Improving the care of patients with cirrhosis using


















- Slides: 22
Improving the care of patients with cirrhosis using care bundles Stuart Mc. Pherson Consultant Hepatologist Liver Unit, Freeman Hospital, Newcastle upon Tyne and Translational and Clinical Research Institute, Newcastle University.

Background • Rates of cirrhosis are rising – doubled in 12 years • Alcohol related liver disease accounts for 70 -85% of liver admissions Liver disease • Decompensated cirrhosis has a high mortality rate ~10% in hospital mortality • NCEPOD report in 2013 identified that care of patients with ARLD was suboptimal • Only 47% patients received ‘good care’ • Cirrhosis is a complex multisystem disorder so requires a systematic approach to management Williams et al Lancet 2015

BSG decompensated cirrhosis care bundle was developed to help address NCEPOD concerns http: //www. bsg. org. uk/care-bundles-general/index. html Mc. Pherson S, Frontline Gastroenterology 2016

Use of the care bundle improves patient care • Outcomes of implementation assessed in 3 hospitals • Newcastle • Sunderland • Royal Cornwall Hospital • 228 patients with decompensated cirrhosis reviewed • High level of usage of the care bundle • Increased to 90% in Newcastle • Improvement in all aspects addressed in the Bundle • Hospital stay reduced from 11 days to 8 days Dyson J et al. Alimentary Pharmacology and Therapeutics Oct 2016

What about discharge? • Patients with decompensated cirrhosis: • Have complex and prolonged admissions • Multiple complications that need ongoing care • Discharge planning may be complex • Need good communication with primary care • Need clear follow up plans • Good education of patients and their carers about their condition • Many have hepatic encephalopathy or alcohol related brain injury • Encourage self-management

Aims 1. Conduct a baseline audit to determine the quality of discharge for patients with decompensated liver disease and frequency of avoidable re-admissions 2. Development of a decompensated cirrhosis discharge bundle to optimise the quality of discharge 3. Development of a decompensated cirrhosis self-management toolkit 4. Assess the impact of the intervention
Audit: methods • Patients with a discharge diagnosis of decompensated cirrhosis were identified using clinical coding • • • Decompensated cirrhosis Ascites Spontaneous bacterial peritonitis Jaundice Variceal bleed Alcoholic/alcohol-related hepatitis • Consecutive cases Jan-Dec 2017 – only first admission counted • Case notes and electronic records reviewed

Baseline results • n=61, 64% male, median 58 years (range 34 to 87) • 74% alcohol-related liver disease • Key findings • Creatinine written in discharge letter in only 1 patient • Written recommendation to check U/Es in only 24% of those on diuretics • 30 day re-admissions – 18 patients (30%) • Not thought preventable - 10 • Unknown – 1 • Potentially preventable 7 (39%) – all ascites presenting to ED • Rest of management was good eg, SBP prophylaxis, HE management, OGDs booked and beta-blockers for varices, thiamine etc
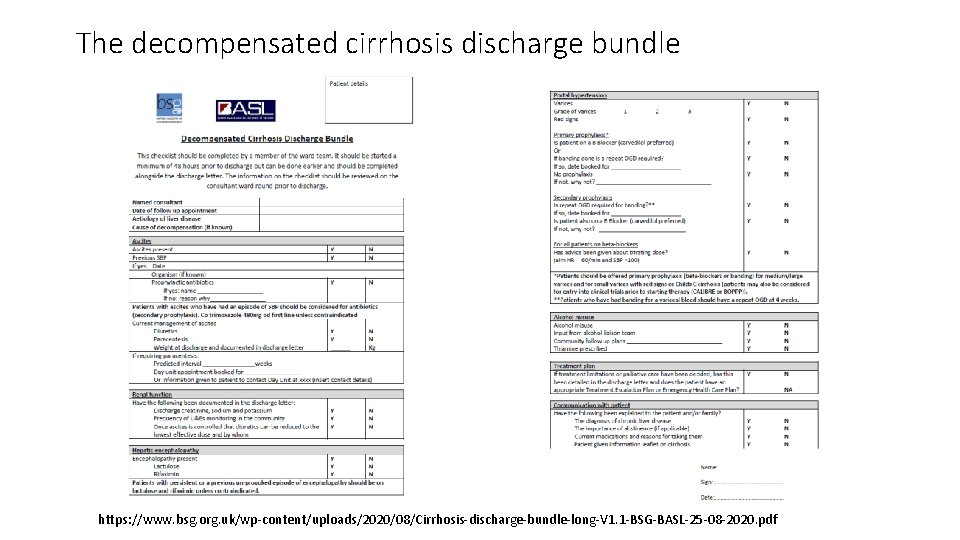
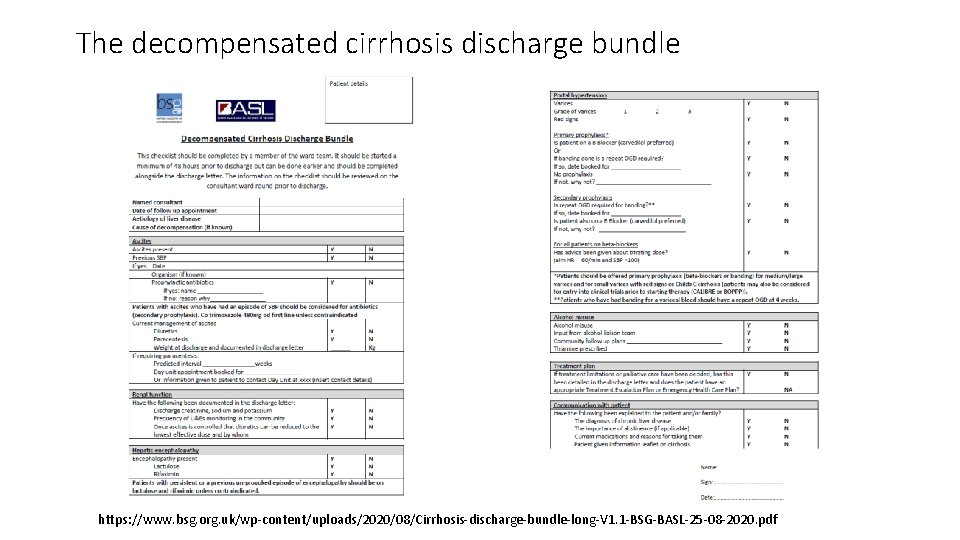
The decompensated cirrhosis discharge bundle https: //www. bsg. org. uk/wp-content/uploads/2020/08/Cirrhosis-discharge-bundle-long-V 1. 1 -BSG-BASL-25 -08 -2020. pdf

The decompensated cirrhosis discharge bundle https: //www. bsg. org. uk/wp-content/uploads/2020/08/Cirrhosis-discharge-bundle-long-V 1. 1 -BSG-BASL-25 -08 -2020. pdf

Give good patient information http: //www. livernorth. org. uk/

Give good patient information http: //www. livernorth. org. uk/

Impact of the intervention Pre- Post-implementation Completed Not completed Total (n) 61 23 (27%) 63 Alcohol team review 64% 81% 66% Community alcohol plan 39% 62% 34% Ascites present 74% 70% 67% Discharge creatinine documented 2% 44% 7% Plan for U&Es check after discharge 24% 54% 48% Variceal bleed 8% 9% 14% B-blockers, repeat OGD planned or TIPSS 100% (5) 100% (2/2) 78% (7/9) Potentially preventable 30 day readmission 39% (7/18) 12% (1/8) 21% (3/14)

Impact of the intervention Pre- Post-implementation Completed Not completed Total (n) 61 23 (27%) 63 Alcohol team review 64% 81% 66% Community alcohol plan 39% 62% 34% Ascites present 74% 70% 67% Discharge creatinine documented 2% 44% 7% Plan for U&Es check after discharge 24% 54% 48% Variceal bleed 8% 9% 14% B-blockers, repeat OGD planned or TIPSS 100% (5) 100% (2/2) 78% (7/9) Potentially preventable 30 day readmission 39% (7/18) 12% (1/8) 21% (3/14)

Impact of the intervention Pre- Post-implementation Completed Not completed Total (n) 61 23 (27%) 63 Alcohol team review 64% 81% 66% Community alcohol plan 39% 62% 34% Ascites present 74% 70% 67% Discharge creatinine documented 2% 44% 7% Plan for U&Es check after discharge 24% 54% 48% Variceal bleed 8% 9% 14% B-blockers, repeat OGD planned or TIPSS 100% (5) 100% (2/2) 78% (7/9) Potentially preventable 30 day readmission 39% (7/18) 12% (1/8) 21% (3/14)

Impact of the intervention Pre- Post-implementation Completed Not completed Total (n) 61 23 (27%) 63 Alcohol team review 64% 81% 66% Community alcohol plan 39% 62% 34% Ascites present 74% 70% 67% Discharge creatinine documented 2% 44% 7% Plan for U&Es check after discharge 24% 54% 48% Variceal bleed 8% 9% 14% B-blockers, repeat OGD planned or TIPSS 100% (5) 100% (2/2) 78% (7/9) Potentially preventable 30 day readmission 39% (7/18) 12% (1/8) 21% (3/14)

Impact of the intervention Pre- Post-implementation Completed Not completed Total (n) 61 23 (27%) 63 Alcohol team review 64% 81% 66% Community alcohol plan 39% 62% 34% Ascites present 74% 70% 67% Discharge creatinine documented 2% 44% 7% Plan for U&Es check after discharge 24% 54% 48% Variceal bleed 8% 9% 14% B-blockers, repeat OGD planned or TIPSS 100% (5) 100% (2/2) 78% (7/9) Potentially preventable 30 day readmission 39% (7/18) 12% (1/8) 21% (3/14)

Impact of the intervention Pre- Post-implementation Completed Not completed Total (n) 61 23 (27%) 63 Alcohol team review 64% 81% 66% Community alcohol plan 39% 62% 34% Ascites present 74% 70% 67% Discharge creatinine documented 2% 44% 7% Plan for U&Es check after discharge 24% 54% 48% Variceal bleed 8% 9% 14% B-blockers, repeat OGD planned or TIPSS 100% (5) 100% (2/2) 78% (7/9) Potentially preventable 30 day readmission 39% (7/18) 12% (1/8) 21% (3/14)
Conclusions from audit • Re-admission rates for decompensated cirrhotics are high • Use of the discharge bundle was associated with improvement in some aspects of care at discharge. • Possible reduction in readmissions – number to small to be definitive • Unfortunately completion rates for the bundle were low (27%) so work is needed to ensure bundles are completed for all patients.

Why were completion rates low compared with admission bundle? • We had a CQUIN for the admission bundle – probably helped with uptake • Anecdotally, juniors like the bundle in the beginning when they start because it tells them what to do, but get lazy once they know what is needed at discharge • Time is always an issue for getting discharge paperwork sorted – bundle should be done well before actual discharge • Need the whole team behind an intervention • Move to electronic record should help with completion rates – next phase of the work.

Acknowledgements • Dr Jess Dyson • Dr Laura Jopson • Dr Philip Copeman • Dr Jennifer Gallacher • Dr Amy Johnston • Dr Titilope Majiyagbe

Questions? stuart. mcpherson 2@nhs. net