Implementing Elder Life Program On Medical Inpatient Hospital
- Slides: 1
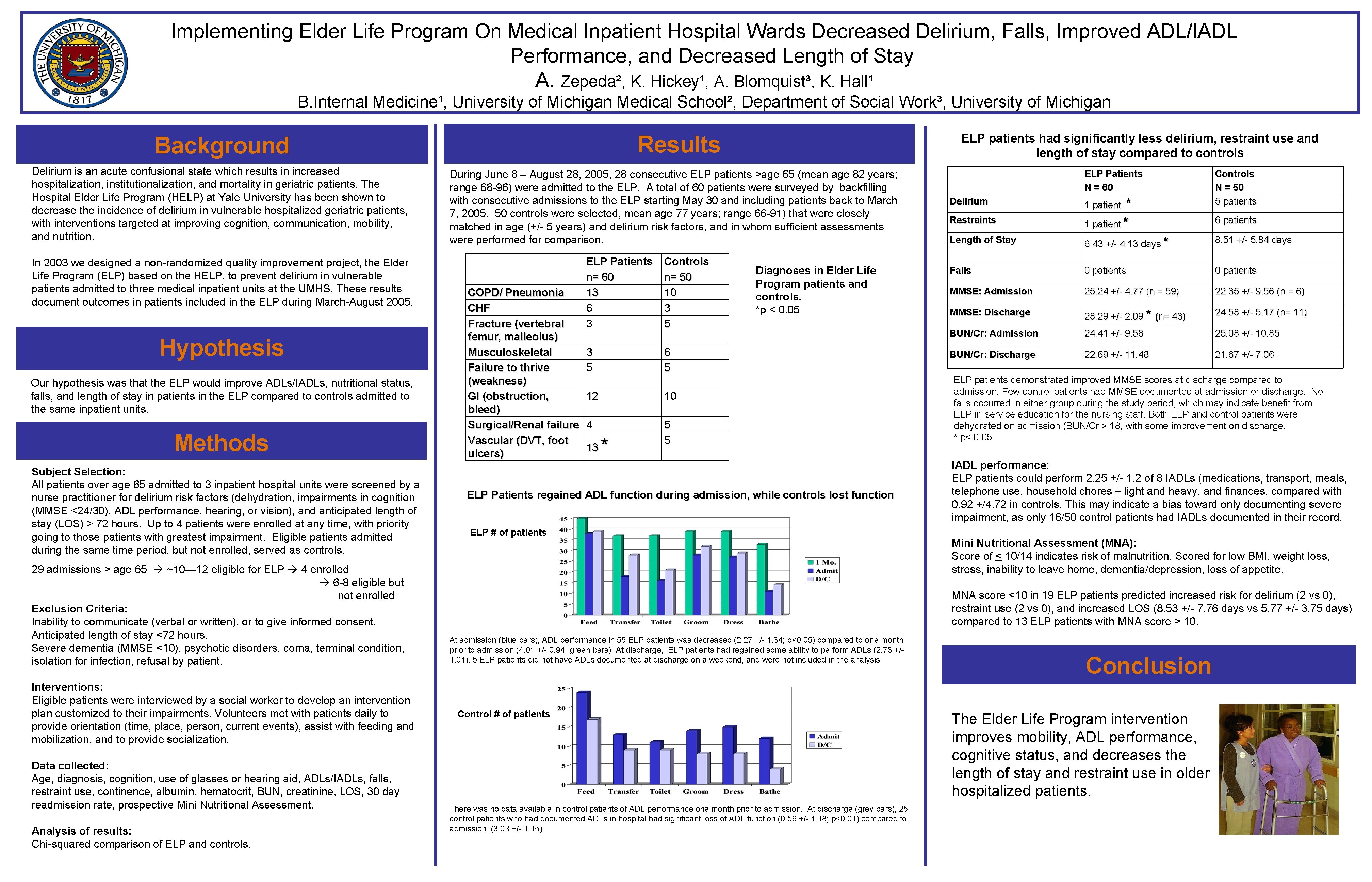
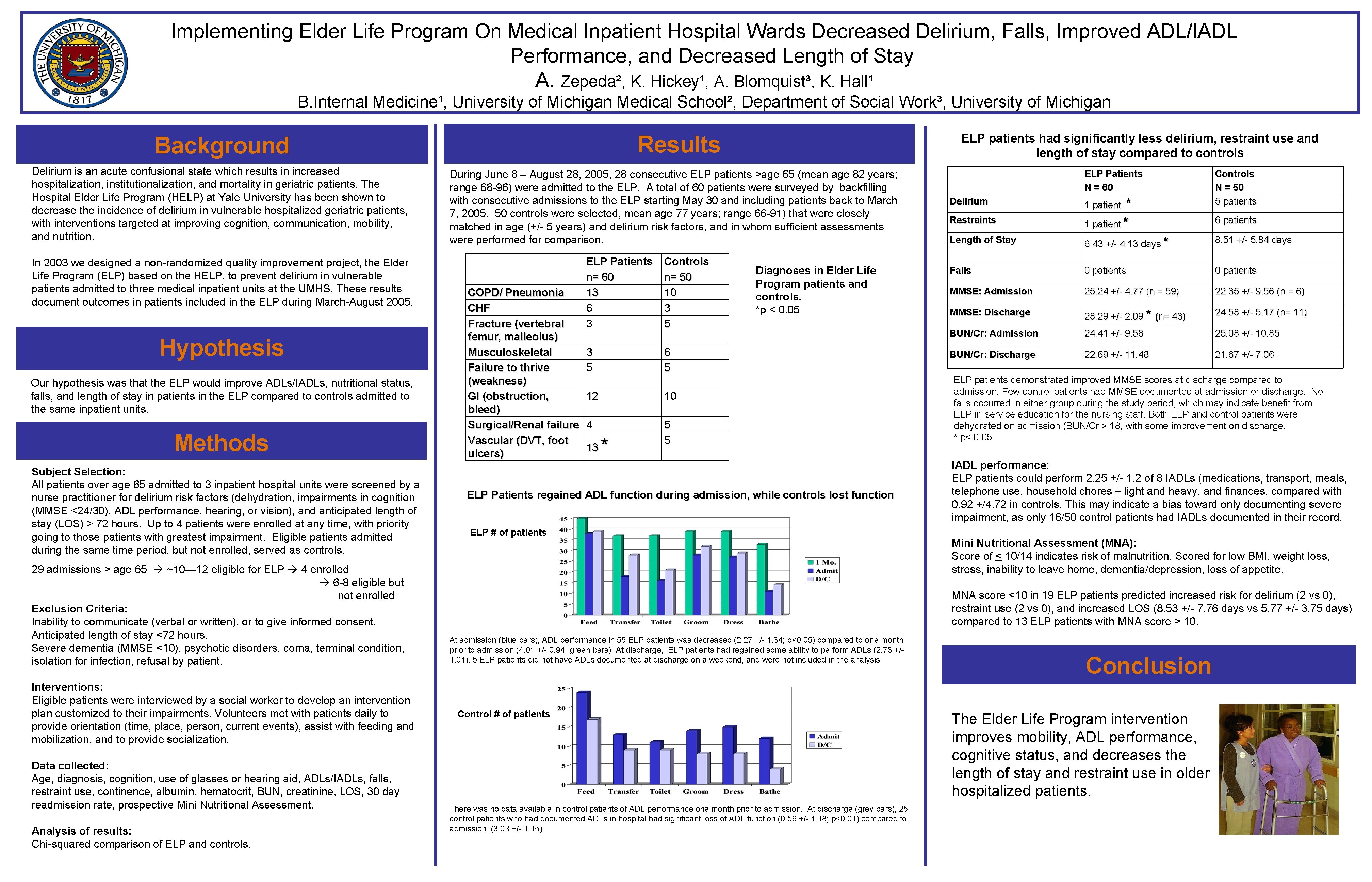
Implementing Elder Life Program On Medical Inpatient Hospital Wards Decreased Delirium, Falls, Improved ADL/IADL Performance, and Decreased Length of Stay A. Zepeda², K. Hickey¹, A. Blomquist³, K. Hall¹ B. Internal Medicine¹, University of Michigan Medical School², Department of Social Work³, University of Michigan Results Background Delirium is an acute confusional state which results in increased hospitalization, institutionalization, and mortality in geriatric patients. The Hospital Elder Life Program (HELP) at Yale University has been shown to decrease the incidence of delirium in vulnerable hospitalized geriatric patients, with interventions targeted at improving cognition, communication, mobility, and nutrition. In 2003 we designed a non-randomized quality improvement project, the Elder Life Program (ELP) based on the HELP, to prevent delirium in vulnerable patients admitted to three medical inpatient units at the UMHS. These results document outcomes in patients included in the ELP during March-August 2005. Hypothesis Our hypothesis was that the ELP would improve ADLs/IADLs, nutritional status, falls, and length of stay in patients in the ELP compared to controls admitted to the same inpatient units. Methods Subject Selection: All patients over age 65 admitted to 3 inpatient hospital units were screened by a nurse practitioner for delirium risk factors (dehydration, impairments in cognition (MMSE <24/30), ADL performance, hearing, or vision), and anticipated length of stay (LOS) > 72 hours. Up to 4 patients were enrolled at any time, with priority going to those patients with greatest impairment. Eligible patients admitted during the same time period, but not enrolled, served as controls. 29 admissions > age 65 ~10— 12 eligible for ELP 4 enrolled 6 -8 eligible but not enrolled Exclusion Criteria: Inability to communicate (verbal or written), or to give informed consent. Anticipated length of stay <72 hours. Severe dementia (MMSE <10), psychotic disorders, coma, terminal condition, isolation for infection, refusal by patient. Interventions: Eligible patients were interviewed by a social worker to develop an intervention plan customized to their impairments. Volunteers met with patients daily to provide orientation (time, place, person, current events), assist with feeding and mobilization, and to provide socialization. Data collected: Age, diagnosis, cognition, use of glasses or hearing aid, ADLs/IADLs, falls, restraint use, continence, albumin, hematocrit, BUN, creatinine, LOS, 30 day readmission rate, prospective Mini Nutritional Assessment. Analysis of results: Chi-squared comparison of ELP and controls. ELP patients had significantly less delirium, restraint use and length of stay compared to controls During June 8 – August 28, 2005, 28 consecutive ELP patients >age 65 (mean age 82 years; range 68 -96) were admitted to the ELP. A total of 60 patients were surveyed by backfilling with consecutive admissions to the ELP starting May 30 and including patients back to March 7, 2005. 50 controls were selected, mean age 77 years; range 66 -91) that were closely matched in age (+/- 5 years) and delirium risk factors, and in whom sufficient assessments were performed for comparison. COPD/ Pneumonia CHF Fracture (vertebral femur, malleolus) Musculoskeletal Failure to thrive (weakness) GI (obstruction, bleed) Surgical/Renal failure Vascular (DVT, foot ulcers) ELP Patients n= 60 13 6 3 Controls n= 50 10 3 5 6 5 12 10 4 5 5 13 * Diagnoses in Elder Life Program patients and controls. *p < 0. 05 ELP Patients regained ADL function during admission, while controls lost function ELP # of patients ELP Patients N = 60 Delirium Restraints * 1 patient Controls N = 50 5 patients 6 patients Length of Stay 6. 43 +/- 4. 13 days * 8. 51 +/- 5. 84 days Falls 0 patients MMSE: Admission 25. 24 +/- 4. 77 (n = 59) 22. 35 +/- 9. 56 (n = 6) MMSE: Discharge 28. 29 +/- 2. 09 * (n= 43) 24. 58 +/- 5. 17 (n= 11) BUN/Cr: Admission 24. 41 +/- 9. 58 25. 08 +/- 10. 85 BUN/Cr: Discharge 22. 69 +/- 11. 48 21. 67 +/- 7. 06 ELP patients demonstrated improved MMSE scores at discharge compared to admission. Few control patients had MMSE documented at admission or discharge. No falls occurred in either group during the study period, which may indicate benefit from ELP in-service education for the nursing staff. Both ELP and control patients were dehydrated on admission (BUN/Cr > 18, with some improvement on discharge. * p< 0. 05. IADL performance: ELP patients could perform 2. 25 +/- 1. 2 of 8 IADLs (medications, transport, meals, telephone use, household chores – light and heavy, and finances, compared with 0. 92 +/4. 72 in controls. This may indicate a bias toward only documenting severe impairment, as only 16/50 control patients had IADLs documented in their record. Mini Nutritional Assessment (MNA): Score of < 10/14 indicates risk of malnutrition. Scored for low BMI, weight loss, stress, inability to leave home, dementia/depression, loss of appetite. MNA score <10 in 19 ELP patients predicted increased risk for delirium (2 vs 0), restraint use (2 vs 0), and increased LOS (8. 53 +/- 7. 76 days vs 5. 77 +/- 3. 75 days) compared to 13 ELP patients with MNA score > 10. At admission (blue bars), ADL performance in 55 ELP patients was decreased (2. 27 +/- 1. 34; p<0. 05) compared to one month prior to admission (4. 01 +/- 0. 94; green bars). At discharge, ELP patients had regained some ability to perform ADLs (2. 76 +/1. 01). 5 ELP patients did not have ADLs documented at discharge on a weekend, and were not included in the analysis. Control # of patients There was no data available in control patients of ADL performance one month prior to admission. At discharge (grey bars), 25 control patients who had documented ADLs in hospital had significant loss of ADL function (0. 59 +/- 1. 18; p<0. 01) compared to admission (3. 03 +/- 1. 15). Conclusion The Elder Life Program intervention improves mobility, ADL performance, cognitive status, and decreases the length of stay and restraint use in older hospitalized patients.