HIFU), cryomyolysis, radiofrequency ablation, and magnetic resonance imaging-directed • cryotherapy
Myomectomy versus embolization • We prefer myomectomy over uterine artery embolization (UAE) for treatment of most women with uterine leiomyomas who wish to conceive • However, we suggest UAE in women at high surgical risk, such as those with previous multiple laparotomies or diffuse uterine leiomyomas where myomectomy might not be technically feasible • We generally avoid UAE in women who wish to conceive because the safety of the procedure with respect to • subsequent pregnancy outcome has not been established.
MANAGEMENT BEFORE PREGNANCY • • Indications for preconception myomectomy Made on a case-by-case basis Age Reproductive history Severity of symptoms Size Site. No good data that preconception myomectomy will improve pregnancy success or the take-home baby
What types of surgery may be done to treat fibroids? • Treatment should be efficient with the maximum efficacy and the minimum risk and cost. • it is not necessary to emphasize that asymptomatic UFs do not require treatment regardless of their size. • However, the bigger the size, the more probable it is that they cause symptomatology.
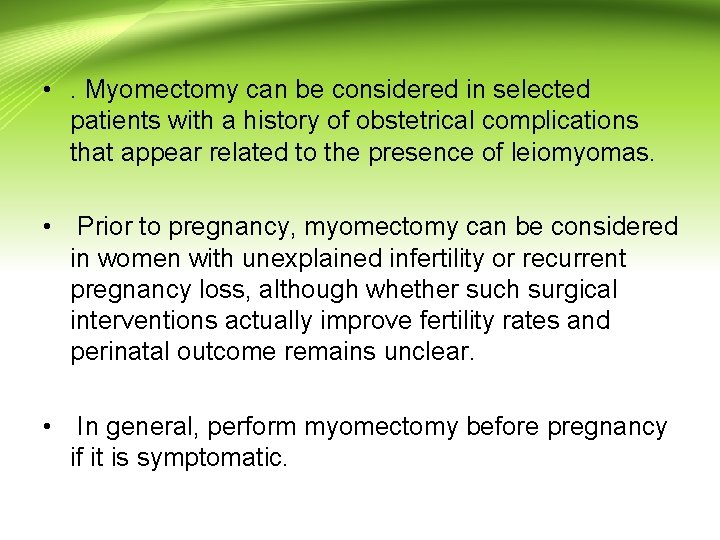
• . Myomectomy can be considered in selected patients with a history of obstetrical complications that appear related to the presence of leiomyomas. • Prior to pregnancy, myomectomy can be considered in women with unexplained infertility or recurrent pregnancy loss, although whether such surgical interventions actually improve fertility rates and perinatal outcome remains unclear. • In general, perform myomectomy before pregnancy if it is symptomatic.
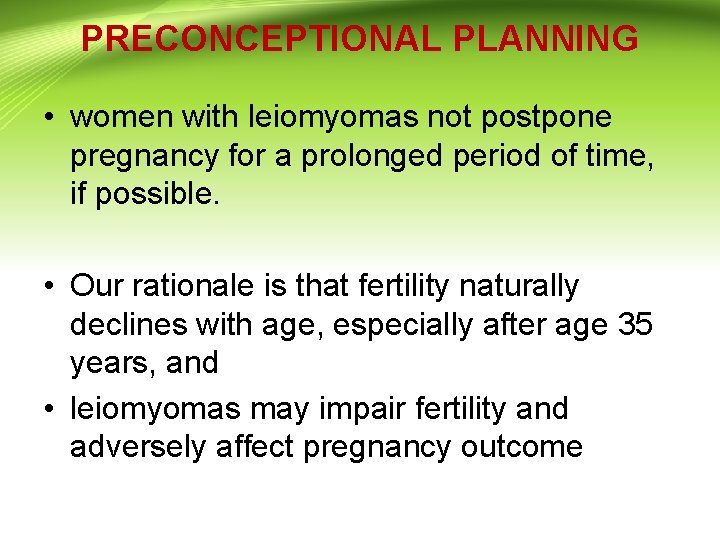
PRECONCEPTIONAL PLANNING • women with leiomyomas not postpone pregnancy for a prolonged period of time, if possible. • Our rationale is that fertility naturally declines with age, especially after age 35 years, and • leiomyomas may impair fertility and adversely affect pregnancy outcome
INFERTILITY AND MISCARRIAGE • Leiomyomas are estimated to account for 1 to 2 percent of infertility. • Fibroids, particularly those that impinge upon the endometrium, may affect fertility by interfering with implantation over the • myoma site, rapidly distending the uterus in early pregnancy, or impairing uterine contractility.
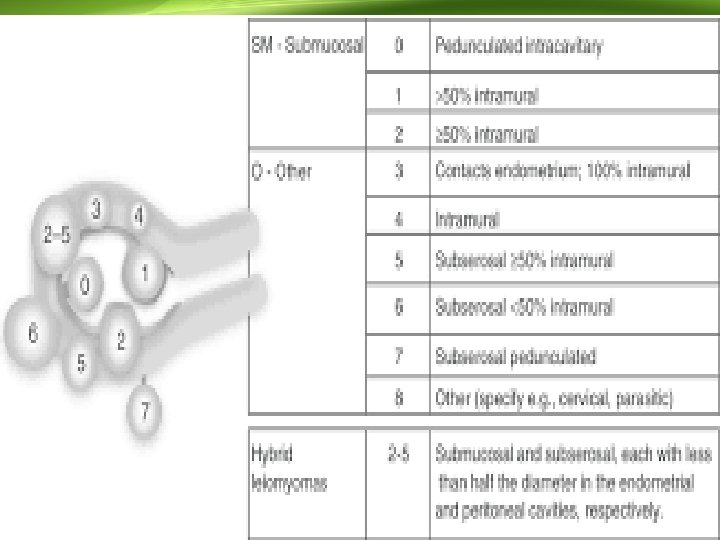
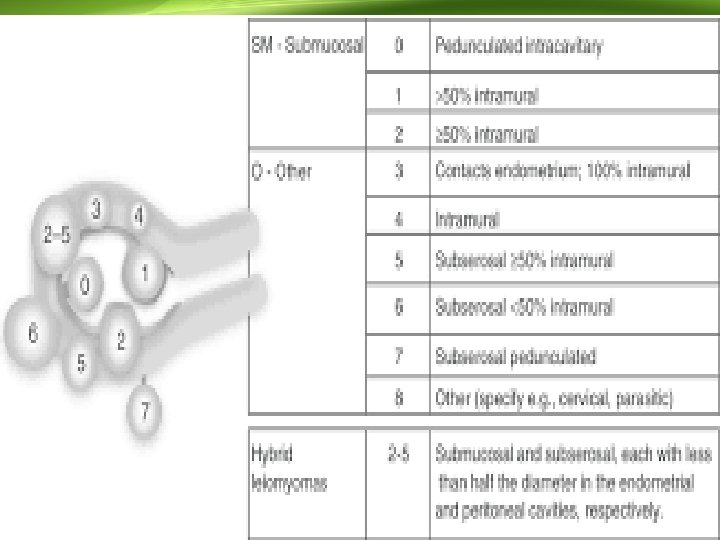
INFERTILITY AND MISCARRIAGE • The location of a fibroid, and not its size, is the key factor regarding fertility. • Leiomyomas that distort the uterine cavity (submucosal or intramural with an intracavitary component) result in difficulty conceiving a pregnancy and an increased risk of miscarriage. • In contrast, subserosal fibroids do not impact fertility. The role of intramural fibroids in infertility is controversial. • Couples should complete a full infertility evaluation before addressing the role of leiomyomas in their infertility
Preparing for in vitro fertilization • The effect of leiomyomas on IVF is dependent upon their location: • submucosal myomas decrease the chance of success, whereas subserosal myomas do not appear to have any effect. • Observational data suggest that intramural myomas may also have a negative impact on IVF outcomes
Preconception/Prenatal counseling: • the risks of obstetrical complications are increased with the presence of fibroids in pregnancy, but neither size or location adequately predict additional adverse outcomes. • Most fibroid growth occurs in the first trimester. Throughout pregnancy approximately 60% of fibroids will increase or decrease by greater than 10% of their original size.
