Implementing Primary Care Networks in West Essex Peter


- Slides: 55
Implementing Primary Care Networks in West Essex Peter Wightman 2 April 2019 GP Shutdown 1
Wider NHS landscape and primary care networks National picture 2
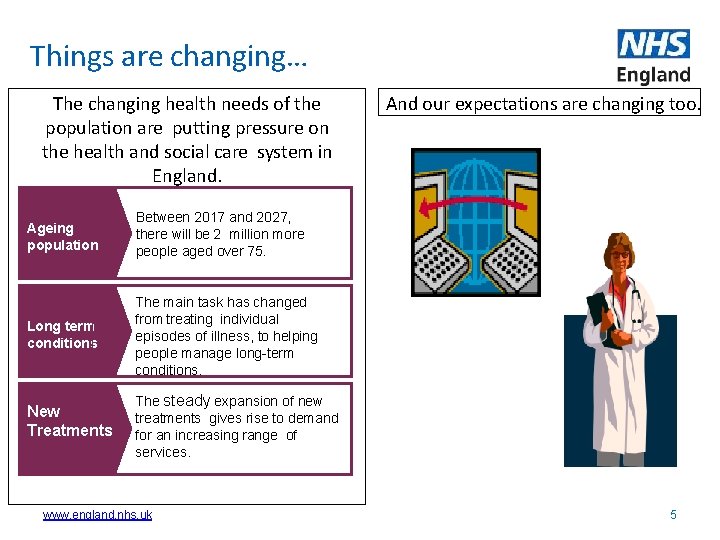
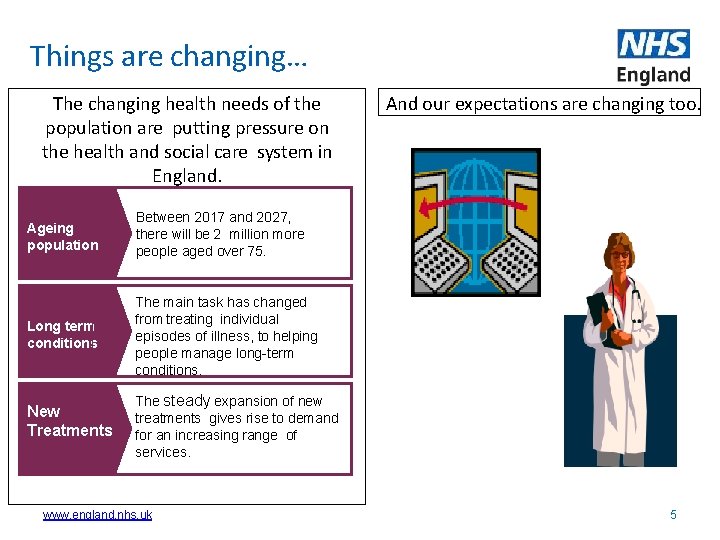
Things are changing… The changing health needs of the population are putting pressure on the health and social care system in England. Ageing population Between 2017 and 2027, there will be 2 million more people aged over 75. Long term conditions The main task has changed from treating individual episodes of illness, to helping people manage long-term conditions. New Treatments The steady expansion of new treatments gives rise to demand for an increasing range of services. www. england. nhs. uk And our expectations are changing too. 5
Current systems need to adapt: • Workforce shortages in traditional roles • Little historical investment in primary and community care • Multiple organisations and IT = provision is fragmented • This is getting in the way of providing person centred holistic patient care 6
The NHS Long Term Plan responds to this, and places Primary Care at the centre … Aims: • Everyone gets the best start in life • World class care for major health problems • Supporting people to age well => Primary care networks as the foundation for Integrated Care Systems www. england. nhs. uk • Preventing ill health and tackling health inequalities • Supporting the workforce • Maximising opportunities presented by data and technology 7 • Continued focus on efficiency
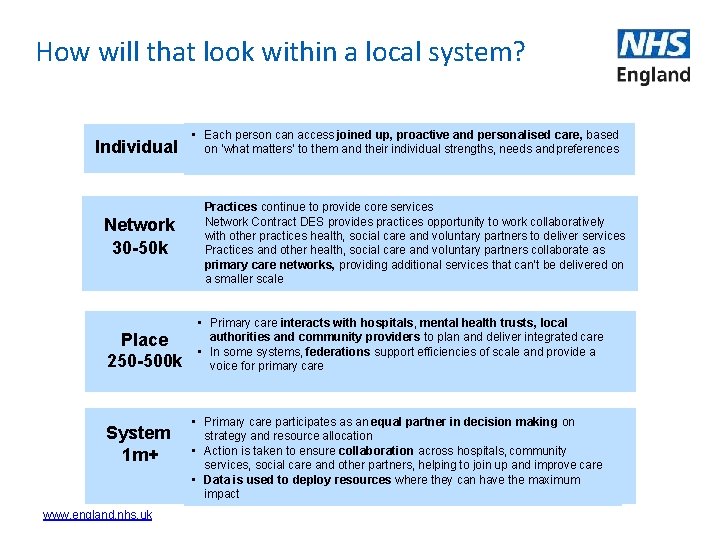
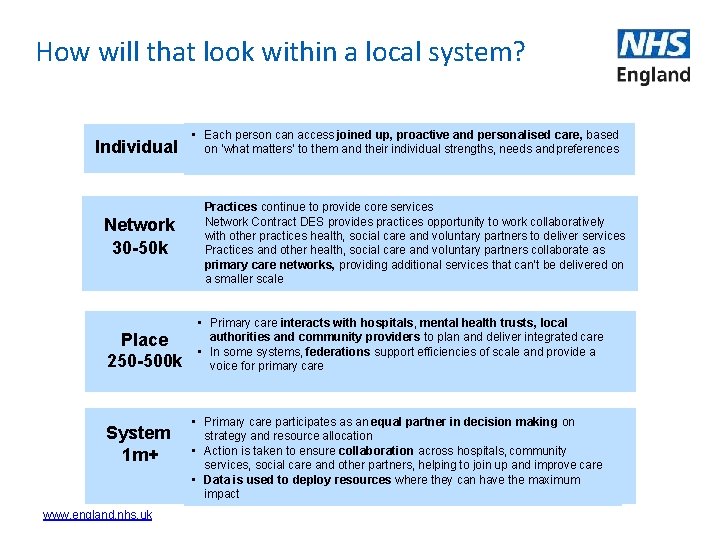
How will that look within a local system? Individual Network 30 -50 k Place 250 -500 k System 1 m+ www. england. nhs. uk • Each person can access joined up, proactive and personalised care, based on ‘what matters’ to them and their individual strengths, needs and preferences • Practices continue to provide core services • Network Contract DES provides practices opportunity to work collaboratively with other practices health, social care and voluntary partners to deliver services • Practices and other health, social care and voluntary partners collaborate as primary care networks, providing additional services that can’t be delivered on a smaller scale • Primary care interacts with hospitals, mental health trusts, local authorities and community providers to plan and deliver integrated care • In some systems, federations support efficiencies of scale and provide a voice for primary care • Primary care participates as an equal partner in decision making on strategy and resource allocation • Action is taken to ensure collaboration across hospitals, community services, social care and other partners, helping to join up and improve care • Data is used to deploy resources where they can have the maximum impact
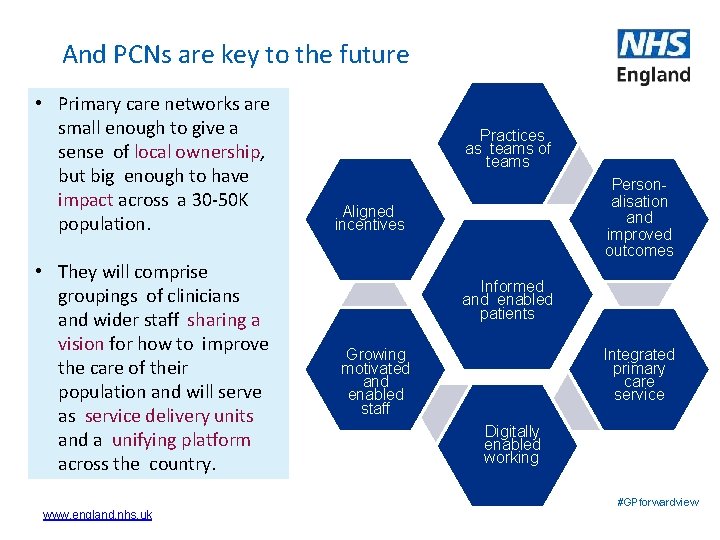
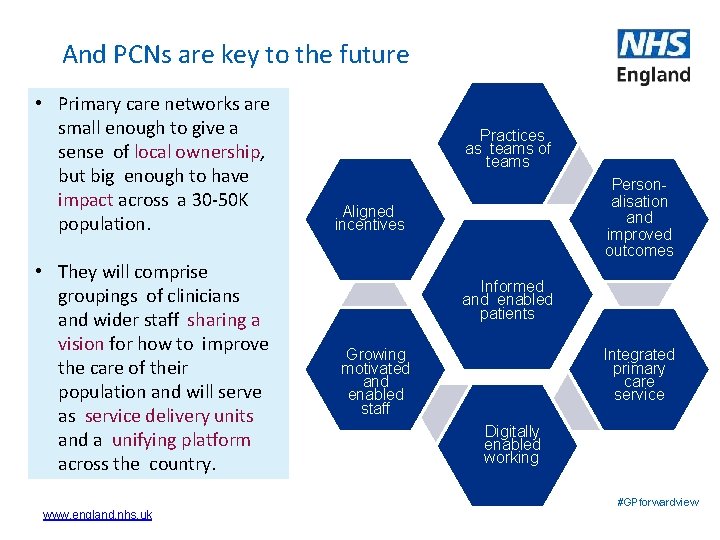
And PCNs are key to the future • Primary care networks are small enough to give a sense of local ownership, but big enough to have impact across a 30 -50 K population. • They will comprise groupings of clinicians and wider staff sharing a vision for how to improve the care of their population and will serve as service delivery units and a unifying platform across the country. www. england. nhs. uk Practices as teams of teams Personalisation and improved outcomes Aligned incentives Informed and enabled patients Integrated primary care service Growing motivated and enabled staff Digitally enabled working #GPforwardview
Wider NHS landscape and primary care networks West Essex picture 8
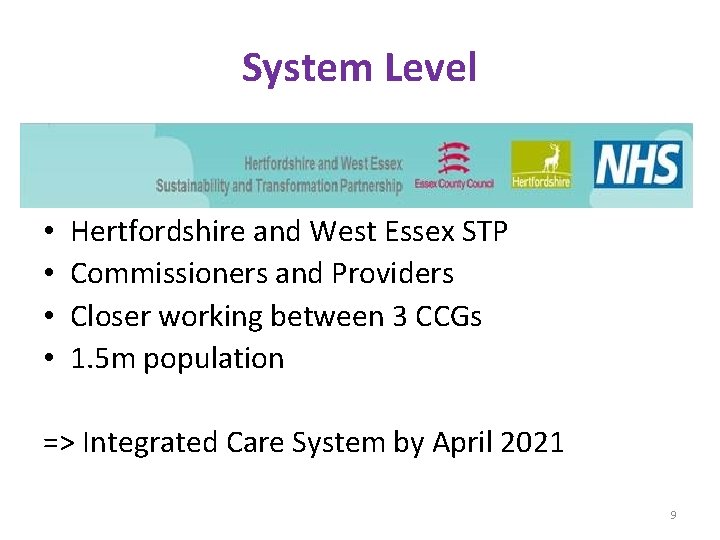
System Level • • Hertfordshire and West Essex STP Commissioners and Providers Closer working between 3 CCGs 1. 5 m population => Integrated Care System by April 2021 9
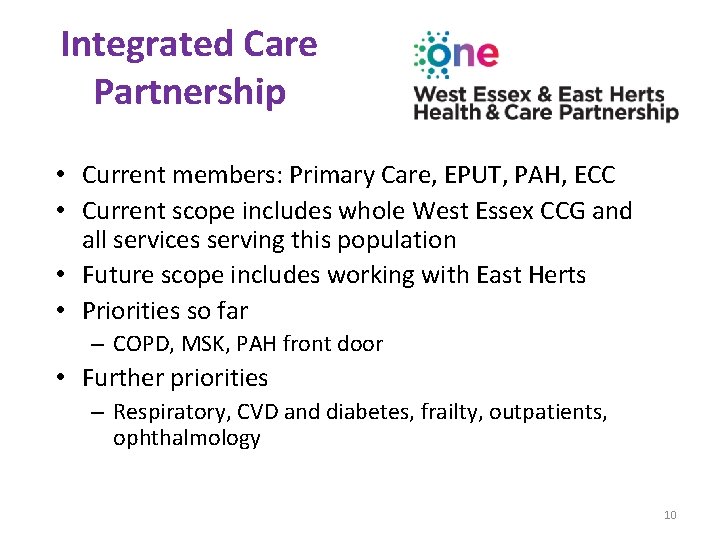
Integrated Care Partnership • Current members: Primary Care, EPUT, PAH, ECC • Current scope includes whole West Essex CCG and all services serving this population • Future scope includes working with East Herts • Priorities so far – COPD, MSK, PAH front door • Further priorities – Respiratory, CVD and diabetes, frailty, outpatients, ophthalmology 10
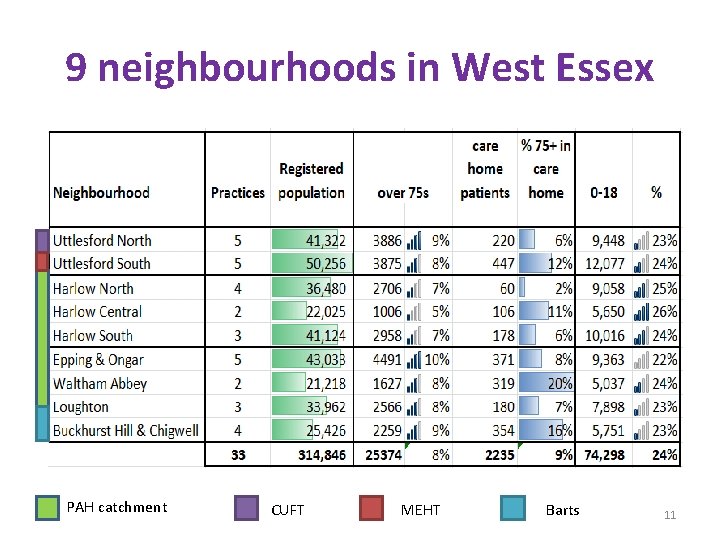
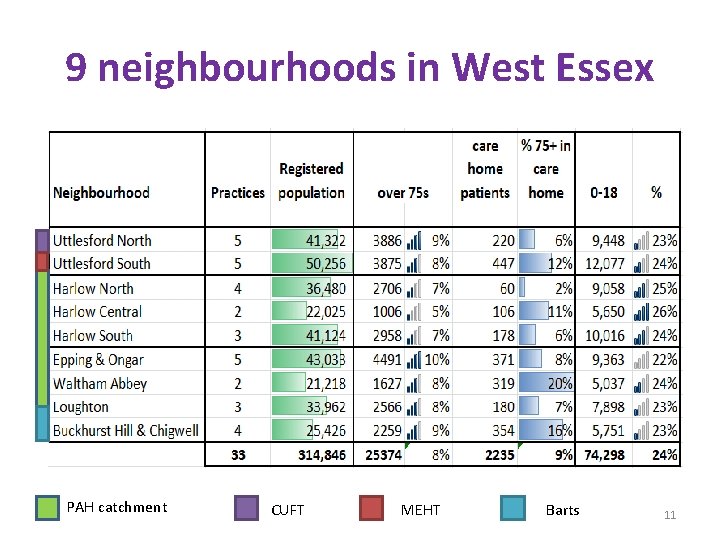
9 neighbourhoods in West Essex PAH catchment CUFT MEHT Barts 11

Lot of progress with neighbourhoods in W Essex • Practices working together • Extended access hubs • Primary care transformation projects • Assigned EPUT and Social care staff • Close work with districts and voluntary sector – care navigators 12
Overview of Primary Care Networks guidance and DES 13
Investment and evolution: A five year framework for GP contract reform to implement The NHS Long Term Plan 31 January 2019
Further guidance published 31 March 2019* Network Contract Directed Enhanced Service • Guidance • Contract specification • Mandatory Network Agreement 15
Purpose of 5 year framework for GP contract reform • Secure and guarantee extra investment for primary care; • Practical changes to help workforce and workload problems in general practice; • Deliver quality and improvement goals of The NHS Long Term Plan; • Show value for money for taxpayers and rest of the NHS; • Get better at local testing before national roll out. 16
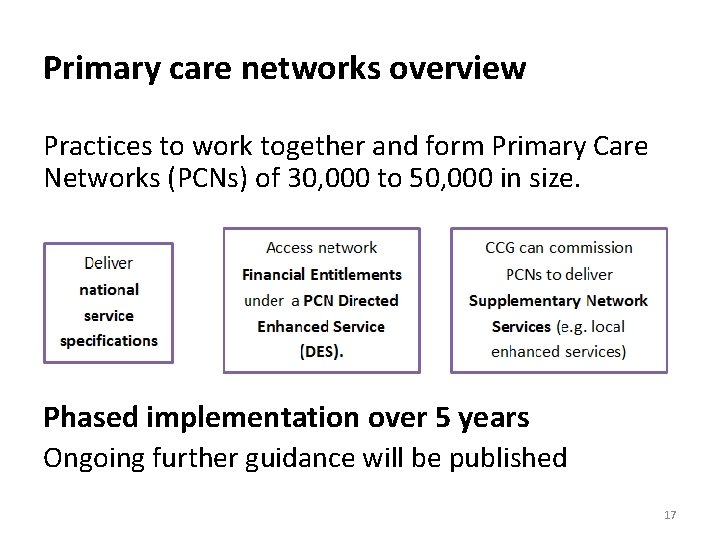
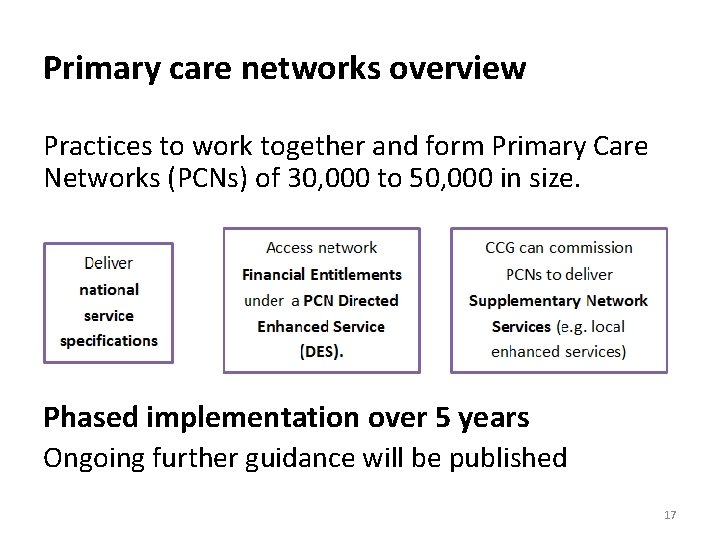
Primary care networks overview Practices to work together and form Primary Care Networks (PCNs) of 30, 000 to 50, 000 in size. Phased implementation over 5 years Ongoing further guidance will be published 17
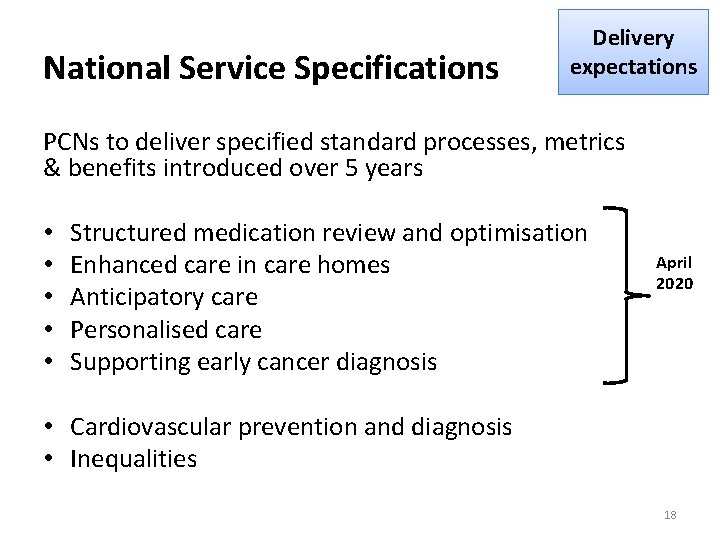
National Service Specifications Delivery expectations PCNs to deliver specified standard processes, metrics & benefits introduced over 5 years • • • Structured medication review and optimisation Enhanced care in care homes Anticipatory care Personalised care Supporting early cancer diagnosis April 2020 • Cardiovascular prevention and diagnosis • Inequalities 18
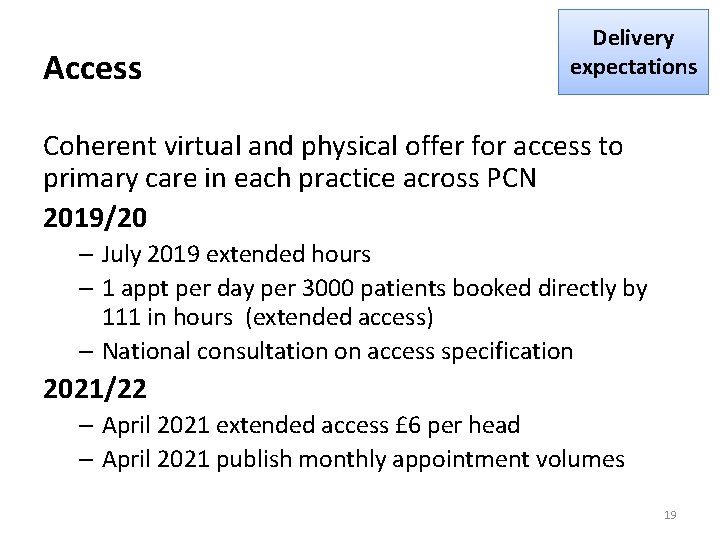
Access Delivery expectations Coherent virtual and physical offer for access to primary care in each practice across PCN 2019/20 – July 2019 extended hours – 1 appt per day per 3000 patients booked directly by 111 in hours (extended access) – National consultation on access specification 2021/22 – April 2021 extended access £ 6 per head – April 2021 publish monthly appointment volumes 19
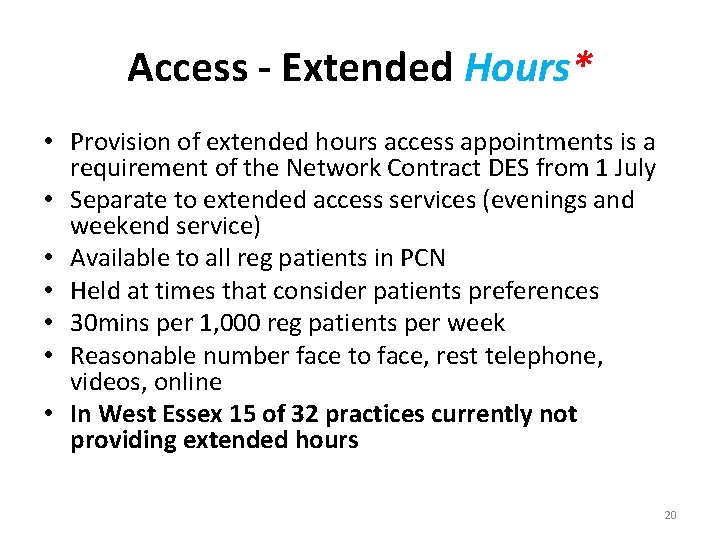
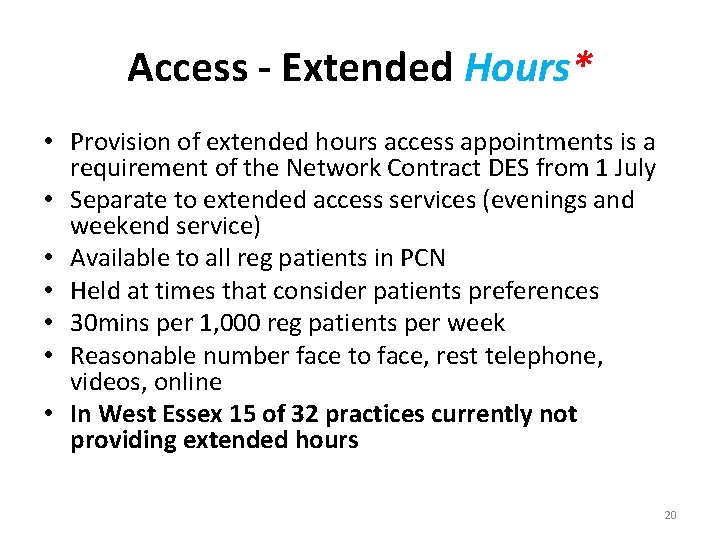
Access - Extended Hours* • Provision of extended hours access appointments is a requirement of the Network Contract DES from 1 July • Separate to extended access services (evenings and weekend service) • Available to all reg patients in PCN • Held at times that consider patients preferences • 30 mins per 1, 000 reg patients per week • Reasonable number face to face, rest telephone, videos, online • In West Essex 15 of 32 practices currently not providing extended hours 20
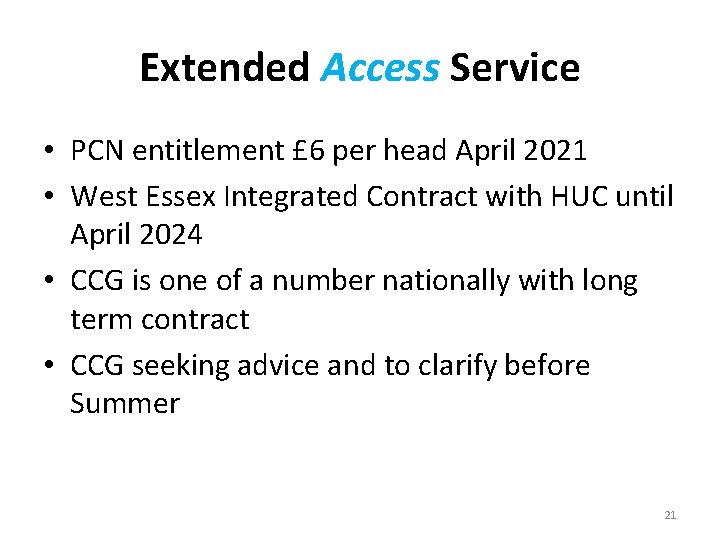
Extended Access Service • PCN entitlement £ 6 per head April 2021 • West Essex Integrated Contract with HUC until April 2024 • CCG is one of a number nationally with long term contract • CCG seeking advice and to clarify before Summer 21
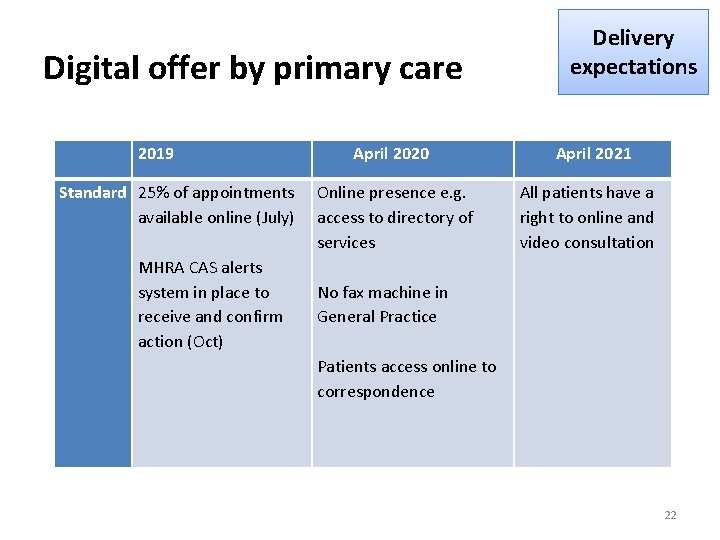
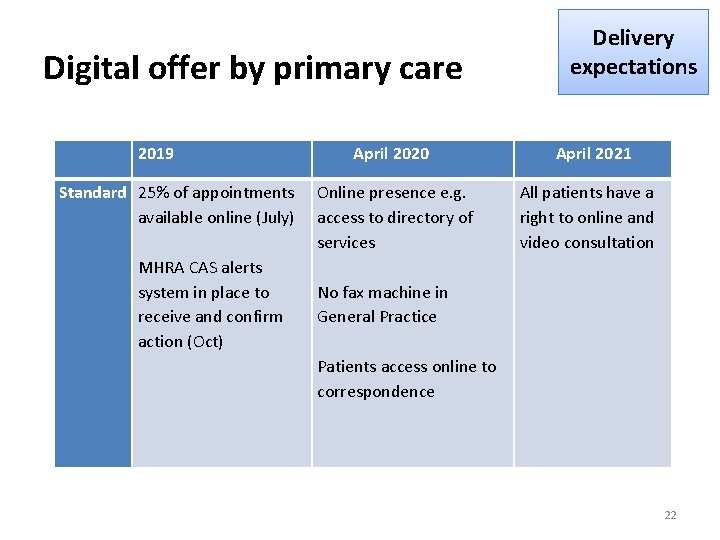
Digital offer by primary care 2019 Standard 25% of appointments available online (July) MHRA CAS alerts system in place to receive and confirm action (Oct) April 2020 Online presence e. g. access to directory of services Delivery expectations April 2021 All patients have a right to online and video consultation No fax machine in General Practice Patients access online to correspondence 22
Key Questions: Geography? 23
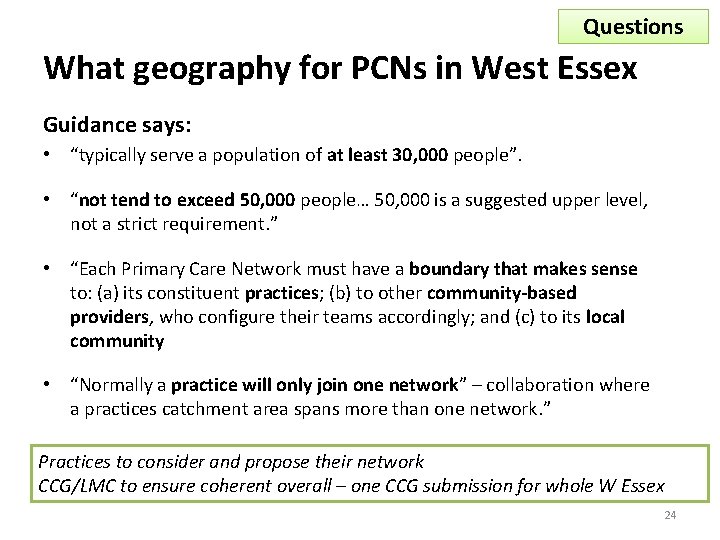
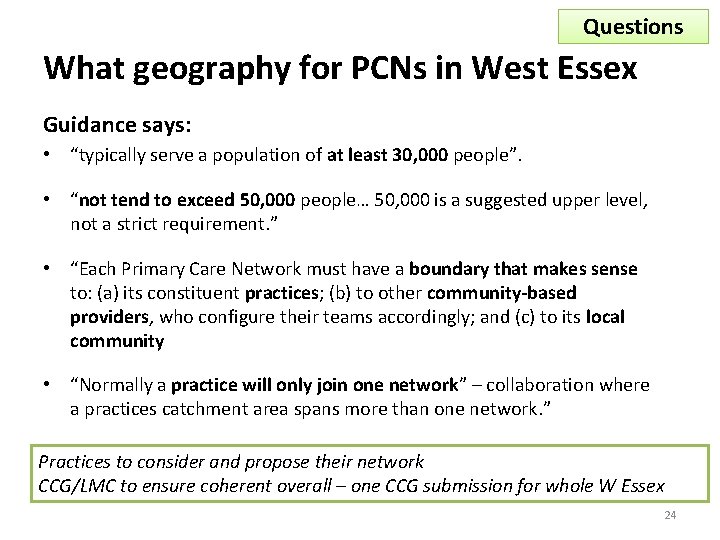
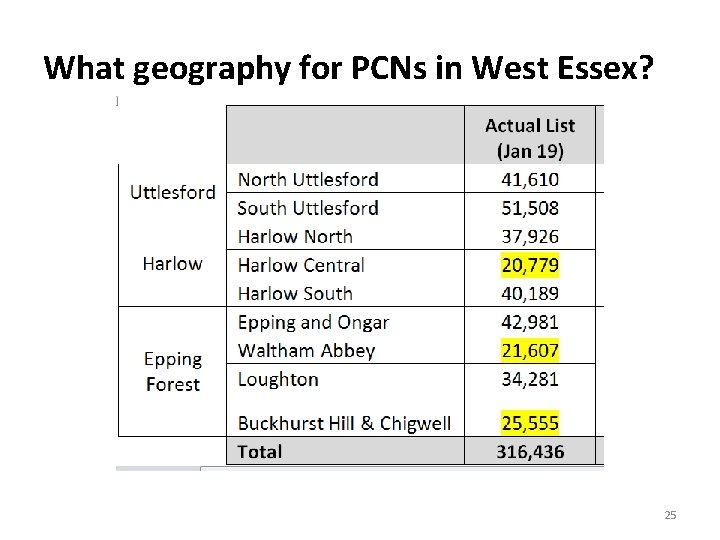
Questions What geography for PCNs in West Essex Guidance says: • “typically serve a population of at least 30, 000 people”. • “not tend to exceed 50, 000 people… 50, 000 is a suggested upper level, not a strict requirement. ” • “Each Primary Care Network must have a boundary that makes sense to: (a) its constituent practices; (b) to other community-based providers, who configure their teams accordingly; and (c) to its local community • “Normally a practice will only join one network” – collaboration where a practices catchment area spans more than one network. ” Practices to consider and propose their network CCG/LMC to ensure coherent overall – one CCG submission for whole W Essex 24
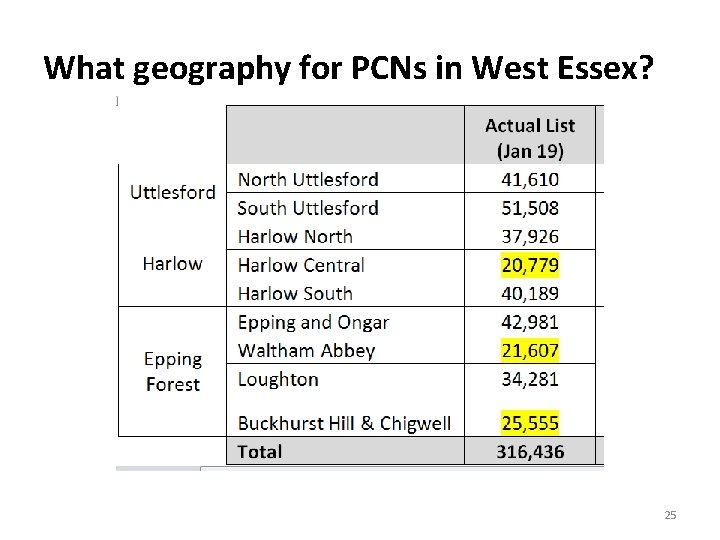
What geography for PCNs in West Essex? 25
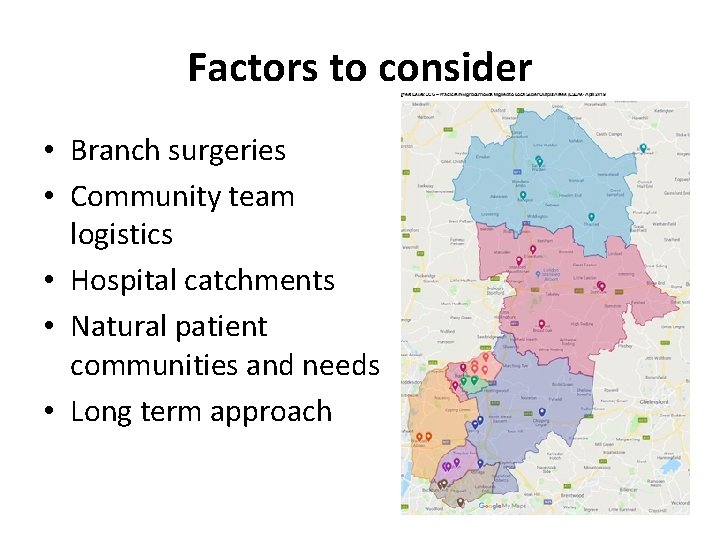
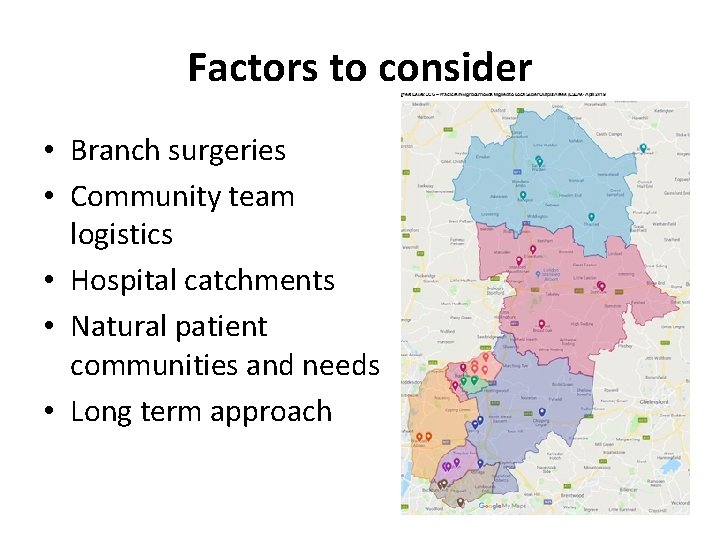
Factors to consider • Branch surgeries • Community team logistics • Hospital catchments • Natural patient communities and needs • Long term approach 26

Opportunities of Additional Roles 27
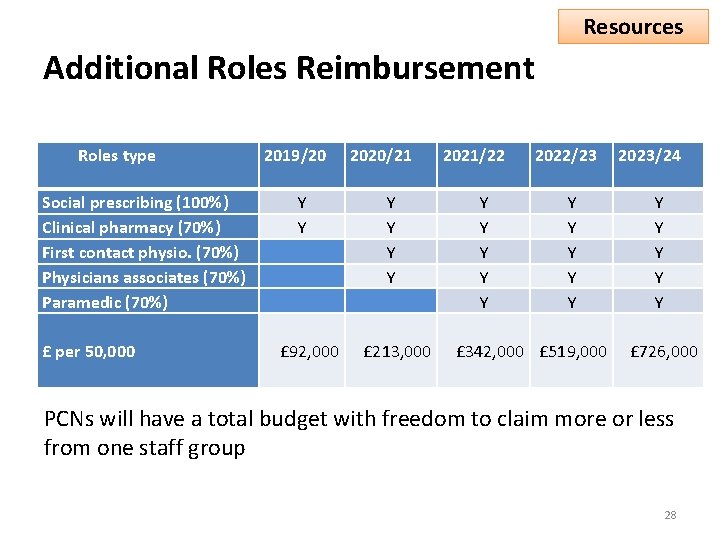
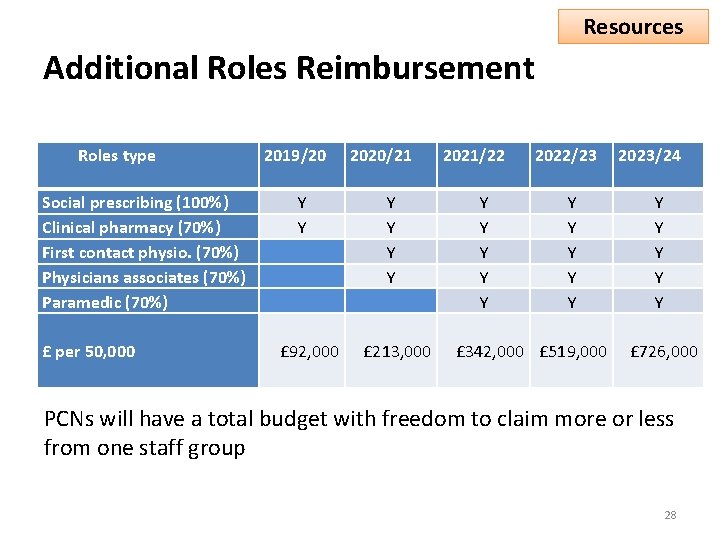
Resources Additional Roles Reimbursement Roles type Social prescribing (100%) Clinical pharmacy (70%) First contact physio. (70%) Physicians associates (70%) Paramedic (70%) £ per 50, 000 2019/20 Y Y £ 92, 000 2020/21 Y Y £ 213, 000 2021/22 Y Y Y 2022/23 Y Y Y £ 342, 000 £ 519, 000 2023/24 Y Y Y £ 726, 000 PCNs will have a total budget with freedom to claim more or less from one staff group 28
Additional Roles • Staff delivering additional network services can be employed by a member of the PCN, or another body (eg. GP federation, voluntary sector, Local Authority, NHS Trust) • PCN and it’s member practices are responsible for ensuring the services are delivered in line with DES 29
Workforce – Additionality* • Baseline - Commissioners and practices confirm staff employed across 5 roles as at 31 March 2019 • Workforce baseline to be agreed as part of PCN registration process • PCN reimbursement claims will be assessed against baseline • Intended to protect existing commissioner investment • Information submission requirement of DES • Exception to baseline - pharmacists employed via 2 national schemes prior to 31 March 19 30
Social Prescribing – Role Overview • Identifying unmet needs and providing support • Spending time getting to know patients and their carers: – Direct support - phone or home visits, – Open invitations to the surgery for a ‘catch up and cuppa’ – Referring patients to appropriate VCS – Build knowledge of local VCS groups / organisations – Attend practice MDTs – First contact for care homes e. g. prescription requests, visit requests and post-discharge coordination of services and medication.
Social Prescribing - Benefits To patients • additional, non-clinical support options via primary care • improved health and wellbeing • less socially isolated and more independent. To practices • Social prescribers can significantly reduce GP consultations (by as much as 28%) • One in five GPs regularly refer patients to social prescribing • Recognition that social support can be an alternative to medication • Simple referral processes To the wider NHS • positive impact on GP consultation rates, A&E attendances, hospital stays, medication use and social care
West Essex - Care Navigation Partnership • GP level service (Smartlife) established as a pilot in 6 practices in 2014, rolled out to all practices in 2015. • Partnership established in 2017 to maximise the service offer by including community agents and Provide Lifestyle Service. • Single service offer for all patients requiring access to non-medical needs. • Home visits undertaken where required.
Options for PCNs to develop link workers • Expansion of Care Navigation Partnership model • Different employer but integrated working with existing service, options might be: – – Employed by practice Employed by voluntary sector organisation Employed by provider organisation other Further conversations can follow based on individual PCN preferences – CCG are happy to support these conversations.
How can Clinical Pharmacists help? • Workload, Safety, Patient Experience • Takes time to implement in partnership E. g. • Polypharmacy reviews • Answering medicine queries • Medicines reconciliation • Supporting achievement of the prescribing safety specifications such as safe anticoagulation prescribing 35
Clinical Pharmacists* • Minimum employment 0. 5 WTE (to allow for training requirements and working across practices in a PCN) • Enrolled in or qualified from Clinical Pharmacist training pathway • Part of a clinical network and supervised by senior clinical pharmacist and GP clinical supervisor • Clinical Pharmacists in General Practice Scheme ends April 19 – guidance specifies how in most cases these funded roles can transfer to PCNs and be claimed (p 12) 36
Medicines optimisation in Care Homes Scheme and PCNs* • The Medicines optimisation in Care Homes Scheme will end 31/3/20 • Staff employed and in post 31/3/19 will be included in baseline (exception to additionality) • PCNs may claim reimbursement for any staff that transfer during 19/20 (up to max) • Expectation that when national scheme ends, staff will be employed under terms of PCN DES to support delivery of national service specification • Further conversations can follow based on individual PCN preferences – CCG are happy to support these conversations. 37
Physiotherapy • West Essex CCG 100% funded service is being implemented by EPUT for all practices by October 2019. • This is integrated into the MSK pathway • There are guarantees for practices for service level • Services supplied after April 2019 are eligible for claim in 2020/21 • Further conversations can follow based on individual PCN preferences for the future of services. 38
ECPs • West Essex CCG 100% funded service continues and is being implemented in remaining areas during 2019. • This will be in the workforce baseline • Each PCN needs to be confident with existing service, how it operates and if/how it wishes to develop • Multiple employer options • Claims can be made from April 2021 • Further conversations can follow based on individual PCN preferences for the future of services. 39
Key Questions: How does PCN organise itself? 40
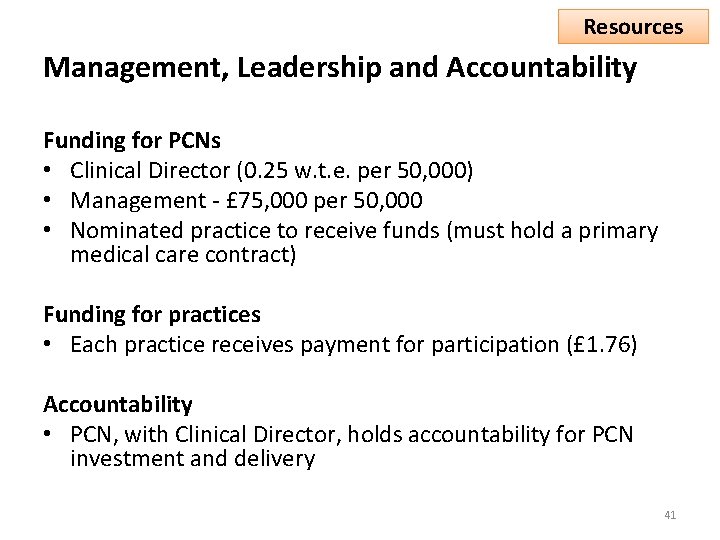
Resources Management, Leadership and Accountability Funding for PCNs • Clinical Director (0. 25 w. t. e. per 50, 000) • Management - £ 75, 000 per 50, 000 • Nominated practice to receive funds (must hold a primary medical care contract) Funding for practices • Each practice receives payment for participation (£ 1. 76) Accountability • PCN, with Clinical Director, holds accountability for PCN investment and delivery 41
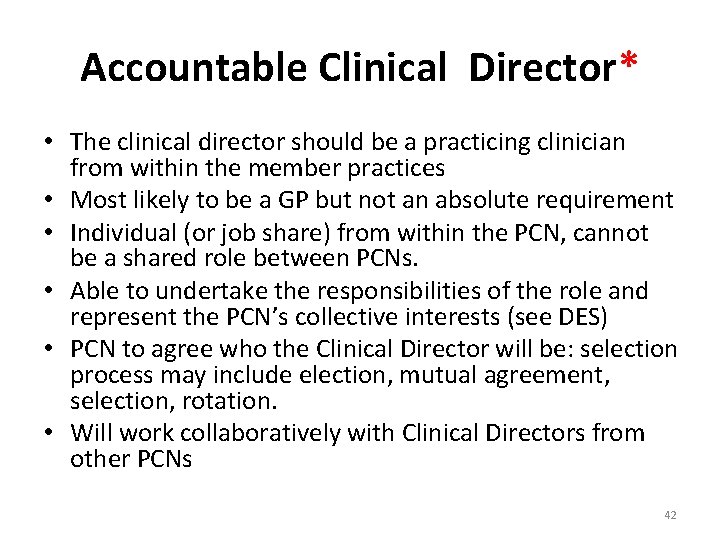
Accountable Clinical Director* • The clinical director should be a practicing clinician from within the member practices • Most likely to be a GP but not an absolute requirement • Individual (or job share) from within the PCN, cannot be a shared role between PCNs. • Able to undertake the responsibilities of the role and represent the PCN’s collective interests (see DES) • PCN to agree who the Clinical Director will be: selection process may include election, mutual agreement, selection, rotation. • Will work collaboratively with Clinical Directors from other PCNs 42
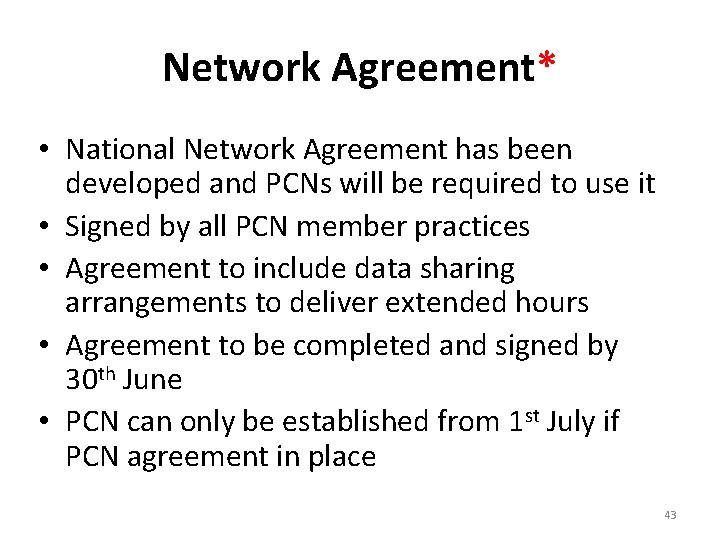
Network Agreement* • National Network Agreement has been developed and PCNs will be required to use it • Signed by all PCN member practices • Agreement to include data sharing arrangements to deliver extended hours • Agreement to be completed and signed by 30 th June • PCN can only be established from 1 st July if PCN agreement in place 43
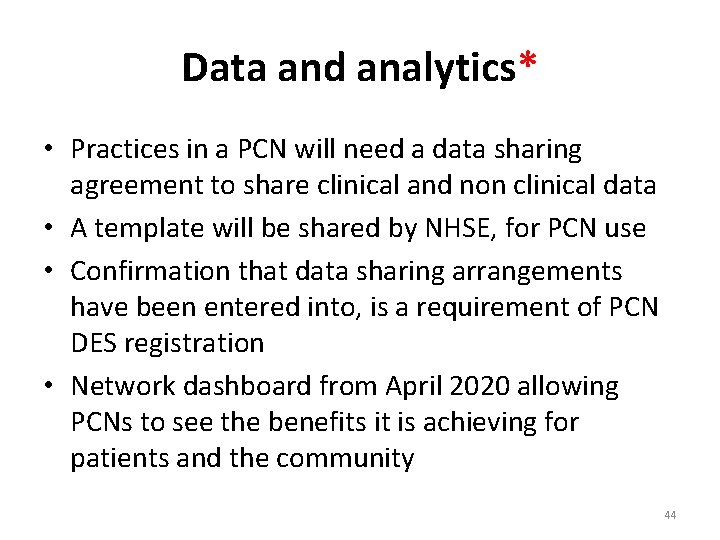
Data and analytics* • Practices in a PCN will need a data sharing agreement to share clinical and non clinical data • A template will be shared by NHSE, for PCN use • Confirmation that data sharing arrangements have been entered into, is a requirement of PCN DES registration • Network dashboard from April 2020 allowing PCNs to see the benefits it is achieving for patients and the community 44
Maintain and develop wider team • General practice takes the leading role in every Primary Care Network, but its important to keep working with the wider network team to achieve the benefits. • PCN DES will include collaboration with non. GP providers from April 2020* • Working with wider partners has led to real change in neighbourhoods in West Essex. 45
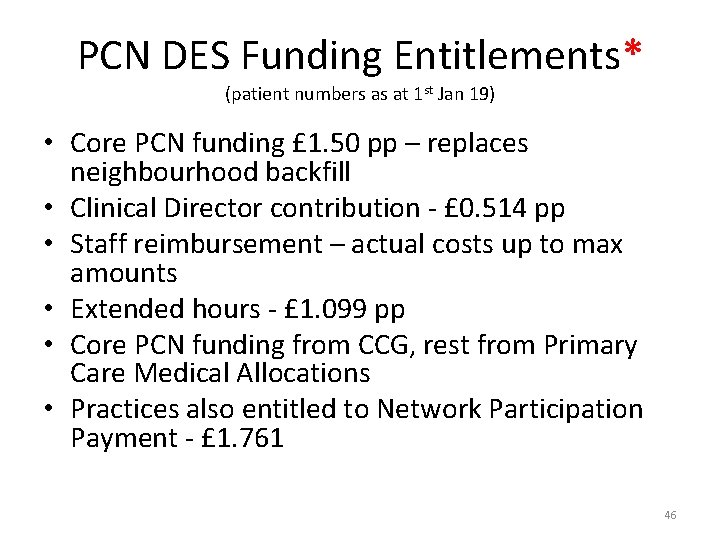
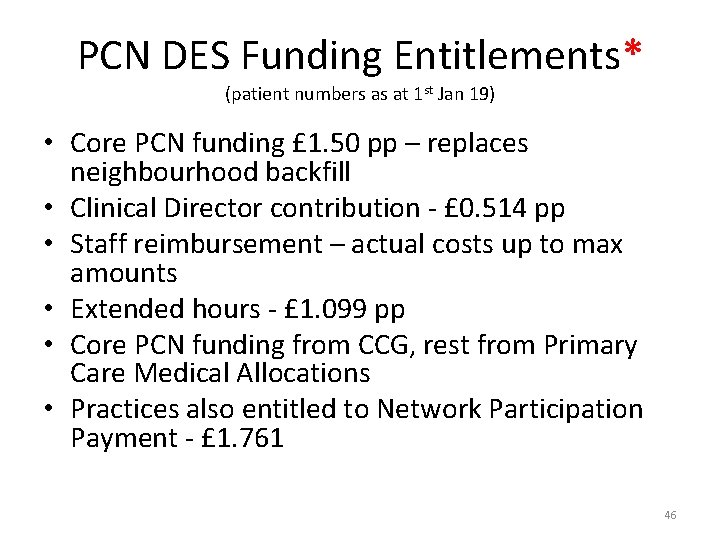
PCN DES Funding Entitlements* (patient numbers as at 1 st Jan 19) • Core PCN funding £ 1. 50 pp – replaces neighbourhood backfill • Clinical Director contribution - £ 0. 514 pp • Staff reimbursement – actual costs up to max amounts • Extended hours - £ 1. 099 pp • Core PCN funding from CCG, rest from Primary Care Medical Allocations • Practices also entitled to Network Participation Payment - £ 1. 761 46
Further Opportunities for PCNs 47
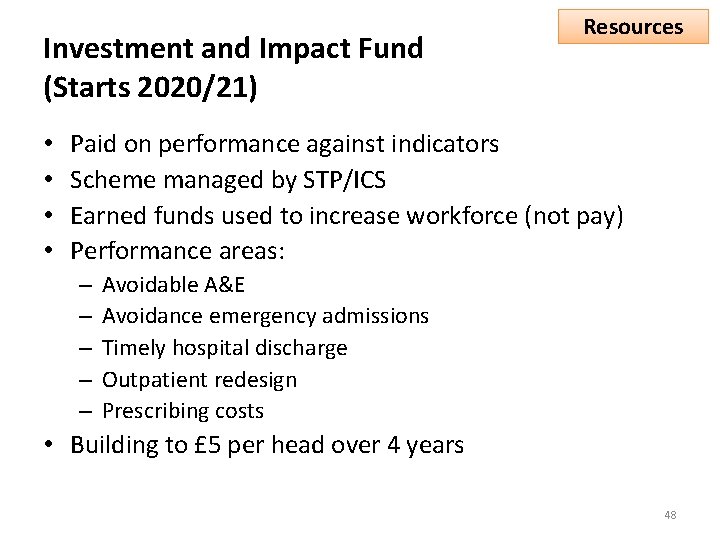
Investment and Impact Fund (Starts 2020/21) • • Resources Paid on performance against indicators Scheme managed by STP/ICS Earned funds used to increase workforce (not pay) Performance areas: – – – Avoidable A&E Avoidance emergency admissions Timely hospital discharge Outpatient redesign Prescribing costs • Building to £ 5 per head over 4 years 48
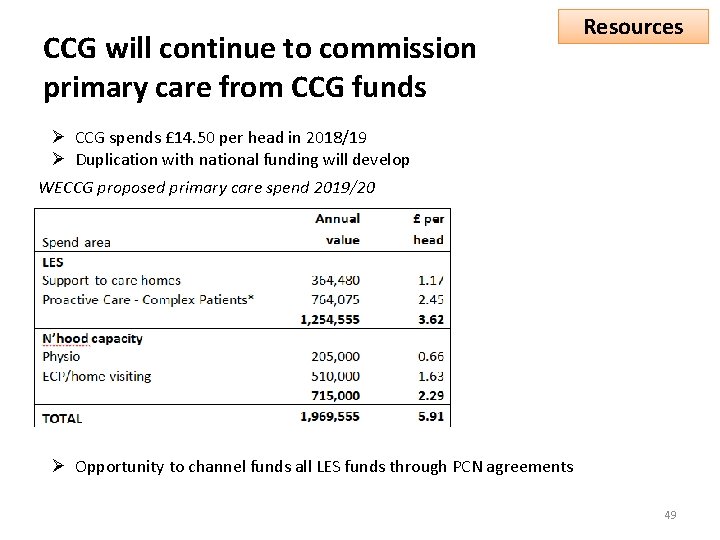
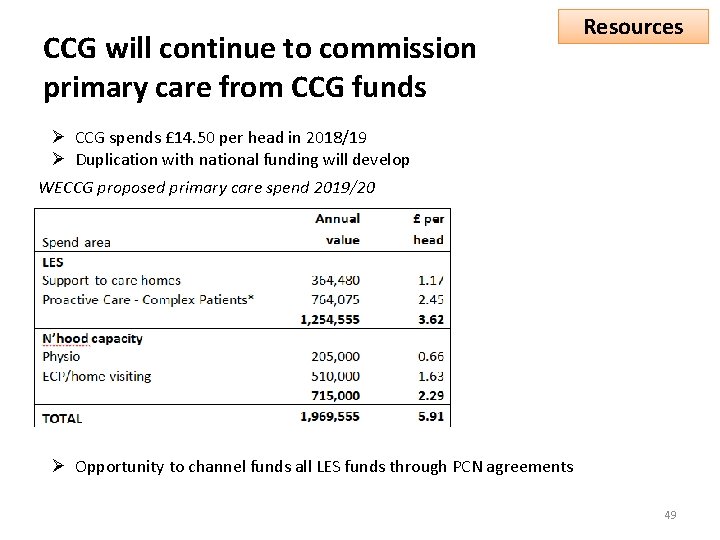
CCG will continue to commission primary care from CCG funds Resources Ø CCG spends £ 14. 50 per head in 2018/19 Ø Duplication with national funding will develop WECCG proposed primary care spend 2019/20 Ø Opportunity to channel funds all LES funds through PCN agreements 49
Next steps 50
Next Steps PCN Application – Which practices – Clinical director – Nominated practice to receive PCN funding – Map 51
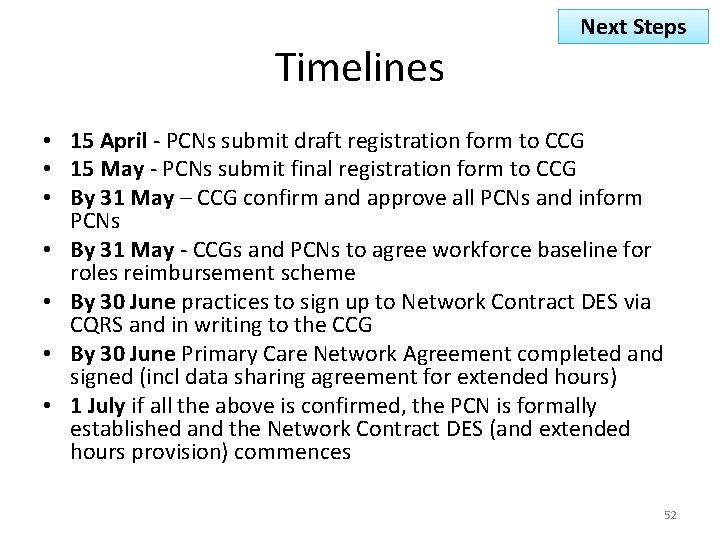
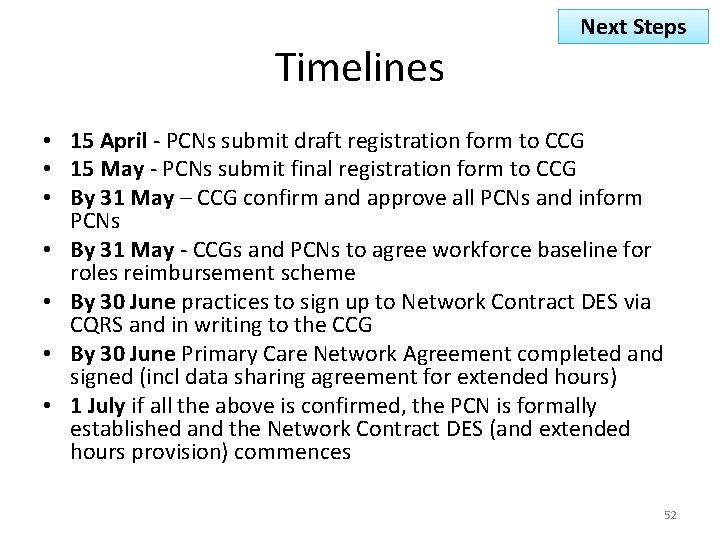
Timelines Next Steps • 15 April - PCNs submit draft registration form to CCG • 15 May - PCNs submit final registration form to CCG • By 31 May – CCG confirm and approve all PCNs and inform PCNs • By 31 May - CCGs and PCNs to agree workforce baseline for roles reimbursement scheme • By 30 June practices to sign up to Network Contract DES via CQRS and in writing to the CCG • By 30 June Primary Care Network Agreement completed and signed (incl data sharing agreement for extended hours) • 1 July if all the above is confirmed, the PCN is formally established and the Network Contract DES (and extended hours provision) commences 52
Next Steps PCN first delivery objectives • Extended Hours DES and 100% coverage across the PCN • Plans for additional roles 2019/20 – Social prescribing – Clinical pharmacist • CCG neighbourhood commissioned services – Emergency care practitioner – First contact physiotherapy – Treatment room and safer anticoagulant prescribing – Spirometry model 53
Table discussion 1 – Establishing PCNs By the end of the afternoon, we suggest you have made progress on the following: – PCN and practices within the PCN – Who may be interested in the Clinical Director role and process for agreeing this – Practice to receive PCN funding – And/or agreement on further discussions needed and timetable • Note any clarification questions you have on the PCN guidance and/or what support you would like from the CCG over the coming months • Templates on the table • CCG staff in Boardroom if you have any queries or would like support • Tea/coffee available all afternoon 54
Table discussion 2 – first areas of work • Extended Hours DES and 100% coverage across the PCN • Plans for additional roles 2019/20 – Social prescribing – Clinical pharmacist • CCG neighbourhood commissioned services – Emergency care practitioner – First contact physiotherapy – Treatment room and safer anticoagulant prescribing – Spirometry model 55
 West essex primary care trust
West essex primary care trust Levels of health care primary secondary tertiary
Levels of health care primary secondary tertiary West essex scitt
West essex scitt Damion macioci
Damion macioci Herts and west essex stp
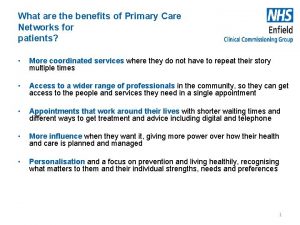
Herts and west essex stp Benefits of primary care networks
Benefits of primary care networks Essex primary scitt
Essex primary scitt Essex primary scitt
Essex primary scitt West lancashire primary care trust
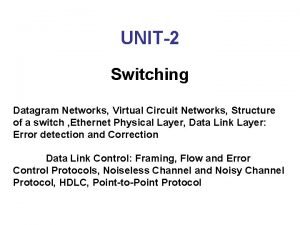
West lancashire primary care trust Difference between datagram and virtual circuit operation
Difference between datagram and virtual circuit operation Basestore iptv
Basestore iptv Wind is horizontal movement of air
Wind is horizontal movement of air What creates wind
What creates wind Noord zuid oost west
Noord zuid oost west East is east and west is west
East is east and west is west Old west vs new west
Old west vs new west West kilbride primary school uniform
West kilbride primary school uniform West kilbride primary school
West kilbride primary school Secta training academy
Secta training academy Iosh training essex
Iosh training essex American hero by essex hemphill analysis
American hero by essex hemphill analysis Oates essex
Oates essex Ciacc essex county
Ciacc essex county Roots and fruits behaviour
Roots and fruits behaviour Effective support for families in essex
Effective support for families in essex 7 kingdoms of england
7 kingdoms of england American hero poem
American hero poem Family solutions essex
Family solutions essex Effective support for children and families in essex
Effective support for children and families in essex Hudson essex passaic soil conservation district
Hudson essex passaic soil conservation district Essex to berkshire
Essex to berkshire Joint meeting of essex and union counties
Joint meeting of essex and union counties Self harm toolkit essex
Self harm toolkit essex 7 minute safeguarding briefings essex
7 minute safeguarding briefings essex Fairplay house essex
Fairplay house essex Essex infolink
Essex infolink Sindrom volkmann
Sindrom volkmann Ligne de hunter
Ligne de hunter Nqt manager essex
Nqt manager essex Beowulf time period
Beowulf time period Jo barclay essex safeguarding
Jo barclay essex safeguarding Essex infolink safeguarding
Essex infolink safeguarding Pronazione e supinazione avambraccio
Pronazione e supinazione avambraccio Talamo del calcaneo
Talamo del calcaneo Jo barclay
Jo barclay Fire risk assessment essex
Fire risk assessment essex Fha connection
Fha connection Ata carnet essex
Ata carnet essex West yorkshire and harrogate health and care partnership
West yorkshire and harrogate health and care partnership South west london health and care partnership
South west london health and care partnership North west end of life care model
North west end of life care model Skh st peter's primary school
Skh st peter's primary school Implementing hrd programs pdf
Implementing hrd programs pdf Management issues central to strategy implementation
Management issues central to strategy implementation Strategic management chapter 7
Strategic management chapter 7 Chapter 7 strategic management
Chapter 7 strategic management