In term uncomplicated pregnancies can intrapartum fetal compromise
- Slides: 1
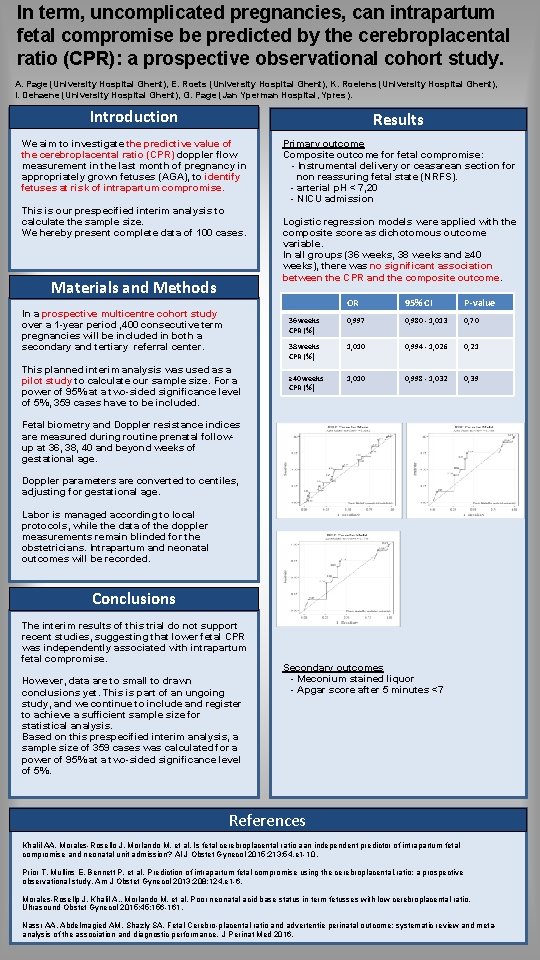
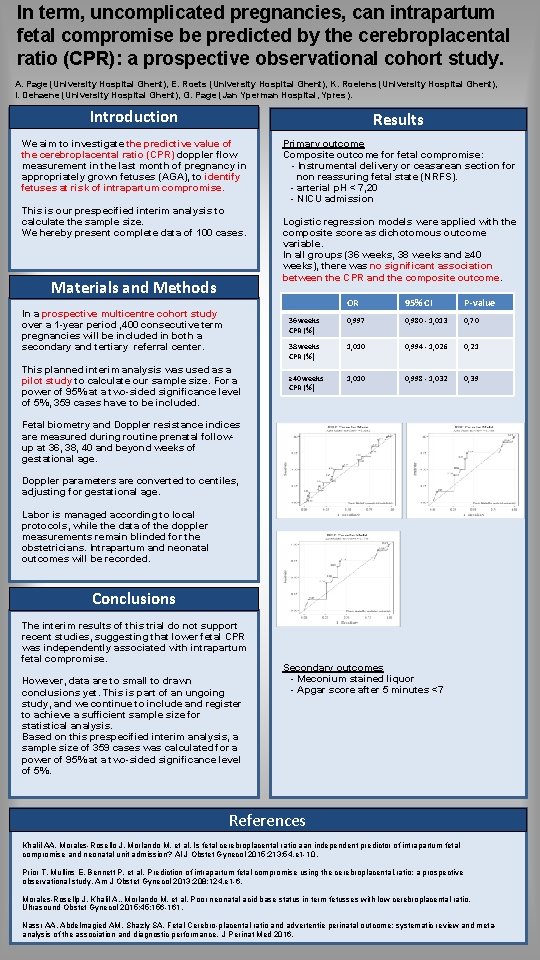
In term, uncomplicated pregnancies, can intrapartum fetal compromise be predicted by the cerebroplacental ratio (CPR): a prospective observational cohort study. A. Page (University Hospital Ghent), E. Roets (University Hospital Ghent), K. Roelens (University Hospital Ghent), I. Dehaene (University Hospital Ghent), G. Page (Jan Yperman Hospital, Ypres). Introduction Results We aim to investigate the predictive value of the cerebroplacental ratio (CPR) doppler flow measurement in the last month of pregnancy in appropriately grown fetuses (AGA), to identify fetuses at risk of intrapartum compromise. Primary outcome Composite outcome for fetal compromise: - Instrumental delivery or ceasarean section for non reassuring fetal state (NRFS). - arterial p. H < 7, 20 - NICU admission This is our prespecified interim analysis to calculate the sample size. We hereby present complete data of 100 cases. Materials and Methods In a prospective multicentre cohort study over a 1 -year period , 400 consecutive term pregnancies will be included in both a secondary and tertiary referral center. This planned interim analysis was used as a pilot study to calculate our sample size. For a power of 95% at a two-sided significance level of 5%, 359 cases have to be included. Logistic regression models were applied with the composite score as dichotomous outcome variable. In all groups (36 weeks, 38 weeks and ≥ 40 weeks), there was no significant association between the CPR and the composite outcome. OR 95% CI P-value 36 weeks CPR (%) 0, 997 0, 980 - 1, 013 0, 70 38 weeks CPR (%) 1, 010 0, 994 - 1, 026 0, 21 ≥ 40 weeks CPR (%) 1, 010 0, 998 - 1, 032 0, 39 Fetal biometry and Doppler resistance indices are measured during routine prenatal followup at 36, 38, 40 and beyond weeks of gestational age. Doppler parameters are converted to centiles, adjusting for gestational age. Labor is managed according to local protocols, while the data of the doppler measurements remain blinded for the obstetricians. Intrapartum and neonatal outcomes will be recorded. Conclusions The interim results of this trial do not support recent studies, suggesting that lower fetal CPR was independently associated with intrapartum fetal compromise. However, data are to small to drawn conclusions yet. This is part of an ungoing study, and we continue to include and register to achieve a sufficient sample size for statistical analysis. Based on this prespecified interim analysis, a sample size of 359 cases was calculated for a power of 95% at a two-sided significance level of 5%. Secondary outcomes - Meconium stained liquor - Apgar score after 5 minutes <7 References Khalil AA, Morales-Rosello J, Morlando M, et al. Is fetal cerebroplacental ratio aan independent predictor of intrapartum fetal compromise and neonatal unit admission? Al J Obstet Gynecol 2015; 213: 54. e 1 -10. Prior T, Mullins E, Bennett P, et al. Prediction of intrapartum fetal compromise using the cerebroplacental, ratio: a prospective observational study. Am J Obstet Gynecol 2013; 208: 124. e 1 -6. Morales-Rosellp J, Khalil A. , Morlando M, et al. Poor neonatal acid base status in term fetusses with low cerebroplacental ratio. Ultrasound Obstet Gynecol 2015; 45: 156 -161. Nassr AA, Abdelmagied AM, Shazly SA. Fetal Cerebro-placental ratio and advertentie perinatal outcome: systematic review and metaanalysis of the association and diagnostic performance. J Perinat Med 2016.