Improving the System of Care for STEMI Patients



- Slides: 45
Improving the System of Care for STEMI Patients 1
List of Commonly Used Terms Electrocardiogram (ECG) A recorded tracing of the electrical activity of the heart Percutaneous Coronary Intervention (PCI) A procedure used to open or widen narrowed or blocked blood vessels supplying the heart ST-Elevation Myocardial Infarction (STEMI) A myocardial infarction for which the ECG shows ST-segment elevation, usually associated with a recently closed coronary artery PCI Hospital/STEMIReceiving Center Hospital that can perform primary PCI Non-PCI Hospital/STEMIReferral Center Hospital that cannot perform primary PCI and may transfer to a center for primary PCI or use fibrinolytics Reperfusion The restoration of blood flow to an organ or tissue. PCI and fibrinolytics are two types of reperfusion strategies. Fibrinolytic An agent used to facilitate fibrin breakdown Improving the System of Care for STEMI Patients 2
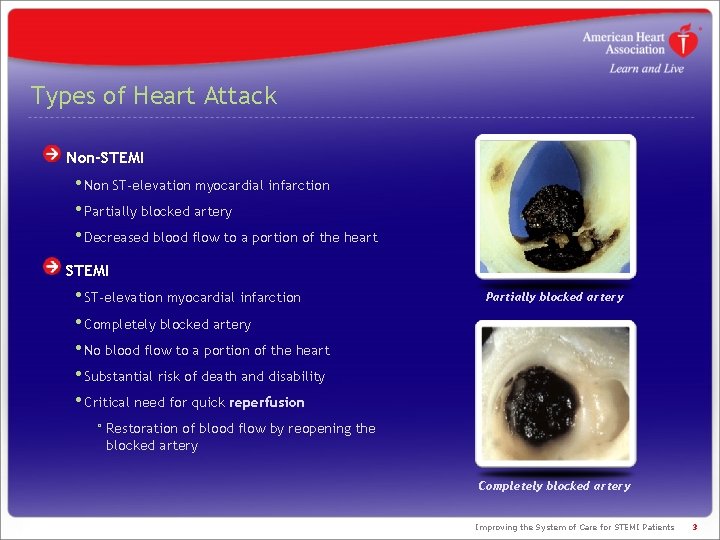
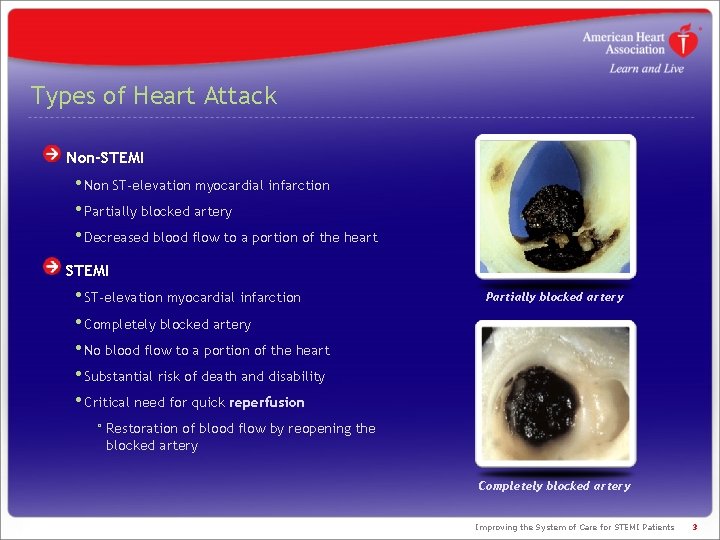
Types of Heart Attack Non-STEMI • Non ST-elevation myocardial infarction • Partially blocked artery • Decreased blood flow to a portion of the heart STEMI • ST-elevation myocardial infarction • Completely blocked artery • No blood flow to a portion of the heart • Substantial risk of death and disability • Critical need for quick reperfusion Partially blocked artery ° Restoration of blood flow by reopening the blocked artery Completely blocked artery Improving the System of Care for STEMI Patients 3
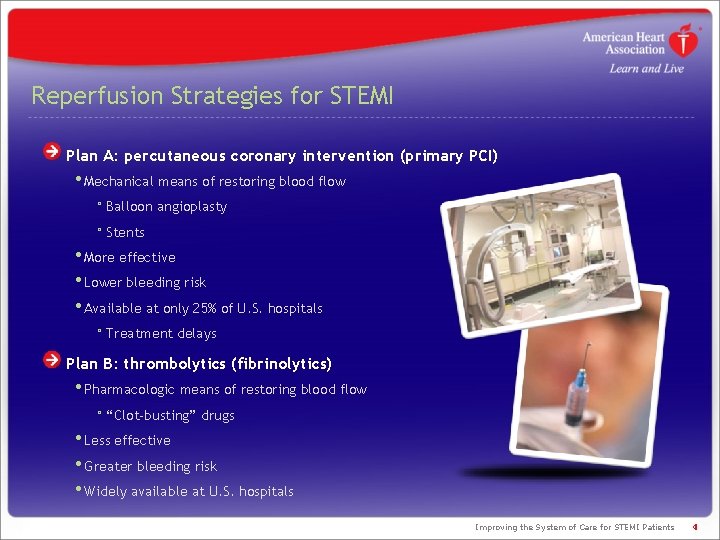
Reperfusion Strategies for STEMI Plan A: percutaneous coronary intervention (primary PCI) • Mechanical means of restoring blood flow ° Balloon angioplasty ° Stents • More effective • Lower bleeding risk • Available at only 25% of U. S. hospitals ° Treatment delays Plan B: thrombolytics (fibrinolytics) • Pharmacologic means of restoring blood flow ° “Clot-busting” drugs • Less effective • Greater bleeding risk • Widely available at U. S. hospitals Improving the System of Care for STEMI Patients 4
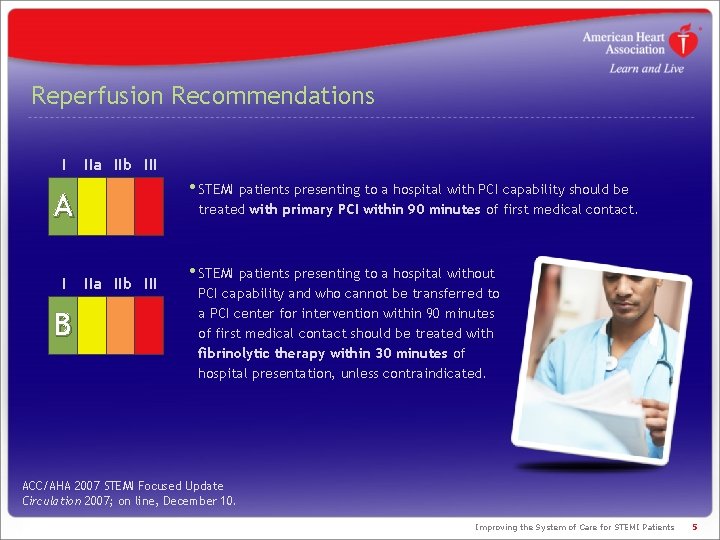
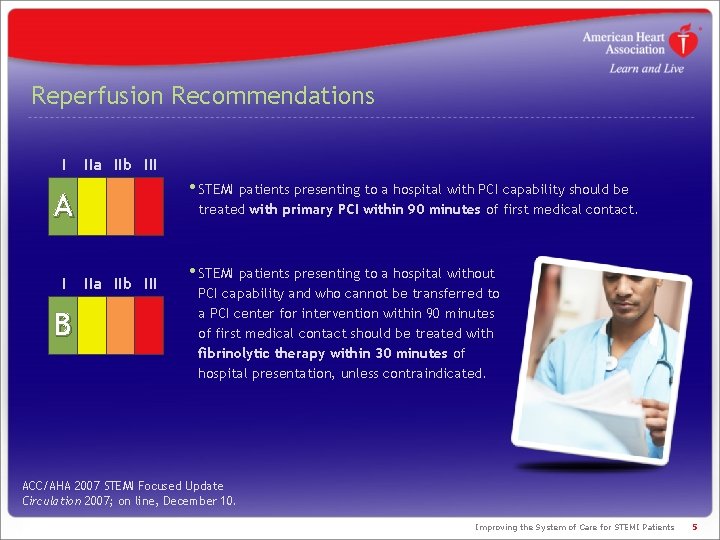
Reperfusion Recommendations I IIa IIb III • STEMI patients presenting to a hospital with PCI capability should be A I B treated with primary PCI within 90 minutes of first medical contact. IIa IIb III • STEMI patients presenting to a hospital without PCI capability and who cannot be transferred to a PCI center for intervention within 90 minutes of first medical contact should be treated with fibrinolytic therapy within 30 minutes of hospital presentation, unless contraindicated. ACC/AHA 2007 STEMI Focused Update Circulation 2007; on line, December 10. Improving the System of Care for STEMI Patients 5
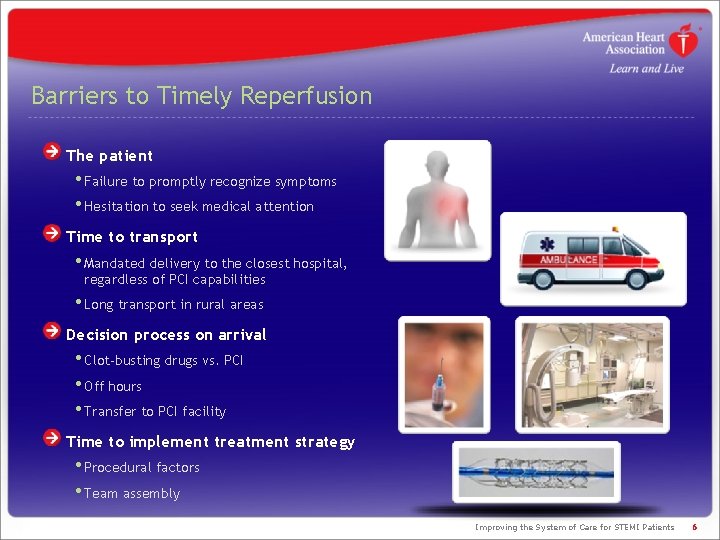
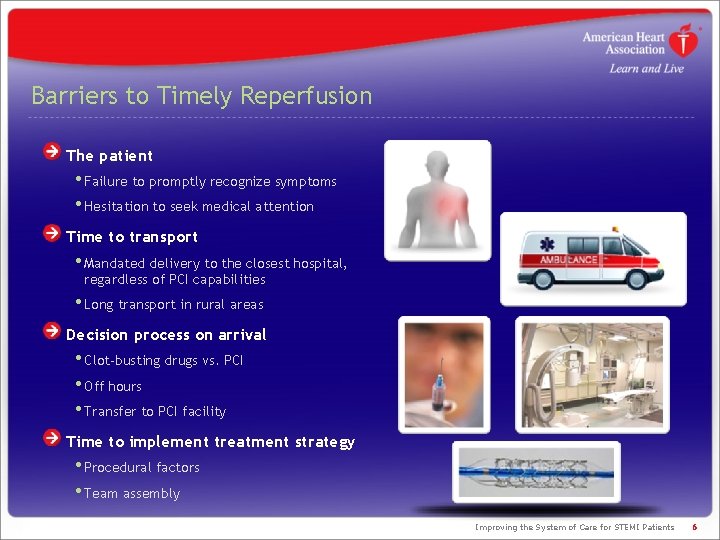
Barriers to Timely Reperfusion The patient • Failure to promptly recognize symptoms • Hesitation to seek medical attention Time to transport • Mandated delivery to the closest hospital, regardless of PCI capabilities • Long transport in rural areas Decision process on arrival • Clot-busting drugs vs. PCI • Off hours • Transfer to PCI facility Time to implement treatment strategy • Procedural factors • Team assembly Improving the System of Care for STEMI Patients 6
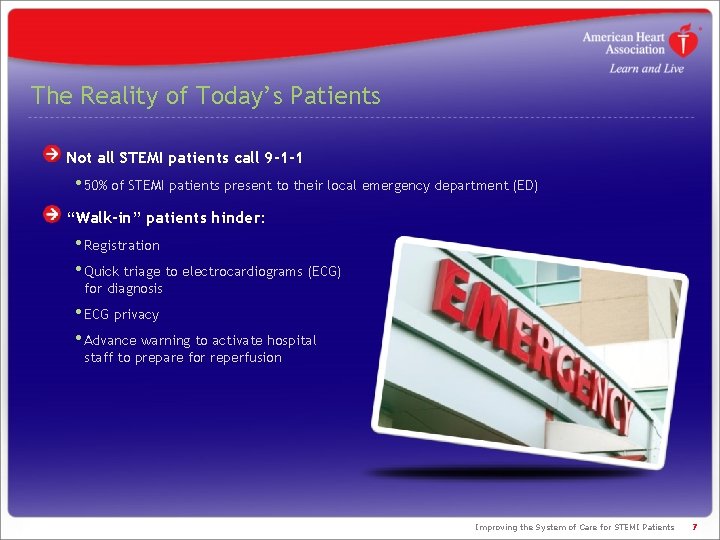
The Reality of Today’s Patients Not all STEMI patients call 9 -1 -1 • 50% of STEMI patients present to their local emergency department (ED) “Walk-in” patients hinder: • Registration • Quick triage to electrocardiograms (ECG) for diagnosis • ECG privacy • Advance warning to activate hospital staff to prepare for reperfusion Improving the System of Care for STEMI Patients 7
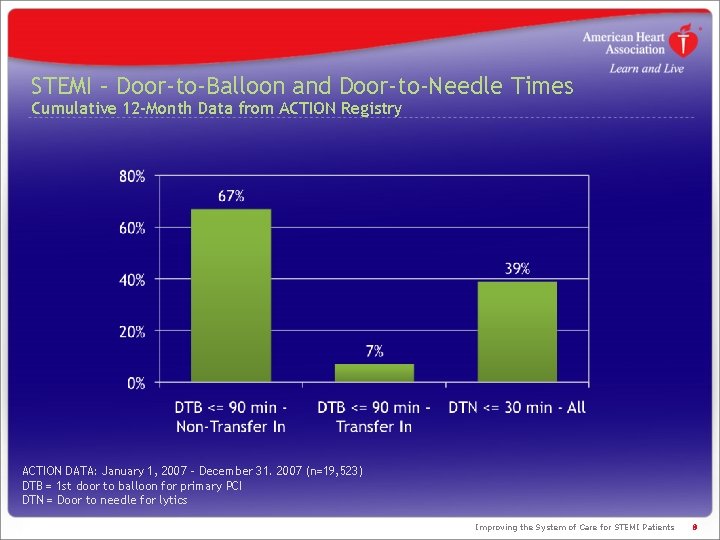
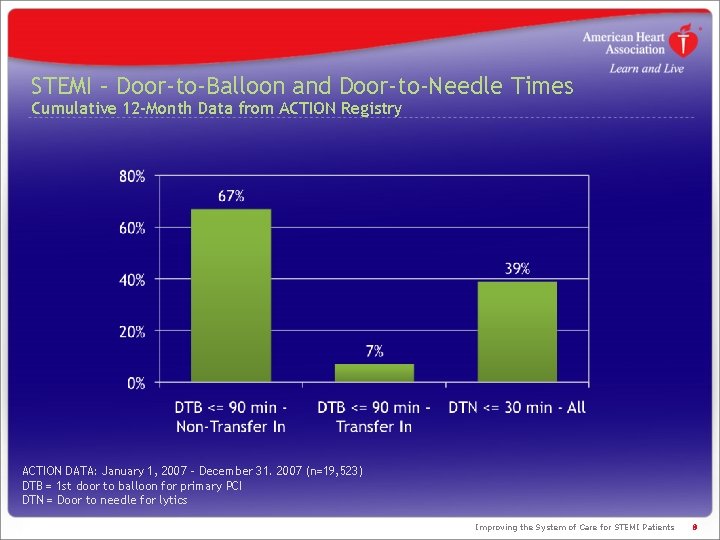
STEMI – Door-to-Balloon and Door-to-Needle Times Cumulative 12 -Month Data from ACTION Registry ACTION DATA: January 1, 2007 – December 31. 2007 (n=19, 523) DTB = 1 st door to balloon for primary PCI DTN = Door to needle for lytics Improving the System of Care for STEMI Patients 8
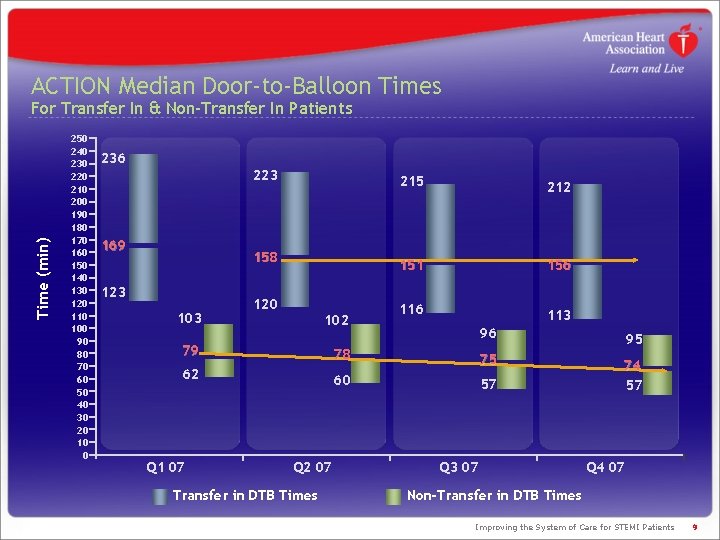
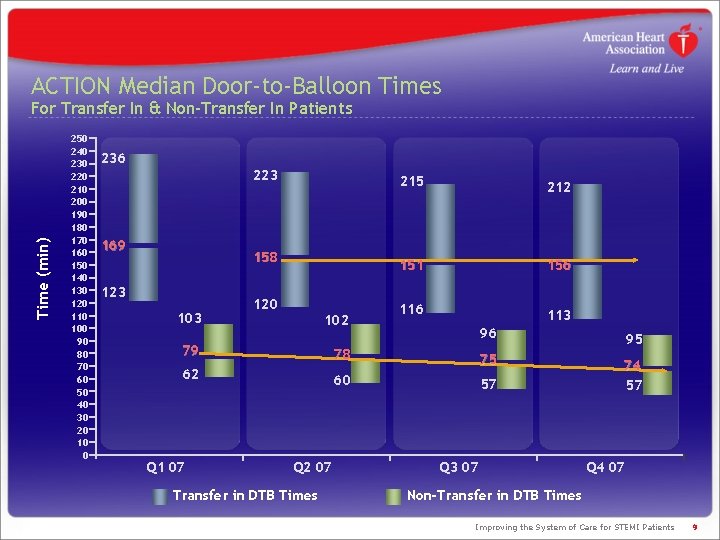
ACTION Median Door-to-Balloon Times Time (min) For Transfer In & Non-Transfer In Patients 250 240 230 220 210 200 190 180 170 160 150 140 130 120 110 100 90 80 70 60 50 40 30 20 10 0 236 223 169 158 123 103 120 102 215 212 151 156 113 96 95 74 57 79 78 62 75 60 57 Q 1 07 Q 2 07 Transfer in DTB Times Q 3 07 Q 4 07 Non-Transfer in DTB Times Improving the System of Care for STEMI Patients 9
How do we increase the number of patients with timely access to reperfusion therapy? Improving the System of Care for STEMI Patients 10
A Life-Saving Initiative National, community-based initiative Goals • Improve quality of care and outcomes in heart attack patients • Improve health care system readiness and response Improving the System of Care for STEMI Patients 11
Mission: Lifeline’s Guiding Principles The initiative values: • Patient-centered care as the #1 priority • High-quality care that is safe, effective and timely • Stakeholder consensus • Increased operational efficiencies • Appropriate incentives for quality • Measureable patient outcomes • An evaluation mechanism • A role for local community hospitals • A reduction in disparities of healthcare delivery Improving the System of Care for STEMI Patients 12
The Uniqueness of Mission: Lifeline will: • Promote the ideal STEMI systems of care • Help STEMI patients get the life-saving care they need in time • Bring together healthcare resources into an efficient, synergistic system • Improve overall quality of care The initiative is unique in that it: • Addresses the continuum of care for STEMI patients • Preserves a role for the local STEMI-referral hospital • Understands the issues specific to rural communities • Promotes different solutions/protocols for rural vs. urban/suburban areas • Recognizes there is no “one-size-fits-all” solution • Knows the issues of implementing national recommendations on a community level Improving the System of Care for STEMI Patients 13
STEMI Chain of Survival Improving the System of Care for STEMI Patients
History 2004 -2006 May 2004 • AHA recruited an Advisory Working Group (AWG) June 2005 • Price Waterhouse Coopers presents its market research to AWG March 2006 • AWG Consensus Statement appears in Circulation • Stakeholders called to action • AWG develops a set of guiding principles • AHA held a conference of multidisciplinary groups involved in STEMI patient care Circulation 2006; 113: 2152 -2163. Improving the System of Care for STEMI Patients 15
History 2007 -Present Early 2007 • Drafts of STEMI Systems of Care manuscripts are finalized • Action items for the AHA begin to take shape April 2007 • A cross-functional team was recruited to spearhead Mission: Lifeline May 2007 • Eleven manuscripts are published in Circulation • Mission: Lifeline was formally launched July 2008 • Affiliate Staff Kick-Off was held Improving the System of Care for STEMI Patients 16
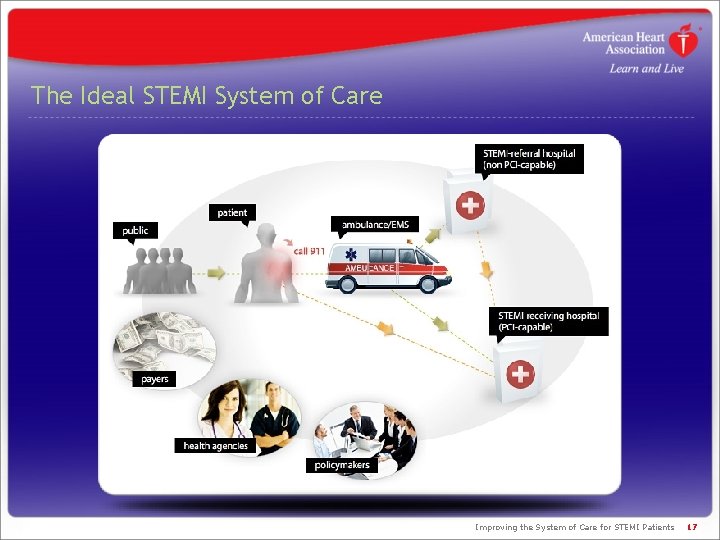
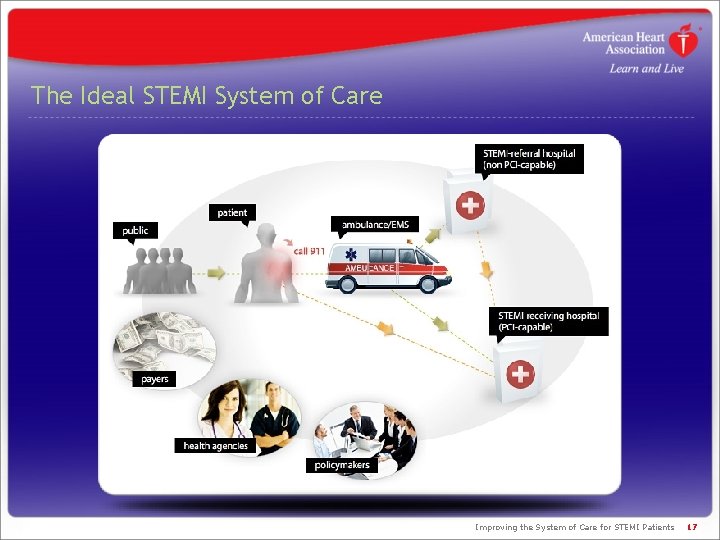
The Ideal STEMI System of Care Improving the System of Care for STEMI Patients 17
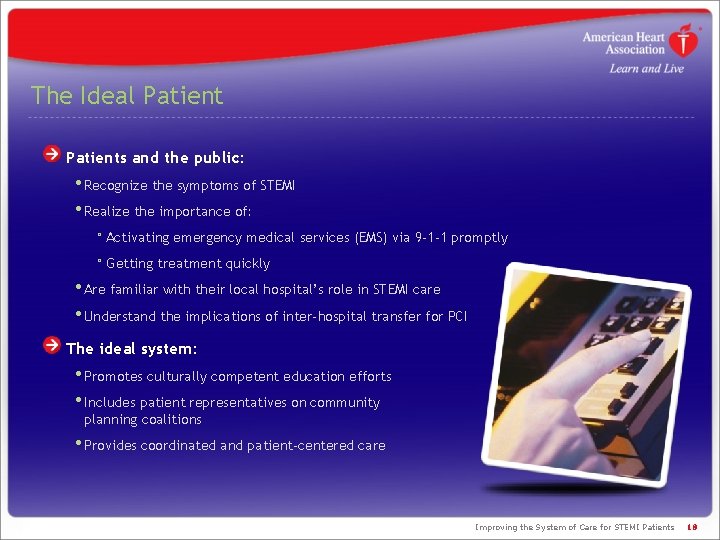
The Ideal Patients and the public: • Recognize the symptoms of STEMI • Realize the importance of: ° Activating emergency medical services (EMS) via 9 -1 -1 promptly ° Getting treatment quickly • Are familiar with their local hospital’s role in STEMI care • Understand the implications of inter-hospital transfer for PCI The ideal system: • Promotes culturally competent education efforts • Includes patient representatives on community planning coalitions • Provides coordinated and patient-centered care Improving the System of Care for STEMI Patients 18
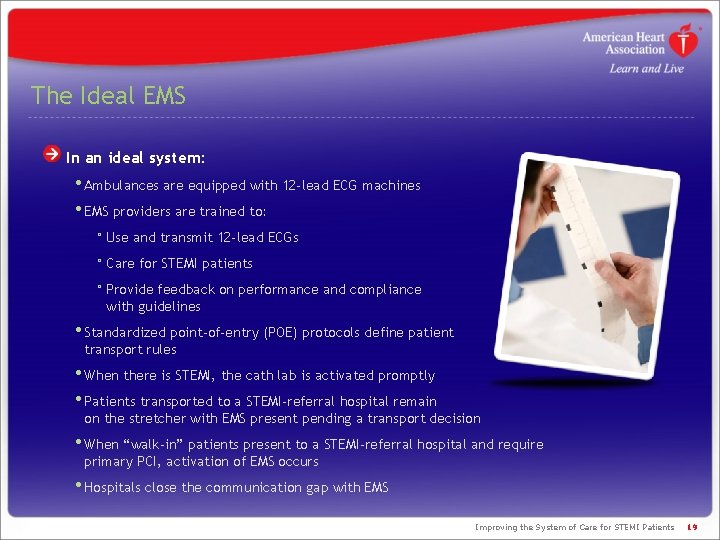
The Ideal EMS In an ideal system: • Ambulances are equipped with 12 -lead ECG machines • EMS providers are trained to: ° Use and transmit 12 -lead ECGs ° Care for STEMI patients ° Provide feedback on performance and compliance with guidelines • Standardized point-of-entry (POE) protocols define patient transport rules • When there is STEMI, the cath lab is activated promptly • Patients transported to a STEMI-referral hospital remain on the stretcher with EMS present pending a transport decision • When “walk-in” patients present to a STEMI-referral hospital and require primary PCI, activation of EMS occurs • Hospitals close the communication gap with EMS Improving the System of Care for STEMI Patients 19
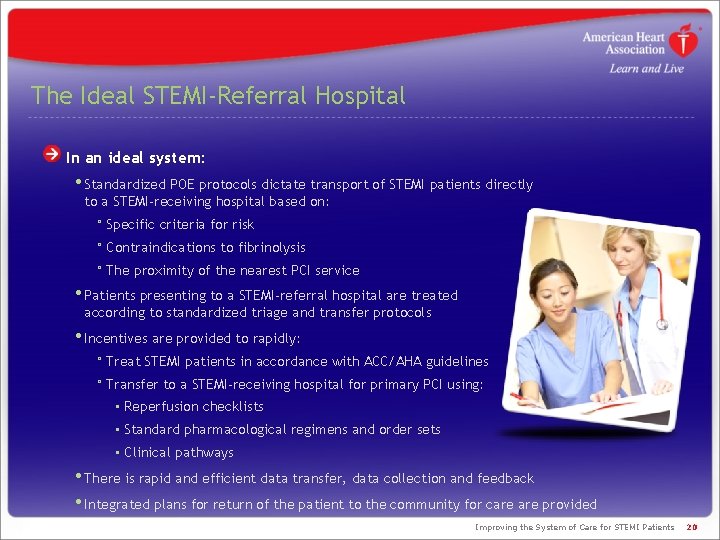
The Ideal STEMI-Referral Hospital In an ideal system: • Standardized POE protocols dictate transport of STEMI patients directly to a STEMI-receiving hospital based on: ° Specific criteria for risk ° Contraindications to fibrinolysis ° The proximity of the nearest PCI service • Patients presenting to a STEMI-referral hospital are treated according to standardized triage and transfer protocols • Incentives are provided to rapidly: ° Treat STEMI patients in accordance with ACC/AHA guidelines ° Transfer to a STEMI-receiving hospital for primary PCI using: • Reperfusion checklists • Standard pharmacological regimens and order sets • Clinical pathways • There is rapid and efficient data transfer, data collection and feedback • Integrated plans for return of the patient to the community for care provided Improving the System of Care for STEMI Patients 20
The Ideal STEMI-Receiving Hospital In an ideal system: • Pre-hospital ECG diagnosis of STEMI, ED notification and cath lab activation occurs according to standard algorithms • Algorithms facilitate: ° A short ED stay for the STEMI patient ° Transport directly from the field to the cath lab • Single-call systems from STEMI-referral hospitals immediately activate the cath lab • Primary PCI is provided as routine treatment for STEMI 24, 7 • STEMI-receiving hospital’s administration puts their support in writing • A multidisciplinary team meets regularly to identify and solve problems • A continuing education program is designed and instituted • A mechanism for monitoring performance, process measures and patient outcomes is established Improving the System of Care for STEMI Patients 21
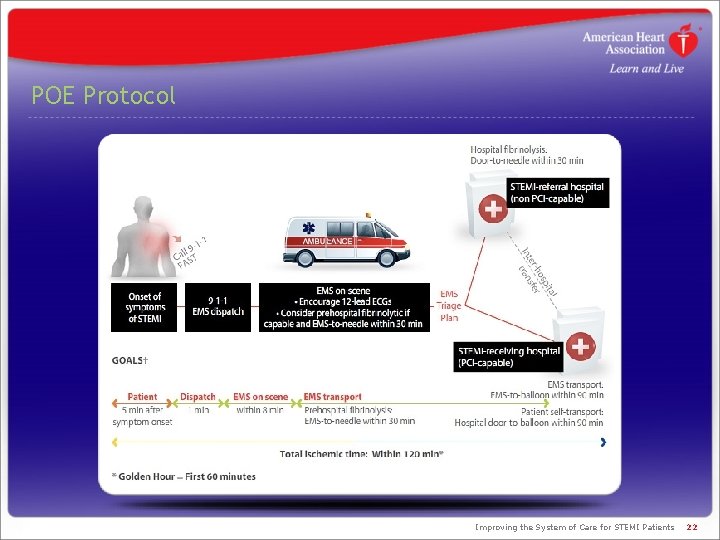
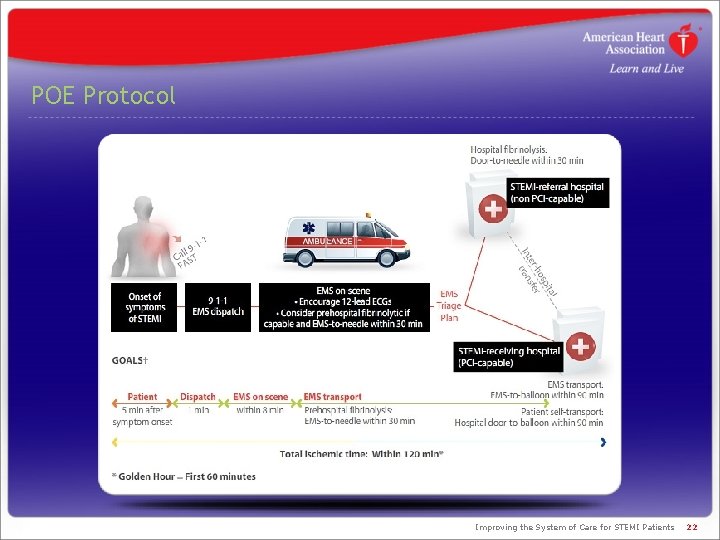
POE Protocol Improving the System of Care for STEMI Patients 22
Coordinated Actions Assess and improve the EMS system Evaluate existing STEMI system models Establish local initiatives Explore the possibility of developing a national STEMI-certification program and/or criteria Launch Mission: Lifeline awareness campaigns Create system resources Engage strategic alliances Improving the System of Care for STEMI Patients 23
Partners for Success Patients and care givers EMS providers Physicians, nurses and other providers STEM-referral (non-PCI) hospitals STEMI-receiving (PCI-capable) hospitals Health systems Departments of health EMS regulatory authority / office of EMS Rural health associations Quality improvement organizations Third-party payers State and local policymakers Improving the System of Care for STEMI Patients 24
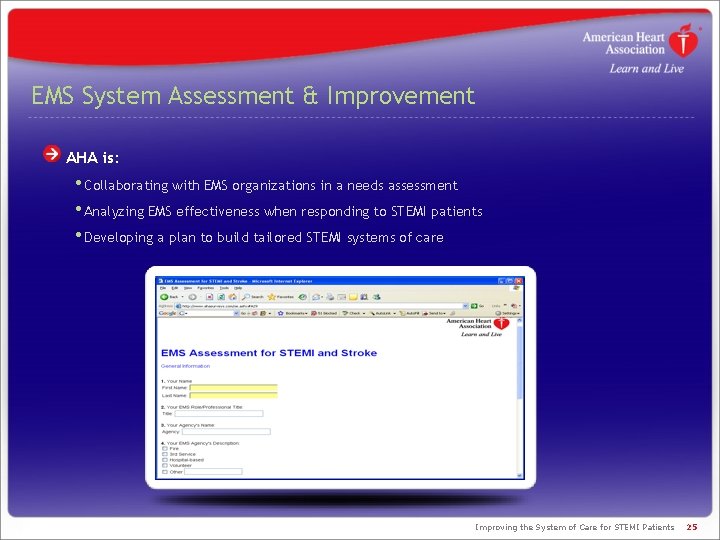
EMS System Assessment & Improvement AHA is: • Collaborating with EMS organizations in a needs assessment • Analyzing EMS effectiveness when responding to STEMI patients • Developing a plan to build tailored STEMI systems of care Improving the System of Care for STEMI Patients 25
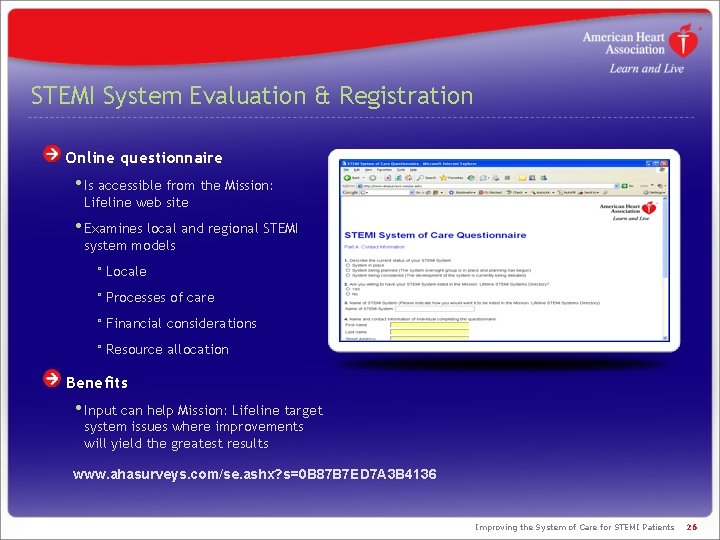
STEMI System Evaluation & Registration Online questionnaire • Is accessible from the Mission: Lifeline web site • Examines local and regional STEMI system models ° Locale ° Processes of care ° Financial considerations ° Resource allocation Benefits • Input can help Mission: Lifeline target system issues where improvements will yield the greatest results www. ahasurveys. com/se. ashx? s=0 B 87 B 7 ED 7 A 3 B 4136 Improving the System of Care for STEMI Patients 26
Local Initiatives The American Heart Association is: • Convening a task force at state and local levels • Helping identify ways to implement national recommendations for STEMI systems in local communities • Registering STEMI systems with the Mission: Lifeline directory Improving the System of Care for STEMI Patients 27
STEMI Certification & Recognition The American Heart Association will: • Develop recommendations for a certification program • Generate and publish criteria to define a: ° STEMI system of care ° EMS ° Non-PCI hospital ° PCI hospital • Support policy approaches that advance the development of STEMI systems • Develop a recognition program to: ° Salute health care teams who comply with guidelines ° Commend STEMI systems for raising quality of care ° Help compliant hospitals differentiate themselves ° Motivate more health care providers to embrace the Mission: Lifeline standards Improving the System of Care for STEMI Patients 28
Implementation Plan Please visit www. americanheart. org/missionlifeline For each component of the system, Mission: Lifeline will: • Define the ideal practice • Recommend strategies to achieve the ideal practice • Provide resources/tools to achieve the ideal practice • Recommend metrics for structure, process and outcomes • Recommend criteria for recognition and certification Improving the System of Care for STEMI Patients 29
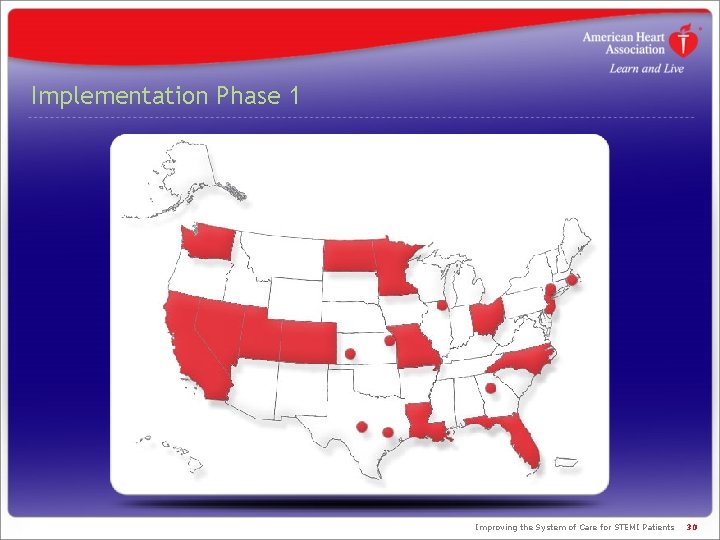
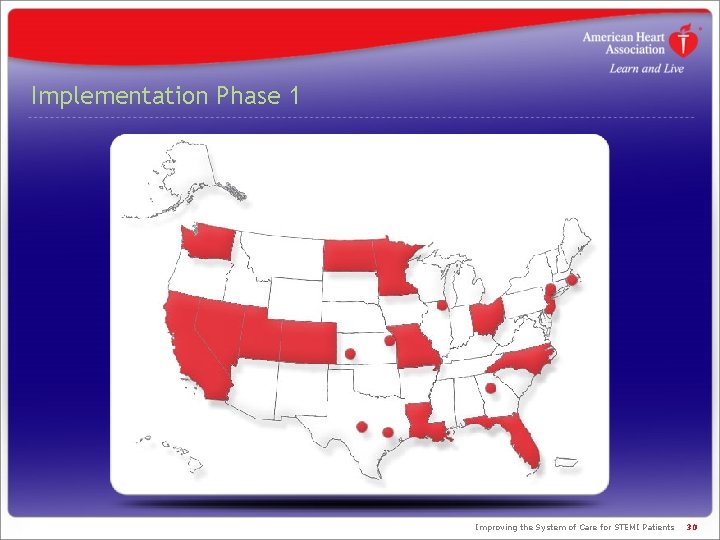
Implementation Phase 1 Improving the System of Care for STEMI Patients 30
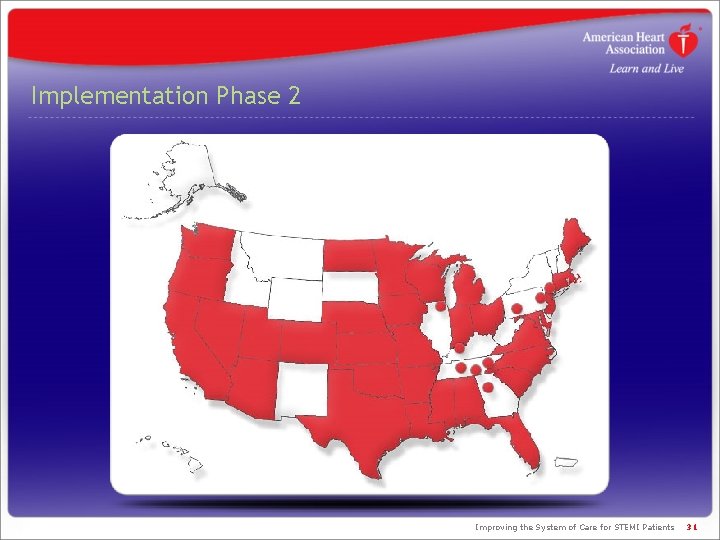
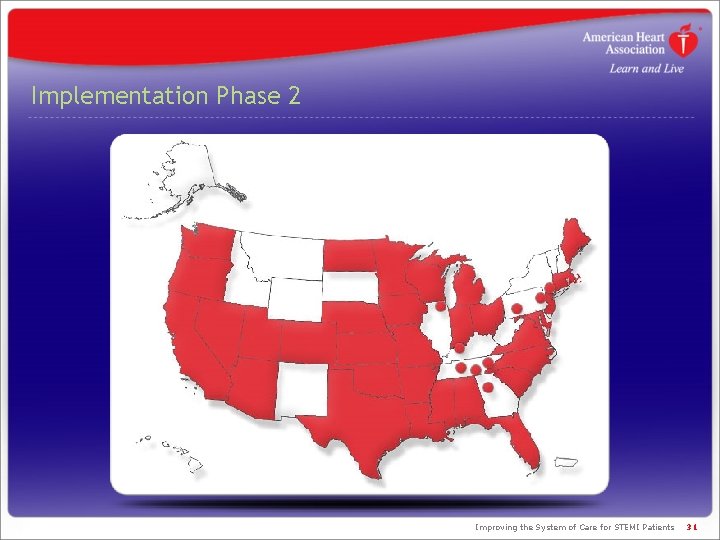
Implementation Phase 2 Improving the System of Care for STEMI Patients 31
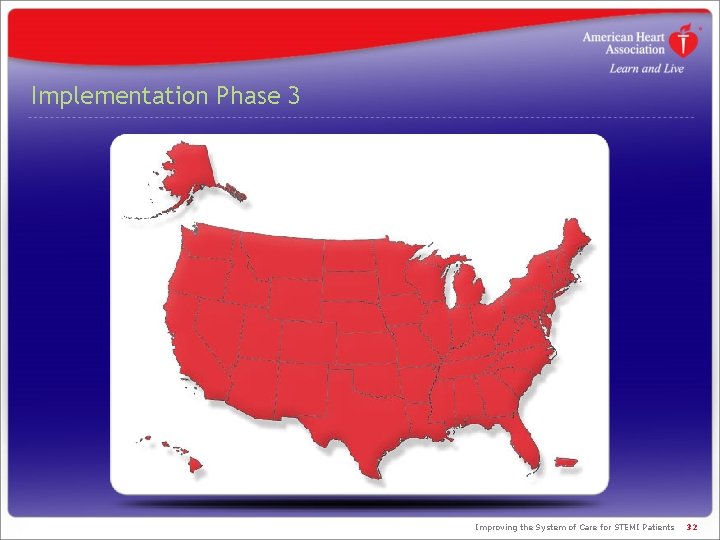
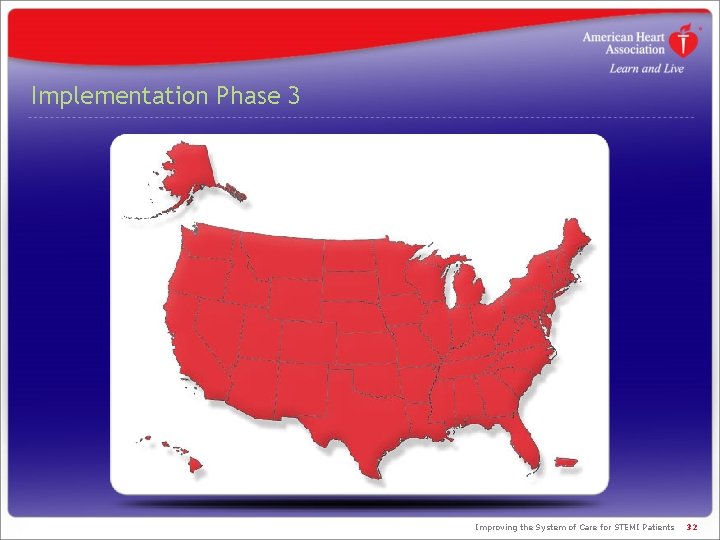
Implementation Phase 3 Improving the System of Care for STEMI Patients 32

How will we measure our impact? Improving the System of Care for STEMI Patients 33
Mission: Lifeline Metrics Data Sources EMS • EMS assessment (NAEMSO and local assessments) • ACTION/Get With The Guidelines (GWTG) • NEMSIS Emergency department • ACTION/GWTG “Non-PCI Version” STEMI-receiving (PCI-capable) hospitals • ACTION/GWTG • NCDR CATH/PCI registry Improving the System of Care for STEMI Patients 34
Who is Mission: Lifeline? Improving the System of Care for STEMI Patients 35
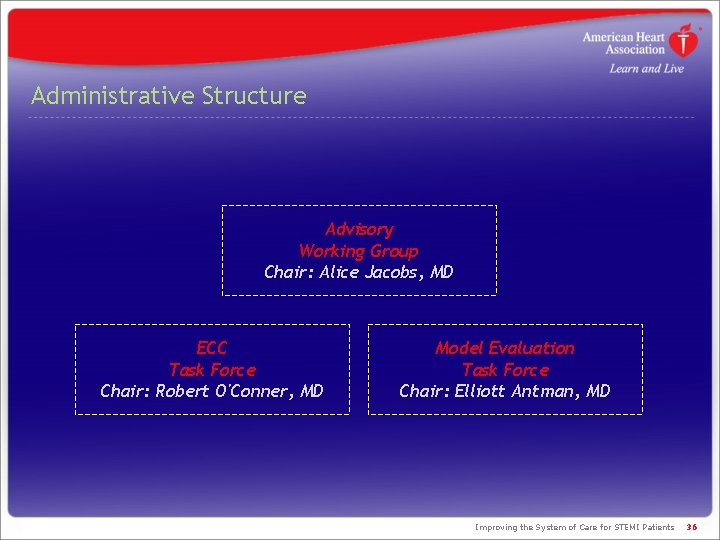
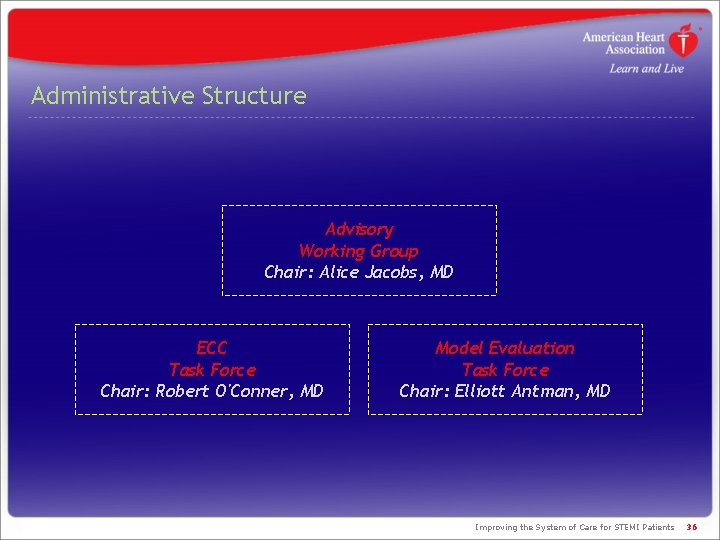
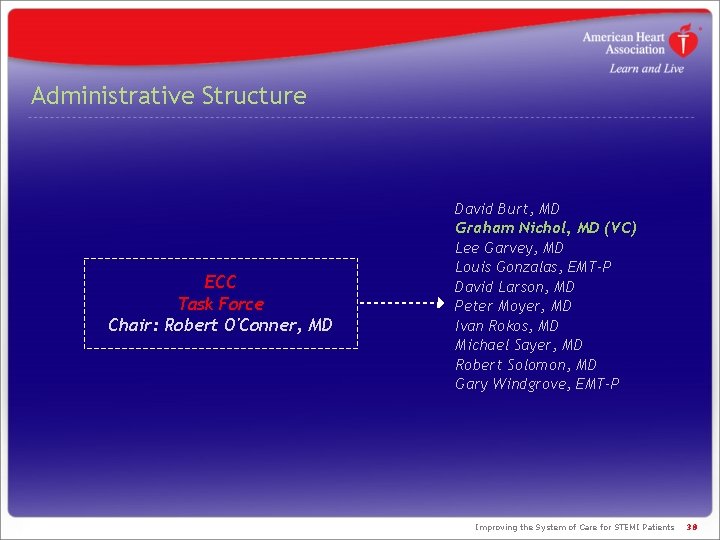
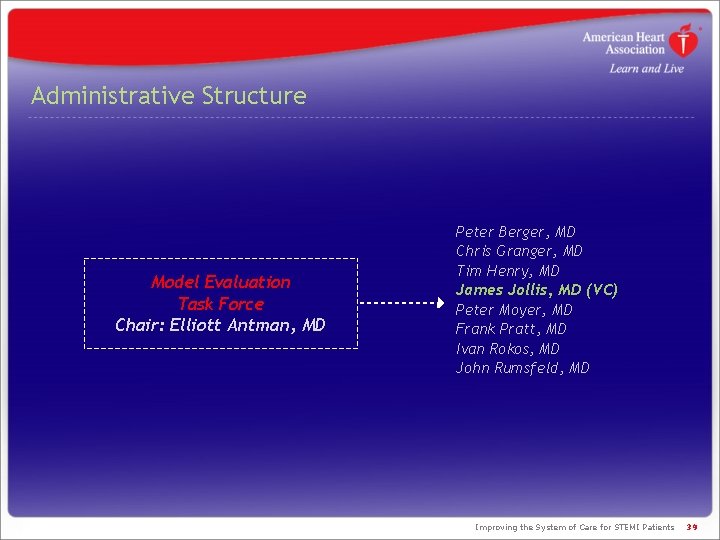
Administrative Structure Advisory Working Group Chair: Alice Jacobs, MD ECC Task Force Chair: Robert O'Conner, MD Model Evaluation Task Force Chair: Elliott Antman, MD Improving the System of Care for STEMI Patients 36
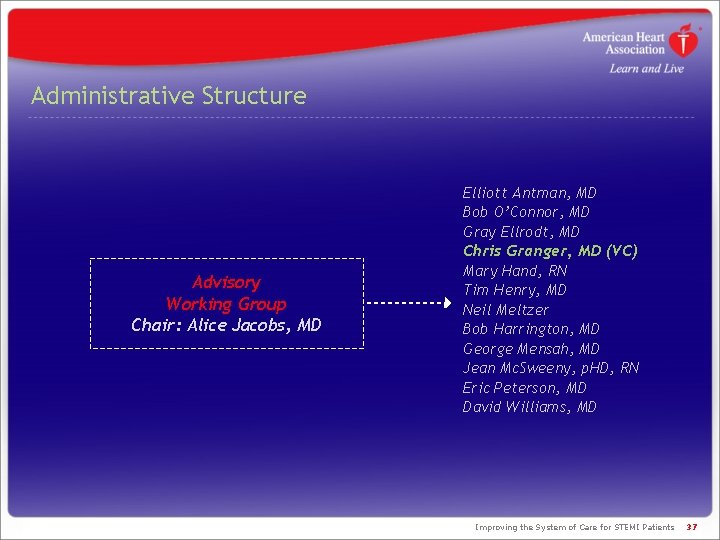
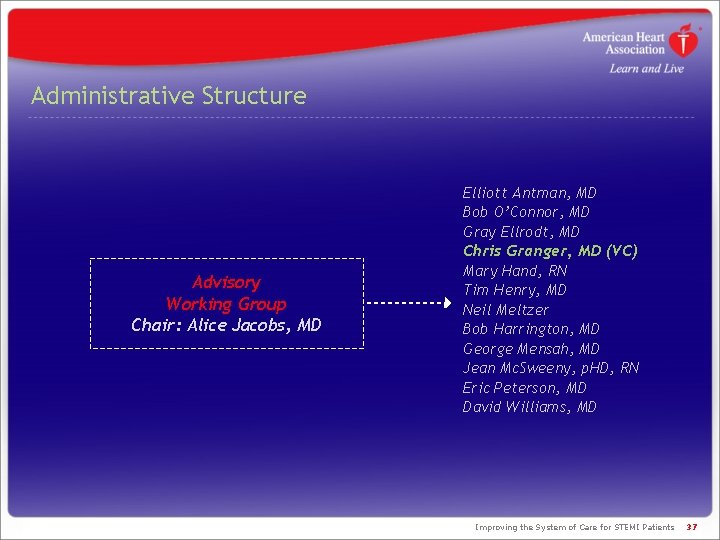
Administrative Structure Advisory Working Group Chair: Alice Jacobs, MD Elliott Antman, MD Bob O’Connor, MD Gray Ellrodt, MD Chris Granger, MD (VC) Mary Hand, RN Tim Henry, MD Neil Meltzer Bob Harrington, MD George Mensah, MD Jean Mc. Sweeny, p. HD, RN Eric Peterson, MD David Williams, MD Improving the System of Care for STEMI Patients 37
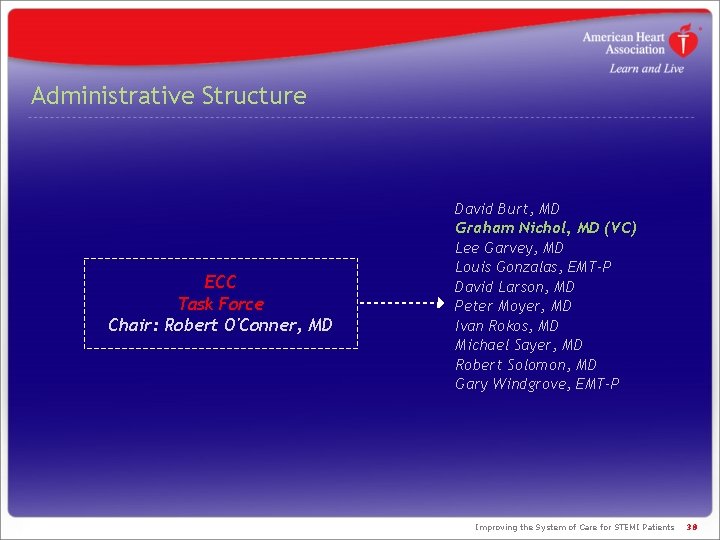
Administrative Structure ECC Task Force Chair: Robert O'Conner, MD David Burt, MD Graham Nichol, MD (VC) Lee Garvey, MD Louis Gonzalas, EMT-P David Larson, MD Peter Moyer, MD Ivan Rokos, MD Michael Sayer, MD Robert Solomon, MD Gary Windgrove, EMT-P Improving the System of Care for STEMI Patients 38
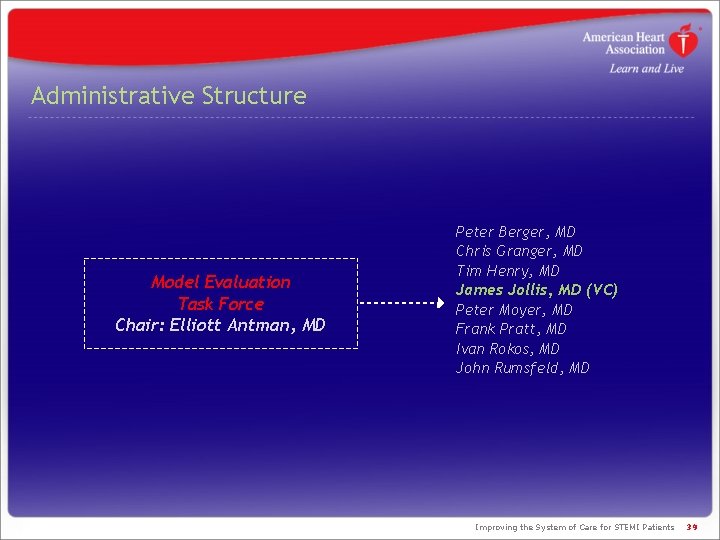
Administrative Structure Model Evaluation Task Force Chair: Elliott Antman, MD Peter Berger, MD Chris Granger, MD Tim Henry, MD James Jollis, MD (VC) Peter Moyer, MD Frank Pratt, MD Ivan Rokos, MD John Rumsfeld, MD Improving the System of Care for STEMI Patients 39
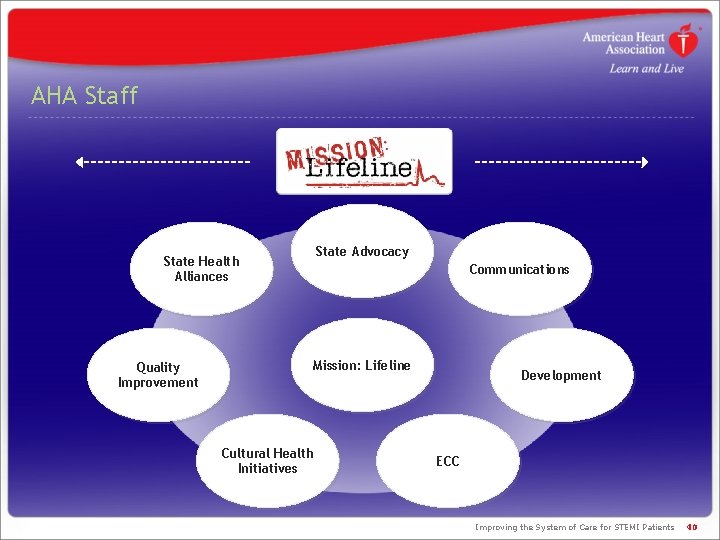
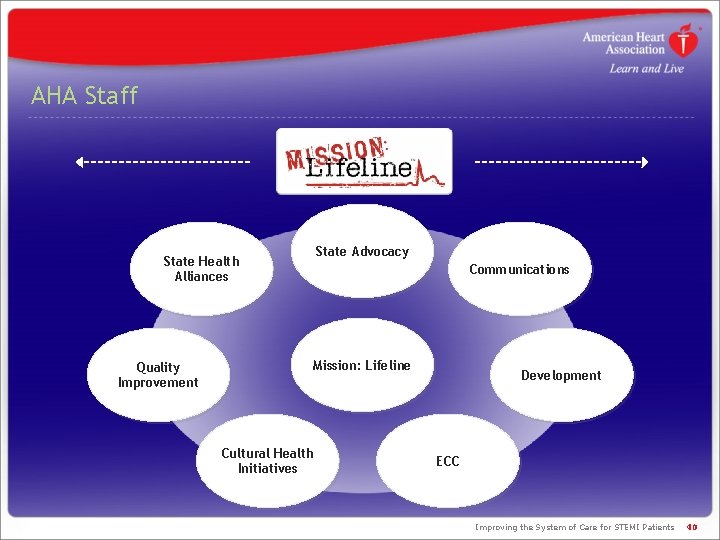
AHA Staff State Advocacy State Health Alliances Quality Improvement Communications Mission: Lifeline Cultural Health Initiatives Development ECC Improving the System of Care for STEMI Patients 40

Organizational Commitment Current model = Partial staff dedication State-level and hospital clinical quality improvement (QI) support • State Health Alliance staff • State Advocacy staff • Quality Improvement staff • Emergency Cardiovascular Care (ECC) Community Strategies managers Training of existing resources Initiative fundraising Current model = State-level and hospital clinical QI support Programmatic support • Stakeholder meetings and/or planning in all 50 states • ACTION/GWTG regional workshops • Reactive advocacy agendas Improving the System of Care for STEMI Patients 41

Increased Organizational Commitment State-level and hospital clinical quality improvement support PLUS Affiliate-level and market-level dedicated Mission: Lifeline resources Improving the System of Care for STEMI Patients 42
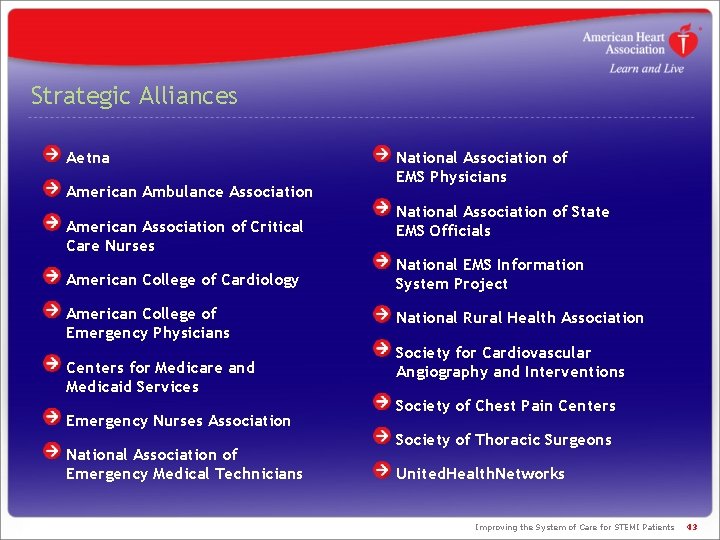
Strategic Alliances Aetna American Ambulance Association American Association of Critical Care Nurses National Association of EMS Physicians National Association of State EMS Officials American College of Cardiology National EMS Information System Project American College of Emergency Physicians National Rural Health Association Centers for Medicare and Medicaid Services Emergency Nurses Association National Association of Emergency Medical Technicians Society for Cardiovascular Angiography and Interventions Society of Chest Pain Centers Society of Thoracic Surgeons United. Health. Networks Improving the System of Care for STEMI Patients 43
Registered STEMI Systems Every day, new systems from all areas of the United States register with Mission: Lifeline. STEMI systems will improve the quality of care for all myocardial infarction patients. http: //www. americanheart. org/presenter. jhtml? identifier=3059652 Improving the System of Care for STEMI Patients
Improving the System of Care for STEMI Patients 45