Improving Validity of Advance Care Planning Documentation Names
- Slides: 24
Improving Validity of Advance Care Planning Documentation Names: David Cheng MD and Sarah Fairbrook NP Mentor: Irene Yeh MD MPH Institution: Dana Farber Cancer Institute Date: 2/3/2017 Keywords: advance care planning, MOLST, medical orders for life-sustaining treatment, documentation, validity, hospital, communication
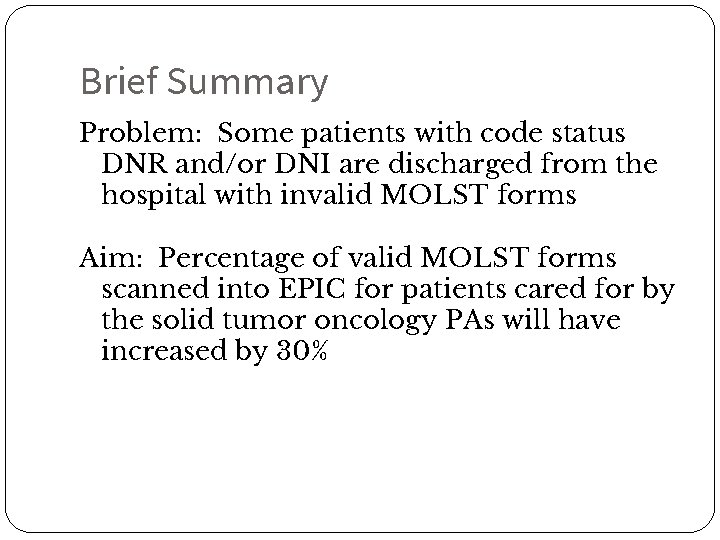
Brief Summary Problem: Some patients with code status DNR and/or DNI are discharged from the hospital with invalid MOLST forms Aim: Percentage of valid MOLST forms scanned into EPIC for patients cared for by the solid tumor oncology PAs will have increased by 30%
Intervention 20 minute educational session with Onc PAs -Activity identifying invalid MOLST forms -Check list handout with necessary components of a valid MOLST -Discussion of workflow barriers and brainstorming solutions
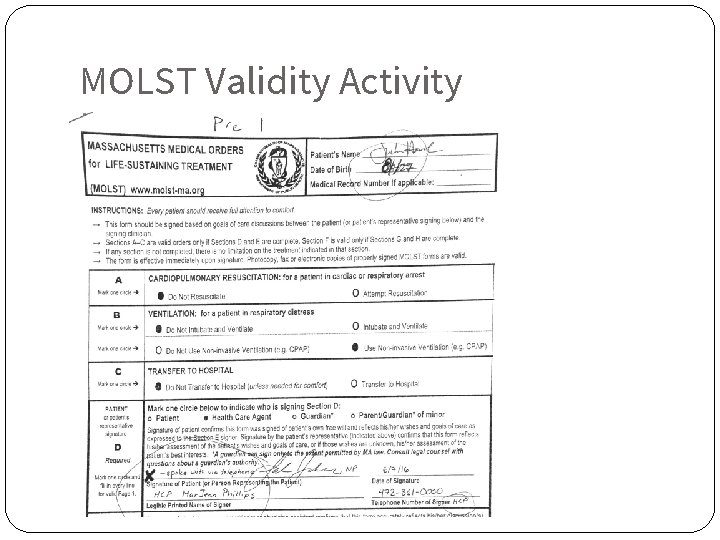
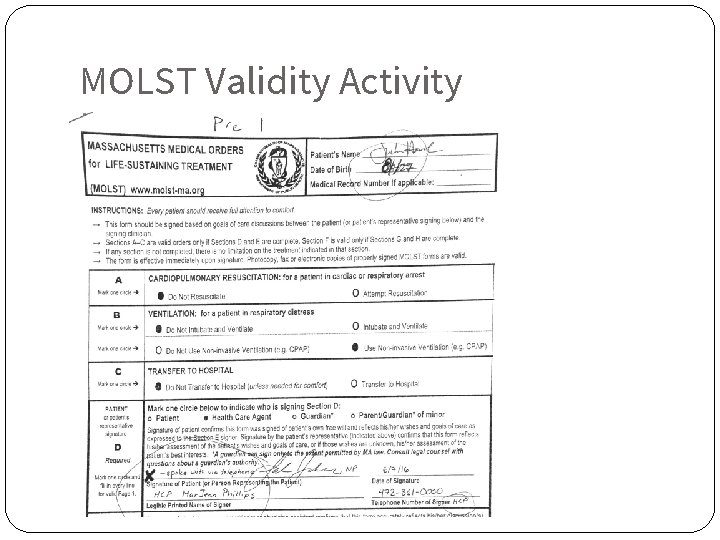
MOLST Validity Activity
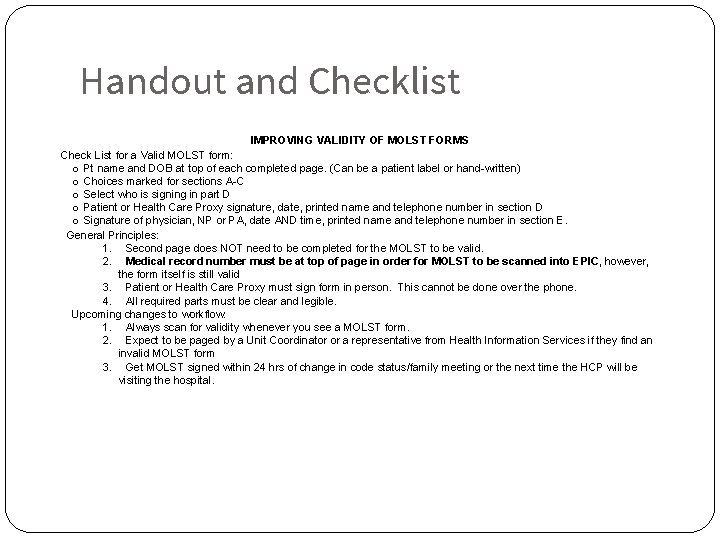
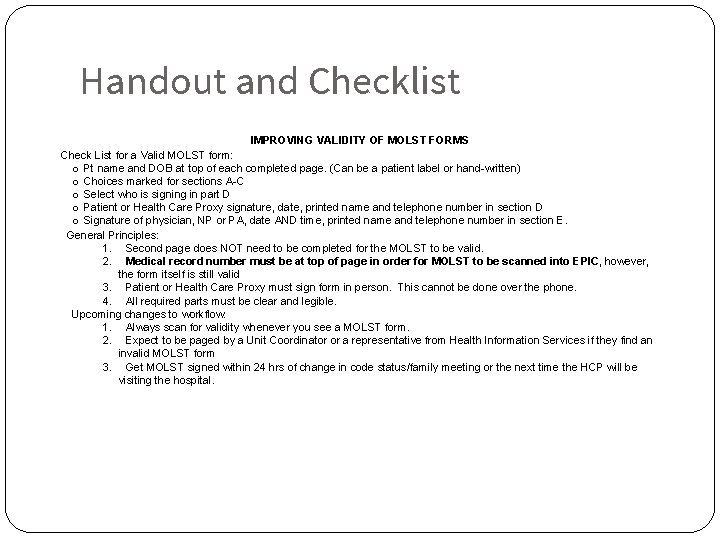
Handout and Checklist IMPROVING VALIDITY OF MOLST FORMS Check List for a Valid MOLST form: o Pt name and DOB at top of each completed page. (Can be a patient label or hand-written) o Choices marked for sections A-C o Select who is signing in part D o Patient or Health Care Proxy signature, date, printed name and telephone number in section D o Signature of physician, NP or PA, date AND time, printed name and telephone number in section E. General Principles: 1. Second page does NOT need to be completed for the MOLST to be valid. 2. Medical record number must be at top of page in order for MOLST to be scanned into EPIC, however, the form itself is still valid 3. Patient or Health Care Proxy must sign form in person. This cannot be done over the phone. 4. All required parts must be clear and legible. Upcoming changes to workflow: 1. Always scan for validity whenever you see a MOLST form. 2. Expect to be paged by a Unit Coordinator or a representative from Health Information Services if they find an invalid MOLST form 3. Get MOLST signed within 24 hrs of change in code status/family meeting or the next time the HCP will be visiting the hospital.
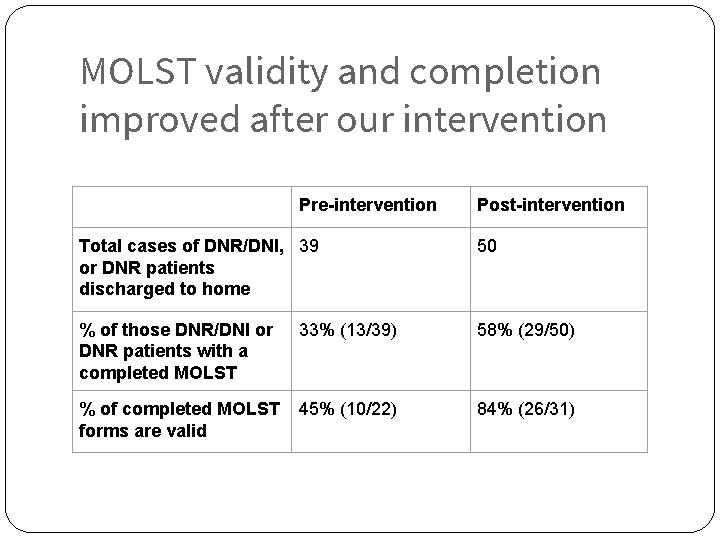
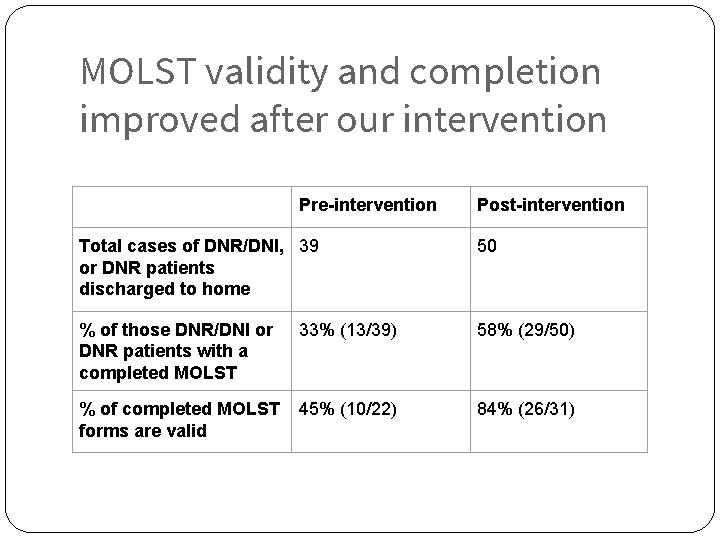
MOLST validity and completion improved after our intervention Pre-intervention Post-intervention Total cases of DNR/DNI, 39 or DNR patients discharged to home 50 % of those DNR/DNI or DNR patients with a completed MOLST 33% (13/39) 58% (29/50) % of completed MOLST forms are valid 45% (10/22) 84% (26/31)
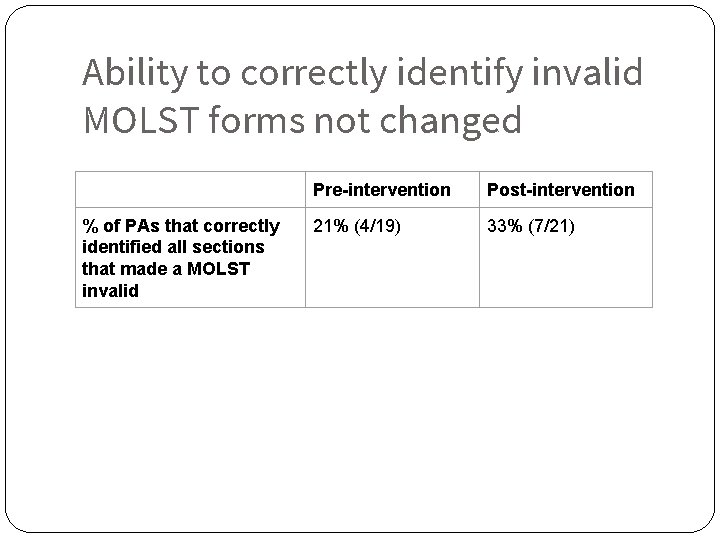
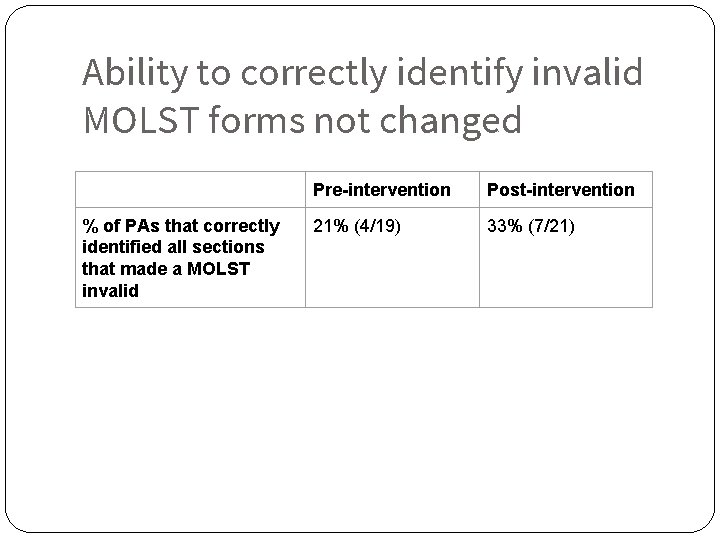
Ability to correctly identify invalid MOLST forms not changed % of PAs that correctly identified all sections that made a MOLST invalid Pre-intervention Post-intervention 21% (4/19) 33% (7/21)
Limitations ●Pre/post-test doesn’t measure ability to complete a valid MOLST form ● What invalidates a MOLST form is not clear ● PA-only service ●Reproducibility of our intervention ● Scalability limited
Next steps ●Repeat intervention to capture housestaff and other PA services ●Exercise to fill out blank MOLST form ●Use of pre/post-testing as reinforcement of knowledge, not as data source ● Committee is in process of re-designing MOLST forms ● Electronic MOLST forms
Conclusion Completion of MOLST forms require system-wide cooperation Clinicians are key-stakeholders in ensuring the validity of completed MOLST forms A brief educational intervention can dramatically improve the number of valid completed MOLST forms
Thank you! ●Coach ●Irene Yeh MD MPH – Palliative Care Attending Physician ● Team Members: ● Erica Morelli PA – Oncology Physician Assistant ● Sean Kukauskas NRP – Director Ambulance Services, Spaulding Rehabilitation Network ● Henry Su - medical student 11
BREAKER SLIDE 12
Problem Statement ● Advance care planning is an essential component of maintaining continuity in a patient’s care ● Invalid MOLST forms are one way in which communication breakdowns occur in transitions of care. ● If a MOLST form is invalid and a patient dies, full resuscitative measures will be attempted, undermining a patient’s autonomy and end-of-life preferences. 13
AIM Statement ● By January 2017, the percentage of valid 14 MOLST forms scanned into EPIC for patients cared for by the solid tumor oncology PAs will have increased by 30%. ● By January 2017, the percentage of completed MOLST forms for patients with DNR and/or DNI code status will increase by 30%. ● PAs will improve ability to identify invalid MOLST forms as evidenced by improvement of 15% from pre-test to posttest score.
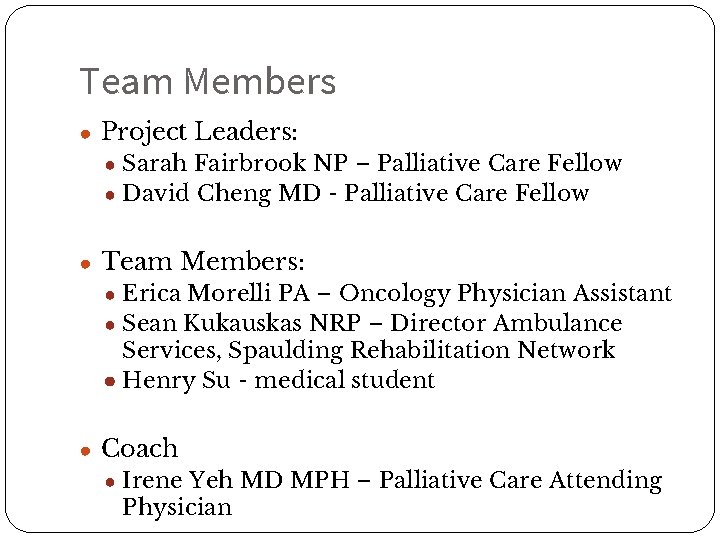
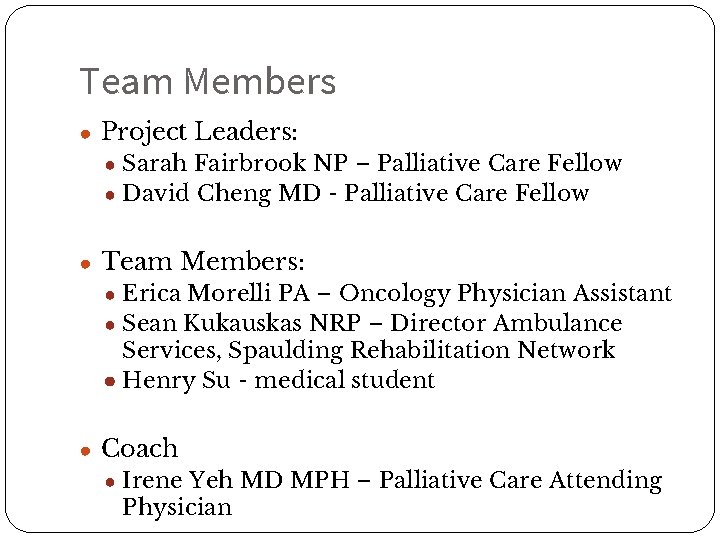
Team Members ● Project Leaders: ● Sarah Fairbrook NP – Palliative Care Fellow ● David Cheng MD - Palliative Care Fellow ● Team Members: ● Erica Morelli PA – Oncology Physician Assistant ● Sean Kukauskas NRP – Director Ambulance Services, Spaulding Rehabilitation Network ● Henry Su - medical student ● Coach ● Irene Yeh MD MPH – Palliative Care Attending 15 Physician
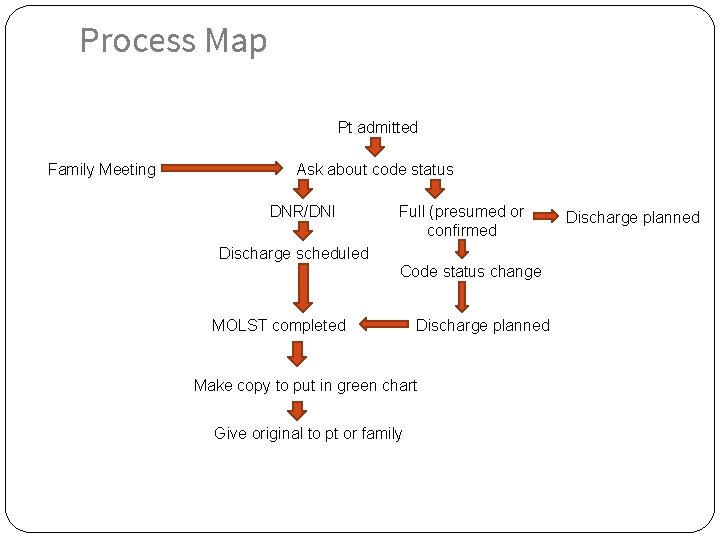
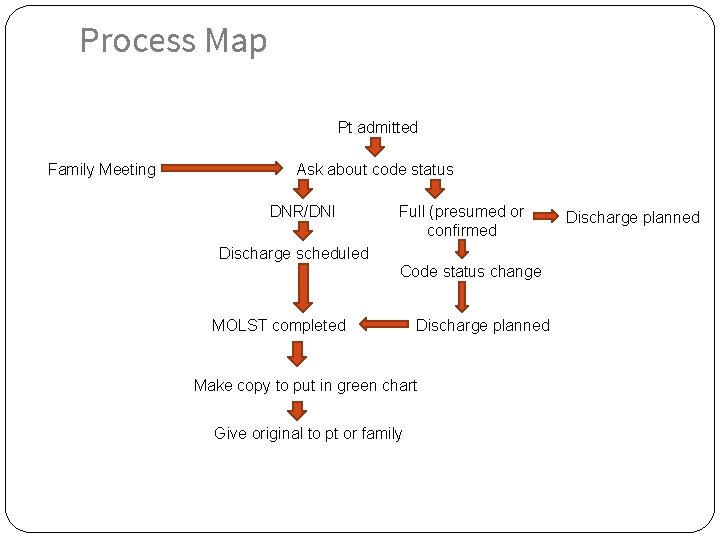
Process Map Pt admitted Family Meeting Ask about code status DNR/DNI Full (presumed or confirmed Discharge scheduled Code status change MOLST completed Discharge planned Make copy to put in green chart Give original to pt or family 16 Discharge planned
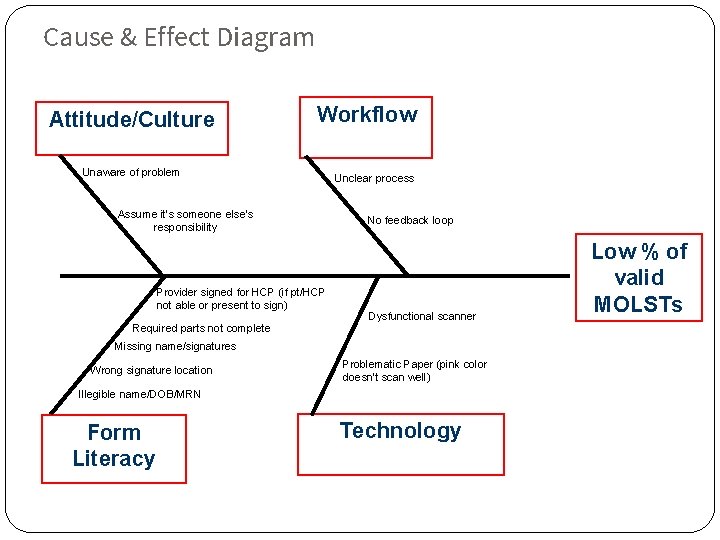
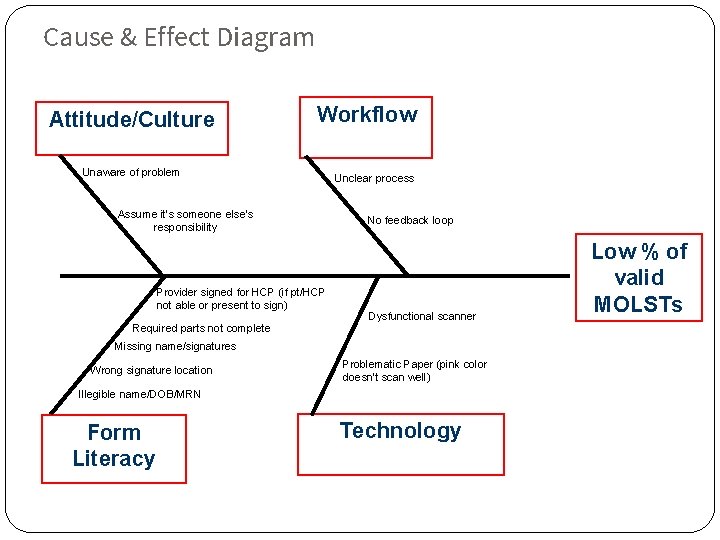
Cause & Effect Diagram Attitude/Culture Workflow Unaware of problem Assume it’s someone else’s responsibility Provider signed for HCP (if pt/HCP not able or present to sign) Required parts not complete Unclear process No feedback loop Dysfunctional scanner Missing name/signatures Wrong signature location Problematic Paper (pink color doesn’t scan well) Illegible name/DOB/MRN Form Literacy 17 Technology Low % of valid MOLSTs
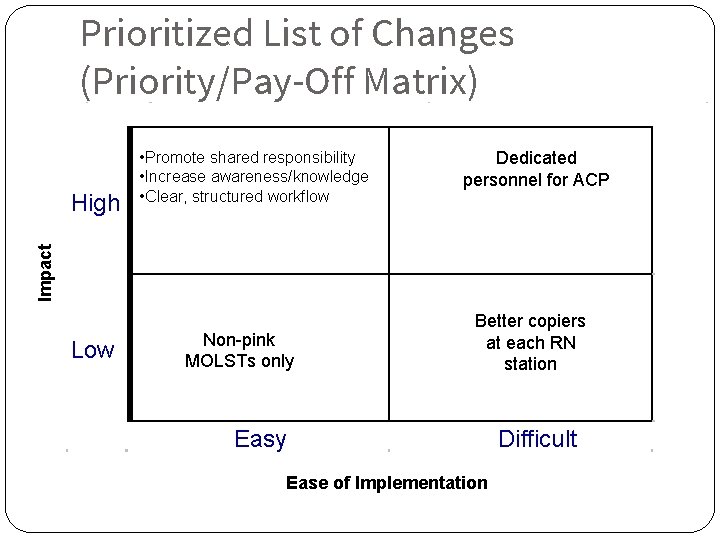
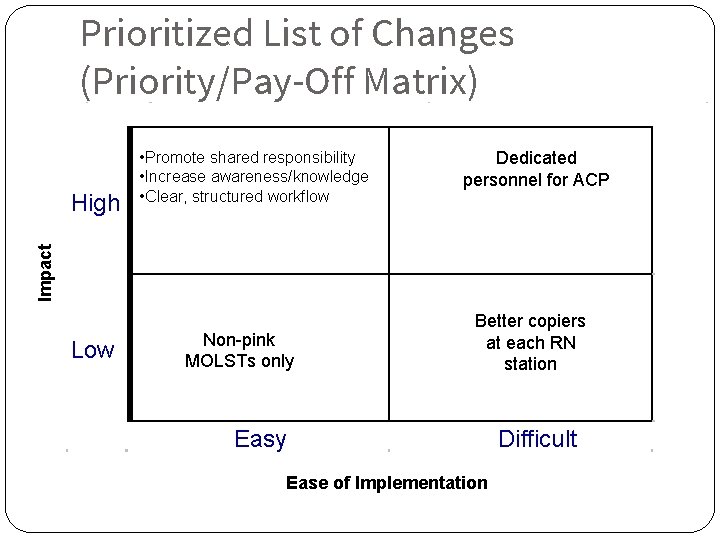
Prioritized List of Changes (Priority/Pay-Off Matrix) Dedicated personnel for ACP Impact High • Promote shared responsibility • Increase awareness/knowledge • Clear, structured workflow Low Non-pink MOLSTs only Better copiers at each RN station Easy Ease of Implementation 18 18 Difficult
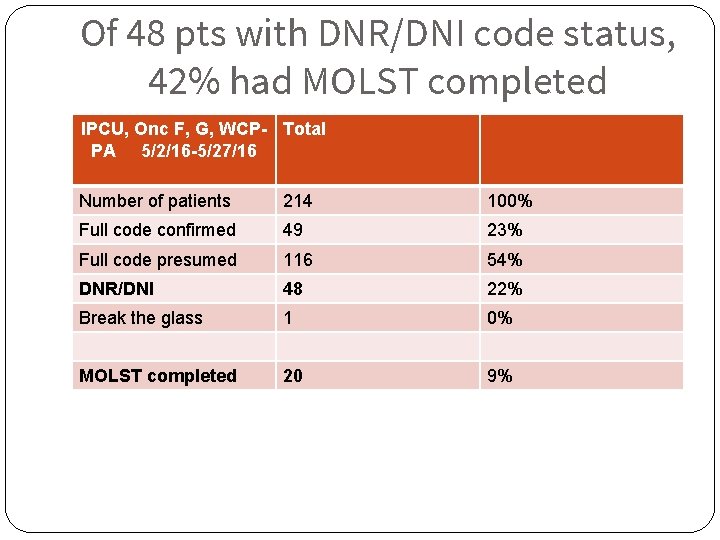
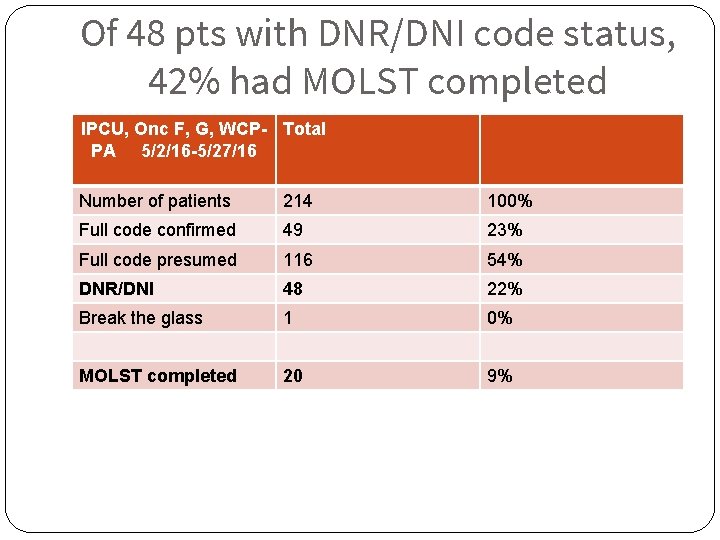
Of 48 pts with DNR/DNI code status, 42% had MOLST completed IPCU, Onc F, G, WCP- Total PA 5/2/16 -5/27/16 19 Number of patients 214 100% Full code confirmed 49 23% Full code presumed 116 54% DNR/DNI 48 22% Break the glass 1 0% MOLST completed 20 9%
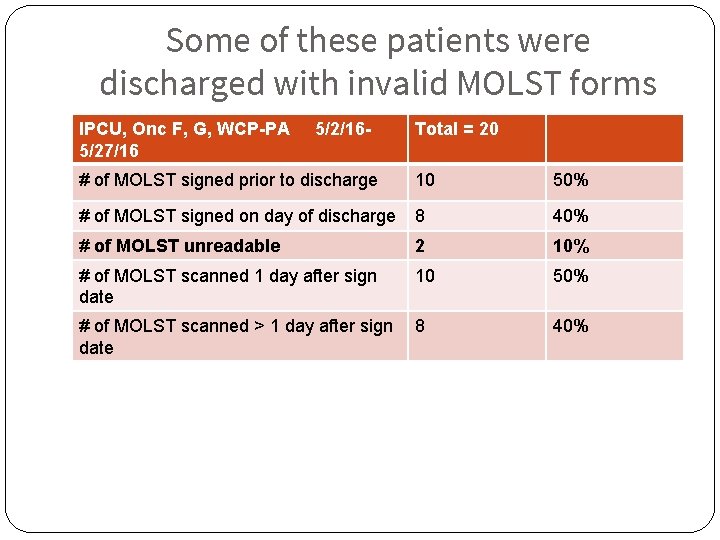
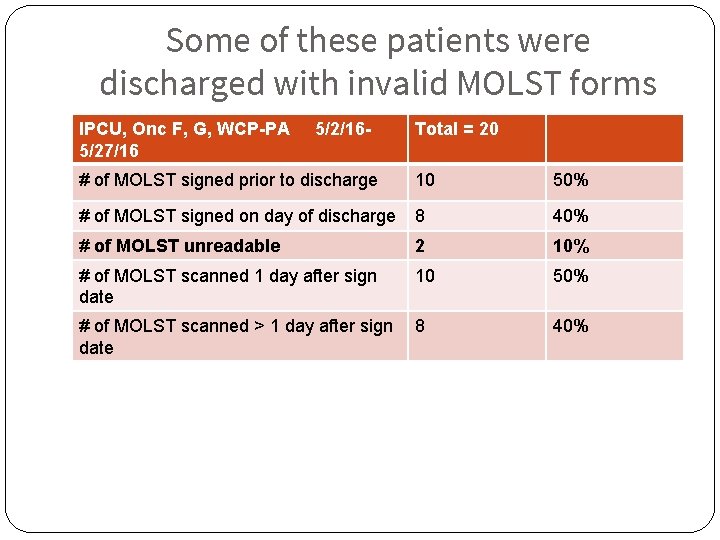
Some of these patients were discharged with invalid MOLST forms IPCU, Onc F, G, WCP-PA 5/27/16 20 5/2/16 - Total = 20 # of MOLST signed prior to discharge 10 50% # of MOLST signed on day of discharge 8 40% # of MOLST unreadable 2 10% # of MOLST scanned 1 day after sign date 10 50% # of MOLST scanned > 1 day after sign date 8 40%
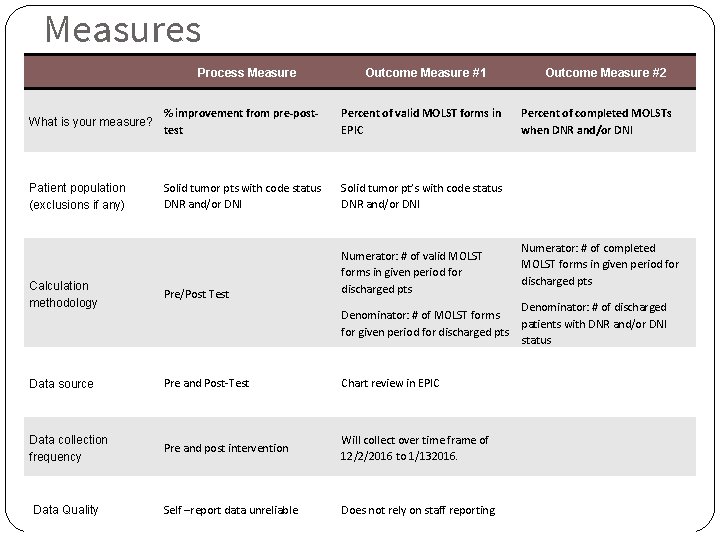
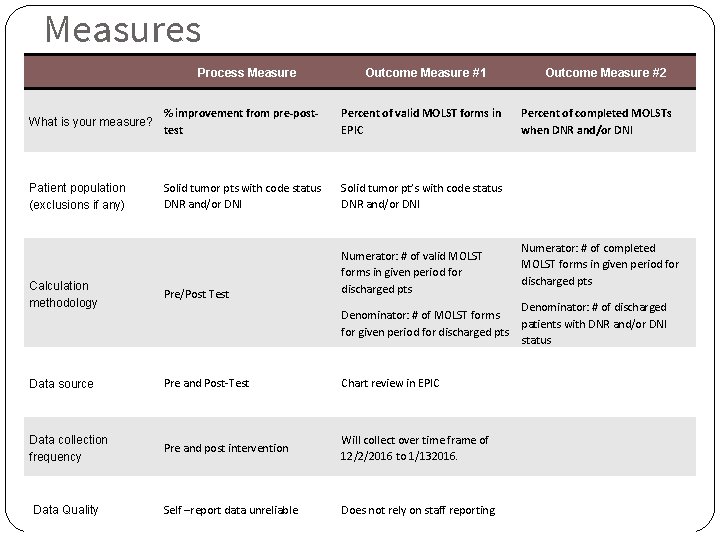
Measures Process Measure Outcome Measure #1 What is your measure? % improvement from pre-posttest Percent of valid MOLST forms in EPIC Patient population (exclusions if any) Solid tumor pts with code status DNR and/or DNI Solid tumor pt’s with code status DNR and/or DNI Calculation methodology Pre/Post Test Numerator: # of valid MOLST forms in given period for discharged pts Data source Pre and Post-Test Chart review in EPIC Data collection frequency Pre and post intervention Will collect over time frame of 12/2/2016 to 1/132016. Self –report data unreliable Does not rely on staff reporting 21 Data Quality Denominator: # of MOLST forms for given period for discharged pts Outcome Measure #2 Percent of completed MOLSTs when DNR and/or DNI Numerator: # of completed MOLST forms in given period for discharged pts Denominator: # of discharged patients with DNR and/or DNI status
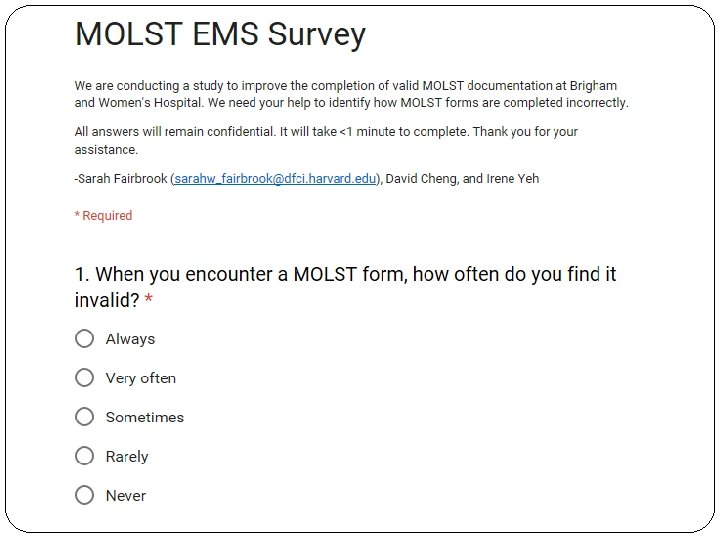
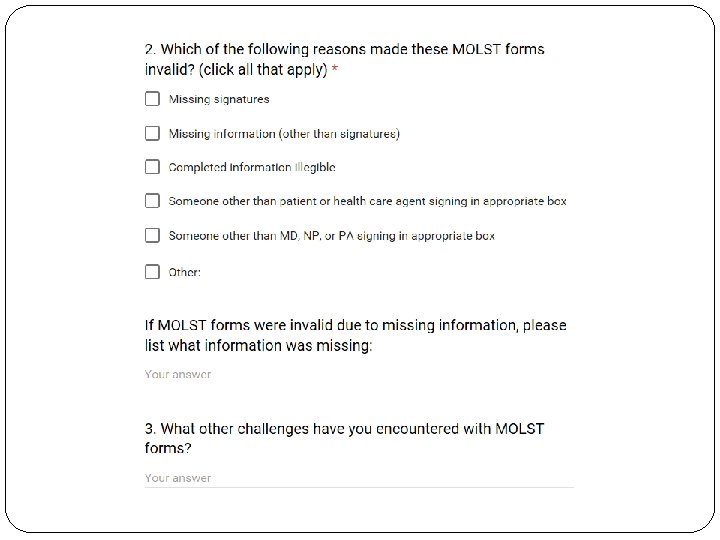
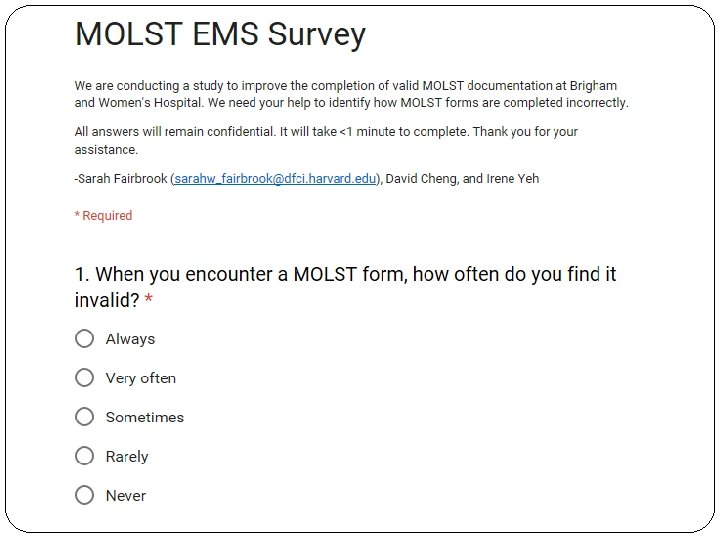
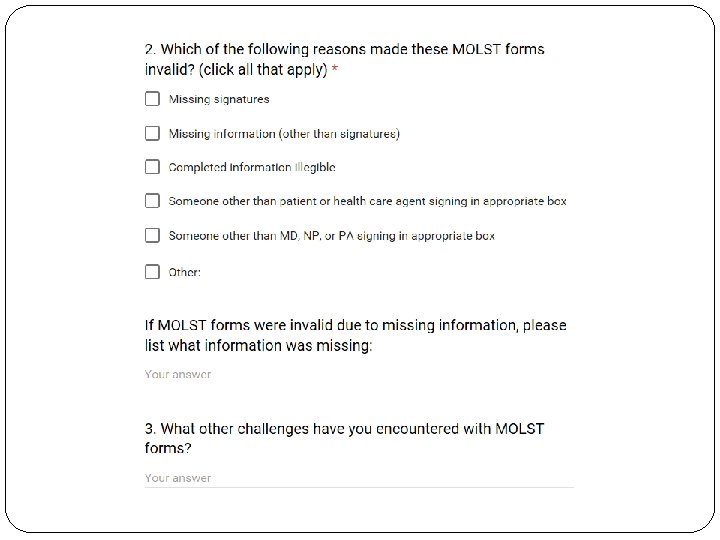
Background Data ● Survey to EMS providers 22