Implementation of Appropriate Use Criteria in the Cath


- Slides: 37
Implementation of Appropriate Use Criteria in the Cath Lab Theodore A Bass, MD MSCAI, FACC Professor of Medicine and Chief Cardiology University of Florida-Jax
Ted Bass, MD I have no relevant financial relationships Past President SCAI Thank you SCAI Quality Team Leadership Kalon Ho, MD Sunil Rao, MD
Implementation of Appropriate Use Criteria in the Cath Lab Why is this Important? Quality Initiatives are Imperative
Since the specialty’s earliest days, Interventional Cardiology has been at the forefront of self-assessment and quality improvement. • A leader in randomized clinical trials • At the forefront of registry-based data collection and analysis

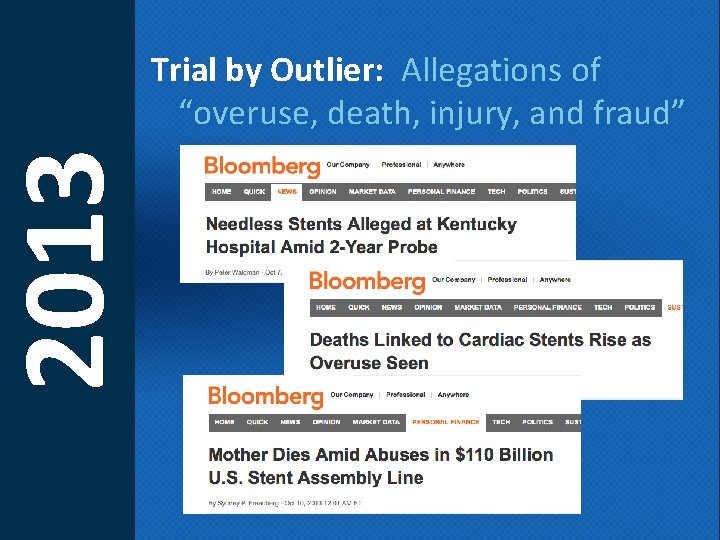
2006 -2012 Six years of troubling headlines, Concerns regarding safety, device (stent) overuse, cost
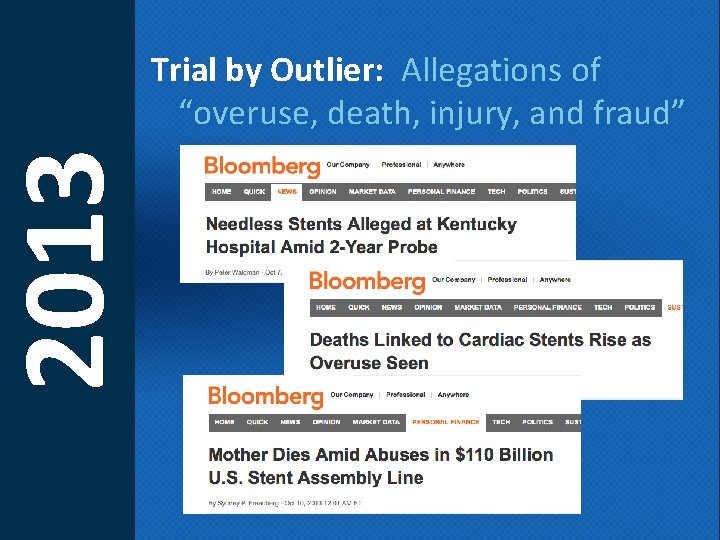
2013 Trial by Outlier: Allegations of “overuse, death, injury, and fraud”
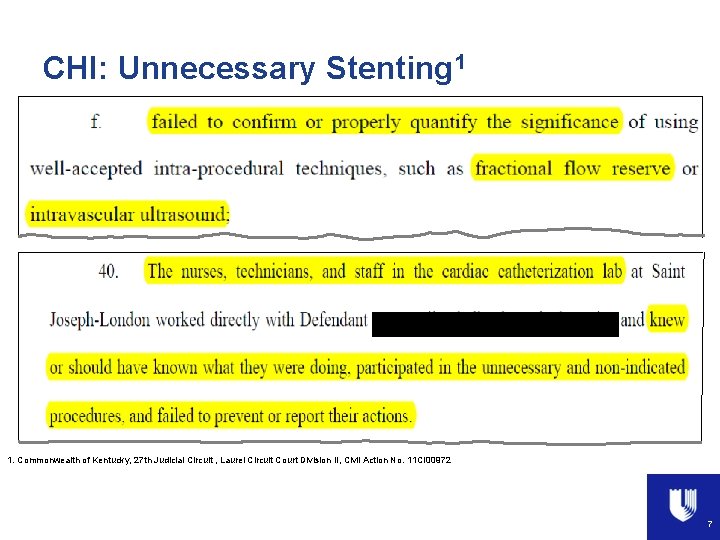
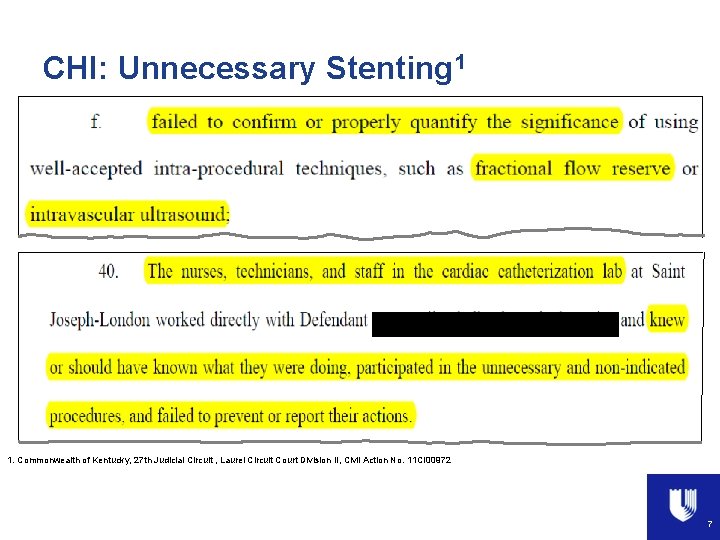
CHI: Unnecessary Stenting 1 1. Commonwealth of Kentucky, 27 th Judicial Circuit , Laurel Circuit Court Division II, Civil Action No. 11 CI 00972 601 -0100. 20/001 7
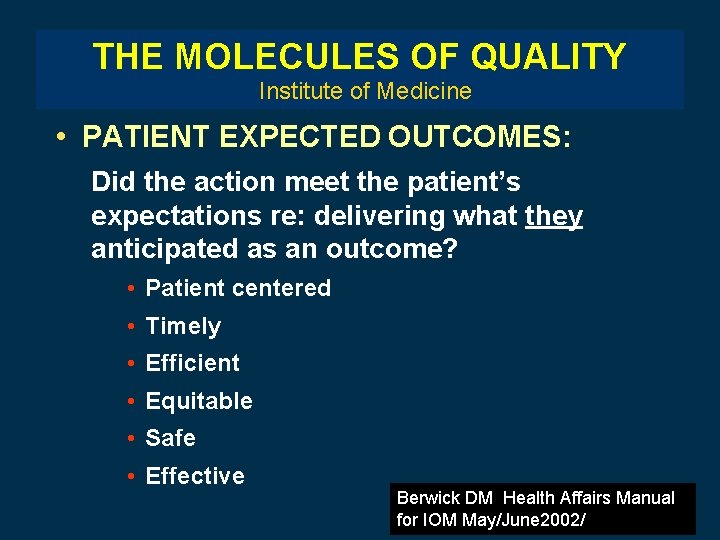
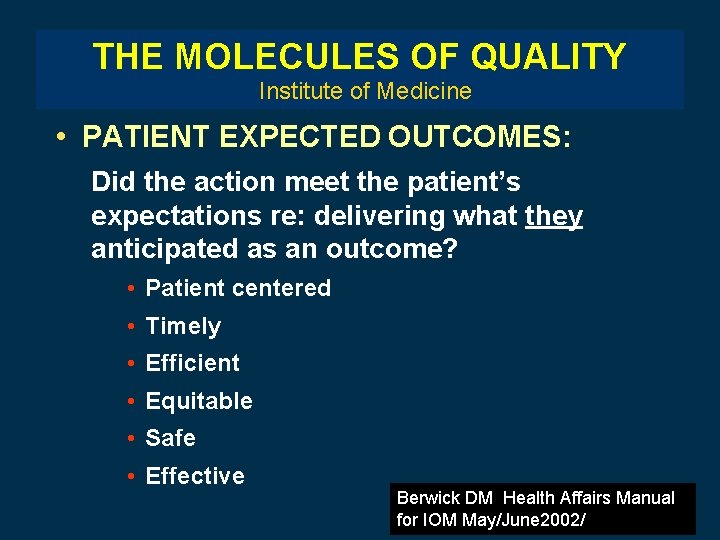
THE MOLECULES OF QUALITY Institute of Medicine • PATIENT EXPECTED OUTCOMES: Did the action meet the patient’s expectations re: delivering what they anticipated as an outcome? • Patient centered • Timely • Efficient • Equitable • Safe • Effective Berwick DM Health Affairs Manual for IOM May/June 2002/
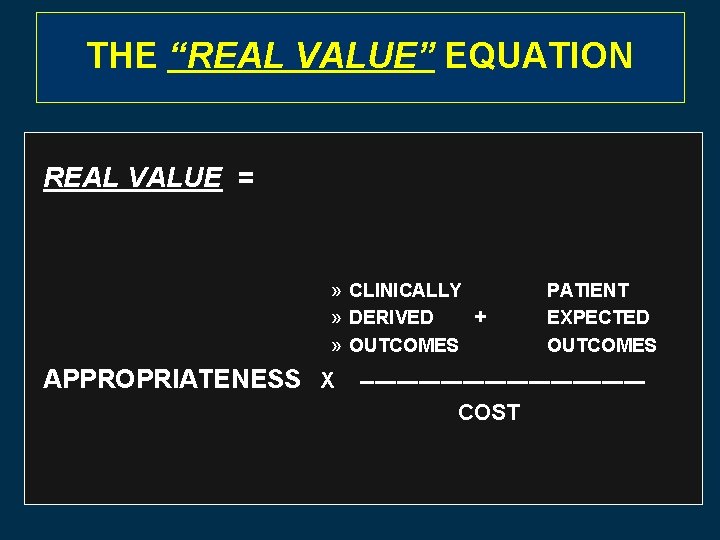
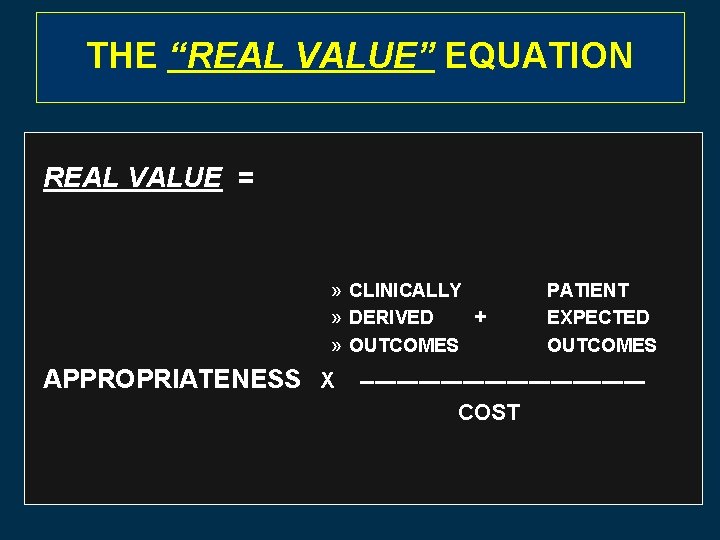
THETHE “REAL VALUE” EQUATION REAL VALUE = QUALITY VALUE =» CLINICALLY -----» DERIVED + COST » OUTCOMES PATIENT EXPECTED OUTCOMES APPROPRIATENESS X -------------------COST
n Quality care is our obligation n Quality care is recognized by payers n Use of available tools can improve quality n Ongoing efforts to provide financial premiums (or penalties) for quality care may further increase incentivize the use of QI tools
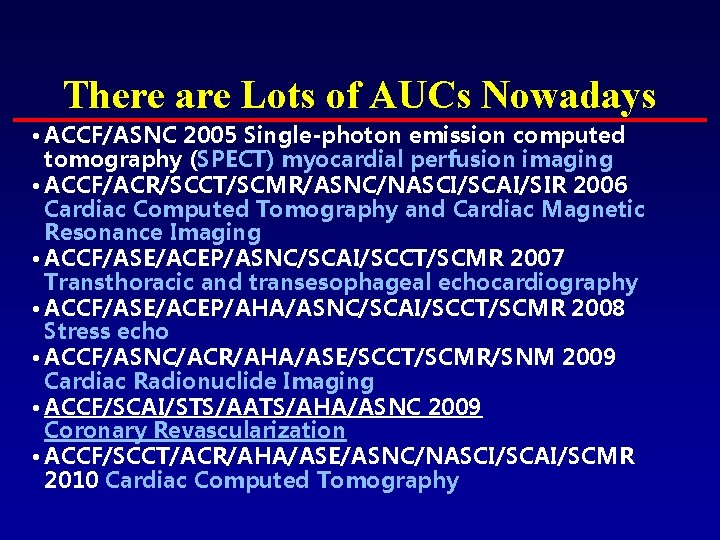
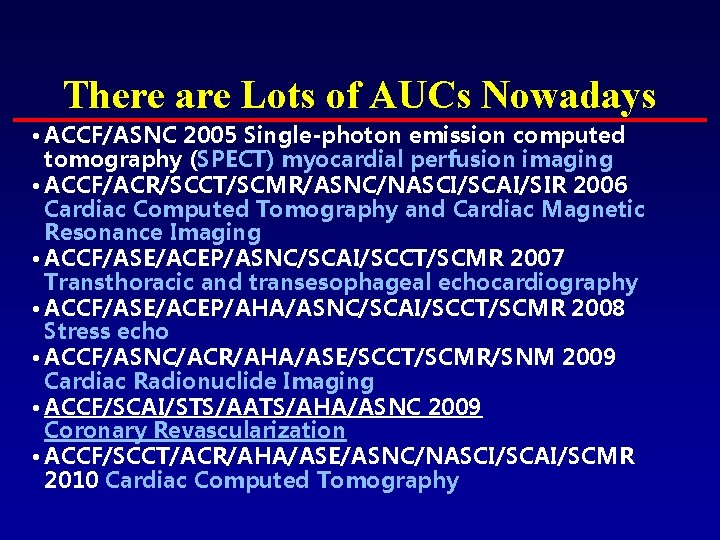
There are Lots of AUCs Nowadays • ACCF/ASNC 2005 Single-photon emission computed tomography (SPECT) myocardial perfusion imaging • ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 Cardiac Computed Tomography and Cardiac Magnetic Resonance Imaging • ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 Transthoracic and transesophageal echocardiography • ACCF/ASE/ACEP/AHA/ASNC/SCAI/SCCT/SCMR 2008 Stress echo • ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Cardiac Radionuclide Imaging • ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Coronary Revascularization • ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Cardiac Computed Tomography
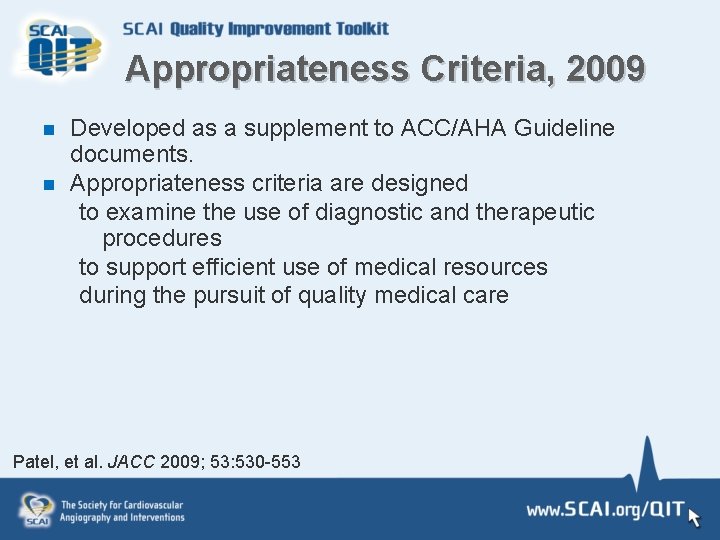
Appropriateness Criteria, 2009 n n Developed as a supplement to ACC/AHA Guideline documents. Appropriateness criteria are designed to examine the use of diagnostic and therapeutic procedures to support efficient use of medical resources during the pursuit of quality medical care Patel, et al. JACC 2009; 53: 530 -553
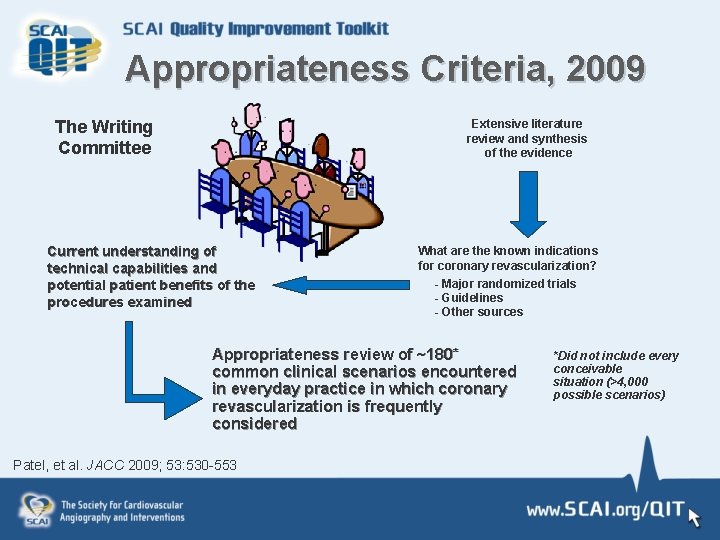
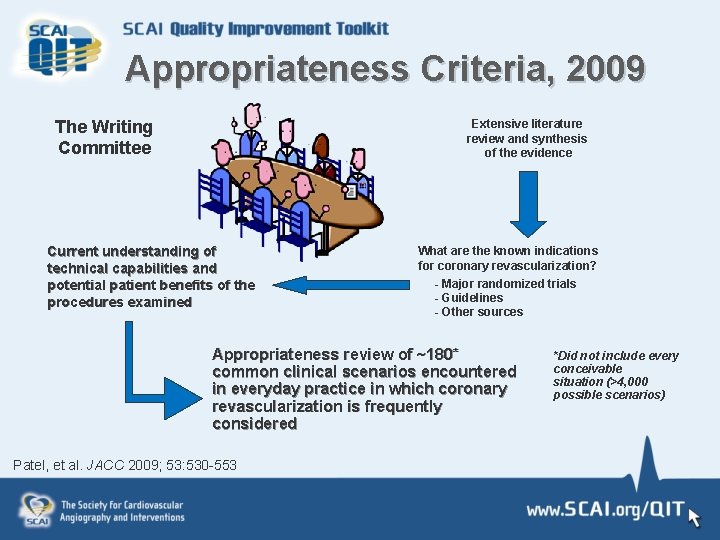
Appropriateness Criteria, 2009 The Writing Committee Extensive literature review and synthesis of the evidence Current understanding of technical capabilities and potential patient benefits of the procedures examined What are the known indications for coronary revascularization? - Major randomized trials - Guidelines - Other sources Appropriateness review of ~180* common clinical scenarios encountered in everyday practice in which coronary revascularization is frequently considered Patel, et al. JACC 2009; 53: 530 -553 *Did not include every conceivable situation (>4, 000 possible scenarios)
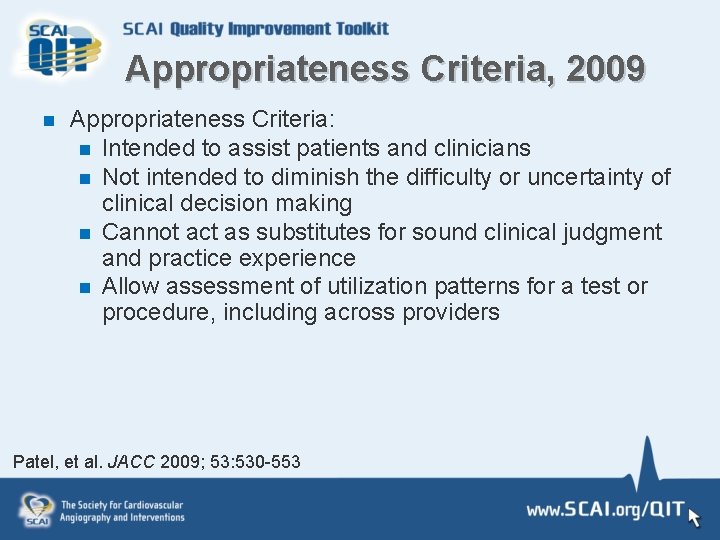
Appropriateness Criteria, 2009 n Appropriateness Criteria: n Intended to assist patients and clinicians n Not intended to diminish the difficulty or uncertainty of clinical decision making n Cannot act as substitutes for sound clinical judgment and practice experience n Allow assessment of utilization patterns for a test or procedure, including across providers Patel, et al. JACC 2009; 53: 530 -553
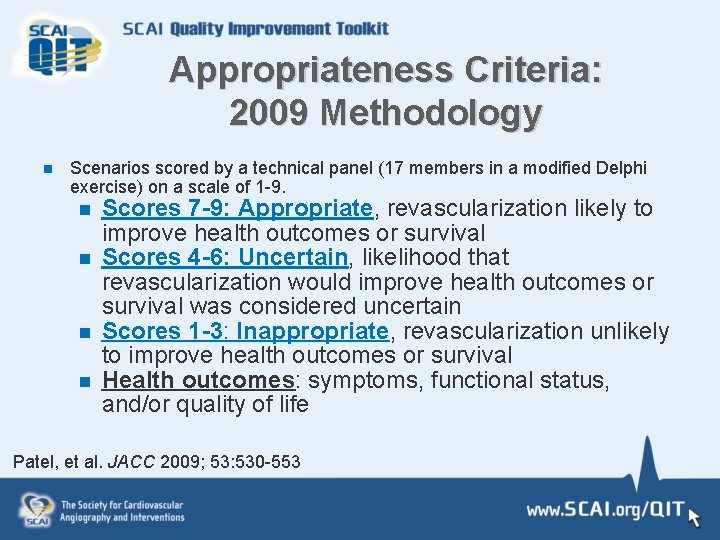
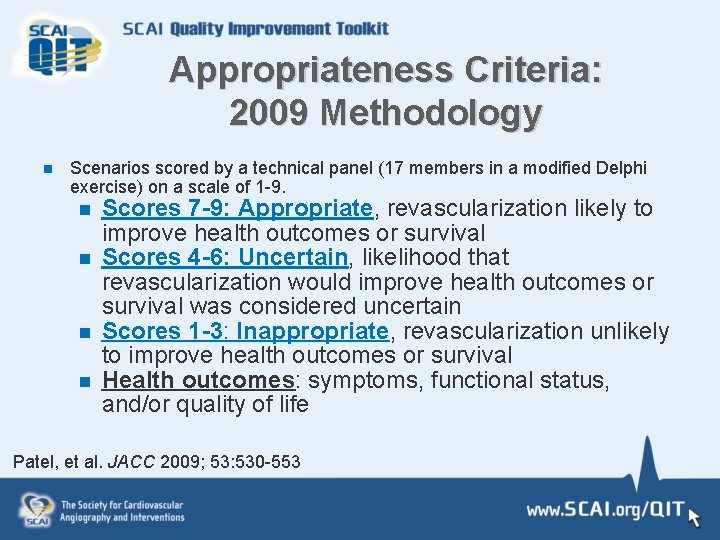
Appropriateness Criteria: 2009 Methodology n Scenarios scored by a technical panel (17 members in a modified Delphi exercise) on a scale of 1 -9. n Scores 7 -9: Appropriate, revascularization likely to n n n improve health outcomes or survival Scores 4 -6: Uncertain, likelihood that revascularization would improve health outcomes or survival was considered uncertain Scores 1 -3: Inappropriate, revascularization unlikely to improve health outcomes or survival Health outcomes: symptoms, functional status, and/or quality of life Patel, et al. JACC 2009; 53: 530 -553
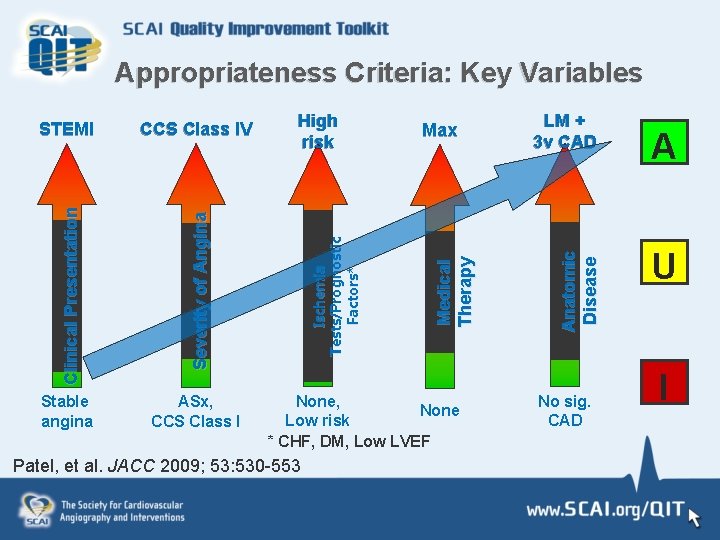
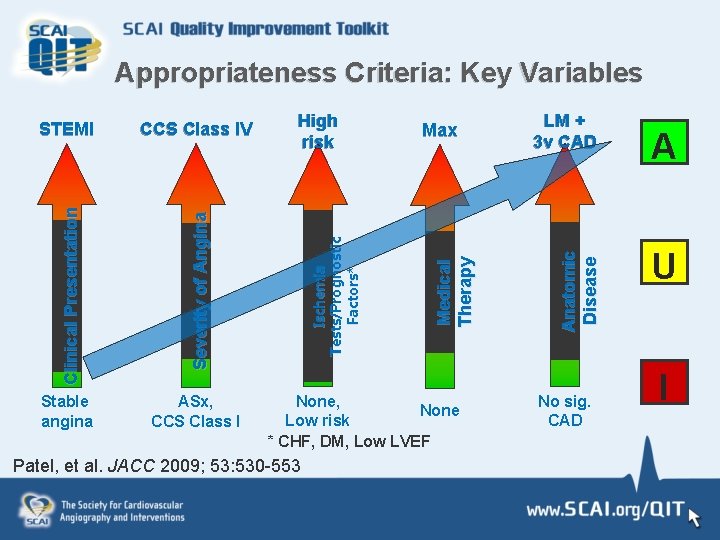
ASx, CCS Class I Max None, None Low risk * CHF, DM, Low LVEF Patel, et al. JACC 2009; 53: 530 -553 LM + 3 v CAD A n a to m i c Di sease S e v e r i ty o f A n g i n a Stable angina High risk Me d i c a l T h erap y CCS Class IV I s c h em i a T es t s / P r o g n o s t i c F a c to r s * STEMI C l i n i c a l P r e s e n ta ti o n Appropriateness Criteria: Key Variables No sig. CAD A U I
Appropriate Use Criteria for Coronary Revascularization Focused Update 2012 Endorsed by:
AUC 2012 n n Reassessment of clinical scenarios felt to be affected by significant changes in the medical literature or gaps from prior criteria A practical standard upon which to assess and better understand variability in the use of cardiovascular procedures Patel, et al. JACC 2012; 59:
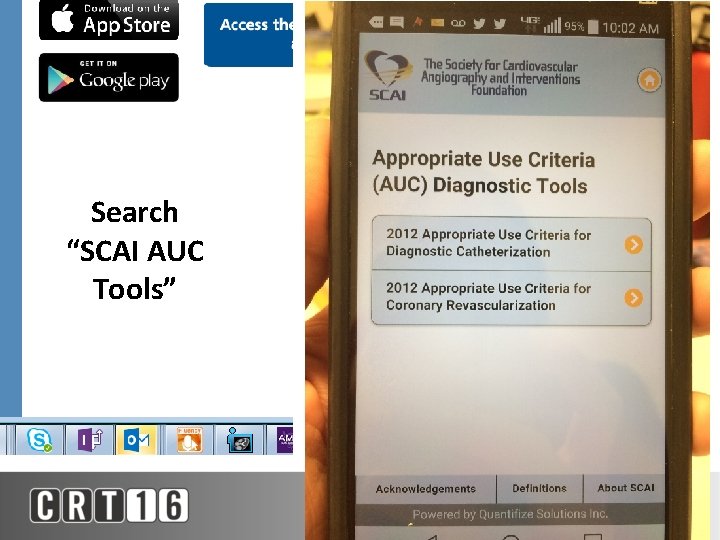
Search “SCAI AUC Tools”
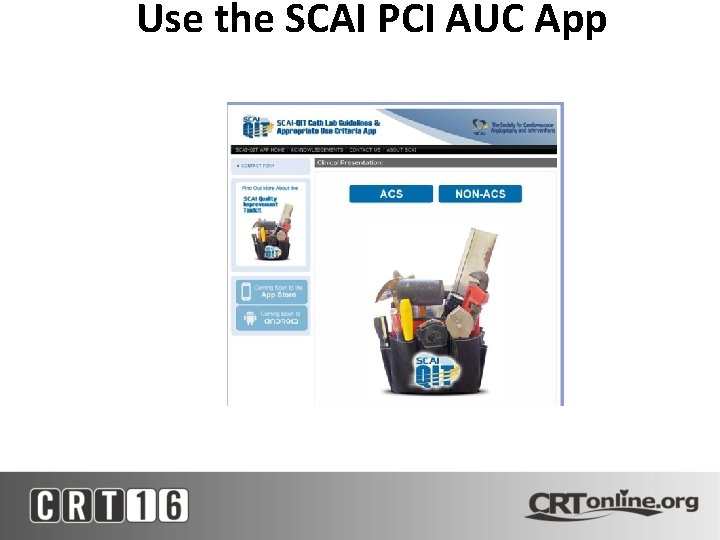
Use the SCAI PCI AUC App
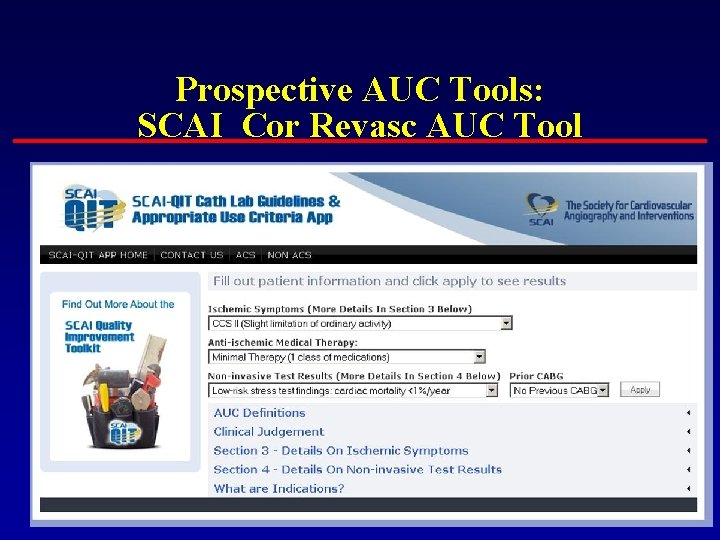
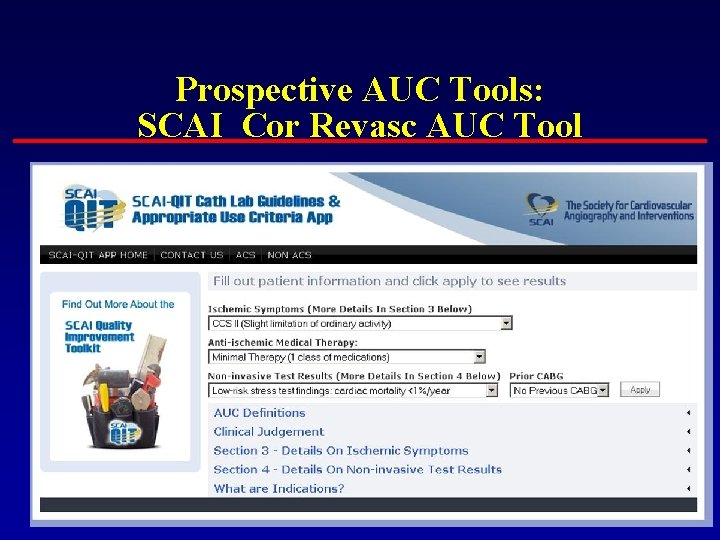
Prospective AUC Tools: SCAI Cor Revasc AUC Tool
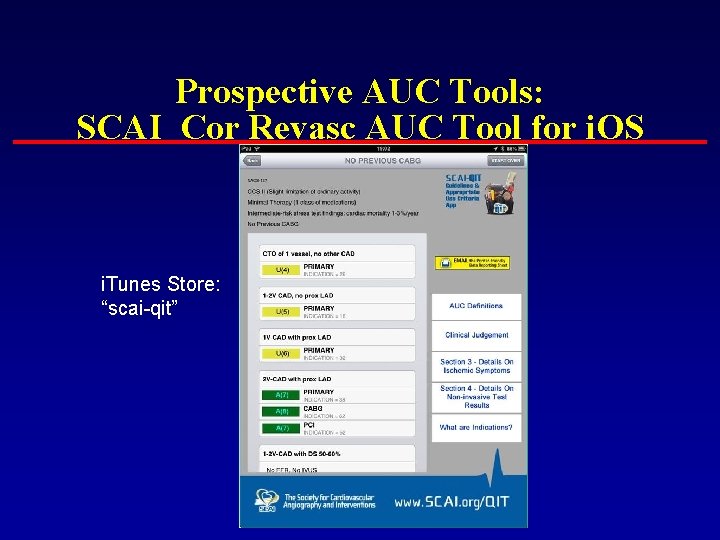
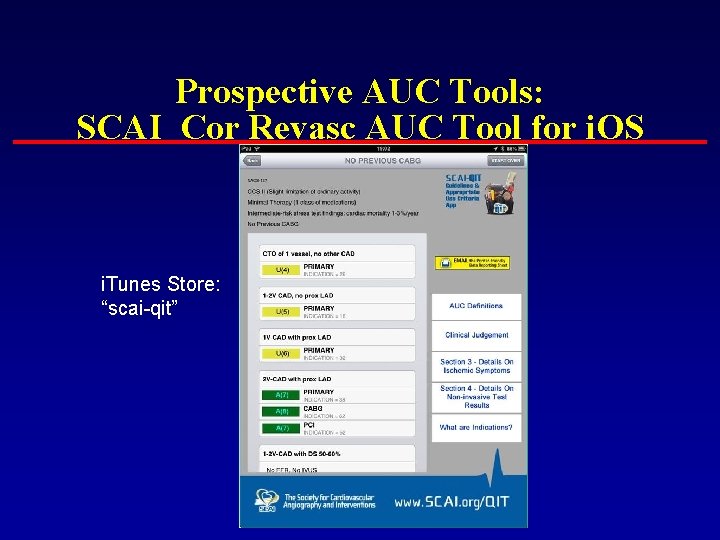
Prospective AUC Tools: SCAI Cor Revasc AUC Tool for i. OS i. Tunes Store: “scai-qit”
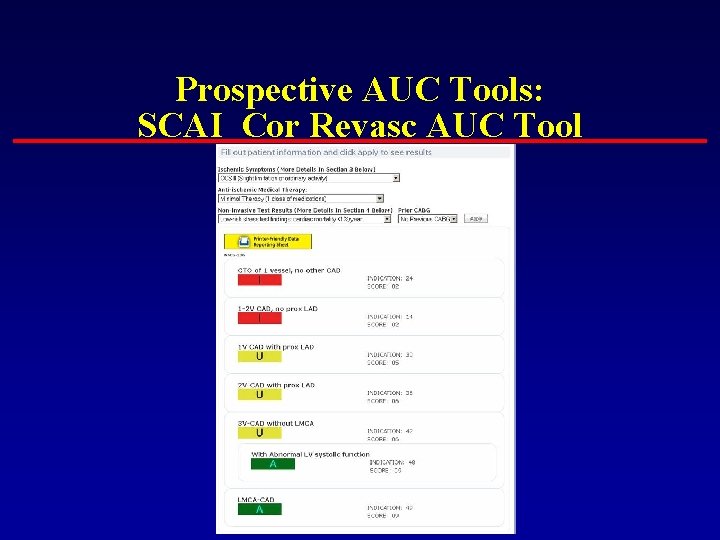
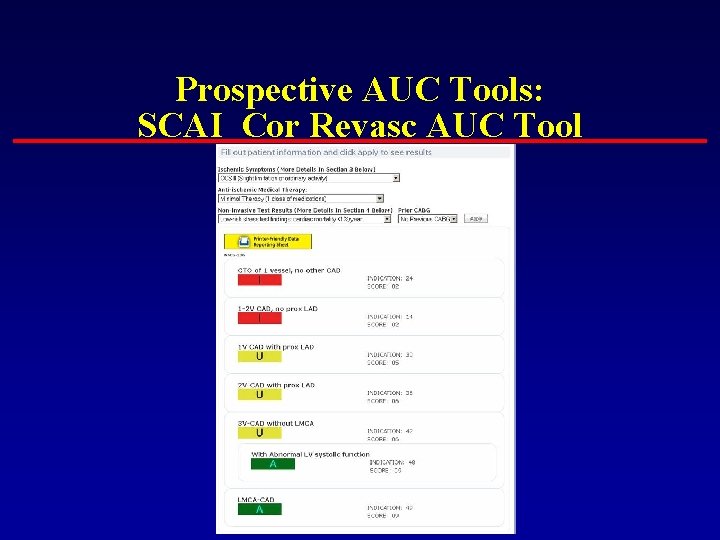
Prospective AUC Tools: SCAI Cor Revasc AUC Tool
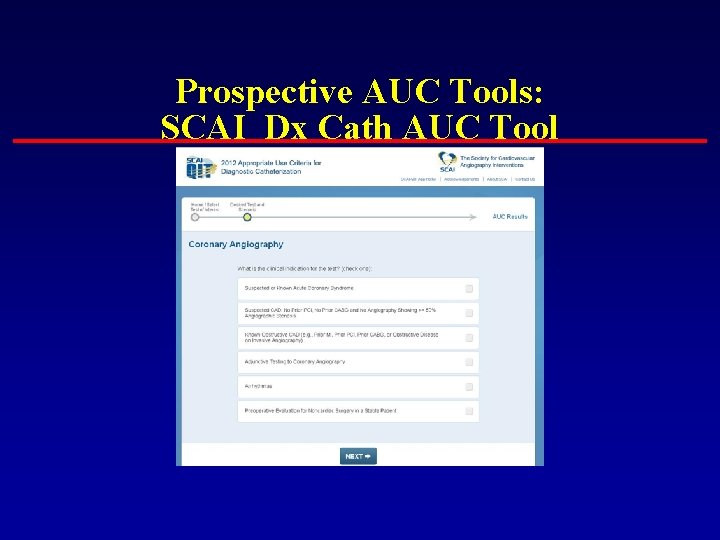
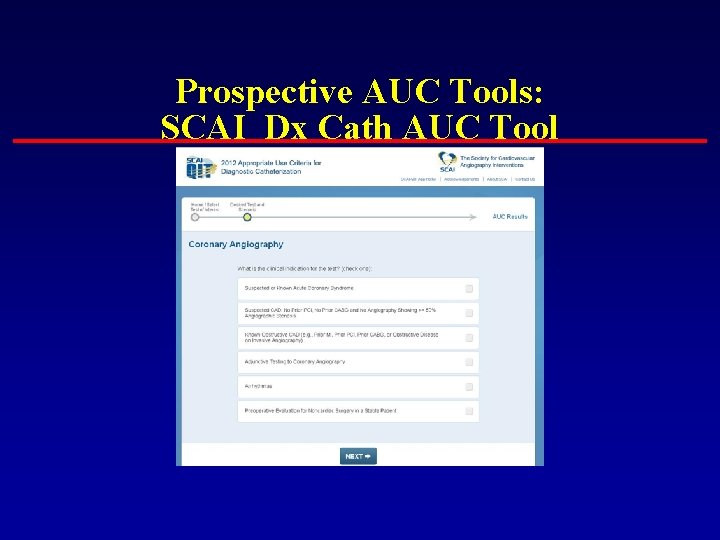
Prospective AUC Tools: SCAI Dx Cath AUC Tool
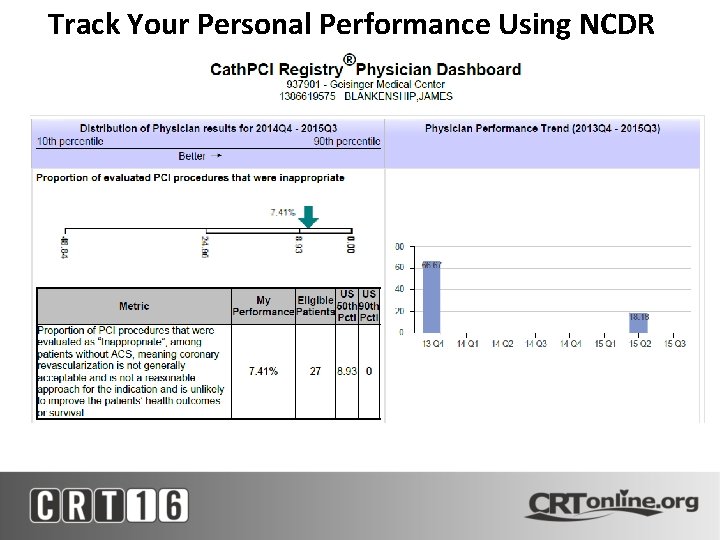
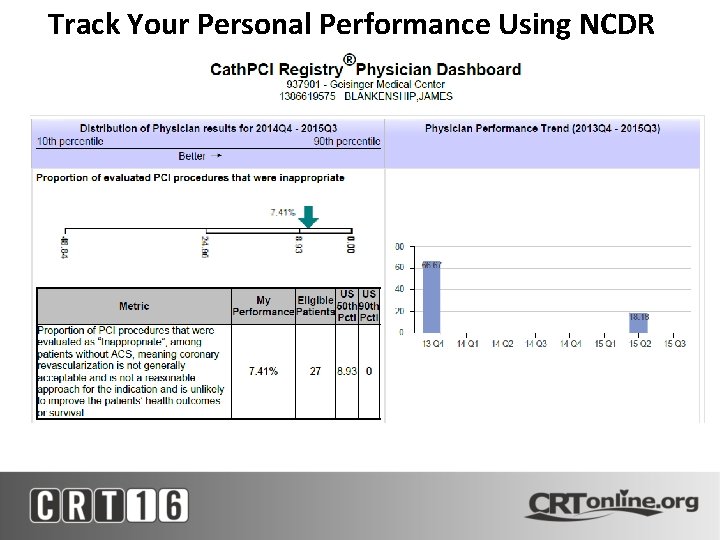
Track Your Personal Performance Using NCDR
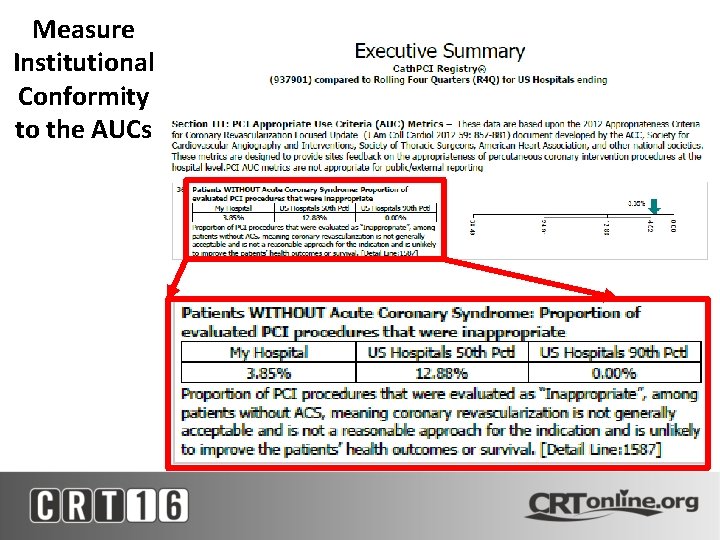
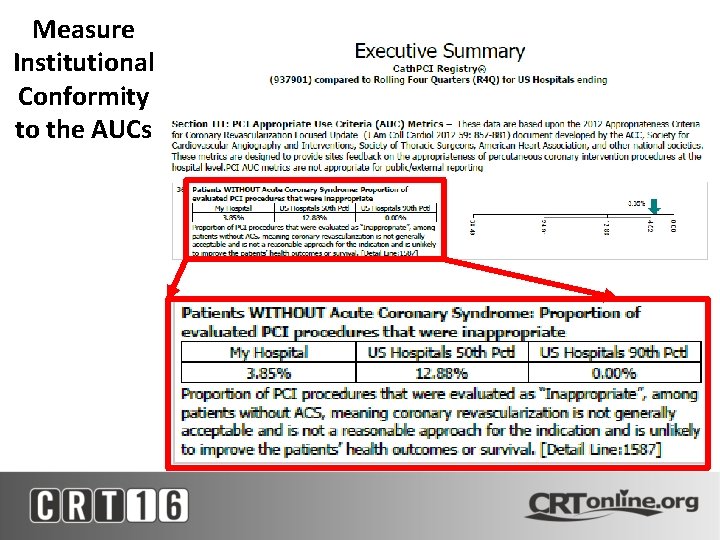
Measure Institutional Conformity to the AUCs
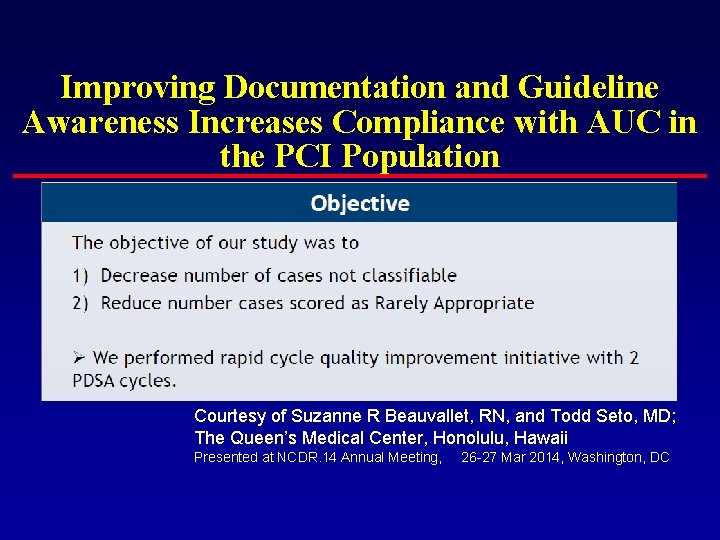
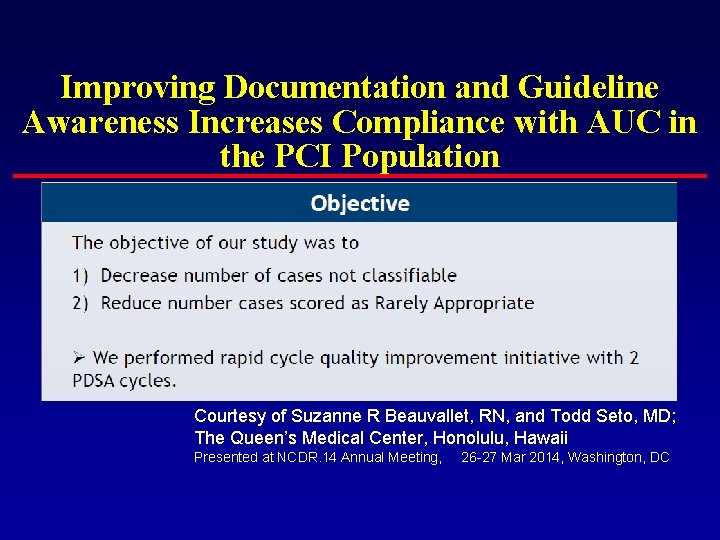
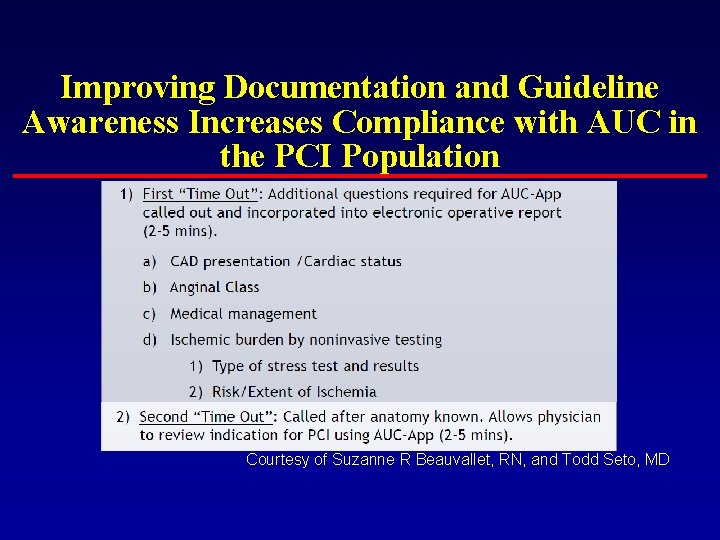
Improving Documentation and Guideline Awareness Increases Compliance with AUC in the PCI Population Courtesy of Suzanne R Beauvallet, RN, and Todd Seto, MD; The Queen’s Medical Center, Honolulu, Hawaii Presented at NCDR. 14 Annual Meeting, 26 -27 Mar 2014, Washington, DC
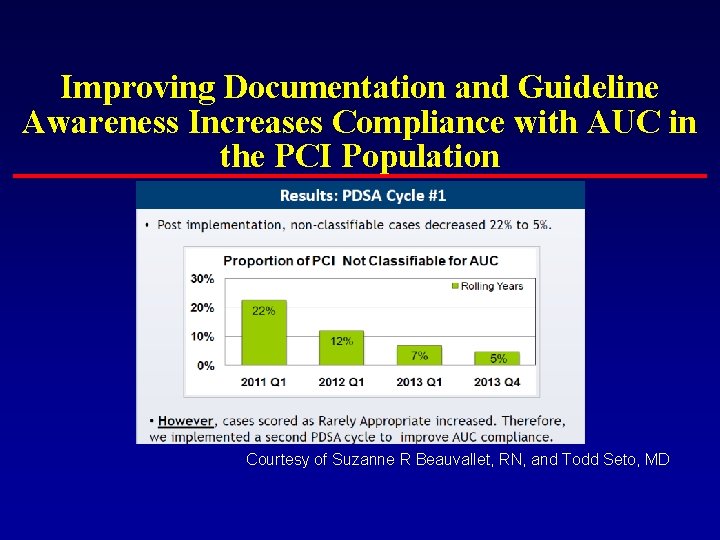
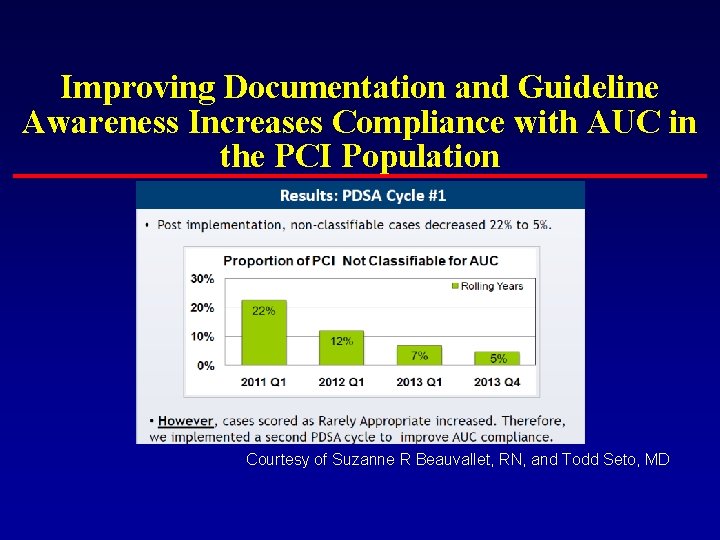
Improving Documentation and Guideline Awareness Increases Compliance with AUC in the PCI Population Courtesy of Suzanne R Beauvallet, RN, and Todd Seto, MD
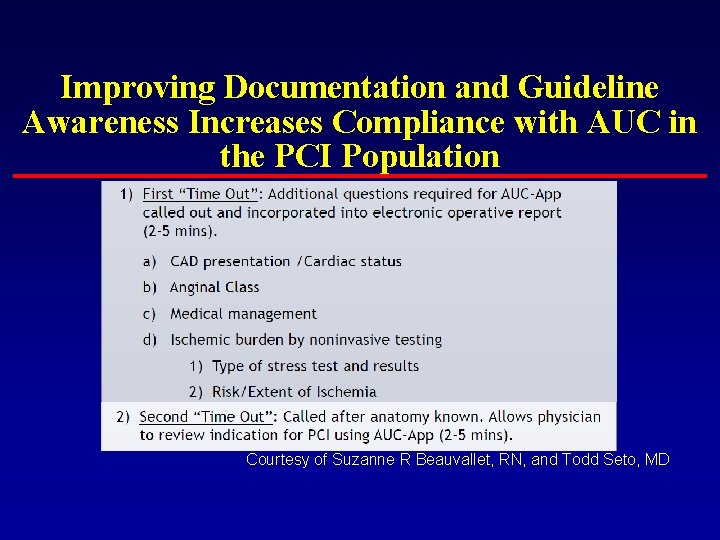
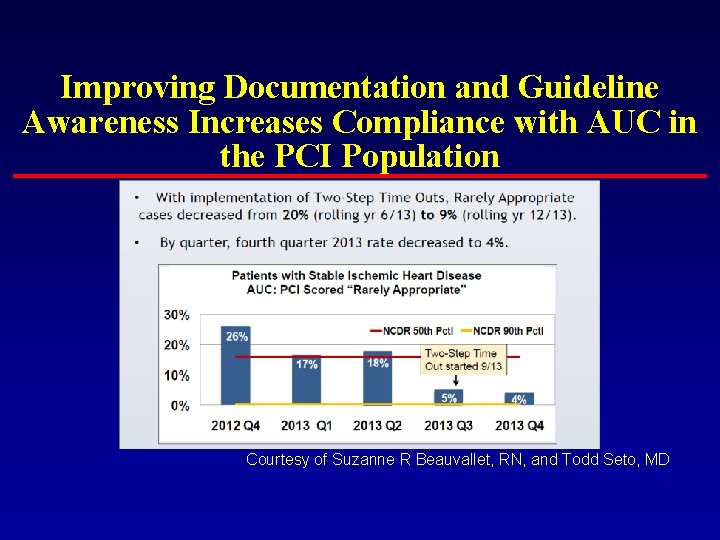
Improving Documentation and Guideline Awareness Increases Compliance with AUC in the PCI Population Courtesy of Suzanne R Beauvallet, RN, and Todd Seto, MD
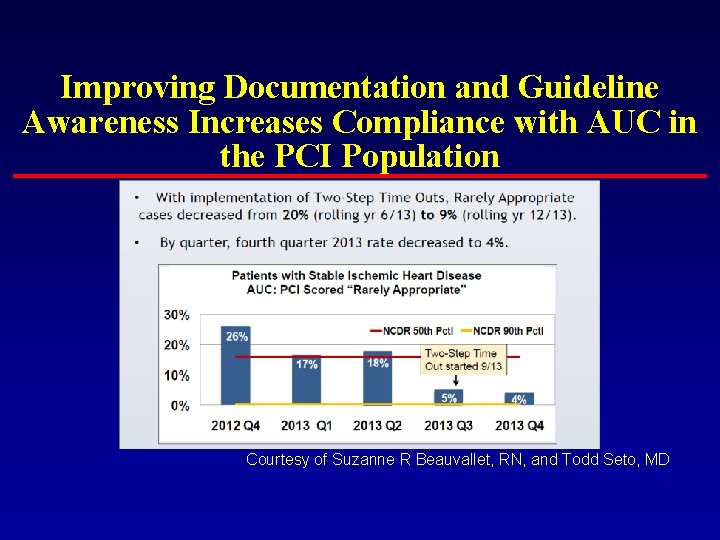
Improving Documentation and Guideline Awareness Increases Compliance with AUC in the PCI Population Courtesy of Suzanne R Beauvallet, RN, and Todd Seto, MD
AUC 2012: In a Nutshell n There may be clinical situations in which a use of coronary revascularization for an indication considered to be appropriate does not always represent reasonable practice, such that the benefit of the procedure does not outweigh the risks. Patel, et al. JACC 2012; 59:
AUC 2012: In a Nutshell n The rating of a revascularization indication as inappropriate or uncertain should not preclude a provider from performing revascularization procedures when there are patient- and condition-specific data to support that decision. Indeed, this may reflect optimal clinical care, if supported by mitigating patient characteristics. Patel, et al. JACC 2012; 59:
AUC 2012: In a Nutshell n Uncertain indications require individual physician judgment and understanding of the patient to better determine the usefulness of revascularization for a particular scenario. The ranking of uncertain (4 to 6) should not be viewed as excluding the use of revascularization for such patients. Patel, et al. JACC 2012; 59:
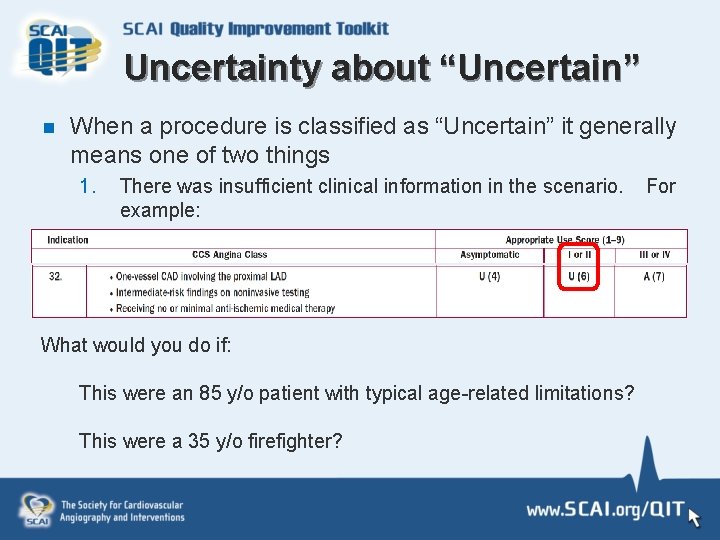
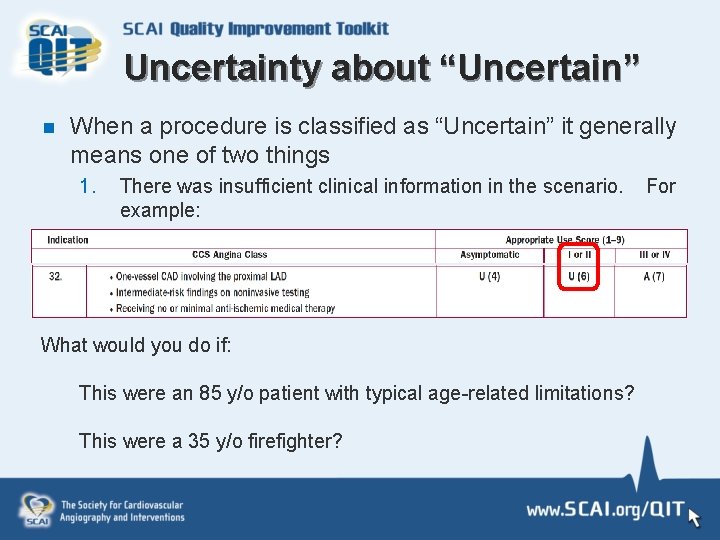
Uncertainty about “Uncertain” n When a procedure is classified as “Uncertain” it generally means one of two things 1. There was insufficient clinical information in the scenario. example: What would you do if: This were an 85 y/o patient with typical age-related limitations? This were a 35 y/o firefighter? For
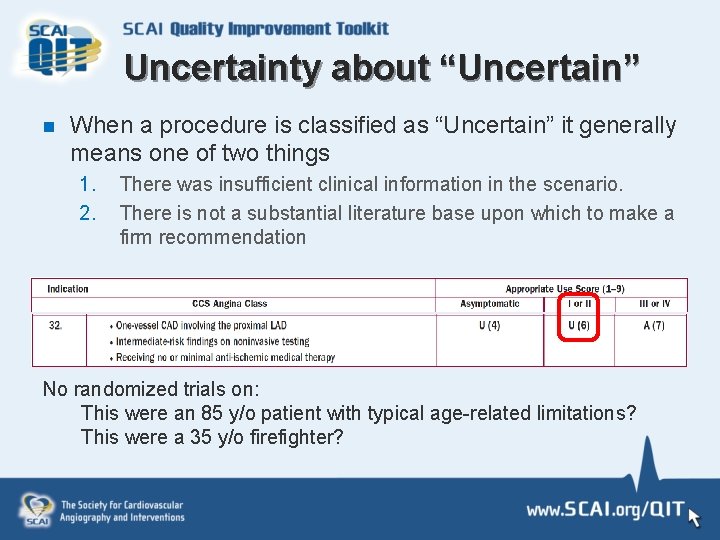
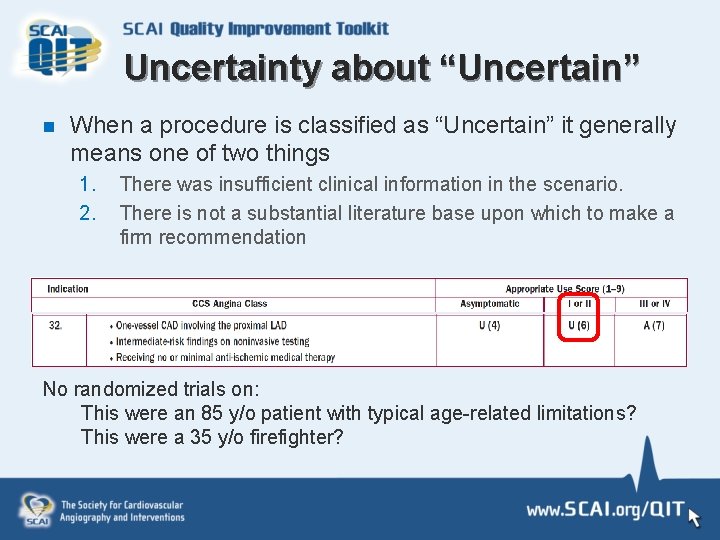
Uncertainty about “Uncertain” n When a procedure is classified as “Uncertain” it generally means one of two things 1. 2. There was insufficient clinical information in the scenario. There is not a substantial literature base upon which to make a firm recommendation No randomized trials on: This were an 85 y/o patient with typical age-related limitations? This were a 35 y/o firefighter?