In the Name of God ACUTE OTITIS MEDIA


























- Slides: 60
In the Name of God ACUTE OTITIS MEDIA

Acute Otitis Media � The most common infection for which antibacterial agents are prescribed for children in the US � 1/3 of office visits to pediatricians � Peak incidence 6 – 12 months old ◦ ≈ 2/3 of children experience at least one episode by 1 year old
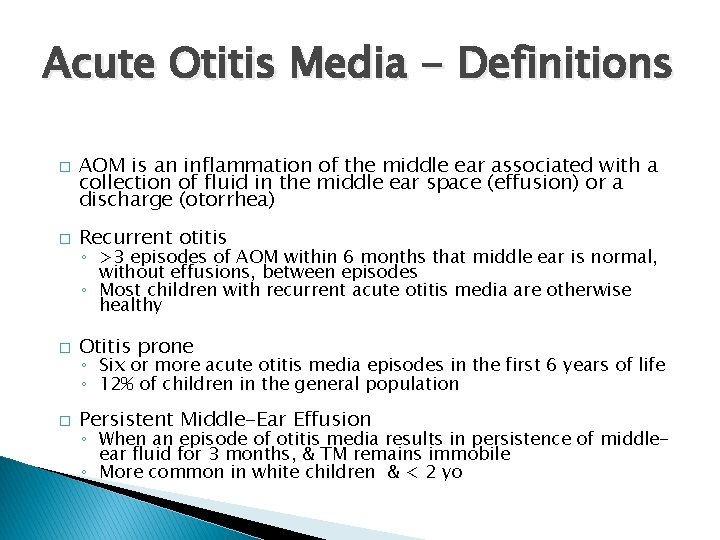
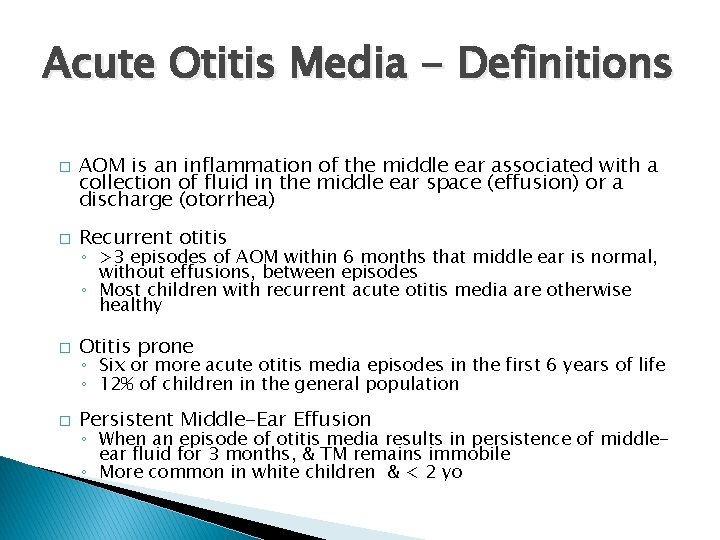
Acute Otitis Media - Definitions � AOM is an inflammation of the middle ear associated with a collection of fluid in the middle ear space (effusion) or a discharge (otorrhea) � Recurrent otitis � Otitis prone � Persistent Middle-Ear Effusion ◦ >3 episodes of AOM within 6 months that middle ear is normal, without effusions, between episodes ◦ Most children with recurrent acute otitis media are otherwise healthy ◦ Six or more acute otitis media episodes in the first 6 years of life ◦ 12% of children in the general population ◦ When an episode of otitis media results in persistence of middleear fluid for 3 months, & TM remains immobile ◦ More common in white children & < 2 yo
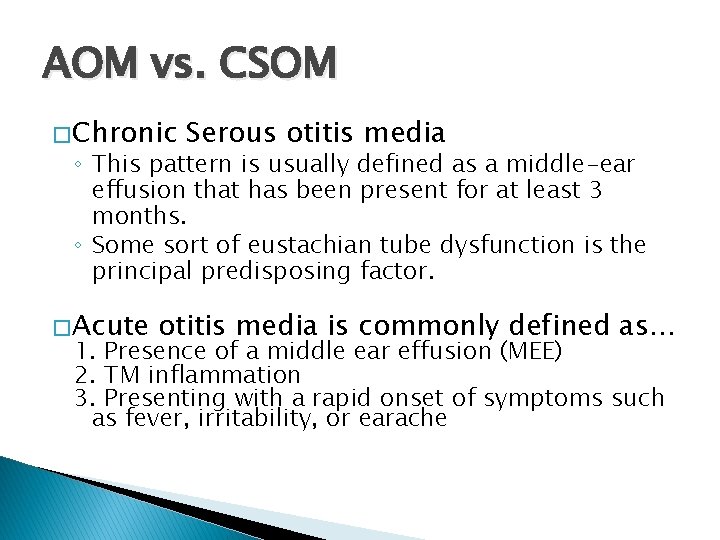
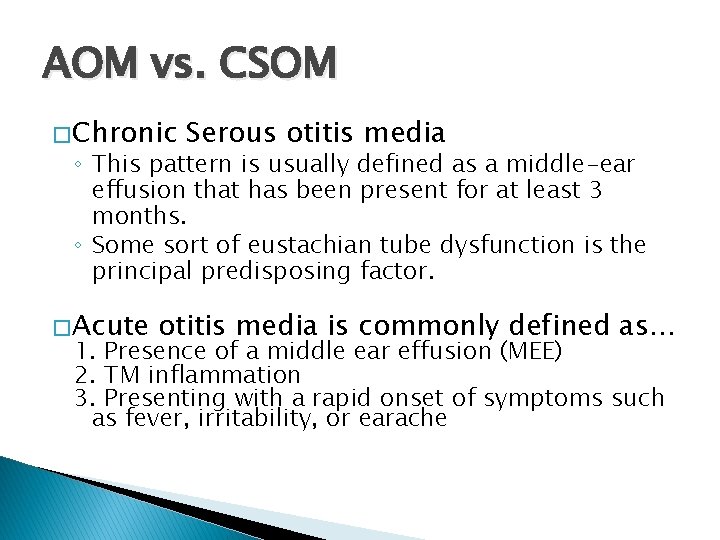
AOM vs. CSOM � Chronic Serous otitis media ◦ This pattern is usually defined as a middle-ear effusion that has been present for at least 3 months. ◦ Some sort of eustachian tube dysfunction is the principal predisposing factor. � Acute otitis media is commonly defined as… 1. Presence of a middle ear effusion (MEE) 2. TM inflammation 3. Presenting with a rapid onset of symptoms such as fever, irritability, or earache
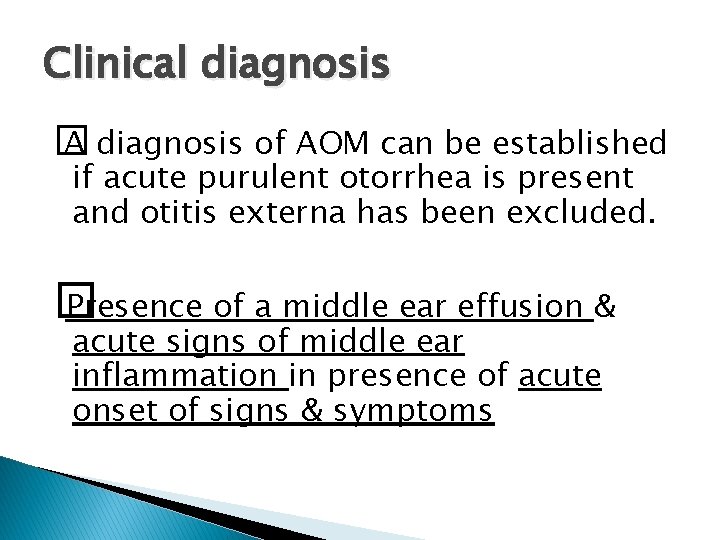
Clinical diagnosis � A diagnosis of AOM can be established if acute purulent otorrhea is present and otitis externa has been excluded. � Presence of a middle ear effusion & acute signs of middle ear inflammation in presence of acute onset of signs & symptoms

History � Children with AOM usually present with … ◦ History of rapid onset of otalgia (or pulling of the ear in an infant), irritability, poor feeding in an infant or toddler, otorrhea, and/or fever ◦ Except otorrhea other findings are nonspecific i. e. Fever, earache, and excessive crying present in children … 90% with AOM 72% without AOM

Laboratory tests � Routine laboratory studies, including complete blood count and ESR, are not useful in the evaluation of otitis media.
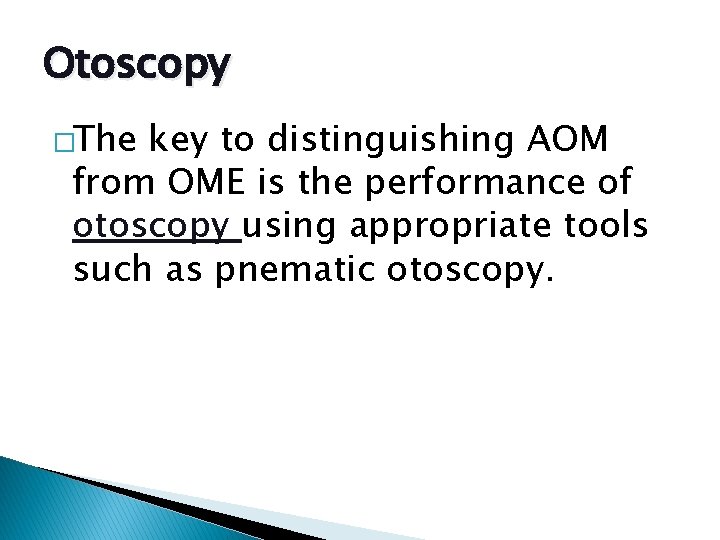
Otoscopy �The key to distinguishing AOM from OME is the performance of otoscopy using appropriate tools such as pnematic otoscopy.
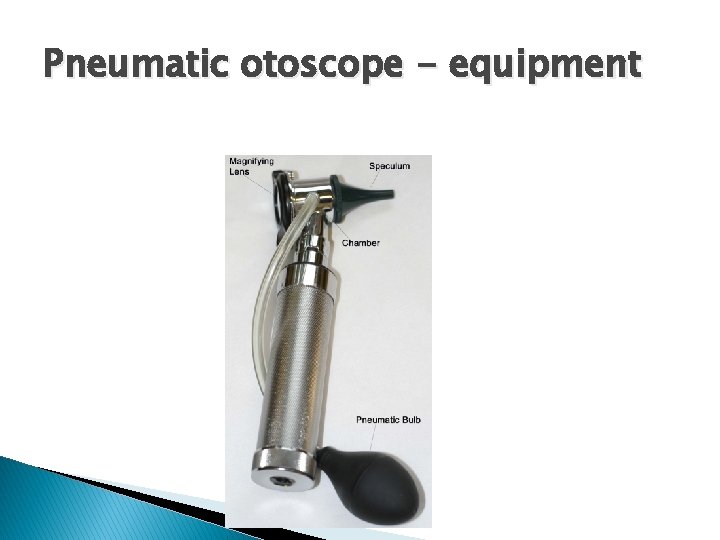
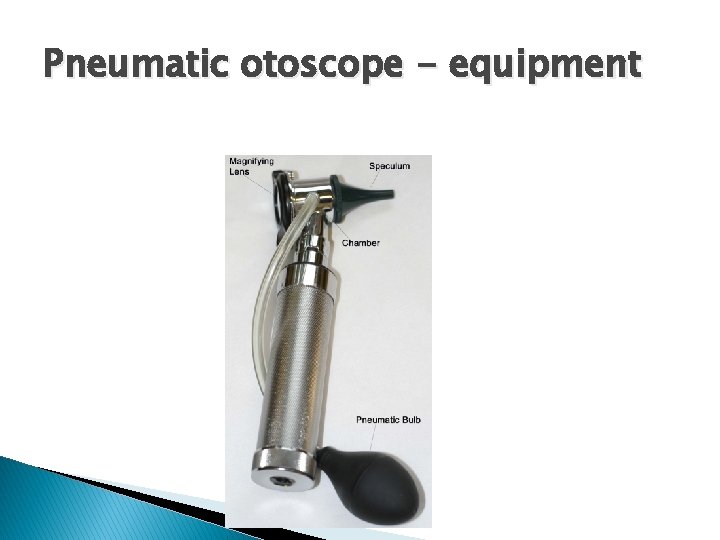
Pneumatic otoscope - equipment

Technique

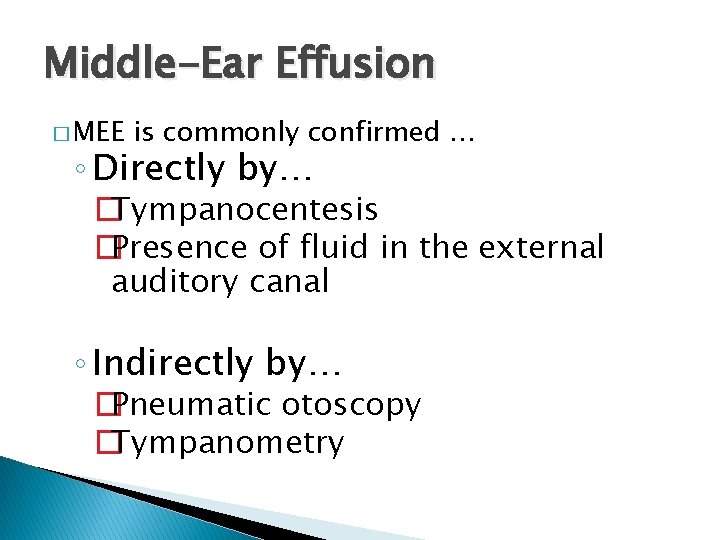
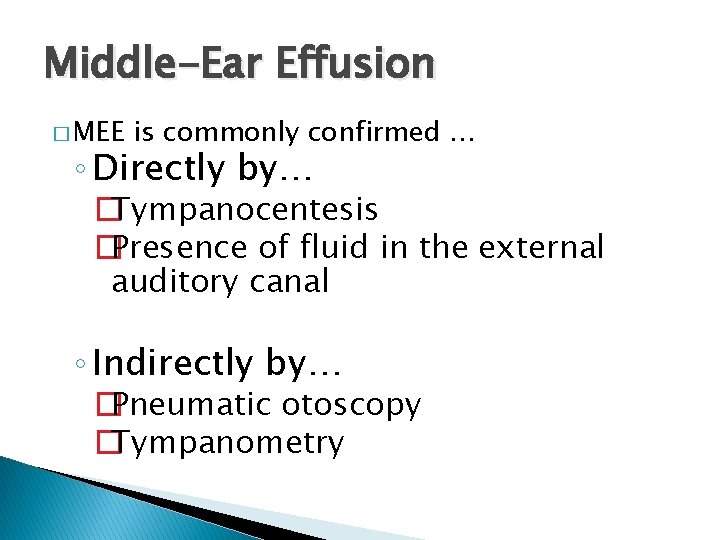
Middle-Ear Effusion � MEE is commonly confirmed … ◦ Directly by… �Tympanocentesis �Presence of fluid in the external auditory canal ◦ Indirectly by… �Pneumatic otoscopy �Tympanometry
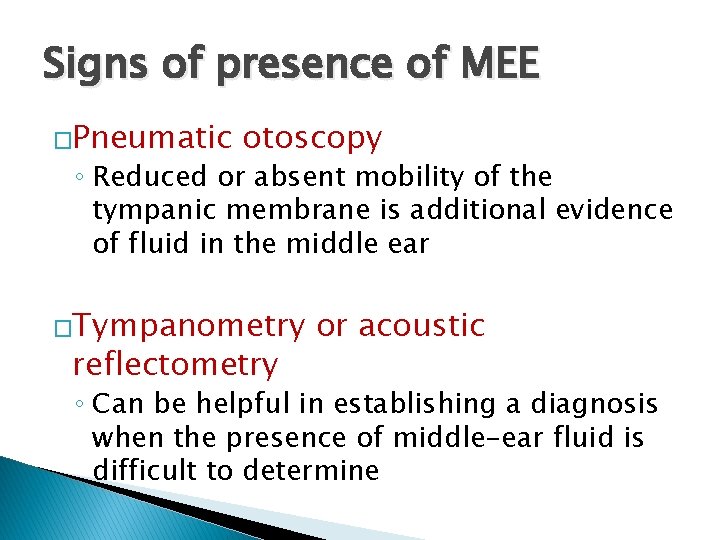
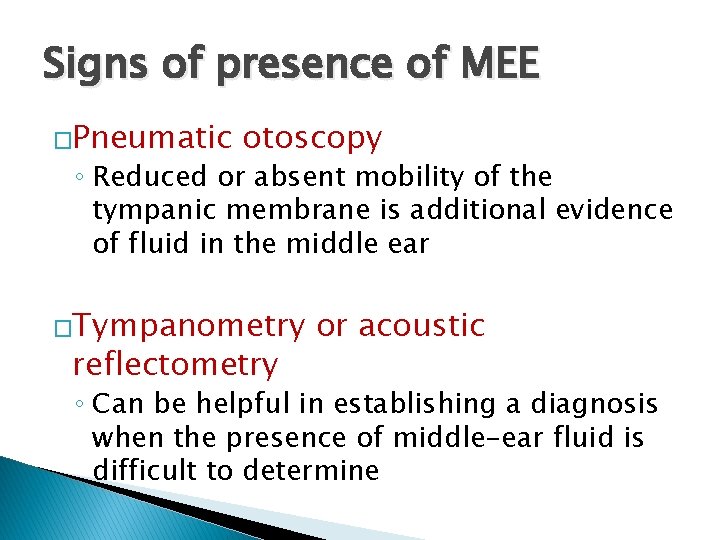
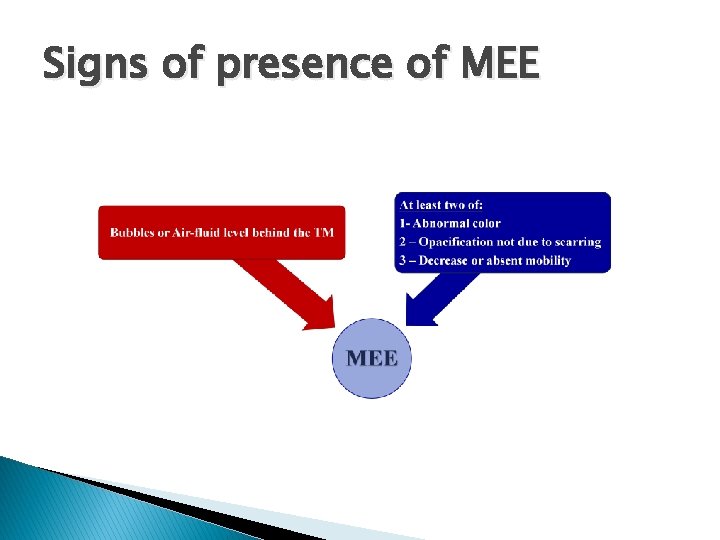
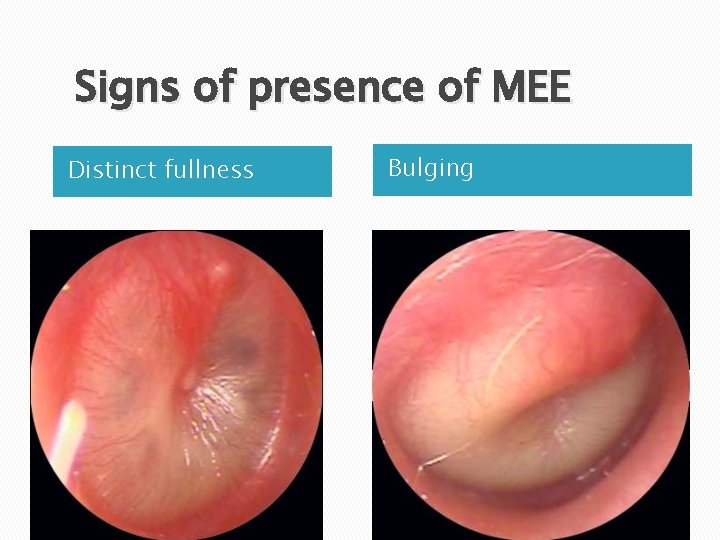
Signs of presence of MEE �Pneumatic otoscopy ◦ Reduced or absent mobility of the tympanic membrane is additional evidence of fluid in the middle ear �Tympanometry reflectometry or acoustic ◦ Can be helpful in establishing a diagnosis when the presence of middle-ear fluid is difficult to determine
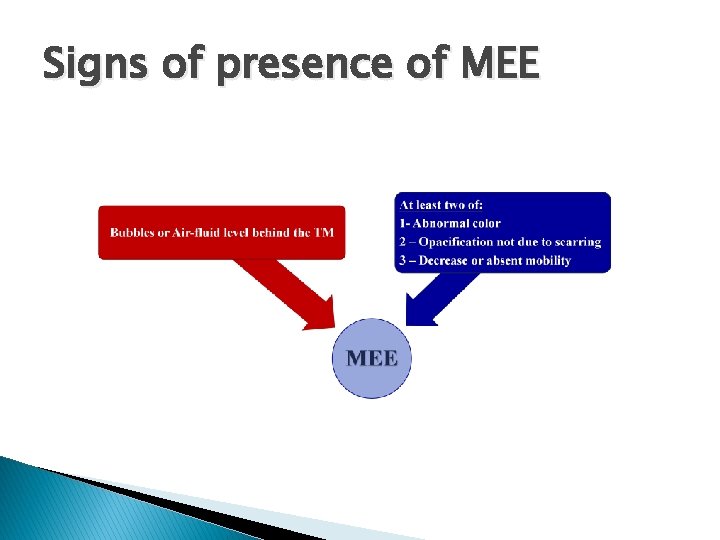
Signs of presence of MEE
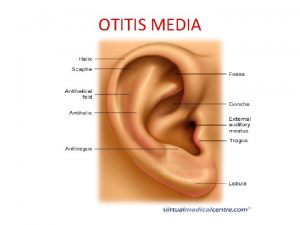
� Systematic assessment of the ◦ Color ◦ Mobility Position ◦ Translucency ◦ External auditory canal and auricle

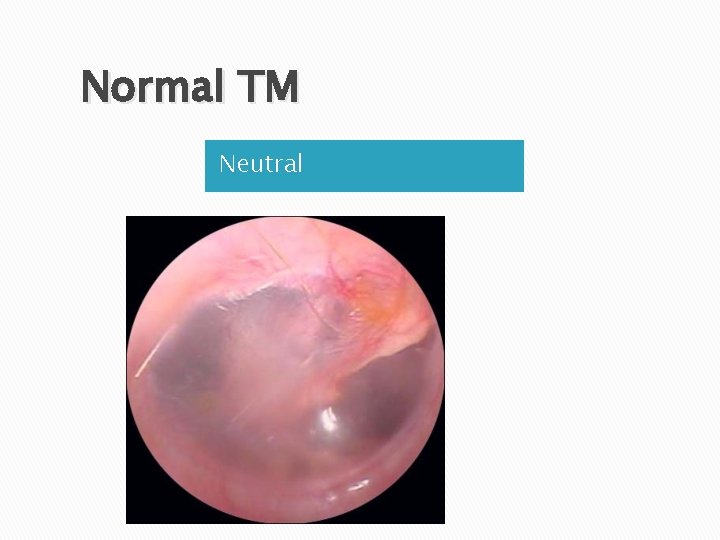
Normal tympanic membrane

Normal TM Translucent
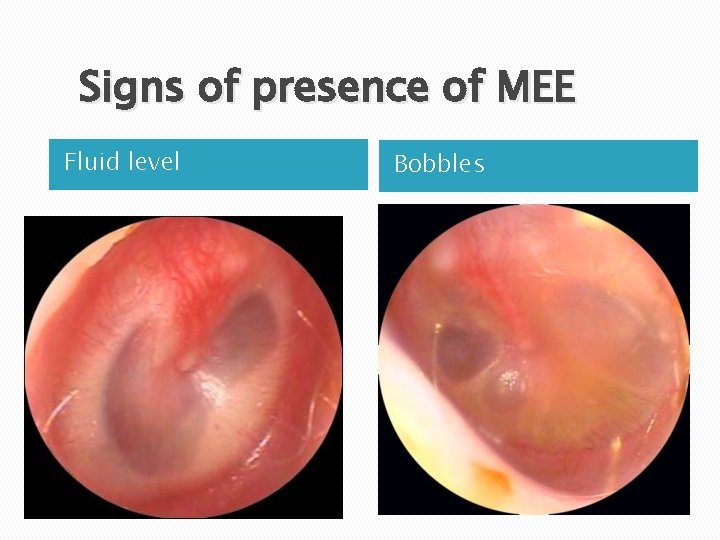
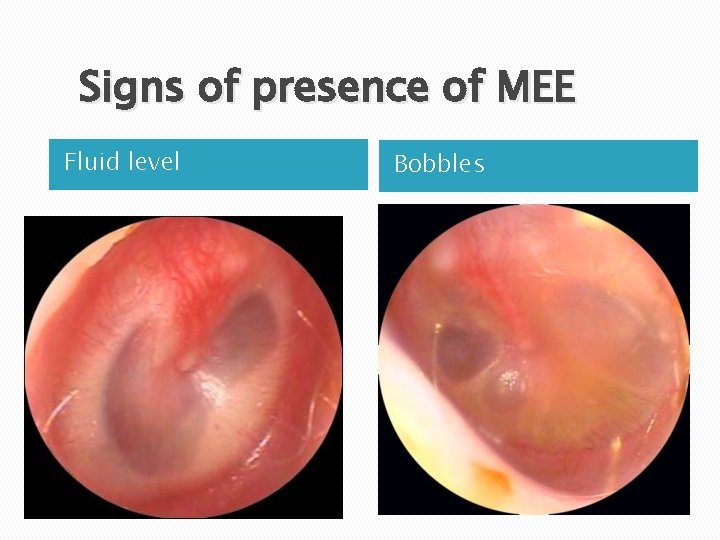
Signs of presence of MEE Fluid level Bobbles
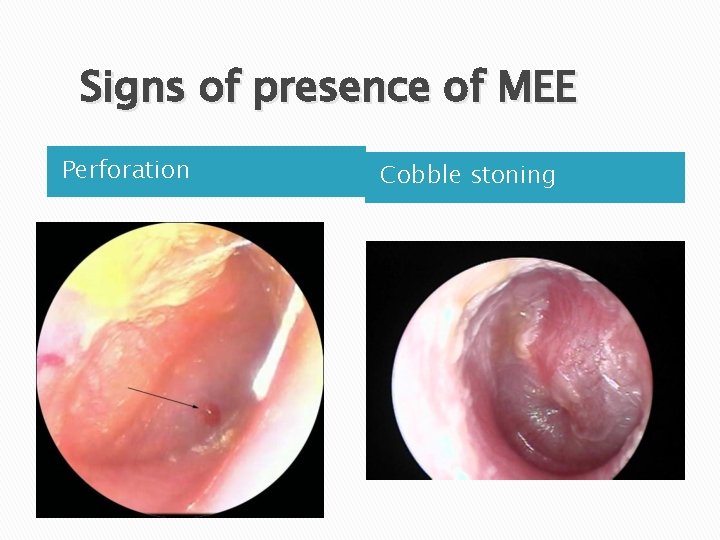
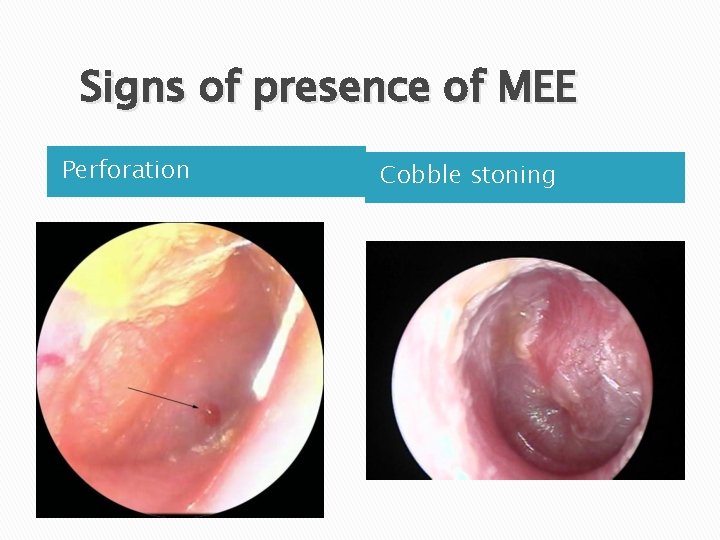
Signs of presence of MEE Perforation Cobble stoning

Signs of presence of MEE Semi-opaque Opaque
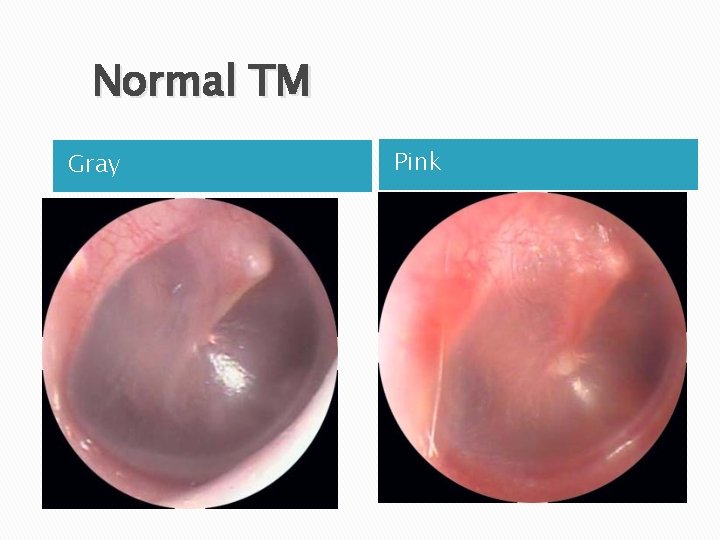
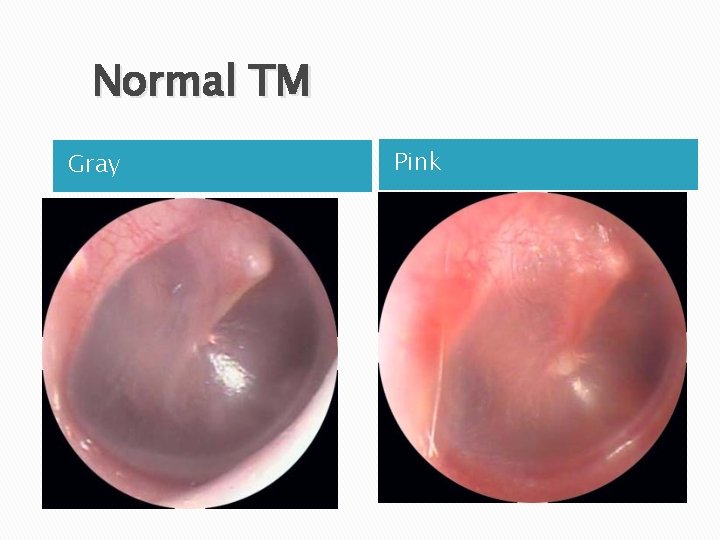
Normal TM Gray Pink
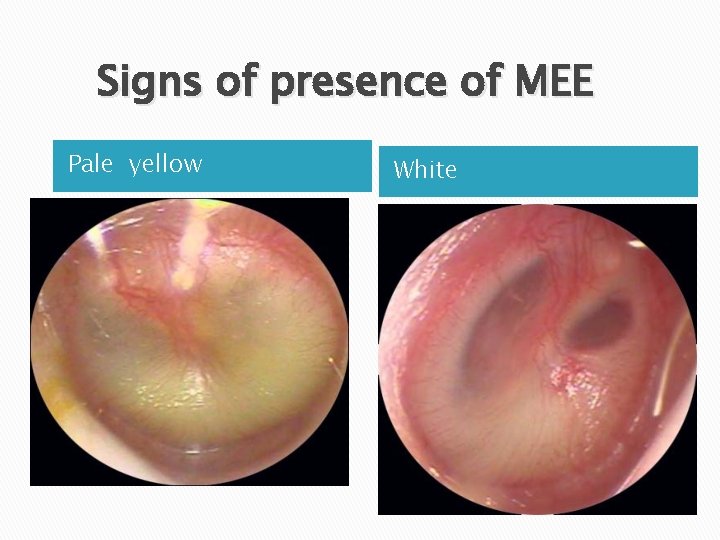
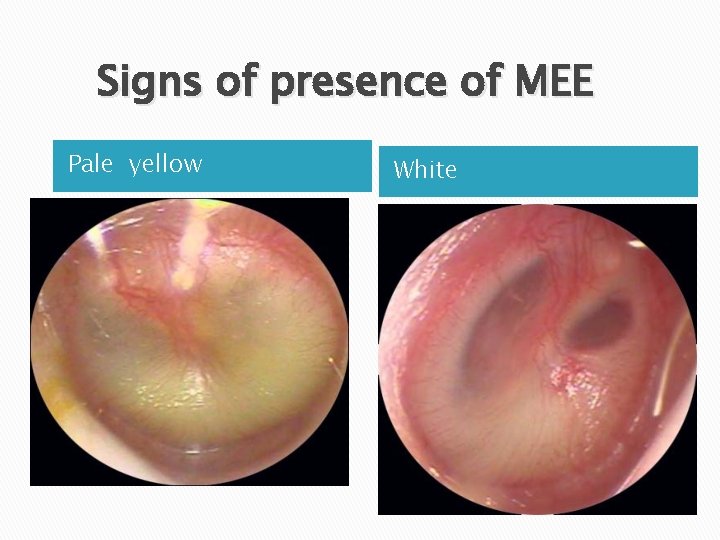
Signs of presence of MEE Pale yellow White

Tympanometry
OME vs. AOM � Major challenge Otitis Media with Effusion Vs. Acute Otitis Media
Signs & symptoms of middle-ear inflammation � Signs or symptoms of middle-ear inflammation indicated by … a. Non – otoscopic findings a. Distinct otalgia (discomfort clearly referable to the ear[s] that results in interference with or precludes normal activity or sleep) b. However, these symptoms must be accompanied by abnormal otoscopic findings b. Otoscopic findings

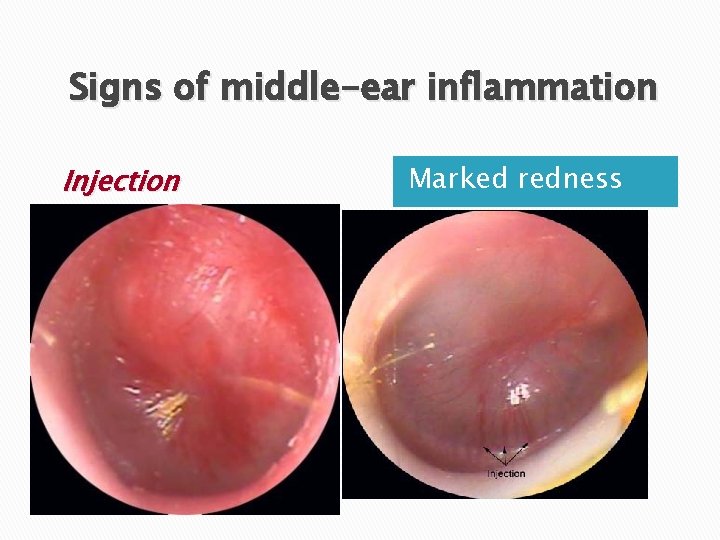
Acute inflammation – otoscopic findings � Signs of acute inflammation are necessary to differentiate AOM from OME. �Distinct fullness or bulging ◦ The best and most reproducible sign of acute inflammation � Marked redness of the tympanic membrane ◦ Marked redness of the tympanic membrane without bulging is an unusual finding in AOM.
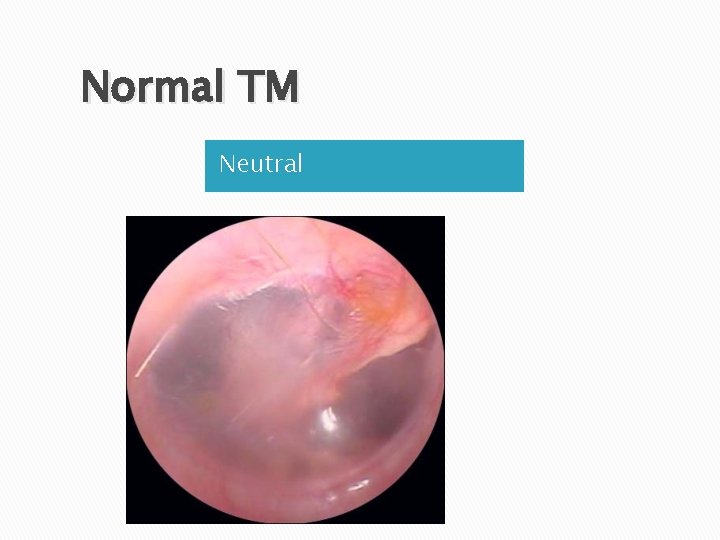
Normal TM Neutral
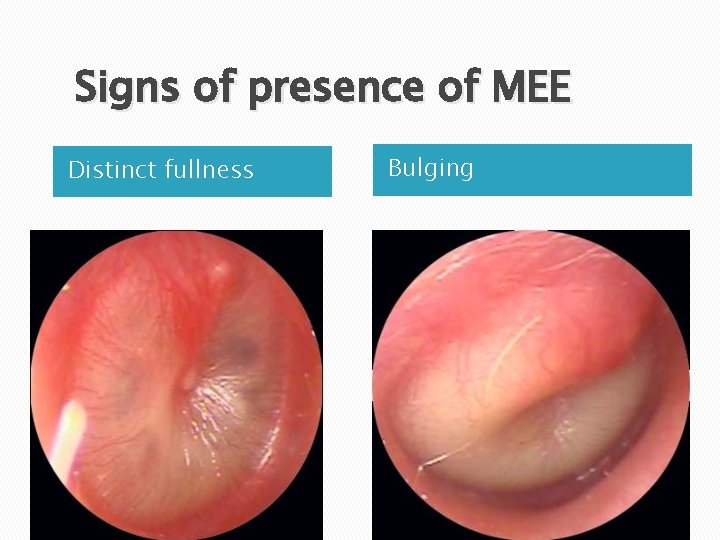
Signs of presence of MEE Distinct fullness Bulging
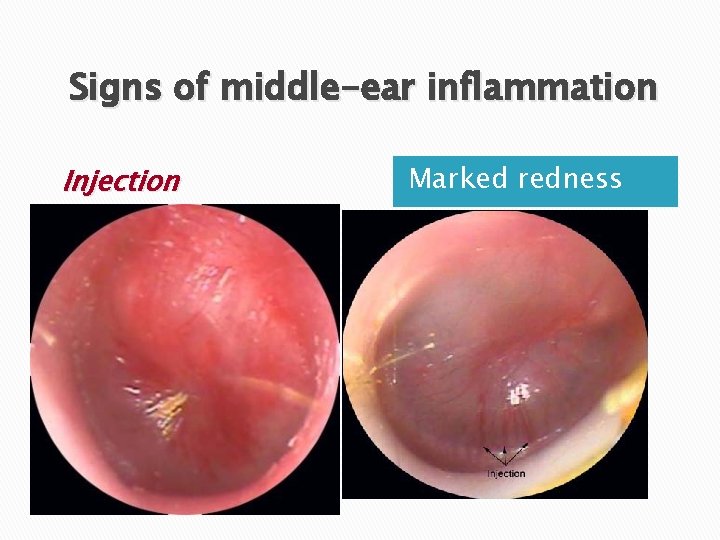
Signs of middle-ear inflammation Injection Marked redness

Established acute otitis media
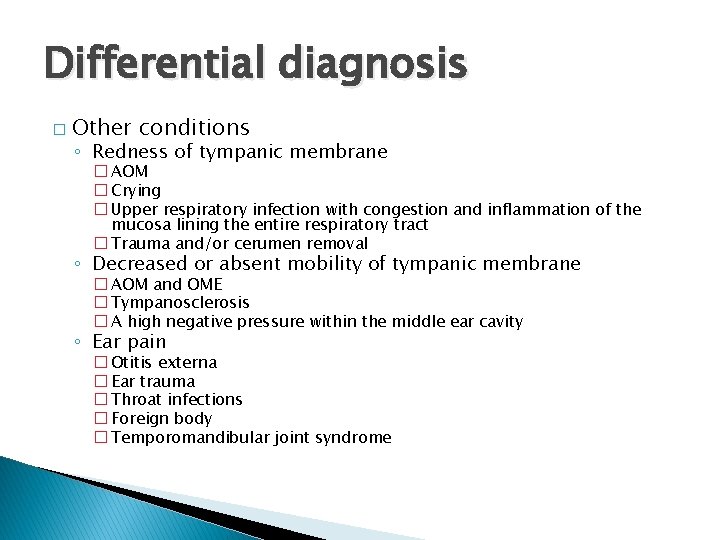
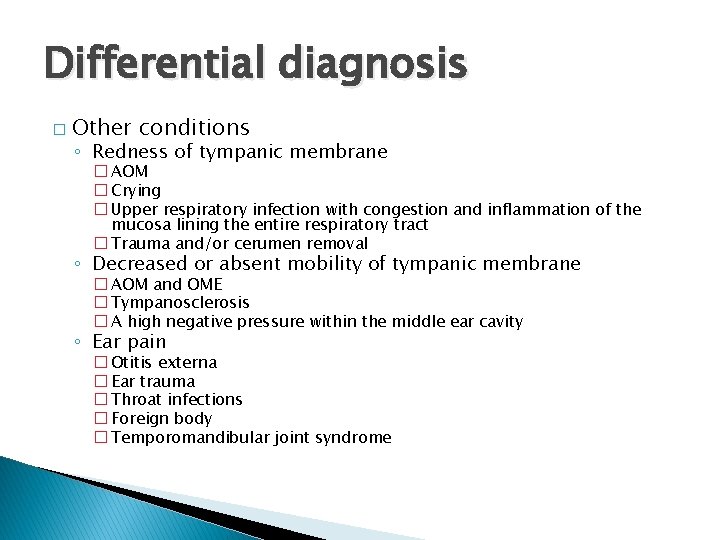
Differential diagnosis � Other conditions ◦ Redness of tympanic membrane � AOM � Crying � Upper respiratory infection with congestion and inflammation of the mucosa lining the entire respiratory tract � Trauma and/or cerumen removal ◦ Decreased or absent mobility of tympanic membrane � AOM and OME � Tympanosclerosis � A high negative pressure within the middle ear cavity ◦ Ear pain � Otitis externa � Ear trauma � Throat infections � Foreign body � Temporomandibular joint syndrome

Uncertainty in diagnosis of AOM � The diagnosis of AOM, particularly in infants and young children, is often made with a degree of uncertainty. � Common factors … ◦ Inability to sufficiently clear the external auditory canal of cerumen ◦ Narrow ear canal ◦ Inability to maintain an adequate seal for successful pneumatic otoscopy or tympanometry � An uncertain diagnosis of AOM is caused most often by inability to confirm the presence of MEE.

Management

Clinical Course � � The systemic and local signs and symptoms of AOM usually resolve in 24 to 72 hours with appropriate antimicrobial therapy, and somewhat more slowly in children who are not treated. However, middle ear effusion persisted for weeks to months after the onset of AOM … ◦ Among children who were successfully treated… � 70% resolution of effusion within two weeks � 90% up to 3 months
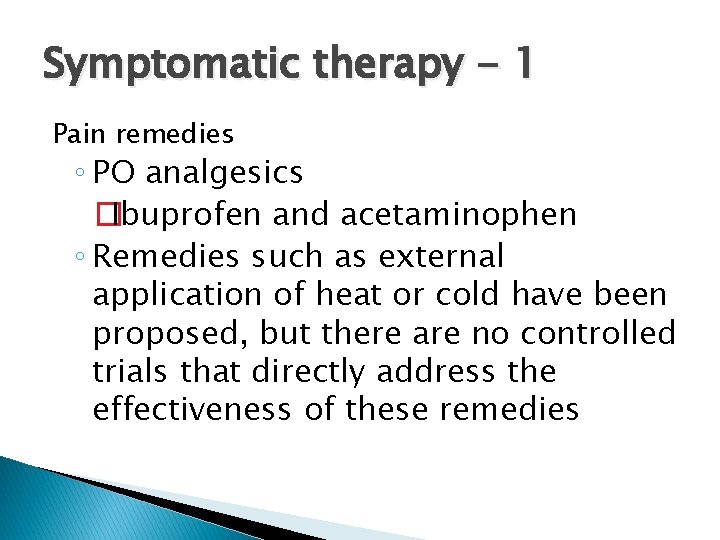
Symptomatic therapy - 1 Pain remedies ◦ PO analgesics �Ibuprofen and acetaminophen ◦ Remedies such as external application of heat or cold have been proposed, but there are no controlled trials that directly address the effectiveness of these remedies
Symptomatic therapy - 2 Oral Decongestants and antihistamines � Alone or in combination were associated with… ◦ Increased medication side effects ◦ Did not improve healing or prevent surgery or other complications in AOM ◦ Not approved for < 2 year old � In addition, treatment with antihistamines may prolong the duration of middle ear effusion � Topical decojestant & steroids

Comparative AOM Outcomes for Observation vs Antibacterial Agent AOM Outcome Antibacteral Rx Observation P Value Relief at 24 hours 60% 59% NS Relief at 2 -3 days 91% 87% NS Relief at 4 -7 days 79% 71% NS Clinical Resolution 82% 72% NS Mastoiditis/Complication 0. 09% 0. 17% NS Persistent MEE 4 -6 wks 45% 48% NS Persistent MEE 3 mo. 21% 26% NS Diarrhea/Vomiting 16% - - Skin Rash/Allergy 2% - -
Watch & See protocol � Observation without use of antibacterial agents in a child with uncomplicated AOM is an option for selected children In this protocol … � Deferring antibacterial treatment of selected children for 48 -72 hrs & limiting management to symptomatic relief

� Observation ◦ ◦ option is based on … Diagnostic certainty Age Illness severity Assurance of follow-up

Criteria for initial antibacterial-agent treatment or observation in children with AOM Age <6 mo Certain Diagnosis Antibacterial therapy 6 mo – 2 yr Antibacterial therapy >2 yr Antibacterial therapy if severe illness Observation option if non-severe illness Uncertain Diagnosis Antibacterial therapy if severe illness Observation option if non-severe illness Observation option

Definitions � Non-severe ◦ Mild otalgia � Severe illness is … illness is & fever <39°C in the past 24 hours ◦ Moderate to severe otalgia �A OR fever 39°C certain diagnosis of AOM meets all 3 criteria … 1) Rapid onset 2) Signs of MEE 3) Signs and symptoms of middle-ear inflammation.

Criteria for initial antibacterial-agent treatment or observation in children with AOM Age <6 mo Certain Diagnosis Antibacterial therapy 6 mo – 2 yr Antibacterial therapy >2 yr Antibacterial therapy if severe illness Observation option if non-severe illness Uncertain Diagnosis Antibacterial therapy if severe illness Observation option if non-severe illness Observation option
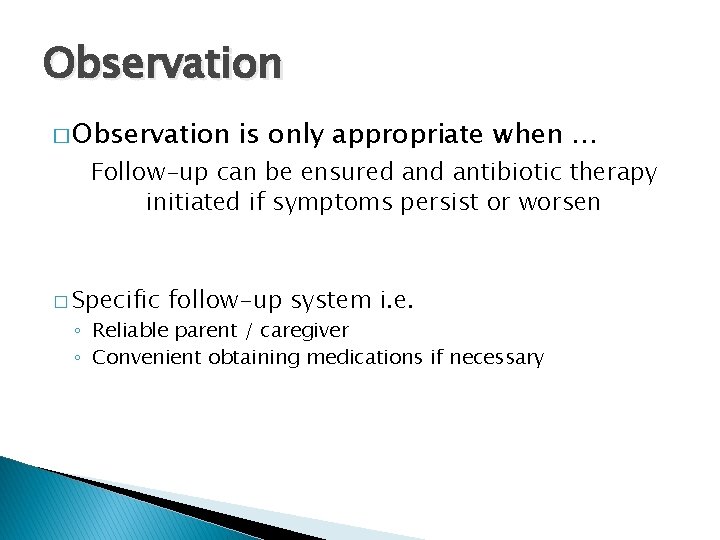
Observation � Observation is only appropriate when … Follow-up can be ensured antibiotic therapy initiated if symptoms persist or worsen � Specific follow-up system i. e. ◦ Reliable parent / caregiver ◦ Convenient obtaining medications if necessary
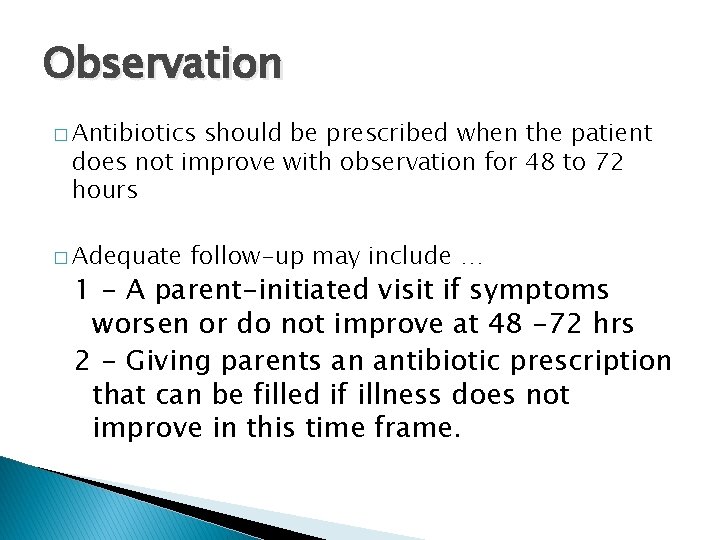
Observation � Antibiotics should be prescribed when the patient does not improve with observation for 48 to 72 hours � Adequate follow-up may include … 1 - A parent-initiated visit if symptoms worsen or do not improve at 48 -72 hrs 2 - Giving parents an antibiotic prescription that can be filled if illness does not improve in this time frame.
Which antibiotic ? ? ? � � � � � Amoxicillin Ammoxicillin + Clavulanate Azithromycin Cefixime Cefuroxime Ceftriaxone Clarithromycin Clindamycin Erythromycin Cotrimoxazole Erythromycin + Cotrimoxazole Penicillin V / G Penicillin Procain 800. 000 / 400. 000 Penicillin 6: 3: 3 / 1. 200. 000 Gentamicin / Amikacin Cephalexin Cloxacillin Metronidazole
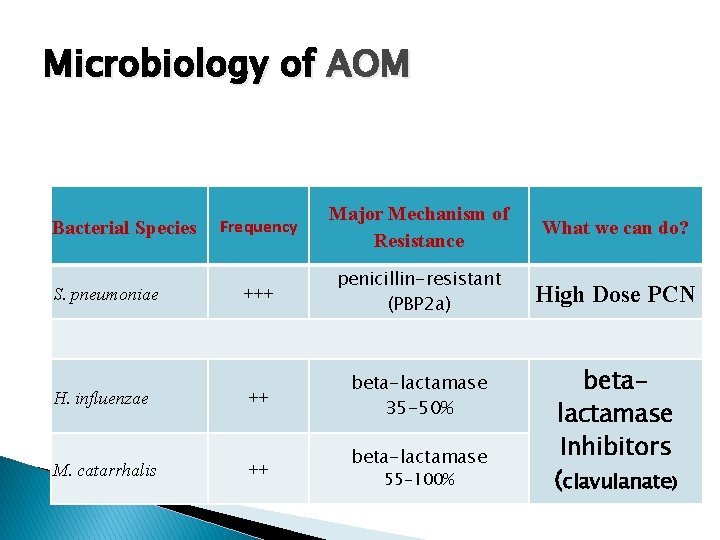
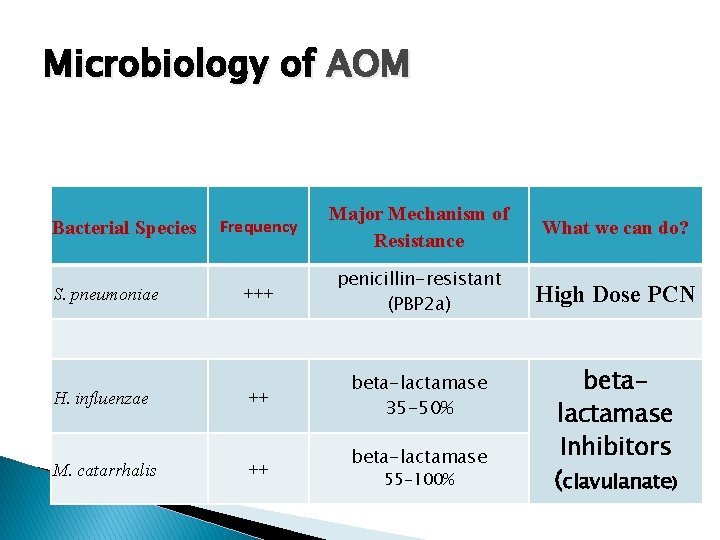
Microbiology of AOM Frequency Major Mechanism of Resistance What we can do? S. pneumoniae +++ penicillin-resistant (PBP 2 a) High Dose PCN H. influenzae ++ beta-lactamase 35 -50% M. catarrhalis ++ Bacterial Species beta-lactamase 55 -100% betalactamase Inhibitors (clavulanate)
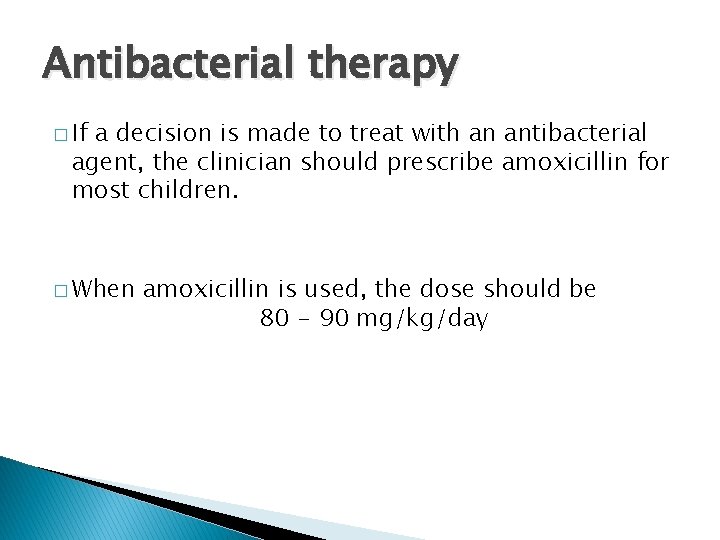
Antibacterial therapy � If a decision is made to treat with an antibacterial agent, the clinician should prescribe amoxicillin for most children. � When amoxicillin is used, the dose should be 80 - 90 mg/kg/day
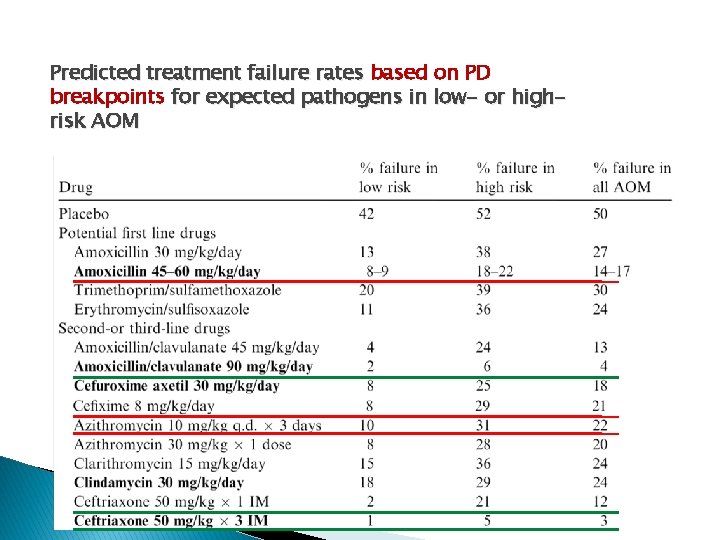
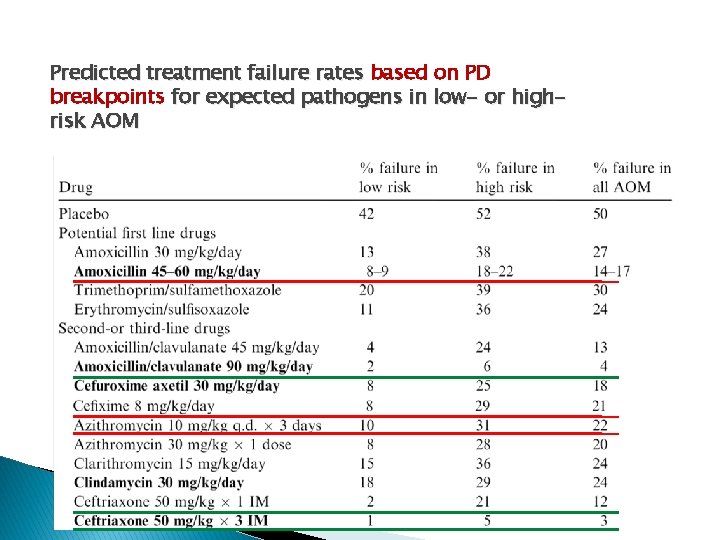
Predicted treatment failure rates based on PD breakpoints for expected pathogens in low- or highrisk AOM
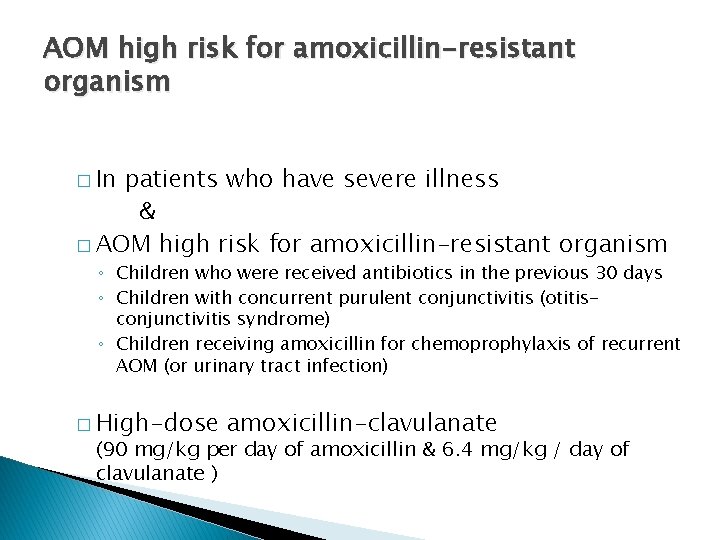
AOM high risk for amoxicillin-resistant organism � In patients who have severe illness & � AOM high risk for amoxicillin-resistant organism ◦ Children who were received antibiotics in the previous 30 days ◦ Children with concurrent purulent conjunctivitis (otitisconjunctivitis syndrome) ◦ Children receiving amoxicillin for chemoprophylaxis of recurrent AOM (or urinary tract infection) � High-dose amoxicillin-clavulanate (90 mg/kg per day of amoxicillin & 6. 4 mg/kg / day of clavulanate )
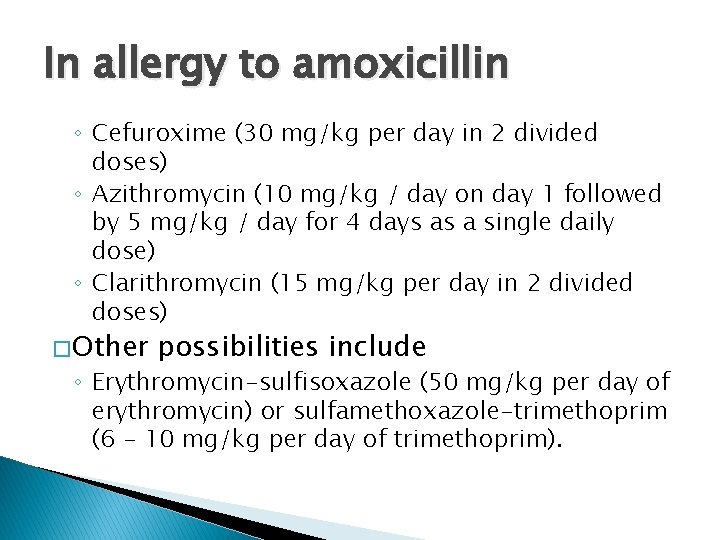
In allergy to amoxicillin ◦ Cefuroxime (30 mg/kg per day in 2 divided doses) ◦ Azithromycin (10 mg/kg / day on day 1 followed by 5 mg/kg / day for 4 days as a single daily dose) ◦ Clarithromycin (15 mg/kg per day in 2 divided doses) � Other possibilities include ◦ Erythromycin-sulfisoxazole (50 mg/kg per day of erythromycin) or sulfamethoxazole-trimethoprim (6 - 10 mg/kg per day of trimethoprim).
In daily clinical practice… �

In daily clinical practice… � q 8 h Amoxicillin (2/3) 125 250 � Bid Faramox (1/2) 200 400 Co-Amoxiclav. (1/3) 156(125+31) 312(250+62) Farmentin (1/2) 228(200+28) 456(400+56)

Duration of therapy � For children ≥ 6 years of age with mild to moderate disease 5 -7 days is appropriate � For younger children and for children with severe disease, a standard 10 -day course is recommended
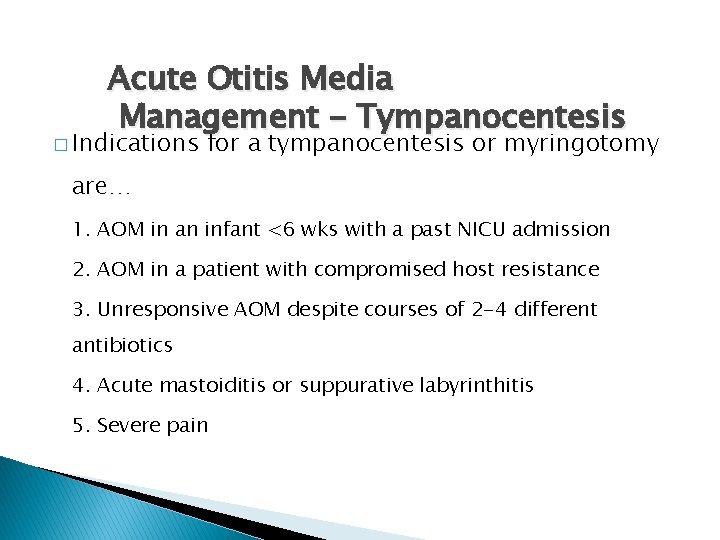
Acute Otitis Media Management - Tympanocentesis � Indications for a tympanocentesis or myringotomy are… 1. AOM in an infant <6 wks with a past NICU admission 2. AOM in a patient with compromised host resistance 3. Unresponsive AOM despite courses of 2 -4 different antibiotics 4. Acute mastoiditis or suppurative labyrinthitis 5. Severe pain

Algorithm to distinguish AOM from OME

Malpractice � Administering PCN 6: 3: 3 in treatment � Decongestants may decreased blood flow to the respiratory mucosa, which may impair delivery of antibiotics � Antihistamines ear effusion may prolong the duration of middle

Prevention � Continue possible exclusive breastfeeding as long as ◦ NO taking a bottle to bed � Smoke-free environment � IF high-risk for recurrent acute otitis media ◦ Prolonged courses of antimicrobial prophylaxis �Amoxicillin (20 to 30 mg/kg/day) given once daily at bedtime for 3 to 6 months or longer � Pneumococcal vaccine & influenza vaccine marginally benefit ◦ Pneumococcal vaccine reduce all otitis media by 6%.

Management of Recurrent Acute Otitis Media �A child has recurrent acute otitis media (RAOM) when 3 new episodes of AOM have occurred in 6 months or 4 episodes within 12 months. Approximately 20% of children younger than two years of age have RAOM. � � Follow patients with RAOM monthly with otoscopy, as AOM episodes are often asymptomatic. � Consider obtaining audiologic and speech evaluations in these cases
Ventilating Tubes with or without Adenoidectomy �Ventilating tubes are indicated when a child has experienced 5 or more new AOM episodes within 12 months. �In selected patients, especially those with associated otitis media with effusion, performing an adenoidectomy as well as inserting tubes may reduce the likelihood of ventilating tube reinsertions and additional otitis media related hospitalizations.

THANKS FOR ATTENTION
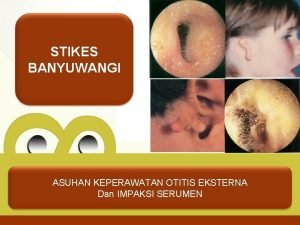
 Acute suppurative otitis media
Acute suppurative otitis media Acute diffuse otitis externa
Acute diffuse otitis externa 09112007 color
09112007 color Clasificación de la otitis media
Clasificación de la otitis media Clasificación de la otitis media
Clasificación de la otitis media Adhesive otitis media
Adhesive otitis media Icd 10 vertigo
Icd 10 vertigo Nonsuppurative otitis media
Nonsuppurative otitis media External auditory meatus
External auditory meatus Tympanosclerosis
Tympanosclerosis Fluid in ears
Fluid in ears Wikimedia
Wikimedia Serous otitis media
Serous otitis media Otitis media with effusion otoscopy
Otitis media with effusion otoscopy Tímpano
Tímpano Otitis media complications
Otitis media complications Otitis media ppt
Otitis media ppt Nursing diagnosis for otitis media slideshare
Nursing diagnosis for otitis media slideshare Classification of otitis media
Classification of otitis media Myringotomy post op nursing interventions
Myringotomy post op nursing interventions Streptococcus pneumoniae otitis media
Streptococcus pneumoniae otitis media Otitis media ppt
Otitis media ppt Oma vs ome
Oma vs ome Otitis eksterna difusa icd 10
Otitis eksterna difusa icd 10 Otitis externa wiki
Otitis externa wiki Coloboma auris
Coloboma auris Sufijo de ropero
Sufijo de ropero Scalp salinizado
Scalp salinizado Askep otitis eksterna
Askep otitis eksterna Otitis
Otitis Differential diagnosis of otitis externa
Differential diagnosis of otitis externa Otitis externa circunscrita
Otitis externa circunscrita Sudeep doshi
Sudeep doshi Name 2 objects with acute angles
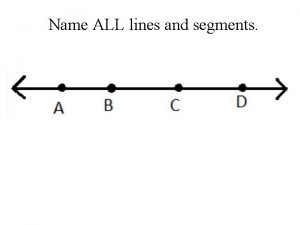
Name 2 objects with acute angles Name three line segments
Name three line segments Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc cc
V cc cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak