Improving the Quality of Bedside Shift Report Behavior
Improving the Quality of Bedside Shift Report Behavior on the Medical-Surgical Unit at Woodland Healthcare Amanda Waggoner, RN, MSN
Purpose • Ineffective nursing handoff communication at shift change • Delay in or inappropriate treatment • Extended LOS • Increased preventable costs • Decreased patient and staff satisfaction • Patient harm • Leading cause of sentinel events • Importance of addressing patient safety risks as a priority https: //www. google. com/search? q=communication+errors+between+nursese&tbm=isch&tbs=rimg: Cfj. HKq. O 1 b. X_1 FIjh_1 x. Req. CT 1 ILj. X 4 Tdmgvg 2 tj. Btocq. K 6 RZ 1 plxlwj. X-
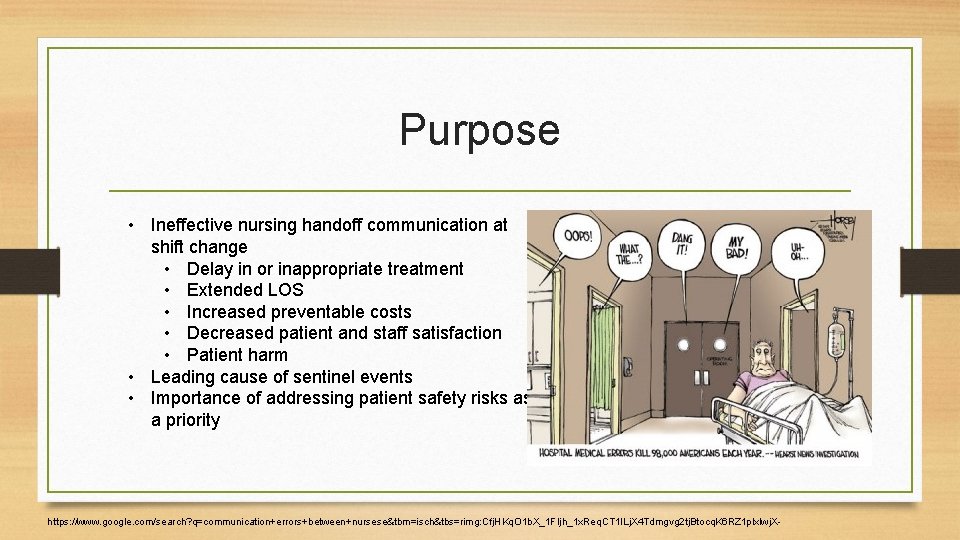
Microsystem Assessment 5 P’s Assessment Began on time, introduction, information exchange (SBAR), patient involvement, Safety San. • 50% of night shift felt report time is adequate 10 6 0 with shift report 10 5 • Lack of BSR altogether • Nursing Satisfaction Survey • Only 40% of day shift Nurses felt satisfied 10 • 15 • Assess quality report at bedside 20 • Process Identification • Observation of BSR Communication BSR performance of twenty 12 hour night shift RNs BSR Did not performedperform BSR
Microsystem Assessment Press Ganey Scores • At shift change, do patient’s feel included in the plan of care? • Yes; Total Mean= 89. 3 • July 03, 2017 Reportable Events • Kinked Foley • Patient Fall • Hypoglycemic Episode • Sex – 59% Females, 41 % Males • Language- 89% English, 11% Spanish https: //myhealth. alberta. ca/alberta/pages/When-you-have-an-indwelling-catheter-after-your-visit. aspx
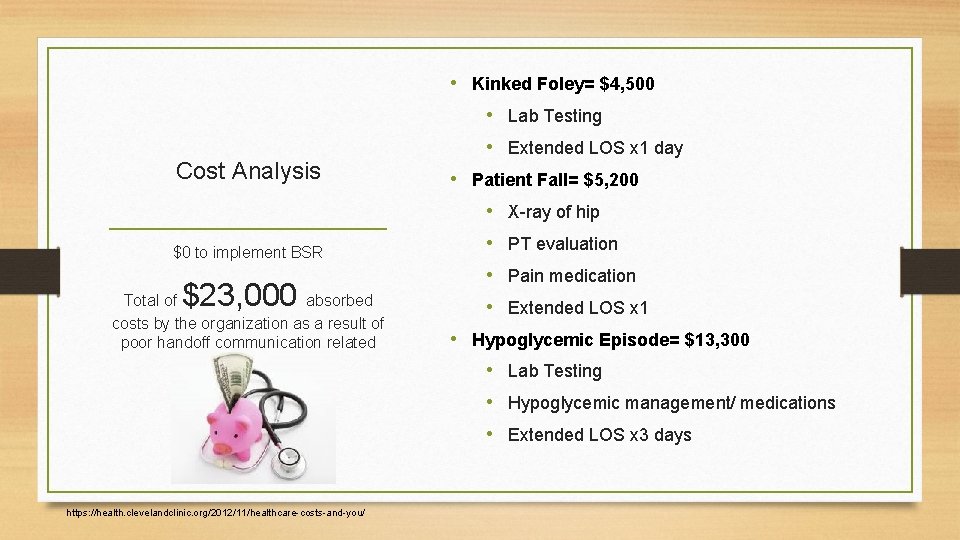
• Kinked Foley= $4, 500 • Lab Testing Cost Analysis • Extended LOS x 1 day • Patient Fall= $5, 200 • X-ray of hip $0 to implement BSR $23, 000 Total of absorbed costs by the organization as a result of poor handoff communication related errors • PT evaluation • Pain medication • Extended LOS x 1 • Hypoglycemic Episode= $13, 300 • Lab Testing • Hypoglycemic management/ medications • Extended LOS x 3 days https: //health. clevelandclinic. org/2012/11/healthcare-costs-and-you/
Qualitative Costs • Emotional Pain/ Suffering • Daily living • Staff perceptions • Financial Responsibilities • Teamwork/ • Physical Pain Communication/ Unit • Relationship Strain • Patient/Staff Satisfaction Scores https: //archive. ahrq. gov/newsletters/research-activities/14 jan/0114 RA 9. html morale
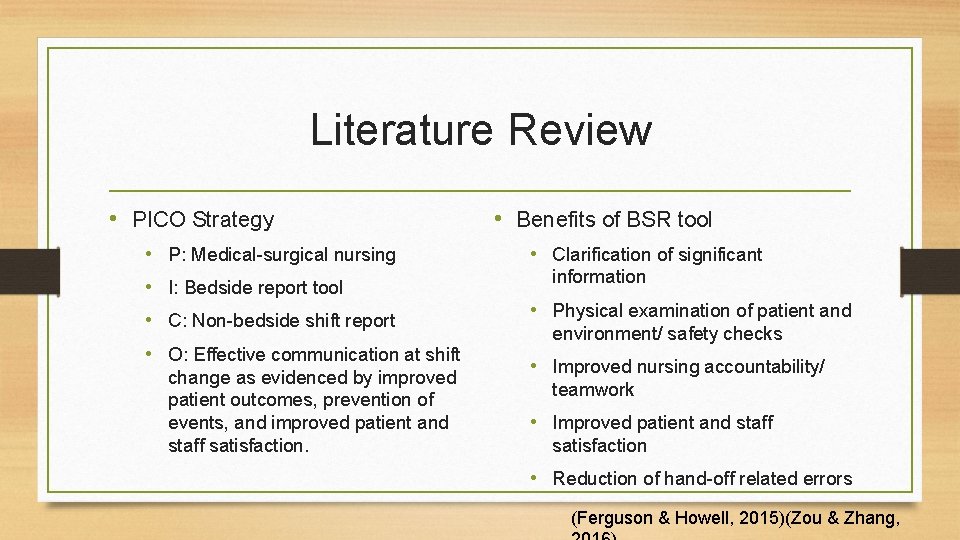
Literature Review • PICO Strategy • • P: Medical-surgical nursing I: Bedside report tool C: Non-bedside shift report O: Effective communication at shift change as evidenced by improved patient outcomes, prevention of events, and improved patient and staff satisfaction. • Benefits of BSR tool • Clarification of significant information • Physical examination of patient and environment/ safety checks • Improved nursing accountability/ teamwork • Improved patient and staff satisfaction • Reduction of hand-off related errors (Ferguson & Howell, 2015)(Zou & Zhang,
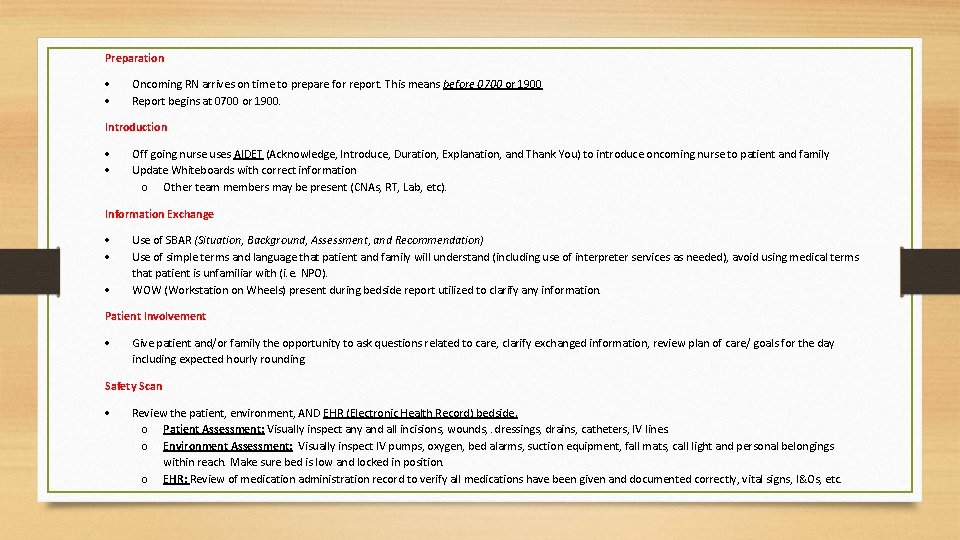
Preparation Oncoming RN arrives on time to prepare for report. This means before 0700 or 1900 Report begins at 0700 or 1900. Introduction Off going nurse uses AIDET (Acknowledge, Introduce, Duration, Explanation, and Thank You) to introduce oncoming nurse to patient and family Update Whiteboards with correct information o Other team members may be present (CNAs, RT, Lab, etc). Information Exchange Use of SBAR (Situation, Background, Assessment, and Recommendation) Use of simple terms and language that patient and family will understand (including use of interpreter services as needed), avoid using medical terms that patient is unfamiliar with (i. e. NPO). WOW (Workstation on Wheels) present during bedside report utilized to clarify any information. Patient Involvement Give patient and/or family the opportunity to ask questions related to care, clarify exchanged information, review plan of care/ goals for the day including expected hourly rounding. Safety Scan Review the patient, environment, AND EHR (Electronic Health Record) bedside. o Patient Assessment: Visually inspect any and all incisions, wounds, . dressings, drains, catheters, IV lines. o Environment Assessment: Visually inspect IV pumps, oxygen, bed alarms, suction equipment, fall mats, call light and personal belongings within reach. Make sure bed is low and locked in position. o EHR: Review of medication administration record to verify all medications have been given and documented correctly, vital signs, I&Os, etc.
Specific Aim Statement Through implementation of a standardized bedside report tool, 95% of twelve-hour night shift nurses on the medical surgical unit at Woodland Healthcare will demonstrate proper quality bedside report at shift change by August 15, 2017.
Methodology Lewin’s Theory of Planned Change • Unfreezing: Presented evidence-based research during huddles, gained stakeholder interests, addressed staff barriers, provided education to staff. • Moving: Monitored and coached staff during BSR. Act as resource for support/ mentoring. • Refreezing: evaluate BSR utilizing competency checklist, post-implementation survey results of staff and patients. Enact sustainability plan.
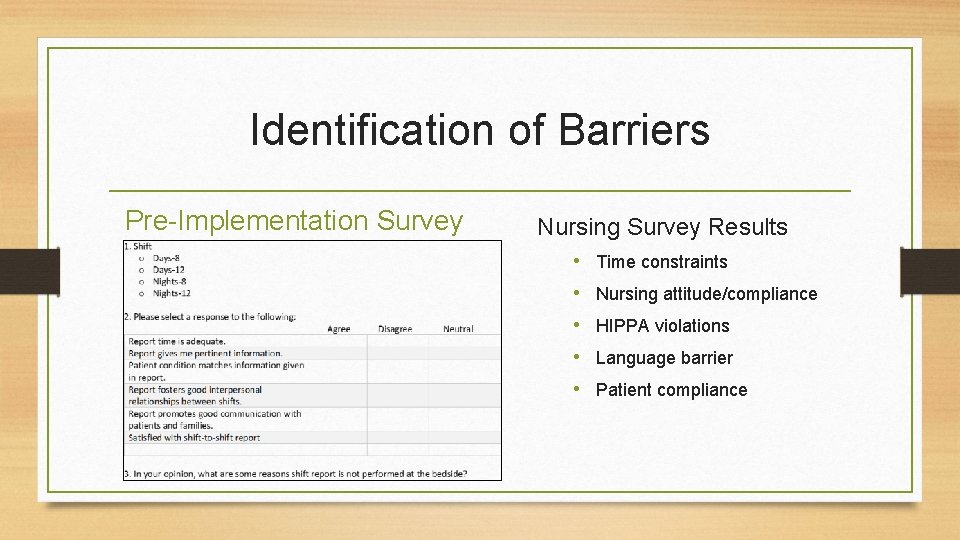
Identification of Barriers Pre-Implementation Survey Nursing Survey Results • Time constraints • Nursing attitude/compliance • HIPPA violations • Language barrier • Patient compliance
Timeline Gantt Chart
Summary Report Evaluation of Outcomes • In the process of collecting postimplementation data and evaluating outcomes: • Nursing Competency Checklist • Press Ganey Survey • Nursing post-implementation survey • Review of reportable events What I learned • The importance of flexibility and networking • Setting realistic goals and objectives • Utilizing effective communication strategies • Application of the PDSA cycle
• PDSA PDSS • Aligning with WHC Mission and Vision Sustainability Plan -Dignity, collaboration, stewardship, justice, and excellence • Having a unit champion - Key player and influencer • Continued perceived benefits for staff and patients - Post results of improvement, storytelling • Maintaining stakeholder support -Running reports and audits, benchmarking http: //www. opendoorhr. com/Quality-Improvement-Process/
References Ferguson, T. D. & Howell, T. L. (2015). Bedside reporting protocols for improving patient care. Nursing Clinics of North America, 50(4), 735 -747. Image one. (2017). Retrieved from https: //www. google. com/search? q=communication+errors+between+nursese&tbm=isch&tbs=rimg: Cfj. HKq. O 1 b. X_1 FIjh_1 x. Req. CT 1 ILj. X 4 Tdmgvg 2 tj. Btocq. K 6 RZ 1 plxlwj. X Image two. (2017). Retrieved from https: //myhealth. alberta. ca/alberta/pages/When-you-have-an-indwelling-catheter-after-your-visit. aspx Image three. (2017) Retrieved from https: //health. clevelandclinic. org/2012/11/healthcare-costs-and-you/ Image four. (2017). Retrieved from https: //archive. ahrq. gov/newsletters/research-activities/14 jan/0114 RA 9. html Image five. (2017). Retrieved from http: //www. opendoorhr. com/Quality-Improvement-Process/ Zou, X. J. & Zhang, Y. P. (2016). Rates of nursing errors and handoffs-related errors in a medical unit following implementation of a standardized nursing handoff form. Journal of Nursing Care Quality, 31 (1), 61 -67.
- Slides: 15