Implementing a Newborn Early Warning System in the
Implementing a Newborn Early Warning System in the SSBC NN T Pillay SSBCNN Oct 2012
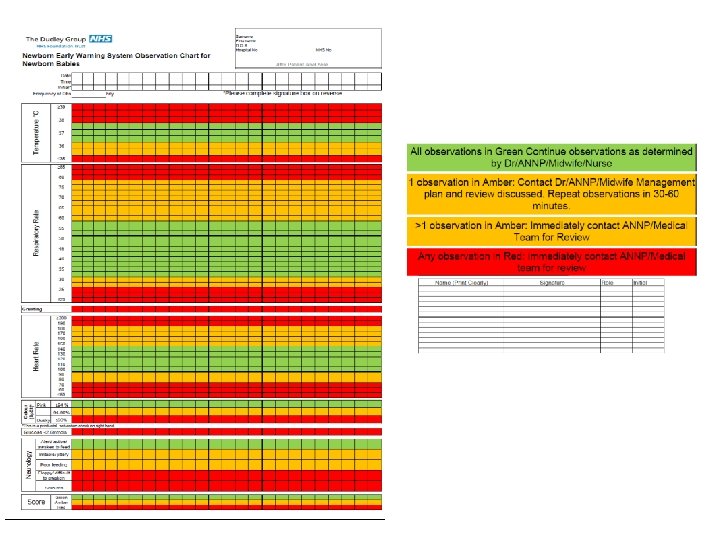
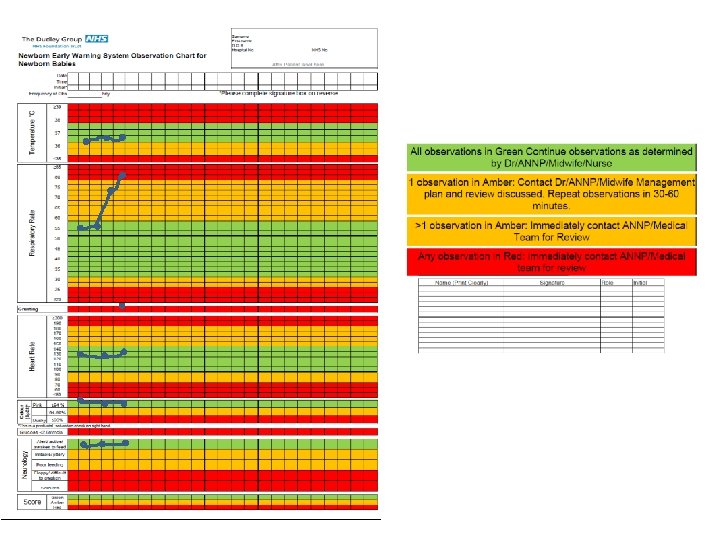
FIGURE 1 The ambulance corps of Baron Dominique-Jean Larrey, circa 1809.
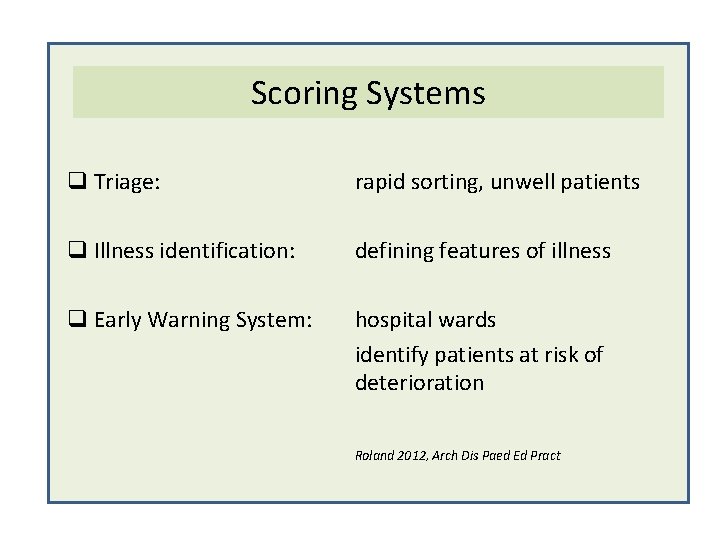
Scoring Systems q Triage: rapid sorting, unwell patients q Illness identification: defining features of illness q Early Warning System: hospital wards identify patients at risk of deterioration Roland 2012, Arch Dis Paed Ed Pract
q Antecedent events of acute deterioration/transfer to ICU: ‘Often early clinical signs missed’ q Early Warning Systems Recommended § CEMACH report 2006 § NPSA 2007, 2009
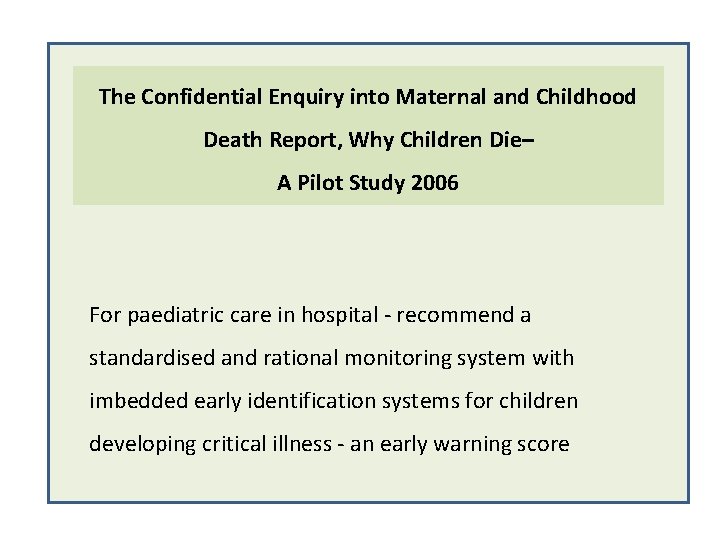
The Confidential Enquiry into Maternal and Childhood Death Report, Why Children Die– A Pilot Study 2006 For paediatric care in hospital - recommend a standardised and rational monitoring system with imbedded early identification systems for children developing critical illness - an early warning score
q Standardisation q Improve care for acutely ill q Addresses variability in detecting clinical Illness early 2012
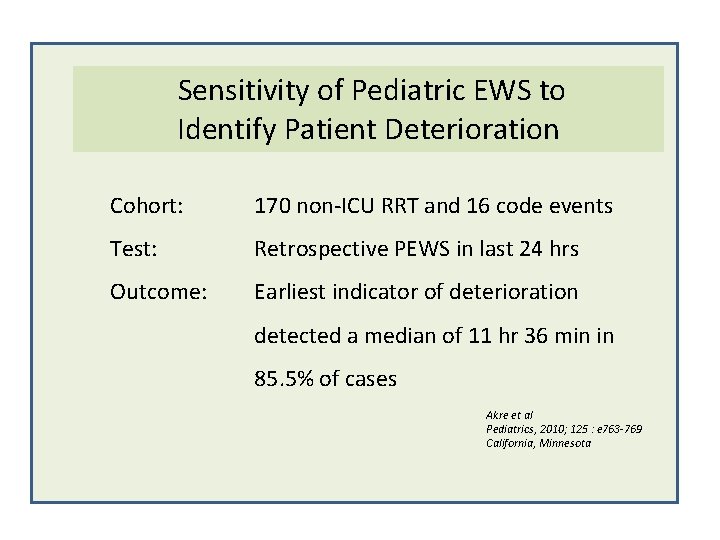
Sensitivity of Pediatric EWS to Identify Patient Deterioration Cohort: 170 non-ICU RRT and 16 code events Test: Retrospective PEWS in last 24 hrs Outcome: Earliest indicator of deterioration detected a median of 11 hr 36 min in 85. 5% of cases Akre et al Pediatrics, 2010; 125 : e 763 -769 California, Minnesota
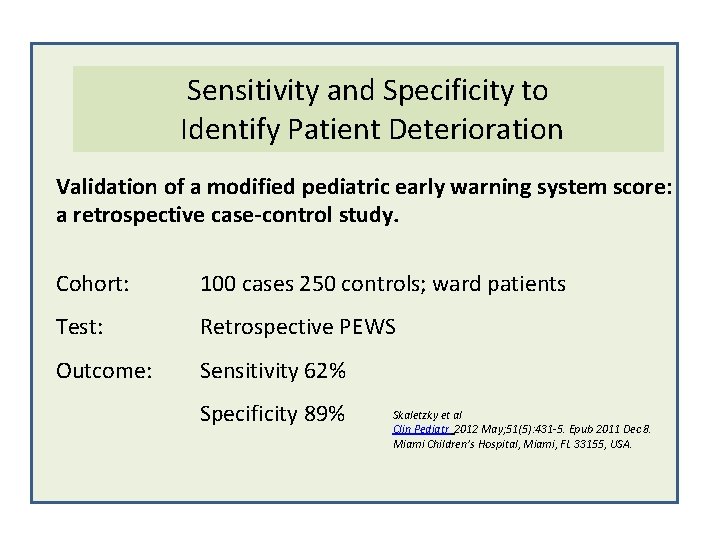
Sensitivity and Specificity to Identify Patient Deterioration Validation of a modified pediatric early warning system score: a retrospective case-control study. Cohort: 100 cases 250 controls; ward patients Test: Retrospective PEWS Outcome: Sensitivity 62% Specificity 89% Skaletzky et al Clin Pediatr 2012 May; 51(5): 431 -5. Epub 2011 Dec 8. Miami Children’s Hospital, Miami, FL 33155, USA.
Can it make a difference to outcome? Paediatric EWS Brighton: • Early identification of children at risk • Fewer codes • More timely transfer to ICU
Neonatal Early Warning System Which baby will it potentially benefit? § Hospitalised § Not critically ill, but under observation § Babies who are stable, but can deteriorate § At Risk Neonatal Infant
Neonatal Early Warning System § No defined directive for babies § Benefit? At Risk Neonatal Infants : ARNI Post natal ward Transitional care, SCBU
Neonatal Early Warning System • limited information on • progressive morbidity in early postnatal period in ARNI • the triage process, from post natal ward observations to review, investigations, intervention, admission to NNU
Neonatal Early Warning System • What impact does time to review/intervene have in ARNI with progressive deterioration?
Neonatal Early Warning System • What impact does time to review/intervene have in ARNI with progressive deterioration? • Sudden Unexpected Postnatal Collapse/Death (incidence 0. 05/1000 live births) J-C Becher Arch Dis Child FN 2012 F 30 -4

Neonatal Early Warning System • Can it influence provision of care? • Can it influence outcomes?
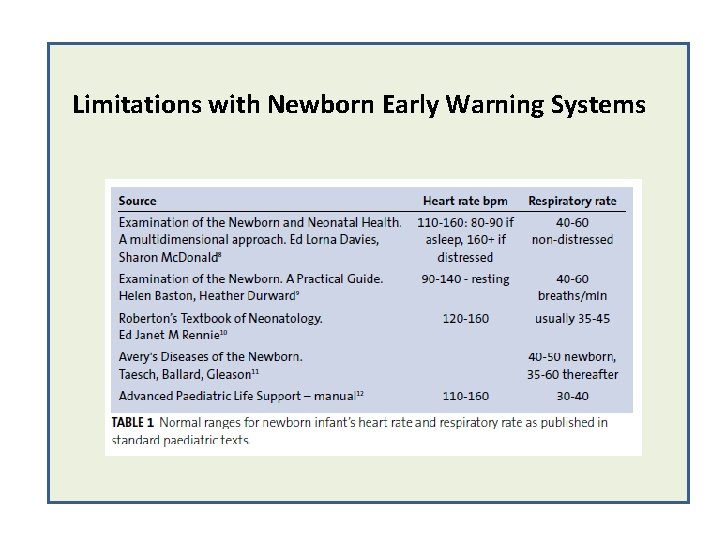
Limitations with Newborn Early Warning Systems
Neonatal Early Warning System Roland, Madar, Connolly. Infant 117 -120, Vol 6, Issue 4, 2012

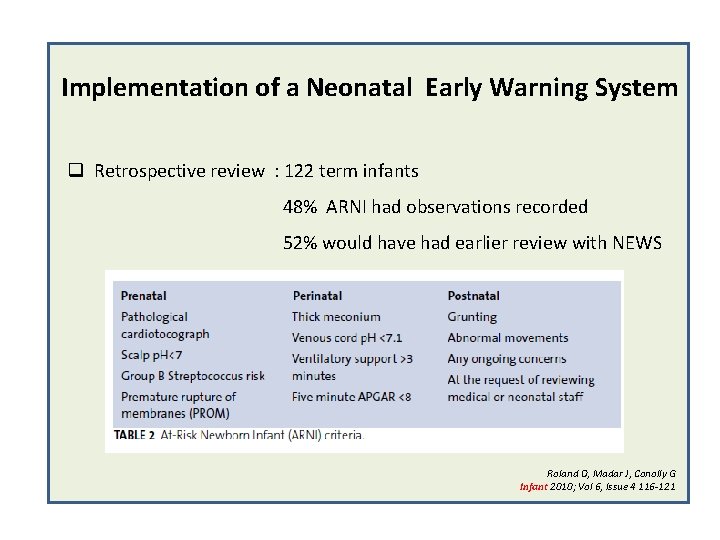
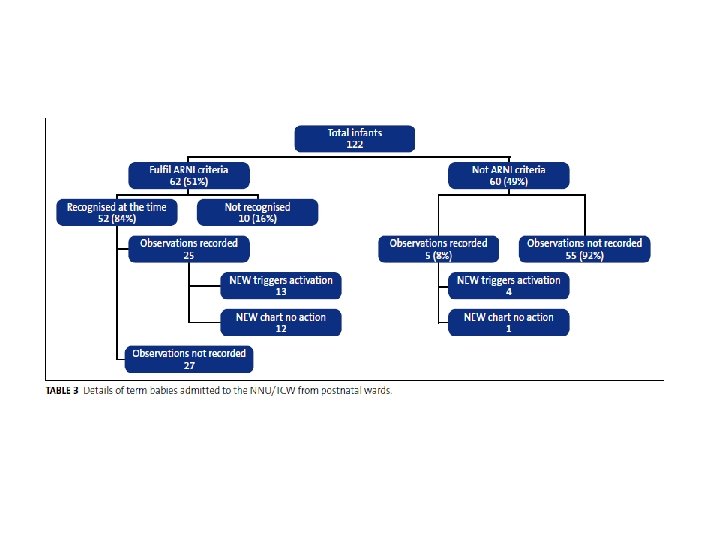
Implementation of a Neonatal Early Warning System q Retrospective review : 122 term infants 48% ARNI had observations recorded 52% would have had earlier review with NEWS Roland D, Madar J, Conolly G Infant 2010; Vol 6, Issue 4 116 -121
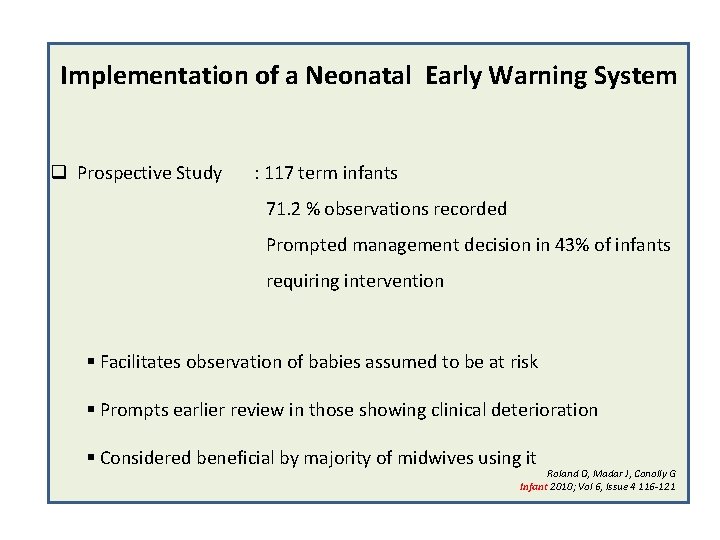
Implementation of a Neonatal Early Warning System q Prospective Study : 117 term infants 71. 2 % observations recorded Prompted management decision in 43% of infants requiring intervention § Facilitates observation of babies assumed to be at risk § Prompts earlier review in those showing clinical deterioration § Considered beneficial by majority of midwives using it Roland D, Madar J, Conolly G Infant 2010; Vol 6, Issue 4 116 -121
Implementation of a Neonatal Early Warning System q England Variable implementation eg Plymouth, Liverpool, Cambridge, Northern Neonatal Network; not standardised q Scotland Widespread standardised implementation in NHS, Orkney, Shetland
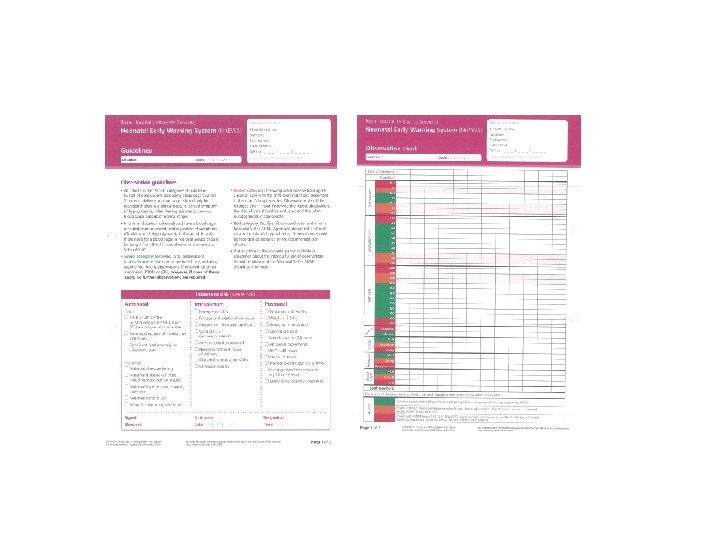
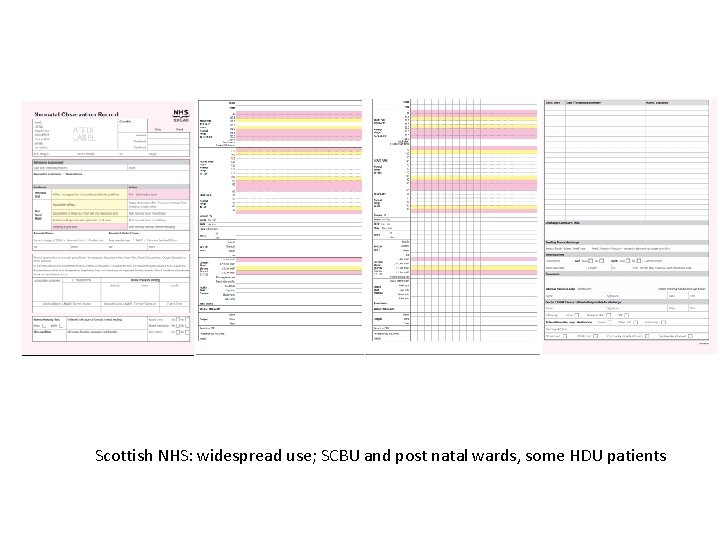
Scottish NHS: widespread use; SCBU and post natal wards, some HDU patients
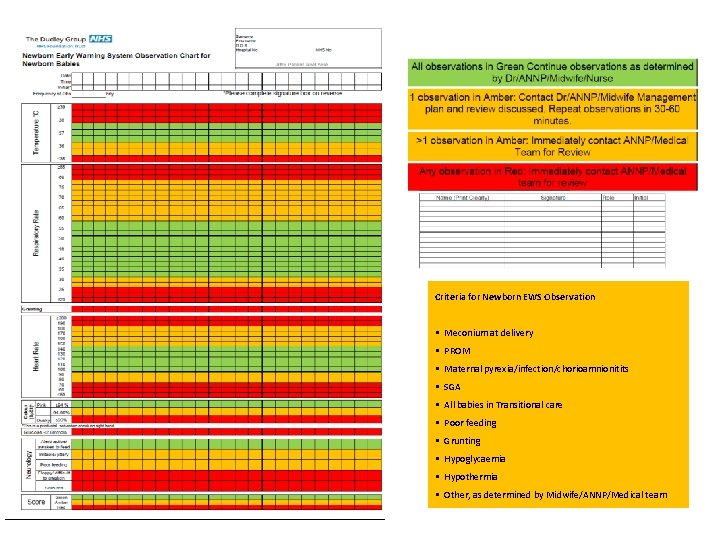
Criteria for Newborn EWS Observation § Meconium at delivery § PROM § Maternal pyrexia/infection/chorioamnionitits § SGA § All babies in Transitional care § Poor feeding § Grunting § Hypoglycaemia § Hypothermia § Other, as determined by Midwife/ANNP/Medical team
SSBC NN Team Theresa Pilsbury (midwifery) NXH Claire Cockburn, Nicola Taylor, Pam Smith (NNU) RHH Anne Clark/Jane Henley Walsall Gina Hartwell (NNU) MSG Emma Hubball (midwifery) UHNS Matthew Nash Grid Trainee
Feedback Positive: § Stopped false calls § Highlighted the 'zig zag' baby § Prompted staff action when they might otherwise not have acted § Empowered midwifery support for post natal babies
Feedback Negative: § Parent perception of scoring § Documentation § Lack of common sense approach to duration /frequency of observations § ‘Why do we need a score if we can recognise a baby becoming ill? ’ § Cost
Nurses role in EWS q Critical thinking q Ease of observation q Easy visualization of problematic baby q Standardized escalation system
Future Questions § Does it add value to post natal care provided? § Does it streamline nursing service provision? § Is it cost effective and time – effective? § Does it empower nursing team to think critically? § Does it make a difference to outcome?
Future Questions Audit/review of effectiveness: § False positives (hypersensitivity) § False negatives (babies not picked up)
Conclusion § § § Fashionable Promoted through National bodies for Adults/Paediatrics No standardised approach in Neonates § No clear idea as to whether it is indicated it will make a difference in At Risk Neonates, not managed in HDU/ICU § Being trialed in SSBC NN
- Slides: 39