Implementing casemix funding in China Implementation challenges and


- Slides: 39
Implementing casemix funding in China: Implementation challenges and capacity building 中国的病例组合支付制度:实施挑战 与能力建设 David Legge George Liu La Trobe University China Health Program
Purpose and outline 目的与概要 • Purpose – develop a framework for thinking about capacity building • Implementation Issues – Technical issues – Strategic issues • Capacity building – capacity assessment – capacity building • 目的 –开发能力建设的 思路 • 实施问题 –技术问题 –战略问题 • 能力建设 –能力评价 –能力建设
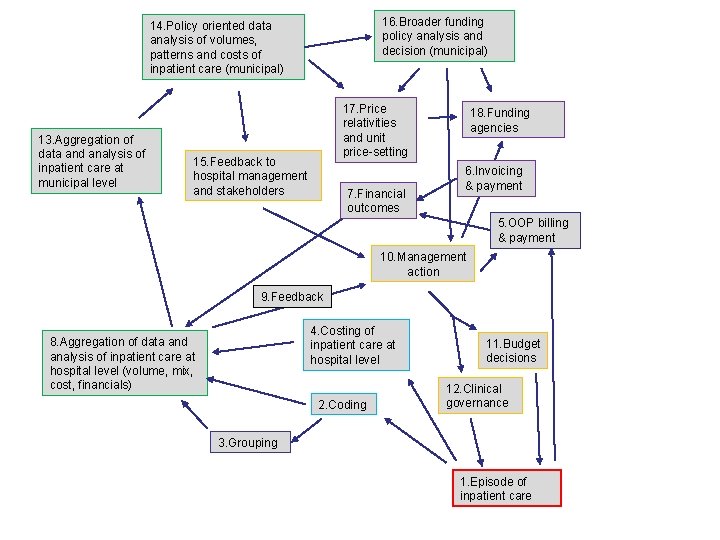
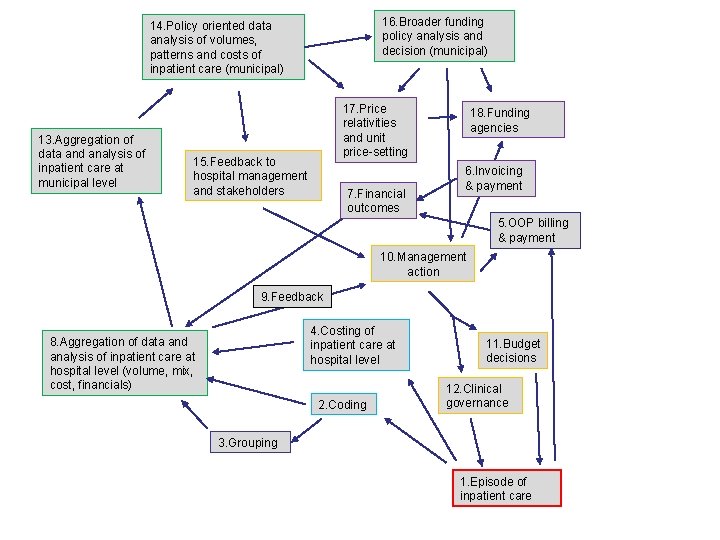
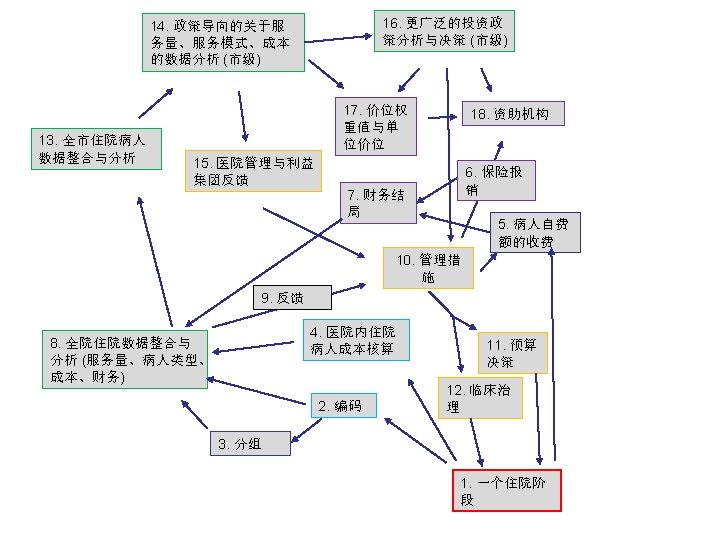
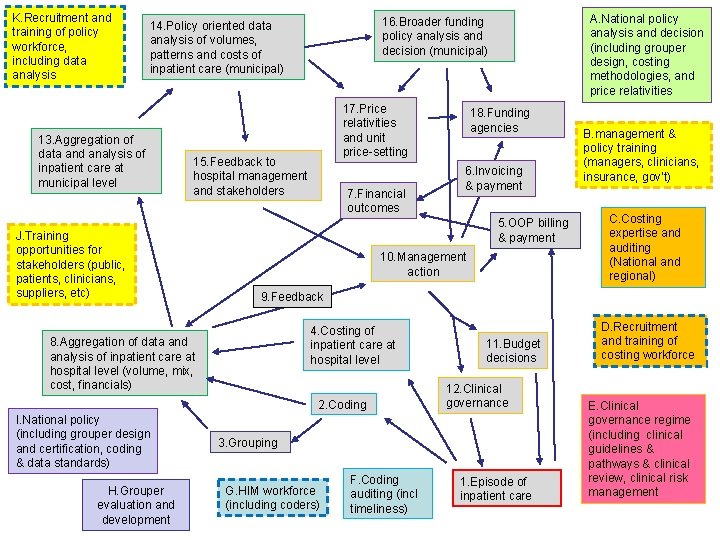
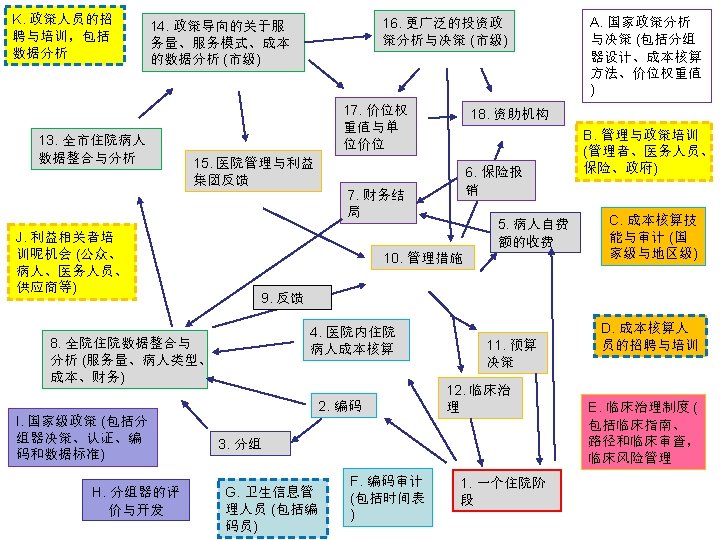
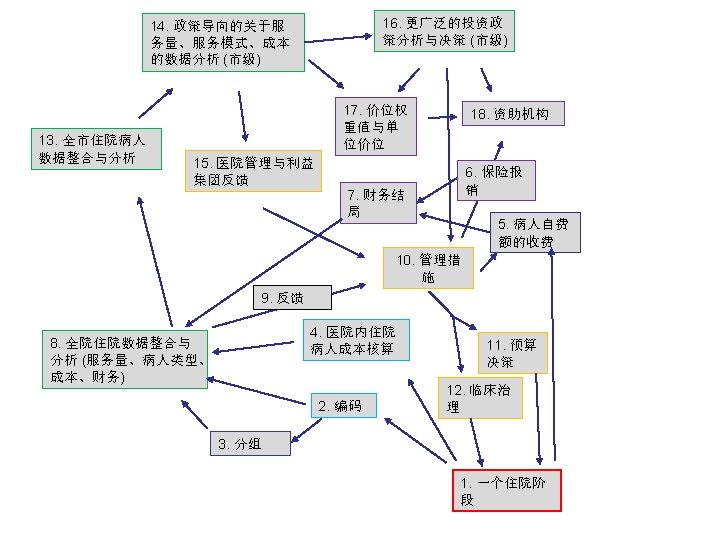
16. Broader funding policy analysis and decision (municipal) 14. Policy oriented data analysis of volumes, patterns and costs of inpatient care (municipal) 13. Aggregation of data and analysis of inpatient care at municipal level 17. Price relativities and unit price-setting 15. Feedback to hospital management and stakeholders 7. Financial outcomes 18. Funding agencies 6. Invoicing & payment 5. OOP billing & payment 10. Management action 9. Feedback 4. Costing of inpatient care at hospital level 8. Aggregation of data and analysis of inpatient care at hospital level (volume, mix, cost, financials) 2. Coding 11. Budget decisions 12. Clinical governance 3. Grouping 1. Episode of inpatient care
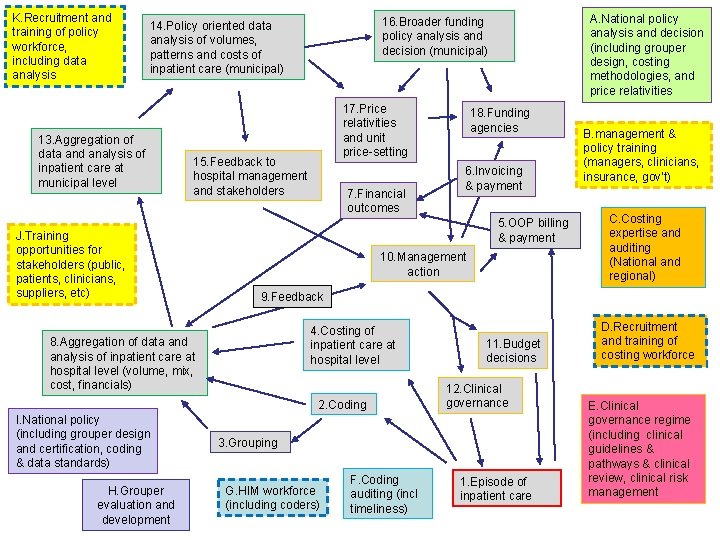
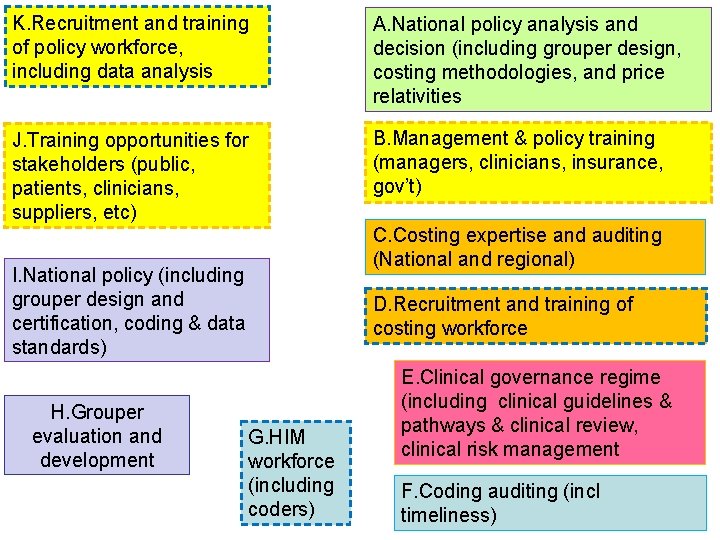
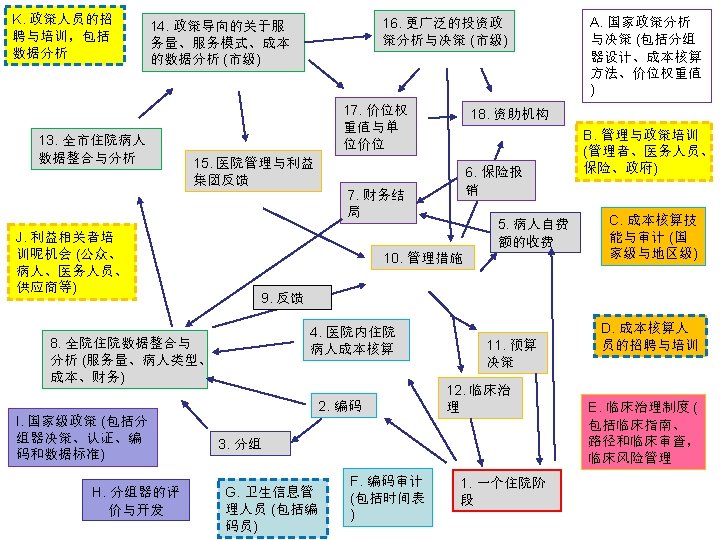
K. Recruitment and training of policy workforce, including data analysis 13. Aggregation of data and analysis of inpatient care at municipal level 17. Price relativities and unit price-setting 15. Feedback to hospital management and stakeholders J. Training opportunities for stakeholders (public, patients, clinicians, suppliers, etc) 7. Financial outcomes 6. Invoicing & payment 10. Management action B. management & policy training (managers, clinicians, insurance, gov’t) C. Costing expertise and auditing (National and regional) 9. Feedback 4. Costing of inpatient care at hospital level 2. Coding H. Grouper evaluation and development 18. Funding agencies 5. OOP billing & payment 8. Aggregation of data and analysis of inpatient care at hospital level (volume, mix, cost, financials) I. National policy (including grouper design and certification, coding & data standards) A. National policy analysis and decision (including grouper design, costing methodologies, and price relativities 16. Broader funding policy analysis and decision (municipal) 14. Policy oriented data analysis of volumes, patterns and costs of inpatient care (municipal) 11. Budget decisions 12. Clinical governance 3. Grouping G. HIM workforce (including coders) F. Coding auditing (incl timeliness) 1. Episode of inpatient care D. Recruitment and training of costing workforce E. Clinical governance regime (including clinical guidelines & pathways & clinical review, clinical risk management
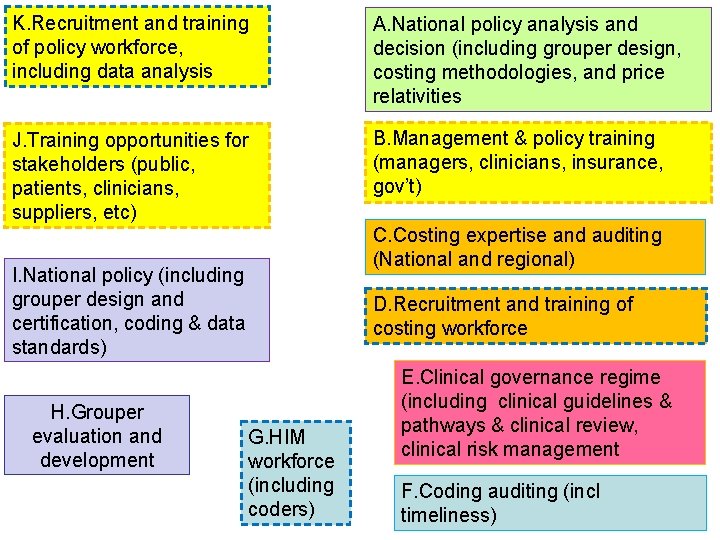
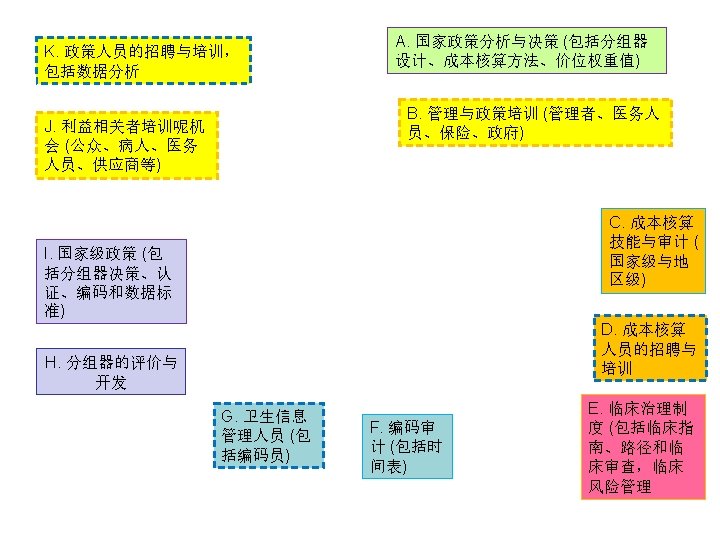
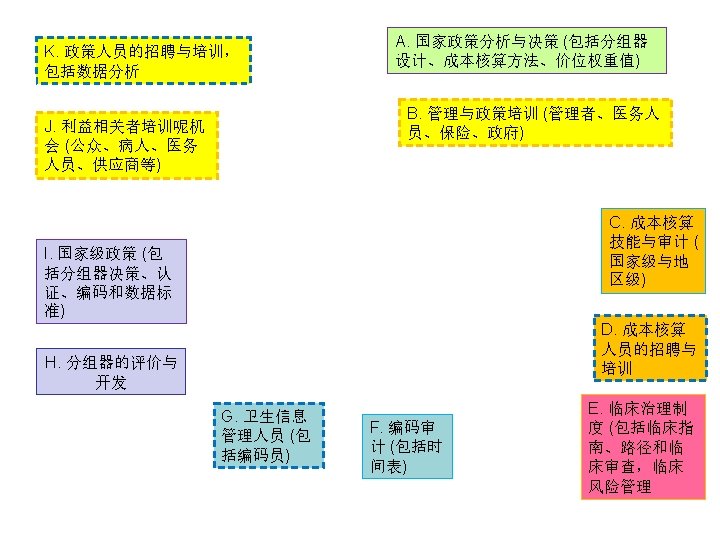
K. Recruitment and training of policy workforce, including data analysis A. National policy analysis and decision (including grouper design, costing methodologies, and price relativities J. Training opportunities for stakeholders (public, patients, clinicians, suppliers, etc) B. Management & policy training (managers, clinicians, insurance, gov’t) I. National policy (including grouper design and certification, coding & data standards) H. Grouper evaluation and development G. HIM workforce (including coders) C. Costing expertise and auditing (National and regional) D. Recruitment and training of costing workforce E. Clinical governance regime (including clinical guidelines & pathways & clinical review, clinical risk management F. Coding auditing (incl timeliness)
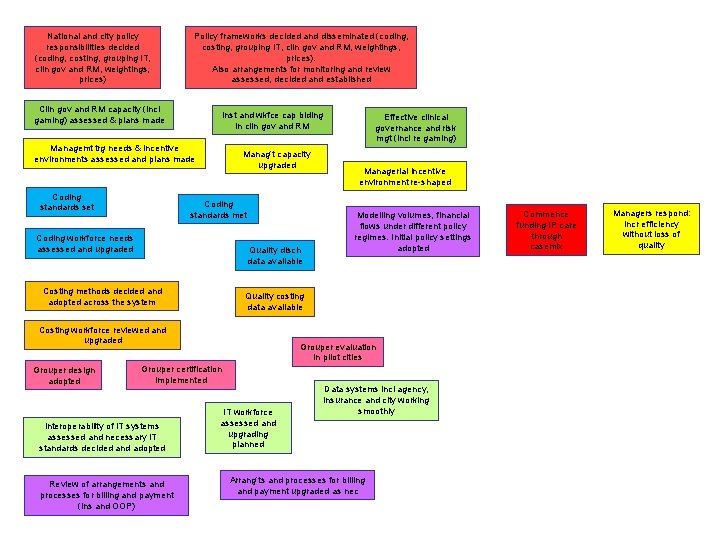
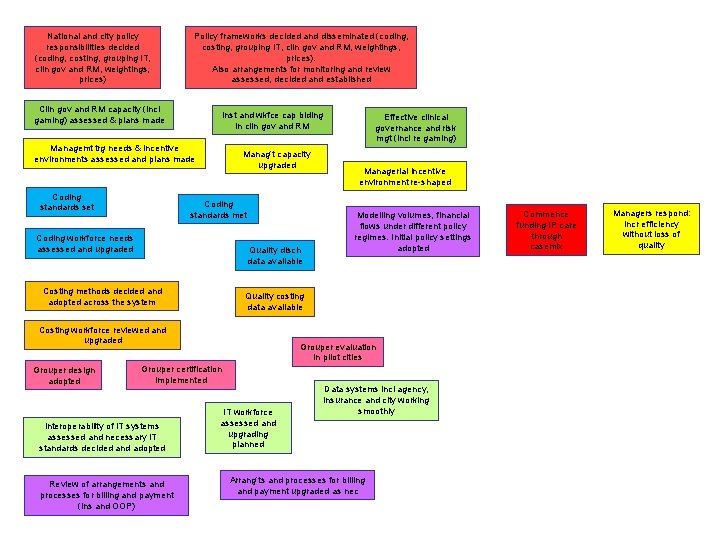
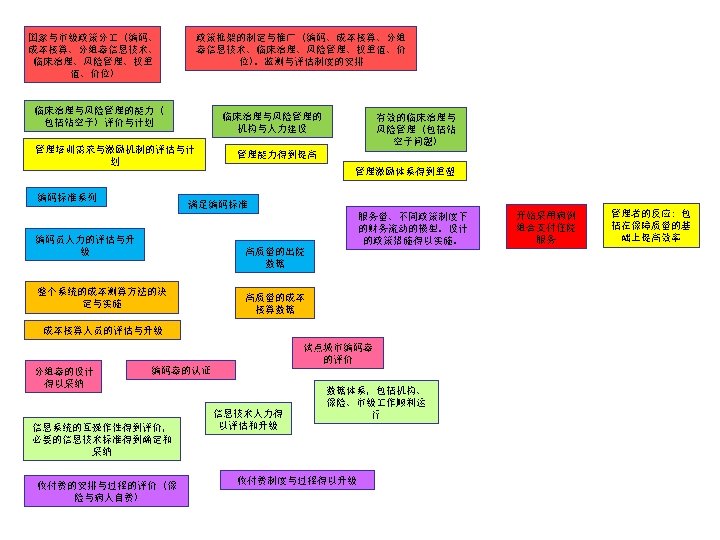
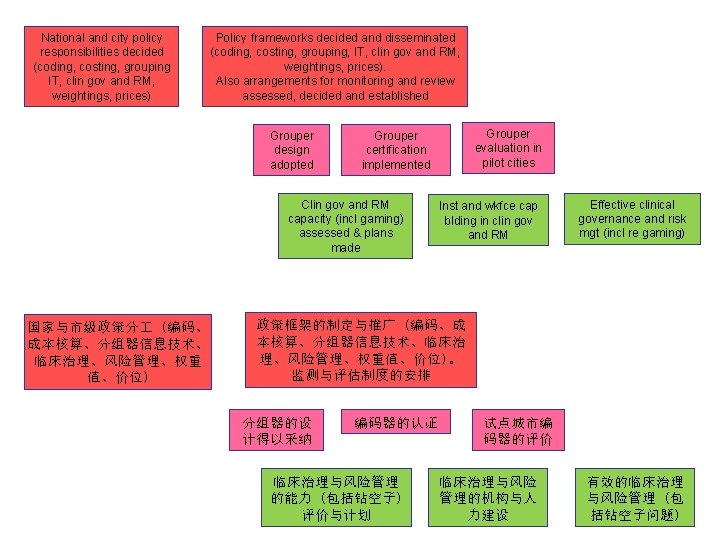
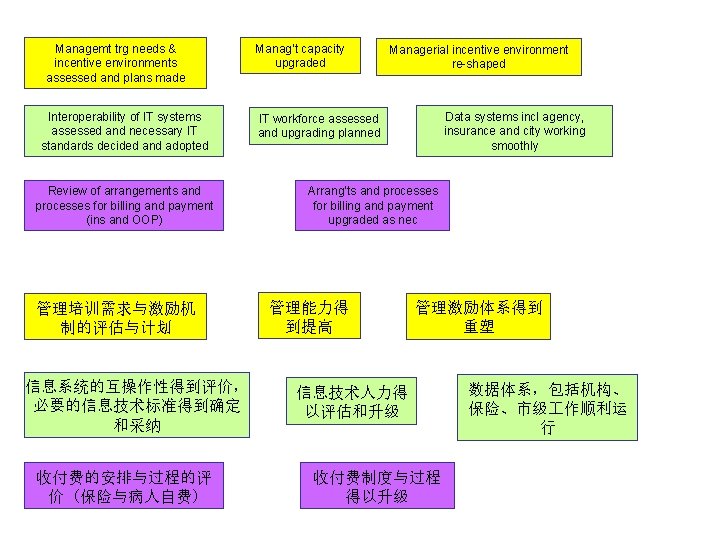
National and city policy responsibilities decided (coding, costing, grouping IT, clin gov and RM, weightings, prices) Policy frameworks decided and disseminated (coding, costing, grouping IT, clin gov and RM, weightings, prices). Also arrangements for monitoring and review assessed, decided and established Clin gov and RM capacity (incl gaming) assessed & plans made Inst and wkfce cap blding in clin gov and RM Managemt trg needs & incentive environments assessed and plans made Coding standards set Manag’t capacity upgraded Coding standards met Coding workforce needs assessed and upgraded Quality disch data available Costing methods decided and adopted across the system Review of arrangements and processes for billing and payment (ins and OOP) Modelling volumes, financial flows under different policy regimes. Initial policy settings adopted Grouper evaluation in pilot cities Grouper certification implemented Interoperability of IT systems assessed and necessary IT standards decided and adopted Managerial incentive environment re-shaped Quality costing data available Costing workforce reviewed and upgraded Grouper design adopted Effective clinical governance and risk mgt (incl re gaming) IT workforce assessed and upgrading planned Data systems incl agency, insurance and city working smoothly Arrang’ts and processes for billing and payment upgraded as nec Commence funding IP care through casemix Managers respond: incr efficiency without loss of quality
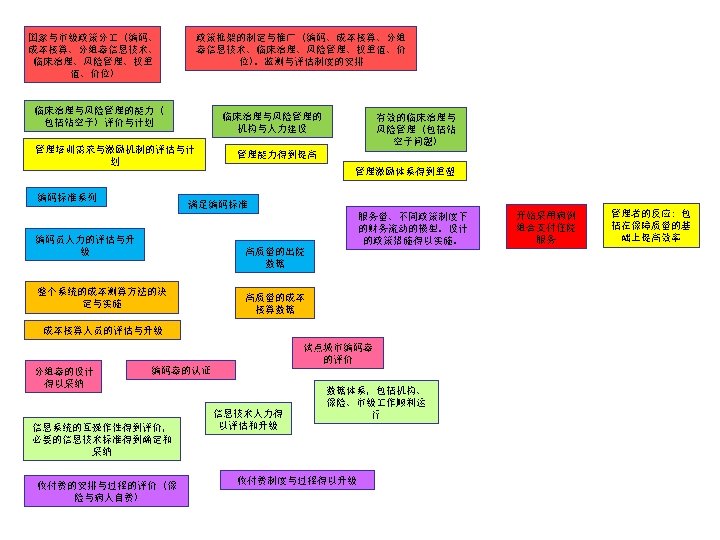
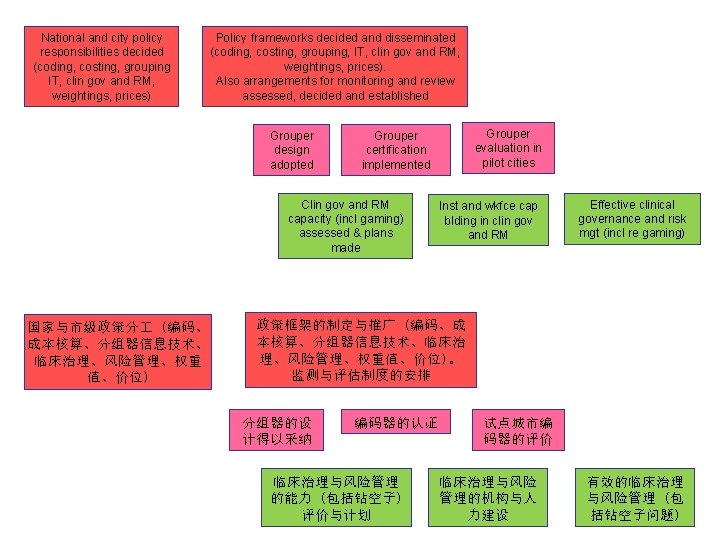
National and city policy responsibilities decided (coding, costing, grouping IT, clin gov and RM, weightings, prices) Policy frameworks decided and disseminated (coding, costing, grouping, IT, clin gov and RM, weightings, prices). Also arrangements for monitoring and review assessed, decided and established Grouper design adopted Clin gov and RM capacity (incl gaming) assessed & plans made 国家与市级政策分 (编码、 成本核算、分组器信息技术、 临床治理、风险管理、权重 值、价位) Grouper evaluation in pilot cities Grouper certification implemented Inst and wkfce cap blding in clin gov and RM Effective clinical governance and risk mgt (incl re gaming) 政策框架的制定与推广 (编码、成 本核算、分组器信息技术、临床治 理、风险管理、权重值、价位)。 监测与评估制度的安排 分组器的设 计得以采纳 编码器的认证 临床治理与风险管理 的能力 (包括钻空子) 评价与计划 试点城市编 码器的评价 临床治理与风险 管理的机构与人 力建设 有效的临床治理 与风险管理 (包 括钻空子问题)
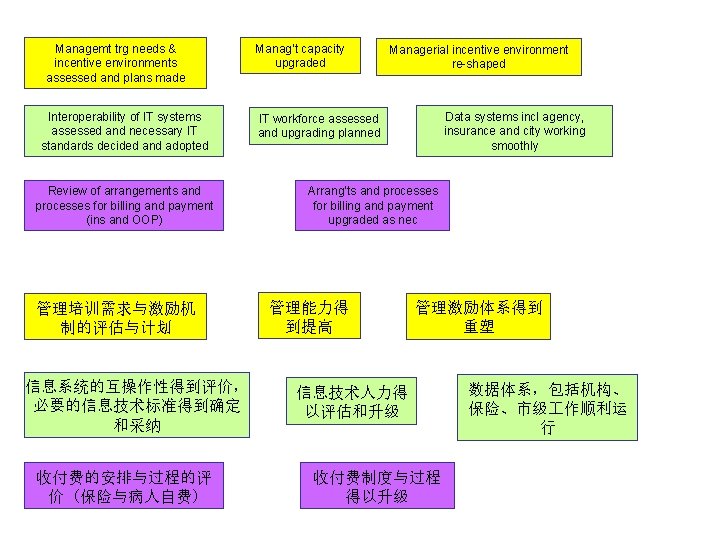
Managemt trg needs & incentive environments assessed and plans made Interoperability of IT systems assessed and necessary IT standards decided and adopted Review of arrangements and processes for billing and payment (ins and OOP) 管理培训需求与激励机 制的评估与计划 信息系统的互操作性得到评价, 必要的信息技术标准得到确定 和采纳 收付费的安排与过程的评 价 (保险与病人自费) Manag’t capacity upgraded Managerial incentive environment re-shaped Data systems incl agency, insurance and city working smoothly IT workforce assessed and upgrading planned Arrang’ts and processes for billing and payment upgraded as nec 管理能力得 到提高 管理激励体系得到 重塑 信息技术人力得 以评估和升级 收付费制度与过程 得以升级 数据体系,包括机构、 保险、市级 作顺利运 行
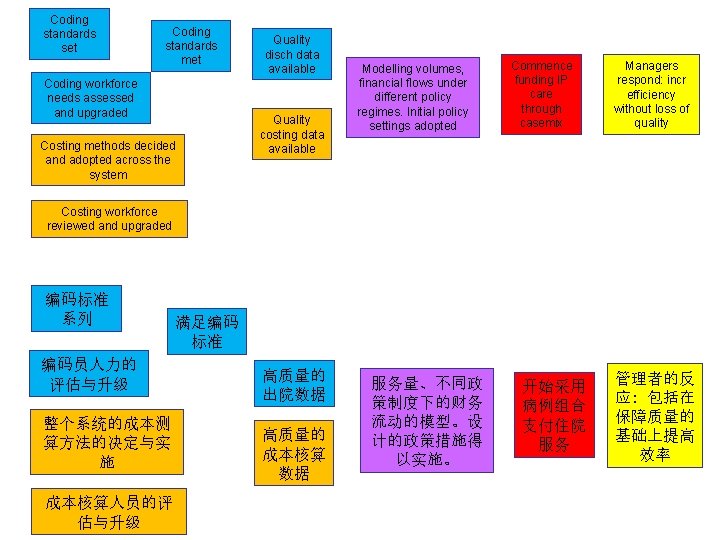
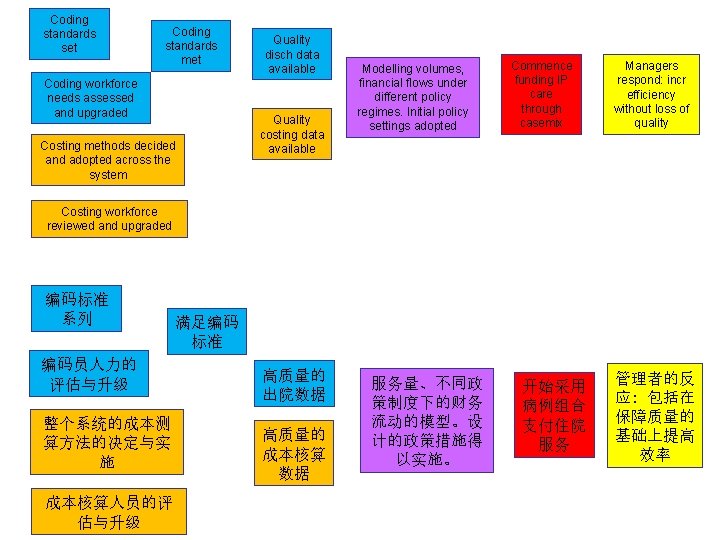
Coding standards set Coding standards met Coding workforce needs assessed and upgraded Costing methods decided and adopted across the system Quality disch data available Quality costing data available Modelling volumes, financial flows under different policy regimes. Initial policy settings adopted Commence funding IP care through casemix Managers respond: incr efficiency without loss of quality Costing workforce reviewed and upgraded 编码标准 系列 编码员人力的 评估与升级 整个系统的成本测 算方法的决定与实 施 成本核算人员的评 估与升级 满足编码 标准 高质量的 出院数据 高质量的 成本核算 数据 服务量、不同政 策制度下的财务 流动的模型。设 计的政策措施得 以实施。 开始采用 病例组合 支付住院 服务 管理者的反 应: 包括在 保障质量的 基础上提高 效率
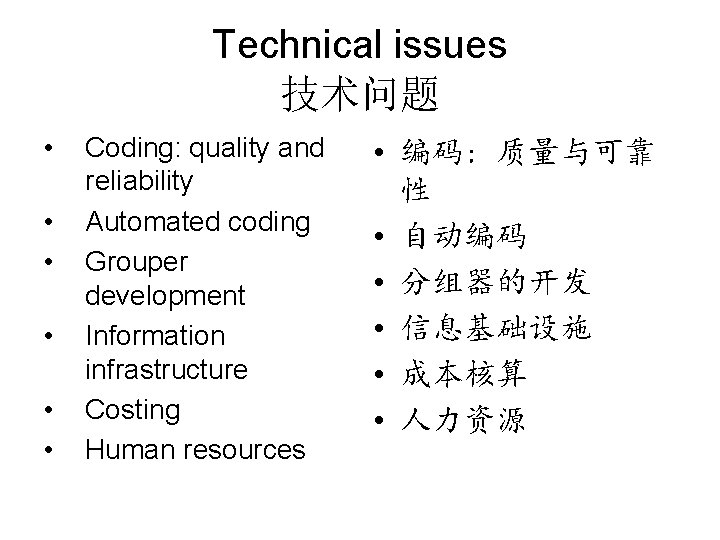
Technical issues 技术问题 • • • Coding: quality and reliability Automated coding Grouper development Information infrastructure Costing Human resources • 编码: 质量与可靠 性 • 自动编码 • 分组器的开发 • 信息基础设施 • 成本核算 • 人力资源
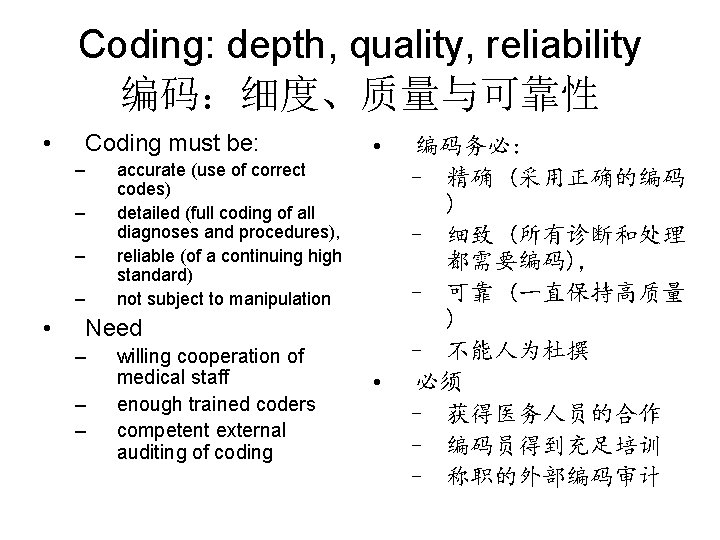
Coding: depth, quality, reliability 编码:细度、质量与可靠性 • Coding must be: – accurate (use of correct codes) detailed (full coding of all diagnoses and procedures), reliable (of a continuing high standard) not subject to manipulation – – – • Need – – – willing cooperation of medical staff enough trained coders competent external auditing of coding • 编码务必: – 精确 (采用正确的编码 ) – 细致 (所有诊断和处理 都需要编码), – 可靠 (一直保持高质量 ) – 不能人为杜撰 • 必须 – 获得医务人员的合作 – 编码员得到充足培训 – 称职的外部编码审计
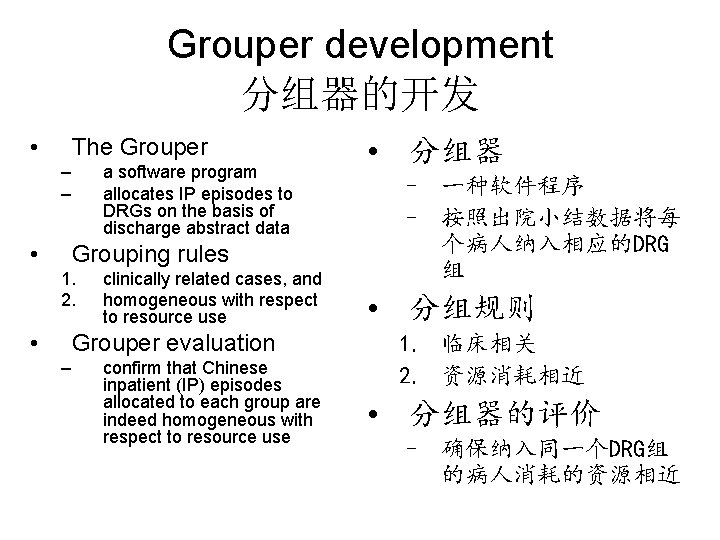
Grouper development 分组器的开发 • The Grouper – – • a software program allocates IP episodes to DRGs on the basis of discharge abstract data Grouping rules 1. 2. • clinically related cases, and homogeneous with respect to resource use Grouper evaluation – confirm that Chinese inpatient (IP) episodes allocated to each group are indeed homogeneous with respect to resource use • 分组器 – 一种软件程序 – 按照出院小结数据将每 个病人纳入相应的DRG 组 • 分组规则 1. 临床相关 2. 资源消耗相近 • 分组器的评价 – 确保纳入同一个DRG组 的病人消耗的资源相近
Information infrastructure 信息基础设施 • Communicating large volumes of data between different sites – – • • hospitals funders data analysts policy makers Standards development Information systems at the agency and regional levels – – technicians analysts • 不同场所的大量数据 交流 – – 医院 付费者 数据分析师 政策开发者 • 标准的开发 • 机构内部和区域范围 的信息系统 – 技术人员 – 分析师
Costing 成本核算 • Accurate current costing • data needed – – • ongoing review and adjustment of the grouper inform managers of their own costs relative to revenues capacity for ongoing collection and analysis of costs – – workforce implications monitoring and improvement of costing systems 需要精确的成本核算 数据 – 不断评估调整分组器 – 向管理者提供自家成 本与收入的相对数值 • 连续采集分析成本数 据的能力 – 人力需要 – 成本核算系统的监测 与改进
Management training 管理培训 • Exploring different ways of doing things – reducing reliance on volume bonus – more efficient triage – improved admissions processes – alternative queuing strategies – reduced down time – etc • Improving unit cost efficiency while controlling volume and protecting quality requires high level management skill • 探索不同的做事方式 – 减弱对量效奖金的依赖 – 更高效的分诊 – 改进入院过程 – 不同的排队等候制度 – 减少停业时间 – 其它 • 改进单位成本效率,同时 控制服务量,并保证服务 质量。这离不开高水平的 管理技能
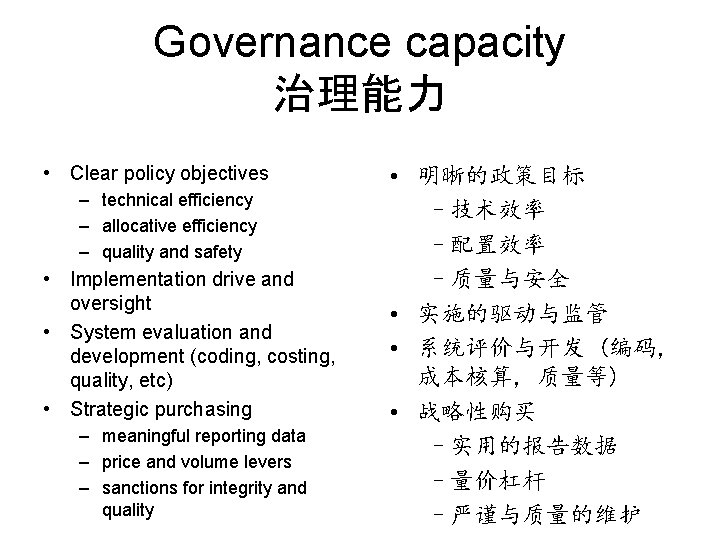
Governance capacity 治理能力 • Clear policy objectives – technical efficiency – allocative efficiency – quality and safety • Implementation drive and oversight • System evaluation and development (coding, costing, quality, etc) • Strategic purchasing – meaningful reporting data – price and volume levers – sanctions for integrity and quality • 明晰的政策目标 –技术效率 –配置效率 –质量与安全 • 实施的驱动与监管 • 系统评价与开发 (编码, 成本核算, 质量等) • 战略性购买 –实用的报告数据 –量价杠杆 –严谨与质量的维护

Human resources 人力资源 • • • Coders Coding auditors Costing experts Information managers Agency managers Policy officials • • • 编码员 编码审计员 成本核算专家 信息管理者 组织机构管理者 政策官员
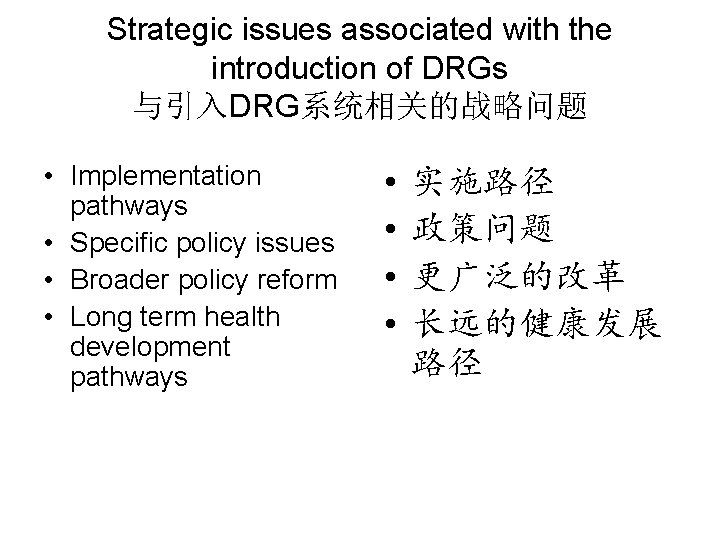
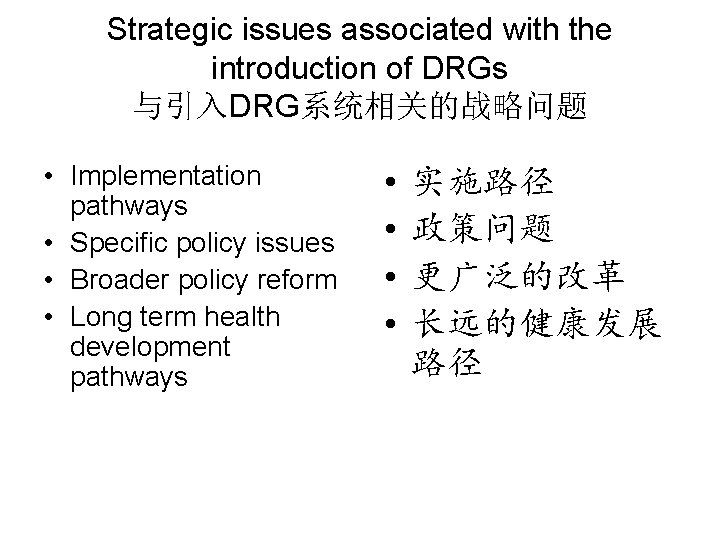
Strategic issues associated with the introduction of DRGs 与引入DRG系统相关的战略问题 • Implementation pathways • Specific policy issues • Broader policy reform • Long term health development pathways • • 实施路径 政策问题 更广泛的改革 长远的健康发展 路径
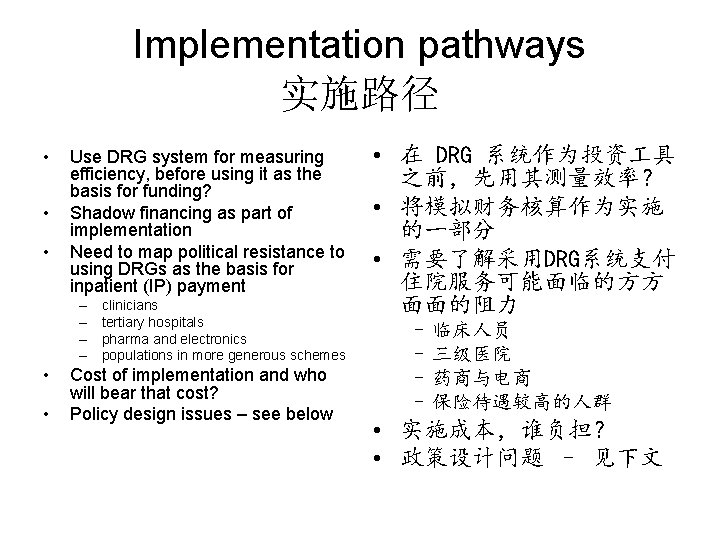
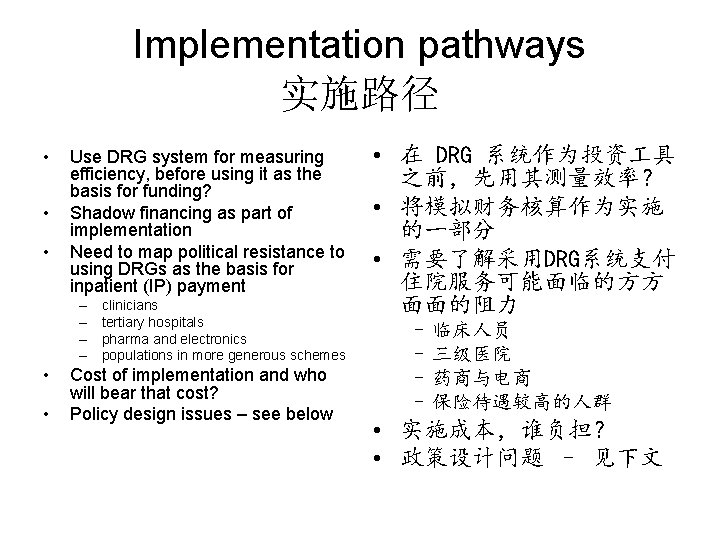
Implementation pathways 实施路径 • • • Use DRG system for measuring efficiency, before using it as the basis for funding? Shadow financing as part of implementation Need to map political resistance to using DRGs as the basis for inpatient (IP) payment – – • • clinicians tertiary hospitals pharma and electronics populations in more generous schemes Cost of implementation and who will bear that cost? Policy design issues – see below • 在 DRG 系统作为投资 具 之前,先用其测量效率? • 将模拟财务核算作为实施 的一部分 • 需要了解采用DRG系统支付 住院服务可能面临的方方 面面的阻力 – 临床人员 – 三级医院 – 药商与电商 – 保险待遇较高的人群 • 实施成本,谁负担? • 政策设计问题 – 见下文
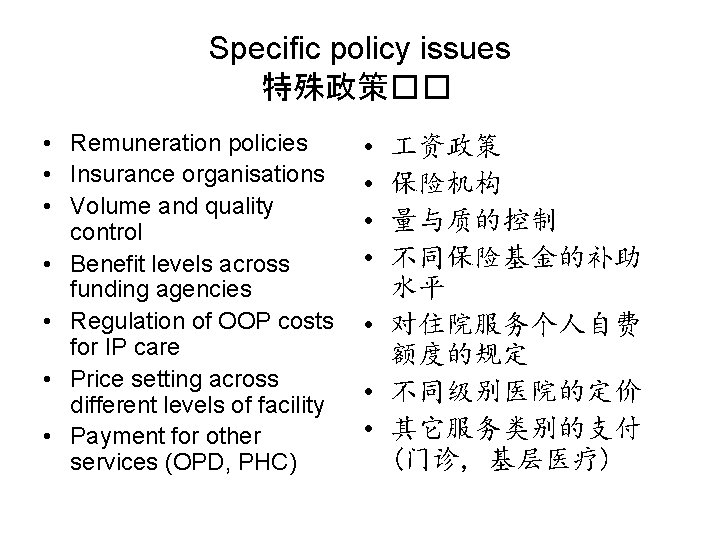
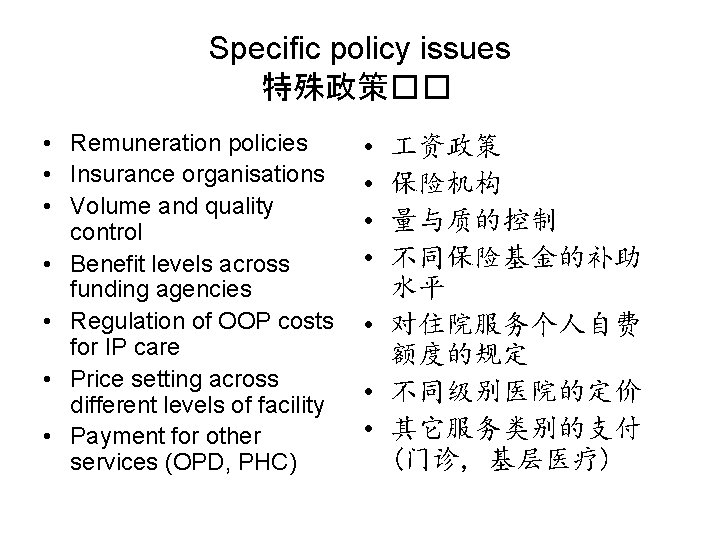
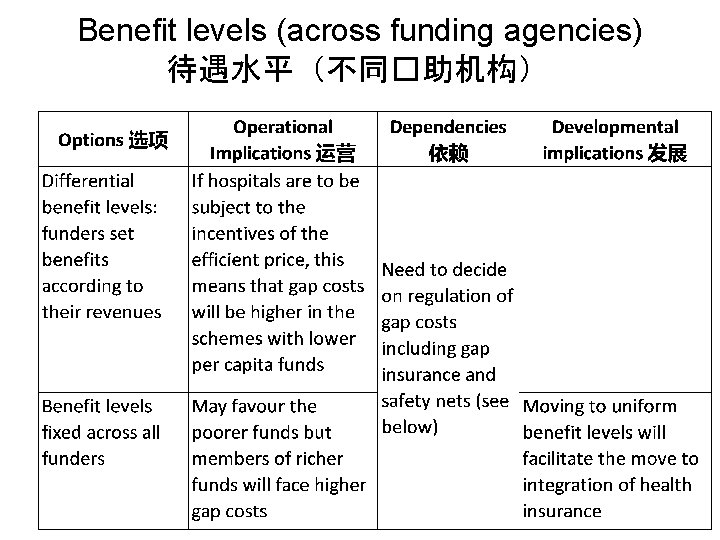
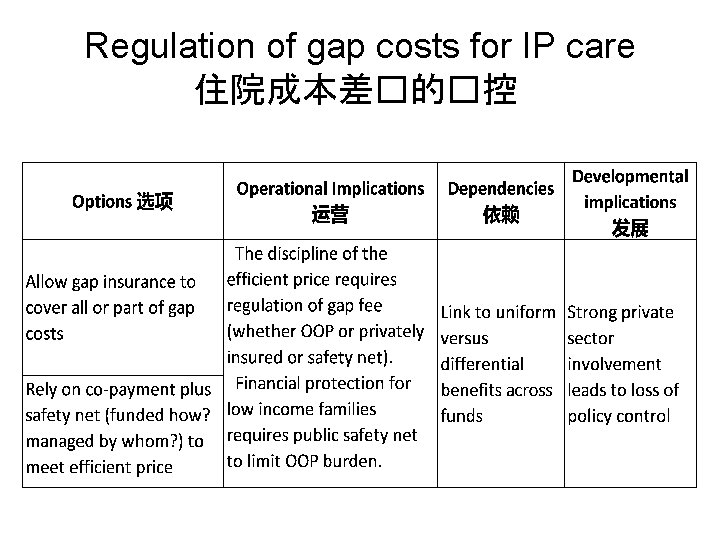
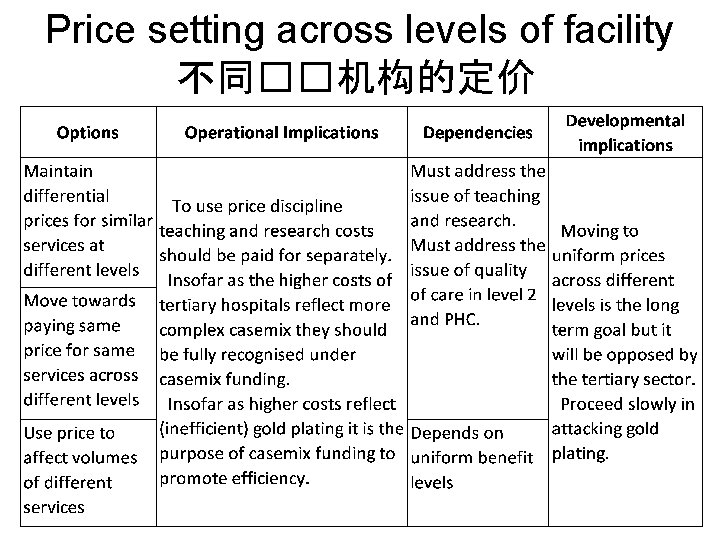
Specific policy issues 特殊政策�� • Remuneration policies • Insurance organisations • Volume and quality control • Benefit levels across funding agencies • Regulation of OOP costs for IP care • Price setting across different levels of facility • Payment for other services (OPD, PHC) • • 资政策 保险机构 量与质的控制 不同保险基金的补助 水平 • 对住院服务个人自费 额度的规定 • 不同级别医院的定价 • 其它服务类别的支付 (门诊, 基层医疗)
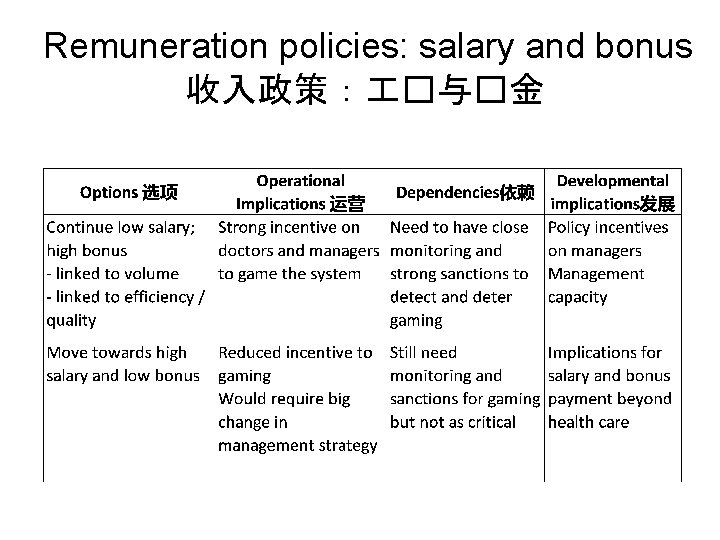
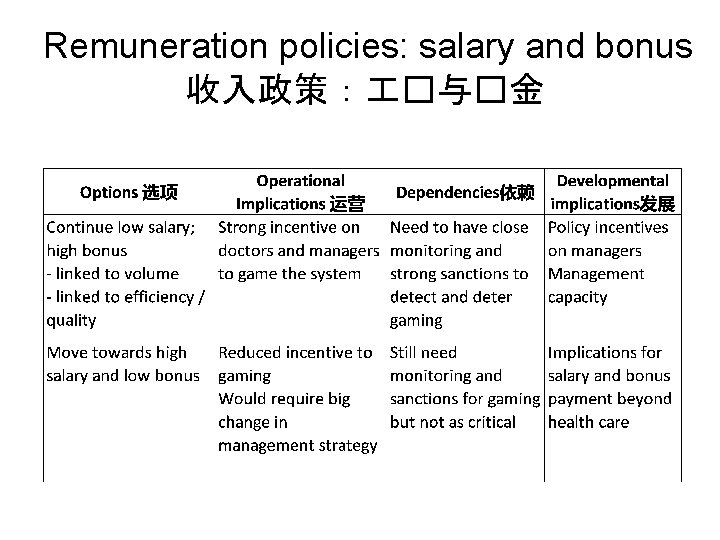
Remuneration policies: salary and bonus 收入政策: �与�金
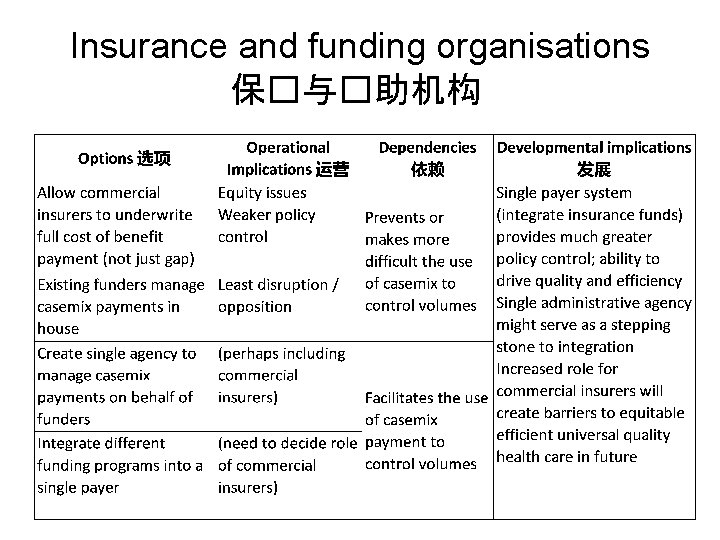
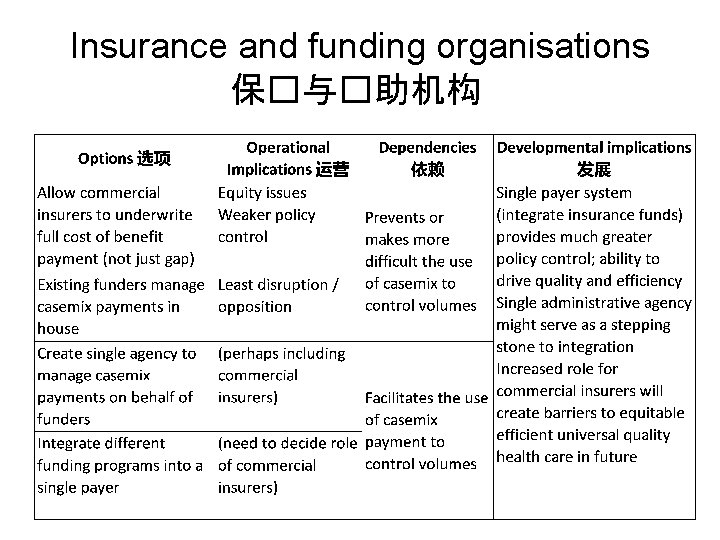
Insurance and funding organisations 保�与�助机构
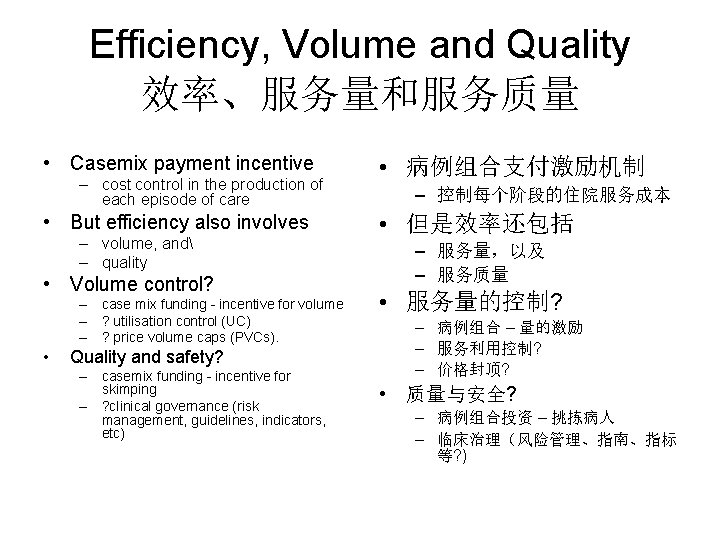
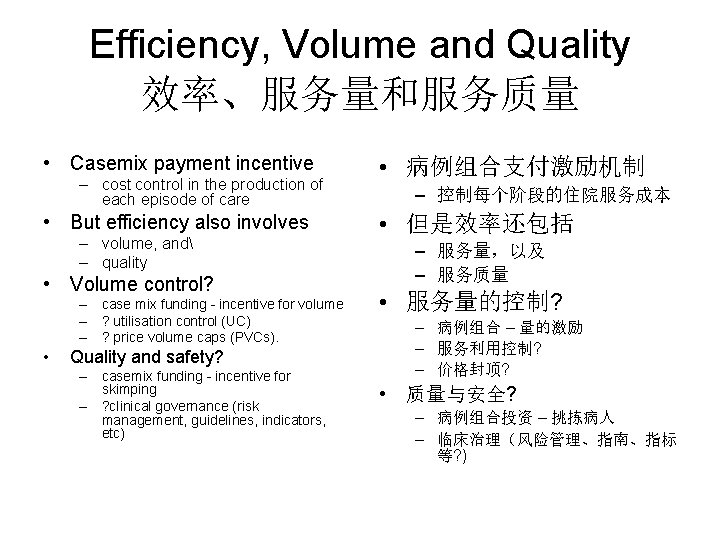
Efficiency, Volume and Quality 效率、服务量和服务质量 • Casemix payment incentive – cost control in the production of each episode of care • But efficiency also involves – volume, and – quality • Volume control? – case mix funding - incentive for volume – ? utilisation control (UC) – ? price volume caps (PVCs). • Quality and safety? – casemix funding - incentive for skimping – ? clinical governance (risk management, guidelines, indicators, etc) • 病例组合支付激励机制 – 控制每个阶段的住院服务成本 • 但是效率还包括 – 服务量,以及 – 服务质量 • 服务量的控制? – 病例组合 – 量的激励 – 服务利用控制? – 价格封顶? • 质量与安全? – 病例组合投资 – 挑拣病人 – 临床治理(风险管理、指南、指标 等? )
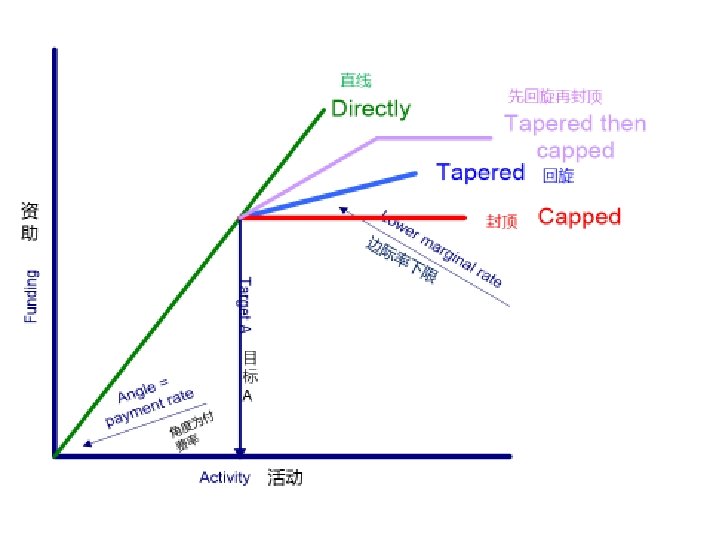
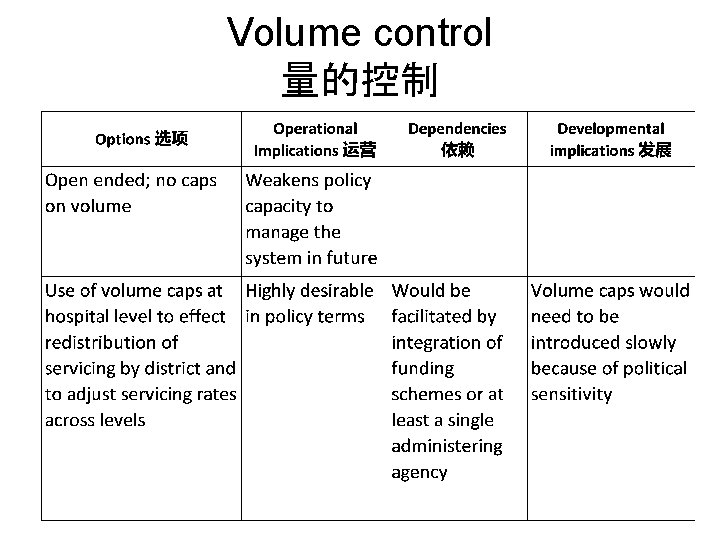
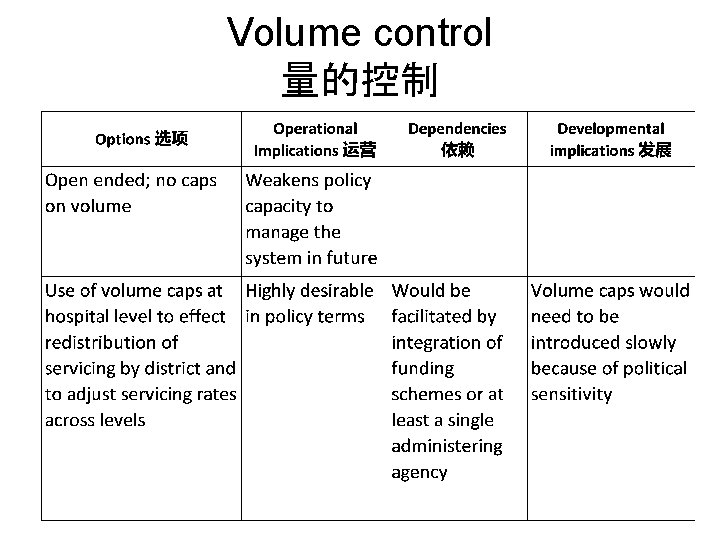
Volume control 量的控制

Quality and safety � 量与安全 • Over-servicing and adverse events • – waste of money – stokes community anger – perceptions distort utilisation patterns • Structure – – • accreditation professional level funding incentives public information Process – clinical guidelines – clinical review – clinical indicators • • • Outcomes – penalties – rewards – measurement • �度服�与不良事件 – 浪��金 – 招惹众怒 – �念会扭曲利用模式 �构 – ���� – ���次 – ��激励 – 公共信息 �程 – �床指南 – �床�估 – �床指� �局 – ��
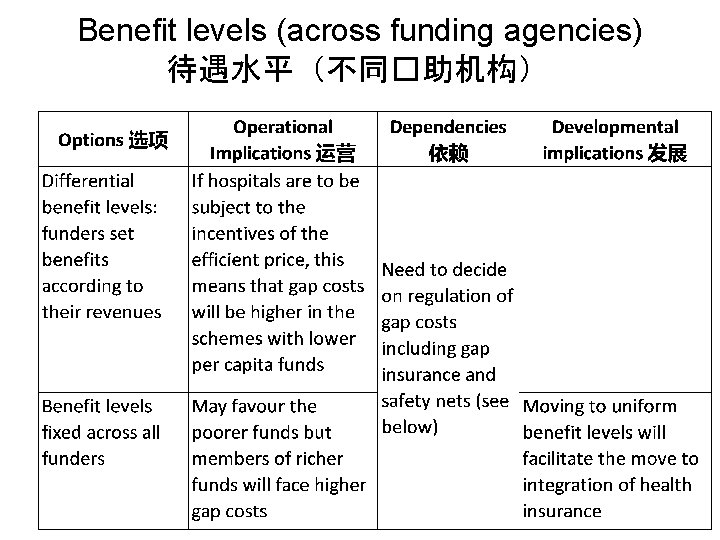
Benefit levels (across funding agencies) 待遇水平(不同�助机构)
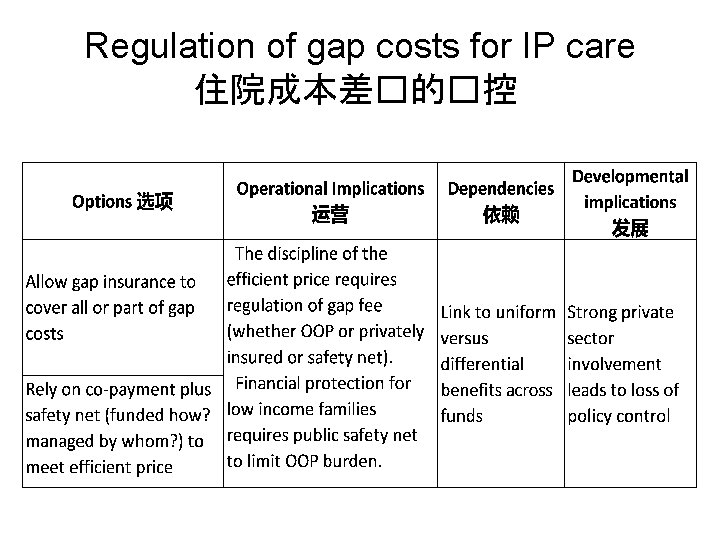
Regulation of gap costs for IP care 住院成本差�的�控
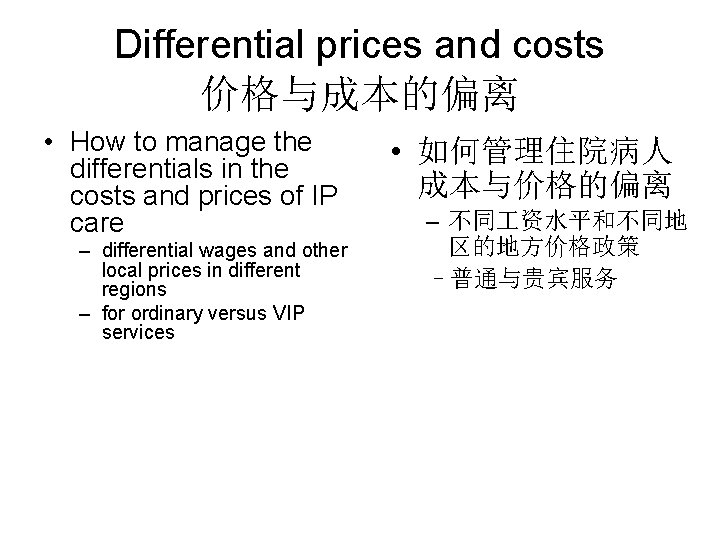
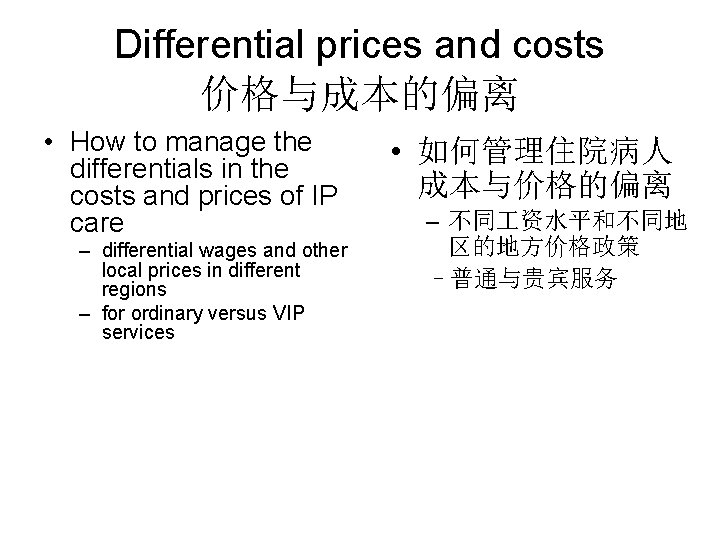
Differential prices and costs 价格与成本的偏离 • How to manage the differentials in the costs and prices of IP care – differential wages and other local prices in different regions – for ordinary versus VIP services • 如何管理住院病人 成本与价格的偏离 – 不同 资水平和不同地 区的地方价格政策 –普通与贵宾服务
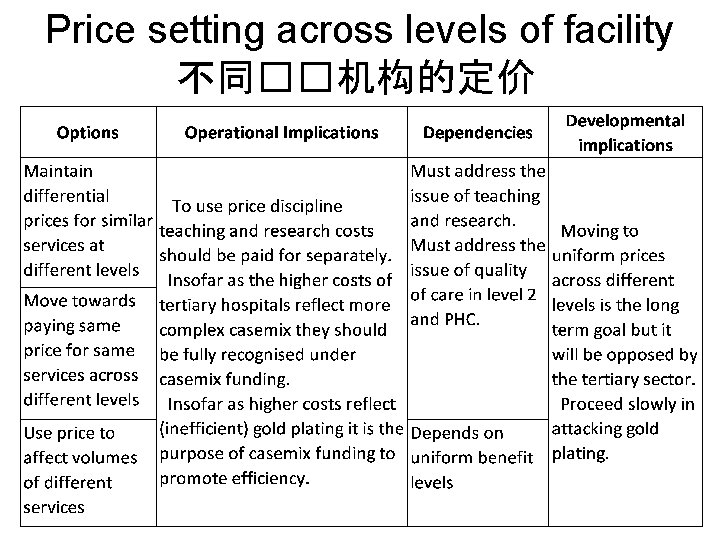
Price setting across levels of facility 不同��机构的定价
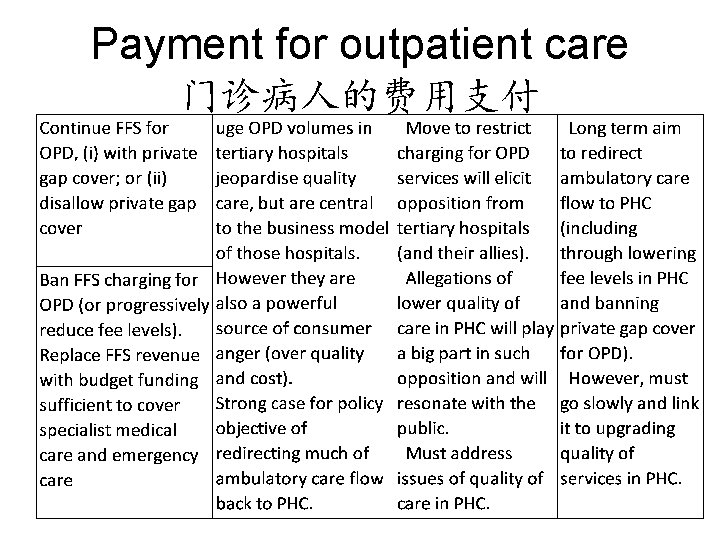
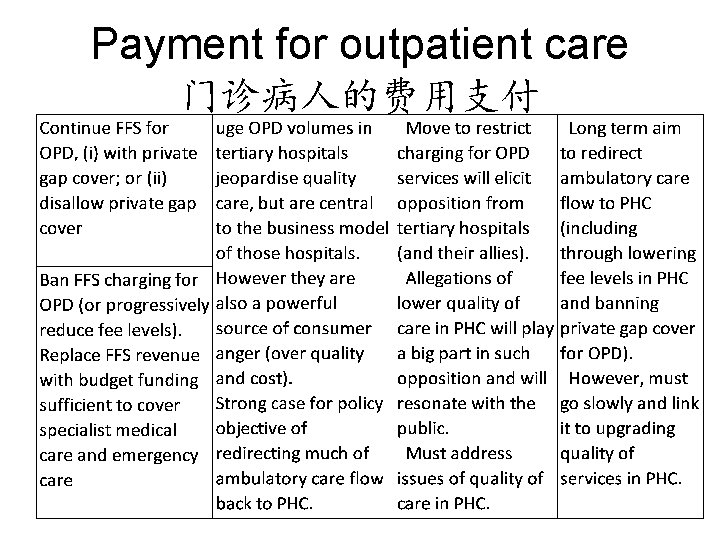
Payment for outpatient care 门诊病人的费用支付
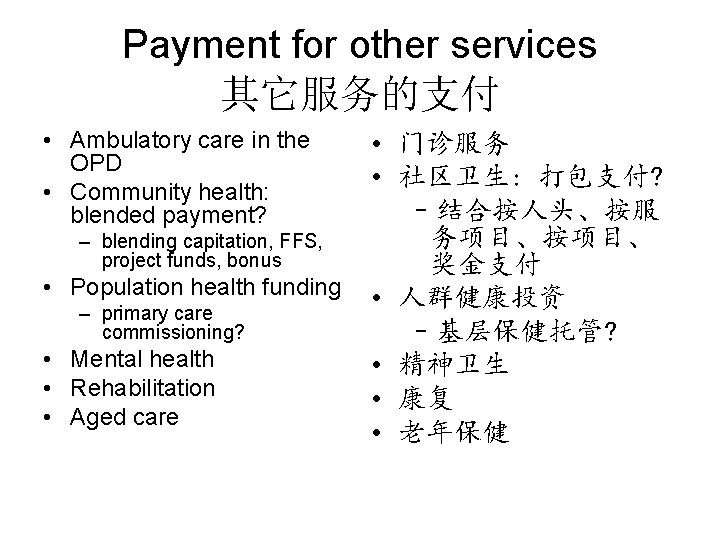
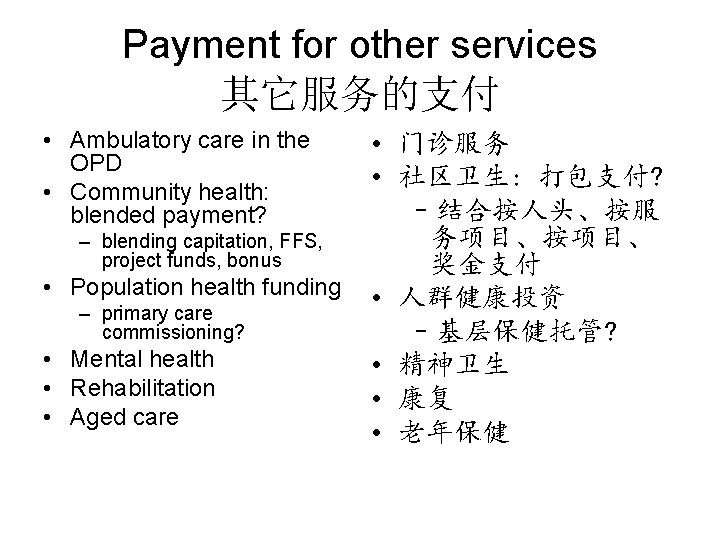
Payment for other services 其它服务的支付 • Ambulatory care in the OPD • Community health: blended payment? • 门诊服务 • 社区卫生: 打包支付? –结合按人头、按服 务项目、按项目、 – blending capitation, FFS, project funds, bonus 奖金支付 • Population health funding • 人群健康投资 – primary care commissioning? –基层保健托管? • Mental health • 精神卫生 • Rehabilitation • 康复 • Aged care • 老年保健
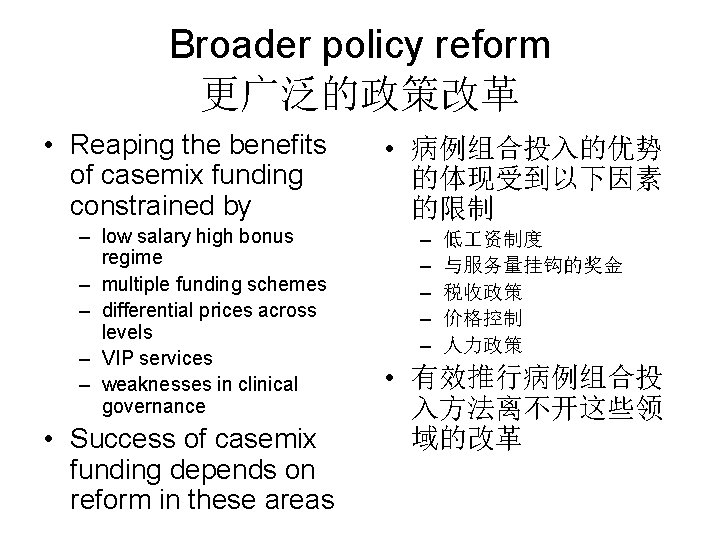
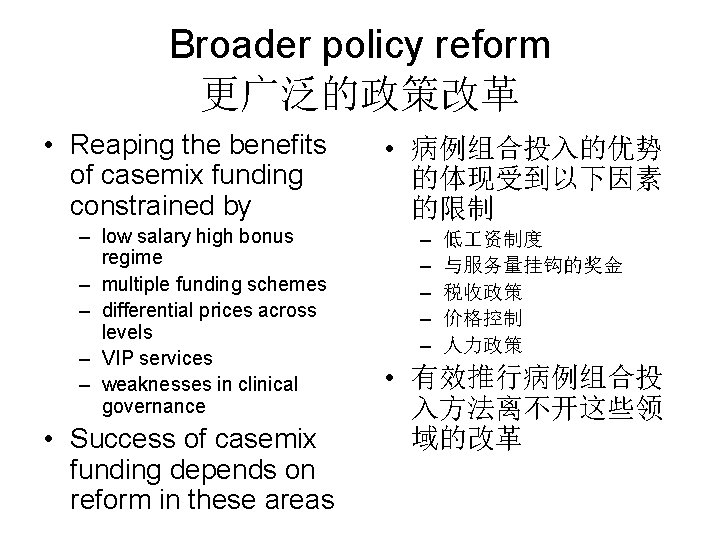
Broader policy reform 更广泛的政策改革 • Reaping the benefits of casemix funding constrained by – low salary high bonus regime – multiple funding schemes – differential prices across levels – VIP services – weaknesses in clinical governance • Success of casemix funding depends on reform in these areas • 病例组合投入的优势 的体现受到以下因素 的限制 – – – 低 资制度 与服务量挂钩的奖金 税收政策 价格控制 人力政策 • 有效推行病例组合投 入方法离不开这些领 域的改革
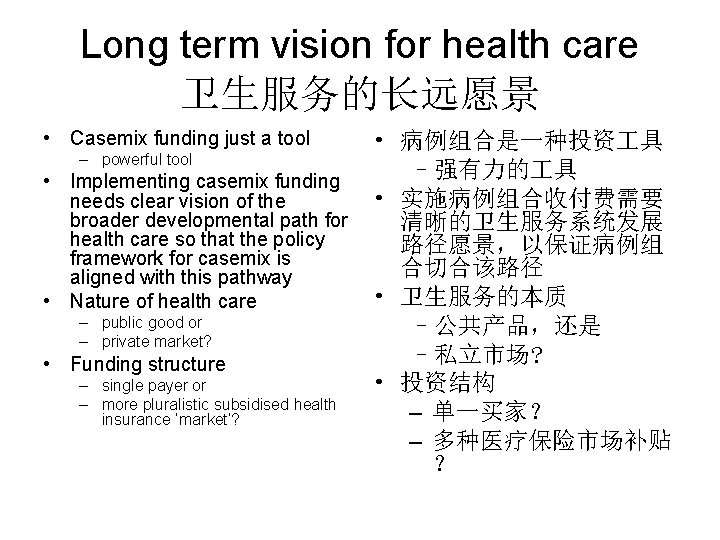
Long term vision for health care 卫生服务的长远愿景 • Casemix funding just a tool • 病例组合是一种投资 具 – powerful tool –强有力的 具 • Implementing casemix funding • 实施病例组合收付费需要 needs clear vision of the broader developmental path for 清晰的卫生服务系统发展 health care so that the policy 路径愿景,以保证病例组 framework for casemix is 合切合该路径 aligned with this pathway • 卫生服务的本质 • Nature of health care – public good or –公共产品,还是 – private market? –私立市场? • Funding structure – single payer or • 投资结构 – more pluralistic subsidised health – 单一买家? insurance ‘market’? – 多种医疗保险市场补贴 ?
Thank you