Implementing the New Residency Accreditation Standards and Getting


- Slides: 42
Implementing the New Residency Accreditation Standards and Getting Ready for a Survey David J. Warner, Pharm. D. Director, Center on Practice Development Practice Advancement Office Lead Consultant, ASHP Consulting
Outline • Review current residency capacity • Show the results of the March residency two-phase match process • Provide an update regarding recent Commission on Credentialing decisions • Show current findings of partial compliance with the 2014 PGY 1 standard and how they differ from top findings with the 2005 standard • Describe tips for implementing the new PGY 1 and PGY 2 Standards • Describe tips for getting ready for a survey
Learning Objective • Describe tips for implementing and preparing for a survey of the new PGY 1 and PGY 2 standards.
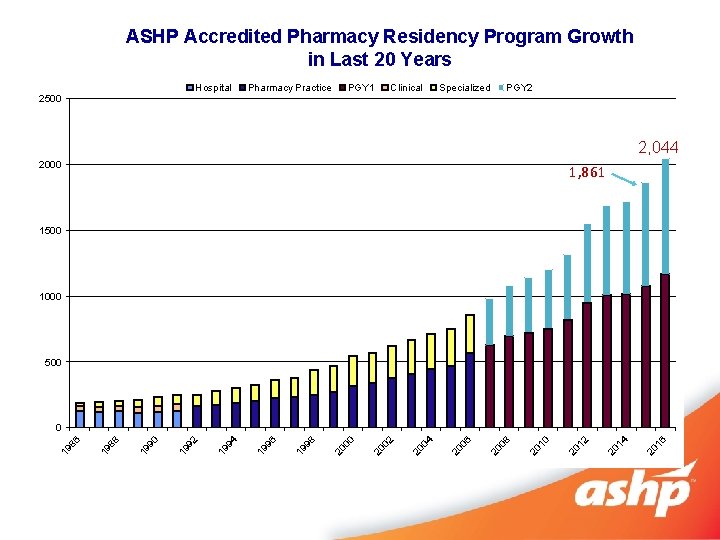
Residency Capacity
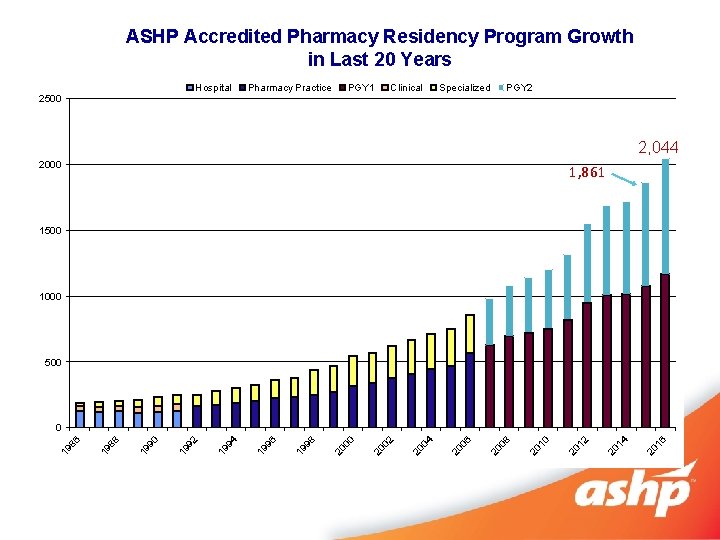
ASHP Accredited Pharmacy Residency Program Growth in Last 20 Years Hospital 2500 Pharmacy Practice PGY 1 Clinical Specialized PGY 2 2, 044 2000 1, 861 1500 1000 500 20 16 20 14 20 12 20 10 20 08 20 06 20 04 20 02 20 00 19 98 19 96 19 94 19 92 19 90 19 88 19 86 0
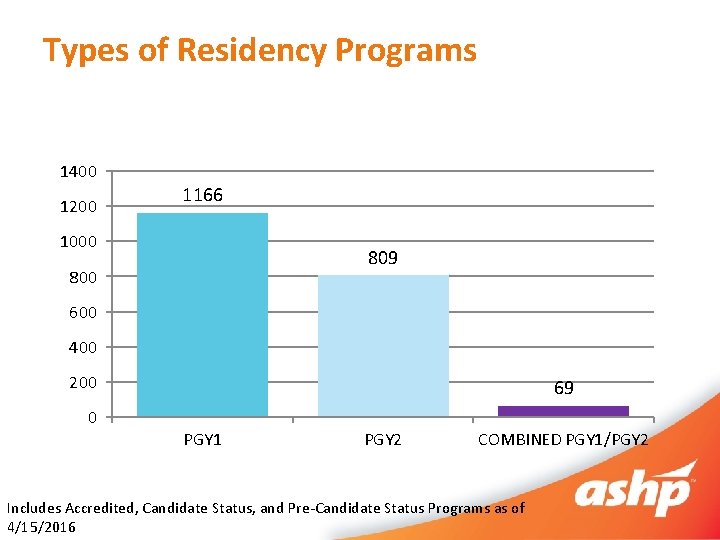
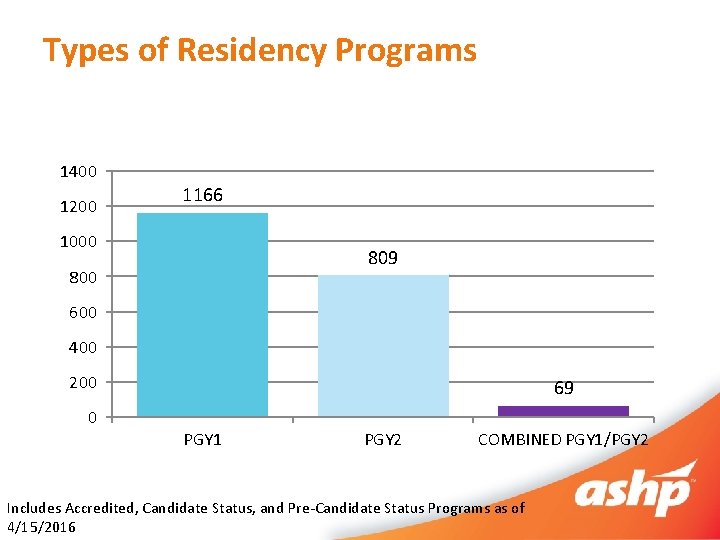
Types of Residency Programs 1400 1200 1166 1000 809 800 600 400 200 0 69 PGY 1 PGY 2 COMBINED PGY 1/PGY 2 Includes Accredited, Candidate Status, and Pre-Candidate Status Programs as of 4/15/2016
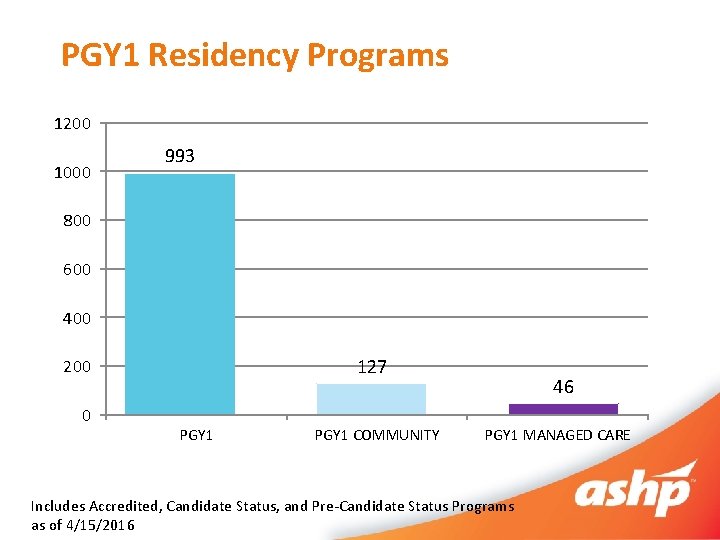
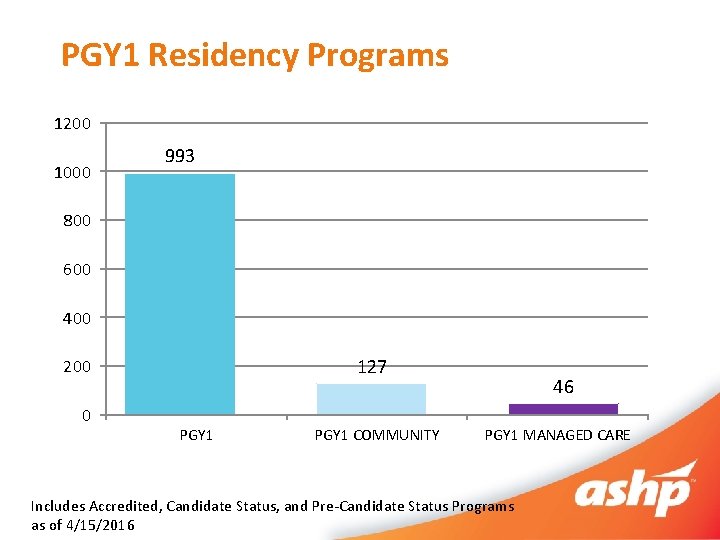
PGY 1 Residency Programs 1200 1000 993 800 600 400 127 200 0 PGY 1 COMMUNITY 46 PGY 1 MANAGED CARE Includes Accredited, Candidate Status, and Pre-Candidate Status Programs as of 4/15/2016
Which type of PGY 2 residency had the largest increase in number of programs between 2015 and 2016? A. B. C. D. Critical Care Ambulatory Care Emergency Medicine Psychiatric Pharmacy
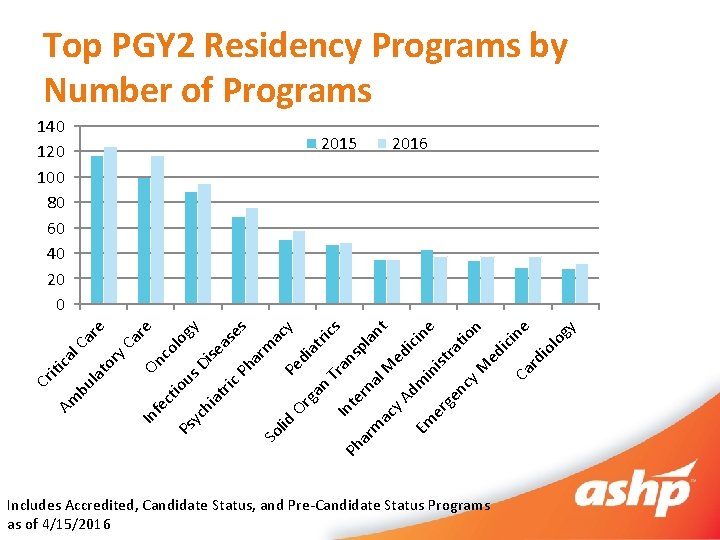
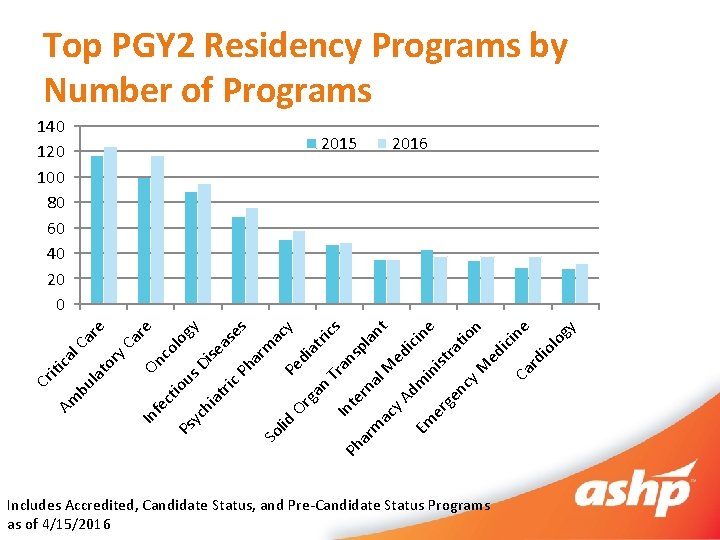
Ph In ga n Or an Tr s ac y at ric di Pe m ar s gy 140 120 100 80 60 40 20 0 te sp rn ar la m al nt ac M y. A ed ici Em dmi ne n er ist ge ra nc t y M ion ed ici ne Ca rd io lo gy lid So lo as e se Di Ph us re Ca co On ry e ar l. C ca iti la to ric at hi yc Ps ct io fe In bu Am Cr Top PGY 2 Residency Programs by Number of Programs 2015 2016 Includes Accredited, Candidate Status, and Pre-Candidate Status Programs as of 4/15/2016
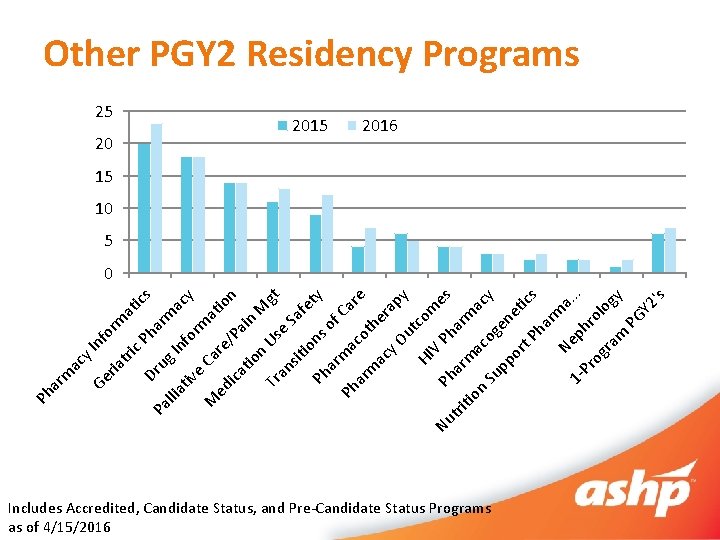
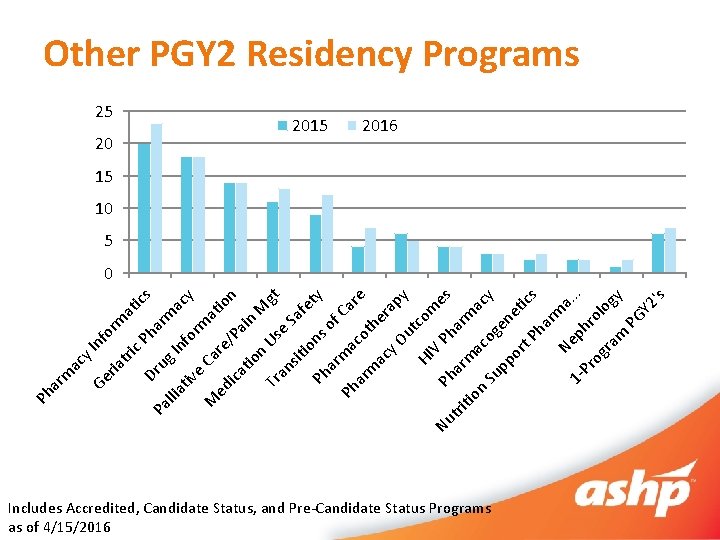
nf or y. I tri ma tic c. P Dr ha s Pa u llia g I rma c tiv nfo rm y e Ca M re atio ed ica /Pa n tio in M n Us gt Tr an e Sa sit fe io ty ns Ph of ar m Ca Ph a re co ar t m ac her y O ap y ut co HI m V Nu Ph es Ph tri ar a tio rm m a ac n og cy Su en pp e or t P tics ha r Ne ma. . 1 Pr phr. o og ra logy m PG Y 2 's ria Ge ac Ph ar m Other PGY 2 Residency Programs 25 20 2015 2016 15 10 5 0 Includes Accredited, Candidate Status, and Pre-Candidate Status Programs as of 4/15/2016
Residency Growth Summary • PGY 1, PGY 2, and combined PGY 1/PGY 2 programs continue to grow • 21% increase in programs in past 3 years • PGY 2 and combined programs outpacing PGY 1 programs in percent growth from 2015 -2016

2016 Two Phase Match
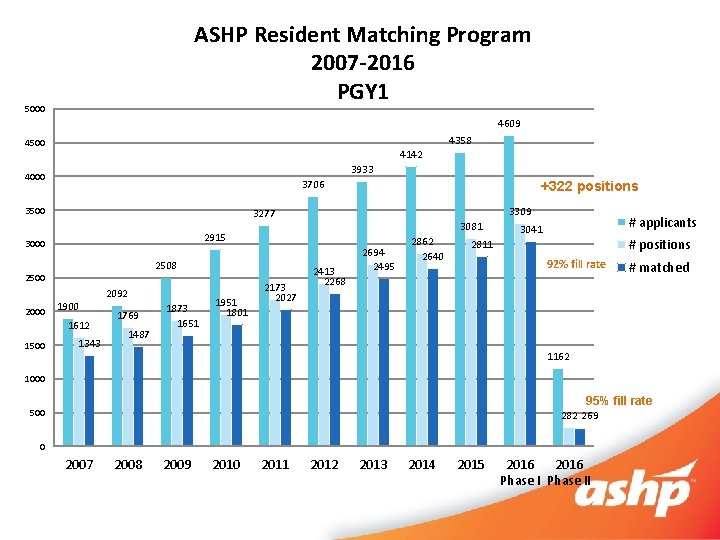
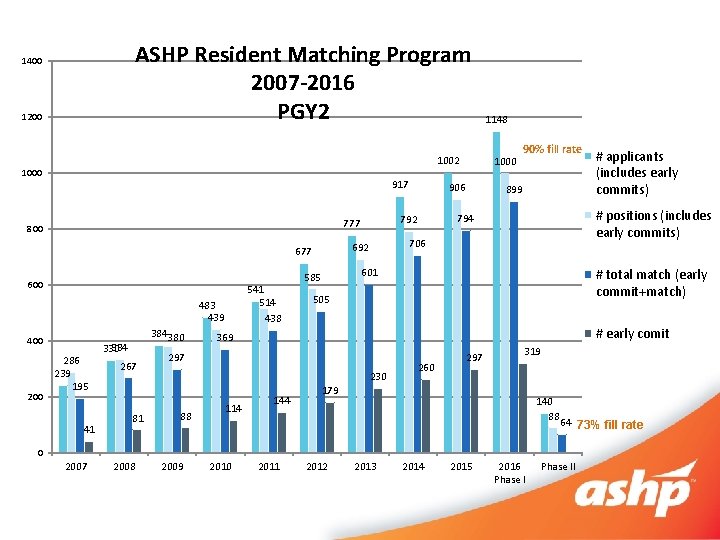
Applicants Participating and Positions Offered Increased in 2016 • PGY 1 – 7. 9% increase in positions offered – 11. 6% increase in applicants participating in Match • PGY 2* – 8. 9% increase in positions offered – 22. 7% increase in applicants participating in match * Includes early commitment process
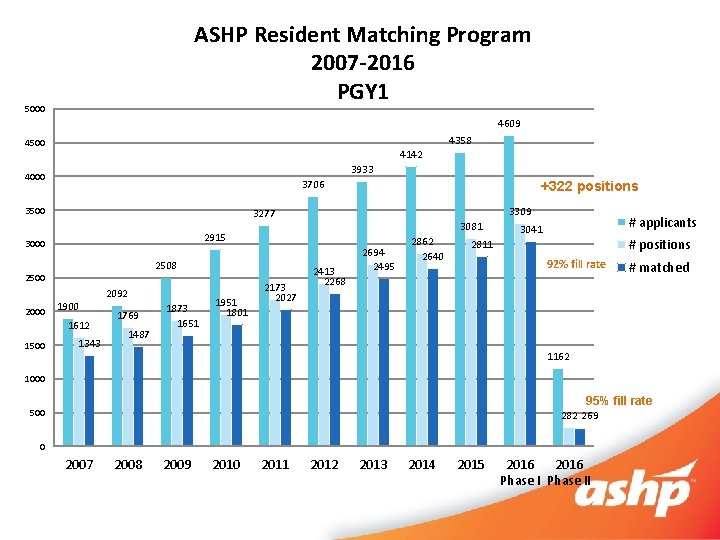
ASHP Resident Matching Program 2007 -2016 PGY 1 5000 4609 4358 4500 4142 3933 4000 3706 3500 3081 2915 2508 2500 1900 1612 1500 3309 3277 3000 2000 +322 positions 1343 2092 1769 1487 1873 1651 1951 1801 2173 2027 2413 2268 2694 2495 2862 2640 # applicants 3041 # positions 2811 92% fill rate # matched 1162 1000 95% fill rate 500 282 269 0 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 Phase II
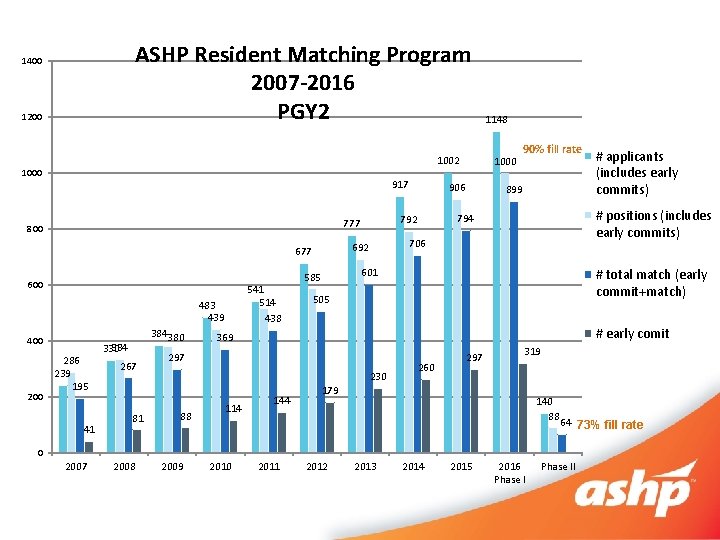
ASHP Resident Matching Program 2007 -2016 PGY 2 1400 1200 1002 1000 917 800 600 541 514 438 483 439 400 286 239 195 41 384380 334 330 267 81 899 # total match (early commit+match) 505 # early comit 369 230 114 144 260 297 319 179 140 88 64 73% fill rate 0 2007 2008 2009 2010 # applicants (includes early commits) # positions (includes early commits) 794 601 585 297 88 90% fill rate 706 692 677 1000 906 792 777 1148 2011 2012 2013 2014 2015 2016 Phase II
What percent of PGY 1 applicants DID NOT match with a program by the end of Phase II? A. B. C. D. 8% 19% 33% 50%
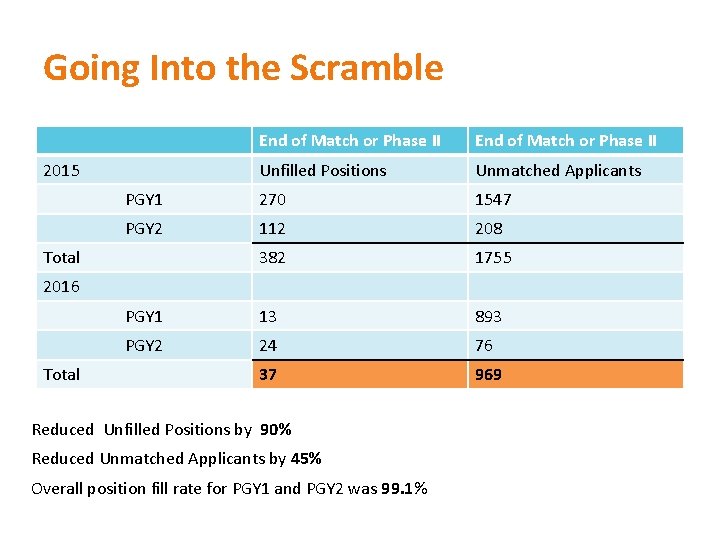
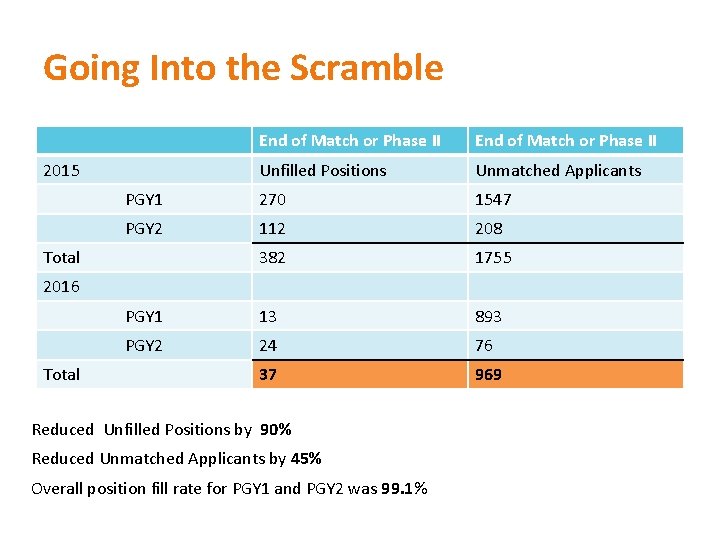
Going Into the Scramble End of Match or Phase II Unfilled Positions Unmatched Applicants PGY 1 270 1547 PGY 2 112 208 382 1755 PGY 1 13 893 PGY 2 24 76 37 969 2015 Total 2016 Total Reduced Unfilled Positions by 90% Reduced Unmatched Applicants by 45% Overall position fill rate for PGY 1 and PGY 2 was 99. 1%
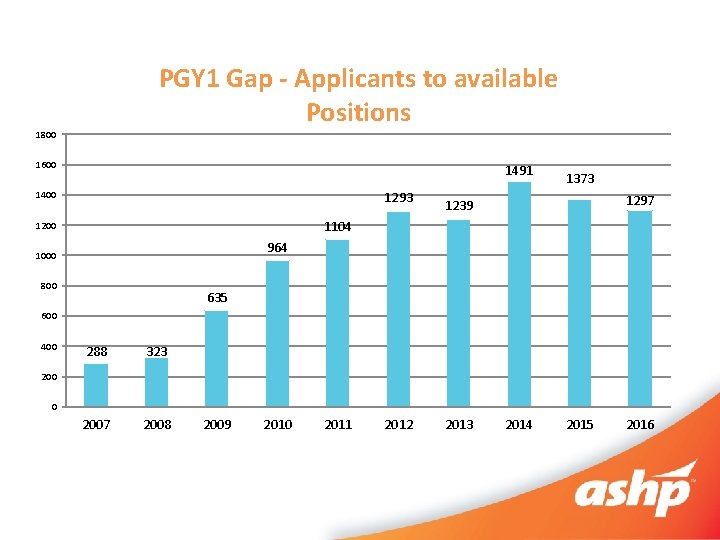
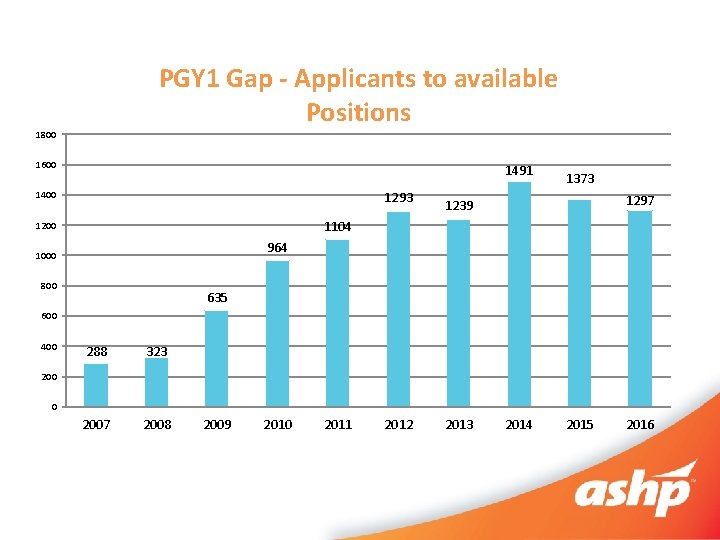
PGY 1 Gap - Applicants to available Positions 1800 1600 1491 1293 1400 1373 1297 1239 1104 1200 964 1000 800 635 600 400 288 323 2007 2008 200 0 2009 2010 2011 2012 2013 2014 2015 2016
Two Phase Match Summary • Match results reflect significant growth in residency programs and additional residency positions in past 3 years • Still significantly more applicants than positions • Two phase match process was successful in filling majority of residency positions in an orderly fashion
News from the Commission on Credentialing
Changes to Standards and Competency Areas for PGY 2 Programs • New PGY 2 standard approved – August 2015 – Optional implementation – July 2016 – Required implementation – July 2017 • New PGY 2 guidance document approved – March 2016 • Pharm. Academic will default to 2015 PGY 2 standard for 2016 residency unless program emails them • Current outcomes, goals, and objectives can be utilized with new standard • Competency areas, goals, and objectives currently under development – Order of development based primarily on number of PGY 2 programs – First sets of revised goals and objectives expected to be approved at August 2016 COC meeting and ready for implementation in Pharm. Academic for 2017 -2018 residency year
PGY 2 Goals and Objectives in Process • • • Critical Care Ambulatory Care Oncology Infectious Diseases Psychiatry Pediatrics Solid Organ Transplant Cardiology Internal Medicine Pharmacotherapy
New Changes to the Guidance Document for the 2014 Standard (April 2016) • Standard 1. 5: Consequences of residents’ failure to obtain appropriate licensure either prior to or within 90 days of the start date of the residency must be addressed in written policy of the residency program – Added as a critical factor – Guidance added: Programs ensure a minimum of 2/3 of residency is completed as a pharmacist licensed to practice in the program’s jurisdiction. • Standard 3. 1: Purpose statement (see standard for required purpose statement) – Guidance changed to: The program documents the required purpose statement in program materials. (changes in red)
New Changes to the Guidance Document for the 2014 Standard-April 2016 (continued) • Standard 6. 3: The pharmacist executive must provide effective leadership and management for the achievement of short- and long-term goals of the pharmacy and the organization for medication-use and medication-use policies. – Removed definitions of short-term goals as one year and long-term goals as greater than 2 years – Changed how it will be surveyed to: • Review of department of pharmacy strategic plan and specific departmental goals and initiatives • Discussion with organization and pharmacy leaders, physicians, nurses and pharmacy staff about the role of pharmacy in strategic planning for the organization and medication-use process
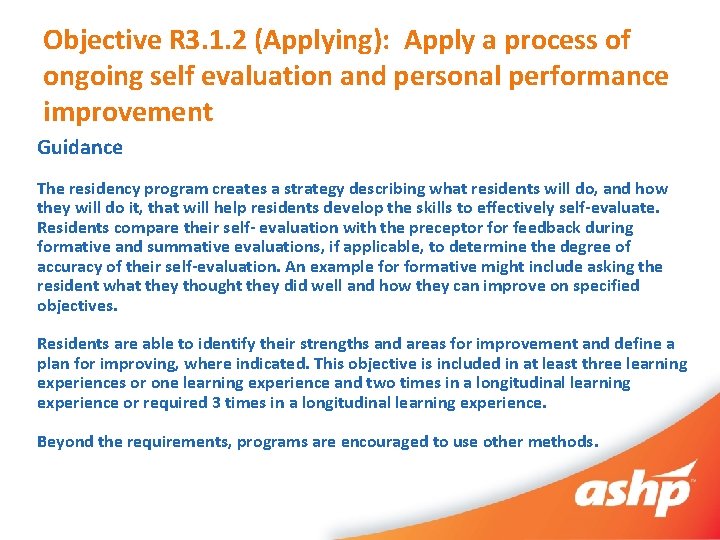
New Changes to the Guidance Documents for the 2014 Competency Areas, Goals, and Objectives (April 2016) • Objective R 3. 1. 2 (Applying): Apply a process of ongoing self evaluation and personal performance improvement – Added guidance on minimum number of times objective must be assigned to be taught and evaluated. • Objective must be taught and formally evaluated at least 3 times – Assigned to 3 different learning experiences – Assigned to be evaluated in 1 learning experience and twice in a longitudinal learning experience – Assigned to be evaluated 3 times in a longitudinal learning experience • How it will be surveyed section also changed to reflect new guidance. Exact wording in next slide
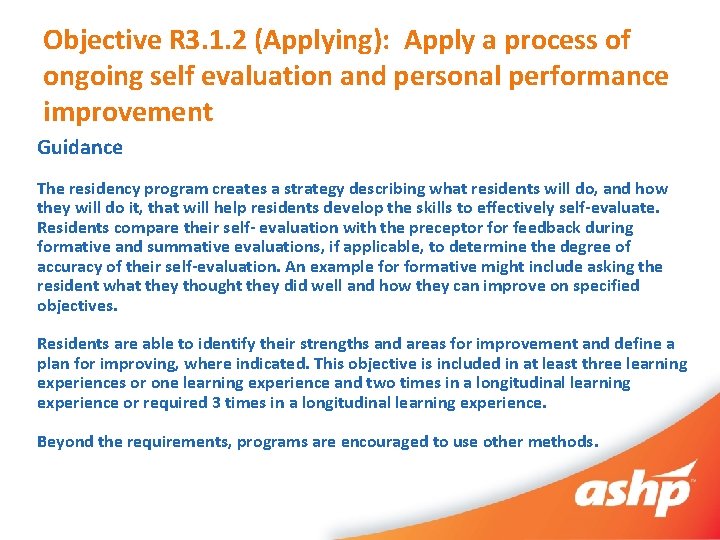
Objective R 3. 1. 2 (Applying): Apply a process of ongoing self evaluation and personal performance improvement Guidance The residency program creates a strategy describing what residents will do, and how they will do it, that will help residents develop the skills to effectively self-evaluate. Residents compare their self- evaluation with the preceptor feedback during formative and summative evaluations, if applicable, to determine the degree of accuracy of their self-evaluation. An example formative might include asking the resident what they thought they did well and how they can improve on specified objectives. Residents are able to identify their strengths and areas for improvement and define a plan for improving, where indicated. This objective is included in at least three learning experiences or one learning experience and two times in a longitudinal learning experience or required 3 times in a longitudinal learning experience. Beyond the requirements, programs are encouraged to use other methods.
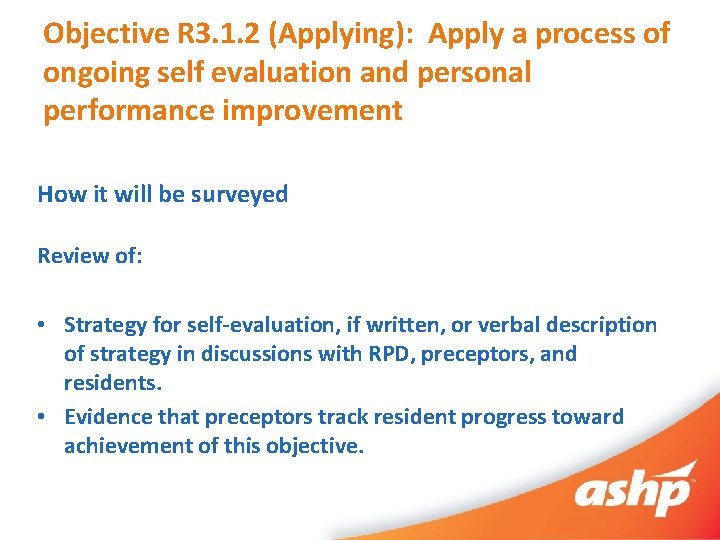
Objective R 3. 1. 2 (Applying): Apply a process of ongoing self evaluation and personal performance improvement How it will be surveyed Review of: • Strategy for self-evaluation, if written, or verbal description of strategy in discussions with RPD, preceptors, and residents. • Evidence that preceptors track resident progress toward achievement of this objective.
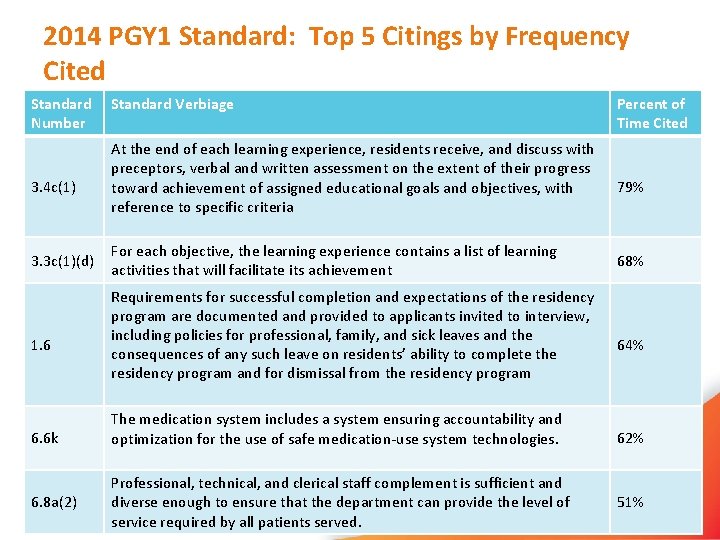
Top Citings: 2014 PGY 1 Standard • 47 programs surveyed on new standard as of March 2016. • On average, surveyors cited 21 elements per survey. The range was 7 -40 elements cited.
Audience Participation Question: The most frequently cited element of the current standard is: A. B. C. D. 4. 8 c – related to preceptor qualifications 1. 5 – related to licensure requirements 3. 3 c(1)(d) – related to learning experience descriptions 3. 4 c(1) – related to preceptor evaluation of residents
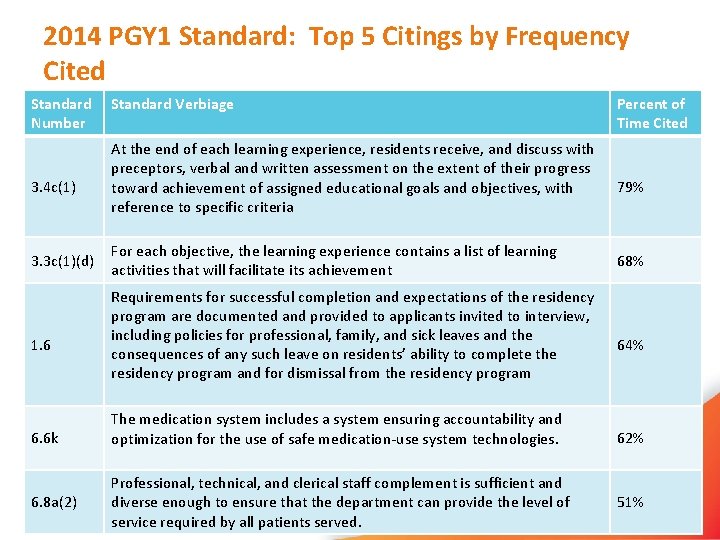
2014 PGY 1 Standard: Top 5 Citings by Frequency Cited Standard Number 3. 4 c(1) 3. 3 c(1)(d) 1. 6 6. 6 k 6. 8 a(2) Standard Verbiage At the end of each learning experience, residents receive, and discuss with preceptors, verbal and written assessment on the extent of their progress toward achievement of assigned educational goals and objectives, with reference to specific criteria For each objective, the learning experience contains a list of learning activities that will facilitate its achievement Requirements for successful completion and expectations of the residency program are documented and provided to applicants invited to interview, including policies for professional, family, and sick leaves and the consequences of any such leave on residents’ ability to complete the residency program and for dismissal from the residency program The medication system includes a system ensuring accountability and optimization for the use of safe medication-use system technologies. Professional, technical, and clerical staff complement is sufficient and diverse enough to ensure that the department can provide the level of service required by all patients served. Percent of Time Cited 79% 68% 64% 62% 51%
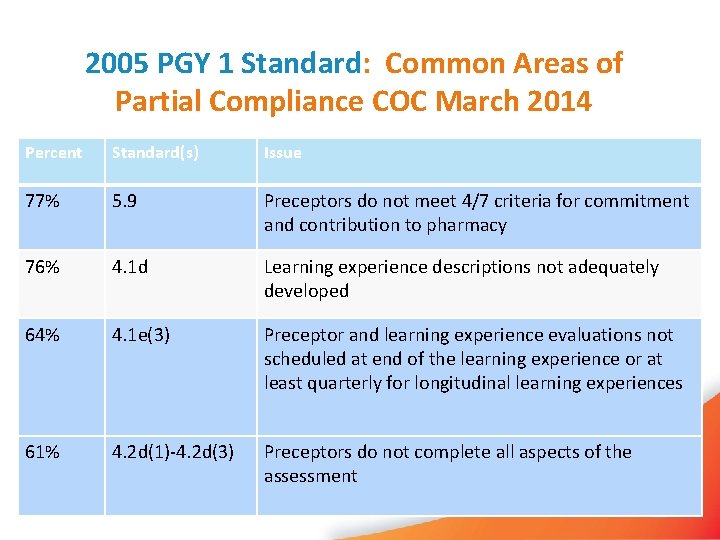
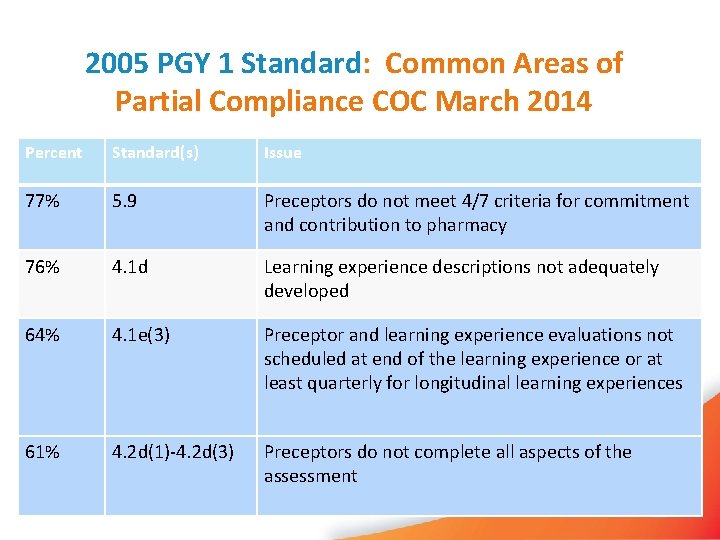
2005 PGY 1 Standard: Common Areas of Partial Compliance COC March 2014 Percent Standard(s) Issue 77% 5. 9 Preceptors do not meet 4/7 criteria for commitment and contribution to pharmacy 76% 4. 1 d Learning experience descriptions not adequately developed 64% 4. 1 e(3) Preceptor and learning experience evaluations not scheduled at end of the learning experience or at least quarterly for longitudinal learning experiences 61% 4. 2 d(1)-4. 2 d(3) Preceptors do not complete all aspects of the assessment
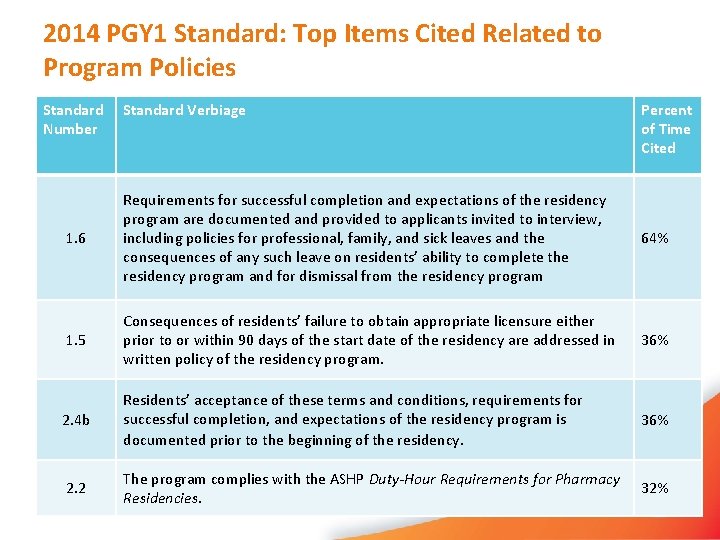
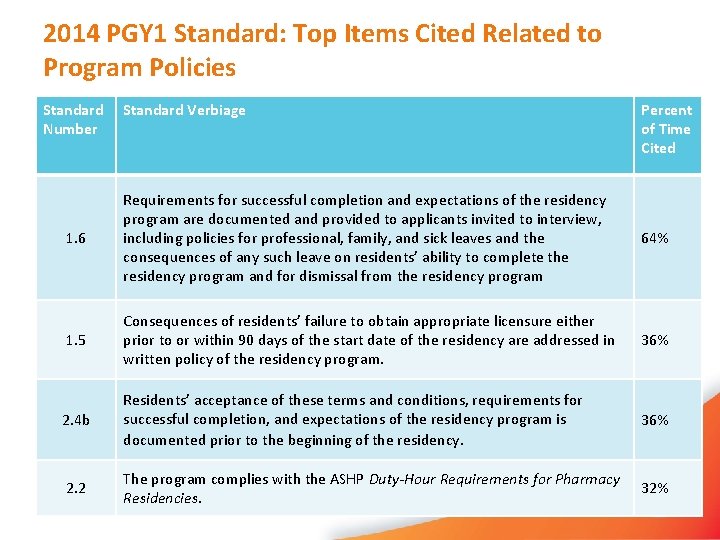
2014 PGY 1 Standard: Top Items Cited Related to Program Policies Standard Number Standard Verbiage Percent of Time Cited 1. 6 Requirements for successful completion and expectations of the residency program are documented and provided to applicants invited to interview, including policies for professional, family, and sick leaves and the consequences of any such leave on residents’ ability to complete the residency program and for dismissal from the residency program 64% 1. 5 Consequences of residents’ failure to obtain appropriate licensure either prior to or within 90 days of the start date of the residency are addressed in written policy of the residency program. 36% 2. 4 b Residents’ acceptance of these terms and conditions, requirements for successful completion, and expectations of the residency program is documented prior to the beginning of the residency. 36% 2. 2 The program complies with the ASHP Duty-Hour Requirements for Pharmacy Residencies. 32%
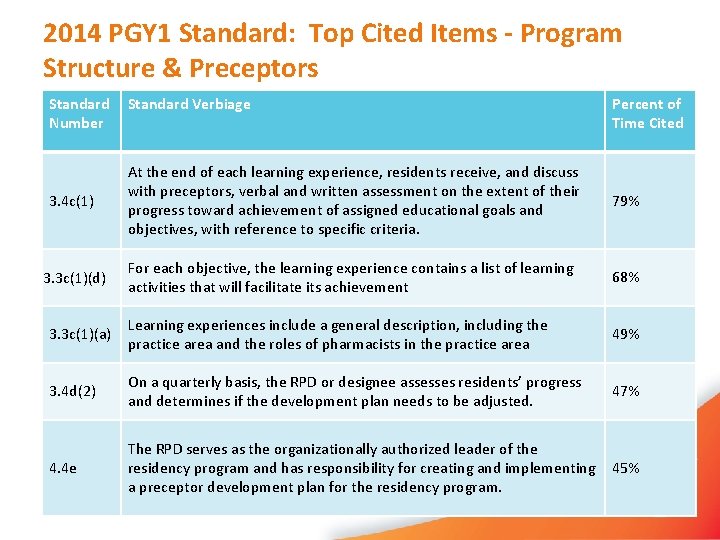
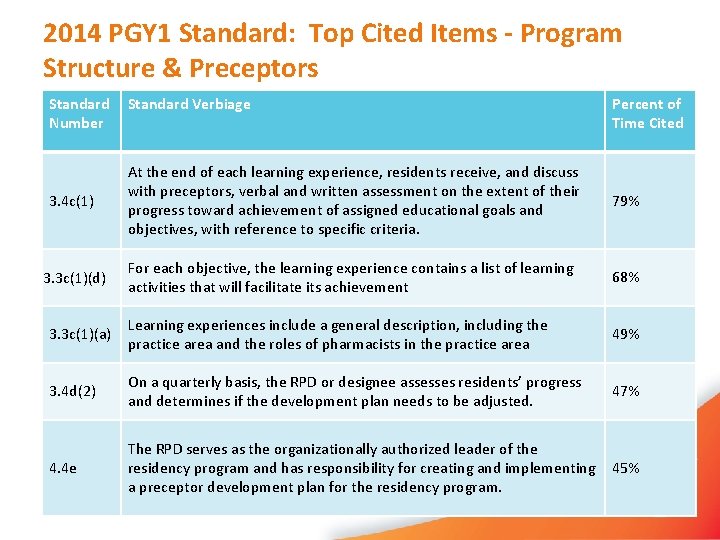
2014 PGY 1 Standard: Top Cited Items - Program Structure & Preceptors Standard Number Standard Verbiage Percent of Time Cited 3. 4 c(1) At the end of each learning experience, residents receive, and discuss with preceptors, verbal and written assessment on the extent of their progress toward achievement of assigned educational goals and objectives, with reference to specific criteria. 79% 3. 3 c(1)(d) For each objective, the learning experience contains a list of learning activities that will facilitate its achievement 68% 3. 3 c(1)(a) Learning experiences include a general description, including the practice area and the roles of pharmacists in the practice area 49% 3. 4 d(2) On a quarterly basis, the RPD or designee assesses residents’ progress and determines if the development plan needs to be adjusted. 47% 4. 4 e The RPD serves as the organizationally authorized leader of the residency program and has responsibility for creating and implementing a preceptor development plan for the residency program. 45%
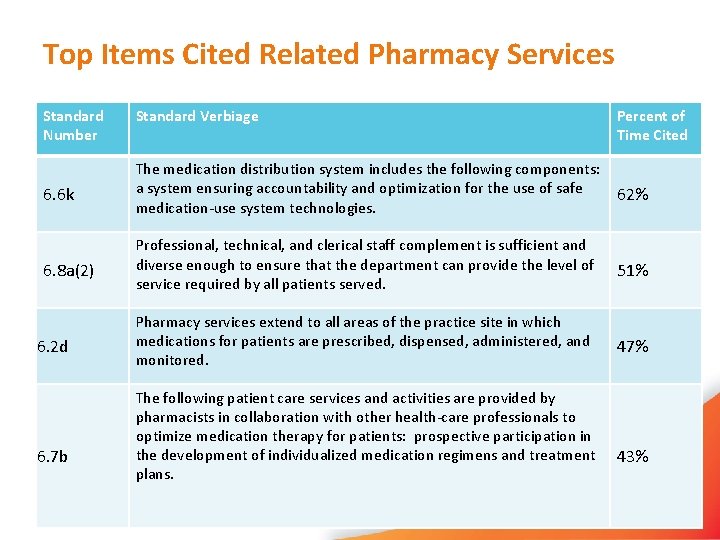
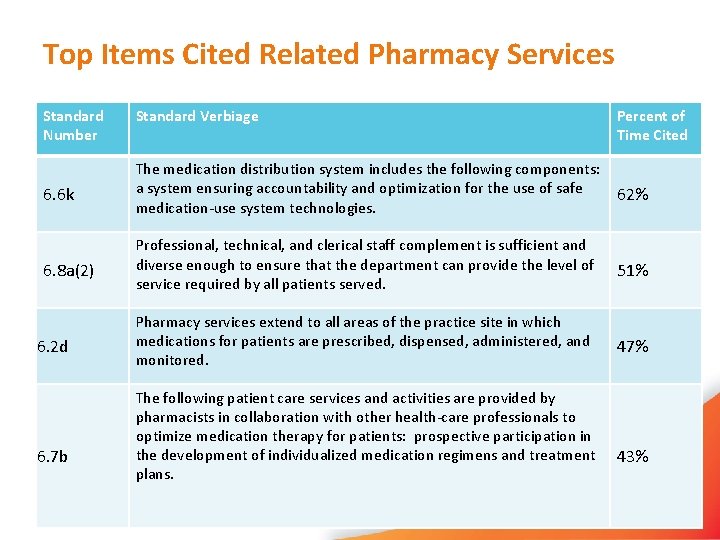
Top Items Cited Related Pharmacy Services Standard Number Standard Verbiage Percent of Time Cited 6. 6 k The medication distribution system includes the following components: a system ensuring accountability and optimization for the use of safe medication-use system technologies. 62% 6. 8 a(2) Professional, technical, and clerical staff complement is sufficient and diverse enough to ensure that the department can provide the level of service required by all patients served. 51% Pharmacy services extend to all areas of the practice site in which medications for patients are prescribed, dispensed, administered, and monitored. 47% 6. 2 d 6. 7 b The following patient care services and activities are provided by pharmacists in collaboration with other health-care professionals to optimize medication therapy for patients: prospective participation in the development of individualized medication regimens and treatment plans. 43%
COC News Summary • Remember programs have the option to use the PGY 2 standard, starting July 2016, but can remain on the old standard until July 2017. • Notify Pharm. Academic if not converting in July, 2016. • Guidance for both standards expected to be updated twice a year. Remember to check for updates in late April and September.
Implementing the New Standards and Getting Ready for a Survey
Implementing the New Standards Have you done any, some, or all of the following? • • • Adopted the new required purpose statements? Updated and documented your program requirements? Re-designed your program using the new C/G/O? Used policies, procedures and program requirements during the candidate selection process? Named a coordinator(s)? Developed and implemented a RAC? Developed a preceptor appointment and re-appointment process? Started/continued with a preceptor development program? Changed to the new Development Plan?
Implementing the New Standards Have you done any, some, or all of the following? • Changed your resident self-evaluation process? • Changed your evaluation requirements for your preceptors and learning experiences? • Developed a plan for continuous quality improvement?
Getting Ready for a Survey Use the new Guidance Documents to assist you in your preparation activities. They may be updated in April and September following the Commission on Credentialing meetings. Keep an eye on the ASHP website! Two important sections of the Guidance Documents: • Interpretation • How it will be Surveyed
Getting Ready for a Survey • Surveyors will have access to Pharm. Academic • Use Pharm. Academic to upload supporting documents • Pre-survey material attachments and on-site exhibits have changed – review and assemble the needed documents • The preceptor Academic and Performance record has changed. Have preceptors use the new form! • Be ready to describe the roles of coordinator(s) and the preceptor appointment and reappointment processes • Attend forums at the NPPC and MCM to learn from the experiences of others and from ASHP lead surveyors and members of the Commission on Credentialing

QUESTIONS?
Implementing the New Residency Accreditation Standards and Getting Ready for a Survey David J. Warner, Pharm. D. Director, Center on Practice Development Practice Advancement Office Lead Consultant, ASHP Consulting