Improving Corneal Symmetry Visual Acuity in Keratoconus with
- Slides: 12
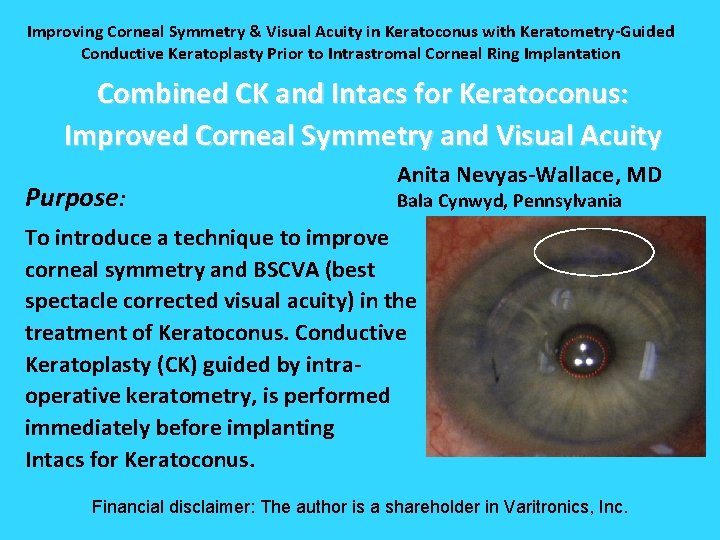
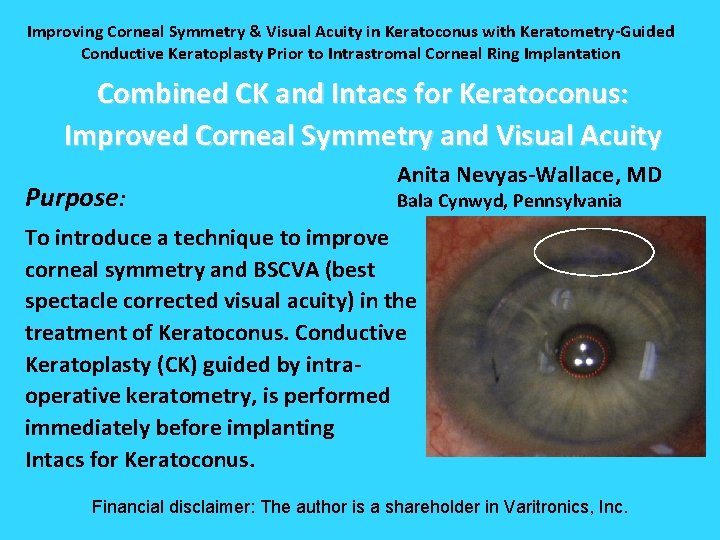
Improving Corneal Symmetry & Visual Acuity in Keratoconus with Keratometry-Guided Conductive Keratoplasty Prior to Intrastromal Corneal Ring Implantation Combined CK and Intacs for Keratoconus: Improved Corneal Symmetry and Visual Acuity Purpose: Anita Nevyas-Wallace, MD Bala Cynwyd, Pennsylvania To introduce a technique to improve corneal symmetry and BSCVA (best spectacle corrected visual acuity) in the treatment of Keratoconus. Conductive Keratoplasty (CK) guided by intraoperative keratometry, is performed immediately before implanting Intacs for Keratoconus. Financial disclaimer: The author is a shareholder in Varitronics, Inc.
Method Report of 3 cases of keratoconus treated with 4 - 6 CK spots placed at the 9 mm optical zone immediately before implantation of a single Intacs segment (Addition Technology, Des Plaines, IL) in the maximally elevated hemi-meridian. Pressing with a blunt instrument mimics the effect of corneal steepening and shrinkage from a CK spot placement is determined by pressing on the cornea in different hemi-meridians and assessing which most circularizes the egg-shaped reflection of the “ring of lights” of the operative keratometer (Varitronics, Inc. , Broomall, PA). Successive spots are placed (maximum six), until slight overcorrection is observed.
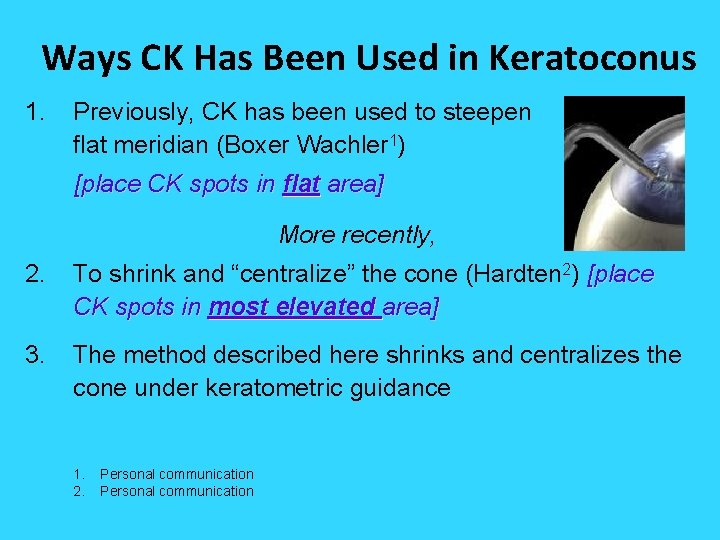
Ways CK Has Been Used in Keratoconus 1. Previously, CK has been used to steepen flat meridian (Boxer Wachler 1) the [place CK spots in flat area] More recently, 2. To shrink and “centralize” the cone (Hardten 2) [place CK spots in most elevated area] 3. The method described here shrinks and centralizes the cone under keratometric guidance 1. 2. Personal communication
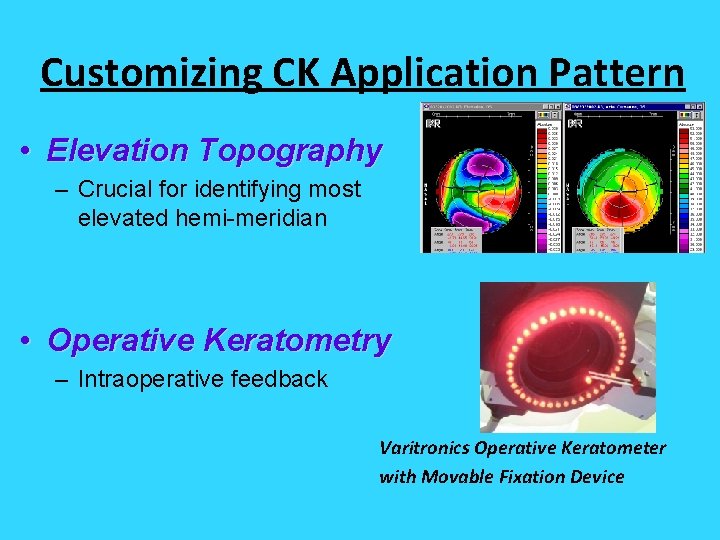
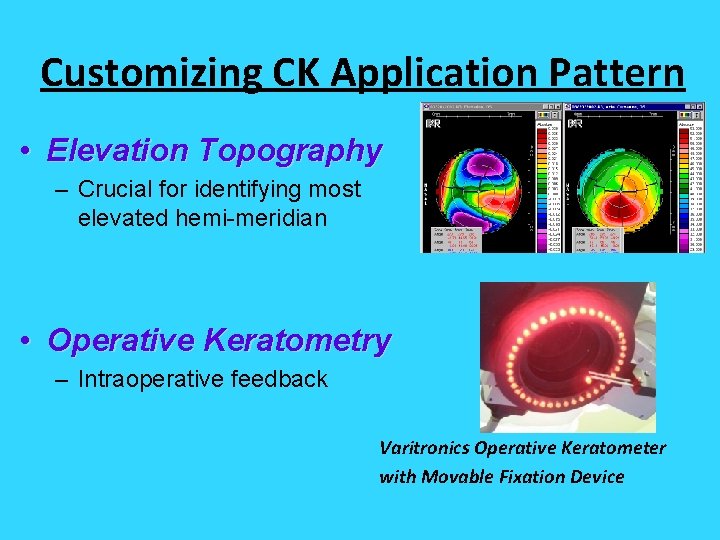
Customizing CK Application Pattern • Elevation Topography – Crucial for identifying most elevated hemi-meridian • Operative Keratometry – Intraoperative feedback Varitronics Operative Keratometer with Movable Fixation Device
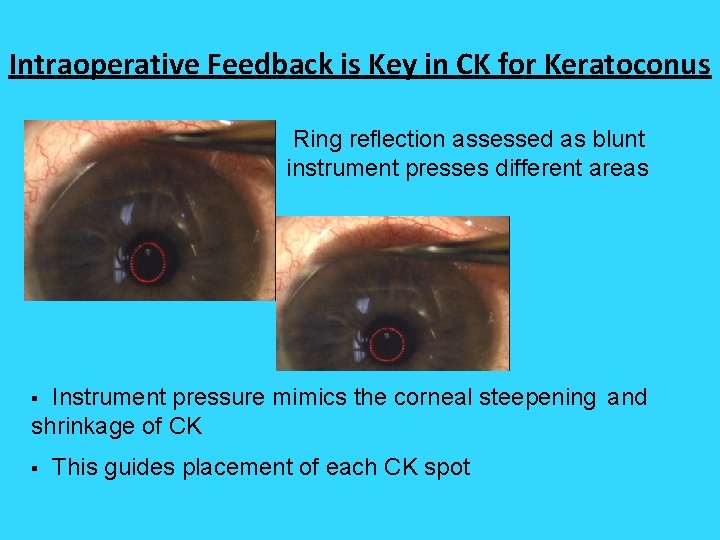
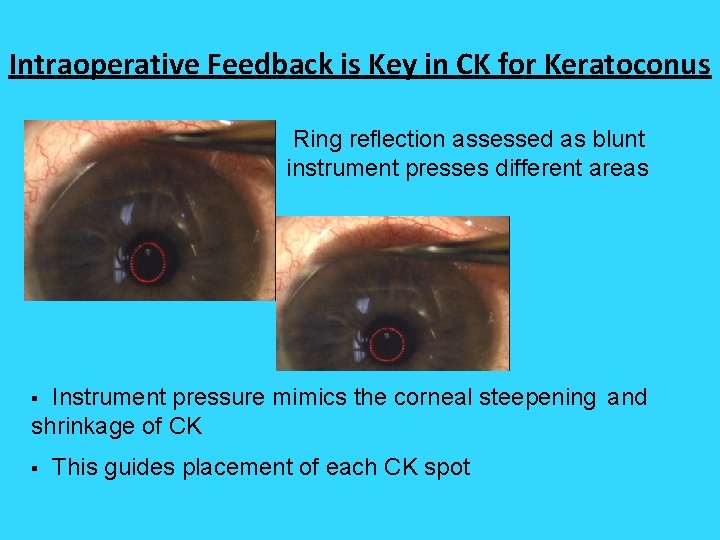
Intraoperative Feedback is Key in CK for Keratoconus Ring reflection assessed as blunt instrument presses different areas Instrument pressure mimics the corneal steepening and shrinkage of CK § § This guides placement of each CK spot
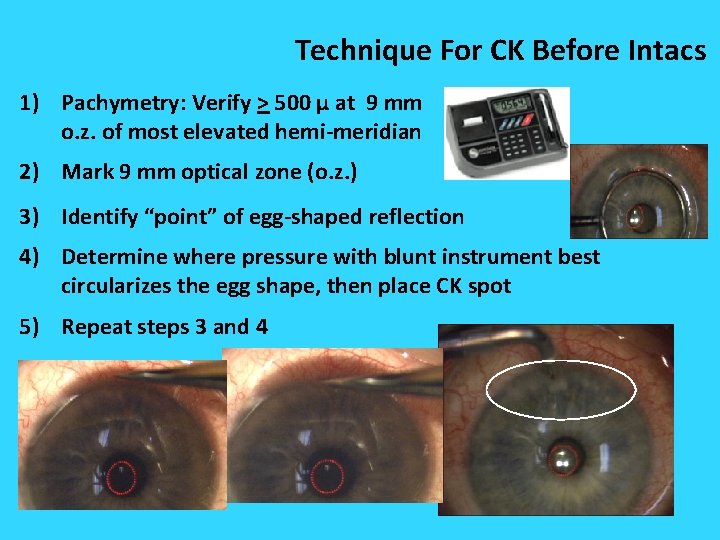
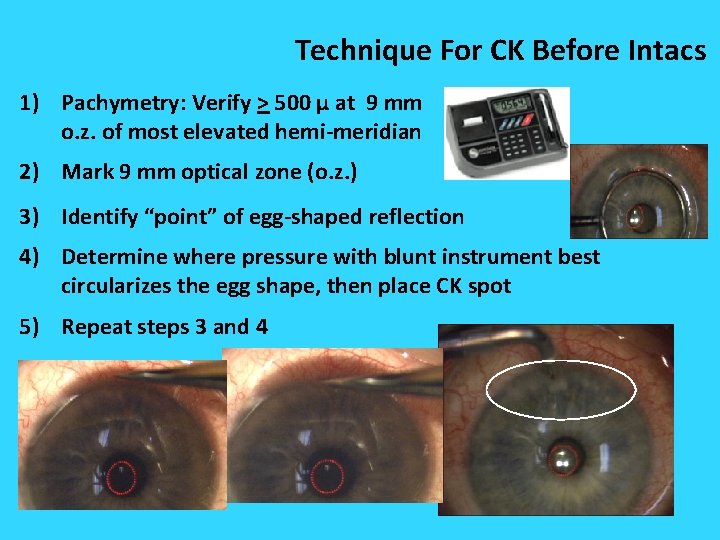
Technique For CK Before Intacs 1) Pachymetry: Verify > 500 μ at 9 mm o. z. of most elevated hemi-meridian 2) Mark 9 mm optical zone (o. z. ) 3) Identify “point” of egg-shaped reflection 4) Determine where pressure with blunt instrument best circularizes the egg shape, then place CK spot 5) Repeat steps 3 and 4
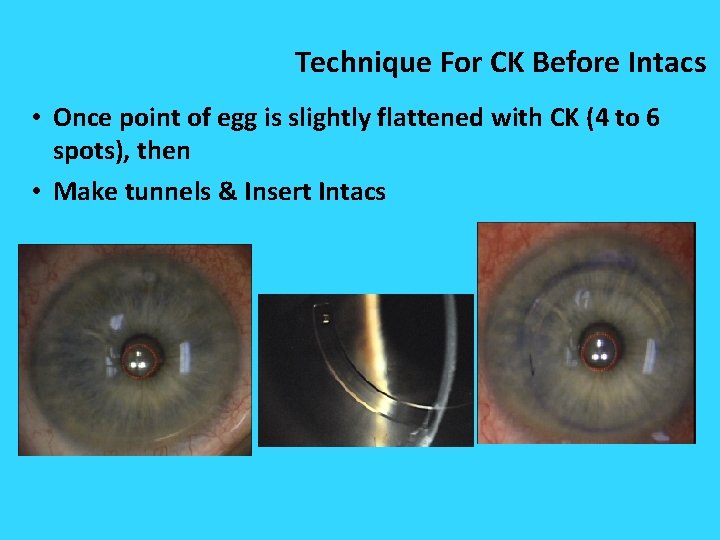
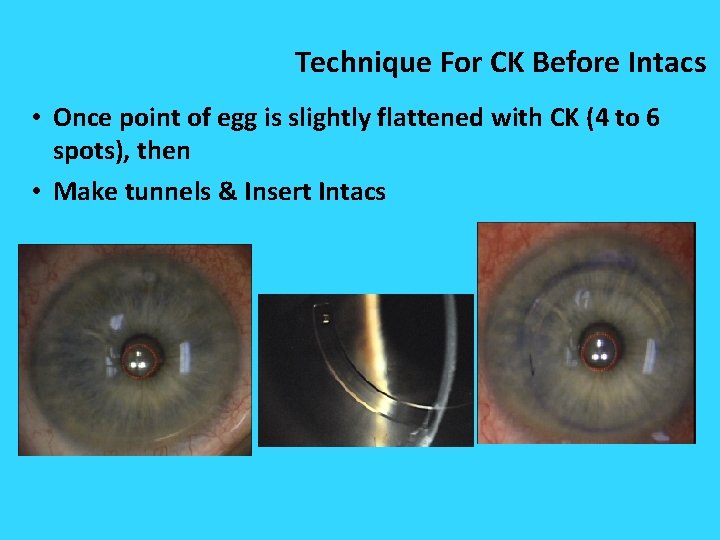
Technique For CK Before Intacs • Once point of egg is slightly flattened with CK (4 to 6 spots), then • Make tunnels & Insert Intacs
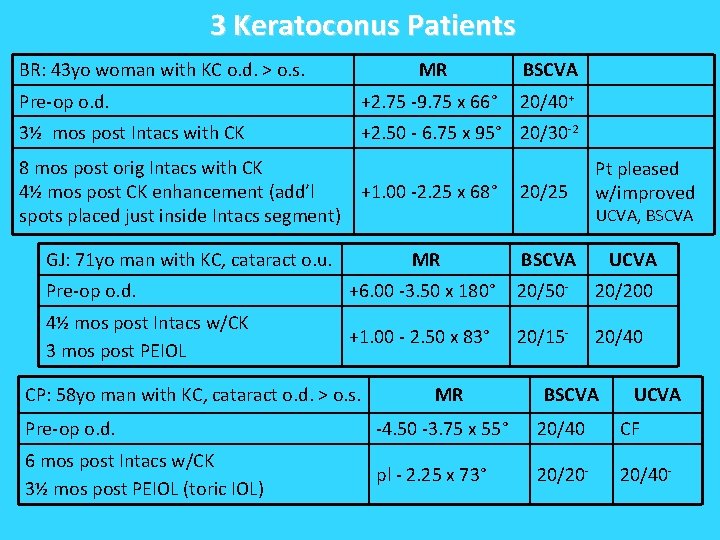
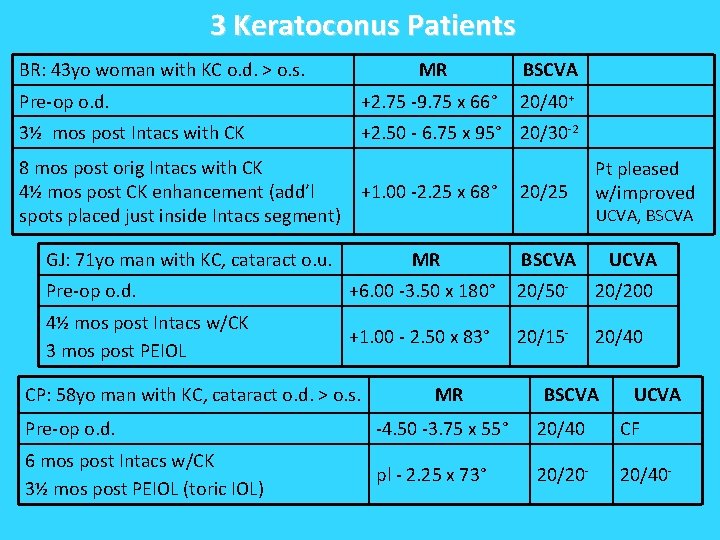
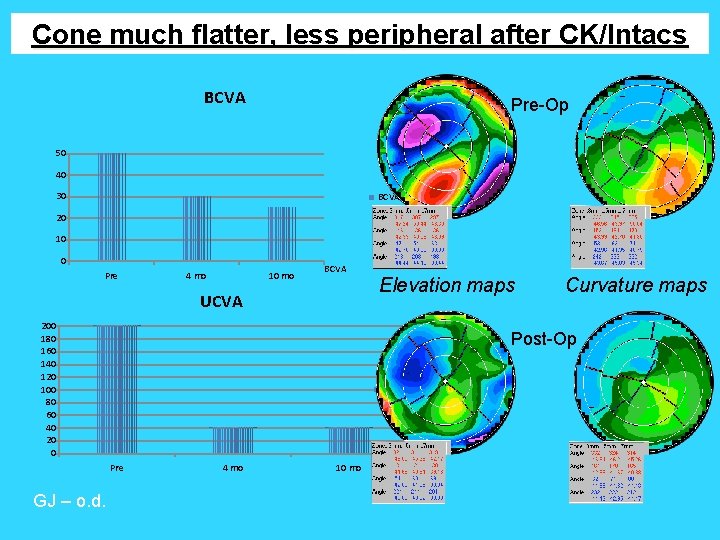
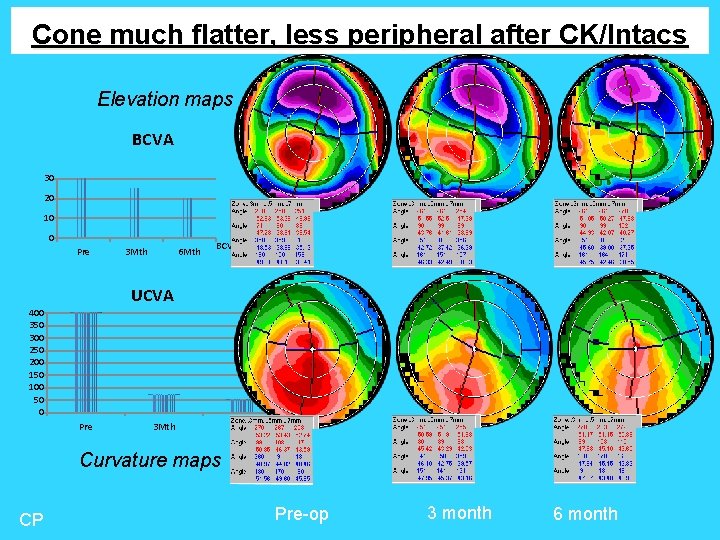
3 Keratoconus Patients BR: 43 yo woman with KC o. d. > o. s. MR BSCVA Pre-op o. d. +2. 75 -9. 75 x 66° 20/40+ 3½ mos post Intacs with CK +2. 50 - 6. 75 x 95° 20/30 -2 8 mos post orig Intacs with CK 4½ mos post CK enhancement (add’l spots placed just inside Intacs segment) +1. 00 -2. 25 x 68° 20/25 Pt pleased w/improved UCVA, BSCVA GJ: 71 yo man with KC, cataract o. u. MR BSCVA Pre-op o. d. +6. 00 -3. 50 x 180° 20/50 - 20/200 4½ mos post Intacs w/CK 3 mos post PEIOL +1. 00 - 2. 50 x 83° 20/15 - 20/40 CP: 58 yo man with KC, cataract o. d. > o. s. MR UCVA BSCVA UCVA Pre-op o. d. -4. 50 -3. 75 x 55° 20/40 CF 6 mos post Intacs w/CK 3½ mos post PEIOL (toric IOL) pl - 2. 25 x 73° 20/20 - 20/40 -
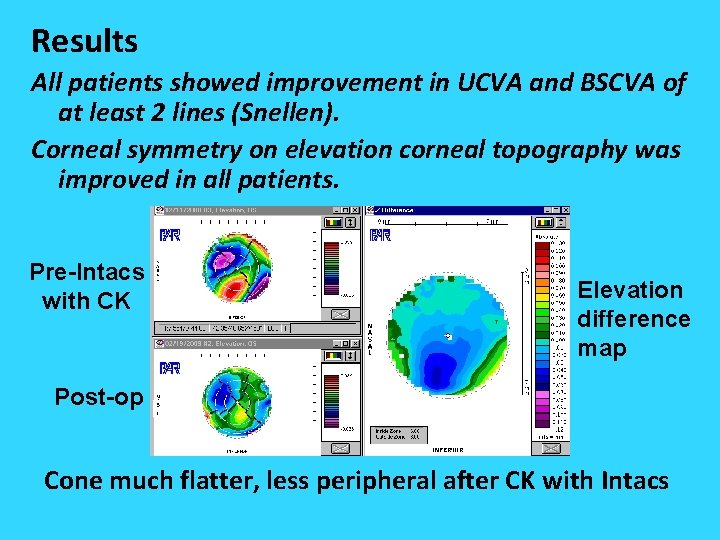
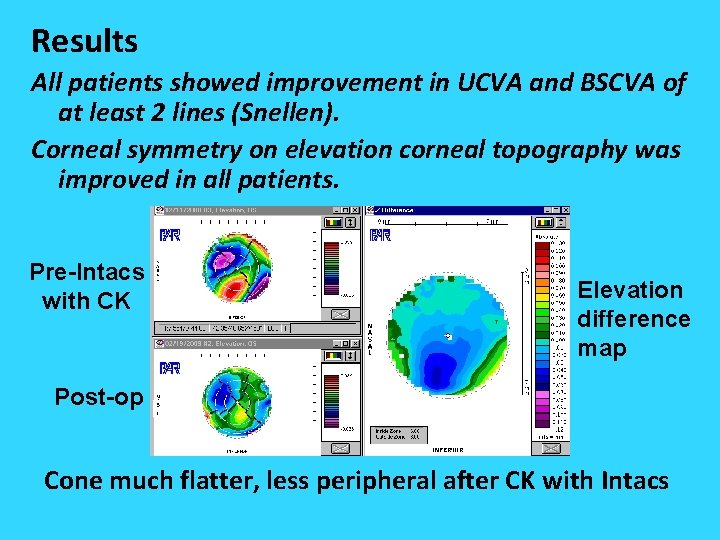
Results All patients showed improvement in UCVA and BSCVA of at least 2 lines (Snellen). Corneal symmetry on elevation corneal topography was improved in all patients. Pre-Intacs with CK Elevation difference map Post-op Post Cone much flatter, less peripheral after CK with Intacs
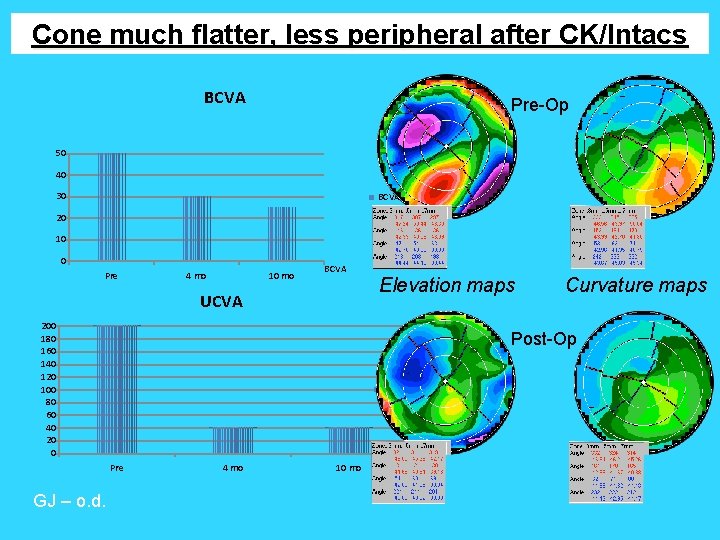
Cone much flatter, less peripheral after CK/Intacs BCVA Pre-Op 50 40 30 BCVA 20 10 0 Pre 4 mo 10 mo BCVA UCVA 200 180 160 140 120 100 80 60 40 20 0 Curvature maps Post-Op UCVA Pre GJ – o. d. Elevation maps 4 mo 10 mo UCVA
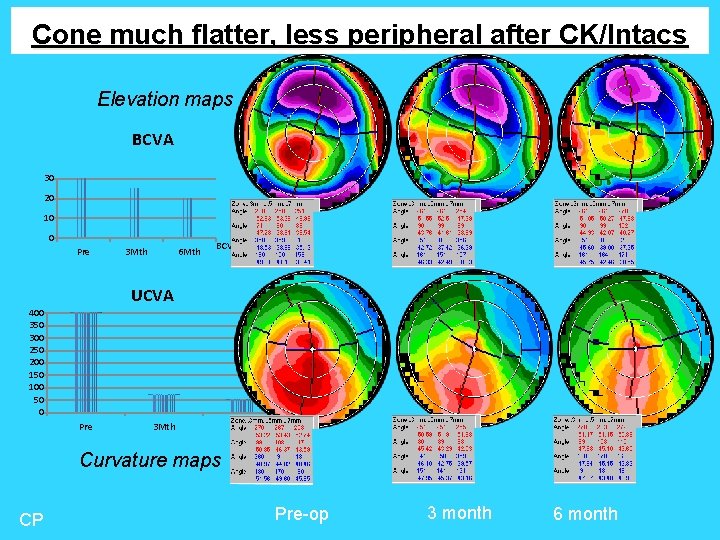
Cone flatter, elevated, more central Cone becomes much flatter, less peripheral after CK/Intacs Elevation maps BCVA 30 20 BCVA 10 0 Pre 3 Mth 6 Mth BCVA UCVA 400 350 300 250 200 150 100 50 0 UCVA Pre 3 Mth 6 Mth UCVA Curvature maps CP Pre-op 3 month 6 month
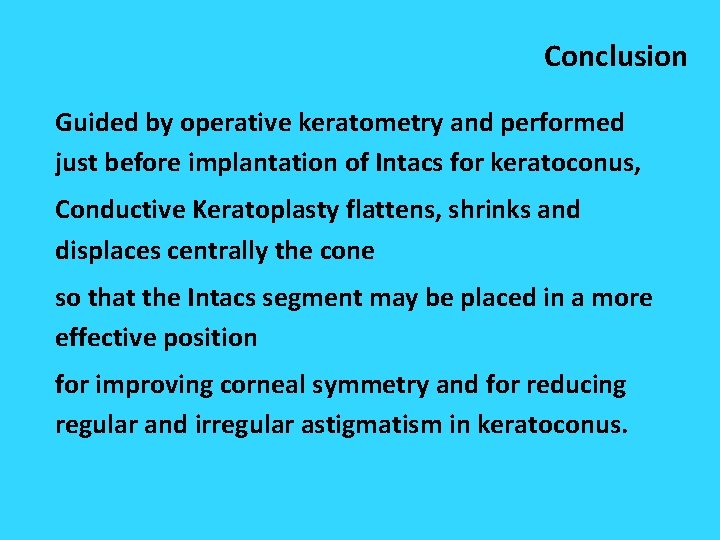
Conclusion Guided by operative keratometry and performed just before implantation of Intacs for keratoconus, Conductive Keratoplasty flattens, shrinks and displaces centrally the cone so that the Intacs segment may be placed in a more effective position for improving corneal symmetry and for reducing regular and irregular astigmatism in keratoconus.