Implementing a Telemedicine Program for Diabetic Retinopathy Screening
Implementing a Telemedicine Program for Diabetic Retinopathy Screening at an Internal Medicine Clinic: Benefits, Barriers & Future Directions CHRISTINA SHEPPLER, PHD Devers Eye Institute Telehealth Alliance of Oregon 2013
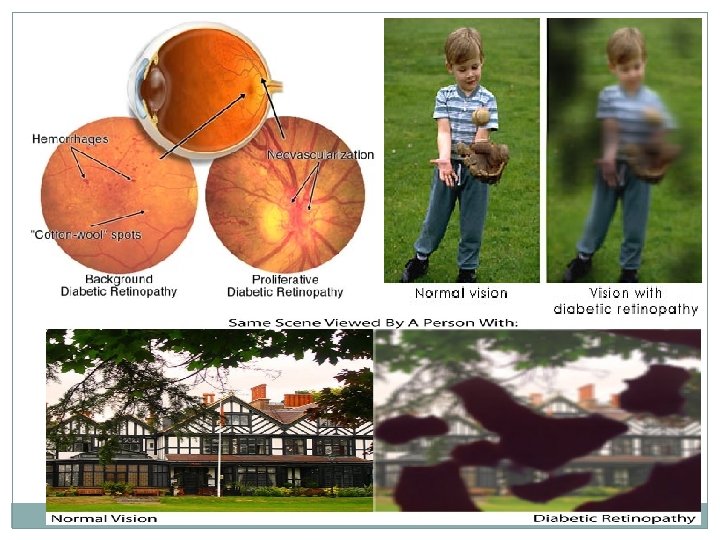
BACKGROUND • Diabetic retinopathy (DR) is the leading cause of blindness in adults aged 20 -74. • DR usually has no symptoms in its early stages • Early diagnosis and treatment can reduce the likelihood of severe vision loss by 90% • Approximately 50% of those diagnosed with diabetes obtain annual eye exams.
PILOT PROGRAM GOALS • Goal 1: Increase the proportion of patients with diabetes that are screened for retinopathy • Goal 2: Address common screening barriers with “one stop” diabetic care • Goal 3: Determine whether telemedicine service would be reimbursed by insurance • We partnered with LMGNW’s Internal Medicine Clinic to pilot the diabetic retinopathy screening telemedicine (DRST) program
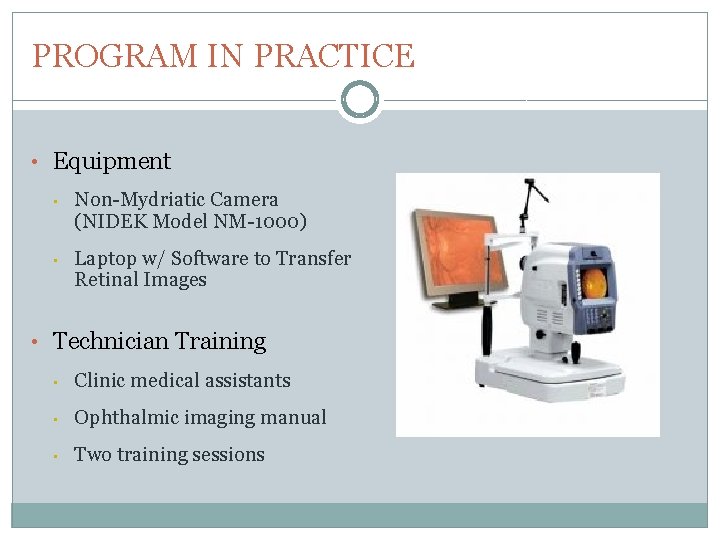
PROGRAM IN PRACTICE • Equipment • Non-Mydriatic Camera (NIDEK Model NM-1000) • Laptop w/ Software to Transfer Retinal Images • Technician Training • Clinic medical assistants • Ophthalmic imaging manual • Two training sessions
PROGRAM IN PRACTICE (continued) • Patient Screening • Charts reviewed to “flag” eligible patients • Approaching Patients • Telemedicine screening presented by physician • Brochures in waiting room
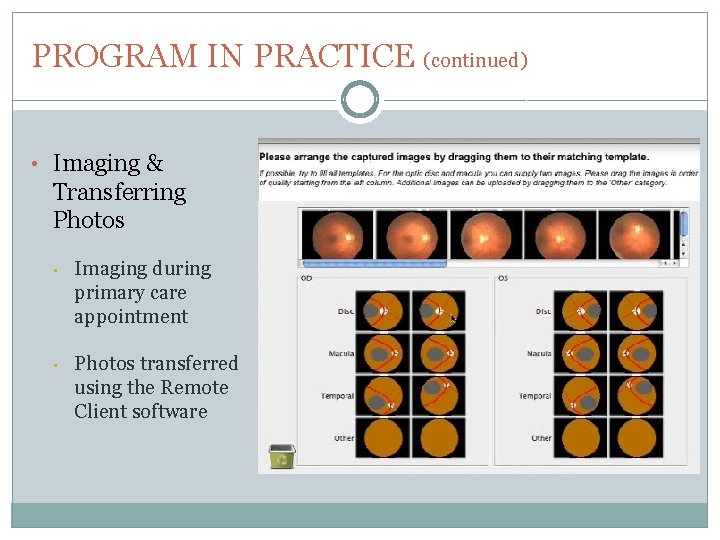
PROGRAM IN PRACTICE (continued) • Imaging & Transferring Photos • Imaging during primary care appointment • Photos transferred using the Remote Client software
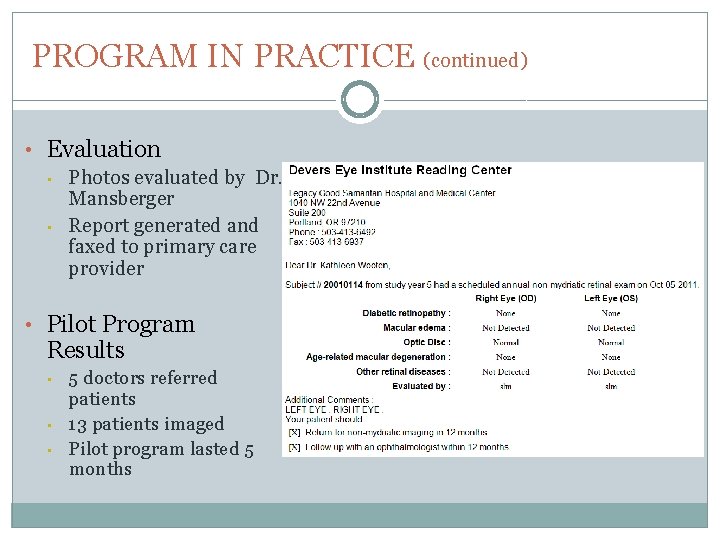
PROGRAM IN PRACTICE (continued) • Evaluation • Photos evaluated by Dr. Mansberger • Report generated and faxed to primary care provider • Pilot Program Results • • • 5 doctors referred patients 13 patients imaged Pilot program lasted 5 months
CURRENT STUDY • OBJECTIVE Obtain feedback from the clinic regarding • perceived benefits of the program • perceived barriers to implementation • possible improvements • sustainability potential • METHODS Semi-structured interviews with • clinic manager • clinic physician • medical assistants
RESULTS • BENEFITS • Capturing the patients who would not normally see an eye doctor • Telemedicine makes screening easy for all patients • New skill for medical assistants
RESULTS (continued) • BARRIERS • Program Not Presented to Patients • Difficulty with Imaging • Medical Assistant Restrictions • Time
RESULTS (continued) • IMPROVEMENTS • Equipment • Additional staff devoted to imaging • Contacting patients in advance • Sending evaluation results
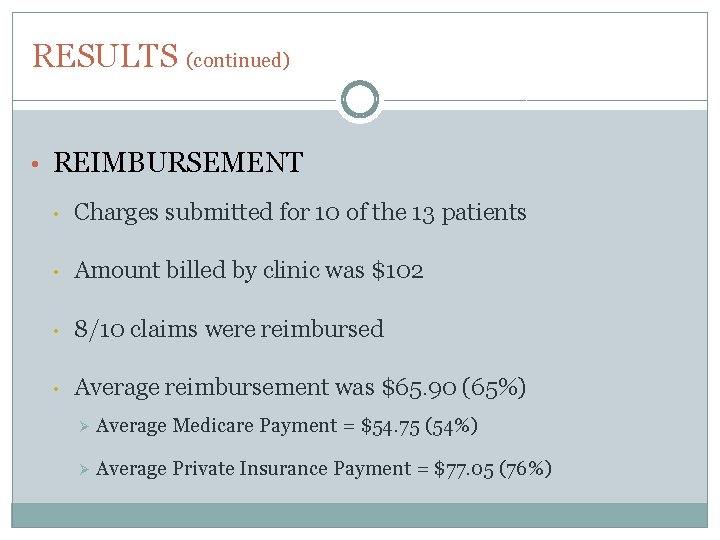
RESULTS (continued) • REIMBURSEMENT • Charges submitted for 10 of the 13 patients • Amount billed by clinic was $102 • 8/10 claims were reimbursed • Average reimbursement was $65. 90 (65%) Ø Average Medicare Payment = $54. 75 (54%) Ø Average Private Insurance Payment = $77. 05 (76%)
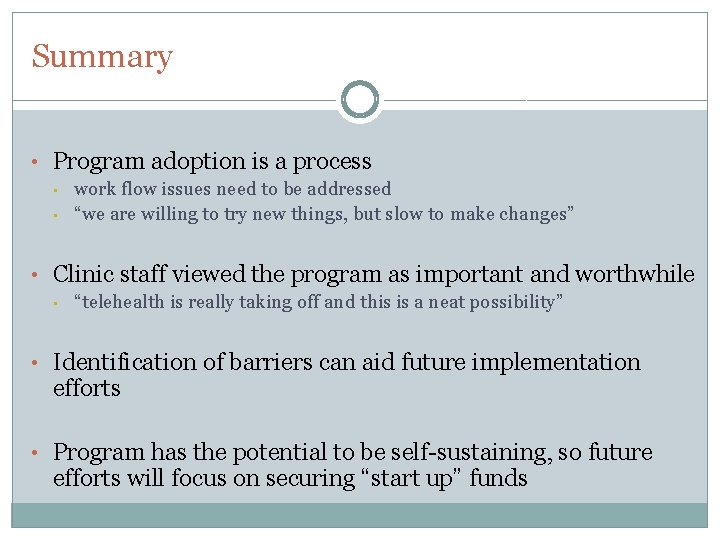
Summary • Program adoption is a process • • work flow issues need to be addressed “we are willing to try new things, but slow to make changes” • Clinic staff viewed the program as important and worthwhile • “telehealth is really taking off and this is a neat possibility” • Identification of barriers can aid future implementation efforts • Program has the potential to be self-sustaining, so future efforts will focus on securing “start up” funds
Questions ?
- Slides: 15