Implementing PatientCentered Medical Home The Cheshire Medical CenterDartmouthHitchcock








- Slides: 50
Implementing Patient-Centered Medical Home: The Cheshire Medical Center/Dartmouth-Hitchcock Keene Experience Betsy Cotter Senior Director of Ambulatory Services 1
Our Community and Organization 2
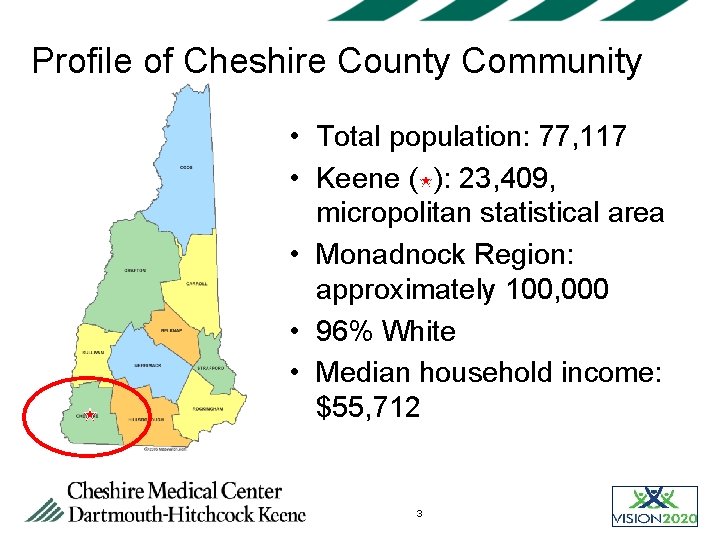
Profile of Cheshire County Community • Total population: 77, 117 • Keene ( ): 23, 409, micropolitan statistical area • Monadnock Region: approximately 100, 000 • 96% White • Median household income: $55, 712 3
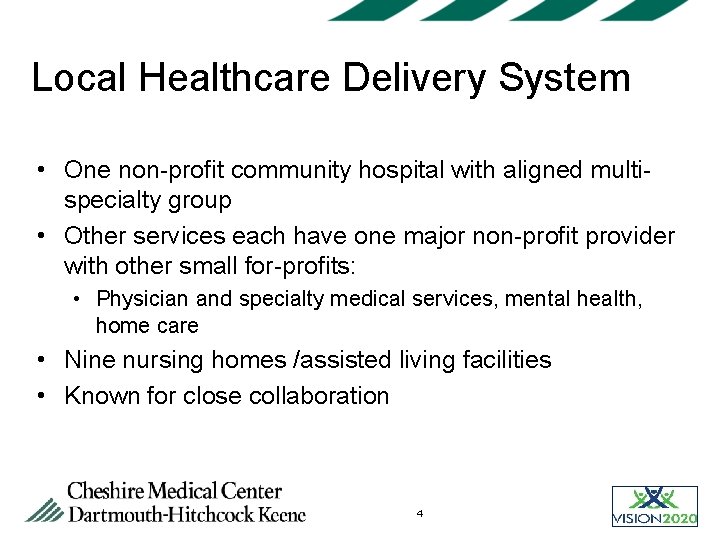
Local Healthcare Delivery System • One non-profit community hospital with aligned multispecialty group • Other services each have one major non-profit provider with other small for-profits: • Physician and specialty medical services, mental health, home care • Nine nursing homes /assisted living facilities • Known for close collaboration 4
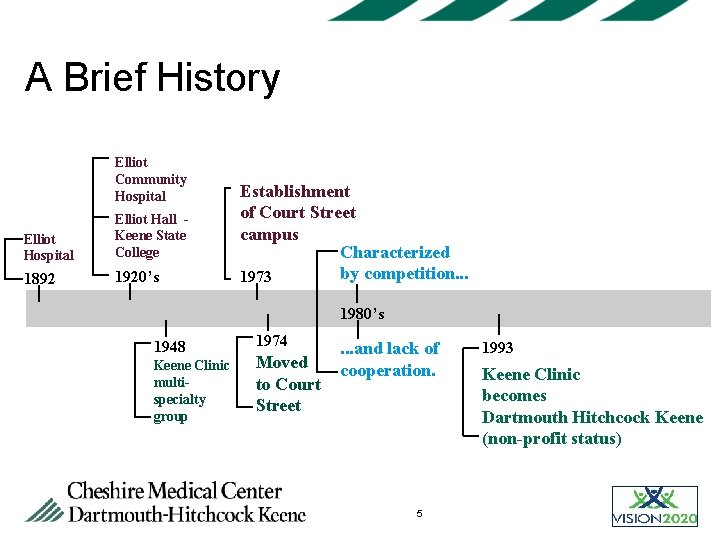
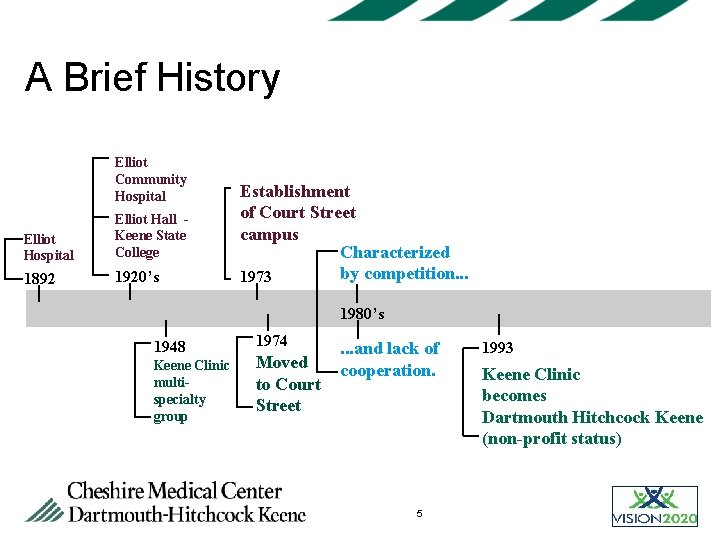
A Brief History Elliot Community Hospital Elliot Hall Keene State College 1892 1920’s Establishment of Court Street campus Characterized by competition. . . 1973 1980’s 1948 Keene Clinic multispecialty group 1974 Moved to Court Street . . . and lack of cooperation. 5 1993 Keene Clinic becomes Dartmouth Hitchcock Keene (non-profit status)
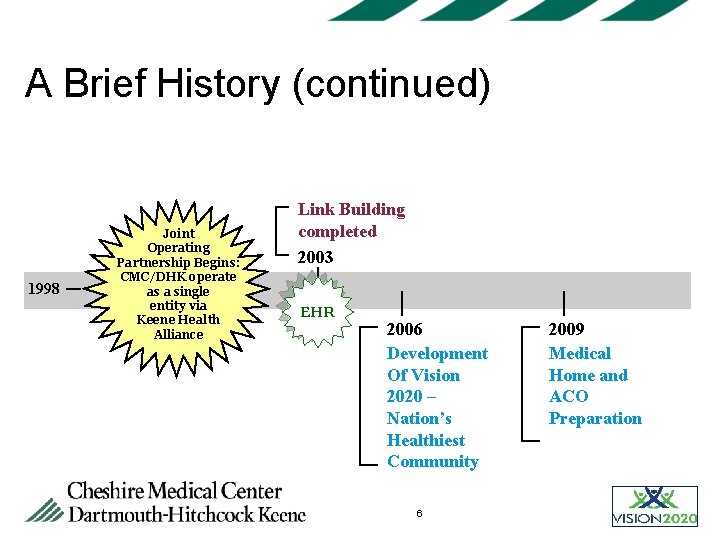
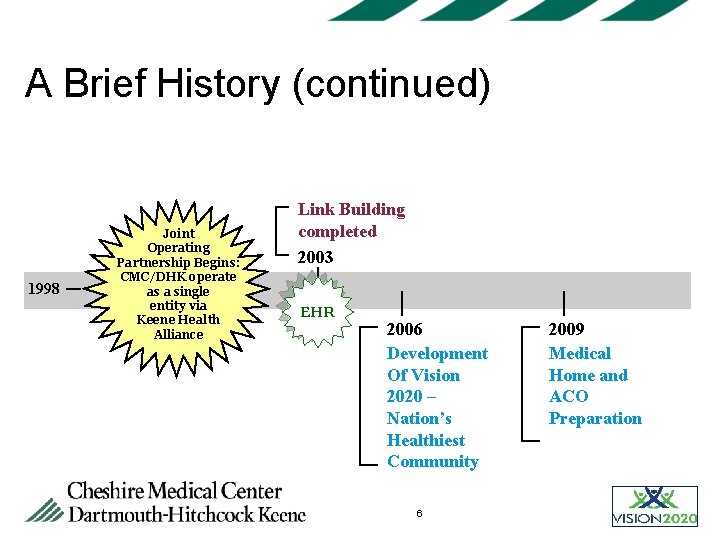
A Brief History (continued) 1998 Joint Operating Partnership Begins: CMC/DHK operate as a single entity via Keene Health Alliance Link Building completed 2003 EHR 2006 Development Of Vision 2020 – Nation’s Healthiest Community 6 2009 Medical Home and ACO Preparation

Cheshire Medical Center / Dartmouth Hitchcock Keene Organizational Relationships DH Healthcare Cheshire Medical Center Dartmouth Hitchcock Clinic Dartmouth Hitchcock Keene KEENE HEALTH ALLIANCE CMC/DHK CAC 7 Joint Operating Partnership

Intent of CMC/DHK Partnership Agreement (KHA) • Build a patient-driven collaborative partnership; integrate physician staff into clinic and hospital operations. • Integrate all hospital operations of CMC and DH Keene clinically, administratively and financially. • Integrate clinical services, infrastructure, and support services with DHK. • Maximize clinical synergy with DH system • Clinical services support, crossover, cooperation • Physician recruiting • Partnership has fostered our ability to create Vision 2020 8
Our Vision and Philosophy 9
A Shared Vision Cheshire County is the healthiest community in the nation by the year 2020 (Vision 2020) 10

Vision 2020 is Culture Change Building a community culture that values “ownership” of population and personal health 11
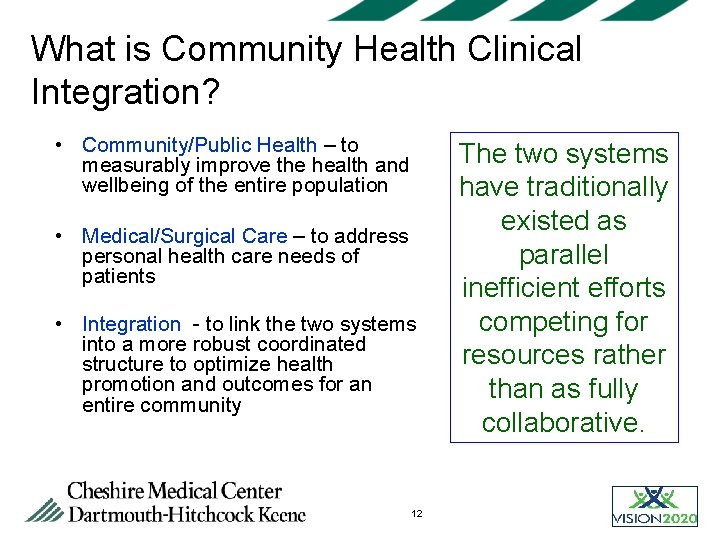
What is Community Health Clinical Integration? • Community/Public Health – to measurably improve the health and wellbeing of the entire population • Medical/Surgical Care – to address personal health care needs of patients • Integration - to link the two systems into a more robust coordinated structure to optimize health promotion and outcomes for an entire community 12 The two systems have traditionally existed as parallel inefficient efforts competing for resources rather than as fully collaborative.
The Imperative and Implementation Considerations 13

Not Enough Time in the Day Advisory Board States: Primary Care alone cannot provide comprehensive care and maintain panel size! PCP estimated time for patient care per day Acute Needs 3. 7 hours Chronic Needs 10. 6 hours Preventative Services 7. 4 hours Total 21. 7 hours (Estimate based on panel size of 2, 500 patients; average DHK PCP panel 2, 200 – some 2, 700 ) 14
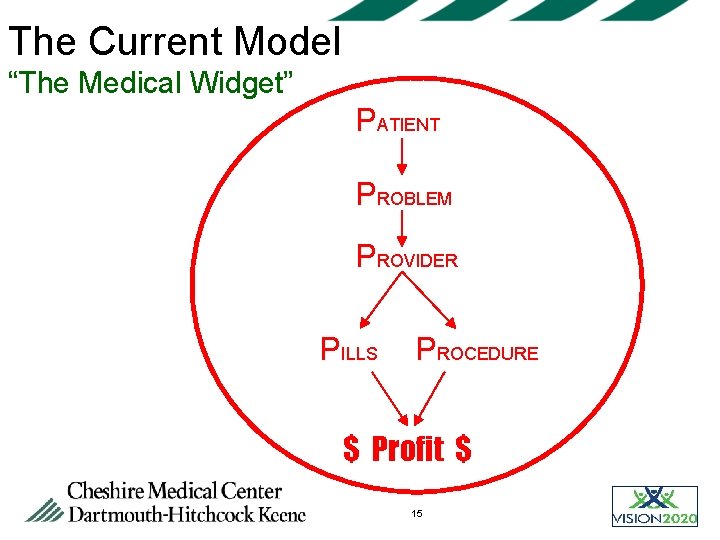
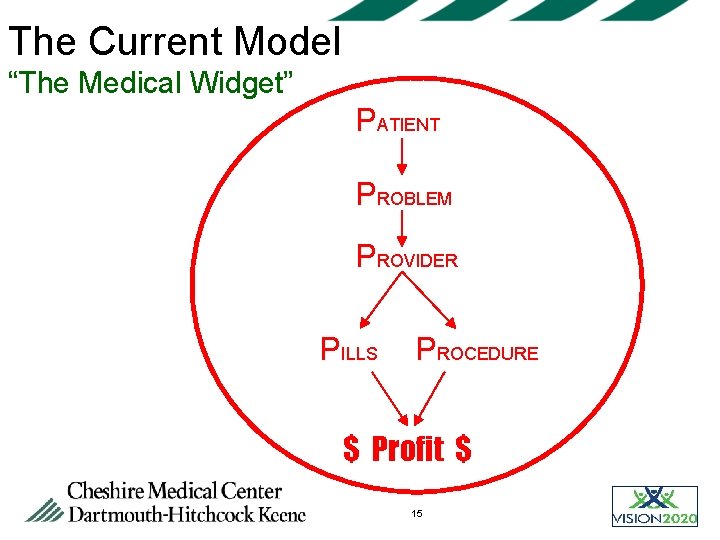
The Current Model “The Medical Widget” PATIENT PROBLEM PROVIDER PILLS PROCEDURE $ Profit $ 15
Transforming Primary Care “…The gap between the supply of primary care physicians and the demand for primary care continues to grow. Primary care practices must find a way to increase their patient capacity without sacrificing quality of care or adding more work to already overburdened providers…. ” Margolius D. Health Affairs; 29: 5 779 16
The Future • Practices must adapt to the reality of large panels • These panels of patients will have increasingly serious illness or complexity of illness • Reimbursement must be addressed! 17
From Individual to Population Focus • Paradigm shift • Team based approach…. not everything needs to land in the lap of the provider. • Consider asking this utopian question “What can our primary care team do today to make our panel of patients as healthy as possible” 18

New Way: Results • A different mode of care: • Patients with less frequent follow-ups have health outcomes equal to more frequent follow-ups • Expanded access for all • Out-of-office care: • Consider time being “scheduled” for desk-top medicine • Impact on providers and patients: • Improved satisfaction for both parties 19
Why the Medical Home Model? The Bottom Line • Primary care is cost and quality effective • PCP supply inadequate to meet needs of the traditional model • Care coordination and disease management of chronic conditions, needed more than ever • The Medical Home Model an effective way forward 20
Key Aspects of the Medical Home 21
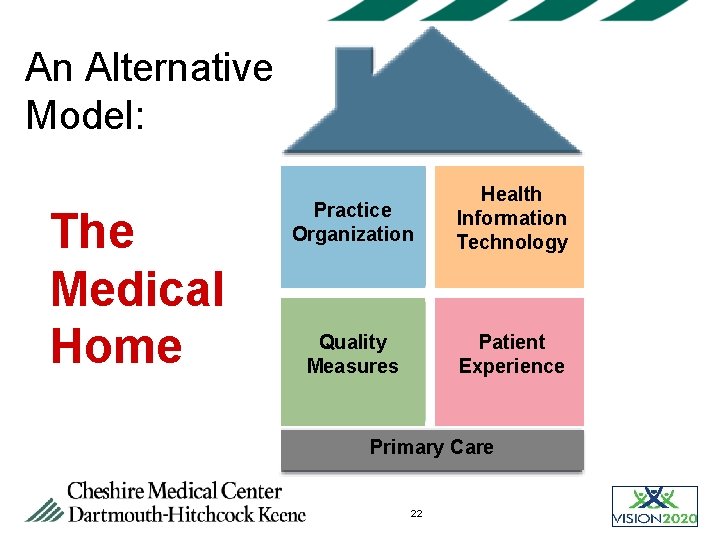
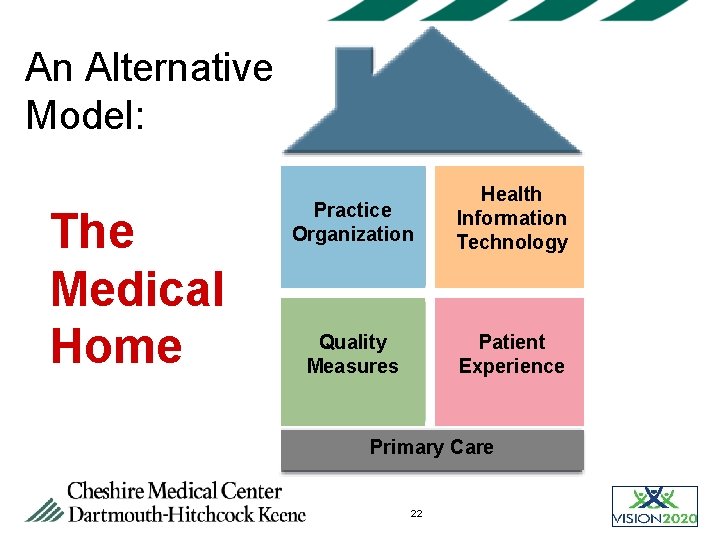
An Alternative Model: The Medical Home Practice Organization Health Information Technology Quality Measures Patient Experience Primary Care 22

Medical Home Task Force First meeting 2/11/09 • FM Nurse leaders • FM Chair & Physician Team Leaders • Pediatrics Chair • Pediatric APRN • Informatics • Care Coordinators • Senior leadership • • • Registry Coordinators Patient Representatives OB-GYN Chair Ob-GYN Team Leader Interested FM MD & APRNs 23
Task Force Mission I. Design a comprehensive and operable Medical Home model for DHK II. Progressively implement and evaluate elements of the Medical Home model as expediently as resources allow 24
Medical Home Principles • • Personal Physician (Provider) Team Based Care Whole Person Orientation Care is Coordinated / Integrated Quality Improvement / Safety / Evidenced-Based Standardization of Practice Enhanced Access however appropriate Payment Reform – system-wide contracting 25

Medical Home Personnel Costs ______________________________________________________________ Approximately 40, 000 adults impaneled with 5, 000+ per care coordinator Staff: • Care Coordinators (RNs) (7) • Patient Registry Coordinators (2) Salary / Benefits $ 700, 000 Behavioral Health Integration: • Ph. D. Psychologists (2) • Psychiatrists (1. 3 FTE) Net Revenue Less Salary / Benefits $ 300, 000 Total: $1, 000 26
Role of Care Coordinators • Listening to and assessing patient’s needs • Building relationships through collaboration and teamwork • Facilitating access and advocating for appropriate care • Developing care action plans in partnership with patient and family 27
Pre-Visit Work New and existing patients • • • Centralized intake calls Medication reconciliation Pre-visit testing Increasing access Querying for patient priorities Patient & provider satisfaction 28
Care Action Plans • Patient centered partnership • Patient-friendly, customized medication list • Portable • “Living” • Future is to embed fully into the EHR 29
Hospital Visits • “Touching” our patients • Building the bridge back to Primary Care • Coordination of discharge planning with inpatient and outpatient care coordinators • Setting the stage for follow up phone calls 30

Post Discharge Calls by ambulatory care coordinator § Continuity § Coordination § Troubleshooting 31
Quality: Access Alternatives to Traditional Office Visit • • • Expansion of FM Acute Care – 2 PCPs for overflow New Patient Phone Visit/questionnaire Pre-visit Planning Ongoing Care Coordination Group Visits for Hypertension, DM, Prenatal Care Self Management DVDs RN Hypertension Visits Home Visit Pilot – MD & NP for home-bound Patient-on-Line – Q&A, refills, appointments 32
Efficiency Everyone Working to the Top of Their License • • APRN PCP’s POC testing and titration Streamlined medication renewal process R. N. disease monitoring visits Medication titration protocols Telephone follow-up Forms completion process – now mostly MA’s 33
Transformational Strategies 1) Sharing & comparing of data amongst providers, nursing, and staff; standardize high-risk or flawed process 2) Use of registry data to improve chronic disease management and preventive care delivery, including gap in care reports from insurers 3) Leverage EHR for safety, communication, and quality measurement. Be wary of the pitfalls. 4) Care is continuous and patient-centered, not episodic doctor -centered. 34
Transformational Strategies (Continued) 5) New concepts in patient access & management 6) QI work becomes a routine part of daily work 7) Administration values and supports this work 35
Accountable Care Organization • Patient Centered Medical Home is the foundation for an ACO • Funding is irrelevant • However the funding premise is that: • Cost savings are shared • Performance measurement – both utilization management and quality (best practice approach) are essential 36
Accountable Care Organization • Evidence-based care drives best practice approach • Best Practice approach drives value • Value = Quality / Cost 37
Applied Medical Home Strategies Improving Care of COPD 38
Improving the Care of C. O. P. D. Exacerbation ØHigh burden ØVariability in care delivery ØYet current best practice is well established 39
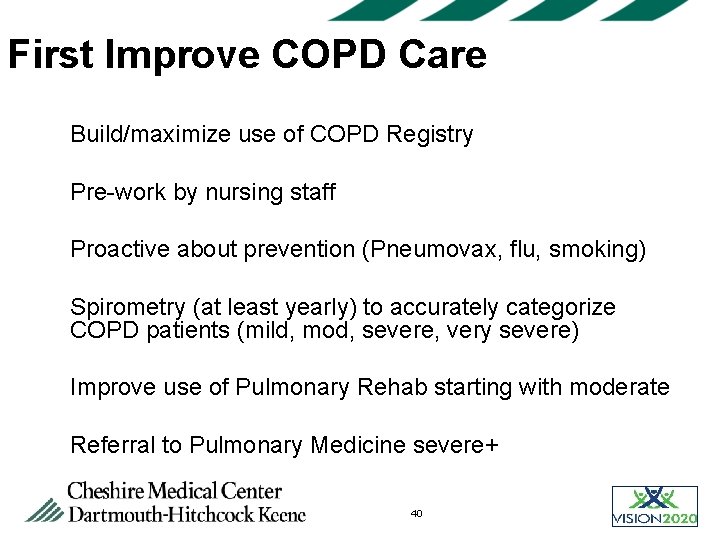
First Improve COPD Care Ø Build/maximize use of COPD Registry Ø Pre-work by nursing staff Ø Proactive about prevention (Pneumovax, flu, smoking) Ø Spirometry (at least yearly) to accurately categorize COPD patients (mild, mod, severe, very severe) Ø Improve use of Pulmonary Rehab starting with moderate Ø Referral to Pulmonary Medicine severe+ 40
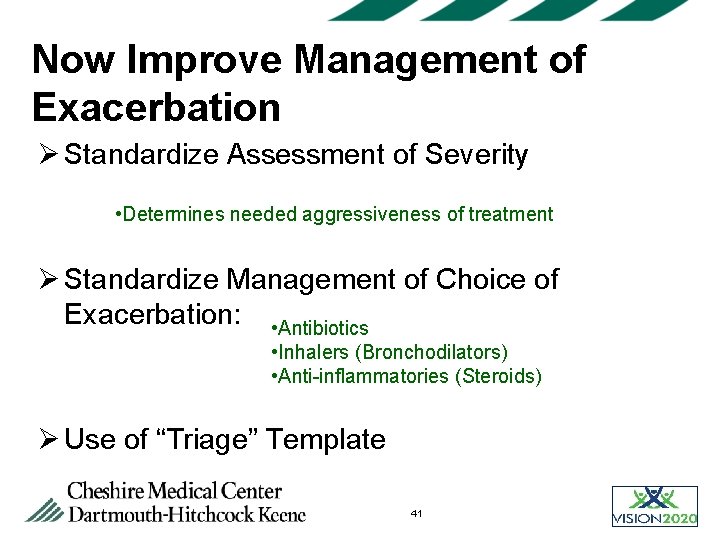
Now Improve Management of Exacerbation Ø Standardize Assessment of Severity • Determines needed aggressiveness of treatment Ø Standardize Management of Choice of Exacerbation: • Antibiotics • Inhalers (Bronchodilators) • Anti-inflammatories (Steroids) Ø Use of “Triage” Template 41
Quality Measures and Outcomes 42
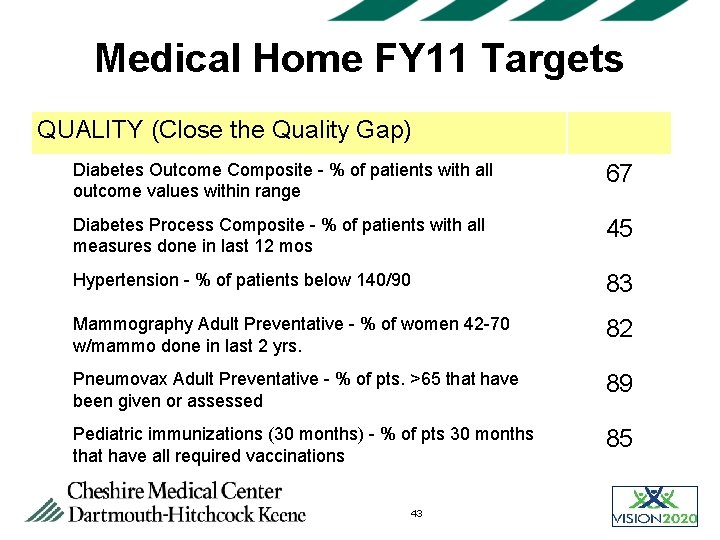
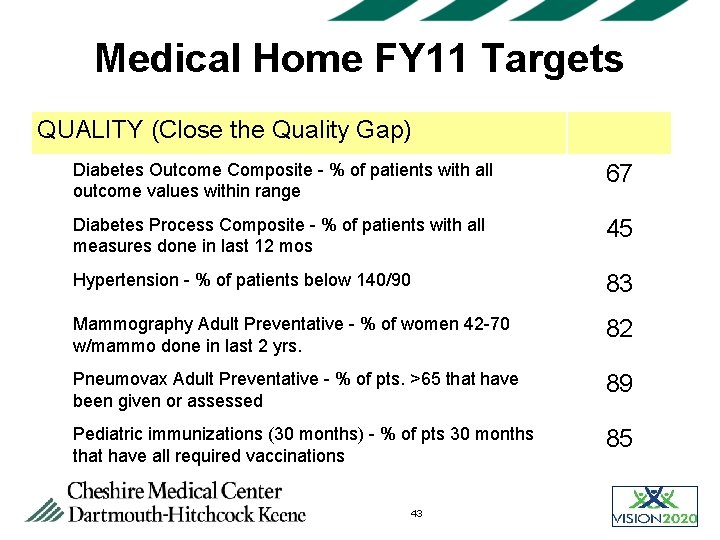
Medical Home FY 11 Targets QUALITY (Close the Quality Gap) Diabetes Outcome Composite - % of patients with all outcome values within range 67 Diabetes Process Composite - % of patients with all measures done in last 12 mos 45 Hypertension - % of patients below 140/90 83 Mammography Adult Preventative - % of women 42 -70 w/mammo done in last 2 yrs. 82 Pneumovax Adult Preventative - % of pts. >65 that have been given or assessed 89 Pediatric immunizations (30 months) - % of pts 30 months that have all required vaccinations 85 43
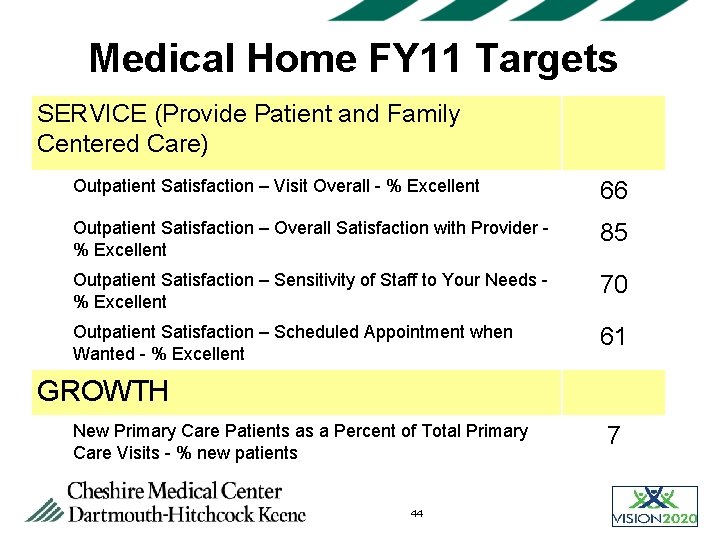
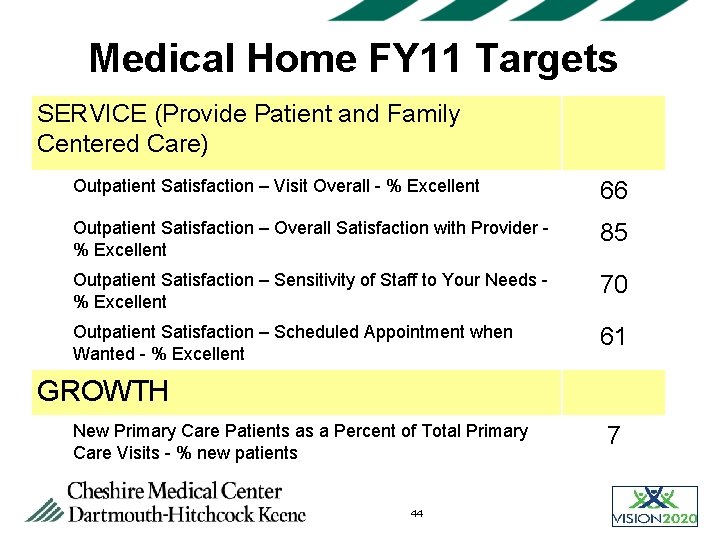
Medical Home FY 11 Targets SERVICE (Provide Patient and Family Centered Care) Outpatient Satisfaction – Visit Overall - % Excellent 66 Outpatient Satisfaction – Overall Satisfaction with Provider % Excellent 85 Outpatient Satisfaction – Sensitivity of Staff to Your Needs % Excellent 70 Outpatient Satisfaction – Scheduled Appointment when Wanted - % Excellent 61 GROWTH New Primary Care Patients as a Percent of Total Primary Care Visits - % new patients 44 7
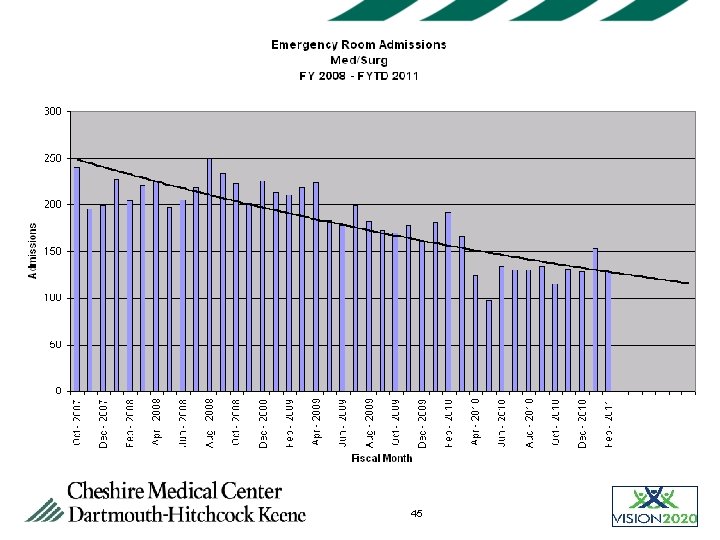
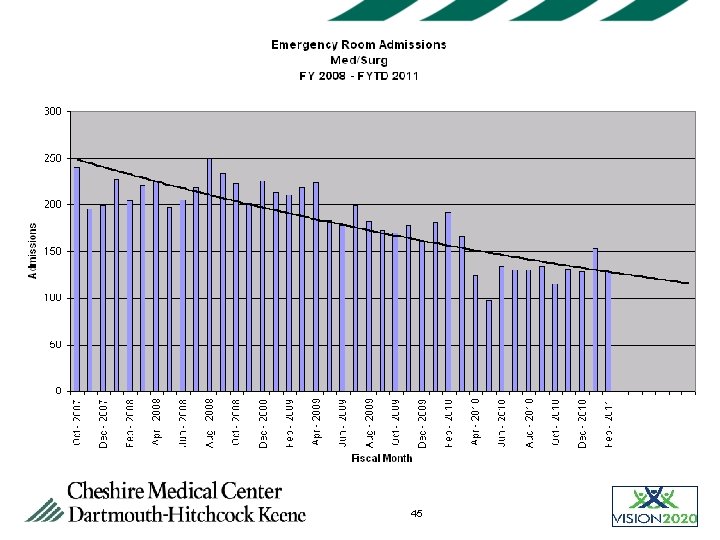
45
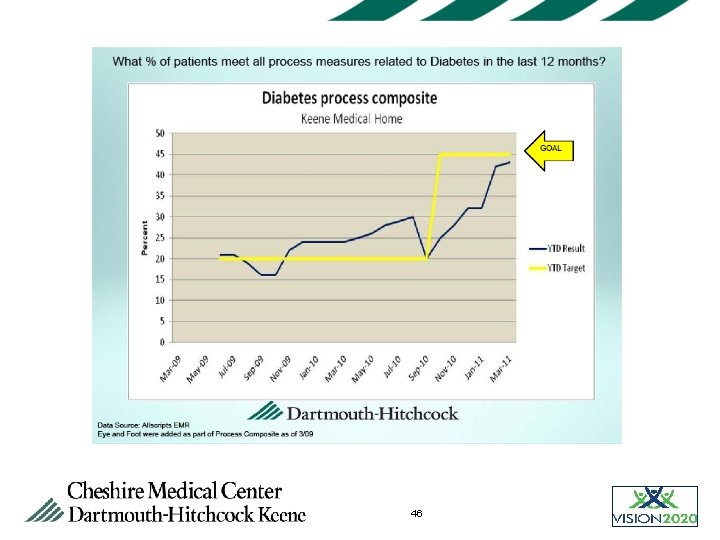
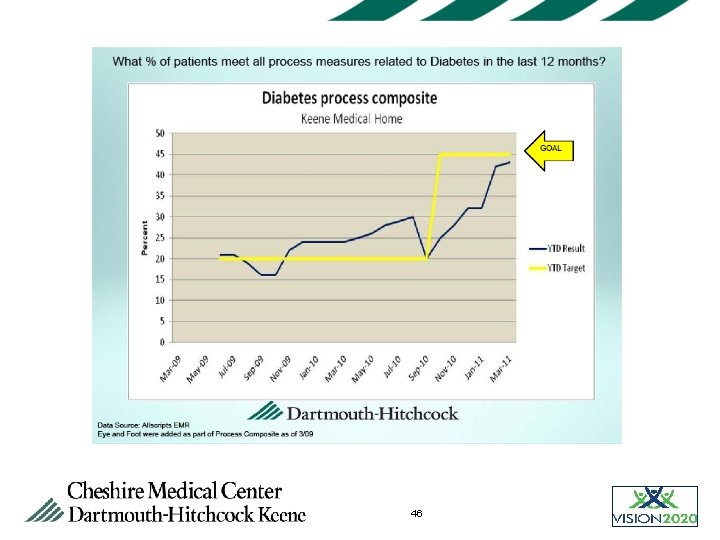
46
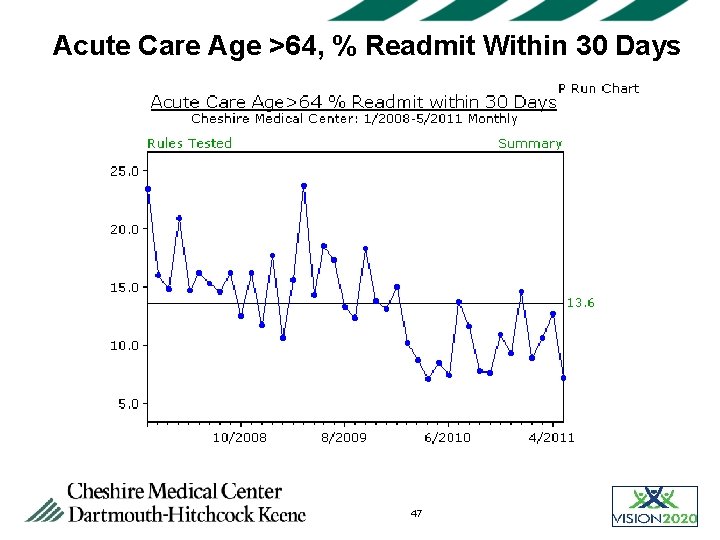
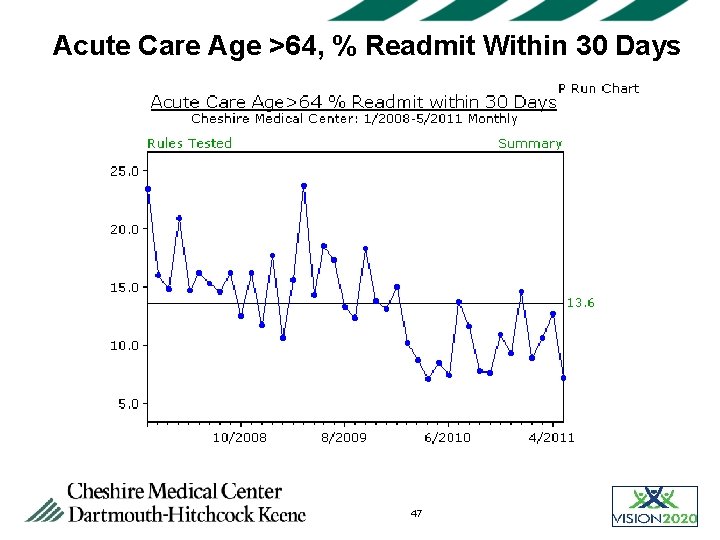
Acute Care Age >64, % Readmit Within 30 Days 47
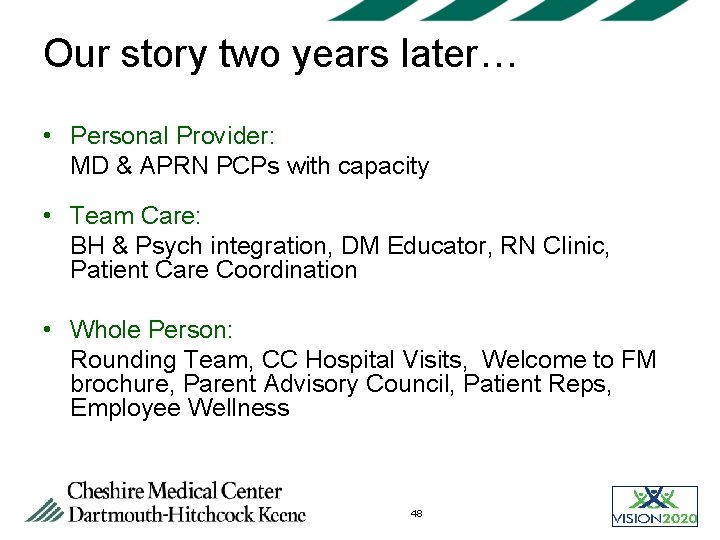
Our story two years later… • Personal Provider: MD & APRN PCPs with capacity • Team Care: BH & Psych integration, DM Educator, RN Clinic, Patient Care Coordination • Whole Person: Rounding Team, CC Hospital Visits, Welcome to FM brochure, Parent Advisory Council, Patient Reps, Employee Wellness 48
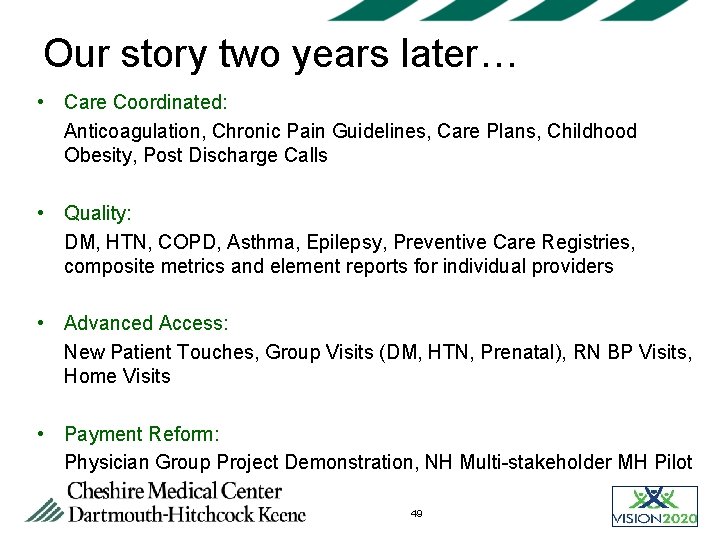
Our story two years later… • Care Coordinated: Anticoagulation, Chronic Pain Guidelines, Care Plans, Childhood Obesity, Post Discharge Calls • Quality: DM, HTN, COPD, Asthma, Epilepsy, Preventive Care Registries, composite metrics and element reports for individual providers • Advanced Access: New Patient Touches, Group Visits (DM, HTN, Prenatal), RN BP Visits, Home Visits • Payment Reform: Physician Group Project Demonstration, NH Multi-stakeholder MH Pilot 49
Summary • Strong leadership, vision, and a clear structure for partnerships are critical • Medical Home is a more sustainable model and improves value • Integration with community health is essential to create the Medical Village of the future • Medical Home is critical to success for ACO 50
 St claret school barrackpore
St claret school barrackpore Fahrenheit 451 pages 67-76 summary
Fahrenheit 451 pages 67-76 summary Cheshire and merseyside stp
Cheshire and merseyside stp Cheshire constabulary
Cheshire constabulary Cheshire cat allusion in fahrenheit 451
Cheshire cat allusion in fahrenheit 451 Cheshire union
Cheshire union Cheshire and merseyside training hub
Cheshire and merseyside training hub Cheshire ireland pay scale
Cheshire ireland pay scale David cheshire aecom
David cheshire aecom Trickster archetype
Trickster archetype Plural of flower
Plural of flower She said that, home economics stands for the ideal home.
She said that, home economics stands for the ideal home. Pengertian homecare
Pengertian homecare Oak springs mobile home park
Oak springs mobile home park Come home come home jesus is calling
Come home come home jesus is calling Home sweet home survival
Home sweet home survival Perbedaan home care dan home visit
Perbedaan home care dan home visit Let's go to my house
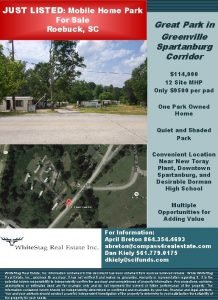
Let's go to my house Mobile home parks for sale in sc
Mobile home parks for sale in sc Jr rabbin imam pretre
Jr rabbin imam pretre Implementing firewall technologies
Implementing firewall technologies Keys to successful project portfolio management
Keys to successful project portfolio management Retail management notes doc
Retail management notes doc Implementing organizational change theory into practice
Implementing organizational change theory into practice Bert spector
Bert spector Planning and implementing crm projects
Planning and implementing crm projects Strategy implementation example
Strategy implementation example Implementing strategies management and operations issues
Implementing strategies management and operations issues Implementing strategies management and operations issues
Implementing strategies management and operations issues Designing and implementing brand strategies
Designing and implementing brand strategies Ubmta
Ubmta Implementing strategies marketing finance/accounting
Implementing strategies marketing finance/accounting Implementing strategies: management and operations issues
Implementing strategies: management and operations issues Designing and implementing brand architecture strategies
Designing and implementing brand architecture strategies Qsen teamwork and collaboration definition
Qsen teamwork and collaboration definition Designing and implementing branding strategies
Designing and implementing branding strategies Implementing hrd programs
Implementing hrd programs Nfpa 1600 business continuity programs
Nfpa 1600 business continuity programs Access rights definition
Access rights definition Tripod pricing strategy
Tripod pricing strategy Nfpa 1600
Nfpa 1600 Challenges of implementing predictive analytics
Challenges of implementing predictive analytics Features and principles of portfolio assessment
Features and principles of portfolio assessment Implementing strategies management and operations issues
Implementing strategies management and operations issues Lp html
Lp html Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết Số.nguyên tố
Số.nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Tư thế worm breton là gì
Tư thế worm breton là gì