Implementation of Child Parent Psychotherapy in a Family
- Slides: 40
Implementation of Child Parent Psychotherapy in a Family Homeless Shelter: Offering Healing from Trauma During Crisis Kate Goetz, LCSW, I/ECMH-C
Session Objectives Identify importance of addressing trauma exposure of homeless children age 0 -5 Provide overview of Child Parent Psychotherapy (CPP) principles, goals, interventions and training process Discuss opportunities and challenges of offering CPP in a family homeless shelter setting
Stories for Children that Grownups Can Watch o Inside Him https: //youtu. be/g 23 V 7 lxo. Sn 0 o Other videos and resources from Illinois Childhood Trauma Coalition available at Lookthroughtheireyes. org
The Stress-Trauma Continuum “Stress may range in intensity from normative strains associated with everyday life to extreme distortions of physiological and emotional balance as the result of catastrophic experiences. ” (Lieberman and Van Horn, 2008)
The Stress-Trauma Continuum “Stress becomes trauma when the intensity of frightening events becomes unmanageable to the point of threatening physical and psychological integrity. ” (Lieberman and Van Horn, 2008)
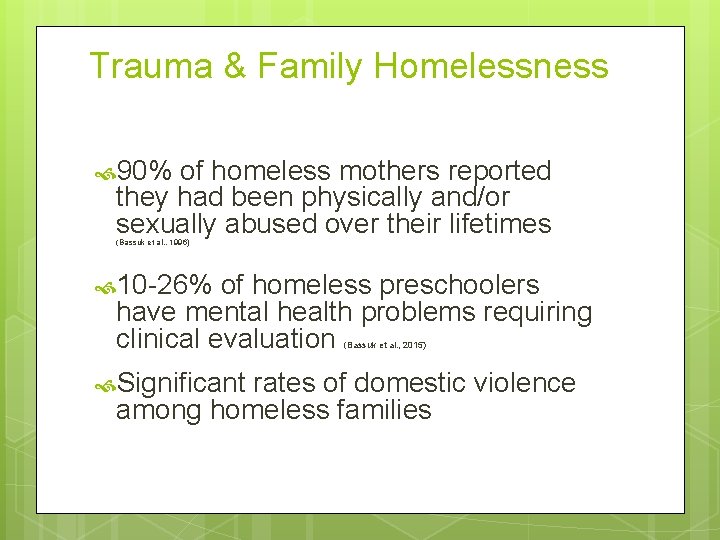
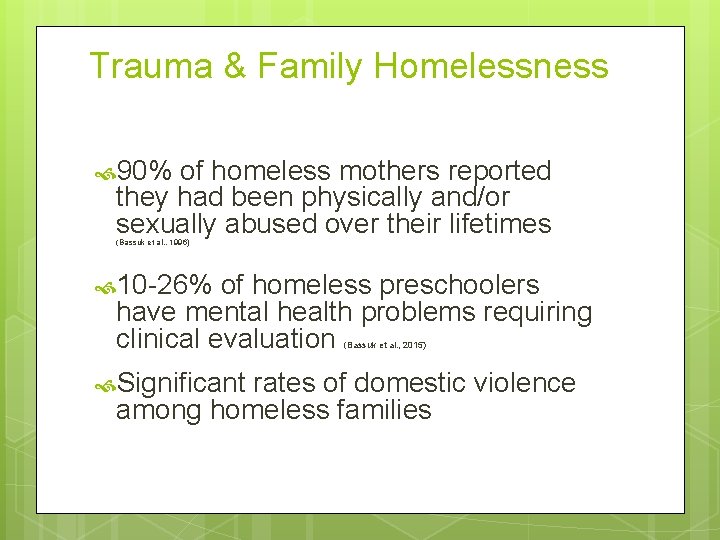
Trauma & Family Homelessness 90% of homeless mothers reported they had been physically and/or sexually abused over their lifetimes (Bassuk et al. , 1996) 10 -26% of homeless preschoolers have mental health problems requiring clinical evaluation (Bassuk et al. , 2015) Significant rates of domestic violence among homeless families
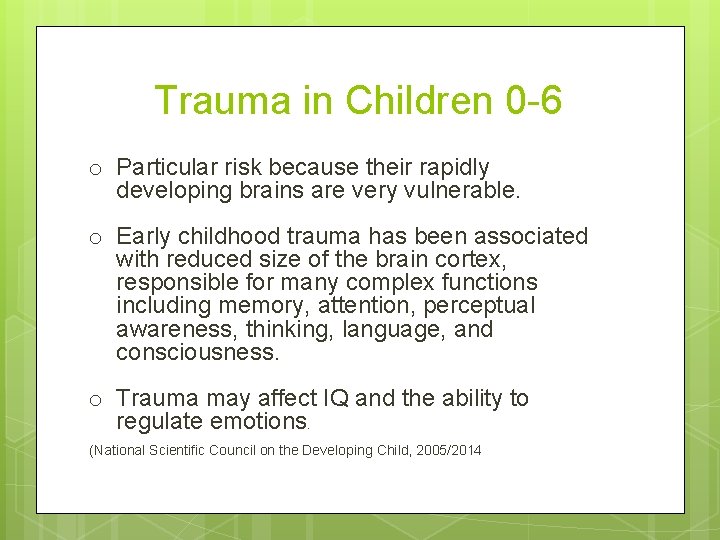
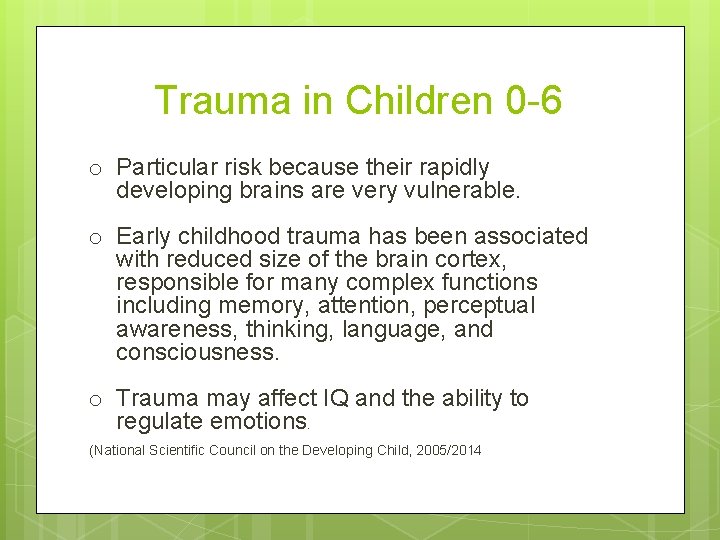
Trauma in Children 0 -6 o Particular risk because their rapidly developing brains are very vulnerable. o Early childhood trauma has been associated with reduced size of the brain cortex, responsible for many complex functions including memory, attention, perceptual awareness, thinking, language, and consciousness. o Trauma may affect IQ and the ability to regulate emotions. (National Scientific Council on the Developing Child, 2005/2014
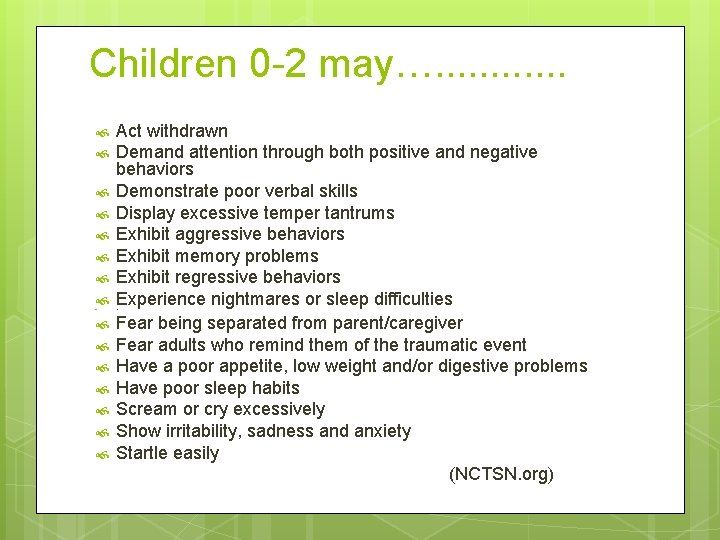
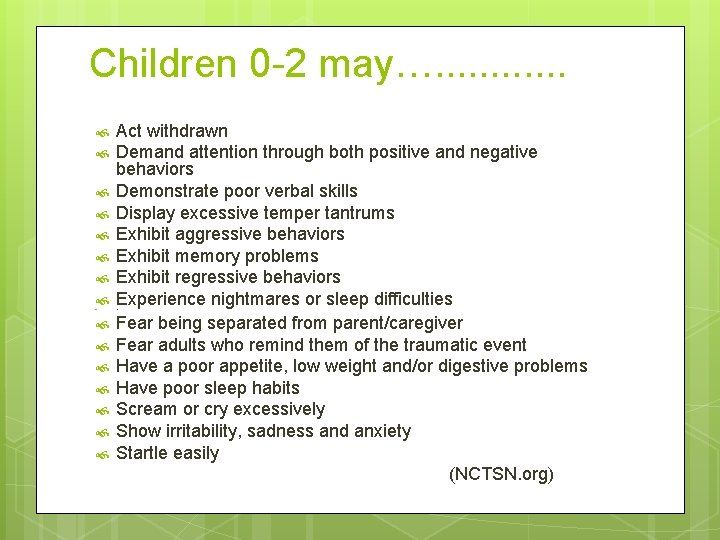
Children 0 -2 may…. . . Act withdrawn Demand attention through both positive and negative behaviors Demonstrate poor verbal skills Display excessive temper tantrums Exhibit aggressive behaviors Exhibit memory problems Exhibit regressive behaviors Experience nightmares or sleep difficulties Fear being separated from parent/caregiver Fear adults who remind them of the traumatic event Have a poor appetite, low weight and/or digestive problems Have poor sleep habits Scream or cry excessively Show irritability, sadness and anxiety Startle easily (NCTSN. org) ver
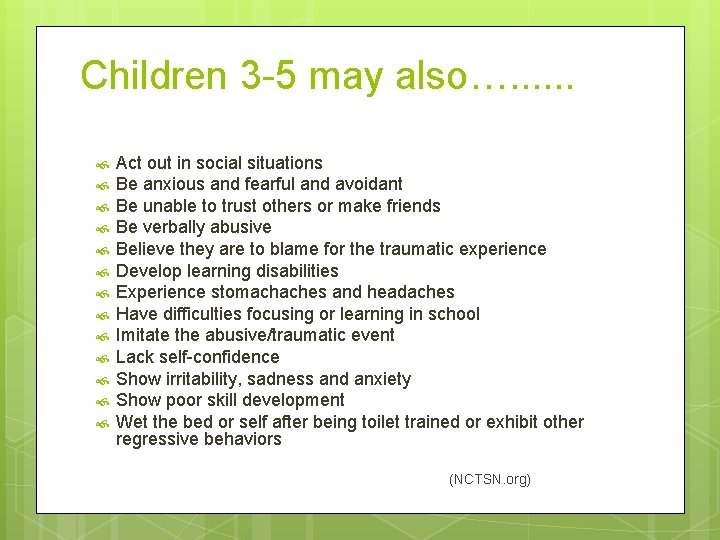
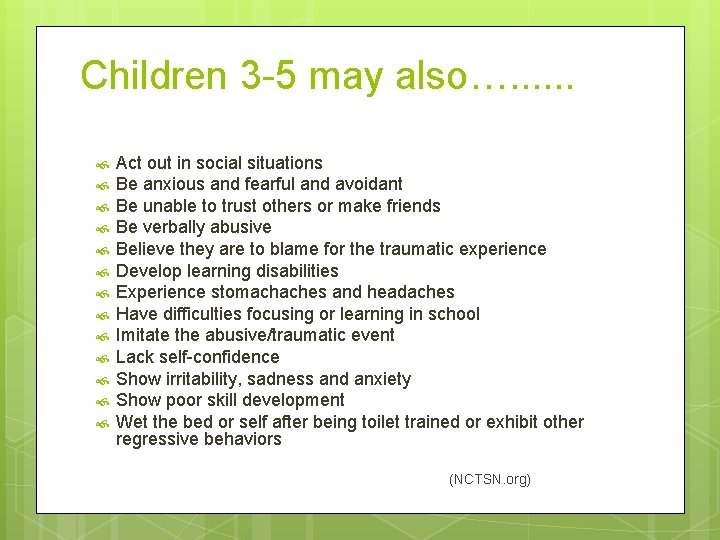
Children 3 -5 may also…. . . Act out in social situations Be anxious and fearful and avoidant Be unable to trust others or make friends Be verbally abusive Believe they are to blame for the traumatic experience Develop learning disabilities Experience stomachaches and headaches Have difficulties focusing or learning in school Imitate the abusive/traumatic event Lack self-confidence Show irritability, sadness and anxiety Show poor skill development Wet the bed or self after being toilet trained or exhibit other regressive behaviors (NCTSN. org)
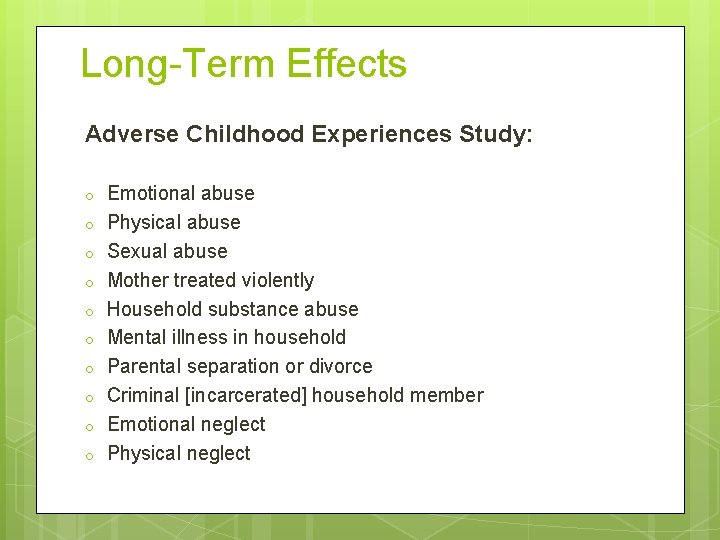
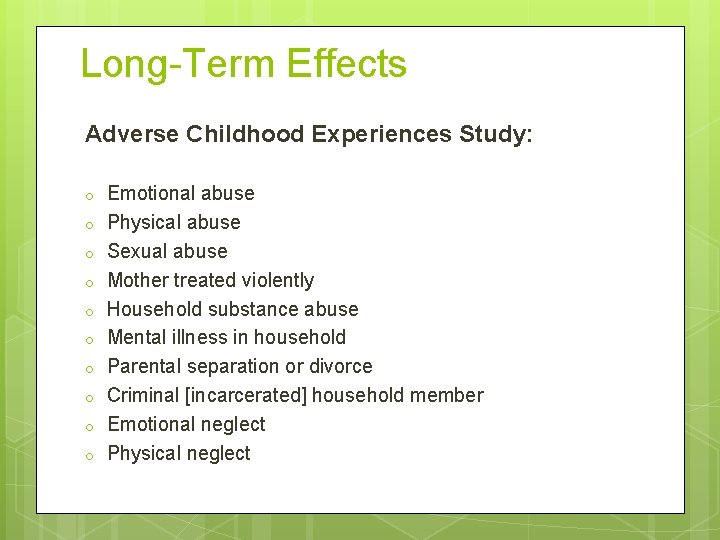
Long-Term Effects Adverse Childhood Experiences Study: o o o o o Emotional abuse Physical abuse Sexual abuse Mother treated violently Household substance abuse Mental illness in household Parental separation or divorce Criminal [incarcerated] household member Emotional neglect Physical neglect
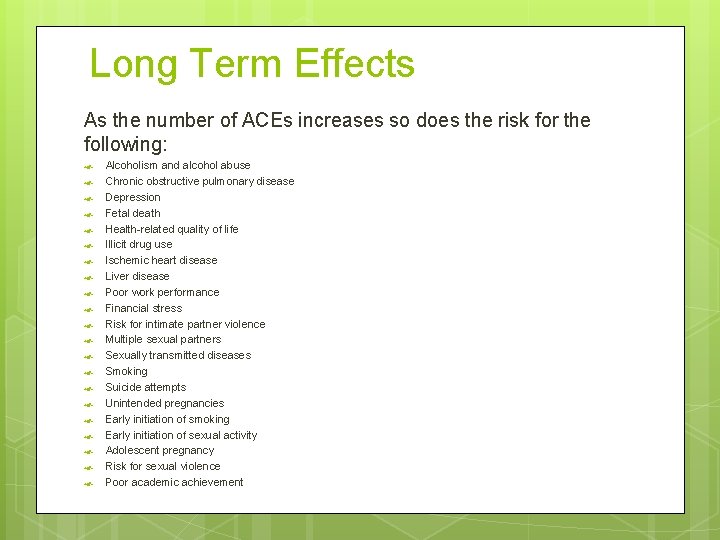
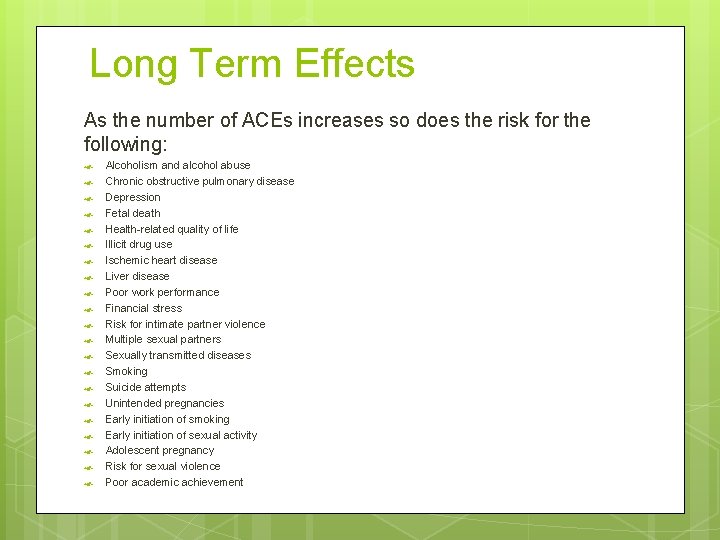
Long Term Effects As the number of ACEs increases so does the risk for the following: Alcoholism and alcohol abuse Chronic obstructive pulmonary disease Depression Fetal death Health-related quality of life Illicit drug use Ischemic heart disease Liver disease Poor work performance Financial stress Risk for intimate partner violence Multiple sexual partners Sexually transmitted diseases Smoking Suicide attempts Unintended pregnancies Early initiation of smoking Early initiation of sexual activity Adolescent pregnancy Risk for sexual violence Poor academic achievement
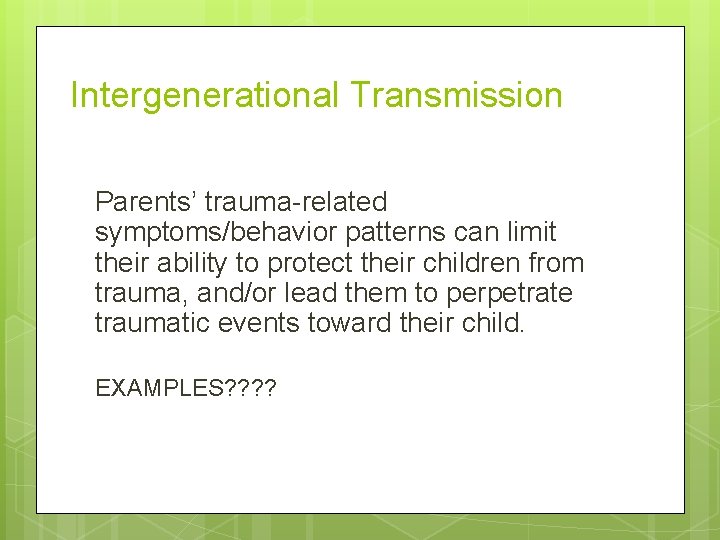
Intergenerational Transmission Parents’ trauma-related symptoms/behavior patterns can limit their ability to protect their children from trauma, and/or lead them to perpetrate traumatic events toward their child. EXAMPLES? ?
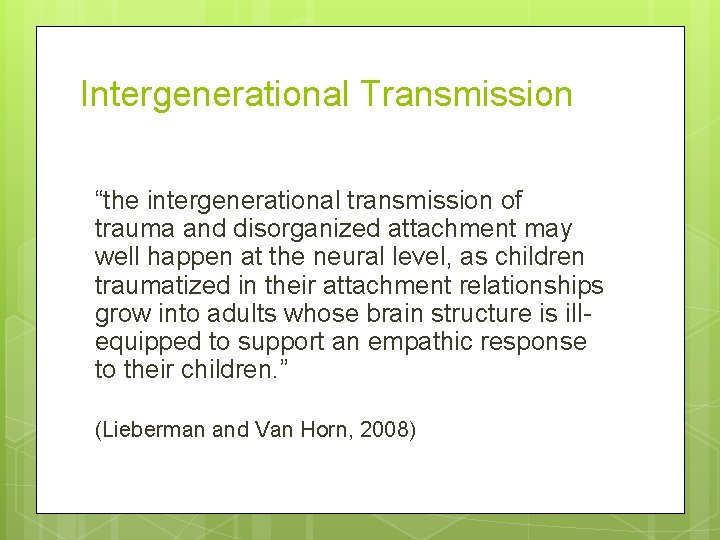
Intergenerational Transmission “the intergenerational transmission of trauma and disorganized attachment may well happen at the neural level, as children traumatized in their attachment relationships grow into adults whose brain structure is illequipped to support an empathic response to their children. ” (Lieberman and Van Horn, 2008)
Systems-Level Trauma POVERTY: Systemic Historical Income/Wealth Inequality Racism Trauma: Slavery, immigrationrelated trauma
Systems-Level Trauma ”Society at large creates conditions in which some individuals and families are held at a distance as ‘others, ’ their plight unwitnessed and their cries unheard by those with power to changes the circumstances of their lives. These families have been mired in poverty, marginalization, racism, and violence often for generations. ” (Lieberman and Van Horn, 2008)
Systems-Level Trauma “The parents’ character structure is marred by the internalization of these societal factors. Within a mental health framework they can be most fairly diagnosed as having a developmental trauma disorder– a personality style so profoundly shaped by the unrelieved experience of internal and external danger that it is bereft of the ability to appraise danger realistically, respond protectively, trust in a benevolent social order and the possibility of loving intimate relationships, learn without major constrictions, and operate confidently in pursuit of personal goals. ” (Lieberman and Van Horn, 2008)
Child-Parent Psychotherapy o Evidence-based dyadic attachment-based treatment for young children exposed to interpersonal violence (http: //www. nctsn. org/sites/default/files/assets/pdfs/cpp_general. pdf) o “a relationship-based approach to treatment for children ages birth through five when their parent’s failure to protect them has derailed their mental health. ” (Lieberman and Van Horn, 2008) o “Client” is not the child or the parent, but the CHILD-PARENT RELATIONSHIP
Child-Parent Psychotherapy Theoretical basis: Based in attachment theory but also integrates psychodynamic, developmental, trauma, social learning, and cognitive behavioral theories. Key components: Focus on safety, affect regulation, improving the child-caregiver relationship, normalization of trauma related response, joint construction of a trauma narrative, with the goal of returning the child to a normal developmental trajectory http: //www. nctsn. org/sites/default/files/assets/pdfs/cpp_general. pdf
Goals of CPP 1. Return to normal development, adaptive coping, and engagement with present activities and future goals. 2. Increased capacity to respond realistically to threat. 3. Maintaining regular levels of affective arousal. 4. Reestablishing trust in bodily sensations. (continued next slide)
Goals of CPP 5. Restoration of reciprocity in intimate relationships. 6. Normalization of the traumatic response. 7. Increasing differentiation between reliving and remembering. 8. Placing the traumatic experience in perspective. (Lieberman et al. , 2015)
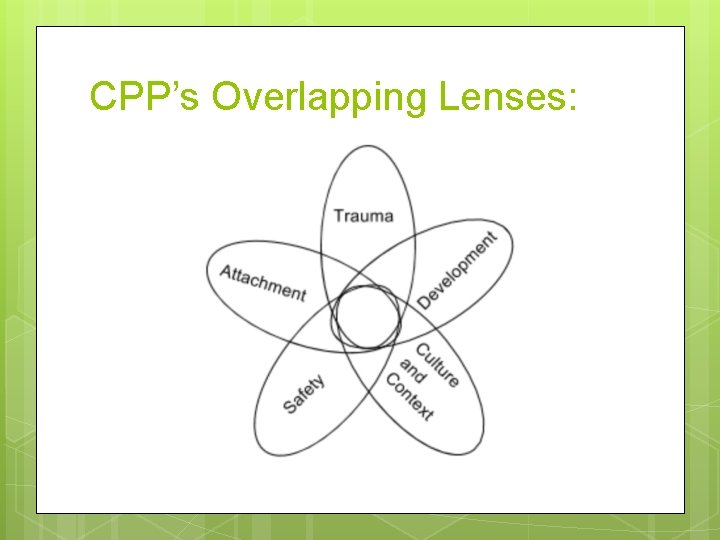
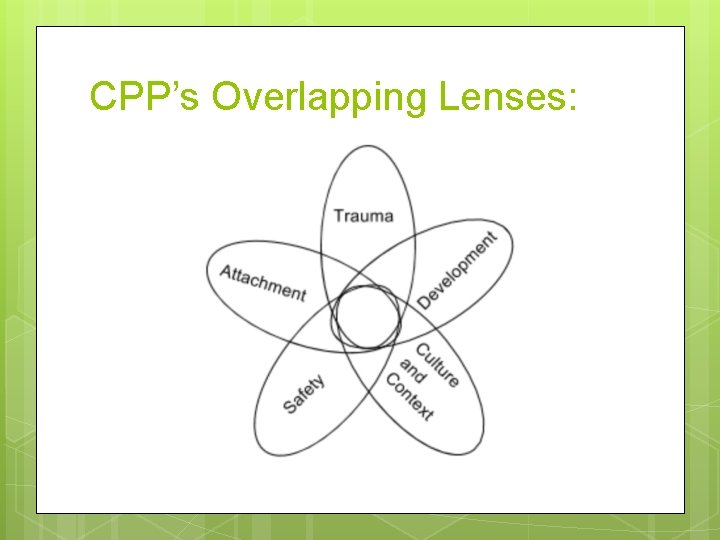
CPP’s Overlapping Lenses:
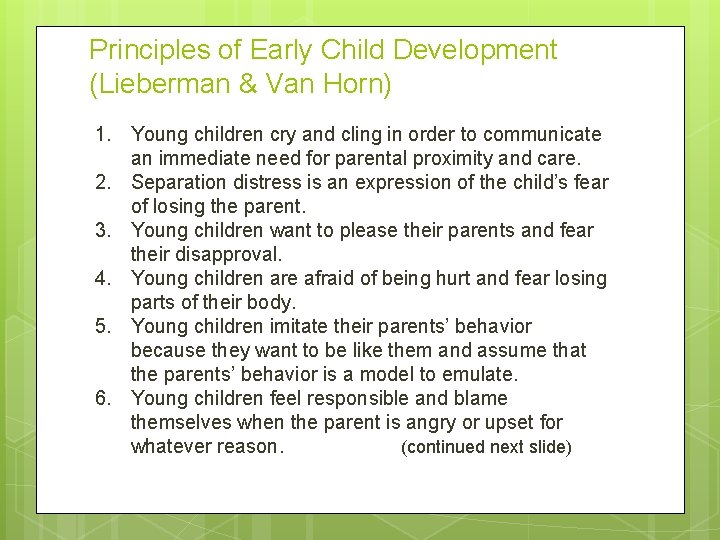
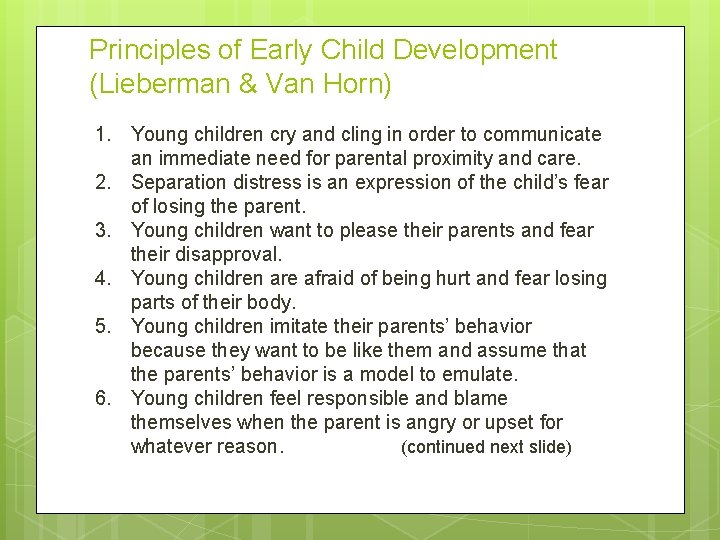
Principles of Early Child Development (Lieberman & Van Horn) 1. Young children cry and cling in order to communicate an immediate need for parental proximity and care. 2. Separation distress is an expression of the child’s fear of losing the parent. 3. Young children want to please their parents and fear their disapproval. 4. Young children are afraid of being hurt and fear losing parts of their body. 5. Young children imitate their parents’ behavior because they want to be like them and assume that the parents’ behavior is a model to emulate. 6. Young children feel responsible and blame themselves when the parent is angry or upset for whatever reason. (continued next slide)
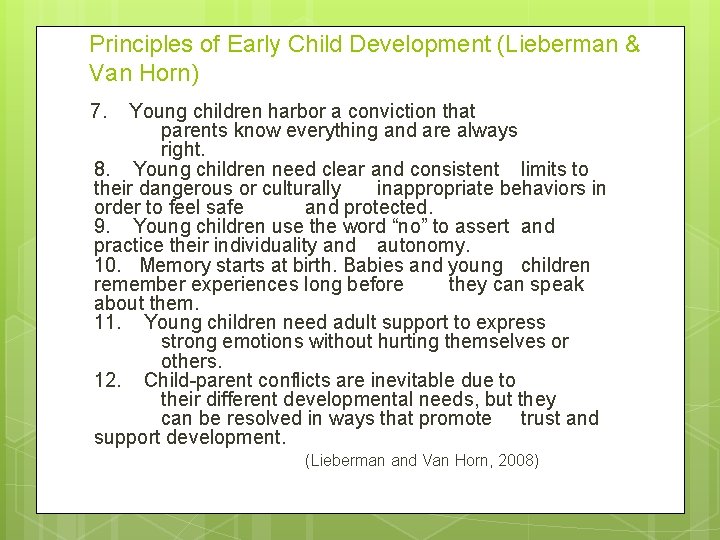
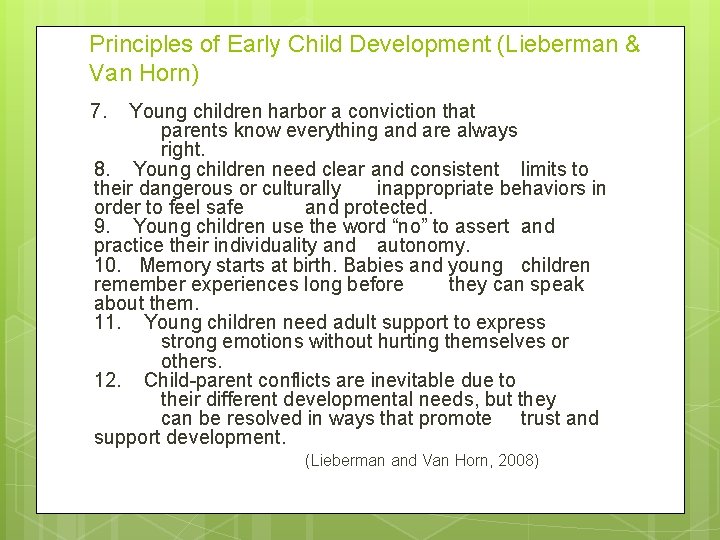
Principles of Early Child Development (Lieberman & Van Horn) 7. Young children harbor a conviction that parents know everything and are always right. 8. Young children need clear and consistent limits to their dangerous or culturally inappropriate behaviors in order to feel safe and protected. 9. Young children use the word “no” to assert and practice their individuality and autonomy. 10. Memory starts at birth. Babies and young children remember experiences long before they can speak about them. 11. Young children need adult support to express strong emotions without hurting themselves or others. 12. Child-parent conflicts are inevitable due to their different developmental needs, but they can be resolved in ways that promote trust and support development. (Lieberman and Van Horn, 2008)
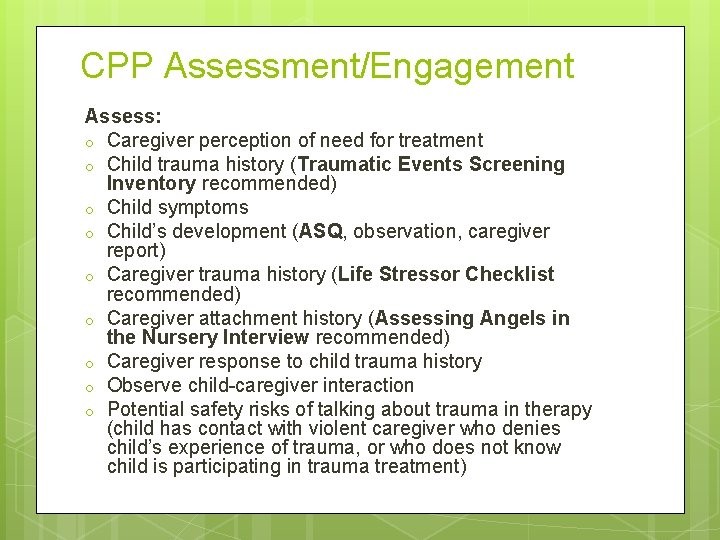
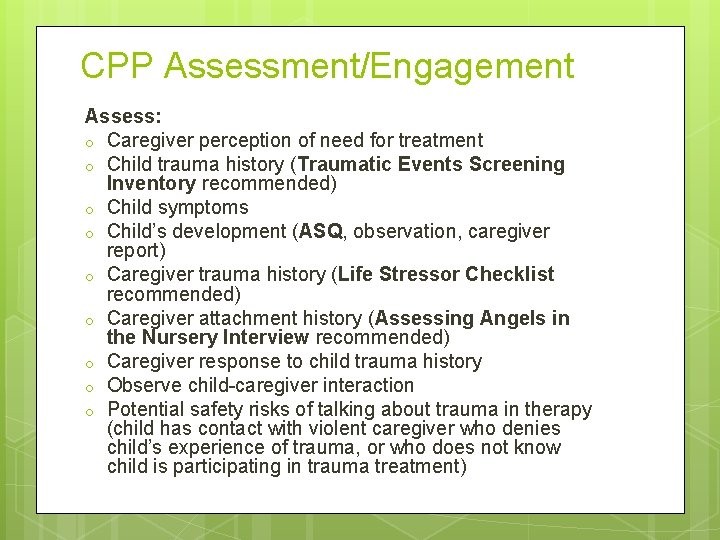
CPP Assessment/Engagement Assess: o Caregiver perception of need for treatment o Child trauma history (Traumatic Events Screening Inventory recommended) o Child symptoms o Child’s development (ASQ, observation, caregiver report) o Caregiver trauma history (Life Stressor Checklist recommended) o Caregiver attachment history (Assessing Angels in the Nursery Interview recommended) o Caregiver response to child trauma history o Observe child-caregiver interaction o Potential safety risks of talking about trauma in therapy (child has contact with violent caregiver who denies child’s experience of trauma, or who does not know child is participating in trauma treatment)
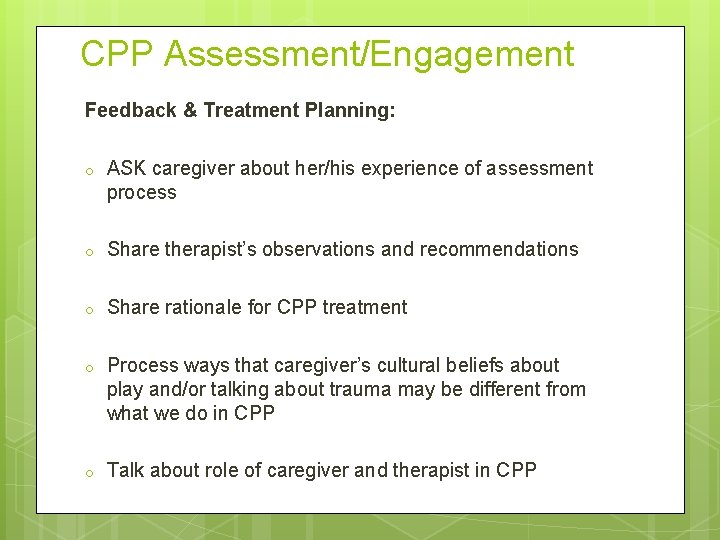
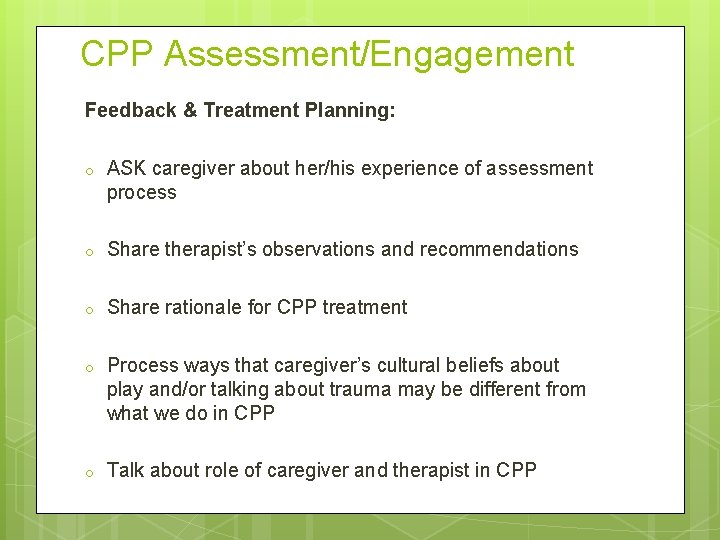
CPP Assessment/Engagement Feedback & Treatment Planning: o ASK caregiver about her/his experience of assessment process o Share therapist’s observations and recommendations o Share rationale for CPP treatment o Process ways that caregiver’s cultural beliefs about play and/or talking about trauma may be different from what we do in CPP o Talk about role of caregiver and therapist in CPP
CPP Assessment/Engagement Plan with caregiver how to introduce child to therapy: CPP triangle of explanations o Experience: “You saw…. . ” “You heard. . . ” o Behavior/Feelings: “And now you. . . ” o Therapy: ”This is a place where we can talk and play about scary things that happened, and you can learn what to do when you are mad. ”
CPP Interventions: WHAT Play: child-directed therapist play as “play translator” may be a way for child to express and/or process traumatic memories, or a developmentally appropriate way to explore the world and engage with parent
CPP Interventions: WHAT Putting feelings into words Protective Physical Contact (caregiver-child: clinician does not initiate but may respond to child as appropriate) Unstructured reflective developmental guidance Modeling appropriate protective behavior Insight-oriented interpretation Addressing traumatic reminders Trauma narrative (more process than product with young children) Retrieving benevolent memories (caregiver’s and child’s) Emotional support (for caregiver) Concrete assistance with problems of living
CPP Interventions: HOW Child-parent and/or individual parent sessions Flexible and responsive, not manualized and sequential Start with simplest and most direct: concrete assistance, developmental guidance Parallel process: supervisor-clinician-parentchild; empathic, reflective, supportive
CPP in a Family Shelter: Opportunities Homeless families very unlikely to access CPP or otherapy in traditional community settings Opportunity to offer treatment that may prevent child maltreatment to families at high risk, before maltreatment occurs Parents may be more open to help when they are in crisis CPP addresses both caregiver and child trauma
CPP in a Family Shelter: Challenges Parents likely focused on basic survival needs, not necessarily their own/their children’s mental/emotional health Variable, often short length of stay: CPP is NOT a short -term treatment (average length of treatment 18 months) High incidence and intensity of untreated childhood trauma among parents, leading to distorted perceptions of child development and child-parent relationships, normalization of traumatic experience, and difficulty building trust with therapist
Anecdotal Experience (17 months) Out of 16 families referred for CPP who engaged for at least 2 sessions/contacts: o 10 parents reported being in foster care as children o Of remaining 6, 5 reported significant attachment disruptions and/or maltreatment as children Near universal early attachment trauma among homeless parents: o Connection to homelessness o Risk for intergenerational transmission of trauma
Anecdotal Experience (17 months) 16 families referred for CPP and engaged for at least 2 sessions/contacts: 3 moved out of region during assessment/engagement phase 2 expressed interest in continuing after moving out of shelter, but did not (of these, one participated consistently for 4 months while in shelter) 1 accepted only support with accessing early childhood special education 1 has remained engaged for 7 months after moving into housing, but with challenges 2 currently engaged, still in shelter 7 terminated participation during or soon after assessment process
Lessons Learned Realistic Expectations: o Homelessness and shelter life are highly stressful o Safety and stabilization realistic while in shelter o Processing caregiver and/or child trauma, changing attachment patterns, restoring/establishing normal development may be more realistic goals after family has stable housing… BUT barriers to ongoing engagement o How does it make sense to measure outcomes/success? ? ? Improving vs. maintaining
Lessons Learned CPP flexibility to work individually with parents on their own trauma to support child -parent work is a good fit for homeless families. o Due to high levels of untreated trauma, many homeless parents need a high level of individual support o Trauma- and attachment-related issues make managing relationships with multiple clinicians challenging o Resource challenges may limit how many clinicians are available in shelter
Lessons Learned CPP principle of starting with simplest and most direct intervention means that “concrete assistance with problems of living” is often the best place to start… and it is often what homeless parents need and want! Clinician’s physical presence in the shelter makes it easier to respond flexibly when scheduled sessions are missed due to survival needs or crises, parent ambivalence, and/or time management issues.
Lessons Learned Need for increased flexibility in assessment process o Many parents who dropped out reported being triggered by assessment questions about trauma and attachment history o Some parents did not understand or buy into purpose of history questions, even with standard CPP explanation of rationale Possible solutions: o Explicitly offer parents choice of completing recommended assessment questionnaires or answering more general, open-ended questions about trauma and attachment history o When family is in crisis, begin using CPP interventions before completing assessment process
CPP in Milieu Settings Individual clinicians can implement CPP principles and interventions in any context, but challenges may arise if other staff in milieu operate on principles not compatible with CPP (examples? ) Non-clinical staff can learn and use CPP’s Principles of Early Child Development and five lenses in their roles, but training and ongoing reflective support take commitment, time, resources
CPP Training Learning Collaborative Model o Agency teams, not individual clinicians o Agency must demonstrate organizational readiness and commitment to sustainability o Supervisors and clinicians train together o Three two-day Learning Sessions and twice-monthly telephone-cased case consultations over 1 ½ year period o For further info: http: //childtrauma. ucsf. edu/child-parentpsychotherapy-training
Citations Lieberman and Van Horn, Psychotherapy with Infants and Young Children: Repairing the Effects of Stress and Trauma on Early Attachment, Guilford, 2008 Bassuk, E. L. , Weinreb, L. F. , Buckner, J. C. , Browne, A. , Salomon, A. , & Bassuk, S. S. (1996). The characteristics and needs of sheltered homeless and low-income housed mothers. Journal of the American Medical Association, 276(8), 640 -646 Bassuk, E. L. , Richard, M. , & Tsertsvadze, A. (2015). The prevalence of mental illness in homeless children: A systematic review and metaanalysis. Journal of the American Academy of Child and Adolescent Psychiatry, 54(2), 86 -96 National Scientific Council on the Developing Child (2005/2014). Excessive Stress Disrupts the Architecture of the Developing Brain: Working Paper No. 3. Updated Edition. Retrieved from www. developingchild. harvard. edu (Lieberman, Ippen, Van Horn, Don’t Hit My Mommy: A Manual for Child-Parent Psychotherapy With Young Children Exposed to Violence and Other Trauma, Second Edition, Zero To Three, 2015)
 Child parent psychotherapy triangle
Child parent psychotherapy triangle Kathryn barnard metaparadigma
Kathryn barnard metaparadigma Kathryn e barnard
Kathryn e barnard Proof of parent-child relationship letter sample
Proof of parent-child relationship letter sample Palin pci
Palin pci Disadvantages of single parent family
Disadvantages of single parent family Advantages and disadvantages of nuclear family
Advantages and disadvantages of nuclear family Binuclear family vs blended family
Binuclear family vs blended family Greek mythology family tree chaos
Greek mythology family tree chaos Difference between guidance and counseling
Difference between guidance and counseling Andrew pethebridge
Andrew pethebridge Token economy in psychology
Token economy in psychology Types of individual psychotherapy
Types of individual psychotherapy Introduction to psychotherapy ppt
Introduction to psychotherapy ppt Bracketing therapy
Bracketing therapy Dodo bird conjecture
Dodo bird conjecture General issues in psychotherapy
General issues in psychotherapy Carl rogers theory
Carl rogers theory Psychotherapy refers to
Psychotherapy refers to Sadaf sajjad
Sadaf sajjad Counselling ppt
Counselling ppt Quantum psychotherapy
Quantum psychotherapy Cognitive disputation
Cognitive disputation Common factors approach psychotherapy integration
Common factors approach psychotherapy integration Types of psychotherapy
Types of psychotherapy Advanced psychotherapy
Advanced psychotherapy Psychotherapy examples
Psychotherapy examples Limitations of psychotherapy
Limitations of psychotherapy Scope of psychotherapy
Scope of psychotherapy What is the solid object relationship model
What is the solid object relationship model Dcpsych
Dcpsych World council for psychotherapy
World council for psychotherapy 이진트리 복사 순회
이진트리 복사 순회 What is a cft
What is a cft Child, youth and family services act, 2017
Child, youth and family services act, 2017 Effect of hospitalization on the family of the child
Effect of hospitalization on the family of the child Cert 4 child youth and family intervention
Cert 4 child youth and family intervention Rocky bay family services
Rocky bay family services Southeast cfs
Southeast cfs Child family investigator colorado
Child family investigator colorado Lorain county children services
Lorain county children services