Impact of Single versus Double Layer Closure on
Impact of Single versus Double Layer Closure on Adverse Outcomes and Uterine Scar Defect : A Systematic Review and Meta-analysis Author(s): Yu Heng KWAN, Chunyan HU, Stella SETIAWAN, Junjie YEO Level: Intermediate Academic Affiliation : Duke-NUS, Graduate Medical School, Medical Students Version No: 1. 0 Adapted from: Roberge S. , Demers S. , Berghella V. , Chaillet N. , Moore L. , Bujold E. Impact of single- vs. double-layer closure on adverse outcomes and uterine scar defect : a systematic review and metaanalysis. American Journal of Obstetrics and Gynecology. 2014; 211: 453 -460. Submitted: February 2015 Editors’ Review:
2 Disclaimer/Liability • The information provided in the VAP is made available in good faith and is derived from sources believed to be reliable and accurate at the time of release. • The materials presented on the VAP may include links to external Internet sites. These external information sources are outside the control of Duke-NUS. The user of the Internet links is responsible for making his or her own decision about the accuracy, reliability and correctness of the information found. • In no event shall Duke-NUS be liable for any indirect, special, incidental, or consequential damages arising out of any use of reliance of any information contained in the VAP. Nor does Duke-NUS assume any responsibility for failure or delay in updating or removing the information contained in the VAP. • Moreover, information provided on the VAP does not constitute medical advice or treatment nor should it be considered as a replacement of the patient/physician relationship or a physician’s professional judgment. Duke-NUS expressly disclaims all liability for treatment, diagnosis, decisions and actions taken or not taken in reliance upon information contained in the VAP. This work is licensed under a Creative Commons Attribution-Non. Commercial-No. Derivs 3. 0 Unported License To view a copy of this license, visit [http: //creativecommons. org/licenses/by-nc-nd/3. 0/]
3 INTRODUCTION
4 Uterine Closure in Cesarean Section • Important step in immediate post operative period and also future gestations • Increasing evidence to suggest surgical technique for uterine closure affects uterine scar healing • Abnormal uterine scar healing is thought to be associated with risk of placenta accreta and uterine rupture in future pregnancies • Optimal uterine closure technique undetermined • A systematic review and meta-analysis conducted to evaluate the effect of type of uterine closure on uterine scar and adverse maternal outcome
5 Uterine Closure: Steps 1. Angle of uterine incision grasped using Allis forceps to stabilise and manoeuvre incision 2. Initial suture placed just beyond angle of uterine incision 3. Continuous suture is performed, each suture penetrating full thickness of myometrium – Continuous/Interrupted – Locked/unlocked 4. Continued just beyond opposite angle of uterine incision 5. If approximation or hemostasis unsatisfactory, consider: – Another layer of continuous suture – Figure of eight/mattress suture for individual bleeders 6. Serosal edges overlying uterus and bladder typically not approximated
6 Uterine Closure: Considerations • First layer of uterine closure always performed • Continuous associated with shorter operative time and lower blood loss compared to interrupted • Locking of primary layer of closure facilitates hemostatsis but may compromise healing; impairment of microcirculation around the wound

7 MATERIALS AND METHODS
8 Methods • Randomized controlled trials comparing number of layers (single vs double) and the use of locking versus unlocking sutures for uterus closure in low transverse cesarean • Key word/Medical subject heading search (Pub. Med, Web of Science, Embase, and Cochrane central register) from 1980 - September 2013 • The quality of studies evaluated by Cochrane handbook criteria for judging risk of bias • Sensitivity analysis for studies with high risk of bias • Quality and integrity of review validated with PRISMA
9 Methods • Immediate outcomes: – – – – Maternal infectious Endometritis Wound infection Blood transfusion Mean blood loss Duration of surgical procedure Length of hospital stay • Long-term adverse outcomes: – Uterine rupture or dehiscence • Post-cesarean ultrasonographic evaluation of uterine scar: – Presence of uterine scar defect – Residual myometrial thickness (in mm)
10 Methods • Risk ratios (RRs) with 95% CI compared binary outcomes between the 2 closure types: – – – Uterine rupture Infectious morbidity Endometritis Wound infection Blood transfusion Scar defect • Mean difference with 95% CI compared continuous outcomes : – – Duration of procedure Length of hospital stay Mean blood loss Residual myometrial thickness
11 Methods • I 2 criteria of Higgins et al. to assess heterogeneity between studies • Sensitivity analysis testing robustness of the findings and to explain heterogeneity between studies comparing: – – suture type (locked or unlocked) thread type (synthetic or chromic) region (North America or other) primary cesarean (yes or no)
12 RESULTS AND DISCUSSION
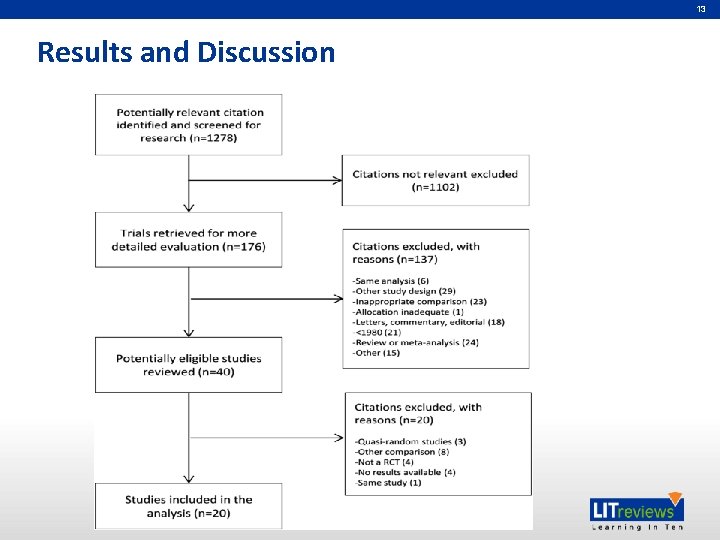
13 Results and Discussion
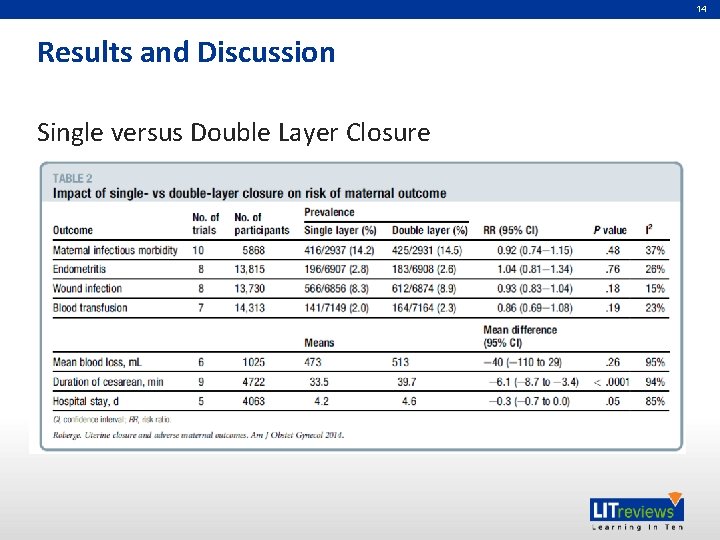
14 Results and Discussion Single versus Double Layer Closure
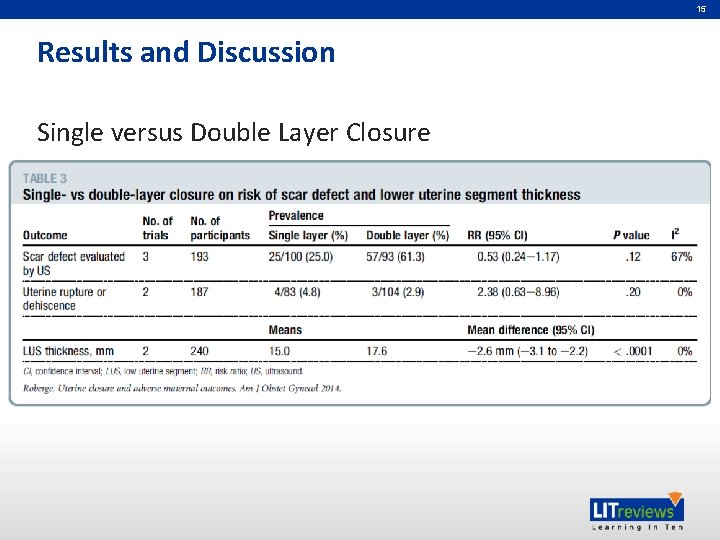
15 Results and Discussion Single versus Double Layer Closure
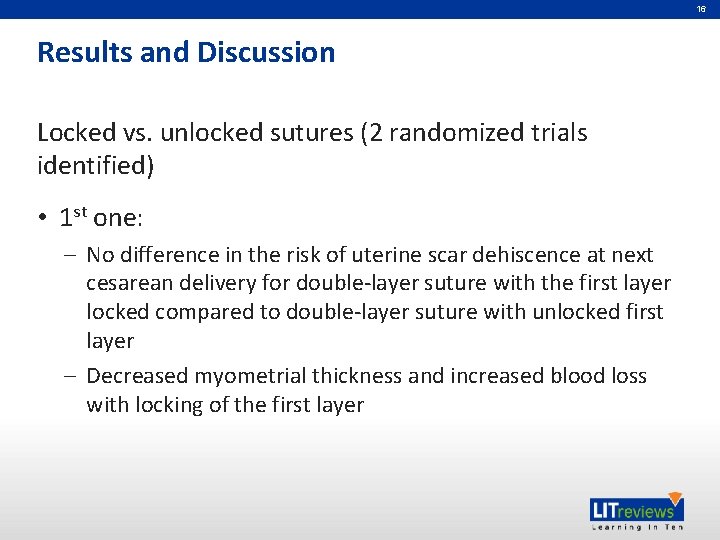
16 Results and Discussion Locked vs. unlocked sutures (2 randomized trials identified) • 1 st one: – No difference in the risk of uterine scar dehiscence at next cesarean delivery for double-layer suture with the first layer locked compared to double-layer suture with unlocked first layer – Decreased myometrial thickness and increased blood loss with locking of the first layer
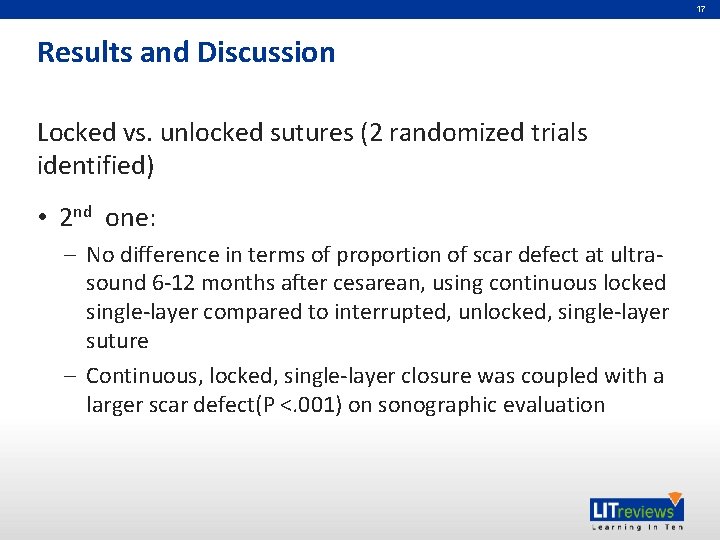
17 Results and Discussion Locked vs. unlocked sutures (2 randomized trials identified) • 2 nd one: – No difference in terms of proportion of scar defect at ultrasound 6 -12 months after cesarean, using continuous locked single-layer compared to interrupted, unlocked, single-layer suture – Continuous, locked, single-layer closure was coupled with a larger scar defect(P <. 001) on sonographic evaluation
18 Author’s Conclusions No difference in terms of the risk of maternal morbidity or long-term outcomes between single- versus double-layer uterus closure at low transverse cesarean Data from randomized trials are insufficient to conclude about the risk of uterine rupture, dehiscence, or gynecological outcomes because of insufficient power. Single-layer closure was associated with decreased residual myometrial thickness and shorter operative time based on 2 (n ¼ 240) and 9 (n ¼ 4722 women) studies, respectively Few data are available on the impact of locked versus unlocked sutures that favor the use of unlocked sutures to obtain a thicker myometrium measured by ultrasound More studies need to be conducted to determine the optimal techniques and sutures needed for LSCS
19 POSITIVE THINGS ABOUT THIS PAPER
20 Positive Things About This Paper • A very targeted and clear objective was stated : To compare the effect of single- versus doublelayer and locked vs unlocked closure of low transverse cesarean on the risk of adverse maternal outcomes, including uterine rupture and uterine scar defect evaluated by ultrasound • Hence facilitating in the search and selection of relevant studies to be included in the analysis
21 Positive Things About This Paper • Only Randomized Controlled Trials (RCT) that compared single versus double layers and use of locking versus unlocking sutures for uterus closure of low transverse cesarean were included • Extensive search was done to find studies that are relevant to the objective of this paper : electronic databases including Pub. Med, Cochrane, Web of Science, and Embase from 1980 to September 2013 were explored using relevant keywords like ‘uterus’, ‘uterine’, ‘dehiscence’, ‘rupture’, ‘separation’, and ‘scar’ Plus, no restriction on language was applied
22 Positive Things About This Paper • All biased were kept to a minimum by using two independent reviewers to run through the titles, abstracts, and texts. Any disagreements between them were resolved by discussion with a third independent reviewer • The quality of all studies used and their potential biasness were evaluated using Cochrane Handbook Criteria • The quality of this review paper was validated with PRISMA, which is the preferred reporting items for systematic review and meta-analysis
23 Positive Things About This Paper • Sensitivity analysis were done to explain the heterogeneity between studies, comparing suture type, regions, thread type, or whether it is primary cesarean or not • The authors provided a clear definition for each important terms they used, thus minimizing any ambiguity and help in better appreciation and understanding of the results We collected data regarding long term adverse outcomes during subsequent pregnancies, such as uterine rupture or dehiscence. Uterine rupture is defined as complete separation of the uterine scar with visceral peritoneum disruption or bladder rupture, necessitating an emergency intervention (or equivalent definition)
24 Positive Things About This Paper • The authors explained the process of data collections to very minute details, thus clarifying any doubts we have along the way We collected all information regarding post-cesarean ultrasonographic evaluation of uterine scar, including the presence of uterine scar defect (defined as the observation of myometrial loss or deformity at the cesarean scar site), residual myometrial thickness (in mm), or residual myometrial thickness less than a specific cutoff determined by the author In case of multiple ultrasound measures in time, available data or those who were close to 6 -month evaluation were analyzed
25 Limitations of this paper
26 Insufficient Power for Secondary Endpoints • Data from RCT are actually insufficient to conclude on the following: – Risk of uterine rupture – Dehiscence – Other gynecological outcomes • But uterine dehiscence were reported to show no statistical significance (RR: 1. 86, 95% CI: 0. 44 -7. 90, p=0. 40)
27 Unreliable Schedule of Ultrasound Scan • Data from scans were done from 6 weeks to 6 months when scar healing takes up to 6 months • Prediction of uterine rupture from scar may be adversely affected due to wrong reference point used when analyzing scar
28 Unreliable Schedule of Ultrasound Scan • Data from scans were done from 6 weeks to 6 months when scar healing takes up to 6 months • Scans sometimes were done transvaginally or transabdomainally, hence were not standardised • Prediction of uterine rupture from scar may be adversely affected due to wrong reference point used when analyzing scar
29 Dissimilar Manner of Randomization • Different studies randomized participants for various procedures such as combined single vs double layer with various outcomes • This results in poor robustness of the meta-analyses because of the small number of studies for this primary outcome. Sensitivity analyses done could not assess the robustness of this study
30 No Restriction of Studies about Types of Incisions, Opening or Closure • There were no restrictions on the studies about the types of skin incisions, abdominal opening or closure of other layers • It was found that peritoneum closure or not may have short term complications such as duration of operation, pain score, and analgesic requirements 1 • This may predispose the study to biasness by not considering the type of studies included 1 Tabasi Z, Mahdian M, Abedzadeh-Kalahroudi M. Closure or non-closure of peritoneum in cesarean section: outcomes of shortterm complications. Arch Trauma Res 2013; 1(4): 176 -9.

Partners in Academic Medicine
- Slides: 31