Immunology the HIV life cycle and stages of




- Slides: 26
Immunology, the HIV life cycle and stages of infection Anele Waters HIV Research Nurse North Middlesex Hospital, London
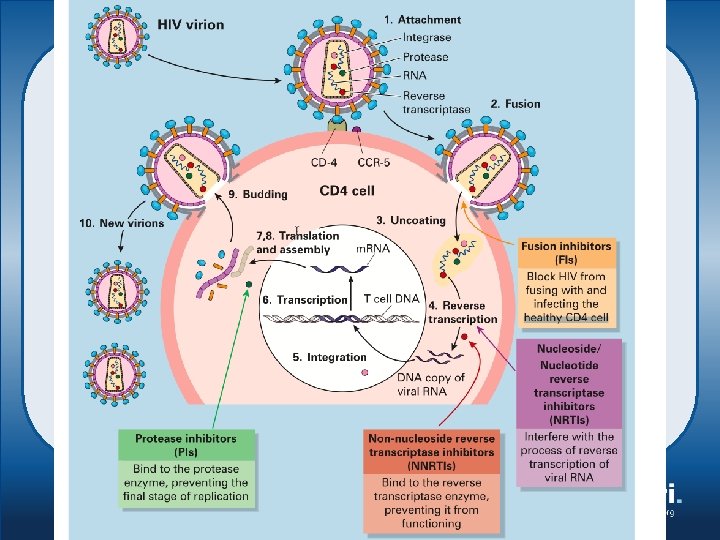
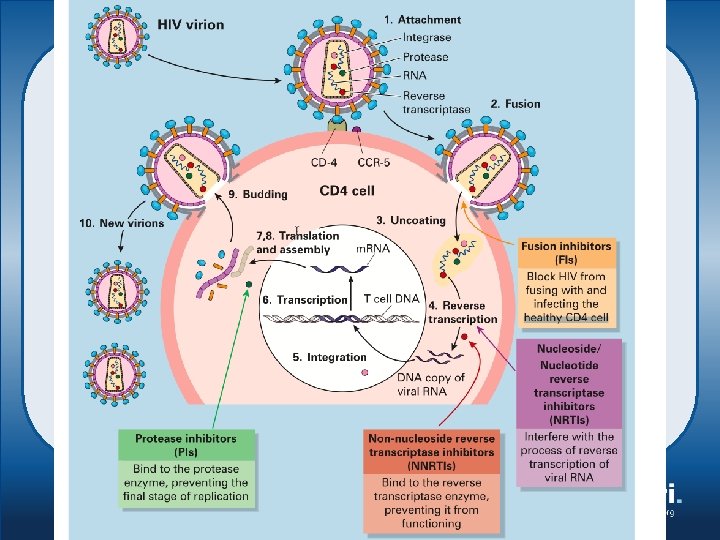
Objectives – To explain how the immune system works – To describe the role of the CD 4 cells within the immune system – To discuss the life cycle of the HIV virus – To describe the stages of HIV infection

The healthy body • Under attack everyday • Viruses, bacteria, funghi, protozoa • The body is protected by structures and processes that fight infection
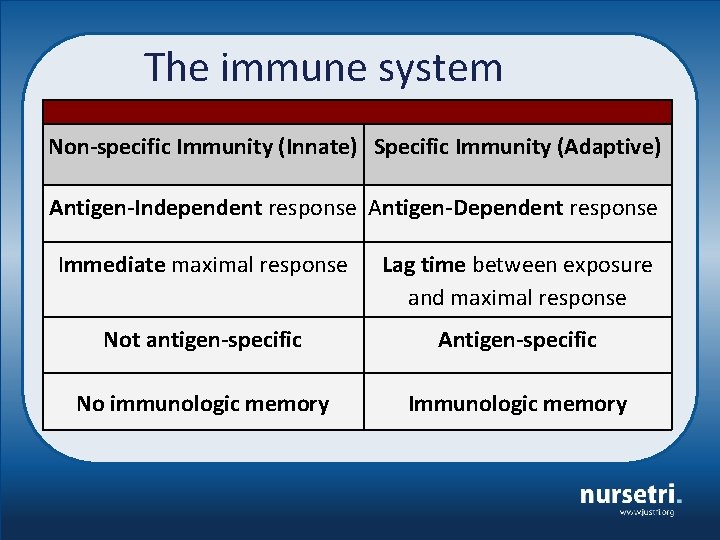
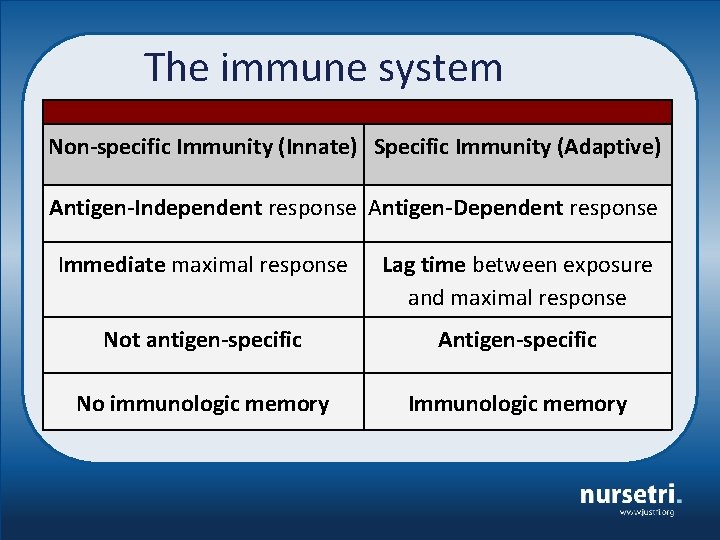
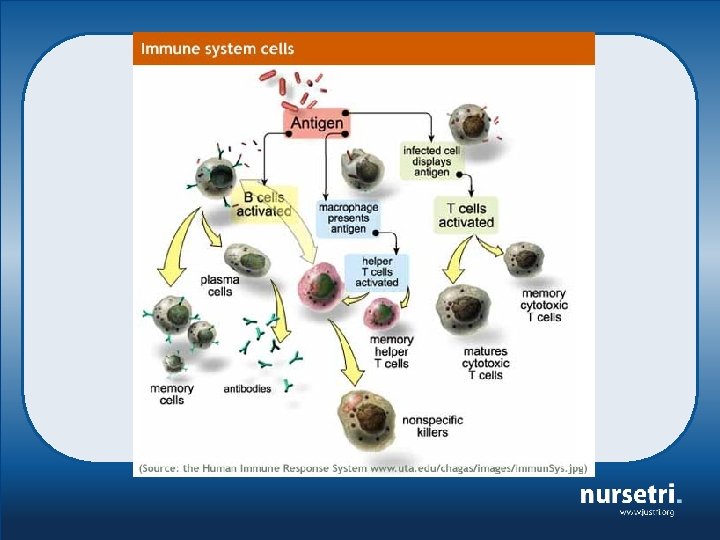
The immune system Non-specific Immunity (Innate) Specific Immunity (Adaptive) Antigen-Independent response Antigen-Dependent response Immediate maximal response Lag time between exposure and maximal response Not antigen-specific Antigen-specific No immunologic memory Immunologic memory
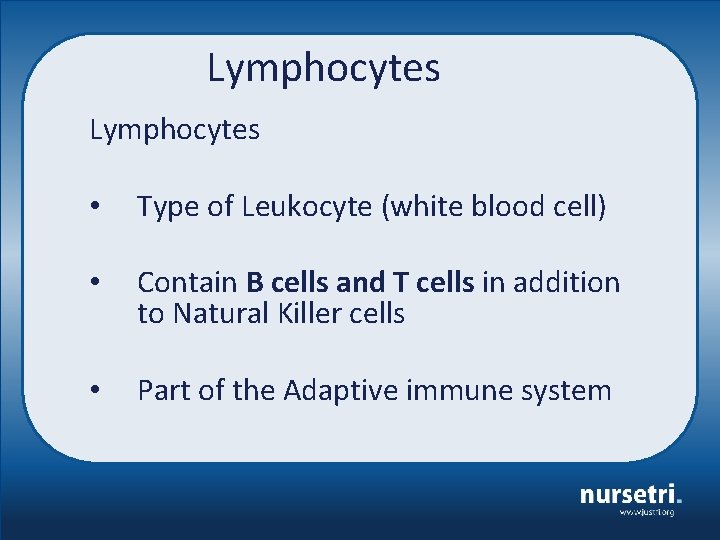
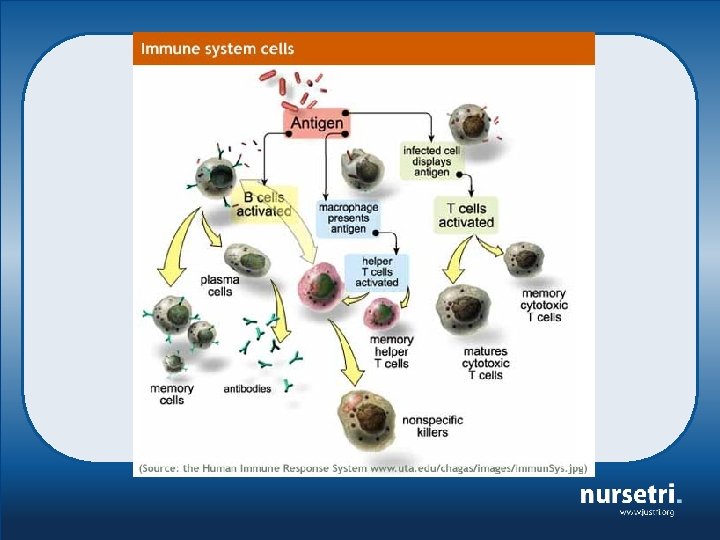
Lymphocytes • Type of Leukocyte (white blood cell) • Contain B cells and T cells in addition to Natural Killer cells • Part of the Adaptive immune system
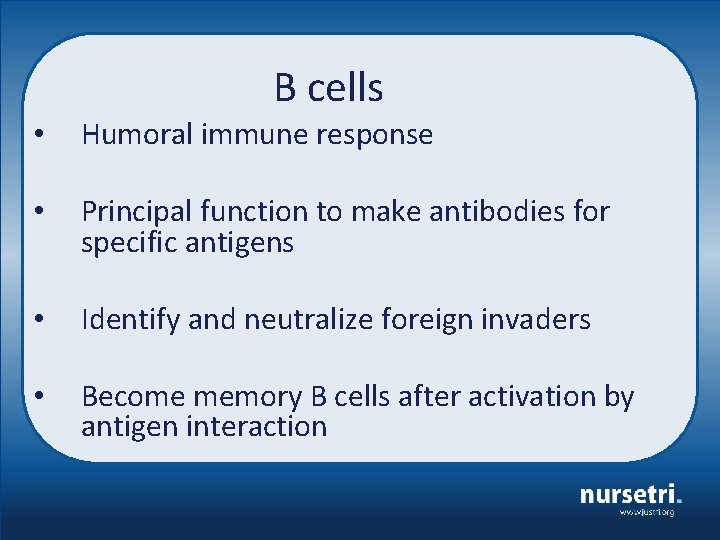
B cells • Humoral immune response • Principal function to make antibodies for specific antigens • Identify and neutralize foreign invaders • Become memory B cells after activation by antigen interaction
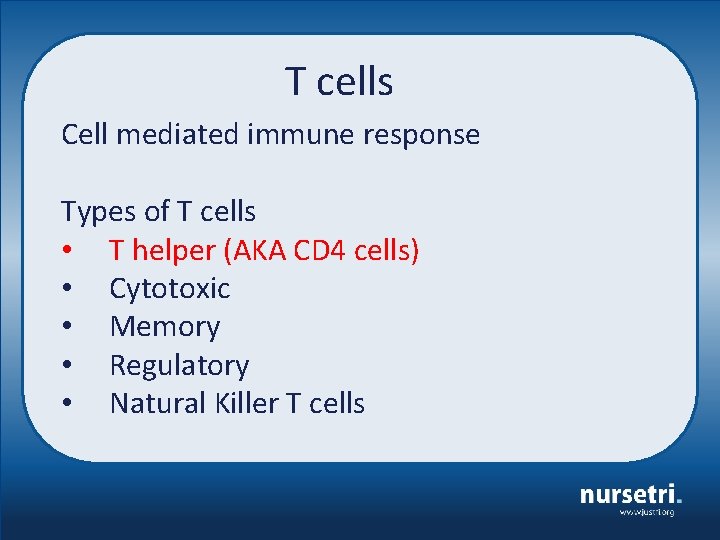
T cells Cell mediated immune response Types of T cells • T helper (AKA CD 4 cells) • Cytotoxic • Memory • Regulatory • Natural Killer T cells
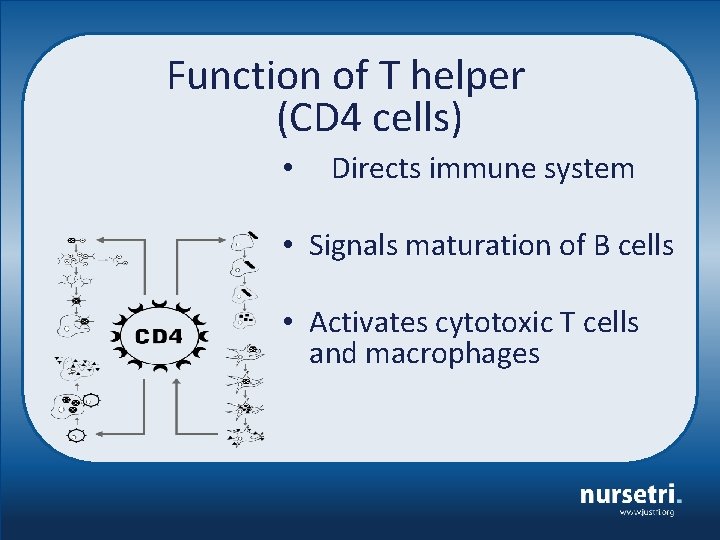
Function of T helper (CD 4 cells) • Directs immune system • Signals maturation of B cells • Activates cytotoxic T cells and macrophages

The Human Immunodeficiency Virus (HIV)
The virus Lentivirus type of Retrovirus Isolated in 1983 Called HIV in 1985 Related simian immunodeficieny virus (SIV) • HIV-1 and HIV-2 • Bushmeat or Hunter theory • •
Early history of HIV • Two samples from Kinshasa, Congo, 1959 and 1960 • 16 -year-old boy from Missouri USA who died in 1969 • Norwegian sailor who had been to Cameroon in 60’s died in 1976 • A Danish surgeon who travelled to Zaire in 1972, died in 1977 • Children involved in research in Uganda 1973

Stages of HIV infection • Primary HIV infection • Asymptomatic HIV infection • Symptomatic HIV infection • AIDS diagnosis
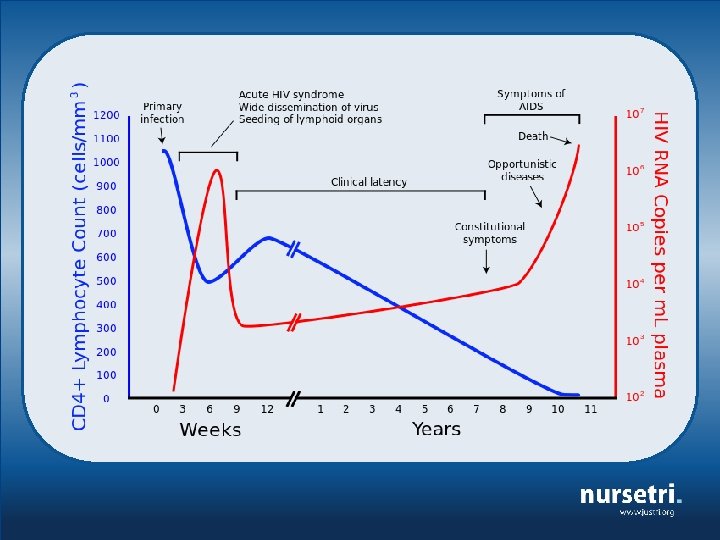
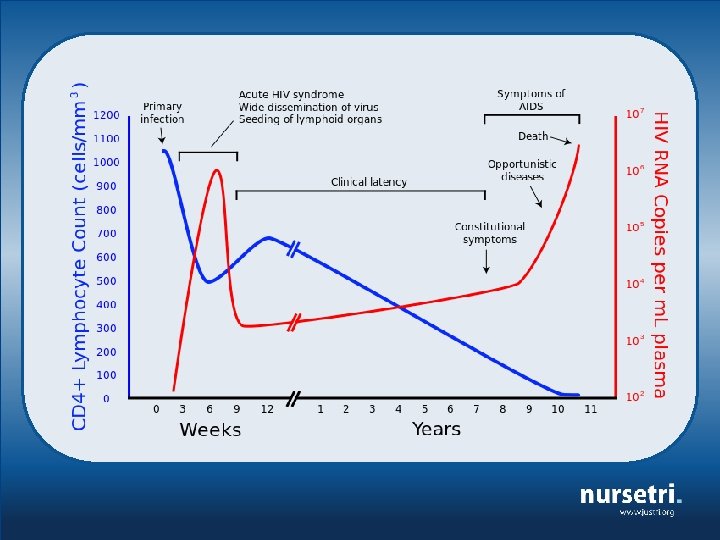
Primary HIV infection • Seroconversion illness • Fever, rash, sore throat, similar to glandular fever • Symptoms soon after exposure and usually lasts 2 weeks • 50 -90% have some degree of symptoms
Primary HIV infection • Inflammatory response • HIV-specific CD 4 cells are infected • Antibody tests are negative • Antigen positive • HIV viral load elevated
Primary HIV infection • HIV antibodies (within 6 wks but <3 mths) • Window period • High levels of HIV in blood, sexual fluids and/or breast milk. • Highly infectious!
Asymptomatic HIV infection • This stage lasts for an average of 7 to 10 years • Free from major symptoms (lymphadenopathy) • Viral load drops from seroconversion but remains infectious • HIV antibody positive • Not dormant, very active in the lymph nodes
Symptomatic HIV infection • Over time immune system becomes severely damaged • The lymph nodes and tissues become damaged • HIV mutates and becomes more pathogenic • CD 4 cells become depleted • Symptoms start mild and increase in severity • Emergence of opportunistic infections
Symptomatic HIV infection Unexplained weight loss Recurrent respiratory tract infections Herpes zoster Recurrent oral ulceration Rashes Fungal nail Unexplained chronic diarrhoea Unexplained persistent fever Persistent oral candidiasis Oral hairy leukoplakia Severe bacterial infections Gingivitis or periodontitis Unexplained anaemia
Progression to AIDS 1993 European AIDS case definition (used by Europe, Canada, Australia and Japan) ØHIV positive ØOne of the specified 28 Opportunistic illnesses (OIs) ØDoes not include CD 4 <200 without an OI
Opportunistic infections Called “opportunistic” because they take advantage of the weakened immune system. With healthy immune systems exposure to certain viruses, bacteria, or parasites cause no problems. These same bacteria and viruses cause great damage to a weakened immune system.

• § § § § § AIDS defining Pneumocystis jirovecii pneumonia Recurrent severe bacterial pneumonia Chronic herpes simplex infection Candidiasis: Esophageal, bronchi, trachea or lungs Extra pulmonary, disseminated tuberculosis Kaposi’s sarcoma Cytomegalovirus, disease and retinitis Encephalopathy, HIV related Herpes simplex, bronchitis, pneumonitis, esophagitis, chronic>1 mth Disseminated mycosis (extrapulmonary histoplasmosis, coccidiomycosis) Mycobacterium (avium complex, TB, kansasii, other) Progressive multifocal leukoencephalopathy Chronic cryptosporidiosis Chronic isosporiasis Lymphoma (cerebral, Burkitt’s, immunoblastic, non-Hodgkin) Salmonella (sepsis, recurrent) Toxoplasmosis (brain) Wasting syndrome Pneumonia (recurrent) Cervical cancer (invasive)