Importance of Bleeding in Patients with Cardiovascular Disease
Importance of Bleeding in Patients with Cardiovascular Disease Roxana Mehran, MD, FACC, FAHA, FESC, FSCAI Professor of Medicine Director, Interventional Cardiovascular Research and Clinical Trials Mount Sinai School of Medicine
Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship Company • Grant/Research Support • Sanofi/BMS- Significant • Consulting Fees/Honoraria • Astra Zeneca, Abbott. Vascular, Ortho Mc. Neal, Regado Biosciences
Impact of Therapies on Outcomes Ischemic events: MI/CKMB↑ Stent Thrombosis Bleeding
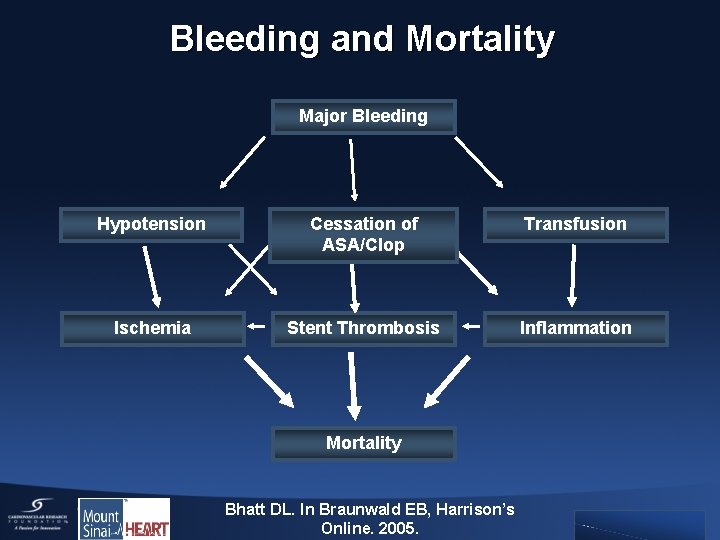
Bleeding and Mortality Major Bleeding Hypotension Cessation of ASA/Clop Transfusion Ischemia Stent Thrombosis Inflammation Mortality Bhatt DL. In Braunwald EB, Harrison’s Online. 2005.
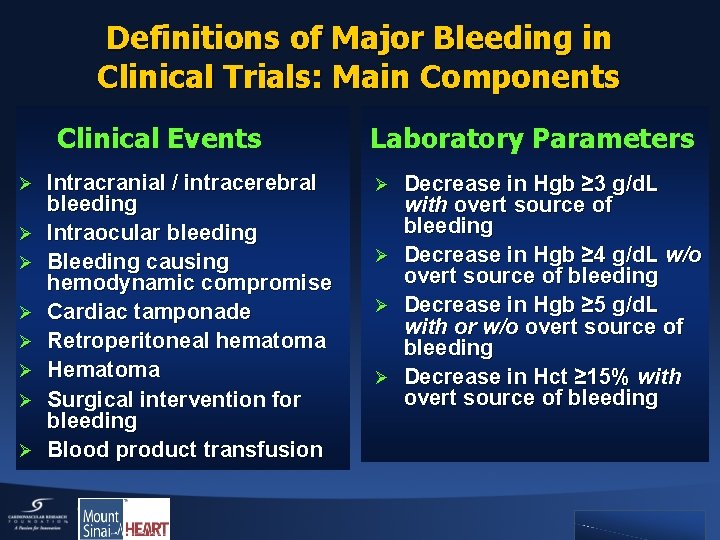
Definitions of Major Bleeding in Clinical Trials: Main Components Clinical Events Ø Ø Ø Ø Intracranial / intracerebral bleeding Intraocular bleeding Bleeding causing hemodynamic compromise Cardiac tamponade Retroperitoneal hematoma Hematoma Surgical intervention for bleeding Blood product transfusion Laboratory Parameters Ø Ø Decrease in Hgb ≥ 3 g/d. L with overt source of bleeding Decrease in Hgb ≥ 4 g/d. L w/o overt source of bleeding Decrease in Hgb ≥ 5 g/d. L with or w/o overt source of bleeding Decrease in Hct ≥ 15% with overt source of bleeding
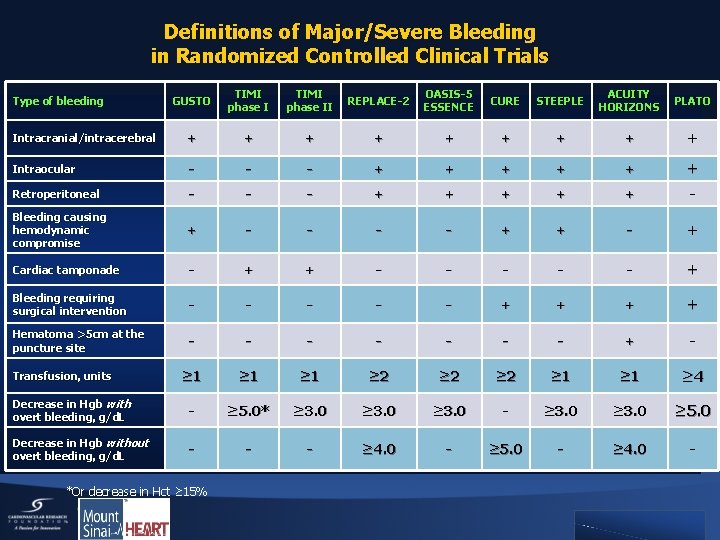
Definitions of Major/Severe Bleeding in Randomized Controlled Clinical Trials GUSTO TIMI phase II REPLACE-2 OASIS-5 ESSENCE CURE STEEPLE ACUITY HORIZONS PLATO Intracranial/intracerebral + + + + + Intraocular - - - + + + Retroperitoneal - - - + + + - Bleeding causing hemodynamic compromise + - - + + - + Cardiac tamponade - + + - - - + Bleeding requiring surgical intervention - - - + + Hematoma >5 cm at the puncture site - - - - + - ≥ 1 ≥ 1 ≥ 2 ≥ 2 ≥ 1 ≥ 4 Decrease in Hgb with overt bleeding, g/d. L - ≥ 5. 0* ≥ 3. 0 - ≥ 3. 0 ≥ 5. 0 Decrease in Hgb without overt bleeding, g/d. L - - - ≥ 4. 0 - ≥ 5. 0 - ≥ 4. 0 - Type of bleeding Transfusion, units *Or decrease in Hct ≥ 15%

Bleeding Definitions TIMI Major Bleeding with >5 g/d. L fall in hgb Intracranial bleeding Intraocular bleeding Access site bleed requiring intervention ≥ 5 cm hematoma at puncture site Reoperation for bleeding Blood product transfusion ACUITY and HORIZONS Major Bleeding Hgb ≥ 3 g/d. L with an overt source TIMI Minor Hgb ≥ 4 g/d. L w/o overt source Retroperitoneal bleeding Gross hematuria or hematemesis Rao AK et al. JACC 1988; 11: 1 -11; Stone GW et al. NEJM 2006; 355: 2203 -16
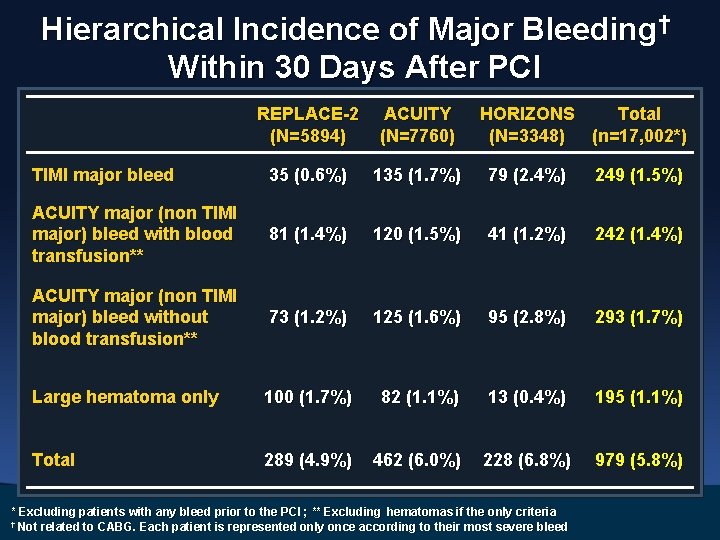
Hierarchical Incidence of Major Bleeding† Within 30 Days After PCI REPLACE-2 (N=5894) ACUITY (N=7760) HORIZONS Total (N=3348) (n=17, 002*) TIMI major bleed 35 (0. 6%) 135 (1. 7%) 79 (2. 4%) 249 (1. 5%) ACUITY major (non TIMI major) bleed with blood transfusion** 81 (1. 4%) 120 (1. 5%) 41 (1. 2%) 242 (1. 4%) ACUITY major (non TIMI major) bleed without blood transfusion** 73 (1. 2%) 125 (1. 6%) 95 (2. 8%) 293 (1. 7%) Large hematoma only 100 (1. 7%) 82 (1. 1%) 13 (0. 4%) 195 (1. 1%) Total 289 (4. 9%) 462 (6. 0%) 228 (6. 8%) 979 (5. 8%) * Excluding patients with any bleed prior to the PCI ; ** Excluding hematomas if the only criteria † Not related to CABG. Each patient is represented only once according to their most severe bleed
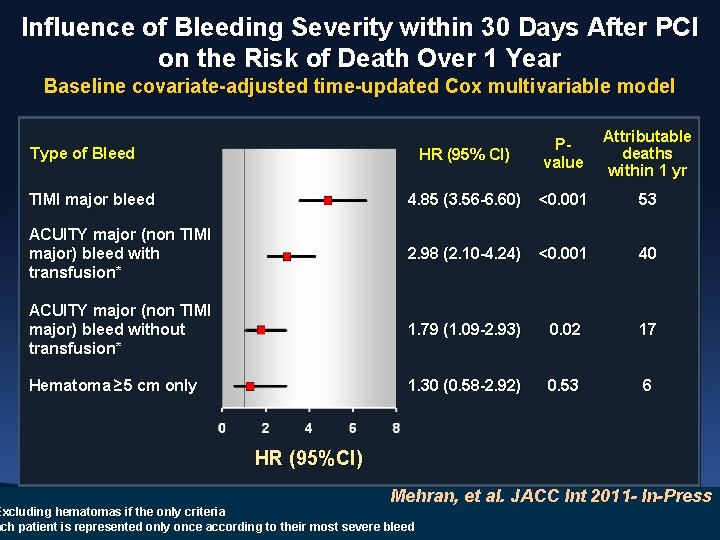
Influence of Bleeding Severity within 30 Days After PCI on the Risk of Death Over 1 Year Baseline covariate-adjusted time-updated Cox multivariable model Attributable deaths within 1 yr HR (95% CI) Pvalue TIMI major bleed 4. 85 (3. 56 -6. 60) <0. 001 53 ACUITY major (non TIMI major) bleed with transfusion* 2. 98 (2. 10 -4. 24) <0. 001 40 ACUITY major (non TIMI major) bleed without transfusion* 1. 79 (1. 09 -2. 93) 0. 02 17 Hematoma ≥ 5 cm only 1. 30 (0. 58 -2. 92) 0. 53 6 Type of Bleed HR (95%CI) Mehran, et al. JACC Int 2011 - In-Press Excluding hematomas if the only criteria ach patient is represented only once according to their most severe bleed
Standardized Bleeding Definitions for Cardiovascular Clinical Trials: A Consensus Report from the Bleeding Academic Research Consortium (BARC) • Roxana Mehran, MD, Sunil V. Rao, MD, Deepak L. Bhatt, MD, MPH, C. Michael Gibson, MS, MD, Adriano Caixeta, MD, Ph. D, John Eikelboom, MD, MBBS, Sanjay Kaul, MD, Stephen D. Wiviott, MD, Venu Menon, MD, Eugenia Nikolsky, MD, Ph. D, Victor Serebruany, MD, Ph. D, Marco Valgimigli, MD, Ph. D, Pascal Vranckx, MD, David Taggart, MD, Ph. D, Joseph F. Sabik, MD, Donald E. Cutlip, MD, Mitchell W. Krucoff, MD, E. Magnus Ohman, MD, Philippe Gabriel Steg, MD, and Harvey White, MB Ch. B DSc Circulation 2011

BARC • • Type 0: No evidence of bleeding. Type 1: Bleeding that is not actionable and does not cause the patient to seek unscheduled performance of studies, hospitalization, or treatment by a health care professional. Examples include, but are not limited to, bruising, hematoma, nosebleeds, or hemorrhoidal bleeding for which the patient does not seek medical attention. Type I bleeding may include episodes that lead to discontinuation of medications by the patient because of bleeding without visiting a health care provider. Circulation 2011

BARC • Type 2: Any clinically overt sign of hemorrhage (e. g. , more bleeding than would be expected for a clinical circumstance; including bleeding found by imaging alone) that is actionable, but does not meet criteria for Type 3 BARC bleeding, • The bleeding must require diagnostic studies, hospitalization or treatment by a health care professional. In particular, the bleeding must meet at least one of the following criteria: ¡ ¡ ¡ 1) Requiring intervention: defined as a health care professional -guided medical treatment or percutaneous intervention to stop or treat bleeding, including temporarily or permanently discontinuing a medication or study drug. 2) Leading to hospitalization or an increased level of care: defined as leading to or prolonging hospitalization or transfer to a hospital unit capable of providing a higher level of care; or 3) Prompting evaluation: defined as leading to an unscheduled visit to a healthcare professional resulting in diagnostic testing (laboratory or imaging). Circulation 2011
BARC • Type 3: Clinical, laboratory, and/or imaging evidence of bleeding with specific healthcare provider responses, as listed below: • a. BARC Type 3 a Bleeding • Any transfusion with overt bleeding; Overt bleeding plus hemoglobin drop ≥ 3 to <5 g/d. L* (provided hemoglobin drop is related to bleeding) • • b. BARC Type 3 b Bleeding Overt bleeding plus hemoglobin drop ≥ 5 g/d. L* (provided hemoglobin drop is related to bleed), Cardiac tamponade, Bleeding requiring surgical intervention for control (excluding dental/nasal/skin/hemorrhoid), Bleeding requiring intravenous vasoactive drugs • c. BARC Type 3 c Bleeding • Intracranial hemorrhage (does not include microbleeds or hemorrhagic transformation; does include intraspinal). Intraocular bleed compromising vision Circulation 2011 In-press
BARC Type 4: CABG-Related Bleeding. • Perioperative intracranial bleeding within 48 • • hours Reoperation following closure of sternotomy for the purpose of controlling bleeding Transfusion of ≥ 5 units of whole blood or packed red blood cells within a 48 hour period* Chest tube output ≥ 2 L within a 24 hour period. Notes: If a CABG-related bleed is not adjudicated as at least a Type 3 severity event, it will be classified as ‘not a bleeding event. ’ If a bleeding event occurs with a clear temporal relationship to CABG (i. e. within a 48 hour timeframe) but does not meet Type 4 severity criteria, it will be classified as ‘not a bleeding event’. * only allogenic transfusions are considered as transfusions for CABG-related bleeds Circulation 2011
BARC Type 5: Fatal Bleeding. • Fatal bleeding is bleeding that directly causes • • death with no other explainable cause. BARC Fatal Bleeding is categorized as either definite or probable as follows: a) Probable fatal bleeding (Type 5 a) is bleeding that is clinically suspicious as the cause of death, but the bleeding is not directly observed and there is no autopsy or confirmatory imaging. b) Definite fatal bleeding (Type 5 b) is bleeding that is directly observed (either by clinical specimen – blood, emesis, stool, etc. - or by imaging) or confirmed on autopsy. Circulation 2011
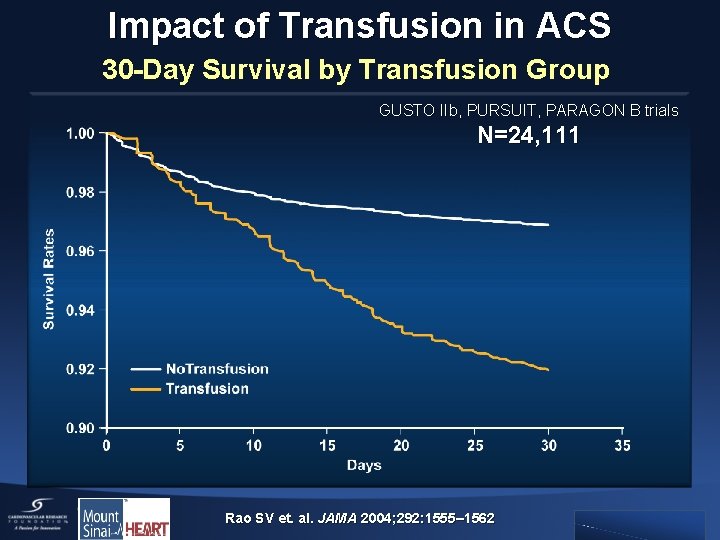
Impact of Transfusion in ACS 30 -Day Survival by Transfusion Group GUSTO IIb, PURSUIT, PARAGON B trials N=24, 111 Rao SV et. al. JAMA 2004; 292: 1555– 1562
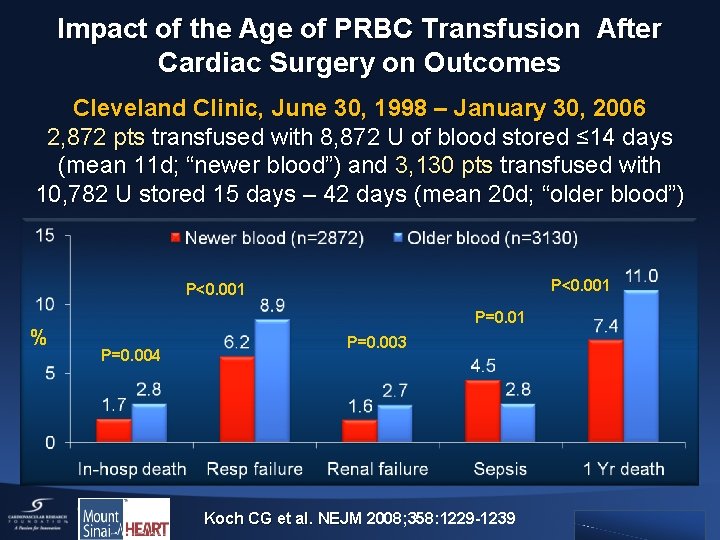
Impact of the Age of PRBC Transfusion After Cardiac Surgery on Outcomes Cleveland Clinic, June 30, 1998 – January 30, 2006 2, 872 pts transfused with 8, 872 U of blood stored ≤ 14 days (mean 11 d; “newer blood”) and 3, 130 pts transfused with 10, 782 U stored 15 days – 42 days (mean 20 d; “older blood”) P<0. 001 % P=0. 01 P=0. 004 P=0. 003 Koch CG et al. NEJM 2008; 358: 1229 -1239 Koch CG et al. NEJM
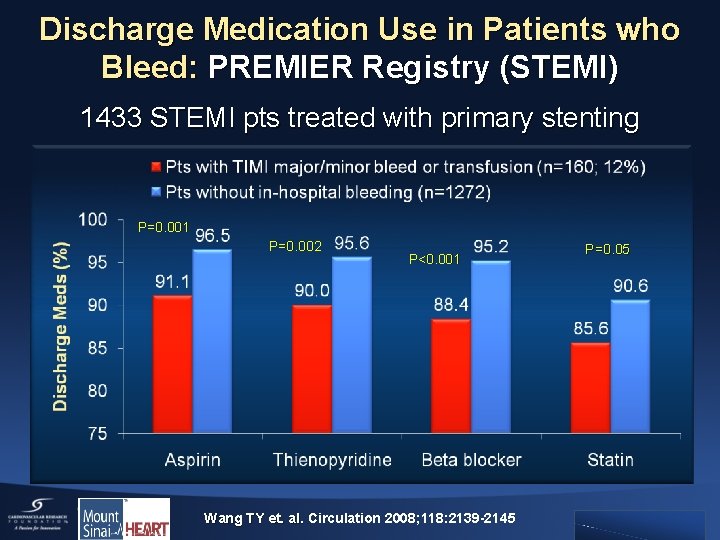
Discharge Medication Use in Patients who Bleed: PREMIER Registry (STEMI) 1433 STEMI pts treated with primary stenting P=0. 001 P=0. 002 P<0. 001 Wang TY et. al. Circulation 2008; 118: 2139 -2145 Wang TY et. al. P=0. 05
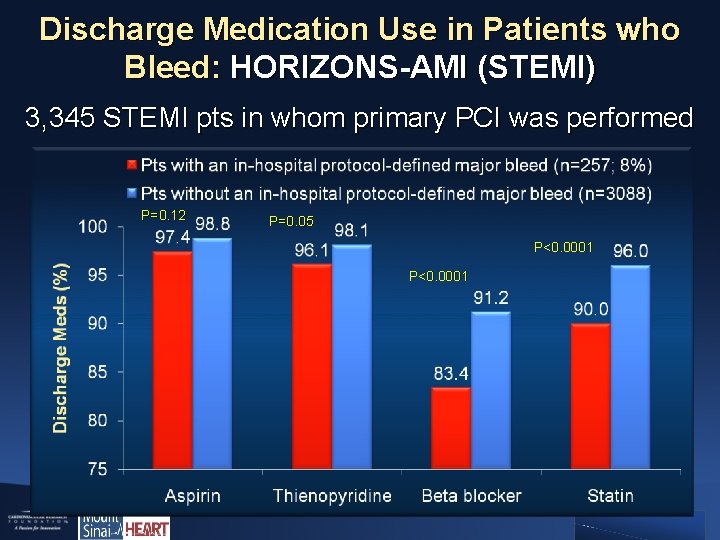
Discharge Medication Use in Patients who Bleed: HORIZONS-AMI (STEMI) 3, 345 STEMI pts in whom primary PCI was performed P=0. 12 P=0. 05 P<0. 0001
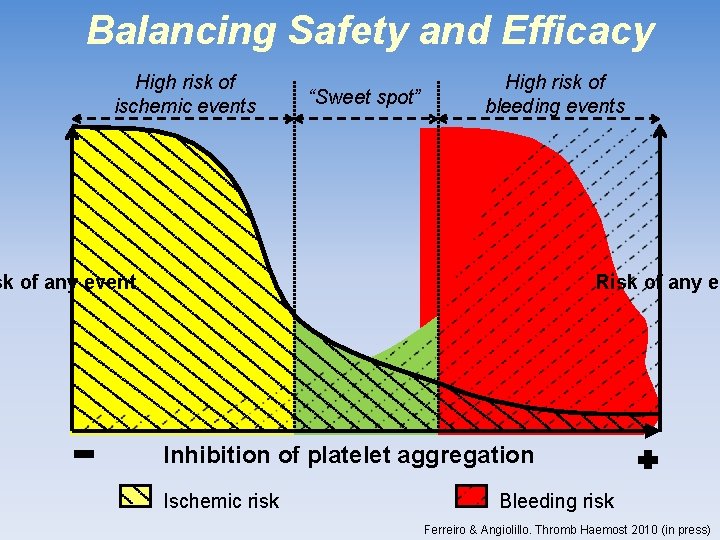
Balancing Safety and Efficacy High risk of ischemic events “Sweet spot” High risk of bleeding events sk of any event Risk of any ev Inhibition of platelet aggregation Ischemic risk Bleeding risk Ferreiro & Angiolillo. Thromb Haemost 2010 (in press)
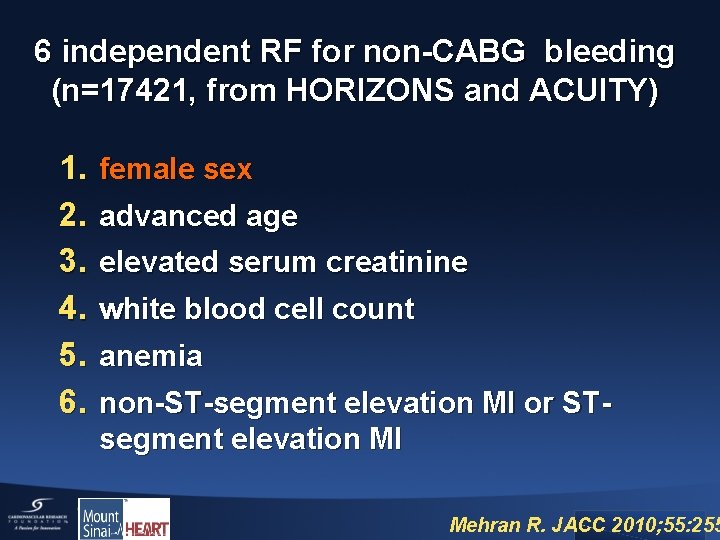
6 independent RF for non-CABG bleeding (n=17421, from HORIZONS and ACUITY) 1. 2. 3. 4. 5. 6. female sex advanced age elevated serum creatinine white blood cell count anemia non-ST-segment elevation MI or STsegment elevation MI Mehran R. JACC 2010; 55: 255
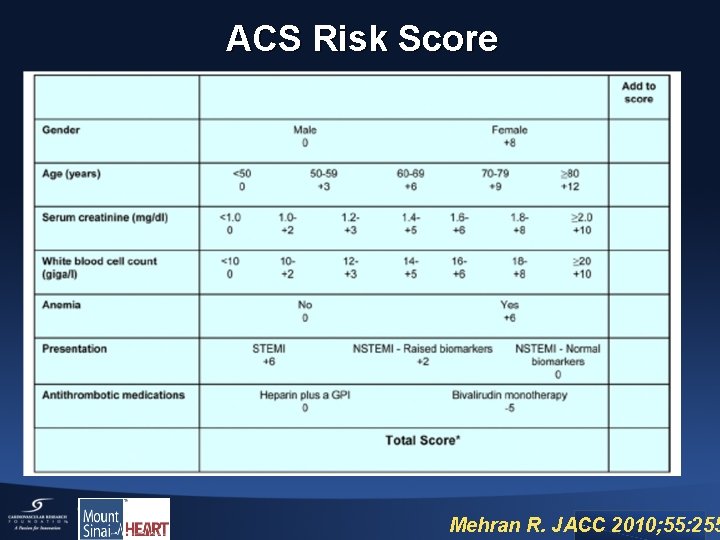
ACS Risk Score Mehran R. JACC 2010; 55: 255
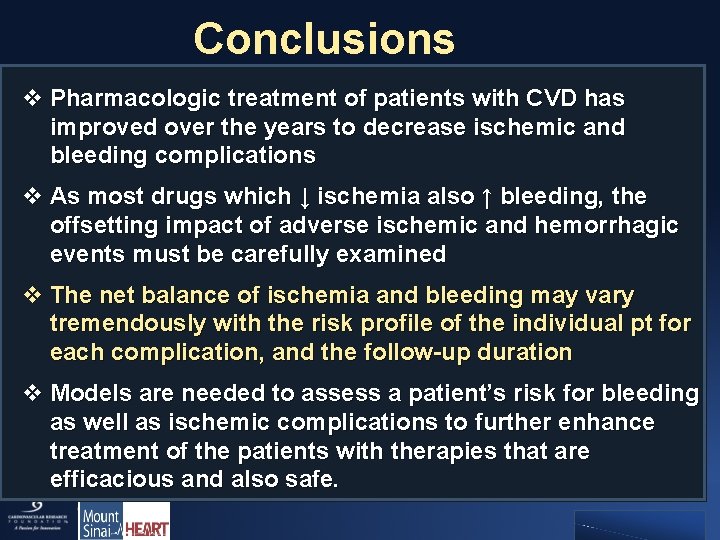
Conclusions v Pharmacologic treatment of patients with CVD has improved over the years to decrease ischemic and bleeding complications v As most drugs which ↓ ischemia also ↑ bleeding, the offsetting impact of adverse ischemic and hemorrhagic events must be carefully examined v The net balance of ischemia and bleeding may vary tremendously with the risk profile of the individual pt for each complication, and the follow-up duration v Models are needed to assess a patient’s risk for bleeding as well as ischemic complications to further enhance treatment of the patients with therapies that are efficacious and also safe.
- Slides: 23