Improving Your Practice Safety Culture Aims Why is




- Slides: 39
Improving Your Practice Safety Culture
Aims • Why is “safety culture” important? . . . . what does this mean? ? • How can we develop our safety culture/does it need developing? • Using “Safequest”

What is Safety Culture?
Safety Culture “Individual and group values, attitudes, perceptions and patterns of behaviour that determine their commitment to safety management” The way things are done around here NHS Education for Scotland 2010
Why is a strong Safety Culture Important? A strong safety culture essential to safe reliable care in any workplace
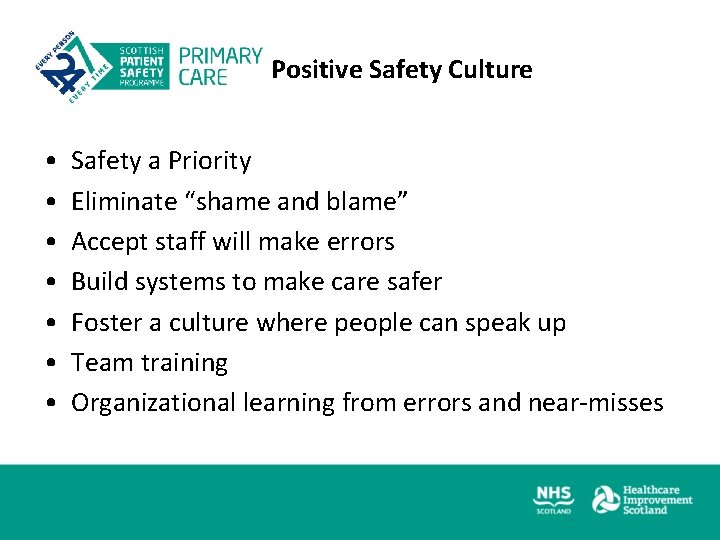
Positive Safety Culture • • Safety a Priority Eliminate “shame and blame” Accept staff will make errors Build systems to make care safer Foster a culture where people can speak up Team training Organizational learning from errors and near-misses
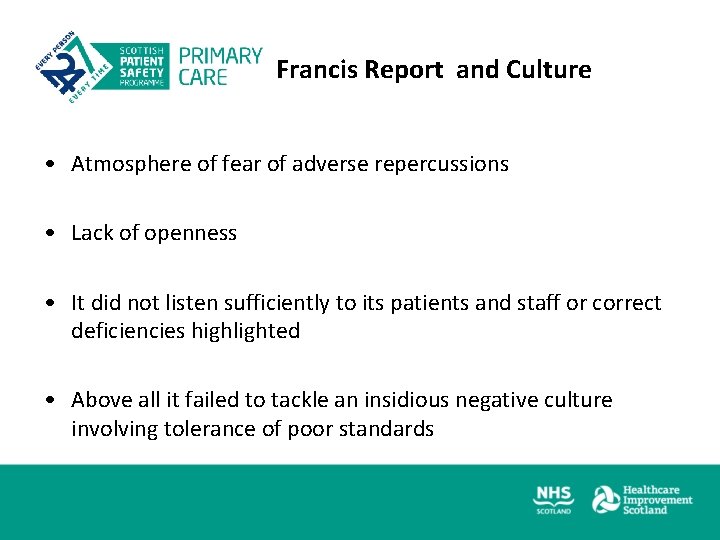
Francis Report and Culture • Atmosphere of fear of adverse repercussions • Lack of openness • It did not listen sufficiently to its patients and staff or correct deficiencies highlighted • Above all it failed to tackle an insidious negative culture involving tolerance of poor standards
Developing your Safety Culture • • • Understanding its importance Thinking about it Measuring your culture Discussing it and reflecting on results Focussed action to Improve it
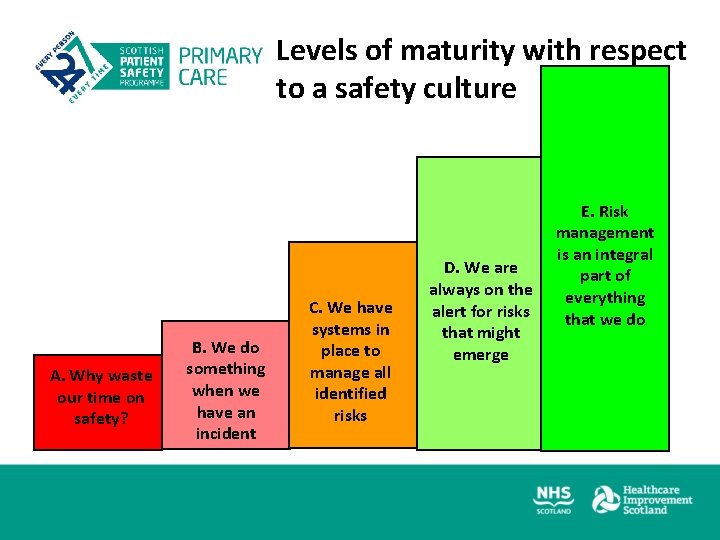
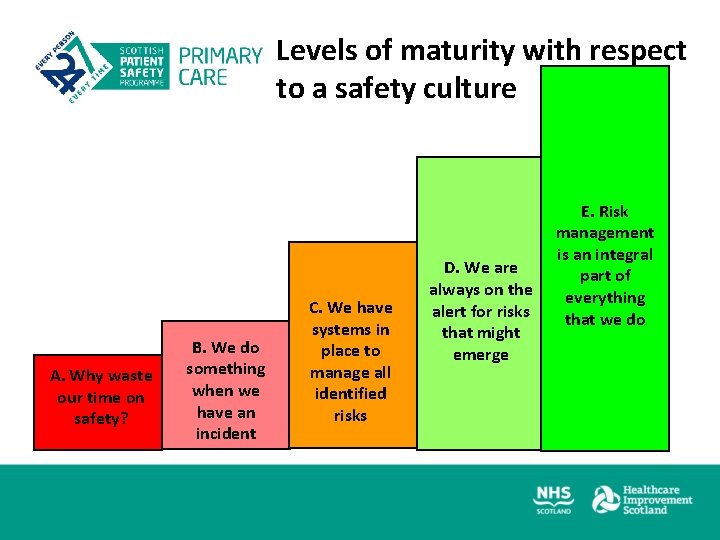
Levels of maturity with respect to a safety culture A. Why waste our time on safety? B. We do something when we have an incident C. We have systems in place to manage all identified risks D. We are always on the alert for risks that might emerge E. Risk management is an integral part of everything that we do
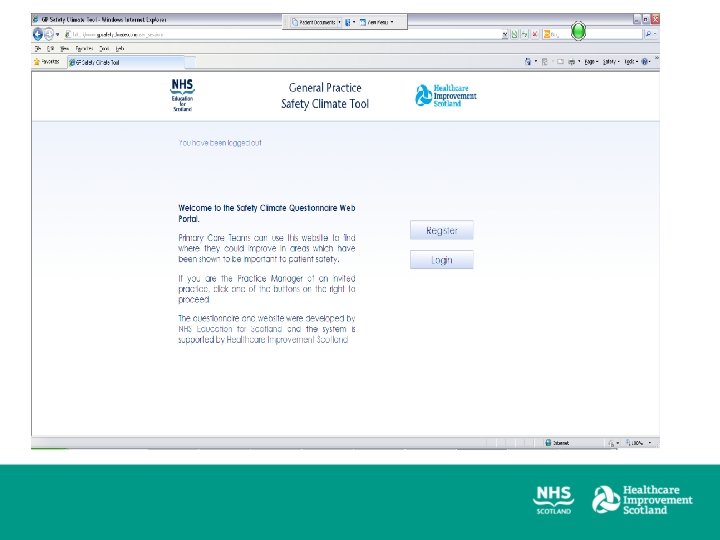
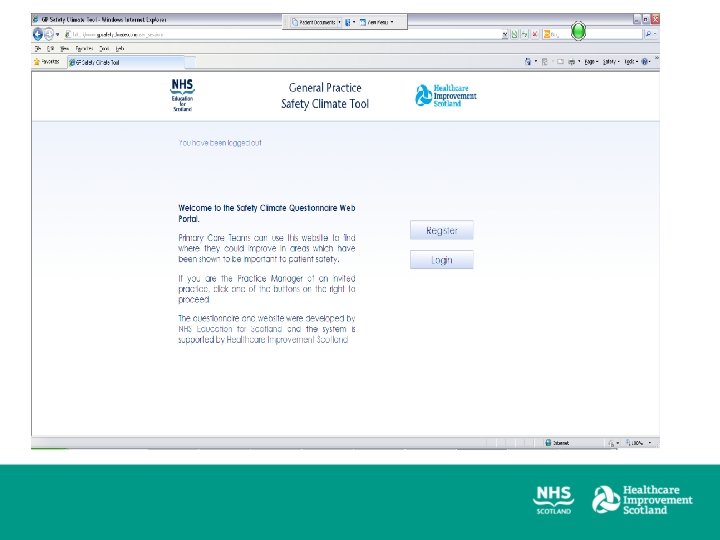
Using the Safe. Quest Safety Climate Survey work in practice?
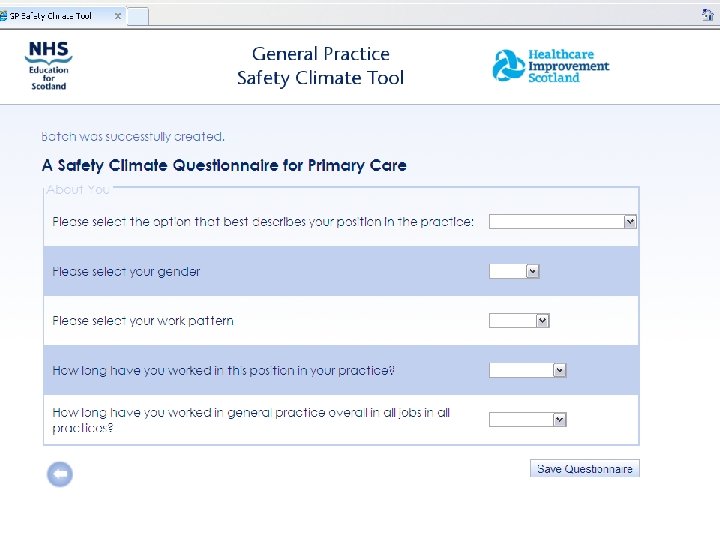
Safety Climate Survey • • • On line Practice centred Measurement Diagnosis Catalyst for change
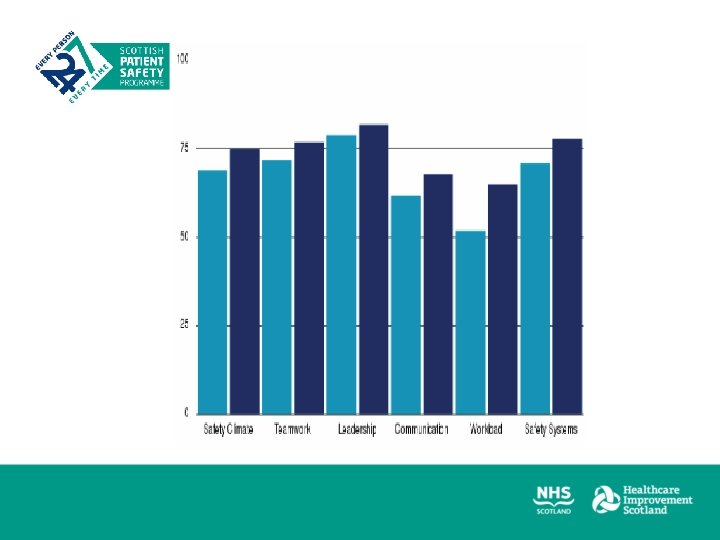
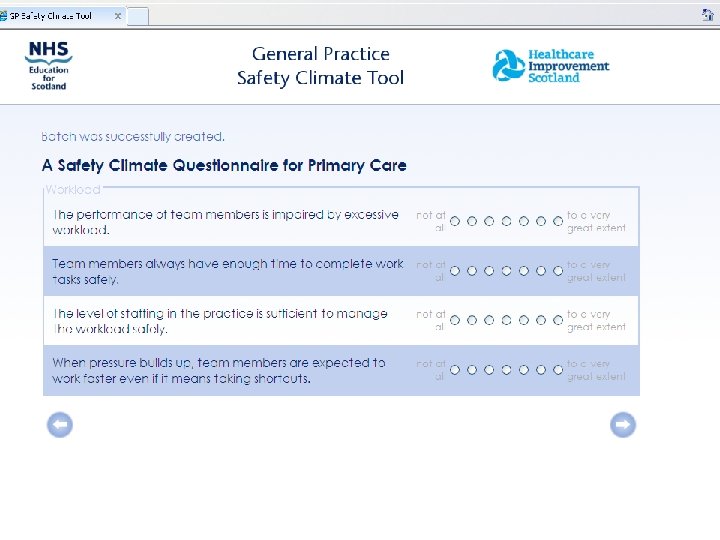
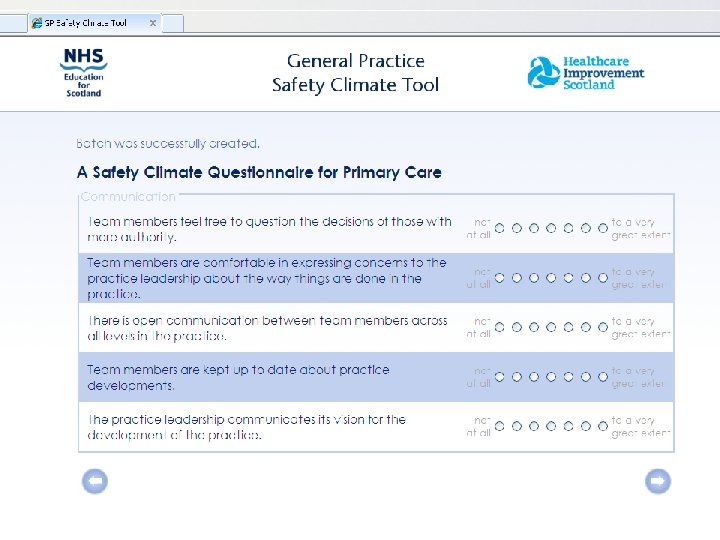
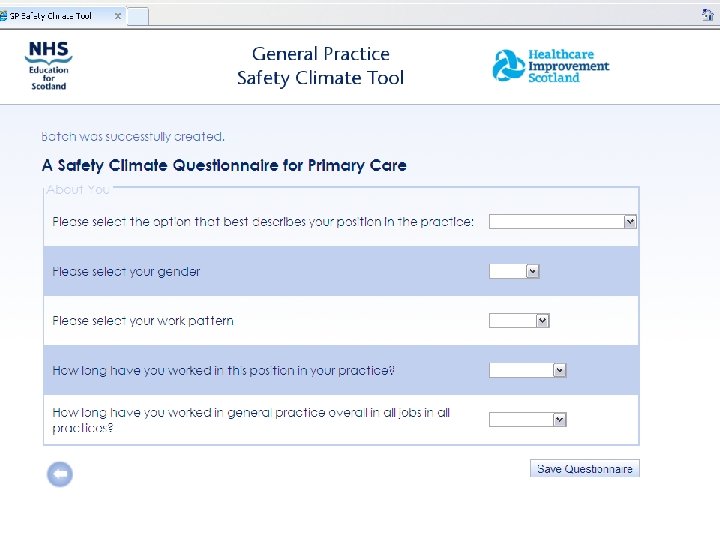
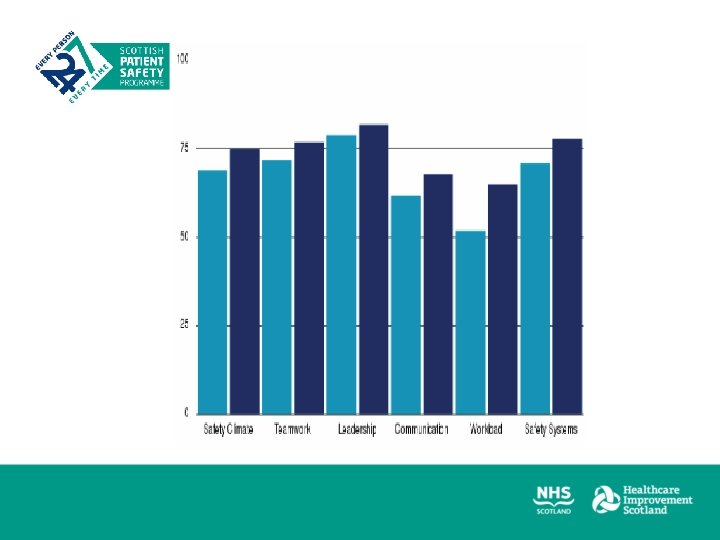
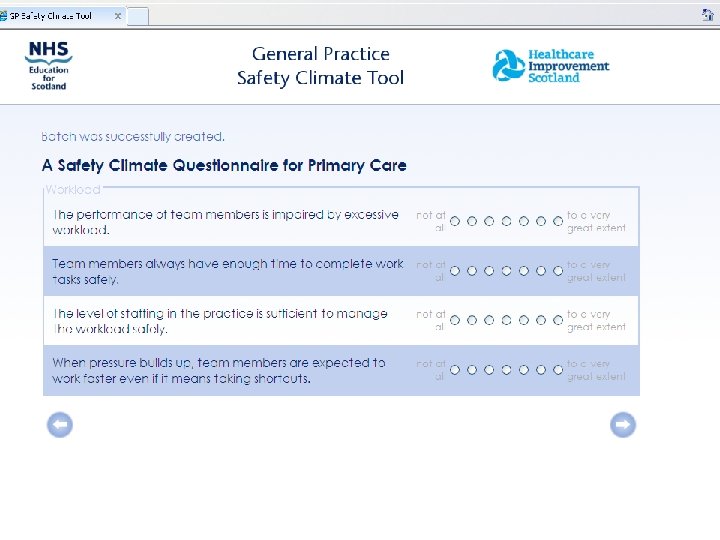
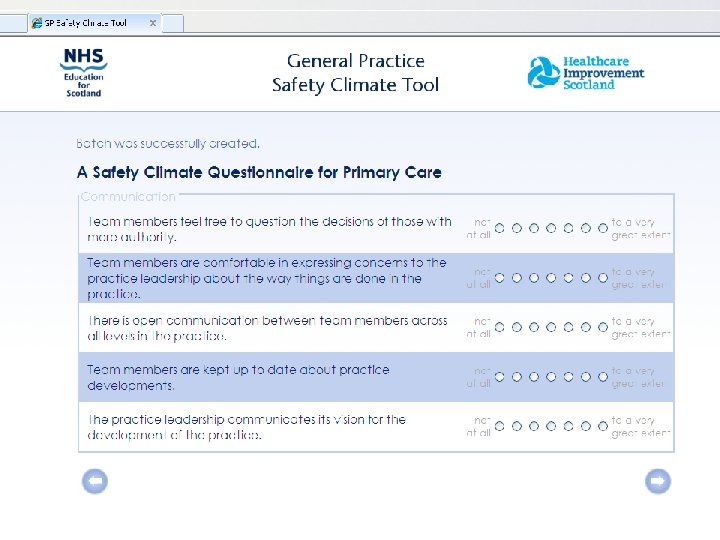
Areas of Focus: • Teamwork • Workload • Communication • Leadership • Safety systems and learning
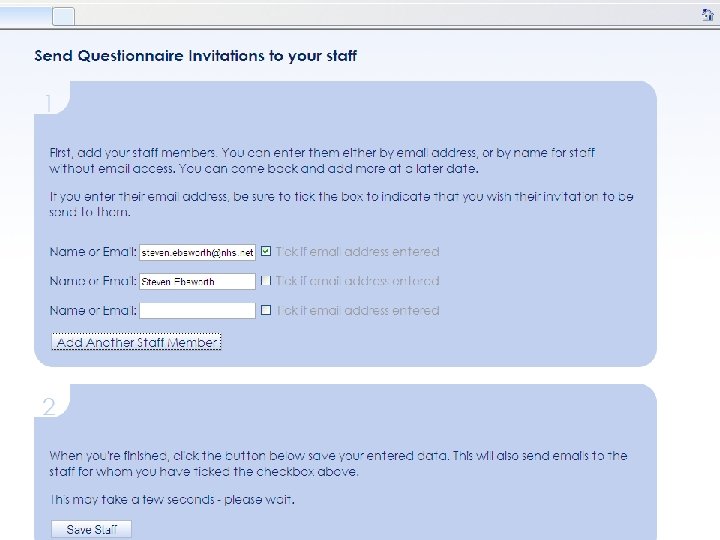
Process Plan Distribute Complete Review Discuss Change
Process PLAN DO STUDY ACT Plan Distribute Complete Review Discuss Change
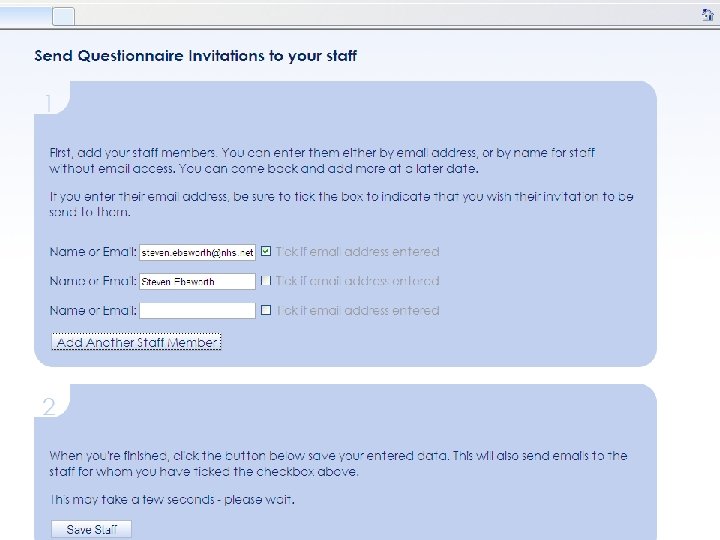
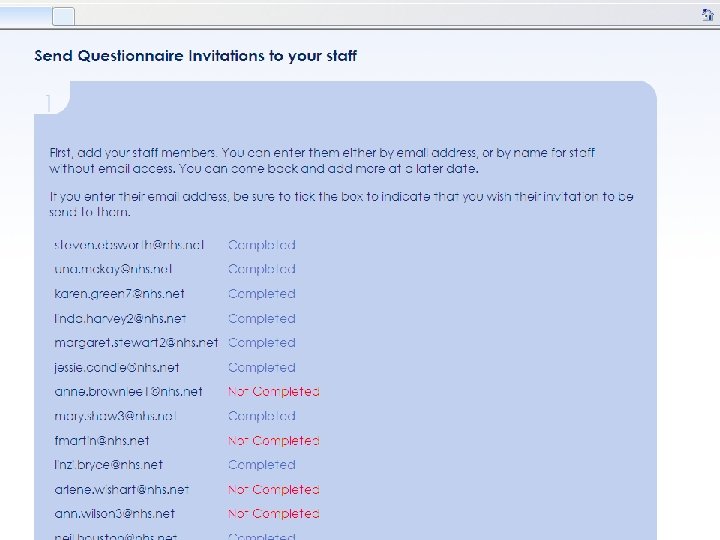
Process Plan Distribute - ? involve “locality managers” Complete

Negative Questions • The Performance of the team is impaired by excessive workload* • When pressure builds up team members are expected to work faster even if it means taking shortcuts* • Where negative questions* results have been reversed and a high score is therefore desirable • Watch out for these ones – can be confusing within report.
What to do with the report? • Close survey when all have completed • Download / Print off • Distribute to all team • Arrange meeting to discuss findings
Sample Report • Have a look at the report • What does it show you? • What questions does it raise? • What questions do you have?
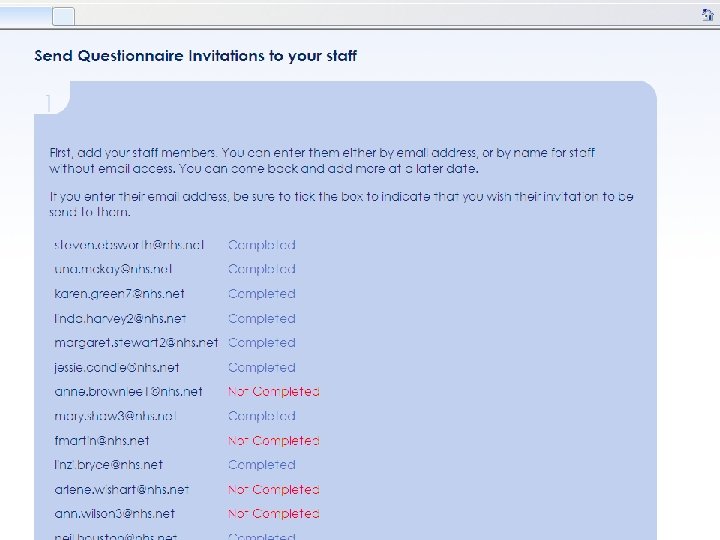
Making the most of your Results • • Identify uptake – is this telling you something? Identify positive/negative elements of culture Look in detail at the questions/areas where you might improve Compare to other practices Compare between staff groups Compare with previous results , if repeating Summarize – Complete QOF summary sheet and Action plan • Links via Refhelp to HIS site - help facilitate discussion!


Group Discussion • What would be the benefits and challenges of completing and discussing the safety climate survey
Insights • “Many of us in the practice staff hadn’t really made the link that us failing to communicate in was a threat to patient safety …. we had a lot of really good stuff came out of it, a lot of very open discussion”
Positive Change Increased frequency of staff meetings. At least one doctor to attend staff meeting. Increased communication over a variety of issues. Newsletter/minutes after each meeting. Quarterly meeting involving whole practice.
Quotes from Practice “ it did sound good, being able to ask questions and get answers straight away from Drs/or receiving instructions etc instead of going through a third party” “beneficial. . encouraged to speak out if you think something isn’t right"
Key points The findings are for your practice teams (consider carefully though) • “Employees”/NHSB staff etc. Don’t get too focused on the numbers Concentrate on how you might use the results to “drive improvements” • Key issue • Emphasis on change/improvement, if needed
Key Points • It’s a tool, a “snapshot” • Discuss, Reflect and Change as a practice team • Takes time to change • Important to repeat • Present in QOF • Specifies 2 x cycles
QOF • Annually • Practice teams • Discuss • Action Plan • Reflection Sheet
Reflection Sheet • What positive aspects of your team’s safety culture were highlighted in the report and your discussions? • What aspects of your safety culture do you as a team feel you could improve? • What steps will you take to improve these aspects of your safety culture? • What else might you change to improve your safety culture? • Would you like any support or guidance to make changes in your practice? If so, what would be useful?
Relevant Links……. . • http: //www. healthcareimprovementscotland. org/our_work/patient_safet y/spsp_primary_care_resources/safety_climate_survey. aspx • Interpretation guides/FAQs/link to safequest • http: //www. sehd. scot. nhs. uk/pca/PCA 2013(M)02 guide. pdf • Qo. F 2013/14 Guidance, section 6 ii QI domain • http: //www. refhelp-borders. scot. nhs. uk/ • See Primary care/GP contract/Patient safety