Impact of having a chronic physical health condition

- Slides: 20
Impact of having a chronic physical health condition on older adults’ mental health Tier 2 and 3
Patient Statement “We’re not just legs and arms and a mouth. . . We are human beings with a mixture of emotions. All these feelings. . . self esteem, self worth, confidence, identity. . . they’re all under attack after a stroke. . . you can feel vulnerable, frightened and you can lose yourself ” Harry Clarke, Counsellor at Connect who has aphasia (From Psychological Care after Stroke, NHS Improvement, 2011)
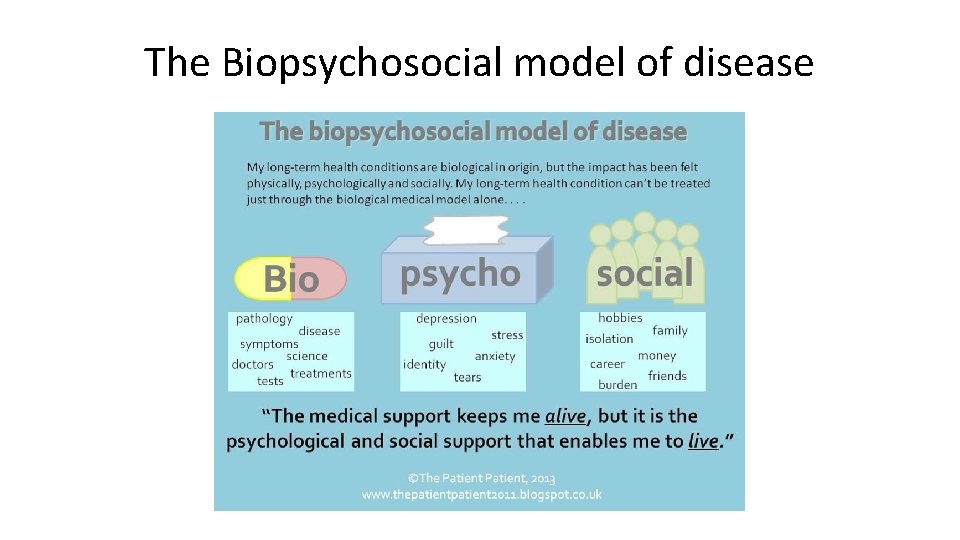
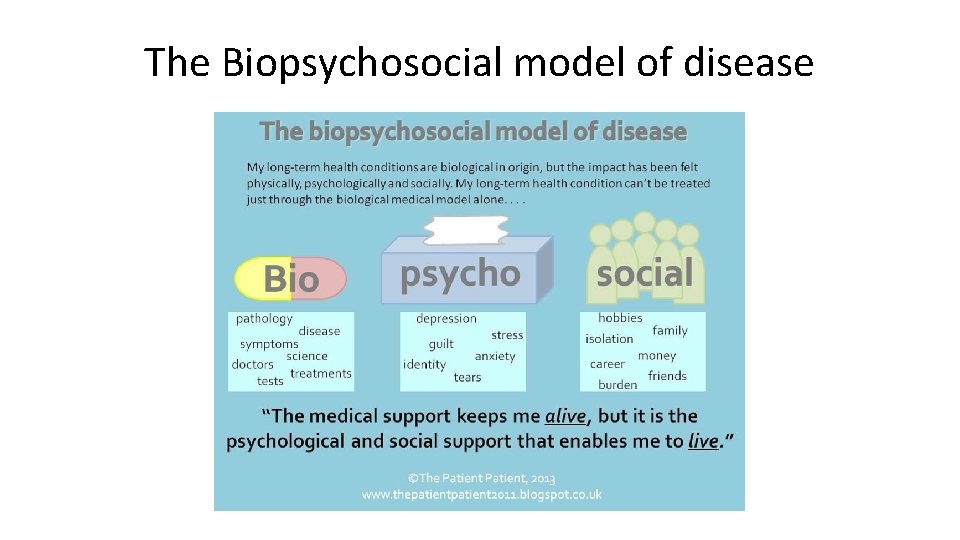
The Biopsychosocial model of disease
What does this mean in practice? • Physical health can have an emotional impact on people • This combination leads to significantly poorer health outcomes and reduced quality of life. • It is important to consider the impact of the physical health conditions and adjustments on the individual • It is important to consider the individual in a holistic manner • Healthy body + healthy mind = Happy person
What do patients with a health condition want? https: //vimeo. com/69073697 People with long term conditions request that they are seen as more than their condition; for health professionals to understand that they have lives, dreams, ambitions, families, friends and hobbies. In other words, to understand the bigger picture – there can be times when a long term condition impacts on life, and times when life impacts on a long term condition (Emotional Support Matters, 2011)
What are Long term physical health conditions? • Long term physical health conditions, or chronic diseases, are conditions that last a year or longer, impact on a person’s life, and may require ongoing care and support. • These physical health conditions include : diabetes, heart disease, stroke, cancer, rheumatoid arthritis, chronic obstructive pulmonary disease (COPD)and epilepsy.
What is it like to have a long term condition? https: //vimeo. com/69079830 The person can need time • To adjust to health change • Engage with treatment and recovery • Relatives might also need time to adjust
Impact of chronic physical health condition on mental health • People with chronic physical health condition are 2 -3 times more likely to develop a mental health condition. • People with two or more chronic physical health condition are up to 7 times more likely to experience depression. • The reason for this increased risk is multifactorial e. g. chronic pain, chronic emotional stress, increased isolation due to disability, chronic high blood sugar levels, hypertension, side effects of medications.
Impact of a sudden change in health A sudden change in health such as a fall and / or a long term condition can mean changes to: • Roles and dynamics in relationships - family and relationship strain • Social life • Their emotional wellbeing - difficulties coping and adapting • They may experience distress
Distress • The shock of having an acute decline in health can produce some degree of distress and is to be expected in many people following a such a health event • The sudden and unscheduled life event, can leave little time to adapt to new circumstances
What does distress look like? After a sudden change in health a person might initially feel. . . • Shocked and unable to understand / accept what has happened • Anger, sadness and depression • Tearful and upset, with fluctuations in their mood • Scared and unsure about the future / fear of further decline in health / disease progression • Emotionally labile • Low motivation and negative beliefs about recovery • Unable / not wanting to eat • Sleepy and become withdrawn • ‘Glad to be alive’ or not • Their relatives may also experience similar feelings Different cultures may have different ways of expressing distress and it is important to bear that in mind
What to look out for? • Distress is expected and adjustment and resolution usually occur as part of the process of recovery. • However, for some people it can be persistent, affect many areas of functioning and, importantly impact on their rehabilitation and ability to achieve their goals. • Get a sense of whether you are seeing the usual process of adjustment, or something more problematic. This can usually be clarified by asking the right questions.
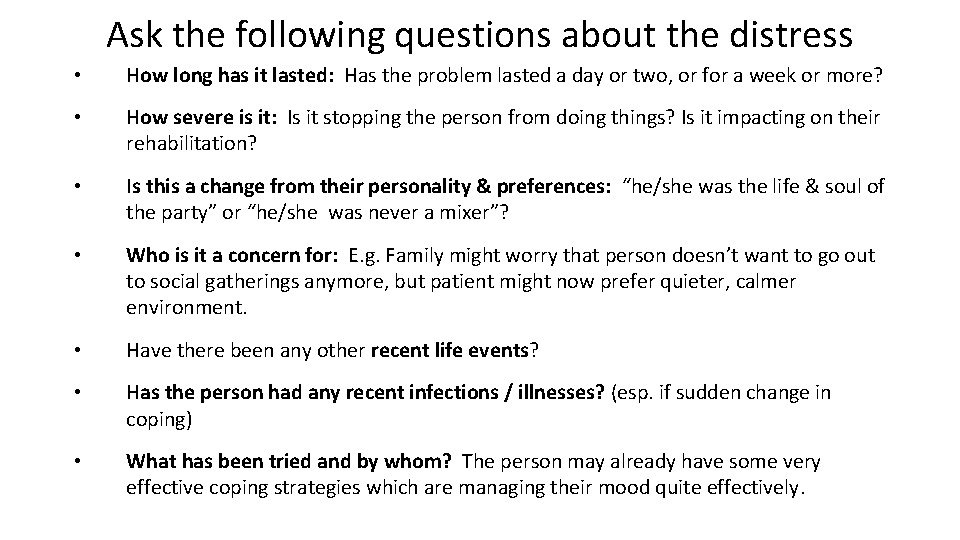
Ask the following questions about the distress • How long has it lasted: Has the problem lasted a day or two, or for a week or more? • How severe is it: Is it stopping the person from doing things? Is it impacting on their rehabilitation? • Is this a change from their personality & preferences: “he/she was the life & soul of the party” or “he/she was never a mixer”? • Who is it a concern for: E. g. Family might worry that person doesn’t want to go out to social gatherings anymore, but patient might now prefer quieter, calmer environment. • Have there been any other recent life events? • Has the person had any recent infections / illnesses? (esp. if sudden change in coping) • What has been tried and by whom? The person may already have some very effective coping strategies which are managing their mood quite effectively.
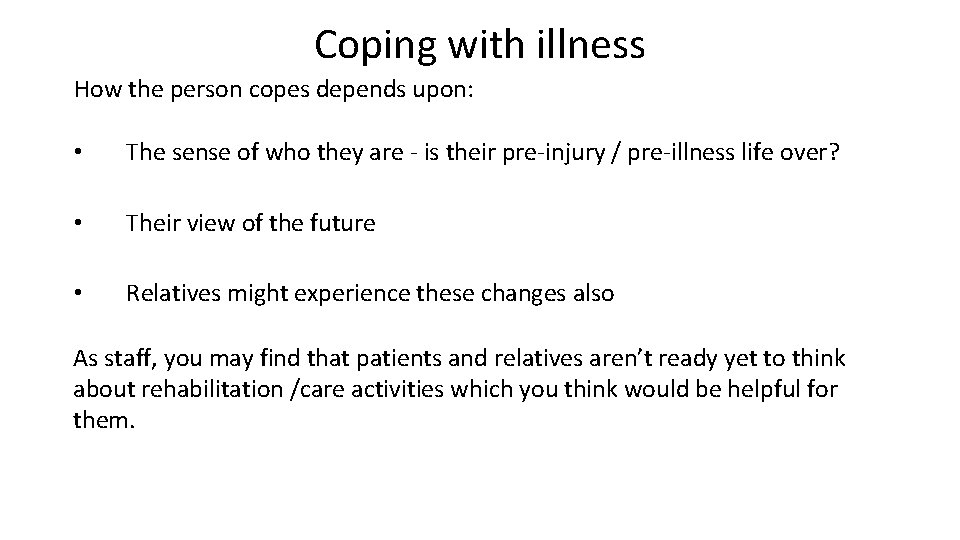
Coping with illness How the person copes depends upon: • The sense of who they are - is their pre-injury / pre-illness life over? • Their view of the future • Relatives might experience these changes also As staff, you may find that patients and relatives aren’t ready yet to think about rehabilitation /care activities which you think would be helpful for them.
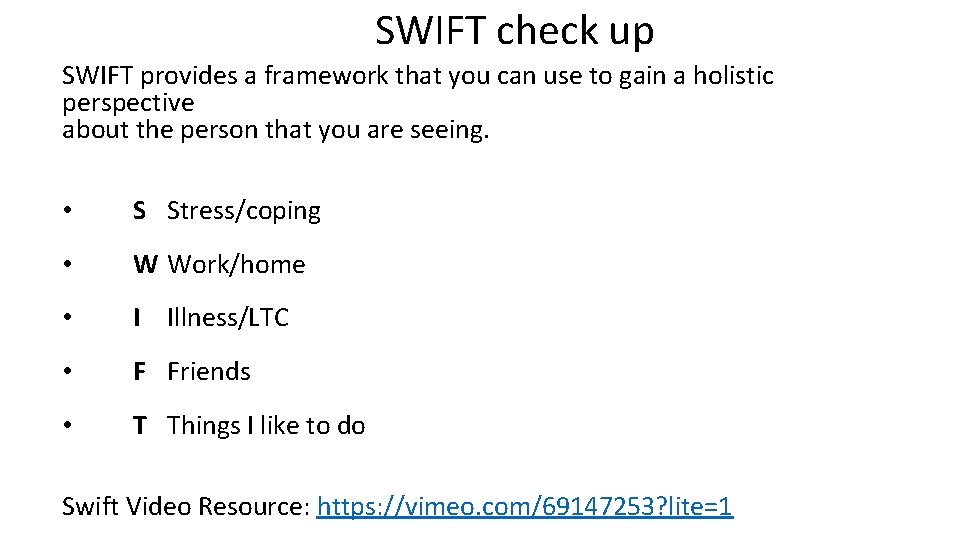
SWIFT check up SWIFT provides a framework that you can use to gain a holistic perspective about the person that you are seeing. • S Stress/coping • W Work/home • I Illness/LTC • F Friends • T Things I like to do Swift Video Resource: https: //vimeo. com/69147253? lite=1
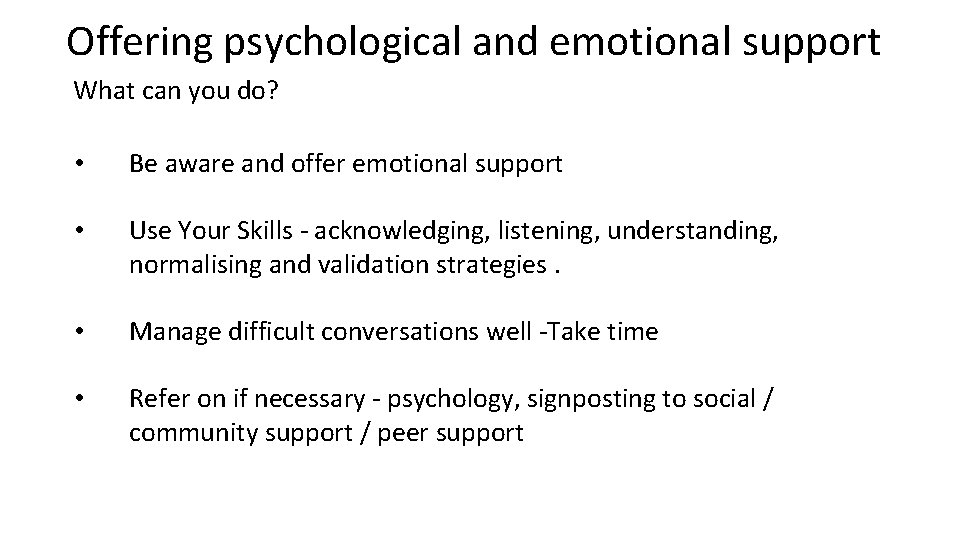
Offering psychological and emotional support What can you do? • Be aware and offer emotional support • Use Your Skills - acknowledging, listening, understanding, normalising and validation strategies. • Manage difficult conversations well -Take time • Refer on if necessary - psychology, signposting to social / community support / peer support

When to refer • The problems feel stuck and not resolving over time • The patient / family identifies concerns as problematic • Concerns are a significant barrier to recovery and rehabilitation • Risk to themselves or others • Suicidal thinking • It is best to flag up potential problems early
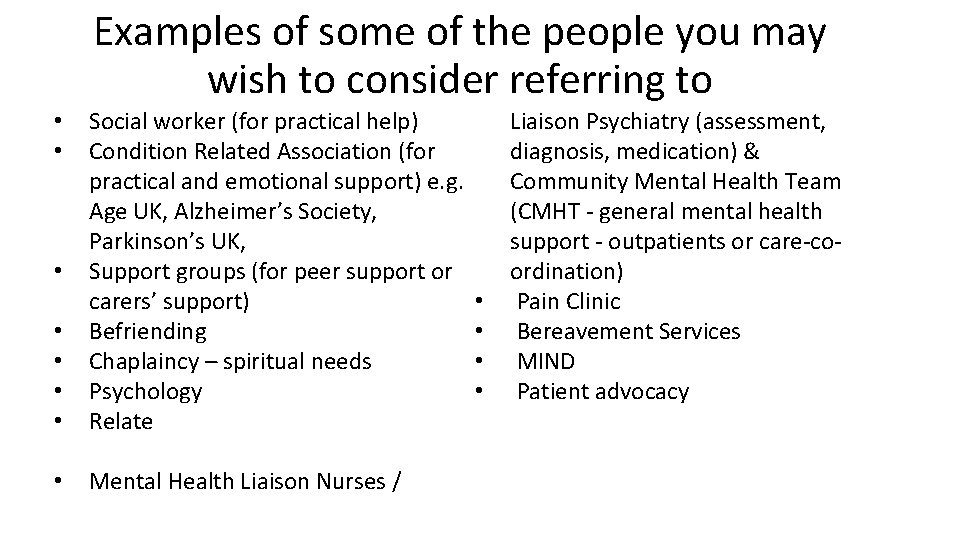
Examples of some of the people you may wish to consider referring to • • Social worker (for practical help) Condition Related Association (for practical and emotional support) e. g. Age UK, Alzheimer’s Society, Parkinson’s UK, Support groups (for peer support or carers’ support) Befriending Chaplaincy – spiritual needs Psychology Relate • Mental Health Liaison Nurses / • • Liaison Psychiatry (assessment, diagnosis, medication) & Community Mental Health Team (CMHT - general mental health support - outpatients or care-coordination) Pain Clinic Bereavement Services MIND Patient advocacy
Looking after yourself • Taking care of yourself is important • You need to know who you can speak to talk about any difficulties such as to being able to debrief after an upsetting consultation • Consider setting up or joining a reflective practice group • Make sure that you have a support system at work to discuss your concerns for example about someone you have seen • If you are finding that work is causing more stress to you than usual, or than you think is healthy then you should talk about this with your line manager or with Occupational Health
Resources • MPC_05_01 Making the Most of Your Physical and Mental Health (mindedforfamilies. org. uk) • This is an easy to access website for older adults and their families which has good advice about changes that the older adult can make to their lifestyle, diet and physical health that will help their wellbeing