Implantable loop recorders ILRs A powerful tool for
Implantable loop recorders (ILR’s): A powerful tool for investigating patients with unexplained transient loss of consciousness Theodoros Ntoskas Senior Fellow Lung and Heart Centre New Cross Hospital Wolverhampton, UK
No Conflict Of Interest
History • 57 year old man, with Down’s syndrome and significant learning difficulties • Other medical problems: • Hypothyroidism • Barret’s oesophagus • • • Suffering of often episodes of TLOC since 2011 First evaluation in Cardiology OP following referral by GP in February 2012 Clinical History - Challenging Examination, ECG, Echocardiogram: normal Possible diagnosis: Reflex Syncope/Postural hypotension Discharged to GP
History • Admission at ED with Collapse February 2013 and December 2014 • February 2015, March 2015 review by neurology and EEG requested • EEG performed in April 2015 : No clear epileptic activity but just nonspecific slow activity. No epileptic treatment started. For new cardiology opinion. • In May 2015 referred to TLOC (Transient Loss Of Consciousness) clinic • Provisional working diagnosis was one of Reflex Syncope. • BUT Implantable Loop Recorder(ILR) implantation option offered for ECGsymptoms correlation • New appointment in October 2015. Pt had one further vacant episode since July. Decision was taken to implant an ILR. (Consent Form 4)
History • March 2016. At the date of implantation sister phoned to cancel the procedure as no sure if this will benefit patient. • April 2016 Best Interest Meeting organized • June 2016 ILR implanted in the presence of patent’s sister • July 2016 Device routine download: • 4 symptoms-activated recording of faint showed sinus rhythm • 2 x episodes of nocturnal bradycardia with pauses of up to 4 secs • January 2017 patient sustained sub capital neck of femoral fractureoperated successfully. No evidence of bradycardia in ILR. • March 2017 the patient sustained a right sided neck of femur fracture after having a fall during a blackout
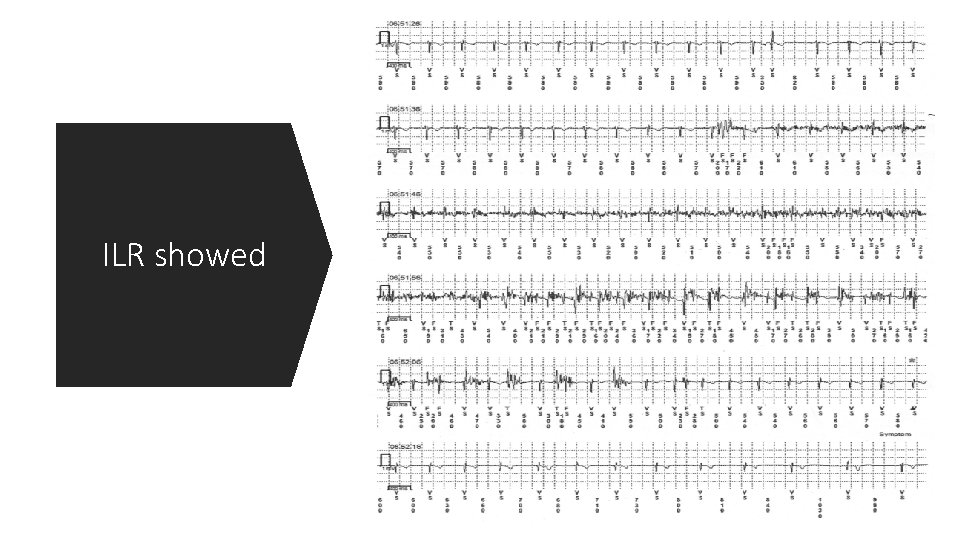
ILR showed
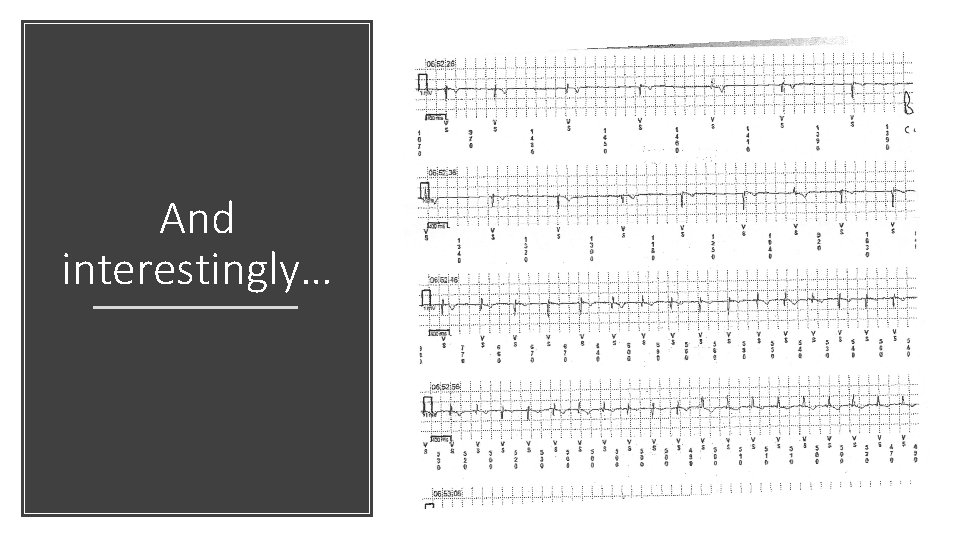
And interestingly…
Antiepileptic treatment DDDR permanent pacemaker Treatment
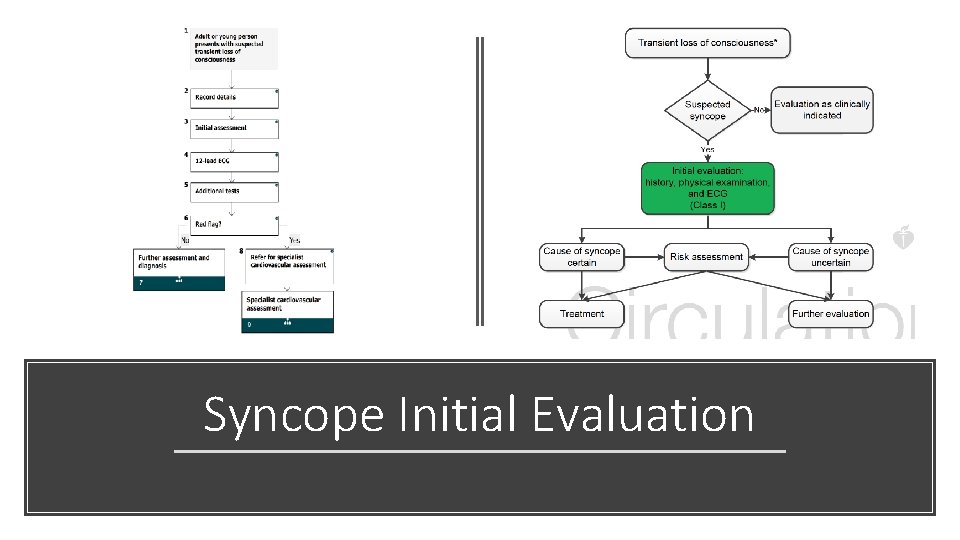
Syncope Initial Evaluation
ILR and Unexplained Syncope
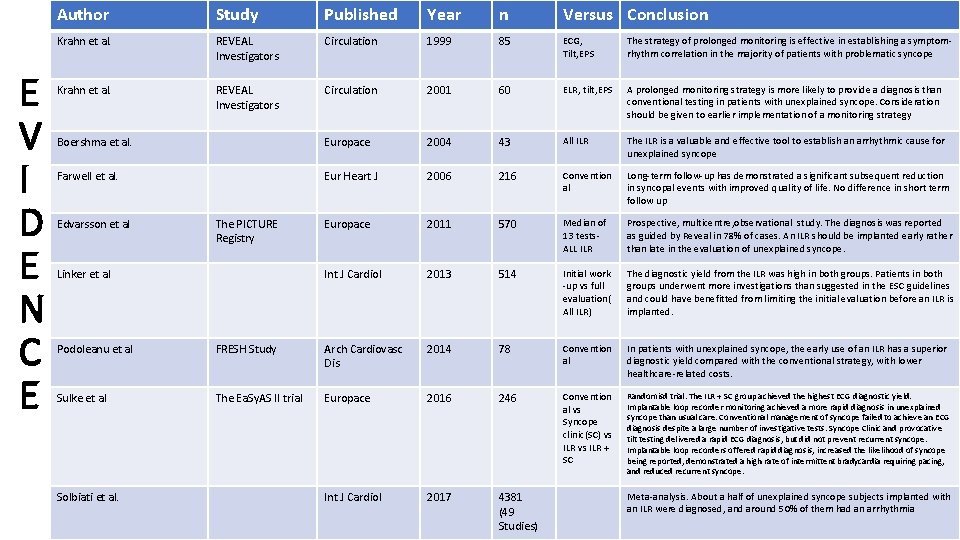
E V I D E N C E Author Study Published Year n Versus Conclusion Krahn et al. REVEAL Investigators Circulation 1999 85 ECG, Tilt, EPS The strategy of prolonged monitoring is effective in establishing a symptomrhythm correlation in the majority of patients with problematic syncope Krahn et al. REVEAL Investigators Circulation 2001 60 ELR, tilt, EPS A prolonged monitoring strategy is more likely to provide a diagnosis than conventional testing in patients with unexplained syncope. Consideration should be given to earlier implementation of a monitoring strategy Boershma et al. Europace 2004 43 All ILR The ILR is a valuable and effective tool to establish an arrhythmic cause for unexplained syncope Farwell et al. Eur Heart J 2006 216 Convention al Long-term follow-up has demonstrated a significant subsequent reduction in syncopal events with improved quality of life. No difference in short term follow up Europace 2011 570 Median of 13 tests- ALL ILR Prospective, multicentre, observational study. The diagnosis was reported as guided by Reveal in 78% of cases. An ILR should be implanted early rather than late in the evaluation of unexplained syncope. Int J Cardiol 2013 514 Initial work -up vs full evaluation( All ILR) The diagnostic yield from the ILR was high in both groups. Patients in both groups underwent more investigations than suggested in the ESC guidelines and could have benefitted from limiting the initial evaluation before an ILR is implanted. Edvarsson et al The PICTURE Registry Linker et al Podoleanu et al FRESH Study Arch Cardiovasc Dis 2014 78 Convention al In patients with unexplained syncope, the early use of an ILR has a superior diagnostic yield compared with the conventional strategy, with lower healthcare-related costs. Sulke et al The Ea. Sy. AS II trial Europace 2016 246 Convention al vs Syncope clinic(SC) vs ILR + SC Randomisd trial. The ILR + SC group achieved the highest ECG diagnostic yield. Implantable loop recorder monitoring achieved a more rapid diagnosis in unexplained syncope than usual care. Conventional management of syncope failed to achieve an ECG diagnosis despite a large number of investigative tests. Syncope Clinic and provocative tilt testing delivered a rapid ECG diagnosis, but did not prevent recurrent syncope. Implantable loop recorders offered rapid diagnosis, increased the likelihood of syncope being reported, demonstrated a high rate of intermittent bradycardia requiring pacing, and reduced recurrent syncope. Int J Cardiol 2017 4381 (49 Studies) Solbiati et al. Meta-analysis. About a half of unexplained syncope subjects implanted with an ILR were diagnosed, and around 50% of them had an arrhythmia
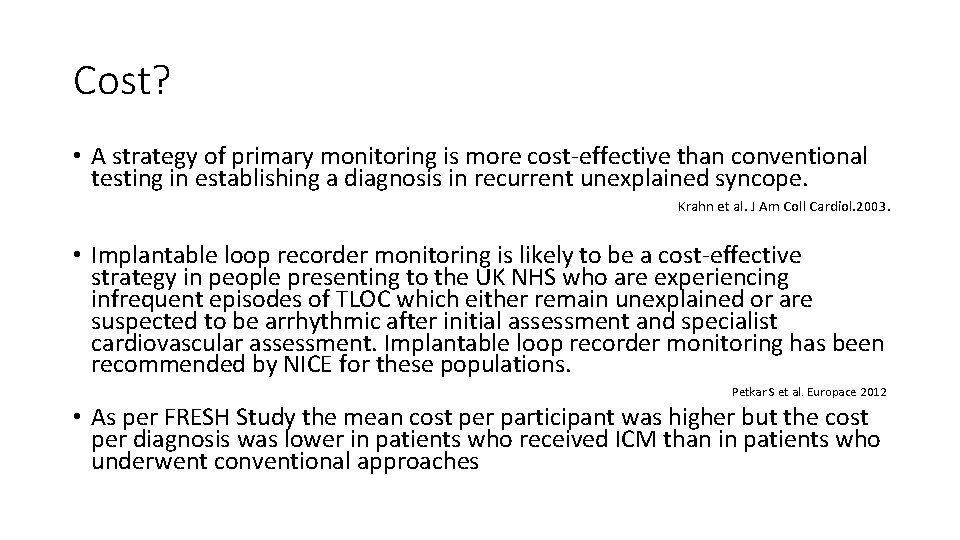
Cost? • A strategy of primary monitoring is more cost-effective than conventional testing in establishing a diagnosis in recurrent unexplained syncope. Krahn et al. J Am Coll Cardiol. 2003. • Implantable loop recorder monitoring is likely to be a cost-effective strategy in people presenting to the UK NHS who are experiencing infrequent episodes of TLOC which either remain unexplained or are suspected to be arrhythmic after initial assessment and specialist cardiovascular assessment. Implantable loop recorder monitoring has been recommended by NICE for these populations. Petkar S et al. Europace 2012 • As per FRESH Study the mean cost per participant was higher but the cost per diagnosis was lower in patients who received ICM than in patients who underwent conventional approaches
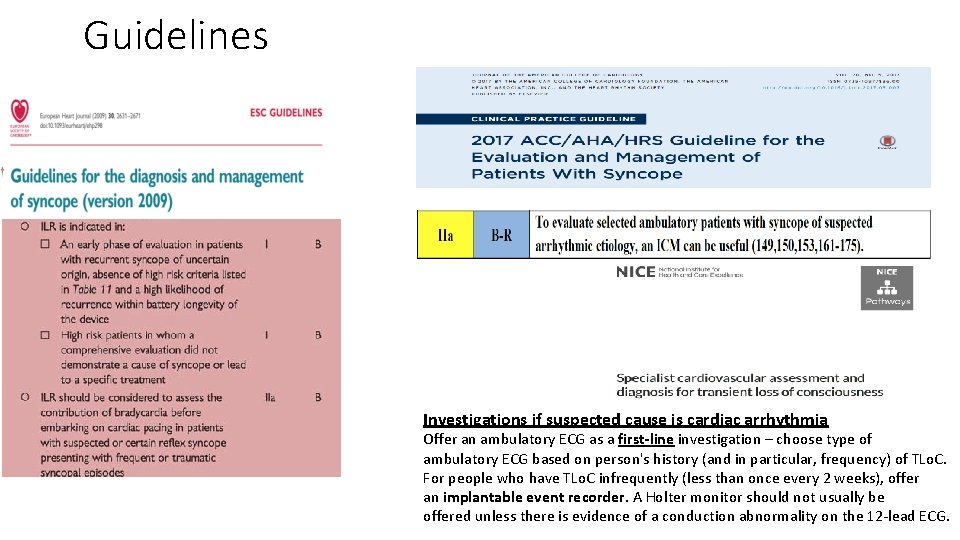
Guidelines Investigations if suspected cause is cardiac arrhythmia Offer an ambulatory ECG as a first-line investigation – choose type of ambulatory ECG based on person's history (and in particular, frequency) of TLo. C. For people who have TLo. C infrequently (less than once every 2 weeks), offer an implantable event recorder. A Holter monitor should not usually be offered unless there is evidence of a conduction abnormality on the 12 -lead ECG.
ILR – Other Indications
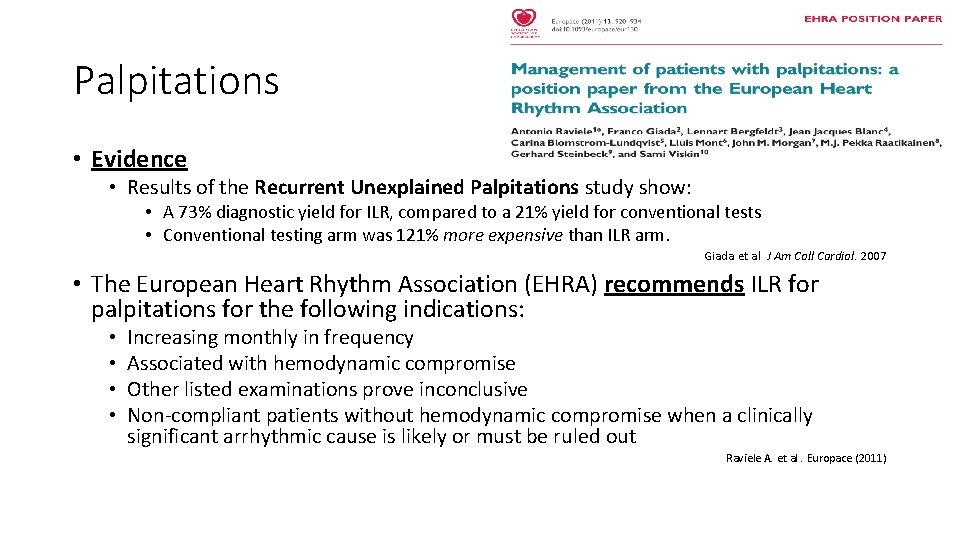
Palpitations • Evidence • Results of the Recurrent Unexplained Palpitations study show: • A 73% diagnostic yield for ILR, compared to a 21% yield for conventional tests • Conventional testing arm was 121% more expensive than ILR arm. Giada et al J Am Coll Cardiol. 2007 • The European Heart Rhythm Association (EHRA) recommends ILR for palpitations for the following indications: • • Increasing monthly in frequency Associated with hemodynamic compromise Other listed examinations prove inconclusive Non-compliant patients without hemodynamic compromise when a clinically significant arrhythmic cause is likely or must be ruled out Raviele A. et al. Europace (2011)
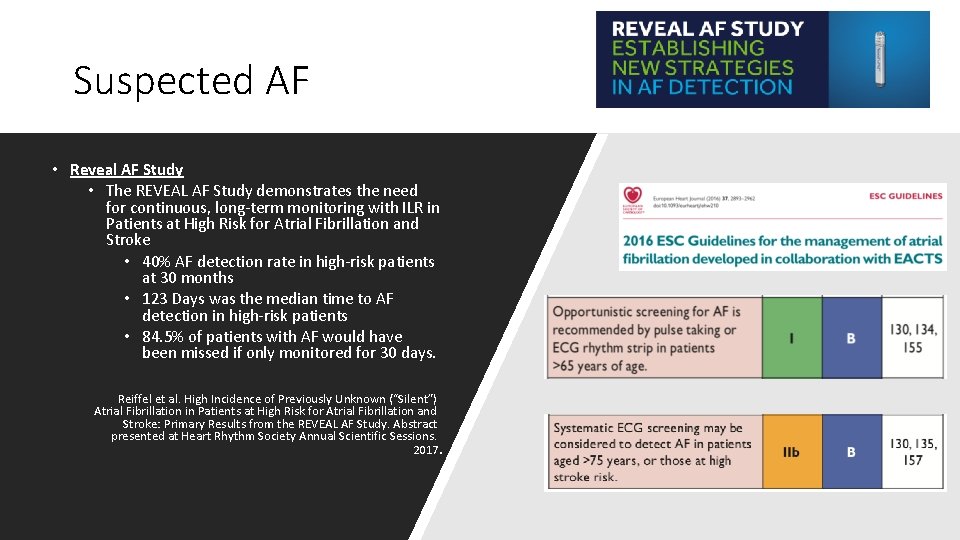
Suspected AF • Reveal AF Study • The REVEAL AF Study demonstrates the need for continuous, long-term monitoring with ILR in Patients at High Risk for Atrial Fibrillation and Stroke • 40% AF detection rate in high-risk patients at 30 months • 123 Days was the median time to AF detection in high-risk patients • 84. 5% of patients with AF would have been missed if only monitored for 30 days. Reiffel et al. High Incidence of Previously Unknown (“Silent”) Atrial Fibrillation in Patients at High Risk for Atrial Fibrillation and Stroke: Primary Results from the REVEAL AF Study. Abstract presented at Heart Rhythm Society Annual Scientific Sessions. 2017.
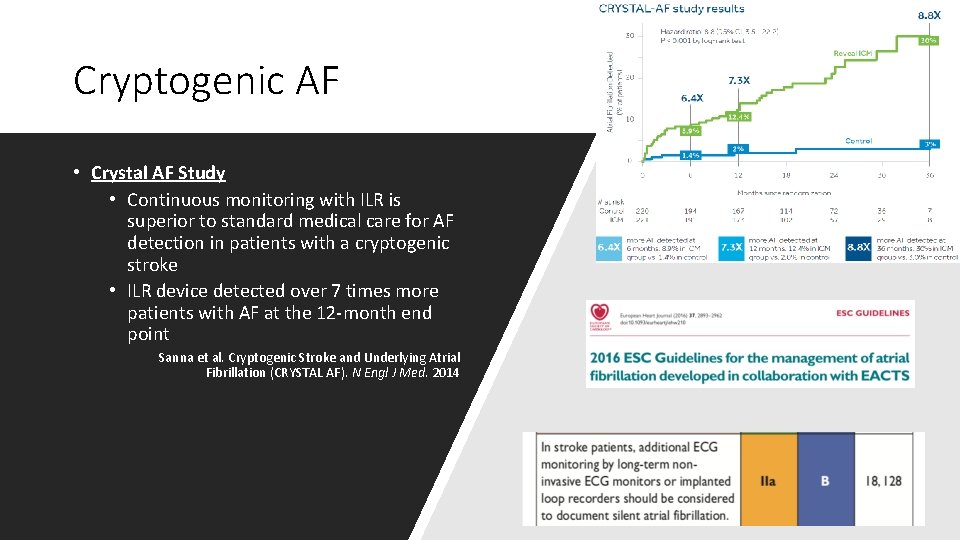
Cryptogenic AF • Crystal AF Study • Continuous monitoring with ILR is superior to standard medical care for AF detection in patients with a cryptogenic stroke • ILR device detected over 7 times more patients with AF at the 12 -month end point Sanna et al. Cryptogenic Stroke and Underlying Atrial Fibrillation (CRYSTAL AF). N Engl J Med. 2014
AF Ablation Management • Discern AF trial • The ratio of Asymptomatic AF episodes increased 3 x after ablation • 12% of patients had ONLY Asymptomatic AF post-ablation Verma et al. Discerning the Incidence of Symptomatic and Asymptomatic Episodes of Atrial Fibrillation Before and After Catheter Ablation. JAMA Intern Med. 2013 • Even in patients presenting with highly symptomatic AF, asymptomatic episodes may occur and significantly increase after catheter ablation. A symptom-only-based follow-up would substantially overestimate the success rate Hindricks G. et al. Perception of Atrial Fibrillation Before and After Radiofrequency Catheter Ablation - Relevance of Asymptomatic Arrhythmia Recurrence. Circulation. 2005; 112: 307 -313. • ABACUS Study • • 96% of patients with AF were found by ILR. “Conventional Monitoring” missed 29% in first 6 mo. Rate Control and Anti-Arrhythmic drugs were discontinued more in the Reveal Arm Asymptomatic AF documented in 70% of pts 16% of ILR patients had other actionable brady/tachy events vs. 0% in “Conventional” arm Kapa S et al. Assessing arrhythmia burden after catheter ablation of atrial fibrillation using an implantable loop recorder: the ABACUS study. J Cardiovasc Electrophysiol. 2013 • New-Onset AF (NOAF) Following Atrial Flutter Ablation. Majority of Patients(55%) had NOAF; ILR Needed to Detect AF Mittal S et al. Long-Term ECG Monitoring Using an Implantable Loop Recorder for the Detection of Atrial Fibrillation Following Cavotricuspid Isthmus Ablation in Patients with Atrial Flutter. Heart Rhythm. 2013 Jul
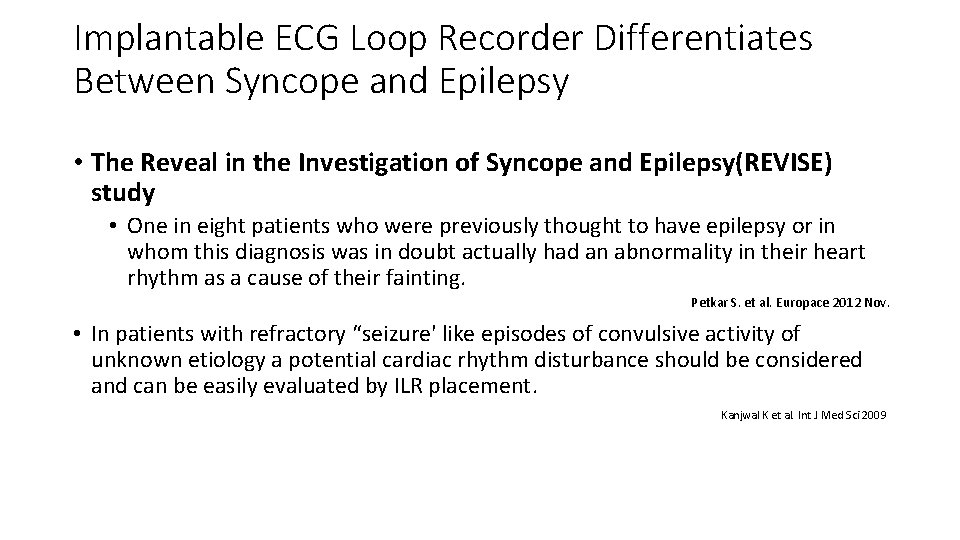
Implantable ECG Loop Recorder Differentiates Between Syncope and Epilepsy • The Reveal in the Investigation of Syncope and Epilepsy(REVISE) study • One in eight patients who were previously thought to have epilepsy or in whom this diagnosis was in doubt actually had an abnormality in their heart rhythm as a cause of their fainting. Petkar S. et al. Europace 2012 Nov. • In patients with refractory “seizure' like episodes of convulsive activity of unknown etiology a potential cardiac rhythm disturbance should be considered and can be easily evaluated by ILR placement. Kanjwal K et al. Int J Med Sci 2009
Highlights • The role of a structured assessment of patients with TLOC as recommended by NICE guidelines • The recommendation of NICE/ESC/ACC guidance to choose tests with the highest diagnostic yield over other easily available but low yielding tests e. g. , ILR’s versus conventional external ECG monitoring/tilt testing • The challenges of caring for patients with learning difficulties and impaired capacity • Collaborative working between neurologists and cardiologists • Indications of the ILR • How to differentiate syncope and epilepsy • The role of ILR’s in the misdiagnosis of epilepsy.

Thank You
- Slides: 21