Implementing an Individualized Discharge Teaching Module at a



- Slides: 43
Implementing an Individualized Discharge Teaching Module at a Critical Access Hospital: An Evidence Based Project leader: Kelly Tiffany, BAN, FNP-s Project advisor: Susan Clouse Smith, DNP, APRN, PNP, FNP-BC Faculty consultant: Jenna Herman, DNP, APRN, FNP-BC
Thank You! The DNP project could not have been completed without the assistance of … Dr. Susan Clouse Smith Dr. Jenna Herman Dr. Billie Madler Jodi Atkinson Karla Spence Jen Laukner Katie Tofteland Alfred Sams Chassidy Sharp
Problem Statement • Poor comprehension of discharge instructions common • Disconnect between patient understanding and comprehension • Disconnect may result in – Medication errors – Misunderstanding – Patient dissatisfaction – Hospital readmissions
Organizational Needs Assessment Resources to help elderly stay in their homes Discharge education lacked: • Diagnosis specific information • Needed documentation • Evaluation of patient comprehension Low readmission rate Room for improved HCAHPS scores
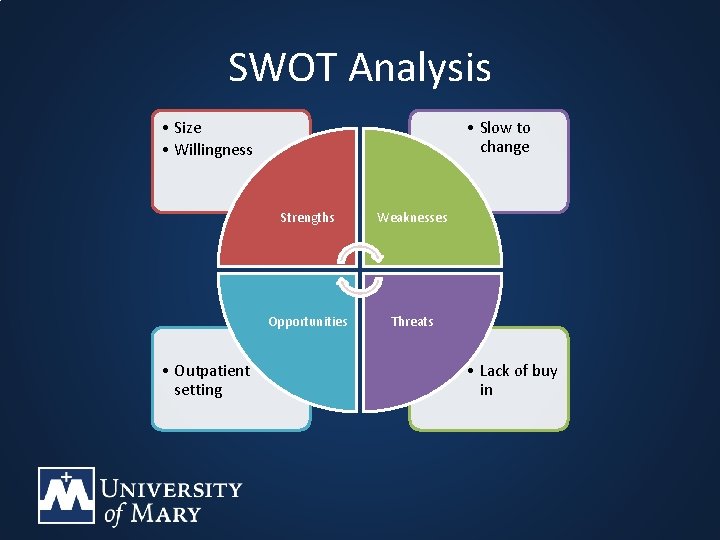
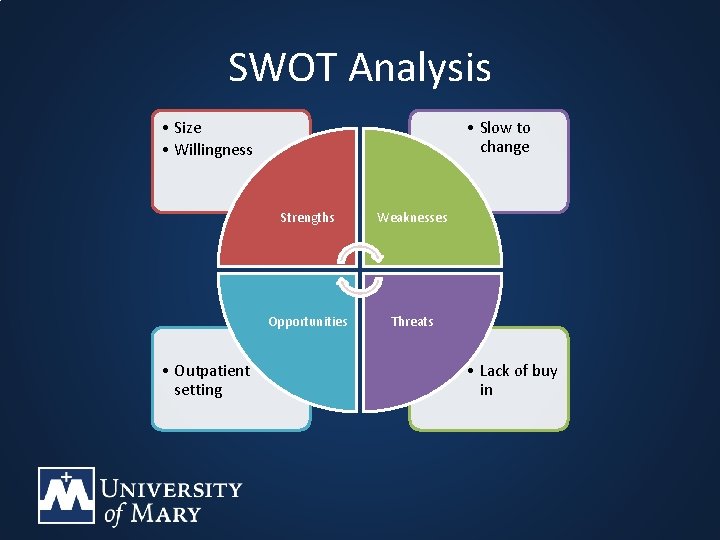
SWOT Analysis • Size • Willingness • Outpatient setting • Slow to change Strengths Weaknesses Opportunities Threats • Lack of buy in
Proposed Solution • DNP project focused on patient discharge education and comprehension • DNP project setting of a CAH • Multiple interventions
PICO “Among adult acute, observational, and skilled swing bed patients in a critical access hospital, how does the implementation of an individualized discharge teaching module, as compared to the organization’s current established discharge teaching module, impact readmission rates and patient satisfaction? ”

Literature Review Transitional Interventions Guidelines Communication Barriers Discharge Planning Discharge Teaching
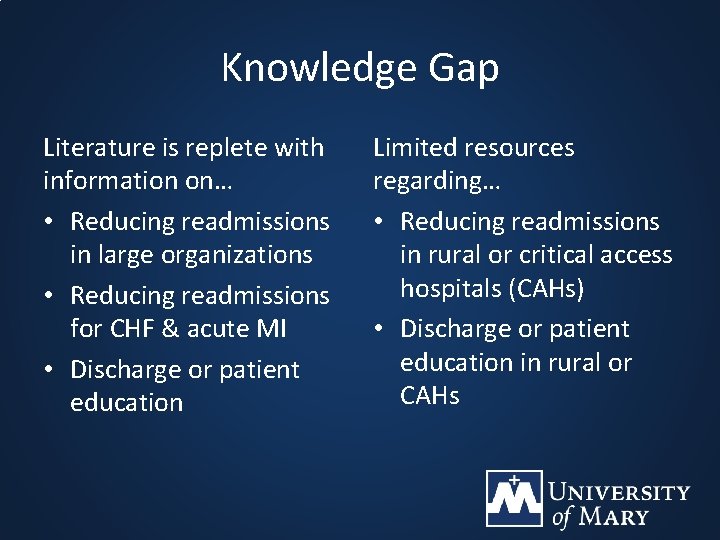
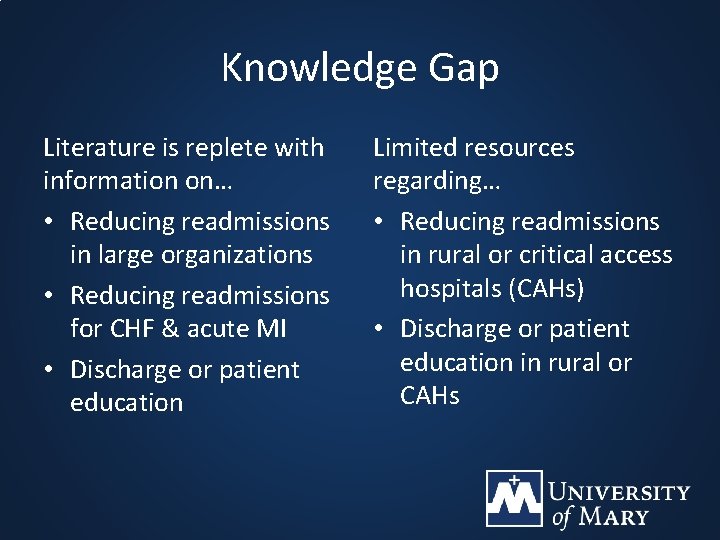
Knowledge Gap Literature is replete with information on… • Reducing readmissions in large organizations • Reducing readmissions for CHF & acute MI • Discharge or patient education Limited resources regarding… • Reducing readmissions in rural or critical access hospitals (CAHs) • Discharge or patient education in rural or CAHs
Theoretical Framework “The Important Elements of Effective Discharge Teaching” (IEEDT) Assessment Individualization Evaluation & Reflection Motivation & Self Efficacy (Mc. Bride & Andrews, 2013)
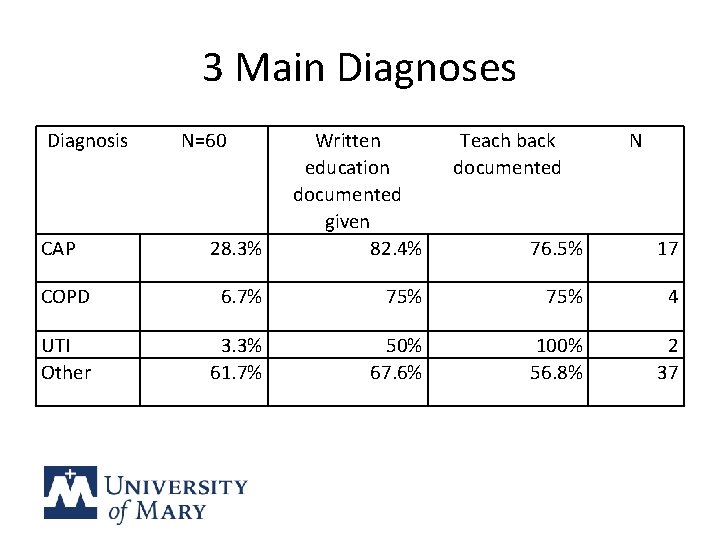
Recommendations By November, 2017 1. Educate on three main diagnoses of admissions: Øpneumonia Øurinary tract infections Øchronic obstructive pulmonary disease 2. Educate on and implement the Ask Me 3 program into the organization
Recommendations By November, 2017 3. Educate and implement the “teach back” method 4. Develop and implement individualized patient centered discharge instruction (PCDI)
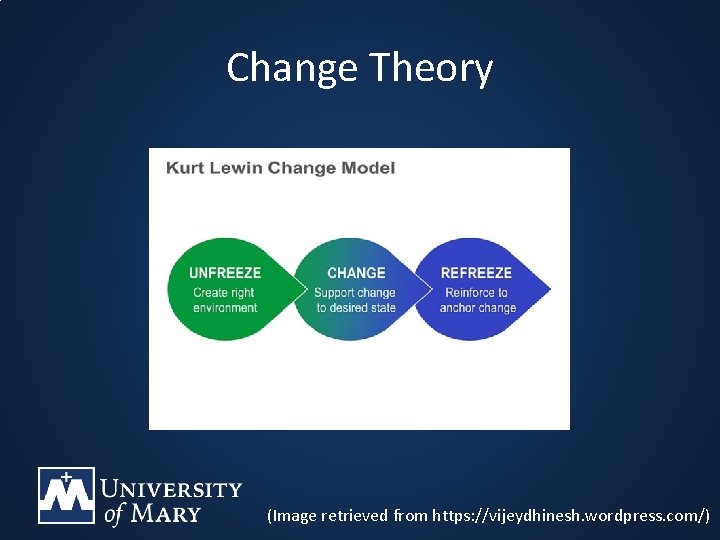
Determinants of Change • • • Motivated team Receptive environment Involvement of physicians or providers Involvement of nursing staff A timeline or plan Image retrieved from https: //vijeydhinesh. wordpress. com/
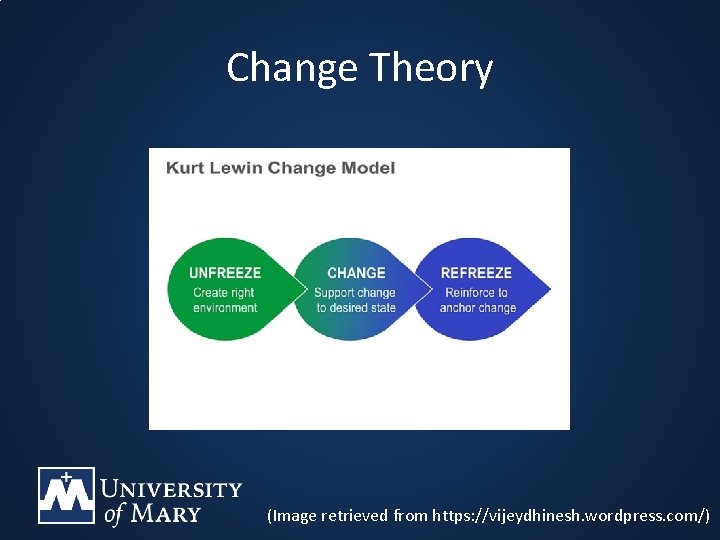
Change Theory (Image retrieved from https: //vijeydhinesh. wordpress. com/)
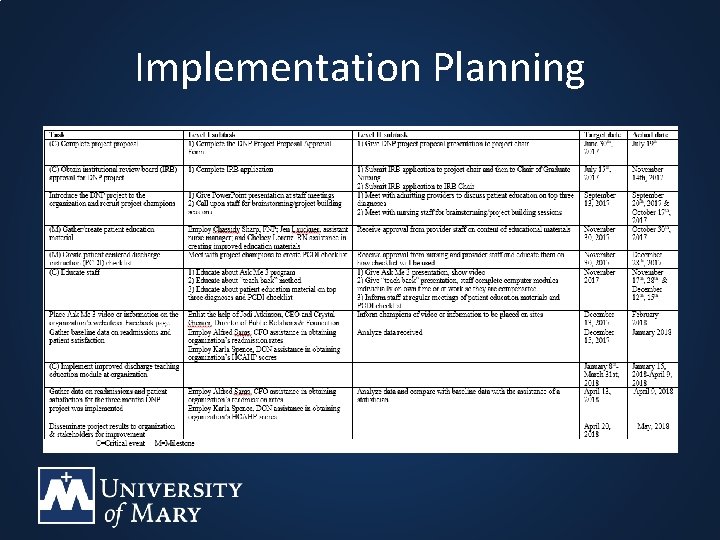
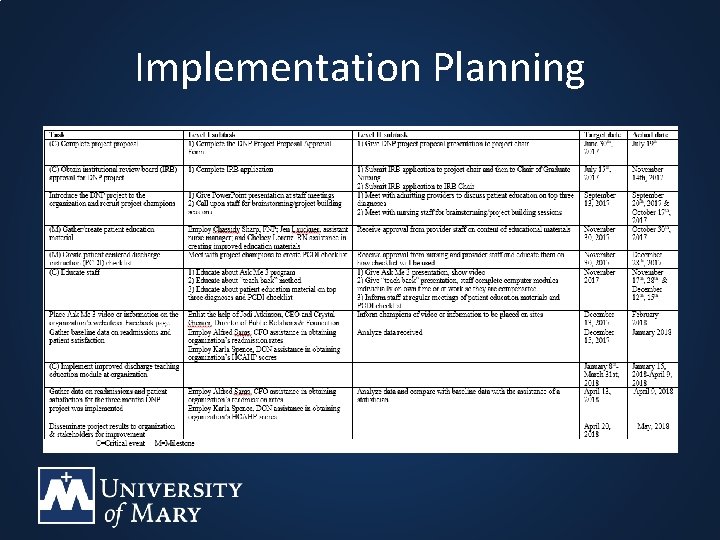
Implementation Planning
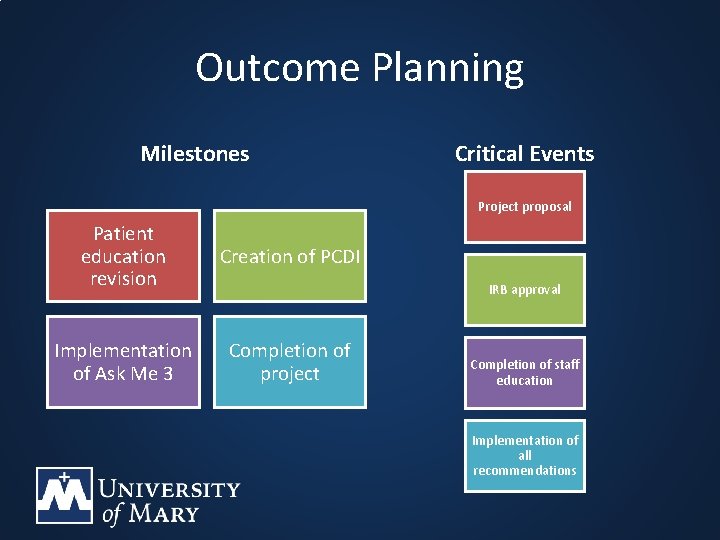
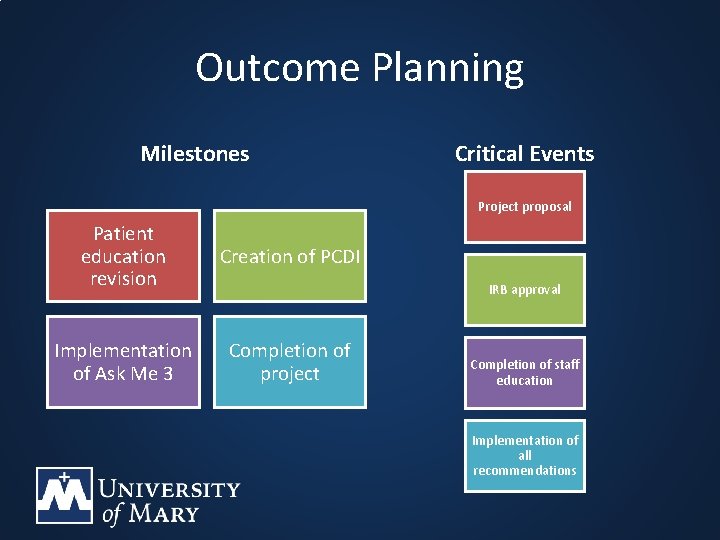
Outcome Planning Milestones Critical Events Project proposal Patient education revision Creation of PCDI Implementation of Ask Me 3 Completion of project IRB approval Completion of staff education Implementation of all recommendations
1. Educate on three main diagnoses • Power. Point presentation • Revision of discharge education on the diagnoses • Material printed • Pre & post knowledge evaluation
2. Educate on and implement Ask Me 3 program • Video provided by Institute for Healthcare Improvement (IHI) for staff and patients • Ask Me 3 materials printed • Posters displayed • Pre & post knowledge evaluation
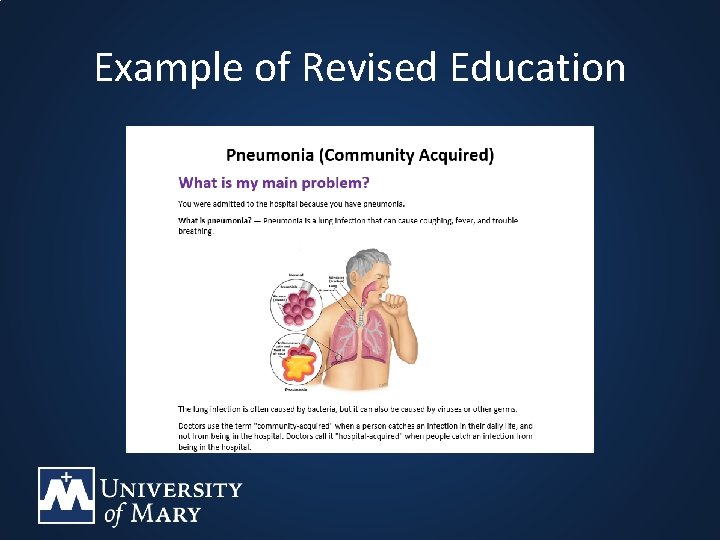
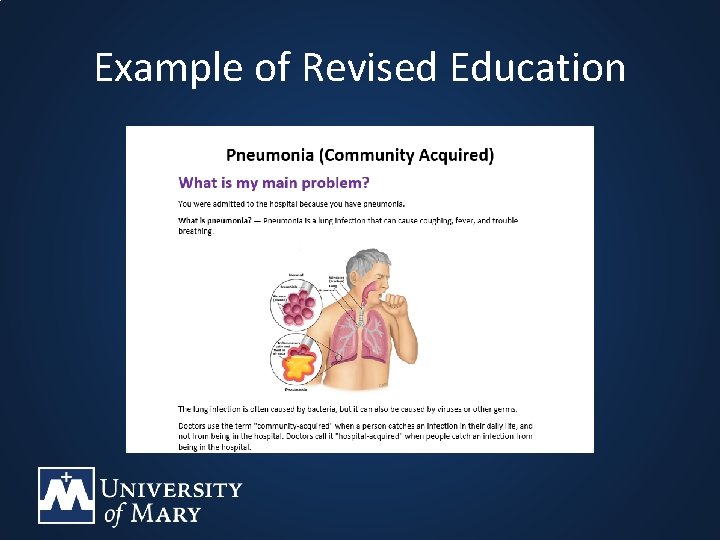
Example of Revised Education
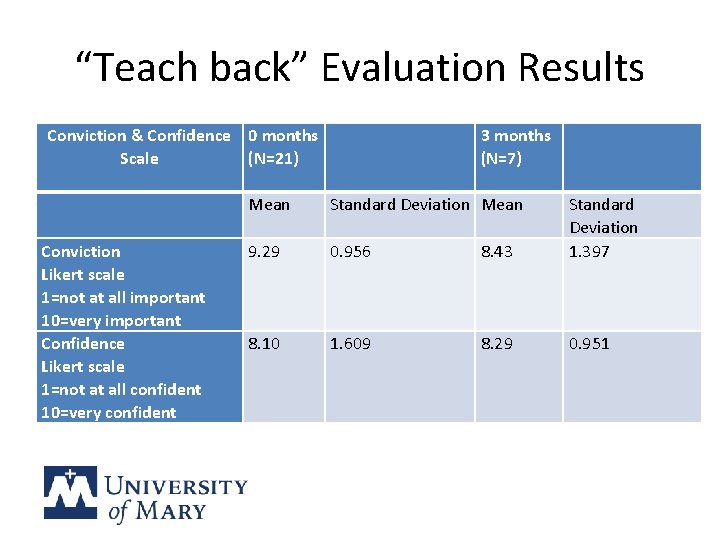
3. Educate and implement “teach back” method • 45 minute computer module • Conviction and Confidence Scale • Pre & post knowledge evaluation
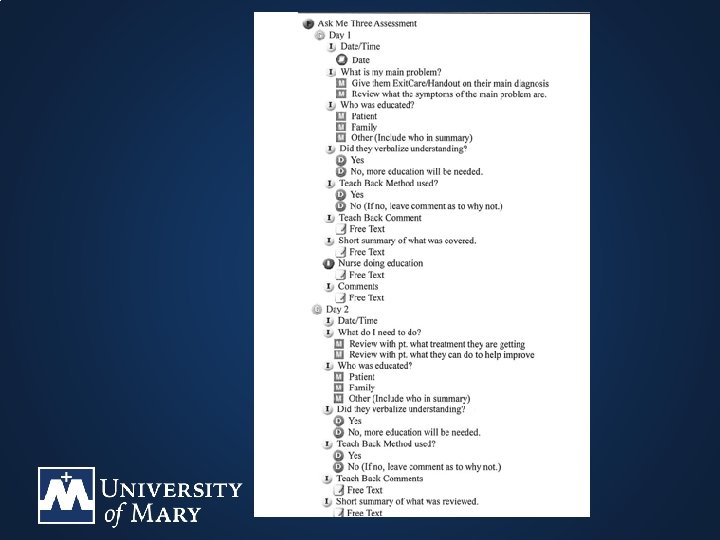
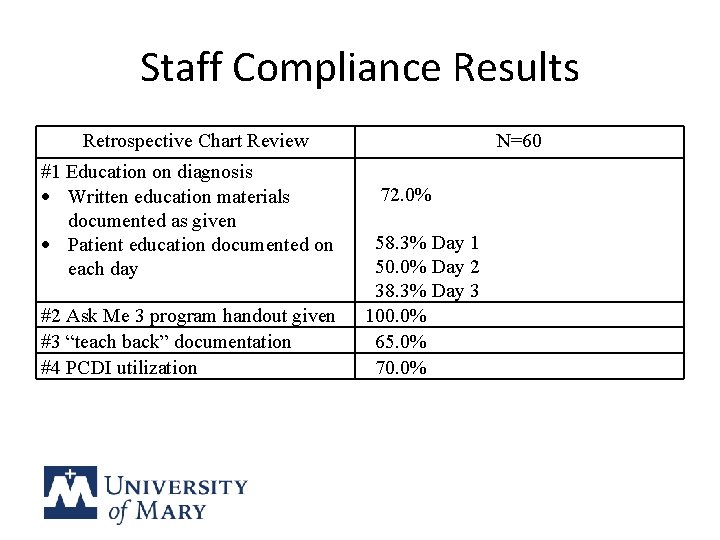
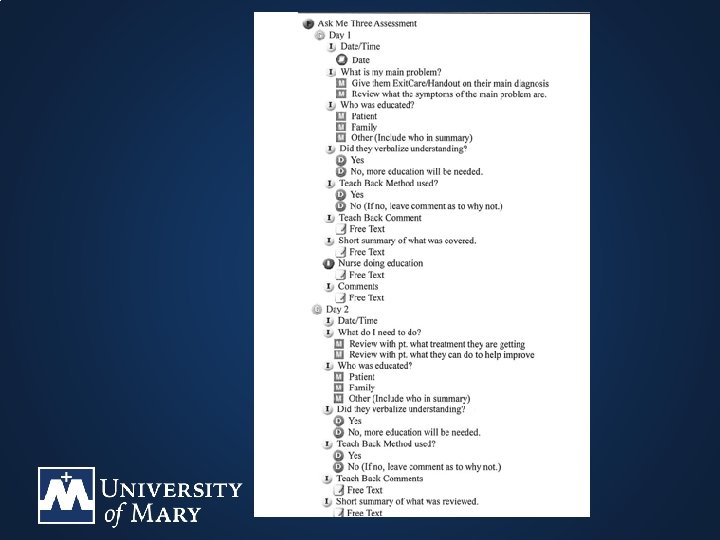
4. Develop and implement PCDI • Ask Me Three Assessment • Build and implement into electronic medical record • Retrospective chart review
Plan for Staff • Attend one of the four scheduled educational sessions • Complete interactive computer module independently • Initiate all interventions during implementation

IRB Process • End of July 2017: IRB Part 1 -4 submitted for DNP project chair review • August 1, 2017: Submitted to Chair of Graduate Nursing • October 13, 2017: Final draft submitted to Chair of Graduate Nursing • November 14, 2017: IRB approval
Evaluation Plan • • • Pre & post knowledge evaluations Conviction and Confidence Scale Retrospective chart review Readmission rates Patient satisfaction scores
Human Protections • • Human participants: DNP project setting staff Staff fully aware of DNP project No written consent obtained Ensured no identifying data on evaluations
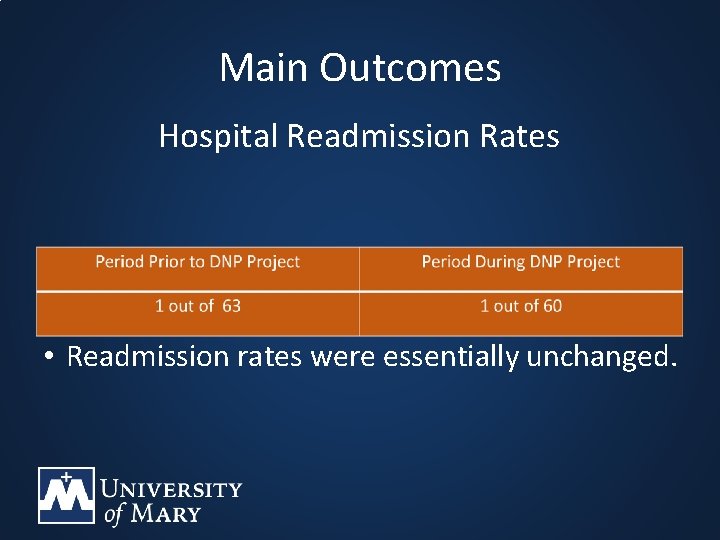
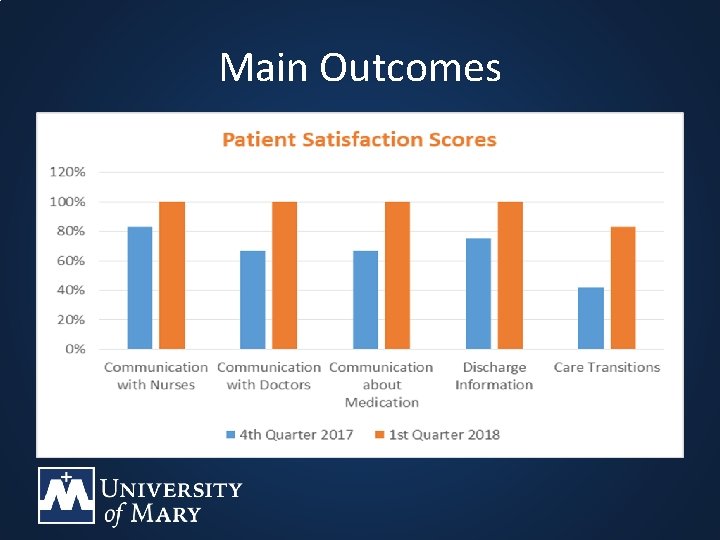
Timeframes • DNP project implementation – January 15 th-April 9 th (12 weeks during) – October 23 rd-January 14 th (12 weeks prior) • HCAHPS scores reported quarterly – 4 th quarter 2017 (October, November, December) – 1 st quarter 2018 (January, February, March)

Influencing Factors Threats & Barriers • Challenge of staff education • CEO excitement • Time of year Facilitators • Timing of educational sessions • DNP setting size • Openness • CEO excitement
Stakeholder Involvement • Karla Spence, DON: Main resource, communicator, staff updater • Jen Laukner, Assistant Nurse Manager: Report generator • Katie Tofteland, Informatics Nurse: Electonic medical record guru • Jodi Atkinson, CEO: Informant and cheerleader
Monitoring the DNP Project • • Visited DNP site every 2 -3 weeks Written communication every 2 -3 weeks Monitored staff compliance Followed up face to face or through written communication
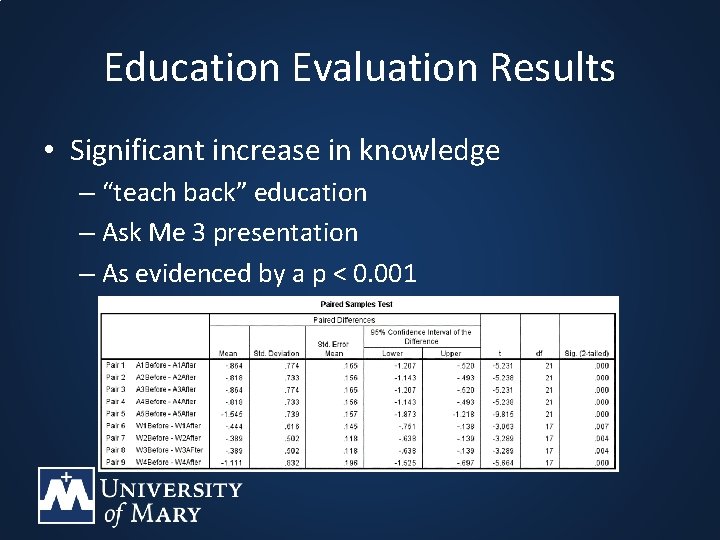
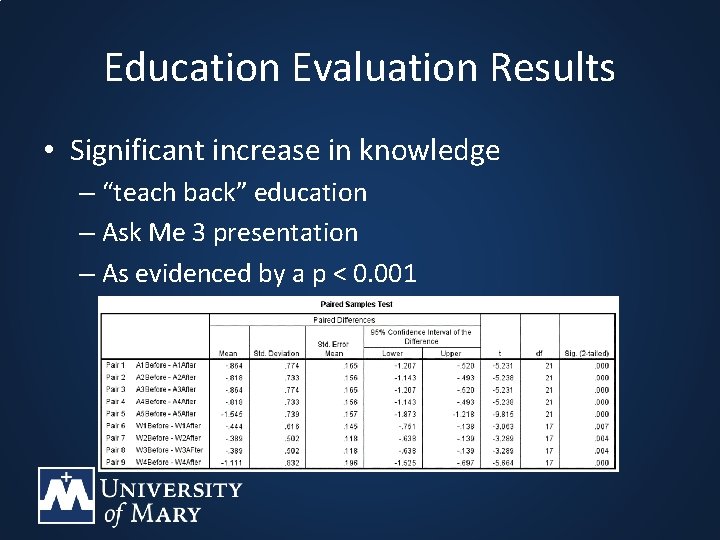
Education Evaluation Results • Significant increase in knowledge – “teach back” education – Ask Me 3 presentation – As evidenced by a p < 0. 001
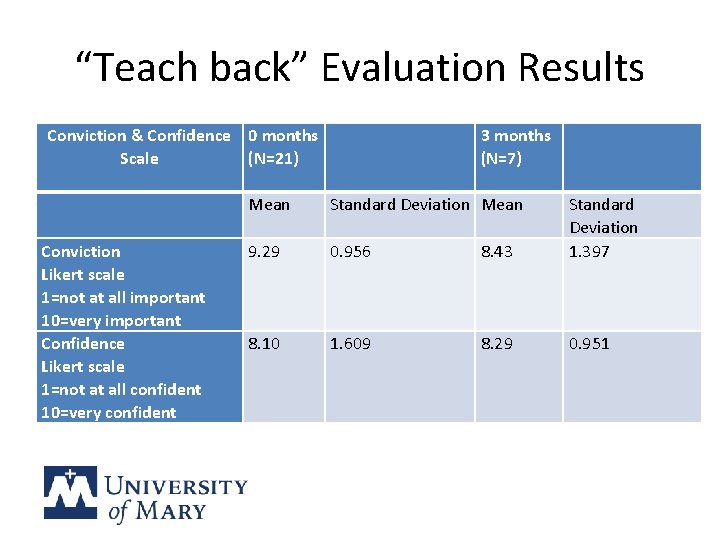
“Teach back” Evaluation Results Conviction & Confidence 0 months 3 months Scale (N=21) (N=7) Mean Standard Deviation Conviction 9. 29 0. 956 8. 43 1. 397 Likert scale 1=not at all important 10=very important Confidence 8. 10 1. 609 8. 29 0. 951 Likert scale 1=not at all confident 10=very confident
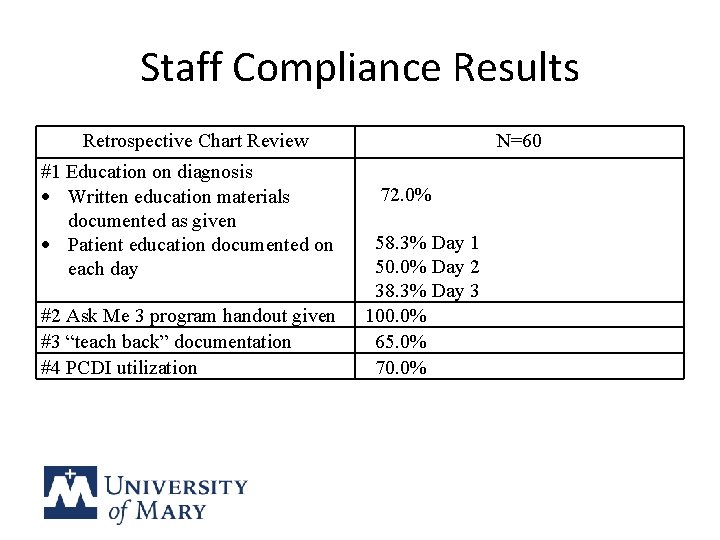
Staff Compliance Results Retrospective Chart Review #1 Education on diagnosis Written education materials documented as given Patient education documented on each day #2 Ask Me 3 program handout given #3 “teach back” documentation #4 PCDI utilization N=60 72. 0% 58. 3% Day 1 50. 0% Day 2 38. 3% Day 3 100. 0% 65. 0% 70. 0%
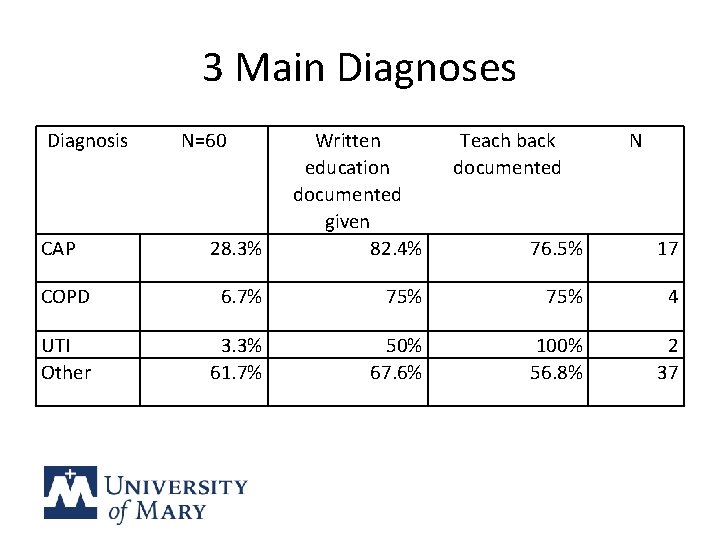
3 Main Diagnoses Diagnosis 28. 3% Written education documented given 82. 4% COPD 6. 7% UTI Other 3. 3% 61. 7% CAP N=60 Teach back documented N 76. 5% 17 75% 4 50% 67. 6% 100% 56. 8% 2 37
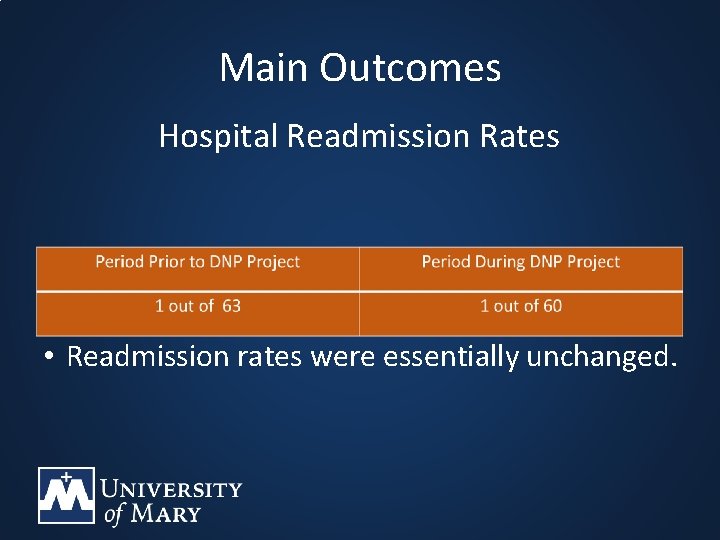
Main Outcomes Hospital Readmission Rates • Readmission rates were essentially unchanged.
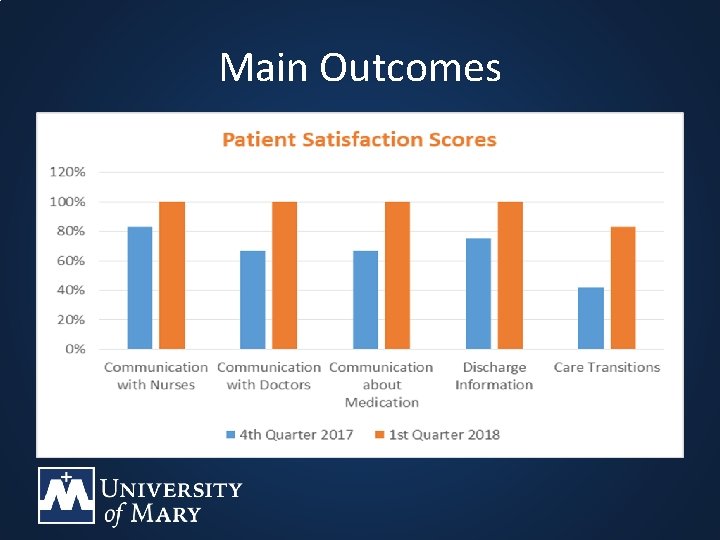
Main Outcomes
Unintended Consequences • Desire to implement Ask Me 3 on outpatient side • Patient education need for comfort care patients/families • Compliance rate lower on observation patients • Staff nurse to continue with her own master’s project
Interpretation • • Patient care improved Patient satisfaction scores increased Findings are transferable Project was cost effective
Project Revisions • Change or eliminate observation and swing bed accounts • Gather demographics on the participants • Use the “teach back” observation tool
Dissemination • Nursing and Medical staff at DNP setting – Monthly meeting in May 14 th & 16 th • Community Members – Health Fair May 7 th • Leaders of CAHs – North Dakota Critical Access Hospital Quality Network • Colleagues and Peers – Colloquium April 27 th & ND Center for Nursing 4 th Annual Conference
Conclusion & Recommendations • DNP setting staff willing to implement interventions • Patients reported higher satisfaction scores • Interventions could be implemented in outpatient settings
References • Center for Theory of Change. (2016). What is theory of change? Retrieved from https: //www. theoryofchange. org/what-is-theory-of-change/ • Grol, R. , Wensing, M. , Eccles, M. , and Davis, D. (Eds. ). (2013). Improving patient care: The implementation of change in clinical practice. (2 nd Edition). Hoboken, NJ: Wiley-Blackwell. • Image on slide 14 retrieved from https: //vijeydhinesh. wordpress. com/ • Institute for Healthcare Improvement (IHI). (2018). Always use teach back! Retrieved from http: //www. ihi. org/resources/Pages/Tools/Always. Use. Teach. Back!. aspx • Mc. Bride, M. and Andrews, G. J. (2013). The transition from acute care to home: A review of issues in discharge teaching and a framework for better practice. Canadian Journal of Cardiovascular Nursing, 23(3), 18– 24. • National Guideline Clearinghouse (NGC). (2014). Care transitions. Retrieved from https: //www. guideline. gov.
References • National Guideline Clearinghouse (NGC). (2012). Transitional care. In: Evidence-based geriatric nursing protocols for best practice. Retrieved from https: //www. guideline. gov • National Patient Safety Foundation. (n. d. ). Ask me 3: Good questions for your good health. Retrieved from http: //www. npsf. org/? page=askme 3 • Nursing Theories. (2011). Change theory. Retrieved from http: //www. currentnursing. com/nursing_theory/change_theory. ht ml • Reavy, K. (2016). Inquiry and Leadership A Resources for the DNP Project. (1 st Ed. ). Philadelphia, PA: F. A Davis Company.