Implementation of a Colorectal Cancer Screening Program in

![Diffusion of Innovation Model Rogers, E. M. (1983). Diffusion of Innovation Model [Digital image]. Diffusion of Innovation Model Rogers, E. M. (1983). Diffusion of Innovation Model [Digital image].](https://slidetodoc.com/presentation_image_h2/b759dad0d7af9b970630271a40c9b32f/image-15.jpg)
![Diffusion of Innovation Adopter Categories Kaminski, J. (2016). Diffusion of Innovation Theory. [Digital image] Diffusion of Innovation Adopter Categories Kaminski, J. (2016). Diffusion of Innovation Theory. [Digital image]](https://slidetodoc.com/presentation_image_h2/b759dad0d7af9b970630271a40c9b32f/image-16.jpg)
- Slides: 28
Implementation of a Colorectal Cancer Screening Program in a Rural Upper Midwest Federally Qualified Health Center: An Evidence Based Project Kayla M. Abrahamson, RN, BSN, FNP-S & Mc. Kenzie R. Peterson, RN, BSN, FNP-S University of Mary Project Chair: Dr. Billie Madler 2 nd Reader: Dr. Annie Gerhardt
Problem Identification • Colorectal cancer (CRC) - 2 nd leading cause of cancerrelated deaths • Risk starts increasing at age 40 and drastically rises at age 50 • Healthy People 2020 goal: >70% screening for those eligible • ND ranked 42 nd out of 51 in CRCS rates • CRC is preventable with routine screening • Estimated 50, 000+ deaths a year related to CRC • >60% are preventable ACS, 2014; CDC, 2016
Proposed Solution/PICO Question How does the implementation of a CRC screening program in a Midwestern, rural healthcare system impact screening and surveillance rates as compared to screening and surveillance rates prior to this program?
Literature Search Databases searched • • • Keywords utilized Cochrane Database of Systematic Reviews Academic Search Premier CINAHL Pub. Med National Guideline Clearinghouse MEDLINE • • colorectal cancer and screening colorectal cancer and surveillance colorectal cancer and screening program colorectal cancer screening and quality improvement colorectal cancer screening colorectal cancer surveillance colorectal cancer and prevention Limiters • • • 10 years Academic or Peer-Reviewed Journals English Language United States Adults - 19 -79 years of age
Literature Synthesis • Themes – Colorectal Cancer Screening (CRCS) Methods – Barriers to CRCS – CRCS screening program recommendations
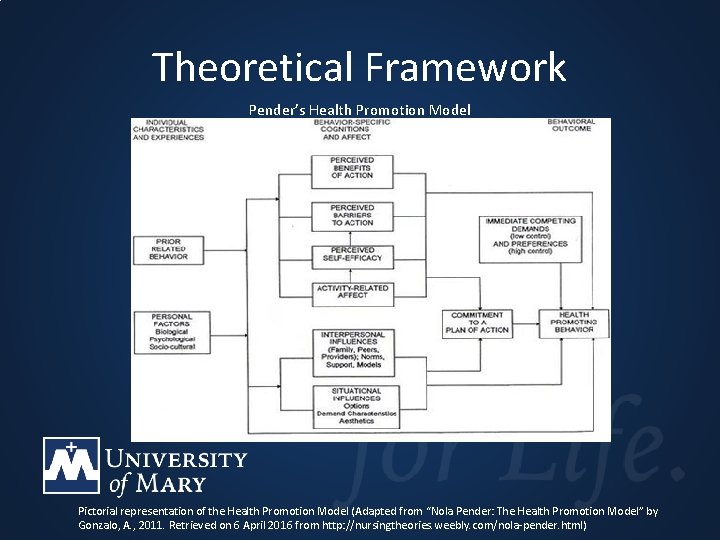
Theoretical Framework • Pender’s Health Promotion Model – Social Cognitive Theory – The Expectancy Value Theory – Centers around health behavior and the influence personal experience has on health Heydari & Khorashadizadeh, 2014; Pender, 2011; Peterson & Bredow, 2013
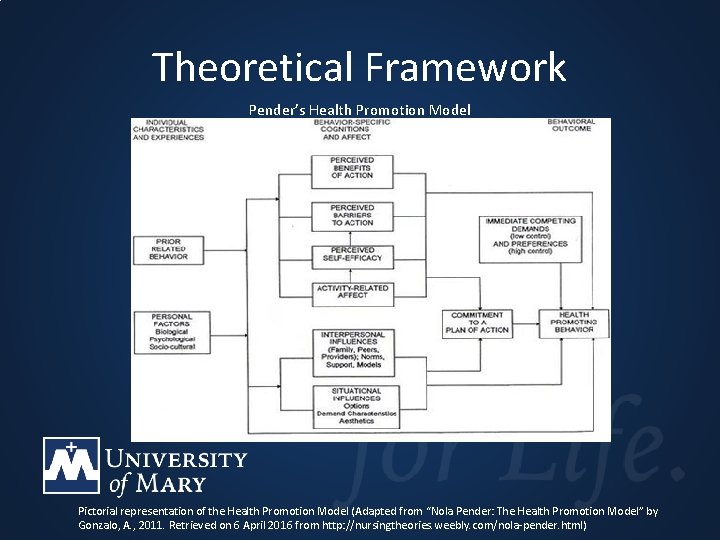
Theoretical Framework Pender’s Health Promotion Model Pictorial representation of the Health Promotion Model (Adapted from “Nola Pender: The Health Promotion Model” by Gonzalo, A. , 2011. Retrieved on 6 April 2016 from http: //nursingtheories. weebly. com/nola-pender. html)

Project Recommendation #1 • Clinical policy and procedure development and implementation • Includes a screening algorithm • “Academic Detailing” Cole et al. , 2015; Corey et al. , 2009; Davis et al. , 2013; Sarfaty, 2008
Project Recommendation #2 • Optimize the EMR to support improved CRCS rates – Documentation protocol – Patient reminder system – Clinical Decision Support Rule – Surveillance Protocol Atlas et al. , 2014; Berkowitz et al. , 2015; Cole, Esplin, & Baldwin, 2015; Geller et al. , 2008; Green et al. , 2013; Kern, Edwards, & Kaushal, 2014; Levy et al. , 2013
Project Recommendation #3 • Clinical Navigation – Workflow analysis to identify staff available to assist in navigation – Navigation involves tracking CRCS – Patient reminder letter Green et al. , 2013; Levy et al. , 2013
Project Recommendation #4 • CRCS Outreach Events – Patient outreach letters – Flu/FIT campaign – FIT cards in place of FOBT Berkowitz et al. , 2015; Cole et al. , 2015; Daly et al. , 2010; Escoffrey et al. , 2014; Green et al. , 2013; Kern, Edwards, & Kaushal, 2014; Lee et al. , 2014; Levy et al. , 2013; Potter et al. , 2013; Xu et al. , 2015
Knowledge Translation • Needs Assessment – Population – Stakeholders – SWOT
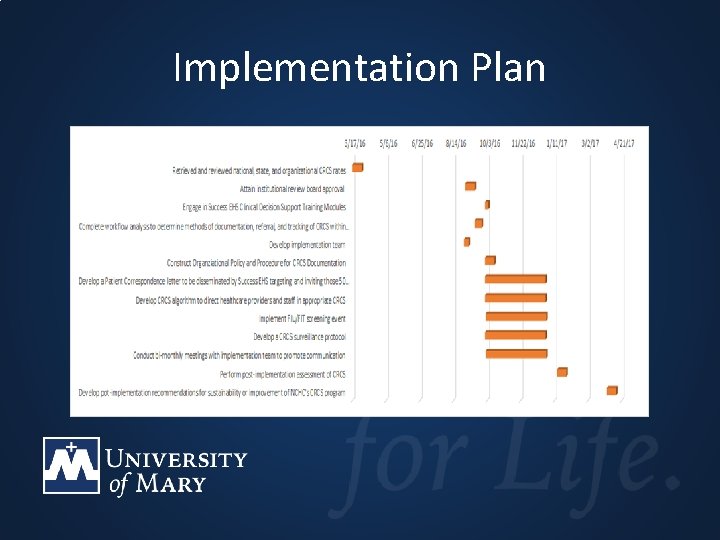
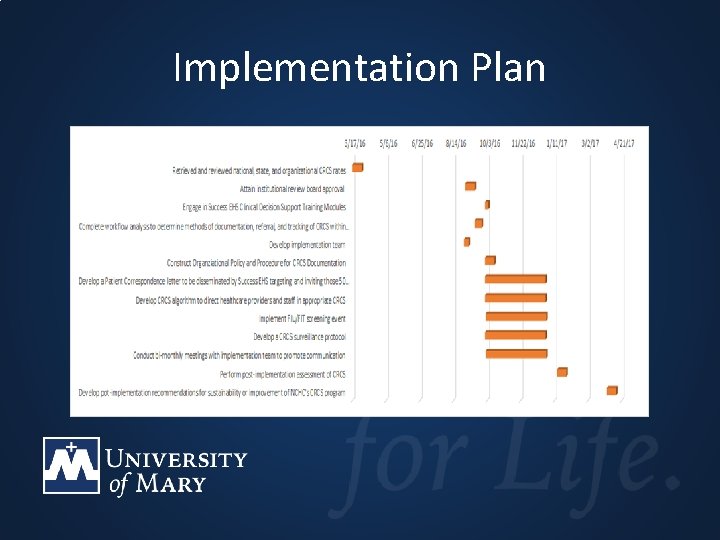
Implementation Plan
Change Theory • • Diffusion of Innovation Published by Everett Rogers in 1962 4 Concepts of Innovation is a 5 Step Process – – – Knowledge Persuasion Decision Implementation Confirmation (Kaminski, 2016; Rogers, 1983, Sanson-Fischer, 2004)
![Diffusion of Innovation Model Rogers E M 1983 Diffusion of Innovation Model Digital image Diffusion of Innovation Model Rogers, E. M. (1983). Diffusion of Innovation Model [Digital image].](https://slidetodoc.com/presentation_image_h2/b759dad0d7af9b970630271a40c9b32f/image-15.jpg)
Diffusion of Innovation Model Rogers, E. M. (1983). Diffusion of Innovation Model [Digital image]. Retrieved June 17, 2016, from http: //phdadventure. webs. com/diffusionofinnovation. htm
![Diffusion of Innovation Adopter Categories Kaminski J 2016 Diffusion of Innovation Theory Digital image Diffusion of Innovation Adopter Categories Kaminski, J. (2016). Diffusion of Innovation Theory. [Digital image]](https://slidetodoc.com/presentation_image_h2/b759dad0d7af9b970630271a40c9b32f/image-16.jpg)
Diffusion of Innovation Adopter Categories Kaminski, J. (2016). Diffusion of Innovation Theory. [Digital image] Canadian Journal of Nursing Informatics, 6(2), Retrieved on 17 June 2016 from cjninet/journal/? p=1444
Project Implementation • Institutional Review Board – Evidence-based project – No IRB at Northland – Obtained IRB approval 9/30/16 • Threats and Barriers – High staff turnover – Change in routine – Increased workflow expectations
Project Implementation • Monitoring – October - March monitoring period – Telephone, email, or on-site visits • Closure – Compare pre-implementation CRCS rates to postimplementation CRCS rates – Formative survey distribution
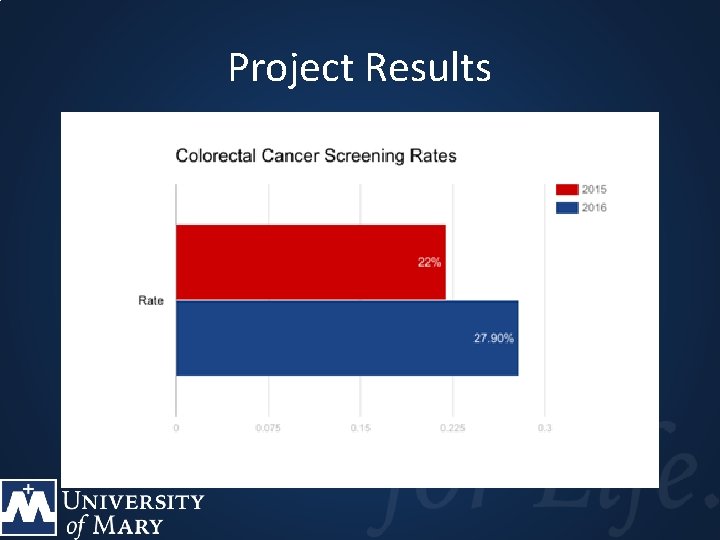
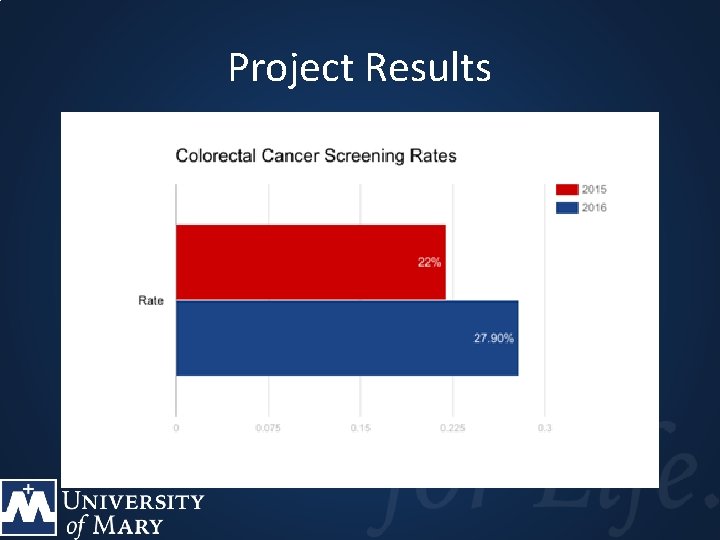
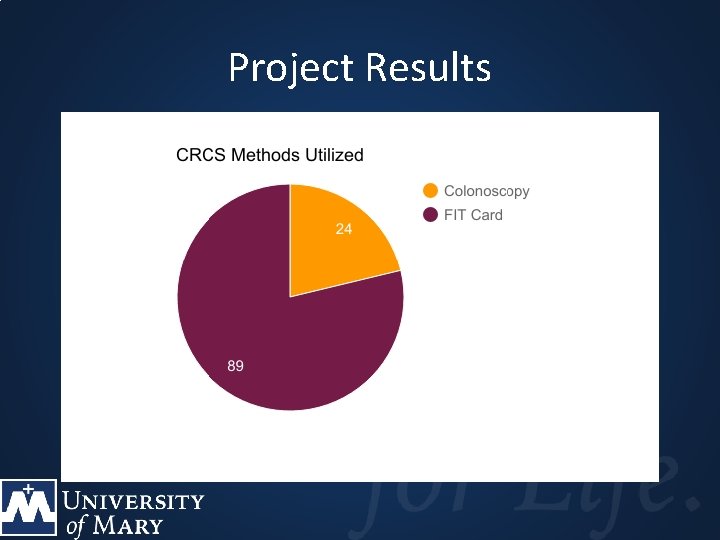
Project Results
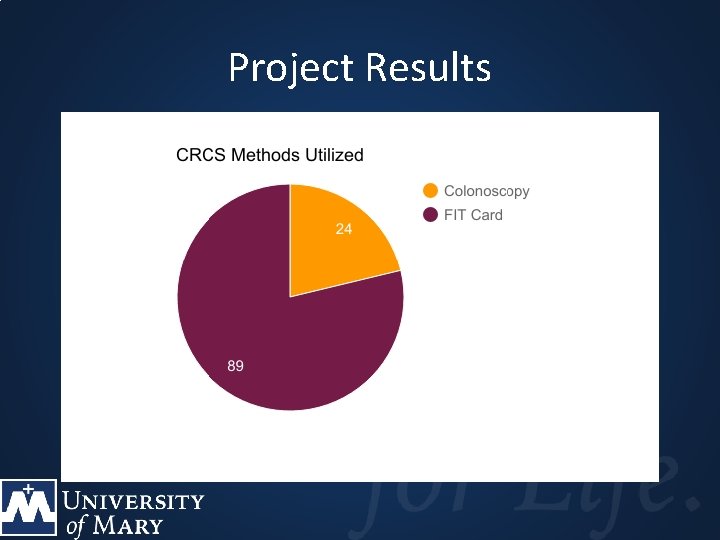
Project Results
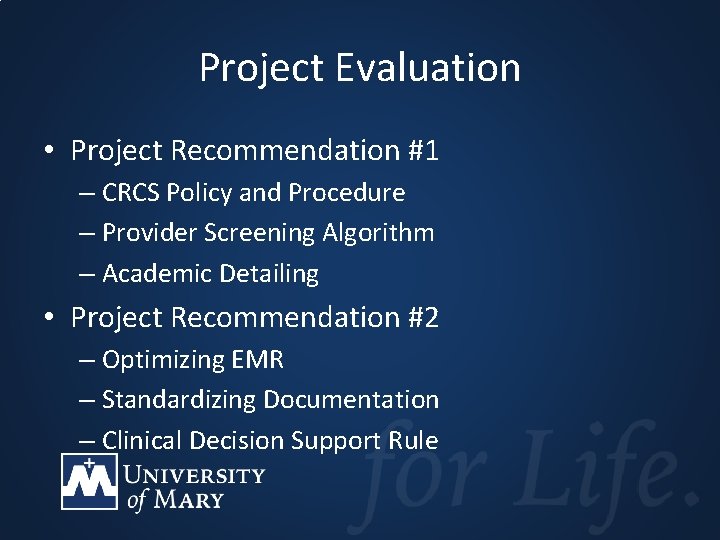
Project Evaluation • Project Recommendation #1 – CRCS Policy and Procedure – Provider Screening Algorithm – Academic Detailing • Project Recommendation #2 – Optimizing EMR – Standardizing Documentation – Clinical Decision Support Rule
Project Evaluation • Project Recommendation #3 – Clinical Navigation • Project Recommendation #4 – Flu/FIT – Outreach Letter and Patient Education
Project Evaluation • Process Improvement Data – Need for staff for Clinical Navigation – Improved EMR optimization – Continued Staff Education on Documentation Requirements
Project Dissemination • Dissemination of Results – Presented at Colloquium – Email to NCHC staff – Presented to NCHC Board – Submission to Scholarly Journal • Future Directions – Continue Flu/FIT, expand to Lab-only Encounter
Conclusion • CRC is 2 nd leading cause of preventable death in the U. S. (ACS, 2014 a) • The CRCS program improved CRCS rates • Project Interventions: – – Policy & Procedure EMR Optimization Patient Navigation Outreach Efforts • Strategies have potential to improve healthcare quality and outcomes
References • • American Cancer Society (2014). Colorectal Cancer Facts & Figures 2014 -2016. Atlanta, GA: American Cancer Society. Retrieved from http: //www. aacr. org/Newsroom/Pages/News. Release. Detail. aspx? Item. ID=795#. Vrk. LOea. Crb. V Atlas, S. J. , Zai, A. H. , Ashburner, J. M. , Chang, Y. , Percac-Lima, S. , Levy, D. E. , . . . & Grant, R. W. (2014). Nonvisit based cancer screening using a novel population management system. Journal of the American Board of Family Medicine, 27(4), 474 -485 Berkowitz, S. A. , Percac-Lima, S. , Ashburner, J. M. , Chang. Y. , Zai, A. H. , He, W. , . . . Atlas, S. J. (2015). Building equity improvement into quality improvement: Reducing socioeconomic disparities in colorectal cancer screening as part of population health management. Journal of General Internal Medicine, 30(7), 942949. doi: 10. 1007/s 11606 -015 -3227 -4 Centers for Disease Control and Prevention [CDC]. (2014). Colorectal (Colon) Cancer: Colorectal Cancer Rates by State. Retrieved from http: //www. cdc. gov/cancer/colorectal/statistics/state. htm Centers for Disease Control and Prevention [CDC]. (2016). Colorectal Cancer Statistics. Retrieved from https: //www. cdc. gov/cancer/colorectal/statistics/ Cole, A. M. , Esplin, A. , & Baldwin, L. (2015). Adaptation of an evidence-based colorectal cancer screening program using the consolidated framework for implementation research. Preventing Chronic Disease, 12(e 213). doi: http: /dx. doi. org/10. 5888/pcd 12. 150300 Corey, P. , Gorski, J. , Schaper, A. , & Newberry, S. (2009). Nurses use motivational interviewing to improve colorectal cancer screening rates. Oncology Nursing Forum, 36(3), 24. Davis, T. , Arnold, C. , Rademaker, A. , Bennett, C. , Bailey, S. , Platt, D. , . . . Wolf, M. (2013). Improving colon cancer screening in community clinics. Cancer, 119, 3879 -3889. Doi: 10. 1002/cncr. 28272
• • References Escoffery, C. , Rodgers, K. C. , Kegler, M. C. , Haardorfer, R. , Howard, D. H. , Liang, S. , . . . Coronado, G. D. (2014). A systematic review of special events to promote breast, cervical, and colorectal cancer screening in the United States. BMC Public Health, 14 (274), 1 -13. Retrieved from http: //www. biomedcentral/14712458/14/274 Green, B. B. , Wang, C. -Y. , Anderson, M. L. , Chubak, J. , Meenan, R. T. , Vernon, S. W. , & Fuller, S. (2013). An automated intervention with stepped increases in support to increase uptake of colorectal cancer screening. Annals of Internal Medicine, 158(5), 301 -311. Healthy People 2020 (2016). Cancer. Retrieved from the Office of Disease Prevention and Health Promotion website at http: //www. healthypeople. gov/2020/topics-objectives/topic/cancer Heydari, A. , & Khorashadizadeh, F. (2014). Pender’s health promotion model in medical research. Journal of the Pakistan Medical Association, 64(9), 1067 -1074. Retrieved from http: //jpma. org. pk/Pdf. Download/6937. pdf HRSA Health Center Program (2014). 2014 Health Center Profile: Northland Health Partners Community Health Center Turtle Lake, ND. Retrieved from the U. S. Department of Health and Human Services at http: //bphc/hrsa/uds/datacenter. aspx? q=d&bid=0810710&state=ND&year=2014 Kaminski, J. (2016). Diffusion of Innovation theory. Canadian Journal of Nursing Informatic, 6(2), Retrieved from the Theory in Nursing Informatics Column at http: //cjni. net. journal/? p=1444 Kern, L. M. , Edwards, A. , & Kaushal, R. (2014). The Patient-Centered Medical Home, electronic health records, and quality of care. Annals of Internal Medicine, 160(11), 741 -749. doi: 10. 7326/M 13 -1798 Levy, B. T. , Daly, J. M. , Schmidt, E. J. , & Xu, Y. (2012). The need for office systems to improve colorectal cancer screening. Journal of Primary Care & Community Health, 3(3), 180 -186. doi: 10. 1177/2150131911423103.
References • • Pender, N. (2011). Health Promotion Model Manual. University of Michigan. Retrieved from https: //deepblue. lib. umich. edu/bitstream/handle/2027. 42/85350/HEALTH_PROMOTION_ MANUAL_Rev_5 -2011. pdf Peterson, S. J. , & Bredow, T. S. (2013). Middle Range Theories: Application to Nursing Research, (3 rd, ed. ). Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. Potter, M. B. , Ackerson, L. M. , Gomez, V. , Walsh, J. M. E. , Green, L. W. , Levin, T. R. , & Somkin, C. P. (2013). Effectiveness and reach of the FLU-FIT Program in an integrated health care: A multisite randomized trial. American Journal of Public Health, 103(6), 1128 -1133. Doi: 10. 2105/AJPH. 2012. 300998 Rogers, E. M. (1983). Diffusions of Innovation (3 rd ed. ). New York, NY: The Free Press. Retrieved from https: //teddykw 2. files. wordpress. com/2012/07/everett-m-rogers-diffusionof-innovations. pdf Sanson-Fischer, R. W. (2004). Diffusion of innovation theory for clinical change. The Medical Journal of Australia, 180(6 suppl), S 55. Retrieved from https: //www. mja. com. au/journal/2004/180/6/diffusioninnovation-theory-clinical-change Sarfaty, M. (2008). How to increase colorectal cancer screening rates in practice: A primary care clinician’s evidence-based toolkit and guide. The National Colorectal Cancer Roundtable. Retrieved from http: //www. cancer. org/acs/groups/content/documents/document/acspc-024588. pdf Xu, Y. , Levy, B. T. , Daly, J. M. , Bergus, G. R. , & Dunkelberg, J. C. (2015). Comparison of patient preferences for fecal immunochemical test or colonoscopy using the analytic hierarchy process. BMC Health Services Research, 15, 175 -184. doi: 10. 1186/s 12913 -015 -0841 -0.