Improving Patient Safety in the NHS Sarah Tilford




- Slides: 23
Improving Patient Safety in the NHS Sarah Tilford Improvement Manager Patient Safety NHS Improvement 2 November 2016
This session • To introduce the national vision for improving patient safety • To give a brief overview of our key work programmes • To illustrate how your collaborative work connects with the national safety improvement priorities 2
The NHS in 2016 • • Over 1 million patients every 36 hours 15. 462 m hospital admissions £ 116. 574 bn planned net expenditure In England: - 155 acute trusts - 56 mental health trusts - 34 community providers - 10 ambulance trusts - c 8, 000 GP practices c 150, 273 doctors c 377, 191 qualified nursing staff 1. 4 Million make it possible
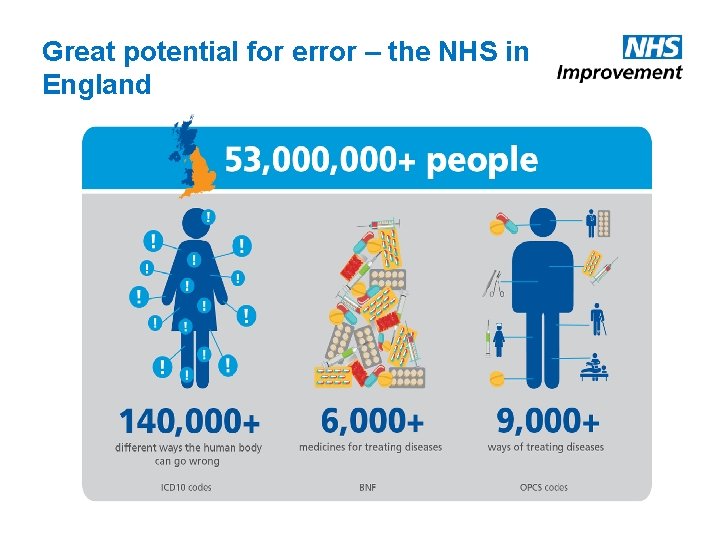
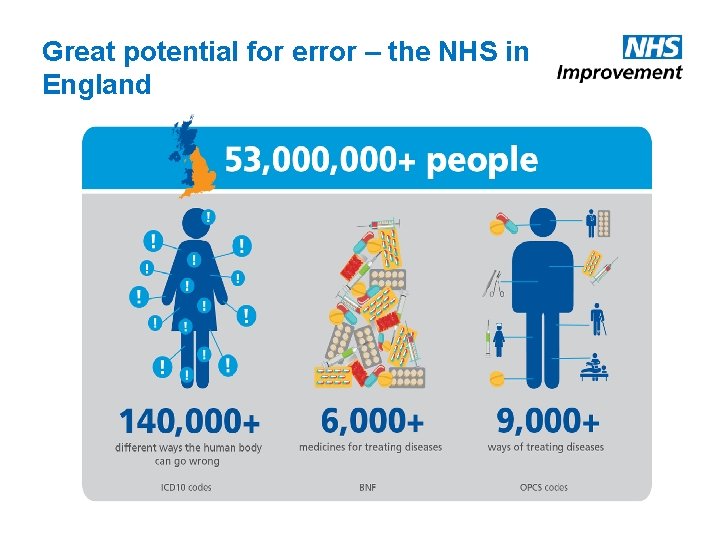
Great potential for error – the NHS in England

Influencing Factors • • 6 System pressures - access, targets , finance Human factors e. g. Slips / lapses System design - fragmented /environmental Organisation v patient centred Cultural norms or behaviours Leadership and teamwork Transparency – ability to listen and learn from error or near misses

Improving the safety of patients in England “The most important single change in the NHS in response to this report would be for it to become, more than ever before, a system devoted to continual learning and improvement of patient care, top to bottom and end to end. ” Professor Don Berwick 7
Patient Safety Vision for 2020 We want to support the NHS to become a system devoted to continuous learning and improvement of patient safety. Increasing our understanding of what goes wrong in healthcare 8 Enhancing the capability and capacity of the NHS to improve safety By tackling the major underlying barriers to widespread safety improvement
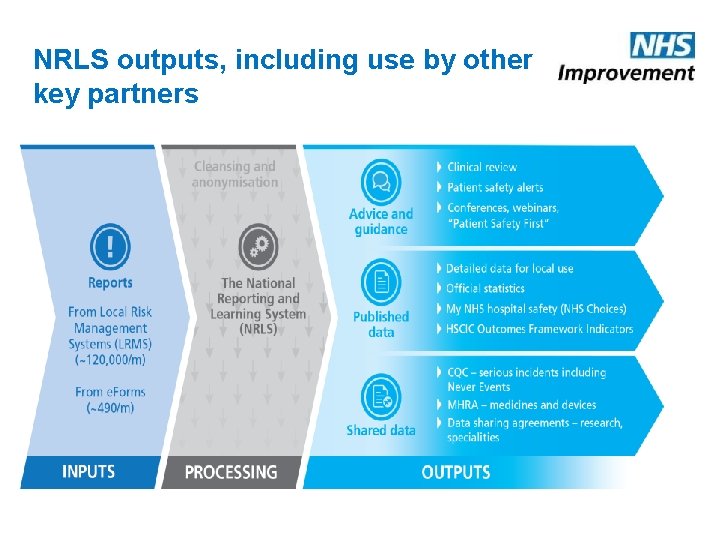
Understanding what goes wrong Our two specific statutory duties apply to all NHS-funded care: • The responsibility for the National Reporting and Learning System • The responsibility for using that information to provide advice and guidance to the NHS ‘for the purposes of maintaining and improving the safety of the services provided by the health service’ (Health and Social Care Act 2012 part 1, section 23, clause 13 R). 9
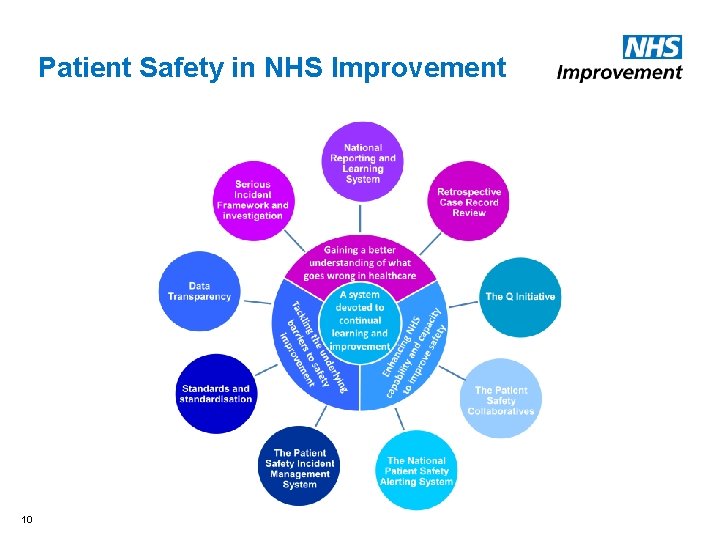
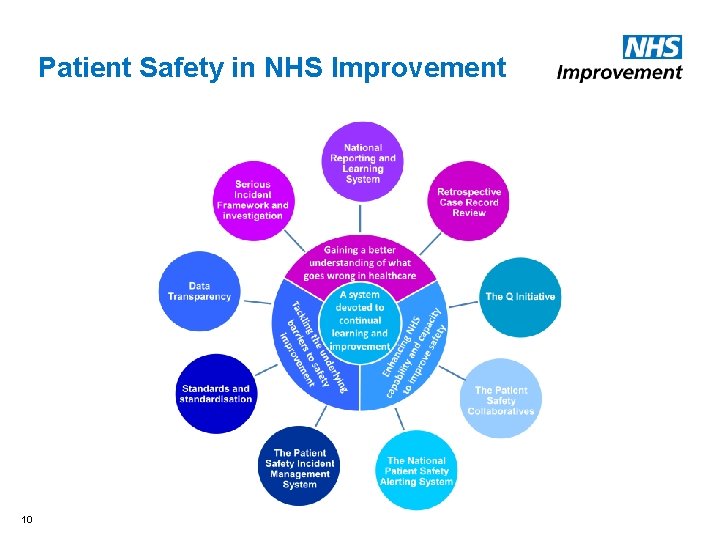
Patient Safety in NHS Improvement 10
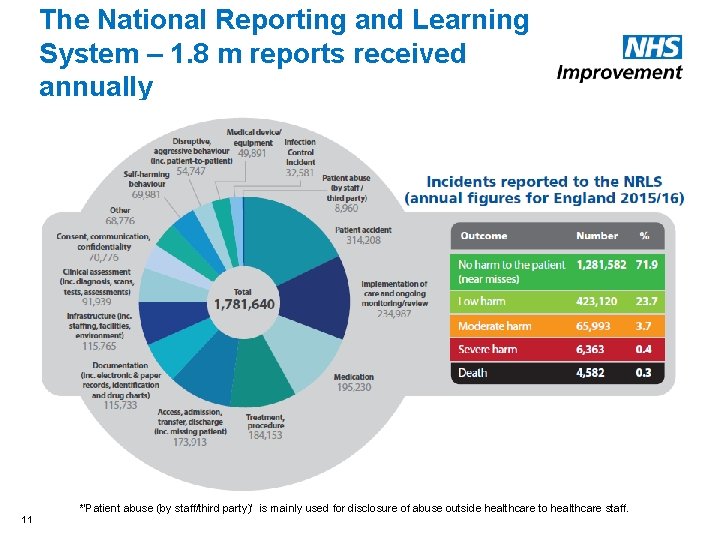
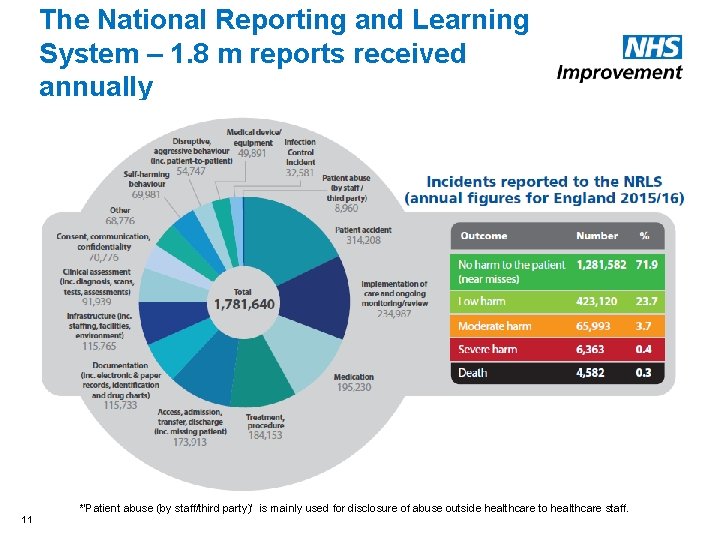
The National Reporting and Learning System – 1. 8 m reports received annually 11 *’Patient abuse (by staff/third party)’ is mainly used for disclosure of abuse outside healthcare to healthcare staff.
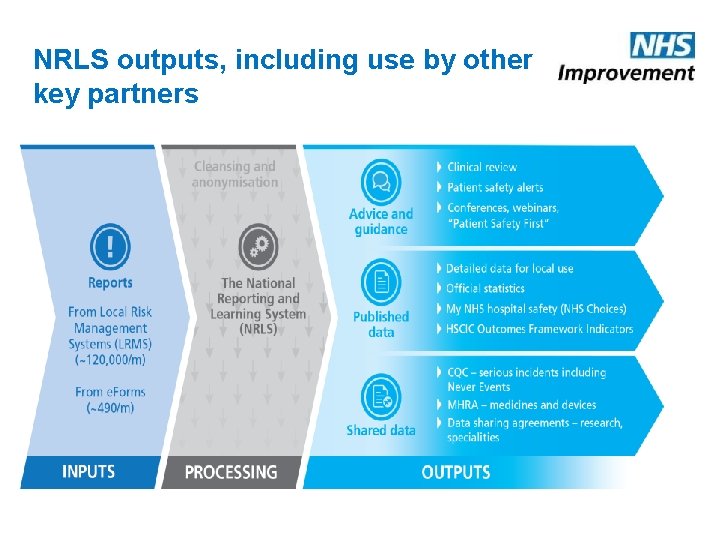
NRLS outputs, including use by other key partners

Patient Safety in NHS Improvement 13
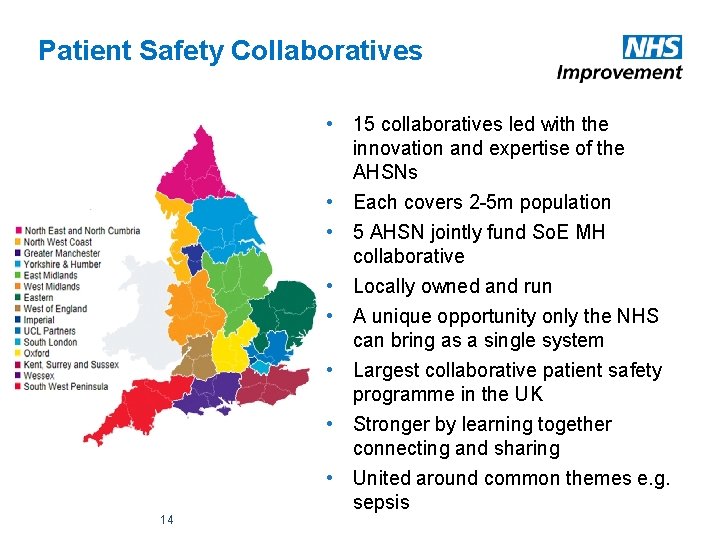
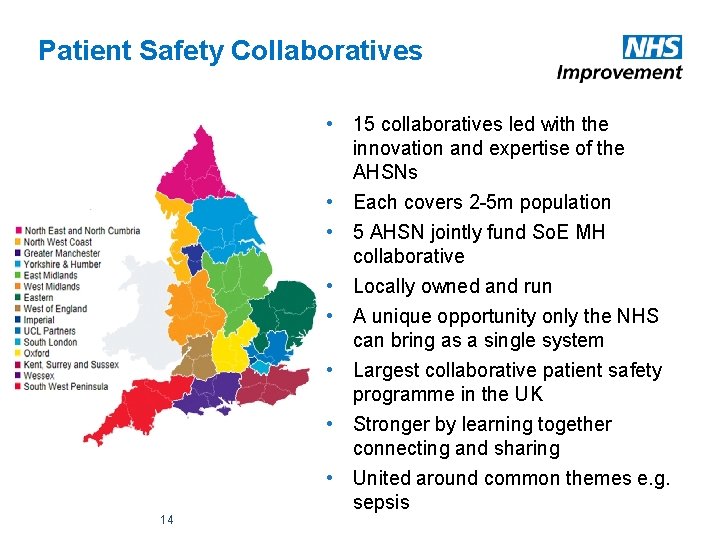
Patient Safety Collaboratives • 15 collaboratives led with the innovation and expertise of the AHSNs • Each covers 2 -5 m population • 5 AHSN jointly fund So. E MH collaborative • Locally owned and run • A unique opportunity only the NHS can bring as a single system • Largest collaborative patient safety programme in the UK • Stronger by learning together connecting and sharing • United around common themes e. g. sepsis 14
Mental Health Collaborative • Longest running MH collaborative – since 2011 • Long history of learning and development across organisations • 160 teams engaged in QI • Gained expertise and independence from IHI • Cost effective 15
South England MH Collaborative Impact Good examples of progress and impact • 50% reduction in AWOL • 23% reduction in prone restraints • 46% reduction in seclusion incidents • 85% reduction in self harm incidents in 1 ward • Executive teams engaged - resolving problems & hearing concerns 16
Collaborative effort – keep going • Focus on local safety concerns in your sector • Develop and test solutions and ideas • Lead implementation of evidence based safer care initiatives • Challenge the status quo • Develop approach adoption and spread (steal with pride) • Harness talents, listen and learn, keep patients at the centre of all you do • Build on your own QI / leadership capability • Increased connectivity, engage in networks e. g. Q, SU 2 S
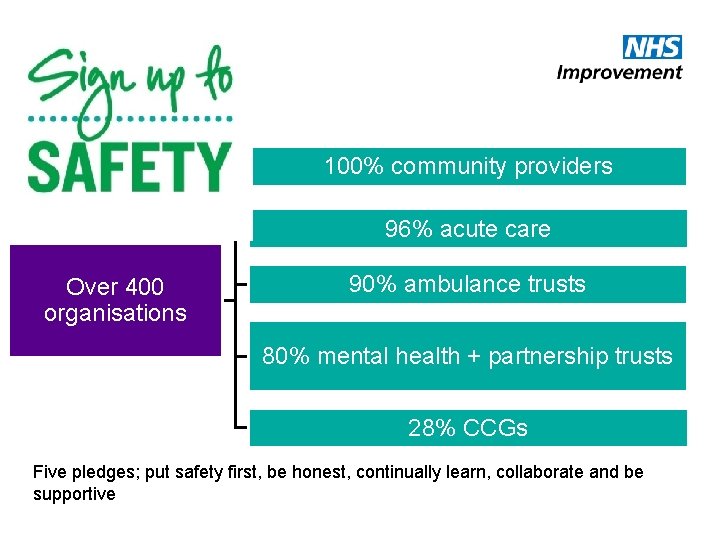
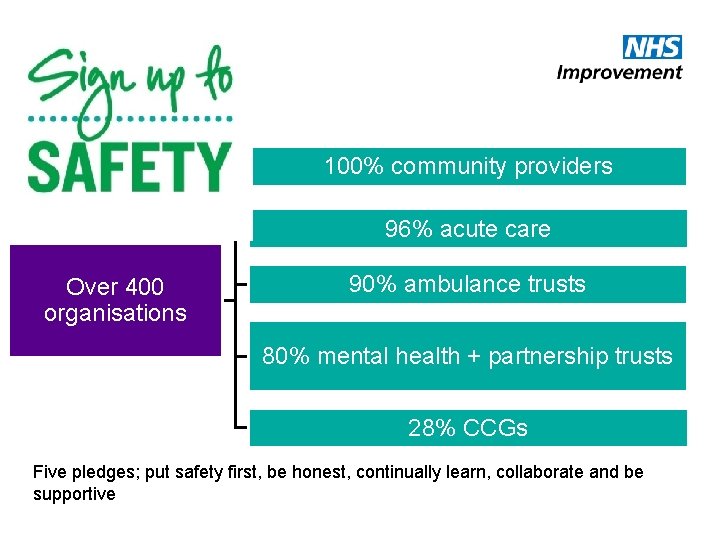
100% community providers 96% acute care Over 400 organisations 90% ambulance trusts 80% mental health + partnership trusts 28% CCGs Five pledges; put safety first, be honest, continually learn, collaborate and be supportive
About Q • Diverse community of people working in improvement in health and care across the UK • Collaboratively designed with 447 members building to 5000 over 5 years • Make it easier for people leading improvement to share ideas, enhance their skills and make changes that bring improvements to health and care • Opportunities to join www. health. org. uk/q for more details 19
Collective Focus for 16/17 • Do more of what works well • Push adoption and spread - identifying key improvements of national significance • Scale up local projects, capture learning and share • Greater focus on – innovation in healthcare – strengthening Incident investigation and learning – leadership and capability building – measure impact and showcase success • Explore culture, behaviours, relationships and human factors
“Systems awareness and systems design are important for health professionals, but they are not enough. They are enabling mechanisms only. It is the ethical dimensions of individuals that are essential to a system’s success. Ultimately, the secret of quality is love. ” Professor Avedis Donabedian
Relationships are key…

THANK YOU s. tilford@nhs. net @sarah_tilford